Abstract
Contact reduction is an effective strategy to mitigate the spreading of epidemic. However, the existing reaction–diffusion equations for infectious disease are unable to characterize this effect. Thus, we here propose an extended susceptible-infected-recovered model by incorporating contact rate into the standard SIR model, and concentrate on investigating its impact on epidemic transmission. We analytically derive the epidemic thresholds on homogeneous and heterogeneous networks, respectively. The effects of contact rate on spreading speed, scale and outbreak threshold are explored on ER and SF networks. Simulations results show that epidemic dissemination is significantly mitigated when contact rate is reduced. Importantly, epidemic spreads faster on heterogeneous networks while broader on homogeneous networks, and the outbreak thresholds of the former are smaller.
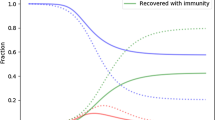
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Spreading of infectious diseases, such as the plague and coronavirus disease COVID-19 causes tremendous damages to human health and social societies. Therefore, how to accurately model the epidemic diffusion process, and to devise effective containment measures to prevent and control disease propagation is of great practical significance. Toward this end, mathematical modeling tools such as the mean-field theory and Markov chain approach have been developed into powerful analytical approaches to exploit propagation dynamics. In the field of epidemiology, epidemic models were originally based on uniformly mixed populations, in which each individual has equal frequency to interact with others. Nevertheless, in real-world social systems, interactions between different individuals are not evenly distributed. Moreover, each individual generally interacts with a limited number of others. Hence, many epidemic spreading systems can be properly described by complex networks whose nodes denote individuals, and edges connecting nodes represent interactions between them. Over the past few decades, spurred by the development of complex network theory and the availability of real epidemic dissemination data, there has been a growing body of investigations exploring propagation dynamics on the basis of complex networks [1,2,3,4,5,6,7,8].
In 1927, Kermack and McKendrick established the threshold theory for the diffusion of epidemic [9], on the basis of which they further built the SIR compartmental model, in which individuals in the population are divided into three classes: susceptible (S), infected (I) and recovered/removed (R), and each individual must be in one of these three states. The classic SIR (susceptible–infected–recovered/removed) model and SIS (susceptible–infected–susceptible) model are originally proposed by Reed and Frost in an unpublished paper in 1920, which is also a pioneering use of differential equations for the description of propagation dynamics [10, 11]. In the original network-based SIR model, it is assumed that the degree of each node is equal to the average degree \(\left\langle k \right\rangle \). However, such an assumption is incapable of characterize the real situation when the degree distribution of a network is broad. Thus, to precisely character the transmission process of epidemic on heterogeneous networks, Pastor-Satorras and Vespignani proposed the heterogeneous mean-field theory [7, 12], in which nodes on the network are subdivided according to their degrees. Here, the essence is that nodes with the same degrees are assumed to be in similar environments and have identical contagion dynamic characteristics.
Over the past few years, a variety of previous works have studied epidemic spreading on complex networks [13,14,15,16]. Especially, Moore et al. explored prediction of the speed of epidemic dissemination, and found an overall sudden transition from low density to almost full network saturation [13]. Moreover, it has been shown that community lockdowns in social networks hardly mitigate epidemic spreading [14]. Besides, Marko Gosak et al. investigated the endogenous social distancing and its underappreciated impact on the epidemic curve, and revealed that spreading similar in peak and case numbers could occur endogenously [15]. Hâncean et al. studied the role of age in the spreading of COVID-19 across a social network, which revealed that age is an important variable for predicting and understanding the spread of COVID-19 [16]. In addition, it is worth noting that the networked coevolution spreading in multilayered networks has generated considerable research interest [17,18,19]. In particular, Wang et al. gave a general overview of the recent progress in the study of coevolution spreading dynamics [17]. Furthermore, Matjaž Perc provided a broad overview of the diffusion dynamics and information spreading in multilayer networks [18]. In addition, Fan et al. proposed a new epidemic model on a two-layered network to illustrate the coupling spread between epidemic and information, which takes the role of simplicial complexes into consideration [19].
In the standard network-based SIR model [20], it is generally assumed that two nodes have close contact if there is a link between them, which is unable to characterize the impact of contact rate on epidemic spreading. Importantly, one of the most significant findings of epidemiology is that it is easiest for epidemic to spread when infectious individuals are in close contact with healthy ones for a long time. Moreover, there exists considerable evidence showing that although dissemination rates are highest in household and congregate settings, the risk of epidemic transmission through close, non-household social contact is also high [21,22,23,24]. Besides, previous studies have revealed that the risk of dissemination increases with the closeness and duration of contact with an individual infected COVID-19, and it is highest with prolonged contact in indoor settings [25,26,27]. In addition, it is worth stressing that Harris demonstrated that New York subway is an important medium for epidemic to transmit, at least it’s where many people are infected [28], which is due mainly to the close contact of individuals in the subway. Noteworthy, recent studies found that singing in close proximity [21], consuming communal food, sharing embraces, and face-to-face conversations [22], as well as going to restaurants and other drinking or eating establishments have been associated with a higher likelihood of infection [29, 30]. As specific examples of epidemic spreading which can be largely explained by close contact exposures, these findings directly motivated our modelling.
In this work, we propose an extended SIR model by integrating contact rate into the classic SIR model, and focus on exploring the spreading speed, scale and outbreak threshold of epidemic on homogeneous and heterogeneous networks. Simulations results show that contact reduction dramatically mitigate epidemic spreading. Remarkably, infectious disease spreads wider on homogeneous networks but faster on heterogeneous networks, and the outbreak thresholds of the latter are smaller.
This article is organized as follows. In Sect. 2, the proposed SIR model is theoretically analyzed in detail, and the outbreak thresholds of epidemic are respectively derived on homogeneous and heterogeneous networks. The numerical results and discussions are presented in Sect. 3. The findings are summarized in Sect. 4.
2 Model
In our model, \(\textit{S}(t)\), \(\rho (t)\) and \(\textit{R}(t)\) are used to represent the density of individuals in susceptible state, infectious state and recovered state at time step t. In the classic SIR model [10, 11], it is assumed that the cycle of epidemic spreading is much smaller than the lifespan of an individual, thus the death of individuals is not taken into consideration. Additionally, the number of nodes and links are assumed to be constant throughout the whole epidemic spreading process, that is, the propagation network is a static one. More explicitly, a susceptible individual is infected by any infective neighbors with a certain probability \({\lambda }\), and an infectious one recovers with rate \({\mu }\) and becomes recovery state of lifelong immunity.
2.1 Theoretical analysis on homogeneous networks
Firstly, we analyze the critical epidemic threshold on homogeneous networks, specifically, on an ER random network [31], the degree distribution of which exhibits Poisson distribution. We assume that each node has the same degree \(\left\langle k \right\rangle \), which is the average number of immediate neighbors of each node. Then the differential equations of SIR model on homogeneous networks can be represented as follows [12, 20, 32]:
where parameter \({\delta }\in [0,1]\) denotes the rate of a susceptible node physically contact an infective neighbor. In the real-world, contact rate is dramatically influenced by the suspension speed of work, self-isolation and the government’s epidemic prevention policy et al. The model will be reduced to the original SIR model when \(\delta =1\); otherwise, the impact of physical contact rate is incorporated into SIR model. It is worth stressing that an S-state node gets infected only if he has close contact with an infective neighbor, whereas, the recovery of an infectious one is a self-recovery process, and has no relation to contact with neighbors in other states.
In SIR model, the evolution process of node states is \({\textit{S}}\rightarrow {\textit{I}}\rightarrow {\textit{R}}\), or the nodes always keep in S-state. It is defined that \(\textit{S}_\infty =\lim _{\textit{t} \rightarrow \infty }S(t)\), \( \rho _\infty =\lim _{ t \rightarrow \infty } \rho (t)\), and \( R_\infty =\lim _{ t \rightarrow \infty }R(t)\). Thus, when \({\textit{t}} \rightarrow \infty \), \({ \rho _\infty } \rightarrow 0\), that is the infectious nodes will eventually become extinction. In other words, there are only susceptible and recovered nodes in population when the propagation process reaches the stationary state, thus \(\textit{S}_\infty + \textit{R}_\infty =1\). Additionally, to facilitate subsequent theoretical analysis, it is assumed that the time is continuous, then \(\textit{R}(t)=\mu \sum \nolimits _{t'=0}^{t}\rho _{t'}\approx \mu \int _{0}^{t}\rho (t')\textrm{d}t'\) can be obtained by integrating Eq. (3). From the above equations, the fraction of susceptible nodes can be obtained as:
Thus
where \(\textit{R}_\infty =0\) denotes the transmission range when epidemic spreading process reaches the steady-state. Obviously, \(\textit{R}_\infty =0\) is a common solution to Eq. (6) if the following conditions are satisfied, constructing a function as follows
Since \(f(1)<0\), then a none-zero solution exists for Eq. (7) if and only if \(\frac{\textrm{d}f({ R_\infty })}{\textrm{d}{ R_\infty }}|_{R_\infty =0}>0\), namely, \(\delta \lambda \left\langle k \right\rangle /\mu -1>0\Rightarrow \lambda >\mu /\delta \left\langle k \right\rangle \). In other words,
That is, when the infective probability \(\lambda \) is greater than \(\frac{\mu }{\delta \left\langle k \right\rangle }\), the epidemic will break out on homogeneous networks.
2.2 Theoretical analysis on heterogeneous networks
In most real-world situations, many networks display heterogeneous properties, such as the Internet and the world-wide-web. To better illustrate the epidemic diffusion process on heterogeneous networks, Pastor-Satorras and Vespignani proposed the mean-field equations for heterogeneous networks [7, 12], in which nodes with identical degrees are assumed to be in similar environments and follow the same kinetic laws. That is, the nodes in heterogeneous networks are further sorted into different categories depending on their degrees. After subdividing the network nodes by their degrees, the effects of different degrees on epidemic dissemination are taken into account. Thus, a new parameter \( \Theta (t)\) is introduced into the SIR model to characterize the corresponding impact. Here, the density of susceptible, infected and recovered nodes with degree k at time step t are represented by \( S_k(t)\), \( \rho _k(t)\) and \( R_k(t)\), respectively [33]. Therefore the mean-field equations for heterogeneous networks are [20]
where \( \Theta (t)\) denotes the rate that an edge of a given node with degree k is connected to an infectious node, which is defined as
where the conditional probability \(P(k'|k)\) represents the possibility that a node with degree k has a direct neighbor with degree \(\textit{k}'\), and \(\rho _{k'}(t)\) denotes the chance that the neighbor with degree \(\textit{k}'\) is an infected one.
From Eqs. (9)–(13), the density of susceptible nodes on heterogeneous networks can be obtained as
where the auxiliary function \( \varPhi (t)\) is defined as
The physical meaning of \( \varPhi (t)\) is the probability that the node at the other end of any given edge in the network is in R state at time step t.
By differentiating Eq. (15), and substituting \(\rho _k(t)\) by \(1- R_k(t)- S_k(t)\), it can be gained that
When the network dynamics reaches the stable state, namely, by setting \( t \rightarrow \infty \) in Eq. (16), \(\frac{ \textrm{d}\varPhi _\infty }{ \textrm{d}t}=0\), then a self-consistent equation for \( \varPhi (t)\) can be obtained as
Let \(f({\varPhi _\infty })=1-\frac{\sum \nolimits _kkP(k)e^{-\delta \lambda k \varPhi _\infty }}{\mu \left\langle k\right\rangle }- \varPhi _\infty \), since \(f(1)<0\), then a positive solution exists for Eq. (17) if and only if \(\frac{f({ \varPhi _\infty })}{\textrm{d}{\varPhi _\infty }}|_{{\varPhi }_\infty =0}>0\). That is \(\frac{\sum \nolimits _kkP(k)\delta \lambda \left\langle k\right\rangle }{\mu \left\langle k\right\rangle }=\delta \lambda \frac{\left\langle k^2\right\rangle }{\mu \left\langle k\right\rangle }>1\Rightarrow \lambda >\frac{\mu \left\langle k\right\rangle }{\delta \left\langle k^2\right\rangle }\). Thus, the threshold for epidemic spreading on heterogeneous networks can be acquired as
3 Numerical simulations
In the standard SIR epidemic, individuals in the population can be only in S and R states when propagation process reaches the stationary state. Consequently, the density of recovered individuals at the stable state and the outbreak threshold of epidemic are two primary quantities to be investigated. Besides, random networks and scale-free networks are classic homogeneous and heterogeneous networks, respectively. Thus, in this section we validate the effects of contact rate on epidemic spreading by carrying out Monte Carlo simulations (MCS) on ER random networks [31] and SF networks [34, 35], and each network holds \(5 \times 10^3\) nodes. In addition, to alleviate the influence of randomness, we run 100 simulations for each data spot.
3.1 Results on homogeneous networks
Fraction of infected individuals \(\rho (t)\) at each time step on ER random networks under different values of contact rate \(\delta \). a \(\left\langle k\right\rangle =10\). b \(\left\langle k\right\rangle =20\). Other parameters setup is \(\lambda =0.1\) and \(\mu =0.1\). Transmission speed is greatly accelerated with rising \(\delta \). Both \(\rho (t)\) and the corresponding critical value are increased when \(\left\langle k\right\rangle \) is risen
In SIR model, the evolution of fraction of infected individuals represents the transmission speed of epidemic. Hence, it is worthwhile to uncover the association between \(\rho (t)\) and \(\delta \) at each time step, as presented in Fig. 1. Notably, for fixed average degree \(\left\langle k\right\rangle \), greater \(\delta \) leads to earlier increase of \(\rho (t)\) and higher proportion of infected nodes, which implicates that the rise of contact rate promotes epidemic transmission. Moreover, both \(\rho (t)\) and the corresponding critical value are further increased when \(\left\langle k\right\rangle \) is risen. This is mainly due to the fact that larger average degree implies an individual having more chance to contact others, which leads to faster dissemination of epidemic.
Fraction of recovered individuals \(\textit{R}(t)\) at steady state on ER random networks as a function of \(\delta \) for distinct values of infectious rate \(\lambda \). a \(\left\langle k\right\rangle =10\), \(\mu =0.1\); b \(\left\langle k\right\rangle =20\), \(\mu =0.1\); c \(\left\langle k\right\rangle =10\), \(\mu =0.3\); d \(\left\langle k\right\rangle =20\), \(\mu =0.3\). Spreading range is increased with rising \(\delta \). The increase of recovery rate \(\mu \) inhibits epidemic dissemination
In order to investigate the impact of contact rate on spreading scale of epidemic, in Fig. 2, we explore the relationship between \(\textit{R}(t)\) and \(\delta \) under distinct infectious rate \(\lambda \) and recovery rate \(\mu \). Irrespective of average degree \(\left\langle k\right\rangle \) and recovery rate \(\mu \), the percentage of recovered individuals \(\textit{R}(t)\) reflects a sharp rise with the increase of parameter \(\delta \), indicating that contact rate plays an essential role in the dissemination range of epidemic. Furthermore, compared to the spreading scale when \(\left\langle k\right\rangle =10\), smaller \(\delta \) causes wider propagation range when \(\left\langle k\right\rangle =20\). Besides, larger contact rate is needed for the same transmission range when recovery rate \(\mu \) is risen from 0.1 to 0.3, which indicates that the increase of recovery rate inhibits the spread of epidemic.
Threshold of epidemic infection rate \(\lambda _c\) on ER random networks as a function of \(\delta \) for different values of recovery rate \(\mu \). a \(\left\langle k\right\rangle =10\); b \(\left\langle k\right\rangle =20\). Other parameter setup is \(\lambda =0.1\). It is easier for epidemic to transmit under greater \(\delta \). Higher transmission threshold can be observed for greater \(\mu \)
In Fig. 3, we examine the influence of contact rate on epidemic thresholds. For fixed recovery rate \(\mu \), the outbreak threshold of epidemic infection rate \(\lambda _c\) gradually decreases as the rise of \(\delta \), suggesting that greater contact rate leads to easier dissemination of epidemic. In addition, under the same values of \(\delta \), higher transmission threshold can be observed for greater value of \(\mu \), indicating that faster recovery mitigates epidemic spreading.
3.2 Results on heterogeneous networks
Fraction of infected individuals \(\rho (t)\) at each time step on SF networks under different values of contact rate \(\delta \). a \(\left\langle k\right\rangle =10\). b \(\left\langle k\right\rangle =20\). Other parameters setup is \(\lambda =0.1\) and \(\mu =0.1\). Compared with ER networks, smaller \(\delta \) causes epidemic propagation on SF networks
Fraction of recovered individuals \(\textit{R}(t)\) at stationary state on SF networks as a function of \(\delta \) for different values of infectious rate \(\lambda \). a \(\left\langle k\right\rangle =10\), \(\mu =0.1\); b \(\left\langle k\right\rangle =20\), \(\mu =0.1\); c \(\left\langle k\right\rangle =10\), \(\mu =0.3\); d \(\left\langle k\right\rangle =20\), \(\mu =0.3\). Compared to SF networks, smaller \(\delta \) results in wider transmission on ER networks
Threshold of epidemic infection rate \(\lambda _c\) on SF networks as a function of \(\delta \) for different values of recovery rate \(\mu \). a \(\left\langle k\right\rangle =10\); b \(\left\langle k\right\rangle =20\). Other parameter setup is \(\lambda =0.1\). Compared to ER networks, the epidemic threshold is smaller on SF networks
Finally, we investigate the impact of contact rate on diffusion speed, scale and outbreak threshold of epidemic on heterogeneous networks under the same setup of model parameters. Notably, compared to the simulation results on ER networks, smaller contact rate \(\delta \) is able to cause epidemic transmission on SF networks, which is demonstrated by the earlier increase of \(\rho (t)\) (as shown in Fig. 4). The main reason of this result is in heterogeneous networks, nodes with large degrees having more possibilities to disseminate epidemic to others. Moreover, wider transmission range on SF networks needs greater contact rate (as illustrated in Fig. 5). In addition, the epidemic threshold is smaller on heterogeneous networks (as shown in Fig. 6). These findings indicate that the heterogeneity of network accelerates epidemic spreading.
4 Conclusions
When an infectious disease spreads in the population, healthy individuals generally reduce contacts to stay healthy, and infected ones reduce contacts consciously to avoid infecting others. Most noteworthy, a considerable amount of works revealed that physical contact plays a significant role in the diffusion of epidemic [21, 22, 28,29,30]. Nevertheless, the existing epidemic models are incapable of characterizing this impact. To that effect, we present an extensive SIR model by introducing contact rate into the standard one. The critical epidemic thresholds are analytically derived on homogeneous and heterogeneous networks as a function of contact rate, infective rate and recovery rate. Furthermore, the effects of contact rate on spreading speed, scale, and outbreak threshold of epidemic are respectively studied on ER and SF networks. Simulation results show that contact reduction is an efficient approach to mitigate epidemic propagation. Notably, under the same setup of model parameters, epidemic spreads faster on heterogeneous networks but wider on homogeneous networks, and the outbreak thresholds of the former are smaller. Current findings are beneficial for us to understand the dissemination characteristic of real epidemic in populations.
In this work, it is assumed that the contact rates between different individuals are identical at each time step. However, in the real-world, the probabilities of physical contact between distinct individuals are generally different, that is, the exposure rate is heterogeneous. Moreover, prior studies have shown that the risk of spreading increases with the closeness and duration of contact with an infected individual [25,26,27]. Hence, in the future work, a more sophisticated SIR model taking into account the heterogeneity of contact rate, the closeness and duration of physical contact will be the focus of future investigations.
References
V. Colizza, R. Pastor-Satorras, A. Vespignani, Reaction–diffusion processes and metapopulation models in heterogeneous networks. Nat. Phys. 3(4), 276–282 (2007)
M. Kuperman, G. Abramson, Small world effect in an epidemiological model. Phys. Rev. Lett. 86(13), 2909 (2001)
R.M. May, A.L. Lloyd, Infection dynamics on scale-free networks. Phys. Rev. E 64(6), 066112 (2001)
Y. Moreno, M. Nekovee, A.F. Pacheco, Dynamics of rumor spreading in complex networks. Phys. Rev. E 69(6), 066130 (2004)
M. Nekovee, Y. Moreno, G. Bianconi et al., Theory of rumor spreading on complex social networks. Physica A 374(1), 457–470 (2007)
M.E. Newman, Spread of epidemic disease on networks. Phys. Rev. E 66(1), 016128 (2002)
R. Pastor-Satorras, A. Vespignani, Epidemic spreading in scale-free networks. Phys. Rev. Lett. 86(14), 3200 (2001)
D.H. Zanette, Dynamics of rumor propagation on small-world networks. Phys. Rev. E 65(4), 041908 (2002)
W.O. Kermack, A.G. McKendrick, A contribution to the mathematical theory of epidemics. Proc. Roy. Soc. Lond. 115(772), 700–721 (1927)
R.M. Anderson, R.M. May, Infectious Diseases of Humans: Dynamics and Control (Oxford University Press, New York, 1992)
N.T. Bailey, The Mathematical Theory of Infectious Diseases and its Applications (Charles Griffin & Company Ltd, Bucks, 1975)
R. Pastor-Satorras, A. Vespignani, Epidemic dynamics and endemic states in complex networks. Phys. Rev. E 63(6), 066117 (2001)
S. Moore, T. Rogers, Predicting the speed of epidemics spreading in networks. Phys. Rev. Lett. 124(6), 068301 (2020)
M. Gosak, M. Duh, R. Markovič et al., Community lockdowns in social networks hardly mitigate epidemic spreading. New J. Phys. 23(4), 043039 (2021)
M. Gosak, M.U.G. Kraemer, H.H. Nax et al., Endogenous social distancing and its underappreciated impact on the epidemic curve. Sci. Rep. 11(1), 1–10 (2021)
M.G. Hâncean, J. Lerner, M. Perc et al., The role of age in the spreading of COVID-19 across a social network in Bucharest. J. Complex Netw. 9(4), cnab026 (2021)
W. Wang, Q.H. Liu, J. Liang et al., Coevolution spreading in complex networks. Phys. Rep. 820, 1–51 (2019)
M. Perc, Diffusion dynamics and information spreading in multilayer networks: an overview. Eur. Phys. J. Spec. Top. 228(11), 2351–2355 (2019)
J. Fan, Q. Yin, C. Xia et al., Epidemics on multilayer simplicial complexes. Proc. Math. Phys. Eng. Sci. 478(2261), 20220059 (2022)
Y. Moreno, R. Pastor-Satorras, A. Vespignani, Epidemic outbreaks in complex heterogeneous networks. Eur. Phys. J. B 26, 521–529 (2002)
L. Hamner, High SARS-CoV-2 attack rate following exposure at a choir practice-Skagit County, Washington, March 2020. Morb. Mortal. Wkly. Rep. 69 (2020)
I. Ghinai, S. Woods, K.A. Ritger et al., Community transmission of SARS-CoV-2 at two family gatherings-Chicago, Illinois, February-March 2020. Morb. Mortal. Wkly. Rep. 69(15), 446 (2020)
R. Pung, C.J. Chiew, B.E. Young et al., Investigation of three clusters of COVID-19 in Singapore: implications for surveillance and response measures. Lancet 395(10229), 1039–1046 (2020)
P. Mahale, C. Rothfuss, S. Bly et al., Multiple COVID-19 outbreaks linked to a wedding reception in rural Maine-August 7–September 14, 2020. Morb. Mortal. Wkly. Rep. 69(45), 1686 (2020)
D.C. Adam, P. Wu, J.Y. Wong et al., Clustering and superspreading potential of SARS-CoV-2 infections in Hong Kong. Nat. Med. 26(11), 1714–1719 (2020)
R. Laxminarayan, B. Wahl, S.R. Dudala et al., Epidemiology and transmission dynamics of COVID-19 in two Indian states. Science 370(6517), 691–697 (2020)
K. Sun, W. Wang, L. Gao et al., Transmission heterogeneities, kinetics, and controllability of SARS-CoV-2. Science 371(6526), eabe2424 (2021)
J.E. Harris, The subways seeded the massive coronavirus epidemic in New York City. NBER (2020)
K.A. Fisher, M.W. Tenforde, L.R. Feldstein et al., Community and close contact exposures associated with COVID-19 among symptomatic adults \(\ge \) 18 years in 11 outpatient health care facilities-United States, July 2020. Morb. Mortal. Wkly. Rep. 69(36), 1258 (2020)
M.W. Tenforde, K.A. Fisher, M.M. Patel, Identifying COVID-19 risk through observational studies to inform control measures. JAMA 325(14), 1464–1465 (2021)
P. Erdos, On random graphs. Mathematicae 6, 290–297 (1959)
A. Barrat, M. Barthelemy, A. Vespignani, Dynamical Processes on Complex Networks (Cambridge University Press, Cambridge, 2008)
J.P. Gleeson, S. Melnik, J.A. Ward et al., Accuracy of mean-field theory for dynamics on real-world networks. Phys. Rev. E 85(2), 026106 (2012)
T. Britton, M. Deijfen, A. Martin-Löf, Generating simple random graphs with prescribed degree distribution. J. Stat. Phys. 124, 1377–1397 (2006)
M. Catanzaro, M. Boguná, R. Pastor-Satorras, Generation of uncorrelated random scale-free networks. Phys. Rev. E 71(2), 027103 (2005)
Acknowledgements
This work was supported by (i) Project supported by the National Natural Science Foundation of China (Grant no. 62062049); (ii) Gansu Provincial Science and Technology Plan Project, China (Grant no. 21ZD8RA008); (iii) The Special Funds for Guiding Local Scientific and Technological Development by the Central Government (Grant no. 22ZY1QA005); (iv) The Science and Technology Plan Project of Lanzhou City (Grant no. 2021-1-150).
Author information
Authors and Affiliations
Contributions
Conceptualization, H-YP; methodology, H-YP and G-HY; software, G-HY and Y-NH; validation, H-YP and Y-NH; writing—original draft, G-HY; writing—review and editing, H-YP and Y-NH. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pei, H., Yan, G. & Huang, Y. Impact of contact rate on epidemic spreading in complex networks. Eur. Phys. J. B 96, 44 (2023). https://doi.org/10.1140/epjb/s10051-023-00513-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1140/epjb/s10051-023-00513-2