Abstract
Analysis of pathological changes in the structural and functional organization of the pyriform cortex in mice of the 5xFAD line, which models the pathogenesis of Alzheimer’s disease, showed that at the age of 7 months there is an increased aggregation of β-amyloid peptide, neuronal death, disintegration of myelin sheaths of nerve fibers, agglutination of synaptic vesicles in synaptic endings and the appearance of a large number of autophagolysosomes in the bodies and processes of neurons. Also, in the pyriform cortex of such animals, foci of gliosis and an almost threefold increase in the content of the glial marker protein GFAP compared with wild type animals were found. All these changes were more pronounced than in the entorhinal cortex of 5xFAD mice that we had previously studied. Between the pyriform and entorhinal regions, a difference in the distribution of the amyloid-degrading metallopeptidase neprilysin (NEP) was also revealed. In the pyriform cortex, this enzyme is found mainly in the intercellular space, whereas in the entorhinal cortex, in the cell bodies. Moreover, in the entorhinal cortex of 5xFAD mice, the number of NEP-positive cells was 60% lower than in wild-type mice. 5xFAD mice also showed a significant deterioration in olfactory function, which was expressed in an almost twofold decrease in the effectiveness of the search for food by smell compared to wild-type mice. These findings suggest significant pathological changes in the pyriform and entorhinal cortex in 5xFAD mice caused by amyloid accumulation, which may cause a deterioration in their sense of smell, and similarly might cause impaired olfactory function in the development of Alzheimer’s disease.







Similar content being viewed by others
Abbreviations
- AD:
-
Alzheimer’s disease
- Аβ:
-
β-amyloid peptide
- GFAP:
-
glial fibrillary acidic protein
REFERENCES
Oakley HO, Cole SL, Logan S, Maus E, Shao P, Craft J, Guillozet-Bongaarts A, Ohno M, Disterhoft J, Van Eldik L, Berry R, Vassar R (2006) Intraneuronal β-amyloid aggregates, neurodegeneration, and neuron loss in transgenic mice with five familial Alzheimer’s disease mutations: Potential factors in amyloid plaque formation. J Neurosci 26: 10129-10140. https://doi.org/10.1523/JNEUROSCI.1202-06.2006
Mirzaei N, Tang SP, Ashworth S, Coello C, Plisson C, Passchier J, Selvaraj V, Tyacke RJ, Nutt DJ, Sastre M (2016) In vivo imaging of microglial activation by positron emission tomography with [(11)C]PBR28 in the 5XFAD model of Alzheimer’s disease. Glia 64: 993–1006. https://doi.org/10.1002/glia.22978
Eimer WA, Vassar R (2013) Neuron loss in the 5XFAD mouse model of Alzheimer’s disease correlates with intraneuronal Abeta42 accumulation and Caspase-3 activation. Mol Neurodegener 8: 2. https://doi.org/10.1186/1750-1326-8-2
Devi L, Ohno M (2010) Phospho-eIF2α level is important for determining abilities of BACE1 reduction to rescue cholinergic neurodegeneration and memory defects in 5XFAD mice. PLoS One 5: e12974. https://doi.org/10.1371/journal.pone.0012974
Shao CY, Mirra SS, Sait HB, Sacktor TC, Sigurdsson EM (2011) Postsynaptic degeneration as revealed by PSD-95 reduction occurs after advanced Aβ and tau pathology in transgenic mouse models of Alzheimer’s disease. Acta Neuropathol 122: 285–292. https://doi.org/10.1007/s00401-011-0843-x
Neuman KM, Molina-Campos E, Musial TF, Price AL, Oh KJ, Wolke ML, Buss EW, Scheff SW, Mufson EJ, Nicholson DA (2015) Evidence for Alzheimer’s disease-linked synapse loss and compensation in mouse and human hippocampal CA1 pyramidal neurons. Brain Struct Funct 220: 3143–3165. https://doi.org/10.1007/s00429-014-0848-z
Kimura R, Ohno M (2009) Impairments in remote memory stabilization precede hippocampal synaptic and cognitive failures in 5XFAD Alzheimer mouse model. Neurobiol Dis 33: 229–235. https://doi.org/10.1016/j.nbd.2008.10.006
Kanno T, Tsuchiya A, Nishizaki T (2014) Hyperphosphorylation of Tau at Ser396 occurs in the much earlier stage than appearance of learning and memory disorders in 5XFAD mice. Behav Brain Res 274: 302–306. https://doi.org/10.1016/j.bbr.2014.08.034
Murphy C (2019) Olfactory and other sensory impairments in Alzheimer disease. Nat Rev Neurol 15: 11–24. https://doi.org/10.1038/s41582-018-0097-5
Cai Y, Xue ZQ, Zhang XM, Li MB, Wang H, Luo XG, Cai H, Yan XX (2012) An age-related axon terminal pathology around the first olfactory relay that involves amyloidogenic protein overexpression without plaque formation. Neurosci 215: 160-73. https://doi.org/10.1016/j.neuroscience.2012.04.043
Gaudel F, Stephan D, Landel V, Sicard G, Féron F, Guiraudie-Capraz G (2018) Expression of the Cerebral Olfactory Receptors Olfr110/111 and Olfr544 Is Altered During Aging and in Alzheimer’s Disease-Like Mice. Mol Neurobiol 56: 2057–2072. https://doi.org/10.1007/s12035-018-1196-4
Tumanova NL, Vasilev DS, Dubrovskaya NM, Nalivaeva NN (2022) Morphofunctional changes in the brain tissue of 5xFAD transgenic mice. Cell Tiss Biol 64: 159–171. https://doi.org/10.31857/S0041377122020080
Nalivaeva NN, Turner AJ (2019) Targeting amyloid clearance in Alzheimer’s disease as a therapeutic strategy. Br J Pharmacol 176: 3447–3463. https://doi.org/10.1111/bph.14593
Nalivaeva NN, Zhuravin IA, Turner AJ (2020) Neprilysin expression and functions in development, ageing and disease. Mech Ageing Dev 192: 111363. https://doi.org/10.1016/j.mad.2020.111363
Vasilev DS, Dubrovskaya NM, Zhuravin IA, Nalivaeva NN (2021) Developmental Profile of Brain Neprilysin Expression Correlates with Olfactory Behaviour of Rats. J Mol Neurosci 71:1772–1785. https://doi.org/10.1007/s12031-020-01786-3
Vasilev D, Dubrovskaya NM, Nalivaeva NN (2022) Caspase Inhibition Restores NEP Expression and Rescues Olfactory Deficit in Rats Caused by Prenatal Hypoxia. J Mol Neurosci 72: 1516–1526. https://doi.org/10.1007/s12031-022-01986-z
Tumanova NL, Vasilev DS, Dubrovskaya NM, Nalivaeva NN, Zhuravin IA (2021) Effect of Prenatal Hypoxia on Cytoarchitectonics and Ultrustructural Organisation of Brain Regions Related to Olfaction in Rats. Cell Tiss Biol 15: 482–492. https://doi.org/10.1134/S1990519X21050114.
Vasilev DS, Dubrovskayaa NM, Tumanova NL, Nalivaeva NN (2022) Analysis of Expression of the Amyloid-Degrading Enzyme Neprilysin in Brain Structures of 5xFAD Transgenic Mice. J Evol Biochem Physiol 58: 193–203. https://doi.org/ 10.1134/S0022093022010173
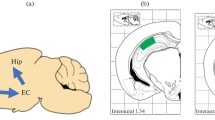
Paxinos G, Franklin KBJ (2001) The mouse brain in stereotaxic coordinates; 2nd Edition. Academic Press, San Diego. https://doi.org/10.1084/jem.20081588
Tumanova NL, Vasil’ev DS, Dubrovskaya NM, Zhuravin IA (2018) Ultrastructural alterations in the sensorimotor cortex upon delayed development of motor behavior in early ontogenesis of rats exposed to prenatal hypoxia. Cell Tiss Biol 12: 419–425. https://doi.org/10.1134/S1990519X18050097
Sun S, Li T, Davies H, Li W, Yang J, Li S, Ling S (2016) Altered Morphologies and Functions of the Olfactory Bulb and Hippocampus Induced by miR-30c. Front Neurosci 10: 207. https://doi.org/10.3389/fnins.2016.00207
De Castro F (2009) Wiring olfaction: The cellular and molecular mechanisms that uide the development of synaptic connections from the nose to the cortex. Front Neurosci 3: 50. https://doi.org/10.3389/neuro.22.004.2009
Schöll M, Carter SF, Westman E, Rodriguez-Vieitez E, Almkvist O, Thordardottir S, Wall A, Graff C, Långström B, Nordberg A (2015) Early astrocytosis in autosomal dominant Alzheimer’s disease measured in vivo by multi-tracer positron emission tomography. Sci Rep 5: 16404. https://doi.org/10.1038/srep16404
Rodriguez-Vieitez E, Ni R, Gulyás B, Tóth M, Häggkvist J, Halldin С, Voytenko L, Marutle A, Nordberg A (2015) Astrocytosis precedes amyloid plaque deposition in Alzheimer APPswe transgenic mouse brain: a correlative positron emission tomography and in vitro imaging study. Eur J Nucl Med Mol Imaging 42: 1119–1132. https://doi.org/10.1007/s00259-015-3047-0
Thal DR, Rub U, Orantes M, Braak H (2002) Phases of A β-deposition in the human brain and its relevance for the development of AD. Neurology 58: 1791–1800. https://doi.org/10.1212/WNL.58.12.1791
Mitrano DA, Houle SE, Pearce P, Quintanilla RM, Lockhart BK, Genovese BC, Schendzielos RA, Croushore EE, Dymond EM, Bogenpohl JW, Grau HJ, Smith Webb L (20210 Olfactory dysfunction in the 3xTg-AD model of Alzheimer’s disease. IBRO Neurosci Rep 10: 51–61. https://doi.org/10.1016/j.ibneur.2020.12.004
Melnik SA, Gladysheva OS, Krylov VN (2009) Age-related changes in the olfactory sensitivity of male mice to the smell of isovaleric acid. Sensory Systems 23: 151–155. (In Russ).
Son G, Yoo S-J, Kang S, Rasheed A, Jung DH, Park H, Cho B, Steinbusch HWM, Chang K-A, Suh Y-H, Moon C (2021) Region-specific amyloid-β accumulation in the olfactory system influences olfactory sensory neuronal dysfunction in 5xFAD mice. Alzheimers Res Ther 13: 4. https://doi.org/10.1186/s13195-020-00730-2
Djordjevic J, Jones-Gotman M, De Sousa K, Chertkow H (2008) Olfaction in patients with mild cognitive impairment and Alzheimer’s disease. Neurobiol Aging 29: 693–706. https://doi.org/10.1016/j.neurobiolaging.2006.11.014
Doty RL (2012) Olfactory dysfunction in Parkinson disease. Nat Rev Neurol 8: 329–339. https://doi.org/10.1038/nrneurol.2012.80
Lepousez G, Mouret A, Loudes C, Epelbaum J, Viollet C (2010) Somatostatin contributes to in vivo gamma oscillation modulation and odor discrimination in the olfactory bulb. J Neurosci 30: 870–875. https://doi.org/10.1523/JNEUROSCI.4958-09.2010
Nocera S, Simon A, Fiquet O, Chen Y, Gascuel J, Datiche F, Schneider N, Epelbaum J, Viollet C (2019) Somatostatin serves a modulatory role in the mouse olfactory bulb: Neuroanatomical and behavioral evidence. Front Behav Neurosci 13: 61. https://doi.org/10.3389/fnbeh.2019.00061
Dubrovskaya NM, Vasilev DS, Tumanova NL, Alekseeva OS, Nalivaeva NN (2022) Prenatal Hypoxia Impairs Olfactory Function in Postnatal Ontogeny in Rats. Neurosci Behav Physiol 52: 262–270. https://doi.org/10.1007/s11055-022-01233-3
Qing H, He G, Ly PTT, Fox CJ, Staufenbiel M, Cai F, Zhang Z, Wei S, Sun X, Chen C-H, Zhou W, Wang K, Song W (2008) Valproic acid inhibits Aβ production, neuritic plaque formation, and behavioral deficits in Alzheimer’s disease mouse models. J Exp Med 205: 2781–2789.
Belyaev ND, Nalivaeva NN, Makova NZ, Turner AJ (2009) Neprilysin gene expression requires binding of the amyloid precursor protein intracellular domain to its promoter: implications for Alzheimer disease. EMBO Rep 10: 94–100. https://doi.org/10.1038/embor.2008.222.
ACKNOWLEDGMENTS
The authors express their deep gratitude to the Center for collective use of scientific equipment for physiological, biochemical and molecular-biological research (CCU) of the IEPhB RAS.
Funding
The work was carried out with the financial support of the State Budget Assignment of I.M. Sechenov Institute of Evolutionary Physiology and Biochemistry of the Russian Academy of Sciences (No 075-00408-21-00).
Author information
Authors and Affiliations
Contributions
NLN: morphological studies, writing an article; DSV: morphological and immunohistochemical studies, statistical data processing, article editing; NMD: behavioral experiments and statistical data processing; NNN: data analysis, writing and editing the text of the article, general management of the work. The text and graphic images of the article are approved by all co-authors.
Corresponding author
Ethics declarations
COMPLIANCE WITH Ethical staNDARDS
All experiments were carried out in compliance with the international guidelines for work with experimental animals, the guidelines of the Russian Academy of Sciences (RAS) and approved by the Scientific Ethical Council of the Institute of Evolutionary Physiology and Biochemistry RAS.
Conflict of interests
Authors declare no conflict of interests.
Additional information
Translated by N. Nalivaeva
Russian Text © The Author(s), 2022, published in Rossiiskii Fiziologicheskii Zhurnal imeni I.M. Sechenova, 2022, Vol. 108, No. 8, pp. 997–1014https://doi.org/10.31857/S086981392208009X.
Rights and permissions
About this article
Cite this article
Tumanova, N.L., Vasilev, D.S., Dubrovskaya, N.M. et al. Neurodegenerative Changes in the Structural and Ultrastructural Organization in the Pyriform Cortex of 5xFAD Transgenic Mice. J Evol Biochem Phys 58, 1225–1239 (2022). https://doi.org/10.1134/S0022093022040251
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1134/S0022093022040251