Abstract
Widespread use of the next-generation sequencing (NGS) technologies revealed that a significant percentage of tumors in children develop as a part of monogenic hereditary diseases. Predisposition to the development of pediatric neoplasms is characteristic of a wide range of conditions including hereditary tumor syndromes, primary immunodeficiencies, RASopathies, and phakomatoses. The mechanisms of tumor molecular pathogenesis are diverse and include disturbances in signaling cascades, defects in DNA repair, chromatin remodeling, and microRNA processing. Timely diagnosis of tumor-associated syndromes is important for the proper choice of cancer treatment, genetic counseling of families, and development of the surveillance programs. The review describes the spectrum of neoplasms characteristic of the most common syndromes and molecular pathogenesis of these diseases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Most tumors arise as a result of accumulation of a critical number of somatic mutations affecting oncogenes and tumor suppressor genes in a single clone of cells. In some cases, high risk of developing neoplasms is inherited from the parents as a Mendelian trait. A number of familial tumor syndromes, i.e., diseases in which tumors are the main and only manifestation, are well known. As a rule, such conditions first appear in adults. Examples include hereditary non-polyposis colorectal cancer (Lynch syndrome), hereditary breast and ovarian cancer, familial medullary thyroid carcinoma, etc. These diseases are well studied; methods for their diagnosis, approaches to treatment, and preventive monitoring have been developed. At the same time, it becomes obvious that the increased risk of neoplasms is also characteristic of a number of hereditary diseases of childhood. The data obtained by high-throughput next-generation sequencing (NGS) indicate that about 10% of tumors in children arise on the background of hereditary defects associated with certain genetic syndromes [1-3].
The spectrum of neoplasms in children differs significantly from that in adults. While the latter have a predominance of solid tumors of epithelial origin, hematological tumors (leukemias and lymphomas), tumors of the brain and spinal cord (medulloblastoma, rhabdoid tumors, gliomas), blastomas (retinoblastoma, nephroblastoma, neuroblastoma) and sarcomas (osteosarcoma, Ewing’s sarcoma) are more often diagnosed in childhood [4]. These neoplasms can occur as a part of a wide range of hereditary diseases, including “classic” tumor syndromes, primary immunodeficiencies, phakomatoses, macrosomia syndromes, RASopathies, etc. Other characteristic features of the childhood tumors include a low tumor mutation burden (i.e., a relatively small number of mutations detected in tumor tissue), as well as increased frequency of somatic translocations leading to formation of the fusion proteins with oncogenic properties [5].
Various criteria for identifying children with oncological diseases who need further genetic testing for hereditary mutations have been proposed [6-8]. These include, in particular, detection of the primary multiple tumors, presence in a child of any tumor of the adult type (e.g., colon cancer, ovarian cancer), presence of facial dysmorphism or congenital malformations, developmental delay, growth disturbances, abnormal skin pigmentation, hematological disorders, immunodeficiency, as well as unusually severe toxicity during chemo- and/or radiation therapy. It is also believed that the presence of a tumor of some histological types (atypical teratoid rhabdoid tumor, medulloblastoma, hepatoblastoma, etc.) with high probability points to the hereditary defect [6, 9].
In some cases, the tumor subtype is quite clearly associated with certain hereditary diseases: for example, hypodiploid acute lymphoblastic leukemia is characteristic of Li–Fraumeni syndrome [2], and the Sonic Hedgehog (SHH) subtype of medulloblastoma is typical of Gorlin syndrome with SUFU mutations [10]. However, most types of tumors are not absolutely syndrome-specific. Thus, one of the most common childhood tumors, Wilms tumor (nephroblastoma), usually occurs sporadically, but can also be part of the clinical manifestations of a number of hereditary diseases [11, 12]. Syndromic forms of Wilms tumor include Beckwith–Wiedemann syndromes, WAGR (Wilms tumor, Aniridia, Genitourinary abnormalities, and mental Retardation), Denis–Drash, Fraser, Perlman, Simpson–Golabi–Behmel syndromes, Fanconi anemia; less commonly, this tumor occurs in the patients with Bloom, DICER1, Li–Fraumeni syndromes, Mulibray nanism, and PIK3CA-associated syndromes [12]. In 10% of isolated cases of Wilms’ tumor, hereditary mutations in the REST, CHEK1, EP300, PALB2, and ARID1A genes are detected [13].
CLASSIC TUMOR SYNDROMES
Retinoblastoma is a malignant tumor of the retina that arises from the primitive retinal stem cells or cone progenitors (Table 1). Observation of the patients with this disease allowed Alfred Knudson in 1971 to formulate the so-called “two-hit” hypothesis of tumorigenesis. According to him, two genetic events are required for the development of hereditary retinoblastoma: an inherited mutation of one allele (the first “hit”) followed by somatic inactivation of the other allele (the second “hit”) during retinal development. This hypothesis was brilliantly confirmed after the discovery of the RB1 gene in 1986 and demonstration of its biallelic inactivation in the tumor cells [14]. The protein is a negative regulator of the cell cycle with mutations leading to loss of function and uncontrolled cell proliferation [15]. The gene was the first tumor suppressor gene identified and served as an archetypal example of the role of such genes in tumorigenesis.
The Li–Fraumeni syndrome was described over 50 years ago. Over time, classical criteria for the syndrome were significantly supplemented: in particular, it turned out that the presence of a positive family history of early cancers or sarcomas is not critical [16]. At the same time, detection of the rare histologic varieties of pediatric tumors is of great diagnostic value (Table 1); the probability of detecting hereditary TP53 mutations is especially high in the case of adrenocortical carcinomas, choroid plexus carcinomas [17], and anaplastic rhabdomyosarcomas [18]. The p53 protein is the guardian of the genome: in response to DNA damage, it initiates transcription of numerous genes involved in the regulation of the cell cycle, DNA repair, apoptosis, and metabolism. Apparently, up to 1.5% of childhood tumors are associated with germline mutations in TP53 [3]; at the same time, interpretation of clinical significance of the hereditary variants of this gene is challenging due to the rather high population frequency and varying penetrance [16].
The Gorlin syndrome is caused by the hereditary mutations in the Patched1 (PTCH1) and Suppressor of fused (SUFU) genes associated with the SHH-mediated signaling cascade. The PTCH1 product is the receptor for SHH; binding of these molecules leads to the change in activity of Smo (smoothened). Normally, PTCH1 is a Smo repressor; in the case of mutation, a signaling complex consisting of Gli-1 (glioma-associated oncogene) and SUFU is activated. In tumors, loss of heterozygosity for the normal allele of SUFU and PTCH1 and activation of SHH signaling, leading, in particular, to inhibition of apoptosis, has been demonstrated [19].
Vast majority of the hereditary tumor syndromes have an autosomal dominant mode of inheritance. A few exceptions include constitutional mismatch repair deficiency (CMMRD) syndrome. It is known that the heterozygous mutations in the mismatch repair genes (MLH1, MSH2, MSH6, PMS2) cause colon and endometrial carcinomas in the structure of Lynch syndrome [20]. Biallelic lesions of these genes are much less common and are associated with the development of a wide range of tumors (primarily hematological and brain neoplasms) with a very early onset. Patients with café-au-lait spots on the skin, Lisch nodules on the iris, and neurofibromas make this disease similar to the type 1 neurofibromatosis. There is a certain association between the genotype and phenotype: for example, hematological tumors occur more often in children with MLH1 and MSH2 defects than in those with MSH6 and PMS2 mutations, while the latter are more likely to develop brain neoplasms [21].
The syndrome of predisposition to rhabdoid tumors is associated with mutations in the subunits of ATP-dependent chromatin-remodeling complex SWI/SNF (BAF) involved in cell differentiation and maintenance of stem cell pluripotency [22]. Obviously, the development of neoplasms is not associated with violation of the stability of the genome, since the rhabdoid tumors are characterized by an unusually low tumor mutation burden [23]. Considering that this complex interacts with the promoters of a huge number of genes, the mechanism of tumor formation is apparently not associated with any single signaling cascade, but rather is caused by epigenetic disturbances in transcriptional regulation [24].
The DICER1 gene associated with the wide range of benign and malignant childhood tumors plays an important role in protein translation. Its product is RNase (ribonuclease) III, which is required for microRNA (miRNA) production by cutting the pre-miRNA or double-stranded RNA. In turn, miRNAs, interacting with messenger RNAs (mRNAs), are involved in the regulation of expression of more than 30% of all protein-coding genes [25]. Most tumors arising in the structure of this syndrome result from combination of the hereditary loss-of-function mutation and acquired somatic missense mutation in one of the five “hot spots” of the RNase IIIb RNase domain [26]. In the patients with pleuropulmonary blastoma and other tumors, mosaicism in missense mutations in the same “hot spots” has also been described, and it is associated with more severe course of the disease, early onset, and formation of multiple primary tumors [27].
PRIMARY IMMUNODEFICIENCIES
Primary immunodeficiencies (PID) or inborn errors of immunity (IEI) are an extremely heterogeneous group of genetic defects of the immune system, leading to the increased incidence of infectious, oncological, and autoimmune complications [28, 29]. Up to 25% of children with primary immunodeficiencies suffer from malignant neoplasms [30]; moreover, cancer is the second leading cause of death in the PID patients after infections [31]. Often, development of a tumor is one of the first clinical manifestations of immunodeficiency. Approximately 60-70% of tumors that occur on the background of PID are represented by lymphomas and leukemias [32].
The risk of tumor development varies greatly depending on the specific form of PID [29]. High oncological risk is typical for the patients with impaired humoral (common variable immune deficiency, X-linked agammaglobulinemia) or cellular immunity (severe combined immune deficiency, X-linked lymphoproliferative syndrome, Wiskott–Aldrich syndrome), as well as with DNA repair defects. In most PID patients with tumor manifestations, the function of B-lymphocytes is impaired to varying degrees, while the T-cell function may be completely or partially intact. Existing data demonstrate that the patients with primary defects of antibody formation, as a rule, have the greatest number of functional capabilities necessary for the process of tumorigenesis (hallmarks of cancer) [33].
Despite unquestionable contribution of the compromised cancer immunosurveillance to the tumor development, the internal causes of oncological predisposition in the PID patients are not universal. These include various disturbances in the processes of differentiation, apoptosis, signaling interactions, metabolism and reorganization of the cytoskeleton of immune cells, as well as mechanisms responsible for chromosomal stability, telomere maintenance, and DNA repair [34, 35].
In addition, an important role is played by the disruption of protection against viruses. In particular, the Epstein–Barr virus (EBV) is involved in pathogenesis of a number of lymphoproliferative diseases, hematological tumors, and some carcinomas [36]. EBV has an increased affinity for B-lymphocytes, which explains predominance of the B-cell EBV-associated lymphomas. The Epstein–Barr virus triggers excessive proliferation of the antibody-producing B cells, followed by induction of the cellular immune response associated with cytotoxic T cells. Absence of the normal cytotoxic response leads to the EBV-mediated B cell proliferation. For example, in the X-linked lymphoproliferative syndrome, defect in the signaling lymphocyte-activating molecule (SLAM)-associated SAP protein results in severe impairment of the cytotoxic lymphocyte function, while the healthy EBV carriers are usually asymptomatic. Another form of the lymphoproliferative syndrome is associated with the hereditary defect in the XIAP gene. The product of this gene inhibits caspases, preventing cell apoptosis; dysfunction leads to the immune imbalance and chronic inflammation, mainly due to hyperexpansion of the virus-specific T-lymphocytes in response to EBV infection [37].
The Wiskott–Aldrich syndrome refers to the combined immunodeficiencies and is associated with mutations in the WAS gene. The product of this gene is involved in reorganization of the actin cytoskeleton, which is necessary for formation of immunological synapses, ensuring cytotoxicity of the natural killers (NK), chemotaxis, and chemokinesis [38].
An increased risk of tumor development in the case of DNA double-strand break repair defects is associated with the decrease in effectiveness of immune surveillance due to defects in the development of T- and B-cells, decrease in the diversity of the clonal repertoire, impaired proliferation of lymphocytes, transformation of B-cells, as well as their immortalization under the influence of EBV [39]. Direct induction of point mutations, translocations, and chromothripsis is also possible [40], which disrupts stability of the genome and increases likelihood of the malignant transformation.
Many PID types are associated with disruption of the important processes affecting T- and B-lymphocytes including V(D)J recombination, antibody class switching, and somatic hypermutation [41]. These events, involving endogenous generation and subsequent repair of the DNA double-strand breaks, are critical for normal development and maturation of the immune system.
In particular, V(D)J recombination is initiated by binding of RAG1 and RAG2 molecules to the signal sequences flanking the V, D, and J regions. The DNA double-strand breaks are formed with the ends stabilized by hairpin structures [42]. After phosphorylation by the catalytic subunit of the DNA–protein kinase complex (DNA–PKc), the Artemis protein, encoded by the DCLRE1C gene and having endonuclease activity, is involved in hairpin elimination [43]. Mutations that cause loss of the RAG1/2 or DCLRE1C function, interfering with normal development of T- and B-lymphocytes, are the cause of severe combined immunodeficiencies. Double-strand breaks are eliminated due to involvement of the proteins participating in non-homologous end-joining of DNA ends (Non-Homologous End-Joining, NHEJ), defects in some of the molecules involved in these processes (Artemis, DNA-PKcs, LIG4, Cernunnos) are also associated with some PID types.
Syndromes with chromosomal instability, primarily associated with recognition of the DNA double-strand breaks, deserve special attention [44]. The patients with ataxia–telangiectasia have the highest risk of neoplasms (Table 2): tumors are observed in 25% of the patients [45]. The ATM gene product serves as a sensor in recognition of the DNA double-strand breaks; mutations lead to the decrease in ability to activate the cell cycle checkpoints in response to exposure to ionizing radiation [46]. Leukemias and lymphomas are especially common; the risk of these diseases is tens and even hundreds of times higher than the population risk [47]. Unfortunately, prognosis for the development of tumors is usually very poor: while the average 5-year life expectancy in children with Hodgkin’s lymphoma exceeds 90%, the average survival of patients with ataxia–telangiectasia is about 3 months, regardless of the presence or absence of treatment [47, 48].
The Bloom syndrome (Table 2) is associated with biallelic mutations in the BLM gene, which encodes a protein of 1417 amino acids and belongs to the RecQ DNA helicase subfamily. The BLM protein plays an important role in maintaining genome stability by being a DNA damage sensor and recruiting other repair proteins to the site of the defect [49]. The BLM helicase ensures accuracy of homologous recombination by destroying Holliday junctions and thus preventing crossover between the sister chromatids [50]. In addition, it controls regression of the stopped replication fork [51]. Participation of BLM in maintaining the structure of telomeres has been described [52]. Impaired helicase function leads to the high level of homologous recombination of chromosomes. This is manifested as an increase in the non-sister chromatid exchange, elevation in the number of quadriradial configurations in the lymphocyte culture, and appearance of the chromosomal breaks and rearrangements, which can be detected during cytogenetic studies. Breast carcinomas associated with the BLM defect do not show loss of heterozygosity (LOH) of the BLM locus, which suggests development of the tumors by the mechanism of haploinsufficiency [53, 54].
The patients with Nijmegen breakage syndrome have a characteristic phenotype (short stature, “bird-like” face, microcephaly) and have severe impairment of humoral and cellular immunity [55]. The nibrin protein (NBN/NBS1) is a part of the MRE11-RAD50-NBS1 (MRN) complex, which plays an important role in response to the main types of cellular stress: DNA damage in the form of double-strand breaks, arrest of replication forks, telomere dysfunction, and viral invasion [56]. It is noteworthy that almost all the patients with Nijmegen syndrome are homozygous for the NBN c.657_661del allele, which occurs with high frequency in Eastern Europe, including Russia [57, 58]. Somatic loss of the normal allele seems to be uncharacteristic of the tumors developing in the carriers of NBN/NBS1 mutations [54, 59].
Patients with the Fanconi anemia have a variety of clinical manifestations, including short stature, skin spots, microcephaly, anomalies of the upper and lower extremities, and pancytopenia. High frequency of hematological and solid tumors is characteristic for those patients with acute myeloid leukemia being the most common [60]. The disease has very high genetic heterogeneity. More than 20 genes responsible for the development of Fanconi anemia have been described; vast majority of the cases are inherited in an autosomal recessive manner. Function of the Fanconi anemia proteins is associated with the repair of interstrand DNA cross-links that prevent replication, as well as with regulation of the cell cycle checkpoints and remodeling of replication forks in response to cellular stress [61]. Thus, disruption of these molecules leads to genome instability and promotes tumorigenesis.
It is noteworthy that the biallelic damage to the ATM, NBN, BLM, FANC genes is the direct cause of childhood genetic diseases combining infectious and tumor manifestations, while heterozygotes (carriers of mutations) are characterized by the increased risk of some solid tumors with late onset [62-65].
RASOPATHIES
RASopathies are a group of diseases associated with hyperactivation of the components of RAS/MAPK signaling cascade, which plays a key role in the cell growth, proliferation, differentiation, and apoptosis. RASopathies include autosomal dominant Noonan, Costello, cardiofaciocutaneous, and CBL syndromes, characterized by proportional short stature and specific facial dysmorphisms (Table 3).
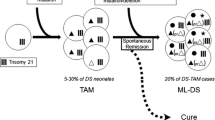
Increased oncological risk is by no means characteristic of all the diseases of this group. Up to 10% of the patients with Noonan syndrome suffer from a transient myeloproliferative disease in their childhood. In most cases, the condition resolves spontaneously, but some patients progress to juvenile myelomonocytic leukemia (JMML). Transition to leukemia is typical for the patients with PTPN11 and KRAS mutations, but not for those with defects in other genes [66]. The PTPN11 gene encodes the non-receptor tyrosine phosphatase SHP2. PTPN11 defects are the most common cause of Noonan syndrome; mutations, as a rule, lead to permanent activation of the catalytic PTP domain of SHP2, enhancing activity of the RAS/MAPK signaling cascade [67]. The KRAS mutations lead to activation of the same signaling cascade in two ways, either through reduced intrinsic or GAP-dependent GTPases activity or through changes in the affinity of guanine nucleotides for the RAS protein [68].
RASopathy also includes such common disease as type 1 neurofibromatosis associated with mutations in the NF1 gene. The product of this gene, neurofibromin, is a negative regulator of RAS; dysfunction leads to the reduced GTPase activity of the protein and, consequently, to the excessive activity of the GTP-bound proteins of RAS family [69].
SYNDROMES WITH MACROSOMIA
The Beckwith–Wiedemann syndrome is characterized by macrosomia, hemihyperplasia, macroglossia, and abdominal wall defects (Table 4). The most common cause of this syndrome is a disturbance of imprinting of the chromosome region 11p15.5; rarer are CDKN1C mutations affecting the maternal allele [70]. The patients are more than 600 times more likely to have nephroblastoma (Wilms tumor); also, they suffer from hepatoblastoma, and, less often, neuroblastoma, embryonic rhabdomyosarcoma, and tumors of the adrenal cortex [71].
Pathogenesis of the tumors is associated with the arrest of cell maturation in the specific cell populations during certain periods of embryonic development, i.e., with interruption of the normal nephrogenesis. Depending on the stage when the disorder occurred, nephroblastoma will contain different proportions of blastematous, epithelial, and stromal components. The highest risk of developing the Wilms tumor is characteristic of the variant of Beckwith–Wiedemann syndrome caused by hypermethylation of the imprinting center 1 (IC1) or uniparental disomy 11p15.5. As a result, expression of the insulin-like growth factor IGF2 is enhanced, followed by hyperactivation of the signaling cascade that promotes cell growth and proliferation [72]. At the same time, oncological risk in the patients with the Beckwith–Wiedemann syndrome associated with the loss of methylation of the imprinting center 2 (IC2) is significantly lower [73].
The X-linked Simpson–Golabi–Behmel syndrome is in many respects similar to the Beckwith–Wiedemann syndrome. Specific manifestations include hypertelorism, coarse facial features, and mental retardation. Pathogenesis is based on the defect in biosynthesis of the heparan sulfate proteoglycans on the cell surface. Functional role of the glypican-3 (product of the GPC3 gene) as a negative regulator of IGF2 and FGF2 expression has been shown [74]. The patients have the highest risk of Wilms tumor, but cases of other tumors (hepatoblastoma, hepatocellular carcinoma) have also been described [75].
Much less common is the Perlman syndrome, an autosomal recessive disorder associated with the DIS3L2 mutations. The product of this gene is a component of the exosome complex and, having the 3′-5′ exoribonuclease activity, regulates RNA processing and degradation [76]. The disease is characterized by very high perinatal mortality, and among the survivors, there is a high risk of Wilms tumor [77].
PHAKOMATOSES
Phakomatoses (from the Greek “phakos” – spot) or neurocutaneous dermatoses represent a group of diseases involving derivatives of the embryonic ectoderm, usually affecting skin and central nervous system (Table 5).
Tuberous sclerosis is a fairly common genetic disease characterized by the development of hamartomas of various organs (brain, kidneys, skin, heart, retina, lungs) and has an autosomal dominant mode of inheritance. The tuberous sclerosis genes, TSC1 and TSC2, are classic tumor suppressors. The hamartin protein (product of the TSC1 gene) in complex with tuberin (product of the TSC2 gene) are negative regulators of the mTOR-mediated signal transduction pathway that plays a critical role in regulating cell growth, size, shape, and proliferation. Mutations lead to the increase in activity of the mTORC1 complex, which, in turn, enhances protein translation, accelerates cell growth, enhances nucleotide synthesis, and reduces autophagy [78]. Observations obtained in relation to the tumors arising in the structure of tuberous sclerosis indicate that their pathogenesis fits into the “2-hit model” of carcinogenesis. In addition to the hereditary defect of the TSC1 or TSC2 genes, there is a deletion of the second intact allele in some somatic cells, which leads to formation of a tumor (hamartoma) of the corresponding organ [79, 80].
Neurofibromatosis type 2 is characterized by the development of bilateral vestibular schwannomas; few café-au-lait spots are observed on the skin of the patients. Pathogenesis is based on mutations in the NF2 gene encoding the merlin protein, which is involved in stabilization of cytoskeleton by inhibiting the PI3K/Akt, Raf/MEK/ERK, and mTOR signaling cascades [81]. Although the mechanism of tumor development is not entirely clear, the phenomenon of loss of heterozygosity at the NF2 locus has been demonstrated for the vestibular schwannomas and meningiomas [82].
TREATMENT
Knowledge of the molecular pathogenesis of childhood tumors is important in relation to several practical aspects. In particular, treatment of some neoplasms can be accompanied by the extremely pronounced toxicity or insensitivity to the treatment [4]. In addition, the ongoing drug or radiation therapy can induce development of the secondary tumors. This phenomenon has been described in the Li–Fraumeni syndrome [17, 83], retinoblastoma [84], and type 1 neurofibromatosis [85]. In the treatment of patients with DNA repair defects, such as Bloom’s syndrome, ataxia–telangiectasia, Fanconi’s anemia, Nijmegen’s syndrome, the reduced dosage of chemotherapy and exclusion of radiation therapy are recommended [86, 87]. Treatment of the tumors arising in the PID patients requires control of infections, such as pneumonia caused by Pneumocystis jirovecii [88].
In some cases, it has been possible to develop drugs targeting the key signaling pathways. Prominent examples are the MEK inhibitor selumetinib, used in the patients with neurofibromatosis type I [69], or everolimus, an mTOR inhibitor successfully applied in the treatment of tuberous sclerosis [89] and RASopathy [90].
Screening strategies for the tumor syndromes in children are being developed [91]. These measures are considered necessary if the chance of developing a childhood tumor exceeds 5% [92]. The results of observation of children with the Li–Fraumeni syndrome and Beckwith–Wiedemann syndrome demonstrate that early detection of the tumors leads to a significant improvement in overall survival [93, 94].
CONCLUSION
The study of tumors arising in the structure of hereditary syndromes makes it possible to expand the existing ideas about the causes of childhood neoplasms. Timely detection of the carriage of germinal mutations increases likelihood of early or even presymptomatic diagnosis, makes it possible to assess the risk of getting the disease in the relatives of the patients, and also stimulates development of the targeted therapy. A detailed description of the “molecular portraits” of tumors provides hope for the discovery of new prognostic and predictive markers contributing to personalization of the treatment. At the same time low tumor mutation burden generally characteristic of the childhood tumors indicates the need for a more meticulous study of the disturbances in epigenetic regulation processes, such as histone and CpG island methylation. Obviously, the prospects for studying pediatric neoplasms are associated with integration of the data obtained using genomic, transcriptomic, and epigenomic approaches.
Abbreviations
- EBV:
-
Epstein–Barr virus
- mTOR:
-
mammalian target of rapamycin
- MEK:
-
mitogen-activated ERK kinase
- PID:
-
primary immunodeficiencies
- RNase:
-
ribonuclease
- SHH:
-
Sonic Hedgehog
References
Parsons, D. W., Roy, A., Yang, Y., Wang, T., Scollon, S., et al. (2016) Diagnostic yield of clinical tumor and germline whole-exome sequencing for children with solid tumors, JAMA Oncol., 2, 616-624, https://doi.org/10.1001/jamaoncol.2015.5699.
Zhang, J., Walsh, M. F., Wu, G., Edmonson, M. N., Gruber, T. A., et al. (2015) Germline mutations in predisposition genes in pediatric cancer, N. Engl. J. Med., 373, 2336-2346, https://doi.org/10.1056/nejmoa1508054.
Gröbner, S. N., Worst, B. C., Weischenfeldt, J., Buchhalter, I., Kleinheinz, K., et al. (2018) The landscape of genomic alterations across childhood cancers, Nature, 555, 321-327, https://doi.org/10.1038/nature25480.
Kratz, C.P., Jongmans, M.C., Cavé, H., Wimmer, K., Behjati, S., et al. (2021) Predisposition to cancer in children and adolescents, Lancet Child Adolesc. Heal., 5, 142-154, https://doi.org/10.1016/S2352-4642(20)30275-3.
Filbin, M., and Monje, M. (2019) Developmental origins and emerging therapeutic opportunities for childhood cancer, Nat. Med., 25, 367-376, https://doi.org/10.1038/s41591-019-0383-9.
Jongmans, M. C. J., Loeffen, J. L. C. M., Waanders, E., Hoogerbrugge, P. M., Ligtenberg, M. J., Kuiper, R. P., and Hoogerbrugge, N. (2016) Recognition of genetic predisposition in pediatric cancer patients: an easy-to-use selection tool, Eur. J. Med. Genet., 59, 116-125, https://doi.org/10.1016/J.EJMG.2016.01.008.
Kesserwan, C., Friedman Ross, L., Bradbury, A. R., and Nichols, K. E. (2016) The advantages and challenges of testing children for heritable predisposition to cancer, Am. Soc. Clin. Oncol. Educ. B., 35, 251-269, https://doi.org/10.1200/EDBK_160621.
Goudie, C., Witkowski, L., Cullinan, N., Reichman, L., Schiller, I., et al. (2021) Performance of the McGill Interactive Pediatric OncoGenetic Guidelines for identifying cancer predisposition syndromes, JAMA Oncol., 7, 1806-1814, https://doi.org/10.1001/JAMAONCOL.2021.4536.
Postema, F. A. M., Hopman, S. M. J., Aalfs, C. M., Berger, L. P. V., Bleeker, F. E., et al. (2017) Childhood tumours with a high probability of being part of a tumour predisposition syndrome; reason for referral for genetic consultation, Eur. J. Cancer, 80, 48-54, https://doi.org/10.1016/j.ejca.2017.04.021.
Brugières, L., Remenieras, A., Pierron, G., Varlet, P., Forget, S., et al. (2012) High frequency of germline SUFU mutations in children with desmoplastic/nodular medulloblastoma younger than 3 years of age, J. Clin. Oncol., 30, 2087-2093, https://doi.org/10.1200/JCO.2011.38.7258.
Kulyova, S. A., and Imyanitov, E. N. (2017) Wilm’s tumor: syndrome-based and molecular diagnostics [in Russian], Onkopediatria, 4, 283-289, https://doi.org/10.15690/onco.v4i4.1814.
Treger, T. D., Chowdhury, T., Pritchard-Jones, K., and Behjati, S. (2019) The genetic changes of Wilms tumour, Nat. Rev. Nephrol., 15, 240-251, https://doi.org/10.1038/S41581-019-0112-0.
Gadd, S., Huff, V., Walz, A. L., Ooms, A. H. A. G., Armstrong, A. E., et al. (2017) A Children’s Oncology Group and TARGET initiative exploring the genetic landscape of Wilms tumor, Nat. Genet., 49, 1487-1494, https://doi.org/10.1038/ng.3940.
Friend, S. H., Horowitz, J. M., Gerber, M. R., Wang, X. F., Bogenmann, E., Li, F. P., and Weinberg, R. A. (1987) Deletions of a DNA sequence in retinoblastomas and mesenchymal tumors: organization of the sequence and its encoded protein, Proc. Natl. Acad. Sci. USA, 84, 9059-9063, https://doi.org/10.1073/PNAS.84.24.9059.
Mendoza, P. R., and Grossniklaus, H. E. (2015) The biology of retinoblastoma, Prog. Mol. Biol. Transl. Sci., 134, 503-516, https://doi.org/10.1016/BS.PMBTS.2015.06.012.
Frebourg, T., Bajalica Lagercrantz, S., Oliveira, C., Magenheim, R., Evans, D. G., European Reference Network GENTURIS (2020) Guidelines for the Li-Fraumeni and heritable TP53-related cancer syndromes, Eur. J. Hum. Genet., 28, 1379-1386, https://doi.org/10.1038/S41431-020-0638-4.
Bougeard, G., Renaux-Petel, M., Flaman, J. M., Charbonnier, C., Fermey, P., et al. (2015) Revisiting Li-Fraumeni syndrome from TP53 mutation carriers, J. Clin. Oncol., 33, 2345-2352, https://doi.org/10.1200/JCO.2014.59.5728.
Hettmer, S., Archer, N. M., Somers, G. R., Novokmet, A., Wagers, A. J., Diller, L., Rodriguez-Galindo, C., Teot, L. A., Malkin, D., et al. (2014) Anaplastic rhabdomyosarcoma in TP53 germline mutation carriers, Cancer, 120, 1068-1075, https://doi.org/10.1002/cncr.28507.
Foulkes, W. D., Kamihara, J., Evans, D. G. R., Brugières, L., Bourdeaut, F., Molenaar, J. J., Walsh, M. F., Brodeur, G. M., Diller, L., et al. (2017) Cancer surveillance in Gorlin syndrome and rhabdoid tumor predisposition syndrome, Clin. Cancer. Res., 23, e62-e67, https://doi.org/10.1158/1078-0432.CCR-17-0595.
Yanus, G. A., Akhapkina, T. A., Iyevleva, A. G., Kornilov, A. V., Suspitsin, E. N., et al. (2020) The spectrum of Lynch syndrome-associated germ-line mutations in Russia, Eur. J. Med. Genet., 63, 103753, https://doi.org/10.1016/j.ejmg.2019.103753.
Wimmer, K., Kratz, C. P., Vasen, H. F. A., Caron, O., Colas, C., et al. (2014) Diagnostic criteria for constitutional mismatch repair deficiency syndrome: suggestions of the European consortium “care for CMMRD” (C4CMMRD), J. Med. Genet., 51, 355-365, https://doi.org/10.1136/JMEDGENET-2014-102284.
Wilson, B. G., and Roberts, C. W. M. (2011) SWI/SNF nucleosome remodellers and cancer, Nat. Rev. Cancer, 11, 481-492, https://doi.org/10.1038/NRC3068.
Lee, R. S., Stewart, C., Carter, S. L., Ambrogio, L., Cibulskis, K., et al. (2012) A remarkably simple genome underlies highly malignant pediatric rhabdoid cancers, J. Clin. Invest., 122, 2983-2988, https://doi.org/10.1172/JCI64400.
Kim, K. H., and Roberts, C. W. M. (2014) Mechanisms by which SMARCB1 loss drives rhabdoid tumor growth, Cancer Genet., 207, 365-372, https://doi.org/10.1016/J.CANCERGEN.2014.04.004.
González, I. A., Stewart, D. R., Schultz, K. A. P., Field, A. P., Hill, D. A., and Dehner, L. P. (2022) DICER1 tumor predisposition syndrome: an evolving story initiated with the pleuropulmonary blastoma, Mod. Pathol., 35, 4-22, https://doi.org/10.1038/S41379-021-00905-8.
De Kock, L., Wu, M. K., and Foulkes, W. D. (2019) Ten years of DICER1 mutations: provenance, distribution, and associated phenotypes, Hum. Mutat., 40, 1939-1953, https://doi.org/10.1002/HUMU.23877.
Hill, D. A., Brenneman, M., Field, A., Williams, G., Doros, L., et al. (2015) Temporal order of RNase IIIb and loss-of-function mutations during development determines phenotype in pleuropulmonary blastoma /DICER1 syndrome: a unique variant of the two-hit tumor suppression model, F1000Res., 4, 214, https://doi.org/10.12688/F1000RESEARCH.6746.2.
Suspitsin, E. N., Guseva, M. N., Kostik, M. M., Sokolenko, A. P., Skripchenko, N. V., et al. (2020) Next-generation sequencing analysis of consecutive Russian patients with clinical suspicion of inborn errors of immunity, Clin. Genet., 98, 231-239, https://doi.org/10.1111/cge.13789.
Tiri, A., Masetti, R., Conti, F., Tignanelli, A., Turrini, E., Bertolini, P., Esposito, S., Pession, A., et al. (2021) Inborn errors of immunity and cancer, Biology (Basel), 10, 313, https://doi.org/10.3390/biology10040313.
Salavoura, K., Kolialexi, A., Tsangaris, G., and Mavrou, A. (2008) Development of cancer in patients with primary immunodeficiencies, Anticancer Res., 28, 1263-1269.
Mortaz, E., Tabarsi, P., Mansouri, D., Khosravi, A., Garssen, J., Velayati, A., and Adcock, I. M. (2016) Cancers related to immunodeficiencies: update and perspectives, Front. Immunol., 7, 365, https://doi.org/10.3389/fimmu.2016.00365.
Bomken, S., van der Werff Ten Bosch, J., Attarbaschi, A., Bacon, C. M., Borkhardt, A., et al. (2018) Current Understanding and future research priorities in malignancy associated with inborn errors of immunity and DNA repair disorders: the perspective of an Interdisciplinary Working Group, Front. Immunol., 9, 2912, https://doi.org/10.3389/fimmu.2018.02912.
Abolhassani, H., Wang, Y., Hammarström, L., and Pan-Hammarström, Q. (2021) Hallmarks of cancers: primary antibody deficiency versus other inborn errors of immunity, Front. Immunol., 12, 720025, https://doi.org/10.3389/FIMMU.2021.720025.
Hauck, F., Voss, R., Urban, C., and Seidel, M. G. (2018) Intrinsic and extrinsic causes of malignancies in patients with primary immunodeficiency disorders, J. Allergy Clin. Immunol., 141, 59-68.e4, https://doi.org/10.1016/j.jaci.2017.06.009.
Kebudi, R., Kiykim, A., and Sahin, M. K. (2019) Primary immunodeficiency and cancer in children; a review of the literature, Curr. Pediatr. Rev., 15, 245-250, https://doi.org/10.2174/1573396315666190917154058.
Shapiro, R. S. (2011) Malignancies in the setting of primary immunodeficiency: implications for hematologists/oncologists, Am. J. Hematol., 86, 48-55, https://doi.org/10.1002/AJH.21903.
Worth, A. J. J., Houldcroft, C. J., and Booth, C. (2016) Severe Epstein–Barr virus infection in primary immunodeficiency and the normal host, Br. J. Haematol., 175, 559-576, https://doi.org/10.1111/BJH.14339.
Notarangelo, L. D., and Ochs, H. D. (2003) Wiskott–Aldrich Syndrome: A model for defective actin reorganization, cell trafficking and synapse formation, Curr. Opin. Immunol., 15, 585-591, https://doi.org/10.1016/S0952-7915(03)00112-2.
Fournier, B., Mahlaoui, N., Moshous, D., and de Villartay, J. P. (2022) Inborn errors of immunity caused by defects in the DNA damage response pathways: Importance of minimizing treatment-related genotoxicity, Pediatr. Allergy Immunol., 33, e13820, https://doi.org/10.1111/PAI.13820.
Ratnaparkhe, M., Wong, J. K. L., Wei, P. C., Hlevnjak, M., Kolb, T., et al. (2018) Defective DNA damage repair leads to frequent catastrophic genomic events in murine and human tumors, Nat. Commun., 9, 4760, https://doi.org/10.1038/S41467-018-06925-4.
De Miranda, N. F. C. C., Björkman, A., and Pan-Hammarström, Q. (2011) DNA repair: The link between primary immunodeficiency and cancer, Ann. N. Y. Acad. Sci., 1246, 50-63, https://doi.org/10.1111/j.1749-6632.2011.06322.x.
Notarangelo, L. D., Kim, M. S., Walter, J. E., and Lee, Y. N. (2016) Human RAG mutations: biochemistry and clinical implications, Nat. Rev. Immunol., 16, 234, https://doi.org/10.1038/NRI.2016.28.
Felgentreff, K., Lee, Y. N., Frugoni, F., Du, L., van der Burg, M., et al. (2015) Functional analysis of naturally occurring DCLRE1C mutations and correlation with the clinical phenotype of ARTEMIS deficiency, J. Allergy Clin. Immunol., 136, 140-150.e7, https://doi.org/10.1016/j.jaci.2015.03.005.
Woodbine, L., Gennery, A. R., and Jeggo, P. A. (2014) The clinical impact of deficiency in DNA non-homologous end-joining, DNA Repair (Amst.), 16, 84-96, https://doi.org/10.1016/j.dnarep.2014.02.011.
Rothblum-Oviatt, C., Wright, J., Lefton-Greif, M. A., McGrath-Morrow, S. A., Crawford, T. O., and Lederman, H. M. (2016) Ataxia telangiectasia: a review, Orphanet J. Rare Dis., 11, 159, https://doi.org/10.1186/s13023-016-0543-7.
Shiloh, Y., and Ziv, Y. (2013) The ATM protein kinase: regulating the cellular response to genotoxic stress, and more, Nat. Rev. Mol. Cell Biol., 14, 197-210, https://doi.org/10.1038/nrm3546.
Sandoval, C., and Swift, M. (2003) Hodgkin disease in ataxia-telangiectasia patients with poor outcomes, Med. Pediatr. Oncol., 40, 162-166, https://doi.org/10.1002/mpo.10251.
Suarez, F., Mahlaoui, N., Canioni, D., Andriamanga, C., Dubois d’Enghien, C., Brousse, N., Jais, J. P., Fischer, A., Hermine, O., Stoppa-Lyonnet, D., et al. (2015) Incidence, presentation, and prognosis of malignancies in ataxia-telangiectasia: a report from the French national registry of primary immune deficiencies, J. Clin. Oncol., 33, 202-208, https://doi.org/10.1200/JCO.2014.56.5101.
Tikoo, S., and Sengupta, S. (2010) Time to bloom, Genome Integr., 1, 14, https://doi.org/10.1186/2041-9414-1-14.
Wu, L., and Hickson, I. O. (2003) The Bloom’s syndrome helicase suppresses crossing over during homologous recombination, Nature, 426, 870-874, https://doi.org/10.1038/nature02253.
Ralf, C., Hickson, I. D., and Wu, L. (2006) The Bloom’s syndrome helicase can promote the regression of a model replication fork, J. Biol. Chem., 281, 22839-22846, https://doi.org/10.1074/jbc.M604268200.
Bohr, V. A. (2008) Rising from the RecQ-age: the role of human RecQ helicases in genome maintenance, Trends Biochem. Sci., 33, 609-620, https://doi.org/10.1016/j.tibs.2008.09.003.
Sokolenko, A. P., Iyevleva, A. G., Preobrazhenskaya, E. V., Mitiushkina, N. V., Abysheva, S. N., et al. (2011) High prevalence and breast cancer predisposing role of the BLM c.1642 C>T (Q548X) mutation in Russia, Int. J. Cancer, 130, 2867-2873, https://doi.org/10.1002/ijc.26342.
Suspitsin, E. N., Yanus, G. A., Sokolenko, A. P., Yatsuk, O. S., Zaitseva, O. A., et al. (2014) Development of breast tumors in CHEK2, NBN/NBS1 and BLM mutation carriers does not commonly involve somatic inactivation of the wild-type allele, Med. Oncol., 31, 828, https://doi.org/10.1007/s12032-013-0828-9.
Wolska-Kuśnierz, B., Gregorek, H., Chrzanowska, K., Piątosa, B., Pietrucha, B., et al. (2015) Nijmegen Breakage Syndrome: clinical and immunological features, long-term outcome and treatment options – a retrospective analysis, J. Clin. Immunol., 35, 538-549, https://doi.org/10.1007/s10875-015-0186-9.
Syed, A., and Tainer, J. A. (2018) The MRE11-RAD50-NBS1 complex conducts the orchestration of damage signaling and outcomes to stress in DNA replication and repair, Annu. Rev. Biochem., 87, 263, https://doi.org/10.1146/ANNUREV-BIOCHEM-062917-012415.
Seemanova, E., Varon, R., Vejvalka, J., Jarolim, P., Seeman, P., et al. (2016) The Slavic NBN founder mutation: a role for reproductive fitness? PLoS One, 11, e0167984, https://doi.org/10.1371/journal.pone.0167984.
Sharapova, S. O., Pashchenko, O. E., Bondarenko, A. V., Vakhlyarskaya, S. S., Prokofjeva, T., et al. (2021) Geographical distribution, incidence, malignancies, and outcome of 136 Eastern Slavic patients with Nijmegen Breakage Syndrome and NBN founder variant c.657_661del5, Front. Immunol., 11, 602482, https://doi.org/10.3389/FIMMU.2020.602482.
Buslov, K. G., Iyevleva, A. G., Chekmariova, E. V., Suspitsin, E. N., Togo, A. V., et al. (2005) NBS1 657del5 mutation may contribute only to a limited fraction of breast cancer cases in Russia, Int. J. Cancer, 114, 585-589, https://doi.org/10.1002/ijc.20765.
Auerbach, A. D. (2009) Fanconi anemia and its diagnosis, Mutat. Res., 668, 4-10, https://doi.org/10.1016/j.mrfmmm.2009.01.013.
Badra Fajardo, N., Taraviras, S., and Lygerou, Z. (2022) Fanconi anemia proteins and genome fragility: unraveling replication defects for cancer therapy, Trends Cancer, 8, 467-481, https://doi.org/10.1016/J.TRECAN.2022.01.015.
Prokofyeva, D., Bogdanova, N., Dubrowinskaja, N., Bermisheva, M., Takhirova, Z., et al. (2012) Nonsense mutation p.Q548X in BLM, the gene mutated in Bloom’s syndrome, is associated with breast cancer in Slavic populations, Breast Cancer Res. Treat., 137, 533-539, https://doi.org/10.1007/s10549-012-2357-1.
Tavtigian, S. V., Oefner, P. J., Babikyan, D., Hartmann, A., Healey, S., et al. (2009) Rare, evolutionarily unlikely missense substitutions in ATM confer increased risk of breast cancer, Am. J. Hum. Genet., 85, 427-446, https://doi.org/10.1016/j.ajhg.2009.08.018.
Van Os, N. J. H., Roeleveld, N., Weemaes, C. M. R., Jongmans, M. C., Janssens, G. O., Taylor, A. M., Hoogerbrugge, N., and Willemsen, M. A. (2016) Health risks for ataxia-telangiectasia mutated heterozygotes: a systematic review, meta-analysis and evidence-based guideline, Clin. Genet., 90, 105-117, https://doi.org/10.1111/cge.12710.
Seemanová, E., Jarolim, P., Seeman, P., Varon, R., Digweed, M., Swift, M., and Sperling, K. (2007) Cancer risk of heterozygotes with the NBN founder mutation, J. Natl. Cancer Inst., 99, 1875-1880, https://doi.org/10.1093/jnci/djm251.
Kratz, C. P., and Izraeli, S. (2017) Down syndrome, RASopathies, and other rare syndromes, Semin. Hematol., 54, 123-128, https://doi.org/10.1053/J.SEMINHEMATOL.2017.04.008.
Liao, J., and Mehta, L. (2019) Molecular genetics of noonan syndrome and RASopathies, Pediatr. Endocrinol. Rev., 16 (Suppl 2), 435-446, https://doi.org/10.17458/per.vol16.2019.lm.molecularnoonan.
Riller, Q., and Rieux-Laucat, F. (2021) RASopathies: from germline mutations to somatic and multigenic diseases, Biomed. J., 44, 422, https://doi.org/10.1016/J.BJ.2021.06.004.
Walker, J. A., and Upadhyaya, M. (2018) Emerging therapeutic targets for neurofibromatosis type 1, Expert Opin. Ther. Targets, 22, 419-437, https://doi.org/10.1080/14728222.2018.1465931.
Choufani, S., Shuman, C., and Weksberg, R. (2013) Molecular findings in Beckwith–Wiedemann syndrome, Am. J. Med. Genet. C Semin. Med. Genet., 163C, 131-140, https://doi.org/10.1002/AJMG.C.31363.
Mussa, A., Molinatto, C., Baldassarre, G., Riberi, E., Russo, S., Larizza, L., Riccio, A., and Ferrero, G. B. (2016) Cancer risk in Beckwith–Wiedemann syndrome: a systematic review and meta-analysis outlining a novel (epi)genotype specific histotype targeted screening protocol, J. Pediatr., 176, 142-149.e1, https://doi.org/10.1016/J.JPEDS.2016.05.038.
Scott, R. H., Stiller, C. A., Walker, L., and Rahman, N. (2006) Syndromes and constitutional chromosomal abnormalities associated with Wilms tumour, J. Med. Genet., 43, 705-715, https://doi.org/10.1136/JMG.2006.041723.
Eggermann, T., Maher, E. R., Kratz, C. P., and Prawitt, D. (2022) Molecular basis of Beckwith–Wiedemann syndrome spectrum with associated tumors and consequences for clinical practice, Cancers (Basel), 14, 3083, https://doi.org/10.3390/cancers14133083.
Pan, Z., Chen, C., Long, H., Lei, C., Tang, G., Li, L., Feng, J., and Chen, F. (2013) Overexpression of GPC3 inhibits hepatocellular carcinoma cell proliferation and invasion through induction of apoptosis, Mol. Med. Rep., 7, 969-974, https://doi.org/10.3892/MMR.2013.1279.
DeBaun, M. R., Ess, J., and Saunders, S. (2001) Simpson Golabi Behmel syndrome: progress toward understanding the molecular basis for overgrowth, malformation, and cancer predisposition, Mol. Genet. Metab., 72, 279-286, https://doi.org/10.1006/MGME.2001.3150.
Astuti, D., Morris, M. R., Cooper, W. N., Staals, R. H., Wake, N. C., et al. (2012) Germline mutations in DIS3L2 cause the Perlman syndrome of overgrowth and Wilms tumor susceptibility, Nat. Genet., 44, 277-284, https://doi.org/10.1038/NG.1071.
Morris, M. R., Astuti, D., and Maher, E. R. (2013) Perlman syndrome: overgrowth, Wilms tumor predisposition and DIS3L2, Am. J. Med. Genet. C Semin. Med. Genet., 163C, 106-113, https://doi.org/10.1002/AJMG.C.31358.
Switon, K., Kotulska, K., Janusz-Kaminska, A., Zmorzynska, J., and Jaworski, J. (2017) Molecular neurobiology of mTOR, Neuroscience, 341, 112-153, https://doi.org/10.1016/j.neuroscience.2016.11.017.
Lam, H. C., Nijmeh, J., and Henske, E. P. (2017) New developments in the genetics and pathogenesis of tumours in tuberous sclerosis complex, J. Pathol., 241, 219-225, https://doi.org/10.1002/path.4827.
Martin, K., Zhou, W., Bowman, M., Shih, J., Au, K. S., et al. (2017) The genomic landscape of tuberous sclerosis complex, Nat. Commun., 8, 15816, https://doi.org/10.1038/ncomms15816.
Xiao, G. H., Chernoff, J., and Testa, J. R. (2003) NF2: the wizardry of merlin, Genes Chromosomes Cancer, 38, 389-399, https://doi.org/10.1002/GCC.10282.
Bachir, S., Shah, S., Shapiro, S., Koehler, A., Mahammedi, A., Samy, R. N., Zuccarello, M., Schorry, E., and Sengupta, S. (2021) Neurofibromatosis type 2 (NF2) and the implications for vestibular schwannoma and meningioma pathogenesis, Int. J. Mol. Sci., 22, 1-12, https://doi.org/10.3390/IJMS22020690.
Sherborne, A. L., Lavergne, V., Yu, K., Lee, L., Davidson, P. R., et al. (2017) Somatic and germline TP53 alterations in second malignant neoplasms from pediatric cancer survivors, Clin. Cancer Res., 23, 1852-1861, https://doi.org/10.1158/1078-0432.CCR-16-0610.
Kleinerman, R. A., Yu, C. L., Little, M. P., Li, Y., Abramson, D., Seddon, J., and Tucker, M. A. (2012) Variation of second cancer risk by family history of retinoblastoma among long-term survivors, J. Clin. Oncol., 30, 950-957, https://doi.org/10.1200/JCO.2011.37.0239.
Sharif, S., Ferner, R., Birch, J. M., Gillespie, J. E., Gattamaneni, H. R., Baser, M. E., and Evans, D. G. (2006) Second primary tumors in neurofibromatosis 1 patients treated for optic glioma: substantial risks after radiotherapy, J. Clin. Oncol., 24, 2570-2575, https://doi.org/10.1200/JCO.2005.03.8349.
Pastorczak, A., Szczepanski, T., and Mlynarski, W. (2016) Clinical course and therapeutic implications for lymphoid malignancies in Nijmegen breakage syndrome, Eur. J. Med. Genet., 59, 126-132, https://doi.org/10.1016/j.ejmg.2016.01.007.
Slack, J., Albert, M. H., Balashov, D., Belohradsky, B. H., Bertaina, A., et al. (2018) Outcome of hematopoietic cell transplantation for DNA double-strand break repair disorders, J. Allergy Clin. Immunol., 141, 322-328.e10, https://doi.org/10.1016/j.jaci.2017.02.036.
Tran, H., Nourse, J., Hall, S., Green, M., Griffiths, L., and Gandhi, M. K. (2008) Immunodeficiency-associated lymphomas, Blood Rev., 22, 261-281, https://doi.org/10.1016/j.blre.2008.03.009.
Luo, C., Ye, W. R., Shi, W., Yin, P., Chen, C., He, Y. B., Chen, M. F., Zu, X. B., and Cai, Y. (2022) Perfect match: mTOR inhibitors and tuberous sclerosis complex, Orphanet J. Rare Dis., 17, 106, https://doi.org/10.1186/S13023-022-02266-0.
Lodi, M., Boccuto, L., Carai, A., Cacchione, A., and Miele, E. (2020) Low-grade gliomas in patients with Noonan syndrome: case-based review of the literature, Diagnostics (Basel, Switzerland), 10, 582, https://doi.org/10.3390/DIAGNOSTICS10080582.
Al-Sarhani, H., Gottumukkala, R. V., Grasparil, A. D. S. 2nd, Tung, E. L., Gee, M. S., and Greer, M. C. (2020) Screening of cancer predisposition syndromes, Pediatr. Radiol., 52, 401-417, https://doi.org/10.1007/s00247-021-05023-w.
Brodeur, G. M., Nichols, K. E., Plon, S. E., Schiffman, J. D., and Malkin, D. (2017) Pediatric cancer predisposition and surveillance: an overview, and a tribute to Alfred G. Knudson Jr, Clin. Cancer Res., 23, e1-e5, https://doi.org/10.1158/1078-0432.CCR-17-0702.
McNeil, E. D., Brown, M., Ching, A., and Debaun, M. R. (2001) Screening for Wilms tumor and hepatoblastoma in children with Beckwith–Wiedemann syndromes: a cost-effective model, Med. Pediatr. Oncol., 37, 349-356, https://doi.org/10.1002/mpo.1209.
Villani, A., Shore, A., Wasserman, J. D., Stephens, D., Kim, R. H., et al. (2016) Biochemical and imaging surveillance in germline TP53 mutation carriers with Li-Fraumeni syndrome: 11-year follow-up of a prospective observational study, Lancet Oncol., 17, 1295-1305, https://doi.org/10.1016/S1470-2045(16)30249-2.
Funding
The work was financially supported by the Russian Science Foundation, grant no. 22-45-08004.
Author information
Authors and Affiliations
Contributions
E.N.S. wrote the manuscript; E.N.I. edited the manuscript.
Corresponding author
Ethics declarations
The authors declare no conflicts of interest in financial or any other sphere. This article does not contain any studies involving human participants or animals performed by any of the authors.
Rights and permissions
Open access. This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution, and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit https://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Suspitsin, E.N., Imyanitov, E.N. Hereditary Conditions Associated with Elevated Cancer Risk in Childhood. Biochemistry Moscow 88, 880–891 (2023). https://doi.org/10.1134/S0006297923070039
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1134/S0006297923070039