Abstract
To date, the best obesity-related indicators (ORIs) for predicting hypertension, dyslipidaemia, Type 2 diabetes mellitus (T2DM) and multimorbidity are still controversial. This study assessed the ability of 17 ORIs [body mass index (BMI), body fat percentage (BF%), c-index, Clínica Universidad de Navarra-Body Adiposity Estimator (CUN-BAE), a body shape index (ABSI), body adiposity index (BAI), waist circumference (WC), waist-hip ratio (WHR), waist-to-height ratio (WHtR), body roundness index (BRI), abdominal volume index (AVI), triglyceride glucose index (TYG), lipid accumulation product (LAP), visceral adiposity index (VAI), Chinese visceral adiposity index (CVAI), waist triglyceride index (WTI) and cardiometabolic index (CMI)] to predict hypertension, dyslipidemia, T2DM, and multimorbidity in populations aged 40–69 years. From November 2017 to December 2022, 10,432 compliant residents participated in this study. Receiver operating characteristic curves were used to assess the ability of ORIs to predict target diseases across the whole population and genders. The DeLong test was used to analyse the heterogeneity of area under curves (AUCs). Multivariable logistic regression was used to analyse the association of ORIs with hypertension, dyslipidaemia, T2DM, and multimorbidity. The prevalence of hypertension, dyslipidaemia, T2DM, and multimorbidity was 67.46%, 39.36%, 12.54% and 63.58%, respectively. After excluding ORIs associated with the target disease components, in the whole population, CVAI (AUC = 0.656), BMI (AUC = 0.655, not significantly different from WC and AVI), CVAI (AUC = 0.645, not significantly different from LAP, CMI, WHR, and WTI), and TYG (AUC = 0.740) were the best predictor of hypertension, dyslipidemia, T2DM, and multimorbidity, respectively (all P < 0.05). In the male population, BF% (AUC = 0.677), BMI (AUC = 0.698), CMI (AUC = 0.648, not significantly different from LAP and CVAI), and TYG (AUC = 0.741) were the best predictors (all P < 0.05). In the female population, CVAI (AUC = 0.677), CUN-BAE (AUC = 0.623, not significantly different from BF%, WC, WHR, WHtR, BRI and BMI), CVAI (AUC = 0.657, not significantly different from WHR), TYG (AUC = 0.740) were the best predictors (all P < 0.05). After adjusting for all covariates, all ORIs were significantly associated with hypertension, dyslipidaemia, T2DM, and multimorbidity (all P < 0.05), except for ABSI and hypertension and BAI and T2DM, which were insignificant. Ultimately, after considering the heterogeneity of prediction of ORIs among different populations, for hypertension, BF% was the best indicator for men and CVAI for the rest of the population. The best predictors of dyslipidaemia, T2DM, and multimorbidity were BMI, CVAI and TYG, respectively. Screening for common chronic diseases in combination with these factors may help to improve the effectiveness.
Similar content being viewed by others
Introduction
Since 2016, chronic diseases have accounted for more than 70% of all deaths worldwide1,2, and cardiovascular diseases (CVDs) are one of the major components. It has been reported that from 1990 to 2019, the number of people with CVDs rose from 271 to 523 million globally. The number of related deaths rose from 12.1 million to 18.6 million, with ischemic heart disease and stroke being the most prominent3. In 2019, there were 101 million cases of stroke and 197 million cases of ischemic heart disease worldwide3,4. In the same year, China had 3.94 million new cases of stroke and 28.76 million prevalent cases of it5. During this period, stroke incidence, prevalence and mortality increased by 70.0%, 85.0% and 43.0%, respectively globally, and by 80.6%, 106.0% and 32.3%, respectively, in China4,5, indicating that CVDs is a severe threat to the health of the global population.
Hypertension, hyperlipidemia, diabetes mellitus, and obesity are modifiable metabolic risk factors for CVDs6,7. In a study involving 47,262 participants from 12 provinces in China, 25% of CVDs were attributable to hypertension, 7.8% to elevated cholesterol, and 6.9% to abdominal obesity8. Another study of Chinese people showed that obesity was one of the strongest predictors of high CVD risk9. Ferket et al.10 pointed out that patients with diabetes have a higher lifetime risk of CVDs than those without diabetes. The American Heart Association also called for obesity to be classified as one of the risk factors for coronary heart disease11. Meanwhile, clustering metabolic risk factors would further increase the risk of CVDs12,13. Based on the above evidence, early identification and intervention in high-risk groups can effectively prevent the onset, duration of action and progression of CVDs, significantly reducing the burden of diseases.
Obesity is a disorder characterized by excessive fat and includes generalized and central/visceral obesity. It is well known that excessive adiposity (especially central obesity) independently worsens most of the metabolic risk factors for CVDs, such as triggering dyslipidemia, elevated blood pressure, elevated blood glucose, insulin resistance and inflammation6. As a result, obesity is increasingly being used to identify people at risk for cardiovascular risk factors (CRFs).
Magnetic resonance imaging (MRI) and computed tomography (CT) are standard means of assessing obesity, but their application is limited by being expensive and time-consuming14. Numerous studies have confirmed that obesity-related indicators (ORIs), represented by body mass index (BMI) and waist circumference (WC), can effectively predict CRFs and are highly sought after because of their simplicity and affordability15,16. However, there are some shortcomings in their description of fat distribution. For example, BMI cannot distinguish between adiposity and lean body mass or identify fat distribution15,16. WC does not take height into account15,16,17. As a result, researchers have been working to develop new ORIs to reduce their bias in predicting CRFs.
Along with the research, body fat percentage (BF%), c-index (CI), Clínica Universidad de Navarra-Body Adiposity Estimator (CUN-BAE), waist-hip ratio (WHR), waist-to-height ratio (WHtR), a body shape index (ABSI), body roundness index (BRI), body adiposity index (BAI), abdominal volume index (AVI), triglyceride glucose index (TYG), lipid accumulation product (LAP), visceral adiposity index (VAI), Chinese visceral adiposity index (CVAI), waist triglyceride index (WTI) and cardiometabolic index (CMI) have been proposed one after another. BF% is proven to be a better predictor of type 2 diabetes mellitus (T2DM) than BMI18. CI is considered an independent risk factor for all-cause mortality in non-cancerous older adults in China19. CUN-BAE has been shown to be one of the value indicators for assessing body fat mass and metabolic syndrome (Mets)20,21. Previous studies have shown that CUN-BAE, WHR, WHtR, ABSI, BRI, BAI, and AVI are good predictors of hypertension or Mets14,16,21. TYG, LAP, VAI, CVAI, WTI and CMI are constructed from traditional ORIs and clinical indicators, including fasting plasma glucose (FPG), triglyceride (TG) and high-density lipoprotein cholesterol (HDL-C). TYG, LAP, VAI and CVAI are essential in identifying Mets, T2DM, hypertension, and CVDs14,22,23,24,25,26,27. Besides, both WTI and CMI can be used as markers for Mets28,29,30.
These indicators have shown discriminatory power in identifying CVDs or CRFs. However, the best indicators remain controversial due to differences between subjects regarding socio-demographic characteristics, cultural background, or the confounding variables included for consideration. In addition, it has been suggested that ORIs can also be used to identify multimorbidity31,32, but research in this area needs to be more extensive. Therefore, this study aimed to evaluate the ability of 17 ORIs to predict CRFs (hypertension, hyperlipidemia and T2DM) and multimorbidity in people aged 40–69 years from Southeast China. Meanwhile, we wanted to identify the most efficient indicators with their optimal cut-off points.
Material and methods
Study design and participants
The data used for the analysis in this study are mainly from baseline data of The National Cohort of Esophageal Cancer-Prospective Cohort Study of Esophageal Cancer and Precancerous Lesions based on High-Risk Population (NCEC-HRP) implemented in Yangzhong City33.
In brief, since June 2017, the NCEC-HRP has officially selected eight screening centres in seven provinces in China to invite local residents aged 40–69 years in rural areas with a high incidence of esophageal cancer (EC) to undergo endoscopy, epidemiological surveys, clinical diagnosis, and follow-up. The aim is to achieve early diagnosis and treatment of EC while establishing an open-sharing platform for epidemiological databases and biobanks33. Yangzhong City was included in the project as it is one of the areas with a high incidence of gastric cancer (GC) and EC33,34,35. Yangzhong City also undertakes a population-based screening program for upper gastrointestinal cancer (UGC, GC/EC) as part of the National Cancer Screening Programme, which targets the same residents in rural areas (townships or villages) with a high incidence of UGC. The program aims to reduce the incidence and mortality of UGC by using endoscopic screening and pathological diagnostic techniques to identify patients with early-stage cancer or precancerous lesions and to intervene or follow up on them34,35. The two programs were completed in collaboration with each other in practice. Details of the study process design, sampling methods, inclusion/exclusion criteria, survey instruments, screening process, diagnostic criteria, data processing, and follow-up methods can be found in the relevant literature33,34,35,36,37. Between November 2017 and December 2022, 11,339 cases of household registration residents aged 40–69 years were recruited using a cluster sampling design. Of all screening registration records, 10,432 completed the entire screening procedure and had complete key variables (Fig. 1). The project was initiated by the Cancer Hospital of the Chinese Academy of Medical Sciences and approved by the Ethics Committees of the Hospital (No. 16-171/1250) and Yangzhong People’s Hospital (No. 202152). All processes followed the Declaration of Helsinki, and informed consent was obtained from the subjects.
Data collection
The target population arrived at the designated screening hospital (Yangzhong People's Hospital) and completed the screening registration and informed consent form, followed by physical measurements by two experienced epidemiological investigators. A one-to-one epidemiological survey based on a standardised questionnaire administered by trained doctors, nurses or epidemiological investigators, with no cues regarding the answers to the questions, was conducted in separate rooms. Then, venous blood was collected and tested for laboratory biochemical indices. Finally, endoscopy and pathological diagnosis were performed.
Variable description
CRFs
The CRFs considered in this study included hypertension, dyslipidaemia and T2DM. Their determination consisted of two methods: first, obtained through the following entry: “Have you ever been diagnosed with any of the following diseases (hypertension, hyperlipidemia and T2DM) by a doctor at the commune/district level or above?” secondly, determined by the results of the physical examination or biochemical index tests. After the subject had rested for 5 min, his or her blood pressure in the right upper arm in a sitting position was measured three times, with an interval of 1–2 min, and the final blood pressure value was averaged over the three times. Venous blood was measured to determine blood glucose and lipid levels (FPG, TC, TG, LDL-C and HDL-C). Hypertension, hyperlipidaemia and T2DM were defined separately by reference to the National Guideline for Hypertension Management in China (2019)38, Guidelines for the Prevention and Treatment of Dyslipidemia in Adults in China (2016 Revised Edition)39 and Guideline for the prevention and treatment of T2DM in China (2020 edition)40, respectively, (Supplementary Table S1).
Digestive system diseases
This study was established based on UGC screening. Therefore, some digestive disorders were determined based on gastroscopy and pathological diagnosis. Since pathological diagnosis is the gold standard for gastroscopic screening, we prioritised determining a pathological diagnosis for screening subjects. In those individuals whose pathology was normal or inflammatory, we judged their health status based on their gastroscopic diagnosis. Other digestive disorders were determined by the following entry: “Have you ever been diagnosed with any of the following disorders by a doctor at the commune/district level or above?” (Supplementary Table S2).
Multimorbidity
In addition to the chronic diseases mentioned above, multimorbidity includes respiratory diseases, cardiovascular and cerebrovascular diseases, endocrine, metabolic and immunological diseases and cancers (excluding GC and EC). They were accessed through the following entry: “Have you ever been diagnosed with any of the following diseases by a doctor at the commune/district level or above?” (Supplementary Table S2). Multimorbidity is the simultaneous presence of two or more chronic diseases in the same individual32.
ORIs
Relevant physical measurements included height, weight, WC, and hip circumference (HC). All measurements were taken according to standard methods14,15,16. All measurements were taken with the respondents wearing light clothing, removing their shoes and hats, and standing upright. WC was measured with a flexible plastic tape measure at the navel position after the patient exhaled, and HC was measured at the widest part of the hips. Height, WC and HC are accurate to 0.1 cm and weight to 0.1 kg. After an overnight fast of at least 10 h, venous blood was drawn from the participants and sent to the laboratory department of Yangzhong People's Hospital. The tests involved included FPG, TG, and HDL-C. Referring to previous studies, BF%41, CI19, CUN-BAE20, BMI16, WC, WHR16, WHtR16, ABSI16, BRI16, BAI14, AVI14, TYG14, LAP14, VAI14,25, CVAI14, WTI28 and CMI30, respectively, were calculated (Supplementary Table S3).
Other variables
Socio-demographic characteristics included gender, age, marital status, education, and family annual income. Health-related characteristics included smoking, alcohol consumption, vegetable and fruit intake, frequency of physical activity, family history of common chronic disease and history of medication for common chronic disease. Current smoking was defined as smoking daily continuously/cumulatively for 6 months16. Consumption of alcohol, regardless of the type, at least 1 time per week within the past year is defined as current drinking42. Daily intake of fruit and vegetable greater than or equal to 500 g was defined as adequate43. The frequency of physical activity was at least 3 times/week, 1–2 times/week or 1–3 times/month, and rarely defined as high, medium, or low, respectively. Family history of common chronic diseases includes hypertension, hyperlipidaemia, coronary heart disease, stroke, T2DM, psychiatric disorders, and so on. History of medication for common diseases included hypertension, hyperlipidaemia and T2DM.
Statistical analysis
All data were analysed by applying SPSS 27.0. Categorical data were described by frequency (%), and continuous data were expressed using mean ± standard deviation. Comparisons between groups were made by t-test or χ2 test. The area under the curves (AUCs) with 95% CIs of receiver operating characteristic (ROC) was calculated to assess the ability to predict CRFs and multimorbidity between different ORIs. Meanwhile, the DeLong test was applied to compare the differences between the AUCs to access the best indicators. The optimal cut-off point was calculated using the maximum Jordon index (Sensitivity + Specificity − 1). Multivariable logistic regression analyses evaluated the association between ORIs z-score [(observation−mean)/SD] and CRFs/multimorbidity, providing ORs and 95% CIs. Two models were applied sequentially: Model 1, unadjusted. Model 2 was adjusted for sex, age, marital status, education, household annual income, smoking, alcohol consumption, vegetable and fruit intake, physical activity, family history of common chronic disease, and history of medication for common chronic disease. In all analyses, P < 0.05 was considered significant.
Results
Participants’ characteristics at baseline
A total of 10,432 subjects were included in the analysis, including 4553 males and 5879 females (Table 1). Compared with women, men had higher proportions of married, education level of senior high school and above, annual household income of ≥ 70,000 Chinese yuan (CNY), current smoking, alcohol consumption, high level of physical activity, history of medication for common chronic disease, dyslipidemia, T2DM, and multimorbidity (all P < 0.05). Men had higher BH, BW, WC, HC, DBP, FPG and TG (all P < 0.05).
Characteristics of ORIs with or without CRFs and multimorbidity
Table 2 shows the distribution characteristics of ORIs in CRFs and multimorbidity. Most ORIs were higher in those with hypertension, dyslipidaemia, T2DM and multimorbidity than in those without (all P < 0.05). Except for gender and HDL-C, the essential characteristics of hypertensive patients (demographic characteristics, health-related characteristics, physical and clinical indicators) were distributed differently from those of non-hypertensive patients (all P < 0.05) (Supplementary Table S4). The essential characteristics of dyslipidaemic patients differed from the distribution of non-dyslipidaemic patients except for marital status, alcohol consumption and adequate vegetable and fruit intake (all P < 0.05) (Supplementary Table S4). Except for marital status, smoking, alcohol consumption, adequate vegetable and fruit intake, BH, HC, and LDL-C, the essential characteristics of diabetic patients were distributed differently from those of non-diabetic patients (all P < 0.05) (Supplementary Table S4). Except for smoking and adequate vegetable and fruit intake, other essential characteristics were differently distributed between multimorbidity and non-multimorbidity patients (all P < 0.05) (Supplementary Table S4).
Comparison of the ability of ORIs for predicting CRFs and multimorbidity
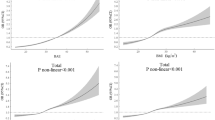
The ORI's ability to predict CRFs and multimorbidity among participants is listed in Table 3. ROC analysis showed that all ORIs could predict CRFs and multimorbidity except BAI, which was not significant in predicting T2DM (all P < 0.05) (Table 3, Fig. 2). As shown in Table 3, after excluding several ORIs involving indicators of the target disease components, CVAI predicted hypertension with the highest AUC (AUC = 0.656, 0.645–0.667). BMI had the highest AUC for predicting dyslipidaemia (AUC = 0.655, 0.645–0.666). CVAI predicted T2DM with the highest AUC (AUC = 0.645, 0.629–0.660). TYG predicted the highest AUC for multimorbidity (AUC = 0.740, 0.731–0.749). The best cut-off values were 90.799, 24.132, 106.953 and 9.060 (Table 4).
We also compared the differences among the AUC of the ORIs in predicting the target diseases (Supplementary Table S5). The results showed a significant difference between the AUC of CVAI predicting hypertension and all other ORIs (all P < 0.05). There was no significant difference in the AUC of BMI, WC and AVI in predicting dyslipidaemia (all P > 0.05). CVAI was not significantly different from LAP, CMI, WHR, and WTI in predicting AUC for T2DM (all P > 0.05). There was a significant difference between the AUC of TYG predicting multimorbidity and all other ORIs (all P < 0.05).
Association (per 1—SD increase) of ORIs with CRFs and multimorbidity
Table 5 demonstrates the relationship of ORIs with CRFs and multimorbidity after Z-score normalisation. After multivariate adjustment, model 2 showed that except for ABSI, which was not significantly associated with hypertension and BAI, which was not significantly associated with T2DM (all P > 0.05), all other ORIs were significantly associated with CRFs and multimorbidity (all P < 0.05). The adjusted OR (per 1-SD increase) values for ORIs and hypertension ranged from 1.166 to 1.799. The adjusted OR (per 1-SD increase) values for ORIs and dyslipidaemia ranged from 1.105 to 168.916. ORIs adjusted for T2DM had OR (per 1-SD increase) values ranging from 1.084 to 2.857. ORIs adjusted for multimorbidity had OR (per 1-SD increase) values ranging from 1.129 to 4.429.
Sensitivity analyses
We analysed the ability of ORIs to predict CRFs and multimorbidity and the optimal cut-off point in different gender populations (Supplementary Tables S6, S7 and Figure S1). After excluding several ORIs involving the target disease components in the male population, the AUC of ORIs in predicting hypertension ranged from 0.522 to 0.677 and was highest for BF%. When predicting dyslipidaemia, the AUC for all ORIs ranged from 0.525 to 0.698 and was highest for BMI. In predicting T2DM, the AUC of ORIs ranged from 0.530 to 0.648 and was highest for CMI (not significantly different from LAP and CVAI). When predicting multimorbidity, the AUC of ORIs ranged from 0.528 to 0.741 and was highest for TYG. The best cut-off points were 25.179, 24.123, 0.761 and 9.125, respectively. In the female population, the AUC of ORIs in predicting hypertension ranged from 0.535 to 0.677 and was highest with CVAI. When predicting dyslipidaemia, the AUC of all ORIs ranged from 0.526 to 0.623 and was highest for CUN-BAE (not significantly different from BF%, WC, WHR, WHtR, BRI and BMI). In predicting T2DM, the AUC of ORIs ranged from 0.575 to 0.657 and was highest in CVAI (not significantly different from WHR). When predicting multimorbidity, the AUC of ORIs ranged from 0.529 to 0.740 and was highest in TYG. The best cut-off points were 91.653, 36.391, 95.355, and 8.961, respectively. We also explored changes in the ability of ORIs to predict multimorbidity by replacing the definition of multimorbidity. ROC analyses showed that the predictive power of the TYG was consistently at its best and differentiated from the other ORIs when multimorbidity was defined as a single individual having ≥ 3, ≥ 4, and ≥ 5 diseases, respectively (all P < 0.05, Supplementary Table S8). Finally, the ROC model was re-run after excluding extreme ORI values that are more than three times the standard deviation from the mean, and the results remained consistent with the previous ones (Supplementary Table S9).
Discussion
Along with changes in economic standards and lifestyles, more and more people are being diagnosed with hypertension, dyslipidaemia, T2DM, Mets and multimorbidity1,2,3,7,12,31,32. In order to meet this challenge, China has carried out large-scale chronic disease prevention and control efforts, one of which is to organise screening of the population for major chronic diseases9,33,34,35. However, the uneven distribution of health resources, insufficient staffing levels in primary care, and low health awareness of the population have severely limited the effectiveness and efficiency of screening, especially in rural areas35,44,45. Therefore, this study analysed and compared the ability of 17 ORIs to predict CRFs and multimorbidity and the correlation between them in a middle-aged and elderly population aged 40–69 years to identify the best prediction tools for different subgroups of chronic diseases. These findings may provide a valuable reference for effectively identifying individuals at high risk for CRFs and multimorbidity in middle-aged and elderly residents in screening practice or health management.
CVAI is the best predictor of hypertension, but there is gender heterogeneity
The CVAI, a composite index combining age, BMI, WC, TG, and HDL-C, was initially developed by Xia et al.46 based on adults in the Xiamen community in China. It is considered a reliable and applicable index for evaluating visceral fat dysfunction in Chinese. Despite the complexity of the formula, several studies have demonstrated that CVAI has good predictive power for metabolic diseases. For example, Han et al. compared the ability of CVAI, VAI, WHtR, WC, and BMI to predict T2DM in a Chinese population based on a large prospective study and found that CVAI was the optimal predictor of T2DM regardless of gender47. A study from southwestern China showed that CVAI was the strongest predictor of CVD in female participants (AUC of 0.687)48. Gui's study, which was conducted on middle-aged and older adults ≥ 45 years of age, found that of the 13 indicators associated with obesity and lipid metrics, CVAI was the best predictor of Mets in women, and TYG-BMI was the best indicator in men49. Li et al.50 found that CVAI was significantly associated with hypertension and prehypertension and had the strongest discriminatory power compared with other indicators (VAI, BMI, WC, WHtR, LDL-C, and WHR). This finding was confirmed by Jung et al.51. Similarly, in a rural cohort study involving 10,304 adult participants, after 6 years of follow-up, the RR of developing hypertension in the highest quartile of the CVAI was 1.29 and 1.53 in men and women, respectively, compared with the lowest quartile. For each unit increased in the CVAI, the odds of developing hypertension increased by 9% in men and 14% in women. Regarding predictive power, CVAI performed better than VAI, ABSI, BMI and WC52.
Our findings yielded supportive results that CVAI is the best predictor of hypertension. Previous studies have shown that it was visceral adipose tissue (VAT) rather than subcutaneous adipose tissue (SAT) or total fat that was more associated with blood pressure52,53,54, which partly explains why the CVAI predicts hypertension better than classical anthropometric measures such as BMI, WC, CI, WHtR and WHR. In this study, despite the significant association between VAI and hypertension, its ability to predict hypertension was much lower than that of CVAI (AUC: 0.656 for CVAI vs. 0.586 for VAI), and even lower than some of the traditional anthropometric measures (WHtR, BMI, and WHR), which is in line with the results of other studies52,55. This is mainly because VAI is one of the indicators used to assess visceral fat in European populations and may not apply to Chinese populations. For example, it has been shown that Asian populations are more prone to visceral fat accumulation at low levels of BMI compared to European populations50,52. CVAI has been developed with the characteristics of Chinese body fat distribution in mind and is, therefore, more applicable to the Chinese population. This study also found that CVAI was one of the best predictors of hypertension in the female population. In men, BF% was the optimal indicator, which is consistent with the findings of Hu et al.55. This suggests, on the one hand, that there are gender differences in the best predictors of hypertension. On the other hand, it suggests that women may be more susceptible to the adverse effects of VAT accumulation than men. Gender heterogeneity in the selection of screening indicators should be emphasised in routine health management or screening. In addition, in the absence of lipid indicators, WHtR/BRI, one of the more readily available anthropometric indicators, also has a relatively good predictive ability for hypertension in the whole population and can be used as an alternative to CVAI.
BMI is the best predictor of dyslipidaemia
This study showed that BMI had the greatest AUC for predicting dyslipidaemia after excluding ORIs associated with lipid indicators (TYG, LAP, VAI, CVAI, WTI and CMI). However, it was similar to WC/AVI. This implies that BMI/WC/AVI are the best predictors of dyslipidaemia. After combining the indicator acquisition, calculation difficulty and gender differences, this study recommended BMI to identify the high-risk dyslipidaemia group.
Positive associations between BMI/WC and dyslipidaemia are not uncommon in previous studies. Evidence that the prevalence of dyslipidaemia increases with increasing BMI and WC levels was seen in Turks56, Ugandans57, Chinese58 and Ethiopians59. A survey in Shanghai, China, showed that BMI and WC can predict dyslipidaemia in both sexes, but there was no significant difference with WHtR60. A study by Lam et al.61 in a Singaporean population found that BMI predicted low HDL-C best, whereas WC predicted high TC, high TG and high LDL-C best. A study of adults aged 20–65 years in the Iranian region reported that WC had the highest AUC in predicting dyslipidaemia (0.622, 95% CI 0.612–0.632), and BMI had an AUC of 0.608 (95% CI 0.598–0.618). However, the study did not compare the difference in AUC between the two indicators62. A prospective urban–rural study involving 44,048 survey respondents aged 35–70 years found that WHtR was the best predictor of dyslipidaemia, followed by WC and BMI63, inconsistent with the findings of the present study, which may be due to the different ages of the populations included in the different studies. However, we can find that the AUC of WHtR, WC and BMI in predicting dyslipidaemia in the studies mentioned above and this study were all between 0.6 and 0.7. In addition, some studies have explored gender differences in ORI predictive ability, but the results have been heterogeneous. Based on data from the 2009 China Health and Nutrition Survey, Tian et al. found that BMI predicted dyslipidaemia in men better than WC, WHtR, ABSI, and BRI, with WHtR/BRI superior in women64. Liu et al.63 concluded that WHtR is the best indicator of dyslipidaemia in men, and WC is optimal in women. In the present study, the optimal indicators among men and women were BMI and CUN-BAE, respectively, and the predictive power of the latter was not significantly different from that of BF%, WC, WHR, WHtR, and BRI. In further analyses, the predictive ability of BF%, WC, WHR, WHtR, BRI, and AVI in the female population was consistent with BMI, suggesting that BMI continues to be a good predictor in the female population. Meanwhile, we found that the optimal cut-off point for BMI was 24.123 for men and 24.000 for women, near the recommended value (BMI overweight: 24) in China16,65. In addition to using ORIs alone, the combined use of indicators was confirmed to improve their efficacy in predicting target diseases further21. Therefore, in addition to using BMI alone in practical applications, we recommend their combined use to improve their efficacy in predicting dyslipidaemia and, thus, improve the efficiency of screening or health management.
CVAI is the best predictor of T2DM
This study showed that CVAI was the best predictor of T2DM after excluding ORIs related to glycaemic indices (TYG), but it was not significantly different from LAP, CMI, WHR and WTI. In the present study, the AUC values of CVAI and LAP were very close to each other, and the former has been described in the previous section. LAP is an indicator constructed based on WC and TG, proposed by Kahn in 2005, and is one of the better indicators of visceral fat accumulation than BMI66. Among them, WC is one of the indicators of response to abdominal obesity, and its ability to predict insulin resistance (IR) and cardiometabolic risk is well known. Its effect on T2DM is stronger than that of BMI67,68. In addition, TG/HDL-C is a potential marker of IR and is strongly associated with prediabetes/T2DM69,70. This may partly explain the relatively good performance of lipid-related ORIs (CVAI, LAP, CMI, and WTI) in predicting T2DM in this study.
Several international scholars have directly explored the association of CVAI/LAP with prediabetes/T2DM. For example, in a study containing 13 obesity- and lipid-related indices, CVAI and LAP were the best predictors of T2DM, except for TYG-related indices, regardless of the genders, and the AUC values were very close to each other (male: 0.654 vs. 0.656; female: 0.672 vs. 0.669)71. A retrospective cohort study of Japanese adults showed that the CVAI was better than BMI and WC in predicting T2DM72, consistent with the findings of Han et al.47. A German study reported that LAP (0.743, 95% CI 0.720–0.765) was less efficacious than TYG but more efficacious than VAI in predicting T2DM73. Evidence from a Chinese elderly population of normal weight suggests that TYG is a valid marker of T2DM regardless of gender and has a superior ability to indicators such as TYG-WC, TYG-WHtR and LAP74. Pan et al.75 investigated the association between longitudinal changes in ORI and T2DM and showed that the predictive power of TYG change values was better than that of LAP and CVAI. However, in this study, we considered that the TYG index includes FPG and that this index is one of the gold standards for determining T2DM. After considering the practical significance, we excluded it when comparing the predictive power of ORIs. The AUC of TYG for predicting T2DM (0.786, 95% CI 0.773–0.799) can still be found in Table 3, and its ability to predict T2DM was optimal among the ORIs involved, consistent with the above study's findings74,75. CMI is a new index for assessing cardiometabolic status. Several recent studies have found a positive association between CMI and T2DM in Chinese and Japanese populations76,77, but its ability to predict T2DM has not been fully explored. Despite the unquestionable positive association of WHR with T2DM, some findings claim that it is less able to predict T2DM than WC or WHtR78,79,80. However, Darko et al.81 concluded that WHR was the best predictor of T2DM in the Ghanaian immigrant population compared to BMI and WC, a finding that was also confirmed by Cheng et al.82. This may be because the WHR-specific proteins, but not the BMI-specific proteins, are associated with T2DM83. Increased WHR have also been shown to be one of the critical factors in reduced urinary glucose excretion in people without diabetes84. In addition, we found that CMI had the best predictive power among men but was not significantly different from LAP and CVAI. CVAI had the best predictive power in the female population but was not significantly different from WHR. Therefore, CVAI is recommended as a screening tool for T2DM. Of course, LAP is also a good proxy indicator.
TYG is the best predictor of multimorbidity
The study showed that TYG, based on TG and FPG, had the strongest ability to predict multimorbidity. As reported by Masilela, elevated TG was the most prevalent form of dyslipidaemia and was more prevalent among individuals with multimorbidity85. FPG is one of the gold standards for responding to blood glucose levels, and it is a good judge of the current status of an individual's blood glucose (IR, prediabetes, T2DM, etc.) 86. T2DM may further be complicated by microvascular or macrovascular complications, including retinopathy, neuropathy, or nephropathy through inflammatory response87, psychological stress88, and other factors, and sarcopenia89,90,91. Therefore, using TYG to screen people at risk for multimorbidity has significant practical implications.
To our knowledge, more current studies on multimorbidity have focused only on ORIs and CVD or CRF aggregation. For example, Wang et al. found that visceral obesity indicators, especially CVAI, were the strongest predictors of CVD in women48. Wai et al. concluded that WC is the best predictor of CVD risk in Addis Ababa, Ethiopians59. A study from Iran reported that WHR is the best predictor of CVD62. A study of children and adolescents found neck circumference was significantly associated with clustered CVD risk factors in both sexes92. Li et al. explored the BMI percentile, WC percentile, WHtR, and WHR in participants aged 6–17 years to identify the accuracy of identifying clusters of CRFs, and the results showed that the relevant anthropometric indices can predict clusters of CRFs. However, the AUC values were low93. BMI, WC, and WHtR were effective predictors of 1 CRF, 2 CRFs, or ≥ 3 CRFs in a population of 1139 people aged 6–17 in northeastern Brazil94. For at least one cardiometabolic abnormality, WHtR and BRI were considered to have the most predictive advantage64. Although the variety of target diseases has been further enriched recently95,96,97, studies of multimorbidity involving multiple systems are fewer or still limited to association analyses and have not explored the ability of multiple old and new ORIs to predict multimorbidity. The multimorbidity in this study included a wide range of diseases, including digestive system diseases, respiratory system diseases, cardiovascular and cerebrovascular diseases, endocrine, metabolic and immune diseases and cancers, with most of the digestive system diseases being diagnosed by endoscopic examination or pathological diagnosis. Combined with the fact that Yangzhong City is a high-prevalence area for upper gastrointestinal tract cancer, this not only improves the accuracy of disease diagnosis but also increases the practical significance of multimorbidity prediction. Given that the general definition of multimorbidity only represents aggregations of 2 or more chronic diseases and that the predictive ability of ORIs may be affected by highly affected diseases such as hypertension, dyslipidemia, and T2DM, we also performed sensitivity analyses by redefining multimorbidity. When multimorbidity was defined as ≥ 3, ≥ 4, and ≥ 5 chronic disease aggregations, respectively, the ability of TYG was stable, with the AUC reaching the maximum (AUC = 0.784) when predicting ≥ 4 chronic disease aggregations, suggesting that the practical significance of prediction can be enhanced by appropriately upgrading the types of diseases included in the multimorbidity when using TYG to predict multimorbidity rather than restricting the multimorbidity only to 2 and more diseases. In addition, sex-stratified analyses found that the AUC for TYG to predict multimorbidity was best in both sexes, suggesting that TYG applies to the whole population.
Limitations
This study was conducted based on a well-designed cohort study, which greatly improved the standardisation and validity of data collection, but some limitations remain. Firstly, as it was a cross-sectional study, the causal relationship between ORIs and diseases of interest could not be determined. Second, the participants were only residents aged 40–69 years old, which is not representative of the entire age group. Thirdly, the indicators involved in this study were calculated based on formulae and may have some bias in assessing obesity levels. Finally, the participants were mainly from Yangzhong City, and the findings could not be generalised to the whole country.
Conclusion
All other ORIs considered predicted hypertension, dyslipidaemia, T2DM and multimorbidity except BAI, which can not predict T2DM. After excluding ORIs associated with the target disease components and after accounting for gender heterogeneity, CVAI was the best predictor of hypertension in the whole population and the female population. BF% was the best predictor of hypertension in the male population. BMI was the best predictor of dyslipidaemia, CVAI was the best predictor of T2DM, and TYG was the best predictor of multimorbidity. During screening for common chronic diseases or multimorbidity, appropriate ORIs should be selected to identify high-risk populations by considering the heterogeneity of the target population’s gender and the predictive ability of the ORIs to improve screening efficiency.
Data availability
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
References
World Health Statistics 2020: Monitoring Health for the SDGs, Sustainable Development Goals. (Geneva: World Health Organization, 2020). Licence: CC BY-NC-SA 3.0 IGO.
World Health Statistics 2019: Monitoring Health for the SDGs, Sustainable Development Goals. (Geneva: World Health Organization, 2019). Licence: CC BY-NC-SA 3.0 IGO.
Roth, G. A. et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: Update from the GBD 2019 study. J. Am. Coll. Cardiol. 76, 2982–3021 (2020).
GBD 2019 Stroke Collaborators. Global, regional, and national burden of stroke and its risk factors, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol. 20, 795–820 (2021).
Ma, Q. et al. Temporal trend and attributable risk factors of stroke burden in China, 1990–2019: An analysis for the Global Burden of Disease Study 2019. Lancet Public Health 6, e897–e906 (2021).
Powell-Wiley, T. M. et al. Obesity and cardiovascular disease: A scientific statement from the American Heart Association. Circulation 143, e984–e1010 (2021).
Li, X. et al. Cardiovascular risk factors in China: A nationwide population-based cohort study. Lancet Public Health 5, e672–e681 (2020).
Li, S. et al. Modifiable risk factors associated with cardiovascular disease and mortality in China: A PURE substudy. Eur. Heart J. 43, 2852–2863 (2022).
Lu, J. et al. Characteristics of high cardiovascular risk in 1.7 million Chinese adults. Ann. Intern. Med. 170, 298–308 (2019).
Ferket, B. S. et al. Lifetime cardiovascular disease risk by coronary artery calcium score in individuals with and without diabetes: An analysis from the multi-ethnic study of atherosclerosis. Diabetes Care 45, 975–982 (2022).
Eckel, R. H. & Krauss, R. M. American Heart Association call to action: obesity as a major risk factor for coronary heart disease AHA Nutrition Committee. Circulation 97, 2099–2100 (1998).
Peters, S. et al. Clustering of risk factors and the risk of incident cardiovascular disease in Asian and Caucasian populations: Results from the Asia Pacific Cohort Studies Collaboration. BMJ Open 8, e019335 (2018).
Thangiah, N. et al. Clustering and tracking the stability of biological CVD risk factors in adolescents: The Malaysian health and adolescents longitudinal research team study (MyHeARTs). Front. Public Health 8, 69 (2020).
Duan, Y. et al. Predictive ability of obesity- and lipid-related indicators for metabolic syndrome in relatively healthy Chinese adults. Front. Endocrinol. (Lausanne) 13, 1016581 (2022).
Wang, F., Chen, Y., Chang, Y., Sun, G. & Sun, Y. New anthropometric indices or old ones: which perform better in estimating cardiovascular risks in Chinese adults. BMC Cardiovasc. Disord 18, 14 (2018).
Lee, X. et al. Comparison of 10 obesity-related indices for predicting hypertension based on ROC analysis in Chinese adults. Front. Public Health 10, 1042236 (2022).
Al-Shami, I. et al. Assessing metabolic syndrome prediction quality using seven anthropometric indices among Jordanian adults: A cross-sectional study. Sci. Rep. 12, 21043 (2022).
Escobedo-de la Peña, J., Ramírez-Hernández, J. A., Fernández-Ramos, M. T., González-Figueroa, E. & Champagne, B. Body fat percentage rather than body mass index related to the high occurrence of type 2 diabetes. Arch. Med. Res. 51, 564–571 (2020).
Zhang, A. et al. Conicity-index predicts all-cause mortality in Chinese older people: A 10-year community follow-up. BMC Geriatr. 22, 971 (2022).
Costa, A. et al. CUN-BAE index as a screening tool to identify increased metabolic risk in apparently healthy normal-weight adults and those with obesity. J. Nutr. 151, 2215–2225 (2021).
Sekgala, M. D., Opperman, M., Mpahleni, B. & Mchiza, Z. J. Anthropometric indices and cut-off points for screening of metabolic syndrome among South African taxi drivers. Front. Nutr. 9, 974749 (2022).
Li, Y. et al. Association between four anthropometric indexes and metabolic syndrome in US adults. Front. Endocrinol. (Lausanne) 13, 889785 (2022).
Park, B., Lee, H. S. & Lee, Y. J. Triglyceride glucose (TyG) index as a predictor of incident type 2 diabetes among nonobese adults: A 12-year longitudinal study of the Korean genome and epidemiology study cohort. Transl. Res. 228, 42–51 (2021).
Marcadenti, A., Fuchs, F. D., Moreira, L. B., Gus, M. & Fuchs, S. C. Adiposity phenotypes are associated with type-2 diabetes: LAP index, body adiposity index, and neck circumference. Atherosclerosis 266, 145–150 (2017).
Fan, Y. et al. Association between visceral adipose index and risk of hypertension in a middle-aged and elderly Chinese population. Nutr. Metab. Cardiovasc. Dis. 31, 2358–2365 (2021).
Wan, H. et al. Associations between abdominal obesity indices and diabetic complications: Chinese visceral adiposity index and neck circumference. Cardiovasc. Diabetol. 19, 118 (2020).
Zhang, X. et al. Visceral obesity-related indices in the identification of individuals with metabolic syndrome among different ethnicities in Xinjiang, China. Diabetes Metab. Syndr. Obes. 14, 1609–1620 (2021).
Ma, C. M. et al. Three novel obese indicators perform better in monitoring management of metabolic syndrome in type 2 diabetes. Sci. Rep. 7, 9843 (2017).
Datta Banik, S. et al. Evaluation of anthropometric indices and lipid parameters to predict metabolic syndrome among adults in Mexico. Diabetes Metab. Syndr. Obes. 14, 691–701 (2021).
Radetti, G. et al. High Tg/HDL-cholesterol ratio highlights a higher risk of metabolic syndrome in children and adolescents with severe obesity. J. Clin. Med. 11, 4488 (2022).
Geng, S., Chen, X., Shi, Z., Bai, K. & Shi, S. Association of anthropometric indices with the development of multimorbidity in middle-aged and older adults: A retrospective cohort study. PLoS ONE 17, e0276216 (2022).
Lu, Y. et al. Waist-to-height ratio, waist circumference, body mass index, waist divided by height(0.5) and the risk of cardiometabolic multimorbidity: A national longitudinal cohort study. Nutr. Metab. Cardiovasc. Dis. 31, 2644–2651 (2021).
Chen, R. et al. The national cohort of esophageal cancer-prospective cohort study of esophageal cancer and precancerous lesions based on high-risk population in China (NCEC-HRP): Study protocol. BMJ Open 9, e027360 (2019).
Chen, R. et al. Effectiveness of one-time endoscopic screening programme in prevention of upper gastrointestinal cancer in China: A multicentre population-based cohort study. Gut 70, 251–260 (2021).
Feng, X. et al. Satisfaction in population-based cancer screening in a Chinese rural high-risk population: The Yangzhong early diagnosis and treatment of upper gastrointestinal cancer. BMC Health Serv. Res. 22, 675 (2022).
Wang, G. Q. & Wei, W. Q. Upper Gastrointestinal Cancer Screening and Early Detection and Treatment Technology Programme (2020 Pilot Version) (People’s Publishing House, 2020).
Feng, X. et al. Prevalence and coprevalence of modifiable risk factors for upper digestive tract cancer among residents aged 40–69 years in Yangzhong city, China: A cross-sectional study. BMJ Open 11, e042006 (2021).
Bureau of Disease Prevention and Control, National Health Commission of People′s Republic of China. et al. [National guideline for hypertension management in China (2019)]. Zhonghua Xin Xue Guan Bing Za Zhi 48, 10–46 (2020).
Zhu, J. R. et al. Chinese guidelines for prevention and control of dyslipidaemia in adults (2016 revision). Chin. Circ. J. 31, 937–953 (2016).
Chinese Elderly Type 2 Diabetes Prevention and Treatment of Clinical Guidelines Writing Group, et al. [Clinical guidelines for prevention and treatment of type 2 diabetes mellitus in the elderly in China (2022 edition)]. Zhonghua Nei Ke Za Zhi 61, 12–50 (2022).
López-Hernández, D. Epidemiological association between body fat percentage and cervical cancer: A cross-sectional population-based survey from Mexico. Arch. Med. Res. 44, 454–458 (2013).
Hu, L. et al. Prevalence and risk factors of prehypertension and hypertension in Southern China. PLoS ONE 12, e0170238 (2017).
Chinese Nutrition Society. Dietary Guidelines for Chinese Residents (People’s Medical Publishing House, 2016).
Feng, X. et al. Satisfaction and its determinants of rural upper gastrointestinal cancer screening in China: A preliminary cross-sectional study. BMJ Open 12, e061483 (2022).
Prescott, N. & Jamison, D. T. The distribution and impact of health resource availability in China. Int. J. Health Plan. Manag. 1, 45–56 (1985).
Xia, M. F. et al. A indicator of visceral adipose dysfunction to evaluate metabolic health in adult Chinese. Sci. Rep. 6, 38214 (2016).
Han, M. et al. Chinese visceral adiposity index: A reliable indicator of visceral fat function associated with risk of type 2 diabetes. Diabetes Metab. Res. Rev. 37, e3370 (2021).
Wang, Y. et al. Visceral adiposity measures are strongly associated with cardiovascular disease among female participants in Southwest China: A population-based prospective study. Front. Endocrinol. (Lausanne) 13, 969753 (2022).
Gui, J. et al. Obesity- and lipid-related indices as a predictor of obesity metabolic syndrome in a national cohort study. Front. Public Health 11, 1073824 (2023).
Li, B. et al. Chinese visceral adiposity index is more closely associated with hypertension and prehypertension than traditional adiposity indices in Chinese population: Results from the REACTION Study. Front. Endocrinol. 13, 921997 (2022).
Jung, J. Y., Oh, C. M., Jo, H. C. & Park, S. K. Predictive ability of the Chinese visceral adiposity index for incident hypertension in working-aged Koreans. Epidemiol. Health 46, e2024034 (2024).
Han, M. et al. Chinese visceral adiposity index, a novel indicator of visceral obesity for assessing the risk of incident hypertension in a prospective cohort study. Br. J. Nutr. 126, 612–620 (2021).
Koh, H. et al. Visceral adiposity, not abdominal subcutaneous fat area, is associated with high blood pressure in Japanese men: The Ohtori study. Hypertens. Res. 34, 565–572 (2011).
Chandra, A. et al. The relationship of body mass and fat distribution with incident hypertension: Observations from the Dallas Heart Study. J. Am. Coll. Cardiol. 64, 997–1002 (2014).
Hu, L. et al. Different adiposity indices and their associations with hypertension among Chinese population from Jiangxi province. BMC Cardiovasc. Disorders 20, 115 (2020).
Erem, C., Hacihasanoglu, A., Deger, O., Kocak, M. & Topbas, M. Prevalence of dyslipidemia and associated risk factors among Turkish adults: Trabzon lipid study. Endocrine 34, 36–51 (2008).
Asiki, G. et al. Prevalence of dyslipidaemia and associated risk factors in a rural population in South-Western Uganda: A community based survey. PLoS ONE 10, e0126166 (2015).
Feng, R. N. et al. BMI is strongly associated with hypertension, and waist circumference is strongly associated with type 2 diabetes and dyslipidemia, in northern Chinese adults. J. Epidemiol. 22, 317–323 (2012).
Wai, W. S. et al. Comparison of measures of adiposity in identifying cardiovascular disease risk among Ethiopian adults. Obesity (Silver Spring) 20, 1887–1895 (2012).
Zhang, Y. et al. Association between anthropometric indicators of obesity and cardiovascular risk factors among adults in Shanghai, China. BMC Public Health 19, 1035 (2019).
Lam, B. C., Koh, G. C., Chen, C., Wong, M. T. & Fallows, S. J. Comparison of body mass index (BMI), body adiposity index (BAI), waist circumference (WC), waist-to-hip ratio (WHR) and waist-to-height ratio (WHtR) as predictors of cardiovascular disease risk factors in an adult population in Singapore. PLoS ONE 10, e0122985 (2015).
Tabary, M. et al. Association of anthropometric indices with cardiovascular disease risk factors among adults: A study in Iran. Eur. J. Cardiovasc. Nurs. 20, 358–366 (2021).
Liu, J. et al. Predictive Values of anthropometric measurements for cardiometabolic risk factors and cardiovascular diseases among 44 048 Chinese. J. Am. Heart Assoc. 8, e010870 (2019).
Tian, S., Zhang, X., Xu, Y. & Dong, H. Feasibility of body roundness index for identifying a clustering of cardiometabolic abnormalities compared to BMI, waist circumference and other anthropometric indices: The China Health and Nutrition Survey, 2008 to 2009. Medicine (Baltimore) 95, e4642 (2016).
Hu, L. et al. Prevalence of overweight, obesity, abdominal obesity and obesity-related risk factors in southern China. PLoS ONE 12, e0183934 (2017).
Kahn, H. S. The, “lipid accumulation product” performs better than the body mass index for recognizing cardiovascular risk: A population-based comparison. BMC Cardiovasc. Disorders 5, 26 (2005).
Seo, D. C., Choe, S. & Torabi, M. R. Is waist circumference ≥102/88cm better than body mass index ≥30 to predict hypertension and diabetes development regardless of gender, age group, and race/ethnicity? Meta-analysis. Prev. Med. 97, 100–108 (2017).
Luo, W. et al. 2 years change of waist circumference and body mass index and associations with type 2 diabetes mellitus in cohort populations. Obes. Res. Clin. Pract. 7, e290-296 (2013).
Yang, T. et al. Correlation between the triglyceride-to-high-density lipoprotein cholesterol ratio and other unconventional lipid parameters with the risk of prediabetes and type 2 diabetes in patients with coronary heart disease: A RCSCD-TCM study in China. Cardiovasc. Diabetol. 21, 93 (2022).
Wu, L., Wu, X., Hu, H. & Wan, Q. Association between triglyceride-to-high-density lipoprotein cholesterol ratio and prediabetes: A cross-sectional study in Chinese non-obese people with a normal range of low-density lipoprotein cholesterol. J. Transl. Med. 20, 484 (2022).
Zhang, X. et al. Optimal obesity- and lipid-related indices for predicting type 2 diabetes in middle-aged and elderly Chinese. Sci. Rep. 14, 10901 (2024).
Shang, L. et al. Association between Chinese visceral adiposity index and incident type 2 diabetes mellitus in Japanese adults. Diabetes Metab. Syndr. Obes. 14, 3743–3751 (2021).
Ahn, N. et al. Visceral adiposity index (VAI), lipid accumulation product (LAP), and product of triglycerides and glucose (TyG) to discriminate prediabetes and diabetes. Sci. Rep. 9, 9693 (2019).
Ke, P. et al. Comparison of obesity indices and triglyceride glucose-related parameters to predict type 2 diabetes mellitus among normal-weight elderly in China. Eat. Weight Disord 27, 1181–1191 (2022).
Pan, L. et al. Comparison of longitudinal changes in four surrogate insulin resistance indexes for incident T2DM in middle-aged and elderly Chinese. Front. Public Health 10, 1046223 (2022).
Qiu, Y. et al. Transition of cardiometabolic status and the risk of type 2 diabetes mellitus among middle-aged and older Chinese: A national cohort study. J. Diabetes Investig. 13, 1426–1437 (2022).
Zha, F. et al. The nonlinear correlation between the cardiometabolic index and the risk of diabetes: A retrospective Japanese cohort study. Front. Endocrinol. (Lausanne) 14, 1120277 (2023).
Wang, Y., Rimm, E. B., Stampfer, M. J., Willett, W. C. & Hu, F. B. Comparison of abdominal adiposity and overall obesity in predicting risk of type 2 diabetes among men. Am. J. Clin. Nutr. 81, 555–563 (2005).
Basit, A., Mustafa, N., Waris, N., Askari, S. & Fawwad, A. Predicting the risk of type 2 diabetes through anthropometric indices in Pakistani adults-a sub-analysis of second National diabetes survey of Pakistan 2016–2017 (NDSP-07). Diabetes Metab. Syndr. 15, 543–547 (2021).
Zhang, F. L. et al. Strong association of waist circumference (WC), body mass index (BMI), waist-to-height ratio (WHtR), and waist-to-hip ratio (WHR) with diabetes: A population-based cross-sectional study in Jilin Province, China. J. Diabetes Res. 2021, 8812431 (2021).
Darko, S. N. et al. Anthropometric indices and their cut-off points in relation to type 2 diabetes among Ghanaian migrants and non-migrants: The RODAM study. Diabetes Res. Clin. Pract. 173, 108687 (2021).
Cheng, C. H. et al. Waist-to-hip ratio is a better anthropometric index than body mass index for predicting the risk of type 2 diabetes in Taiwanese population. Nutr. Res. 30, 585–593 (2010).
Bao, X. et al. Proteomic profiles of body mass index and waist-to-hip ratio and their role in incidence of diabetes. J. Clin. Endocrinol. Metab. 107, e2982–e2990 (2022).
Chen, J., Qiu, S., Guo, H., Li, W. & Sun, Z. Increased waist-to-hip ratio is associated with decreased urine glucose excretion in adults with no history of diabetes. Endocrine 64, 239–245 (2019).
Masilela, C., Adeniyi, O. V. & Benjeddou, M. Prevalence, patterns and determinants of dyslipidaemia among South African adults with comorbidities. Sci. Rep. 12, 337 (2022).
Mechanick, J. I., Garber, A. J., Grunberger, G., Handelsman, Y. & Garvey, W. T. Dysglycemia-based chronic disease: AN American Association of Clinical Endocrinologists position statement. Endocr. Pract. 24, 995–1011 (2018).
Lontchi-Yimagou, E., Sobngwi, E., Matsha, T. E. & Kengne, A. P. Diabetes mellitus and inflammation. Curr. Diabetes Rep. 13, 435–444 (2013).
Hackett, R. A. & Steptoe, A. Type 2 diabetes mellitus and psychological stress—A modifiable risk factor. Nat. Rev. Endocrinol. 13, 547–560 (2017).
Zheng, W., Guo, J. & Liu, Z. S. Effects of metabolic memory on inflammation and fibrosis associated with diabetic kidney disease: An epigenetic perspective. Clin. Epigenetics 13, 87 (2021).
Dagliati, A. et al. Machine learning methods to predict diabetes complications. J. Diabetes Sci. Technol. 12, 295–302 (2018).
Izzo, A., Massimino, E., Riccardi, G. & Della Pepa, G. A narrative review on sarcopenia in type 2 diabetes mellitus: Prevalence and Associated factors. Nutrients 13, 183 (2021).
Castro-Piñero, J. et al. Neck circumference and clustered cardiovascular risk factors in children and adolescents: Cross-sectional study. BMJ Open 7, e016048 (2017).
Li, Y. et al. The predictive value of anthropometric indices for cardiometabolic risk factors in Chinese children and adolescents: A national multicenter school-based study. PLoS ONE 15, e0227954 (2020).
de Quadros, T. et al. Utility of anthropometric indicators to screen for clustered cardiometabolic risk factors in children and adolescents. J. Pediatr. Endocrinol. Metab. 32, 49–55 (2019).
Liu, J. et al. Optimum non-invasive predictive indicators for metabolic dysfunction-associated fatty liver disease and its subgroups in the Chinese population: A retrospective case-control study. Front. Endocrinol. (Lausanne) 13, 1035418 (2022).
Matsui, R., Inaki, N., Tsuji, T. & Fukunaga, T. Relationship between fat mass indices and postoperative complications after laparoscopic gastrectomy in patients with gastric cancer: A propensity score matching analysis. Anticancer Res. 42, 4841–4848 (2022).
Wang, S. Y. et al. Association of novel and conventional obesity indices with colorectal cancer risk in older Chinese: A 14-year follow-up of the Guangzhou Biobank Cohort Study. BMC Cancer 23, 286 (2023).
Acknowledgements
The author would like to thank the residents and staff involved in the present study.
Funding
This study was supported by the China Early Gastrointestinal Cancer Physicians Growing Together Program (Grant No. GTCZ-2021-JS-32-0001), Zhenjiang City key research and development plan (Grant No. SH2022051) and 2023 Jiangsu Province Preventive Medicine general Project (Ym2023031).
Author information
Authors and Affiliations
Contributions
X.F. drafted the manuscript. X.F., J.H.Z., Z.L.H., and H.Y.T. contributed to the conception and design of the study. X.F., Z.L.H., S.H.Y. and H.Y.T. conducted data collection and fundamental statistical analysis. All authors discussed the result and agreed on the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Feng, X., Zhu, J., Hua, Z. et al. Comparison of obesity indicators for predicting cardiovascular risk factors and multimorbidity among the Chinese population based on ROC analysis. Sci Rep 14, 20942 (2024). https://doi.org/10.1038/s41598-024-71914-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-71914-1
- Springer Nature Limited