Abstract
Currently, in vitro cultured corneal epithelial transplantation is effective in treating limbal stem cell dysfunction (LSCD). Selecting carriers is crucial for constructing the corneal epithelium through tissue engineering. In this study, the traditional amniotic membrane (AM) was modified, and mesenchymal stem cells (MSCs) were inoculated into the ultra-thin amniotic membrane (UAM) stroma to construct a novel UAM-MSC tissue-engineered corneal epithelial carrier, that could effectively simulate the limbal stem cells (LSCs) microenvironment. The structure of different carriers cultured tissue-engineered corneal epithelium and the managed rabbit LSCD model corneas were observed through hematoxylin–eosin staining. Cell phenotypes were evaluated through fluorescence staining, Western blotting, and RT-qPCR. Additionally, cell junction genes and expression markers related to anti-neovascularization were evaluated using RT-qPCR. Corneal epithelium cell junctions were observed via an electron microscope. The tissue-engineered corneal epithelium culture medium was analyzed through mass spectrometry. Tissue-engineered corneal epithelial cells expanded by LSCs on UAM-MSCs had good transparency. Simultaneously, progenitor cell (K14, PNCA, p63) and corneal epithelial (PAX6) gene expression in tissue-engineered corneal epithelium constructed using UAM-MSCs was higher than that in corneal epithelial cells amplified by UAM and de-epithelialized amniotic membrane. Electron microscopy revealed that corneal epithelial cells grafted with UAM-MSCs were closely connected. In conclusion, the UAM-MSCs vector we constructed could better simulate the limbal microenvironment; the cultured tissue-engineered corneal epithelium had better transparency, anti-neovascularization properties, closer intercellular connections, and closer resemblance to the natural corneal epithelial tissue phenotype.
Similar content being viewed by others
Introduction
Limbal stem cells (LSCs), namely corneal epithelial stem cells, are located in the basal layer of limbal epithelial cells. LSCs not only regenerate and replenish corneal epithelial cells but also produce anti-inflammatory factors that protect the eyes from infection1,2,3,4. Many LSCs are crucial for maintaining the dynamic stability of the corneal epithelium and transparency of corneal tissue5. Stem cells from different tissues thrive in stable microenvironments. Microenvironmental factors regulate stem cell proliferation and differentiation. Disruption in the microenvironment leads to abnormal stem cell differentiation6. Limbal stem cell dysfunction (LSCD) is often caused by ophthalmic chemical injury, thermal burn, ocular cicatricial pemphigoid, and severe xerophthalmia, which disrupt the stem cell matrix microenvironment, leading to reduced stem cell number or loss of directional differentiation potential. It typically involves extensive damage to ocular surface tissue, persistent corneal epithelial defects, chronic inflammation, corneal epithelial conjunctival invasion, and neovascularization, followed by decreased corneal transparency, which causes severe visual impairment and blindness in patients7. Presently, the main treatment of LSCD involves transplantation of autologous or allogeneic limbal stem cells and tissue-engineered corneal epithelium8,9,10. Immune rejection remains a primary cause of allograft transplantation failure11,12. Even 3 years after transplantation, rejection rates remain high12. Autologous conjunctival limbal transplantation circumvents immune rejection with minimal risk of inducing LSCD. This method is commonly used in patients with unilateral LSCD13. However, without microenvironmental repair, simple transplantation of limbal stem cells from healthy eyes leads to long-term survival failure of the transplanted LSCs, necessitating repeated transplantation. Therefore, tissue-engineered corneal epithelial cell transplantation is an effective treatment in patients with LSCD.
The construction of tissue-engineered corneal epithelium needs to meet three conditions: obtaining seed cells, selecting carrier materials, and using appropriate culture methods. Among these, carrier selection is pivotal as it influences the maintenance of stem cell phenotype, determines differentiation direction, and stem cell proliferation and apoptosis, all closely related to the stem cell microenvironment6,14. Previous studies have shown that the amniotic membrane (AM) contains the thickest basement membrane in humans; its matrix contains numerous stromal cells, particularly living stromal cells. AM also contains numerous growth factors, such as EGF, bFGF, HGF, and TGF-β, which promote cell growth and differentiation. In certain aspects, AM can mimic the stem cell microenvironment, making it suitable as a carrier for the in vitro expansion of corneal epithelial stem cells15,16. However, owing to the loose structure of the spongy layer of the AM, maintaining consistent transparency due to its different sources and thickness poses challenges, which can impact transplantation outcomes. To achieve clearer post-operative vision, some researchers17 removed the spongy structure of the amniotic matrix from epithelialized AM to obtain an ultra-thin amniotic membrane (UAM). Comparative studies with the de-epithelialized amniotic membrane (DAM) revealed that tissue-engineered corneal epithelium constructed using UAM had higher transparency and more stem cells. Additionally, the existing carrier materials include various natural materials18 and synthetic biomaterials19. However, since these carriers lack living stromal cells, they cannot effectively mimic the limbal stem cell microenvironment, affecting stem cell survival after transplantation and causing transplantation failure. Therefore, how can we effectively simulate the limbal microenvironment?
The limbal microenvironment, with its unique gene expression and extracellular matrix (ECM) protein profile, is particularly suitable for the growth of limbal epithelial stem cells (LESCs) and crucial for maintaining their quantity and function20,21. The limbal microenvironment consists of many cell types, including melanocytes22, immune cells23, vascular cells24, nerve cells25, and stromal (mesenchymal) cells25. Recently, mesenchymal stem cells (MSCs) have garnered increasing attention for their role in regulating LESC growth. Mesenchymal CD90- and CD105-positive cells are preferentially distributed in the limbal epithelial region and closely interact with LESCs26,27. Anatomically, MSCs bind directly to LESCs through many molecular substrates and signaling pathways to form limbal niche cell components, including aquaporin-1 and vimentin28, chondroitin sulfate27, SDF-1/CXCR4 29, BMP/WNT30, and IL-6/STAT331. In addition to having strong proliferation, paracrine function32, and non-immunogenicity, MSCs can regulate and immunosuppress macrophages through multiple pathways such as Notch, NF-κB, PI3K/Akt, and JAK/STAT33. Some researchers have used bone marrow MSCs for treating ocular chemical injury and found that MSCs could inhibit inflammation, promote epithelial growth, ameliorate limbal ischemia, preserve LSCs, specifically when they are defective in both eyes, repair or regenerate damaged limbal/corneal epithelium, and reconstruct the limbal stem cell microenvironment34,35. We hypothesized that preparing UAM with frozen-thawed AM and incorporating umbilical cord MSCs could better mimic the limbal microenvironment while maintaining transparency, thereby promoting corneal epithelium growth. Therefore, we co-cultured MSCs and tissue-engineered corneal epithelium for the first time to evaluate their transparency and thickness using UAM-MSCs. Additionally, we investigated the effects of MSCs on corneal progenitor cell markers (K14 and ABCG2) and corneal epithelial cell characteristics (PAX6). Furthermore, we transplanted UAM-MSC tissue-engineered corneal epithelium into an LSCD rabbit model to evaluate its efficacy in treating LSCD.
Methods
Animals
Male New Zealand white rabbits weighing 2–2.5 kg and aged 3–4 months were provided by the Animal Center of Guizhou Medical University (Guizhou, China). The study was approved by the Animal Ethics Committee of Guizhou Medical University (NO. 2000928); all methods were carried out in accordance with relevant guidelines and regulations. All procedures conformed to the Declaration of the ARRIVE guidelines. Fasting for 8 h was required before invasive operation and general anesthesia was administered by intravenous injection (30 mg/kg) into the rabbit’s ear. To obtain the corneas, rabbits were euthanized with pentobarbital (200 mg/kg, intravenous). The anesthesia and euthanasia of rabbits accorded to the American Veterinary Medical Association (AVMA) Guidelines.
Preparation of UAM
The human placenta was obtained from a healthy donor during a cesarean section in accordance with the principles of the Helsinki Declaration and was approved by the Institutional Review Committee of the affiliated Hospital of Guizhou Medical University (NO. 2023–539). The AM was separated from the placenta, rinsed with HBSS until blood stains were removed, and stored at − 80 °C. The AM was then laid flat on the amniotic ring. After removing the AM epithelium using 0.02% EDTA digestion, the AM was immersed in a sufficient amount of 1.5 mg/mL IV collagenase using a sterilized nanosponge and placed under the amniotic ring. The circular face of the cylindrical sponge was close to the DAM substrate; the loose collagen within the amniotic matrix was removed by digesting for approximately 75–90 min at 37 °C. The dense part was retained, obtaining the UAM. All procedures were performed under aseptic conditions to prevent microbial contamination during the preparation.
Cultivation and purification of umbilical cord MSCs
The human umbilical cord was obtained from a healthy donor during a cesarean section in accordance with the principles of the Helsinki Declaration and approved by the Institutional Review Committee of the affiliated Hospital of Guizhou Medical University (NO. 2023–539) for human research.
Under sterile conditions, the umbilical cord was cleaned, arteriovenous vessels were stripped, and fahrenheit glue was separated and cut into 1 × 1 mm-sized tissue blocks. After overnight digestion with type IV collagenase, the cells were cultured in DMEM containing 1% double antibodies, 15% serum, and low glucose. All procedures were performed under aseptic conditions to prevent microbial contamination during the preparation process.
Construction of the carrier
MSCs extracted from the umbilical cord were cultured and identified (Supplemental Fig. 1) for the third to fifth passages. Approximately 6 × 105 MSCs were inoculated onto the basal surface of the UAM, with MSC growth observed within 24 h. After 1–2 days of culture, a new UAM-MSC vector was obtained.
Optical transmittance characteristics of the carrier
To estimate the optical transmittance of intact DAM, UAM, and UAM inoculated with umbilical cord MSCs, scanning images were obtained. Subsequently, LSCs were cultured on the epithelial surface of AM tissue, photographed with a digital camera, and their transparency was compared.
ImageJ software, version 1.51j8 (NIH, Bethesda, MD; http://imagej.nih.gov/ij; last access date, Jun 28th, 2015) with Java software version 1.8.0_112 (64-bit; Oracle, Redwood City, CA) was applied to measure the transparency. The software can recognize the gray level of the letter ”A” below of the carrier and measure the mean value of gray level of the area.
Construction of tissue-engineered corneal epithelial cells
The New Zealand rabbits were euthanized, and the central corneal tissue was removed using a 9 mm-diameter ring drill. The residual limbal tissue was cut into 2 × 2 mm-sized tissue blocks. The tissue blocks were then incubated in a hormone-supplemented epithelial cell culture medium (SHEM) containing 2 mg/mL DispaseII (Roche, Basel, Switzerland) at 4 °C for 14 h. The epithelial cells were isolated and cultured on 6-well plates coated with DAM, UAM, and UAM-MSCs containing SHEM. SHEM was prepared from an equal volume of HEPES buffered DMEM (Gbico, USA) containing bicarbonate and Ham's F12.5% fetal bovine serum, 0.5% dimethyl sulfoxide 2.5 mL, 10 ng/mL human epidermal growth factor (500 μL), 1% transferrin (5 mL), 0.5 μg/mL hydrocortisone (100 μL), and 1% penicillin, streptomycin, and amphotericin. The culture medium was changed every 2 days. After 10 days of culture, the epithelial cells were air lifted (reducing the amount of culture medium, maintaining 100ul medium to expose the surface epithelial cells to the air) and cultured for 3 days to promote stratified proliferation36. The epithelium was labeled using the CFDA SE cell tracer kit (Invitrogen, Carlsbad, CA, USA) the day before transplantation.
Hematoxylin–eosin staining
AM tissue was fixed for 30 min in 4% paraformaldehyde at 4 °C, embedded in OCT compound (Sakura, Tissue-Tek, Torrance, USA), and stored at − 80 °C. The frozen Sects. (6 μm thick) were stained with hematoxylin–eosin (Shanghai Sang-gong Biotechnology Co., Shanghai, China) and observed under a light microscope (Nikon Eclipse50i, Tokyo, Japan).
Immunofluorescence staining
Frozen Sects. (6 μm thick) were fixed in 4% paraformaldehyde for 15 min at room temperature and incubated for 10 min in 0.2% TritonX-100 (Solarbio, Beijing, China). After three 5-min rinses with PBS, the sections were pre-incubated with 2% bovine serum albumin (Servicebio, Wuhan, China). Subsequently, they were each incubated with one of the following antibodies at 4 °C: anti-K12 (1:50, Abcam, UK), anti-K14 (1:50, Abcam, UK), or anti-PAX6 (1:50, Abcam, UK) antibodies for 14–16 h overnight. Following four PBS washes for 10 min each, the sections were incubated with AlexaFluor594-labeled immunoglobulin (1:300, Invitrogen, Carlsbad, CA, USA) at 25 °C for 1 h. After rinsing with PBS four times for 10 min each time, the slices were incubated with DAPI (Solarbio, Beijing, China) at 25 °C for 15 min, rinsed with PBS three times for 5 min each time, and images were captured using a laser confocal microscope.
Western blotting analysis
After culture, the epithelial cell slices were collected with a cell scraper and extracted from the cold lysis buffer composed of highly efficient RIPA tissue/cell lysate and protease inhibitors (Solarbio, Beijing, China). The protein concentration was determined using a BAC protein assay kit (Solarbio, Beijing, China). Western blotting analysis was carried out using anti-K12 (1:1000, Abcam, UK), anti-K14 (1:1000, Abcam, UK), and anti-PAX6 (1:500, Abcam, Cambridge, UK) antibodies. The results were visualized using an enhanced chemiluminescence reagent (Xiamen Lulong Company, Xiamen, China) and recorded using a transmittance meter (ChemiDoc XRS, Bio-Rad, Hercules, USA).
RNA extraction and RT-PCR
DAM, UAM, and UAM-MSC epithelial cell slices were collected via cell scraping, RNA was extracted using TRIzol® (Invitrogen, Carlsbad, CA, USA), and the same amount of RNA was reverse transcribed into cDNA using a high-efficiency reverse transcription kit (EZBioscience, Roseville, MN, USA). RT-PCR was conducted using the CFX96TM RT-PCR detection system and a 2 × SYBR Green qPCR Master Mix kit (EZBioscience, Roseville, MN, USA), following the manufacturer’s instructions. Regarding each experiment, a template-minus control, representing a response system without a template, was used as a negative control for subsequent PCR reactions. The amplification procedure involved denaturing for 5 min at 95 °C, followed by denaturing at 95 °C and annealing at 60 °C for 40 cycles. SYBR Green fluorescence was detected after each extension step, and the amplification specificity was evaluated via melting curve analysis. Compared with the GAPDH as internal control gene, the relative quantitative RT-PCR was analyzed using the comparative CT method. The primer pairs used are listed in Table 1.
Transplantation of tissue-engineered corneal epithelium in a rabbit total LSCD model
New Zealand rabbits were anesthetized with an intramuscular injection of 1% pentobarbital sodium (3 mL/kg). A 2 mm wide and 0.2 mm deep limbal lamellar keratectomy was performed on one eye of each rabbit and the central corneal epithelial cavity to establish an LSCD model. Subsequently, the animals were randomly divided into three groups: the first group underwent tissue-engineered corneal epithelium transplantation with DAM as the carrier, the second group with UAM as the carrier, and the third group with UAM-MSCs as the carrier. The tissue-engineered corneal epithelium was fixed to the corneal limbus of the recipient using a 10–0 suture. Subsequently, another complete layer of AM was fixed on the bulbar conjunctiva as a dressing to cover and protect the transplanted tissue-engineered corneal epithelium, which is a routine procedure in ocular surface reconstruction. After the operation, calf blood deproteinized ophthalmic gel (Sugaojie, Shenyang, China) was administered three times daily; tobramycin/dexamethasone eye drops (Alcon, USA), three times daily; and tobramycin/dexamethasone eye ointment (Alcon, Spain), once daily. Observations and imaging were performed every 2 days using a slit lamp microscope (Chongqing Kanghua Science and Technology, Chongqing, China). After 1 week, the AM dressing was removed. The repair of corneal epithelial injury, neovascularization and ocular surface Inflammatory index values were observed under slit lamp microscope. The animals were euthanized 2 weeks after the operation, and the cornea and limbal tissues were harvested for histological examination.
Evaluation of inflammation index value
Inflammatory index values were assigned based on the following evaluation: ciliary hyperemia (absent, 0; present but extending less than 1 mm, 1; hyperemia extending between 1 and 2 mm, 2; present and extending more than 2 mm, 3); central corneal edema (absent, 0; present with visible iris details, 1; present without visible iris details, 2; present without visible pupil, 3); and peripheral corneal edema (absent, 0; present with visible iris details, 1; present without visible iris details, 2; present with no visible iris, 3). The final inflammatory index result was obtained by summing the scores of the different parameters and dividing by 9 as previously reported37).
Protein IBT quantification
Tissue-engineered corneal epithelia from the DAM, UAM, and UAM-MSCs groups were cultured in SHEM at 37 °C in a 95% air and 5% CO2 incubator for 13 days, with the liquid changed every other day. On day 13, the SHEM was removed, washed gently with PBS twice, and replaced with serum-free SHEM without phenol red reagent. After 24 h of culture, the medium was collected, and each group was labeled. It was then transported to the Huada Genome Research Institute laboratory (Shenzhen, Guangdong, China) for IBT quantification under dry ice conditions (− 78.5 °C).
Gene Ontology (GO) classification, protein–protein interaction(PPI) analysis, and Kyoto Encyclopedia of genes and genomes (KEGG) pathway enrichment
GO classification (Beijing Huada Institute of Genomics, Shenzhen, Guangdong, China) combined with gene ontology analysis (www.geneontology.org) was used to analyze the function of differentially expressed genes. Protein interaction analysis of 207 differential genes was conducted using the Dr. Tom platform and PPI software. The related pathways were enriched via KEGG and visualized in a bubble diagram format.
Statistical analysis
Graphpad Prism 9 and ImageJ were used for data processing and analysis. Summary data are expressed as the mean ± standard deviation. Single-factor F analysis was used for comparing measurement data among multiple groups, and a t-test was used for comparison between groups, with p < 0.05 considered statistically significant.
Results
Biological and physical characteristics of the tissue-engineered corneal epithelium based on UAM-MSCs
Figure 1A demonstrates the in vitro expansion process of LSCs on DAM, UAM, and UAM-MSC surfaces observed under a microscope. Following epithelial inoculation, we noted that the cell size and smooth adhesion to the limbal epithelium surface were the similar in the two groups. As shown in Fig. 1A, the epithelium in all three groups initially adhered closely to the AM carrier, with cells gradually migrating to the D1–D3 periphery and displaying an oval epithelial-like shape. Starting from D4, adherent cells gradually proliferated outward, generally to the right of D8–D10, achieving 100% fusion of epithelial cells. At this stage, the air–liquid interface culture method was used, leading to the stratification and growth of cells within approximately 3 days. On day 14, stratified epithelial tissue formation was observed under a phase-contrast microscope, indicating readiness for stem cell transplantation. Figure 1B shows the growth of MSCs on the substrate side of AM. Generally, to the right of D8–D10, MSCs can reach 100% fusion state. Figure 1C-E shows the optical transparency of three types of tissue-engineered corneal epithelium. The transparency of UAM-MSCs was better than that of DAM. Although UAM-MSCs have an additional layer of cells compared with UAM, their transparency closely resembled that of UAM. Through in vitro observation of limbal stem cell expansion, no significant difference in the growth rate of epithelial cells was observed among the three carrier groups. The tissue-engineered corneal epithelium based on DAM, UAM, and UAM-MSCs was harvested and embedded in the OCT compound. Frozen Sections. (6 µm thick) were stained with hematoxylin–eosin. As shown in Fig. 1F, the tissue-engineered corneal epithelium based on DAM had approximately 3–5 layers of cells. The underlying AM matrix appears thinner after culture; however, its loose stroma structure remained evident. Adhesion between DAM and the epithelium was loose, with obviously separated edges. The tissue-engineering corneal epithelium based on UAM had approximately 5–7 cells with good polarity. The surface cells were flat, while the bottom cells were columnar. Compared with the UAM group, the tissue-engineered corneal epithelium based on UAM-MSCs was thicker, with flat and columnar surface and bottom cells, respectively.
Construction of tissue-engineered corneal epithelium based on DAM, UAM, and UAM-MSCs. (A) Amplification process of limbal stem cells on the epithelial surface of the three carriers. (B) Expansion process of mesenchymal stem cells on the stromal surface of UAM-MSCs. (C–E) Transparency of the three carriers. (F) Results of hematoxylin–eosin staining of tissue-engineered corneal epithelium based on the three carriers. Scale bars: 100 μm (A, B), 50 μm (D). DAM, de-epithelialized amniotic; UAM, ultra-thin amniotic membrane; UAM-MSCs, UAM-membrane mesenchymal stem cells.
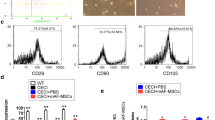
To further observe the cell phenotype of the tissue-engineered corneal epithelium based on UAM-MSCs, we collected epithelial specimens and detected the expression of cell-related markers by immunofluorescence staining, Western blotting, and RT-qPCR. Figure 2A demonstrates through immunofluorescence results that the expression of corneal progenitor cell marker K14 and corneal epithelial characteristic marker PAX6 in the UAM-MSC group was stronger than that in the other two groups. Western blotting (Fig. 2B) and RT-qPCR (Fig. 2C) analysis further proved that K14 expression in the UAM-MSC group was stronger than that in the other two groups. Additionally, RT-qPCR results showed that the expression of corneal progenitor cell markers p63 (Fig. 2F), PCNA (Fig. 2G) and corneal epithelial characteristic marker PAX6 (Fig. 2D) in the UAM-MSC group was higher than that in the other two groups. K12 (Fig. 2E), a marker of terminal differentiation in corneal epithelial cells, was the least expressed in the UAM group and the highest expressed in the DAM group. This discrepancy may be attributed to the increased thickness of the tissue-engineered corneal epithelium in the UAM-MSCs group.
Cell phenotype of tissue-engineered corneal epithelium. (A) Immunofluorescence staining results of K12(red), K14(red), PAX6(red), and the DAPI blue nucleus, which are related to corneal epithelial cell proliferation and differentiation. (B) Protein expression levels of K12, K14, and PAX6. (C–G) RNA expression levels of PCNA, PAX6, K12, p63, and K14. Scale bars: 50 μm (A).
Therapeutic effect of the novel UAM-MSCs tissue-engineered corneal epithelium on the limbal stem cell injury model
Initially, we scraped rabbit LSCs and central epithelial cells to establish a stem cell injury model. Subsequently, DAM, UAM, and UAM-MSC tissue-engineered corneal epithelium were transplanted into the animal injury model, followed by observation of epithelial growth with images analyzed using ImageJ. Figure 3A shows that after 7 days of transplantation, the AM excipients covered by the eye surface were not dissolved; no significant difference was observed among the three groups. After removing the AM dressing covering the tissue-engineered corneal epithelium, the corneal epithelial healing rate was significantly faster in the UAM-MSCs group than that in the UAM and DAM groups. Fourteen days after the operation, the corneal stroma remained turbid, with uneven corneal epithelium in the DAM group. Fluorescein sodium staining revealed patchy staining and incomplete epithelium in the lower periphery of the cornea. In the UAM transplantation group, the corneal stroma remained slightly opaque, with uneven corneal epithelium. Fluorescein sodium staining showed scattered corneal stroma in the center of the cornea, with an incomplete epithelium. However, in the UAM-MSCs transplantation group, the cornea was transparent, the graft adhered well to the corneal stroma, the corneal surface epithelium was smooth, and the fluorescein sodium staining was negative.
Tissue-engineered corneal epithelial transplantation in the treatment of limbal stem cell injury. (A) Slit lamp photography of the three types of tissue-engineered corneal epithelium for treating limbal stem cell deficiency. (B) Tracing of corneal epithelial stem cells using CFDASE before and 2 weeks after transplantation. (C) The Inflammatory index values of the three groups. (D) Three types of tissue-engineered corneal epithelium transplantation for treating limbal stem cell injury model rabbit cornea frozen section hematoxylin–eosin staining. Scale bars: 50 μm (C).
To confirm the identity of the transplanted rabbit corneal epithelium and determine its survival on the eye surface, we used CFDASE to trace the cells before transplantation (Fig. 3B). The eyeballs were removed 2 weeks after transplantation, and green fluorescence was found on the corneal surface of the three transplantation groups under a fluorescence microscope. The transplanted rabbit corneal epithelial cells were confirmed to be tissue-engineered corneal epithelial cells. However, the fluorescence in all three transplantation groups weakened after transplantation, likely due to corneal stem cell proliferation and the continuous, equal distribution of fluorescent agents caused by nuclear division.
The rabbits were euthanized 2 weeks after transplantation, and their corneas were sectioned and stained. Figure 3C shows that the Inflammatory index values of the three groups is not high. Moreover, the Inflammatory index values of the UAM-MSCs group is the lowest. Figure 3D reveals that the DAM group exhibited 2–3 layers of central corneal epithelial cells and 4–5 layers in the peripheral limbus. The UAM group displayed 3–4 layers of central corneal epithelial cells and 5–6 layers of corneal epithelial cells in the peripheral limbus. In the UAM-MSC group, there were 5–6 layers of central corneal epithelial cells and 6–7 layers of corneal epithelial cells in the peripheral limbus. Part of inflammatory cell infiltration (black arrow) was observed in limbal stroma in the DAM group. However, no obvious inflammatory cell infiltration was found in the UAM and UAM-MSCs groups.
To further determine the phenotype of corneal epithelial cells after transplantation, rabbit corneas were stained with immunofluorescence, and RT-qPCR was used to detect the expression of markers associated with cell differentiation (K12 and K3), progenitor cell-related (K14, and ABCG2) and corneal epithelial characteristic marker PAX6. Figure 4A demonstrates through immunofluorescence that the expression of the corneal epithelial progenitor cell marker K14 and corneal characteristic marker PAX6 was observed across all epithelial layers in the UAM-MSC group, with stronger expression than that in the other two groups. K12, a marker of terminal differentiation in corneal epithelial cells, was slightly expressed in the central cornea of the UAM-MSC group but not expressed in the limbus and was more pronounced in both the UAM and DAM groups. RT-qPCR analysis further confirmed the stronger expression of corneal progenitor cell markers p63 (Fig. 4D), ABCG2 (Fig. 4E), and corneal characteristic marker PAX6 (Fig. 4F) in the UAM-MSC group than that in the other two groups, while the expression of corneal epithelial terminal differentiation markers K3 (Fig. 4B) and K12 (Fig. 4C) was significantly lower than that in the other two groups. This indicates better preservation of the stem cell dryness in the corneal epithelium of rabbits in the UAM-MSC group.
Cell phenotype of rabbit corneal epithelial cells after three types of tissue-engineered transplantation. (A) Immunofluorescence staining results for K12(red), K14(red), PAX6(red), and the DAPI blue nucleus, which are related to corneal epithelial cell proliferation and differentiation. (B–F) RNA expression levels of K3, K12, p63, ABCG2, and PAX6. Scale bars: 100 μm (A).
To further observe the expression of rabbit corneal epithelial cell junction in the three groups after tissue-engineered corneal epithelial transplantation, the corneal specimens from rabbits were examined using transmission electron microscopy and RT-qPCR to detect the RNA expression of cell link markers Connexin43, E-cadherin, and Claudin1. Figure 5A shows the transmission electron microscopy results, revealing tighter cell–cell and cell-basement membrane junctions in the UAM-MSC group, and the RNA expression levels of Connexin43 (Fig. 5B) and E-cadherin (Fig. 5C) were higher in this group than that in the other two groups, indicating enhanced epithelial cell connectivity in the UAM-MSC group.
The junction of corneal epithelial cells after treatment of the LSCD model with three kinds of tissue-engineered corneal epithelial grafts. (A) Results of the transmission electron microscope examination of the cell junction. The yellow arrows show the thickness of tissue engineered corneal epithelium constructed by three kinds of carriers (magnification 1.0 k), and the green arrows and red arrows show 3.0 k and 20.0 k magnification, respectively. (B–D) RNA expression levels of cell junction-related markers Connexin 43, E-cadherin, and Claudin1. (E–F) RNA expression level of neovascularization factor TIMP-1 and thrombospondin-1. Scale bars: 10 μm (Aa, Ad, Ag), 5 μm (Ab, Ae, Ah), 500 nm (Ac, Af, Ai). LSCD, limbal stem cell dysfunction.
TIMPs and thrombospondin are anti-neovascularization-related factors mainly expressed in the basal cells of normal corneal epithelium, with these factors closely related to peripheral corneal neovascularization after transplantation. We collected RNA from rabbit corneal epithelium after tissue-engineered corneal epithelial transplantation. RT-PCR revealed higher expression levels of thrombospondin-1 (Fig. 5E) and TIMP-1 (Fig. 5F) in rabbit corneal epithelial cells in the UAM-MSC group than those of the other two groups. After introducing MSCs, the secretion of anti-neovascularization factors in corneal epithelial cells will also increase, reducing the risk of corneal neovascularization after transplantation.
Protein IBT quantification
To further understand the effect of MSCs on corneal epithelial cells and their mechanism, the culture medium for the tissue-engineered corneal epithelium based on DAM, UAM, and UAM-MSCs was collected and analyzed using mass spectrometry. As shown in Fig. 6B, there were 131 differentially expressed proteins between the UAM and DAM groups, including 76 upregulated and 55 downregulated proteins, while significant differences were observed between the UAM-MSC and DAM, UAM-MSC and UAM groups. There were 1,233 differentially expressed proteins between the UAM-MSC and UAM, including 674 upregulated and 559 downregulated proteins. Figure 6C–E shows the differentially expressed proteins between the UAM-MSC and UAM groups, with Fig. 6C showing their GO classification. there were 207 differentially expressed proteins between the UAM-MSC and UAM group, including 182 upregulated and 25 downregulated proteins, with fold changes exceeding threefold and p < 0.05. The most significant protein molecule was Cyclin1 (CCN1); the difference multiples was 9.82. Figure 6D illustrates the KEGG pathway enrichment results of the 207 differentially expressed genes. Figure 6E shows the interaction network map of the 207 differentially expressed proteins, of which Fibronectin1 (FN1) and (Triosephosphate Isomerase 1(TPI1) proteins exhibited the most interaction. FN1 and TPI1 interacted with 25 and 18 proteins, with difference multiples of 3.32 and 6.08, respectively.
Protein IBT quantification. (A) Differential proteins clustering heat map. (B) The number of differential genes between DAM, UAM and UAM-MSCs. (C) Classification of differentially expressed genes between the UAM-MSC and UAM groups. (D) Result of enrichment differentially expressed genes in the KEGG pathway (ratio > 3, p < 0.05). (E) Protein interaction network map of the differentially expressed genes. DAM, de-epithelialized amniotic; UAM, ultra-thin amniotic membrane; UAM-MSCs, UAM-membrane mesenchymal stem cells.
Discussion
The new UAM-MSCs carrier was beneficial for corneal epithelial reconstruction due to its transparency as a tissue carrier, improving recipient visual acuity compared with using full-thickness AM. Additionally, the basal surface inoculated with MSCs closely resembled the normal limbal anatomical structure. Concurrently, MSCs could secrete various factors during cell culture and after transplantation, enhancing the simulation of the limbal microenvironment. Therefore, UAM-MSCs may be an ideal carrier for constructing tissue-engineered corneal epithelium.
MSCs, regarded as multipotent progenitor cells, can arise from either embryonic or adult sources38. Wharton’s jelly umbilical cord, umbilical cord blood, placenta, and embryo can provide embryonic stem cells, whereas dental pulp, bone marrow, adipose tissue, and other tissues are considered adult sources39. Embryonic MSCs contain a large number of primitive phenotypes, more active telomeres, and higher propagation ability compared with stem cells derived from adult tissues40. In addition, compared with other MSCs, MSCs from umbilical cord is a medical waste, easy to obtain, and does no harm patients. Therefore, we chose umbilical cord source MSCs.
Cultivated limbal epithelial cell transplantation (CLET) are cultured in vitro by taking a small piece of limbal tissue from donor eyes, amplifying epithelial cells with or without trophoblast cells, and transplanting them with cell carriers41,42. CLET can greatly reduce the complications of limbal transplantation (in the case of autologous or allogeneic limbal tissue transplantation), prompting ongoing research for suitable CLET methods43. Presently, the prevalent culture method involves culturing cells using heterogeneous cell culture products without feeder layer cells (such as serum and growth factors)44. Although the use of trophoblast cells is not necessary when culturing CLET, it provides a suitable microenvironment similar to the limbal niche for LESC self-renewal and maintenance. Mouse 3T3 cells treated with radiation or mitomycin C (mitosis inactive) have been used to feed cells41,42. Limbal mesenchymal cells, a variety of non-hematopoietic fibroblasts with plasticity, are an important component of limbal niches that maintain the activity and potential of LESCs by secreting nutritional factors and various cytokines45,46. Therefore, we used MSCs as trophoblast cells to culture LSCs in vitro. Our study showed that the corneal epithelial cells amplified by our constructed UAM-MSCs vector could have normal epithelial cell polarity with flat surface cells and columnar basal layer cells. The preservation of corneal epithelial cell phenotype transplanted into UAM-MSCs was verified by detecting the expression of K12, K3, K14, PAX6, and ABCG2. K14, expressed in the basal cells of the human limbal and central corneal epithelium, is a marker of basal cells with mitotic activity in the stratified epithelium47. K14 is an important keratin expressed in the stratified epithelium, involved in cell proliferation and migration48. K3 and K12, marking terminally differentiated corneal epithelial cells, were not expressed in normal limbal epithelial basal cells49. PAX6 is essential for vertebrate eye development. It can directly or indirectly regulate a variety of proteins and transcription factors, promote cell proliferation, and inhibit apoptosis50. ABCG2 is a positive marker of LSCs, specifically expressed in the basal layer of the limbal epithelium51. Our results showed that the basal cells of tissue-engineered corneal epithelium cultured with UAM-MSCs were negative for K3 and K12, with high K14 expression, while the cells above the basal layer were positive for K3 and K12, with low K14 expression. The expression pattern of cytokeratin showed undifferentiated basal cell progenitor phenotypes, with corneal differentiated phenotypes in cells above the basal layer. ABCG2 is highly expressed in tissue-engineered epithelium based on UAM-MSCs, supporting the notion that UAM-MSCs help maintain the state of limbal progenitor cells. High expression of PAX6 in UAM-MSCs-based tissue-engineered epithelium suggests superior maintenance of corneal epithelial characteristics. The existence of these markers indicates normal differentiation of UAM-MSCs-based engineered corneal epithelium, closely resembling the response of limbal epithelial cells in vivo and constructing tissue-engineered corneal epithelium closer to the normal cornea.
Limbal niche deficiency/dysfunction plays a major pathological role in the loss of regenerative ability in LESCs. Previous studies have shown that in severe LSCD cases, simple LESC supplementation may be insufficient52,53,54,55. Specifically, when epithelial stem cells are transplanted into the hostile ocular surface environment, restoring a healthy stem cell niche becomes unfeasible, leading to the potential loss of LSCs over time. Therefore, simultaneous restoration of the limbal stem cell niche is essential during tissue-engineered corneal epithelial transplantation. The strategy focuses on reducing inflammation and restoring the normal function of resident cells and ECM. In severe injuries, persistent pathological inflammation of the limbus and cornea changes the function of LESCs56. Studies have shown that inflammation significantly induces the production and release of neutrophils, resulting in the expression of interleukin (IL)-6, IL-8, and tumor necrosis factor-α57 through the nuclear factor kappa B and P38MAPK signaling pathways and changing cell interactions and regulatory proteins, resulting in structural interference of limbal niches and loss of stem cell markers for LESCs58,59. Therefore, inflammation control regulates neutrophil changes to reduce the inflammatory response. Complements and neutrophils are two key elements of the innate immune system60. Studies have shown that MSCs exosome inhibits complement activation through CD59, disrupts the feedback cycle between complement and neutrophils, and inhibits the amplification and persistence of inflammation during infection60. In addition, studies have shown that T cells are crucial for regulating inflammation61. MSCs exosome has immunomodulatory properties, which significantly inhibit the immune response of cytotoxic T cells (Tc1 cells) and type 1 helper T cells (Th1), reduce the levels of pro-inflammatory factor α and interferon-γ, and induce regulatory T cells and anti-inflammatory IL-10 levels62. CCN1 produced by fibroblasts and endothelial cells, is considered an important matrix protein. Through the combination of various integrins to promote tissue repair and immune cell adhesion and combining with a variety of immune cells, including T cells, B cells, NK cells, and monocytes, to achieve immune regulation, CCN1 can inhibit acute inflammation in vivo63. Thus, as resident cells in the limbal niche, MSCs can also secrete normal ECM components, such as type I collagen and CCN1, reconstruct ECM, further restore the cellular microenvironment, and considerably promote corneal epithelial cell proliferation and differentiation35,64.
Epithelial cell junctions, including the tight junctions between epithelial cells and the semi-desmosome structures between epithelial cells and the basement membrane65, are essential for maintaining the epithelial barrier function. Under normal circumstances, the corneal epithelium expresses ZO-1, Claudin-1, Ocludin, and other intercellular adhesion molecules to maintain corneal barrier function. Integrin protein on the basement membrane of epithelial cells interconnects with other ECM components such as collagen and laminin through receptor-ligand binding66,67, which is crucial for maintaining the stability of epithelial cells. When the ECM and basement membrane are destroyed and collagenase production increases, new intact epithelial cells produced through normal corneal metabolism cannot adhere to the basement membrane, and the tight junction function between cells will not be restored. At this time, delayed epithelial repair or healing will lead to ulcers. After introducing MSCs, they not only directly bind to LESCs through various molecular substrates and signaling pathways, which promotes the connection between corneal epithelial cells and the basement membrane, but also secrete normal corneal ECM components, such as type I collagen, to reconstruct the ECM and restore the cellular microenvironment. Therefore, the cell–cell and cell-basement membrane connections after MSCs-UAM-based corneal epithelial transplantation are tighter. We suggest that the cornea transplanted with this corneal epithelium has improved corneal barrier function and reduced susceptibility to corneal epithelial-related diseases.
After a corneal injury, persistent hypoxia and inflammation reduce the anti-angiogenesis and colony-forming ability of LESCs, leading to an imbalance between pro-angiogenic and anti-angiogenic factors, which stimulates the production of pathological heme and lymphatic vessels, leading to excessive angiogenic stimulation20. Angiogenic mediators include vascular endothelial growth factor, matrix metalloproteinases, basic fibroblast growth factor, platelet-derived growth factor, and interleukin-168,69. MSCs can reduce corneal inflammation by inhibiting the infiltration of inflammatory cells into the corneal stroma34, reducing the production of pro-inflammatory cytokines by macrophages70, preventing the formation of peroxynitrite, a toxic reaction product between nitric oxide and superoxide, to reduce apoptosis, the level of MMP, and the production of pro-inflammatory cytokines, thus inhibiting corneal inflammation and neovascularization, significantly promoting corneal healing34,35. TPI1 (propionate phosphate isomerase 1) is an enzyme involved in the process of glycolysis. Exosomes with a low TPI1 knockout can promote glycolysis in receptor cells. Exosomes treated with low TPI1 knockout can increase glucose uptake, lactic acid secretion, and ATP production, reprogram glucose metabolism in recipient cells, subsequently promoting tumor progression. Therefore, TPI1 can inhibit the growth, migration, and invasion of hepatocellular carcinoma cells71,72. Owing to the high expression of the anti-neovascularization factor, metabolic regulation by TPI1, and the denser carrier structure, we anticipate that the rabbit corneas transplanted with UAM-MSC corneal epithelial cells will maintain transparency for an extended duration.
The limitation is that, In this experiment, we have not yet verified whether MSCs could remain on the surface of rabbit cells after transplantation. There are concerns about their uncontrolled proliferation or overgrowth, which can lead to unwanted effects. Implementing kill switches in the context of MSCs involves incorporating mechanisms to control and terminate their growth when necessary. One potential approach is to engineer MSCs with genetic circuits that allow for conditional cell death or growth arrest. These circuits can be designed to respond to specific signals or triggers in the cellular environment73. In the next experiment, we will further clarify the fate of MSCs after transplantation into the cornea to ensure procedural safety. In addition, the culture of rabbit cells on human AM and the transplantation of human AM and MSCs into rabbits cells may lead to the risk of rejection. However, MSCs, considered to be immune-privileged cells74, also exhibit potential immunomodulatory effects through affecting the innate immune system by suppressing the maturation and activation of dendritic cells (DCs) as well as the cytotoxicity of natural killer cells and suppressing adaptive immune responses by inhibiting the proliferation and secretion of cytokines by T cells, as well as impeding the maturation of B cells75. In the course of our experiment, no obvious rejection was observed. At the same time, we routinely use anti-inflammatory and anti-rejection drugs after operation, which can avoid the risk of rejection after transplantation to the greatest extent.
In summary, we designed a new tissue-engineered corneal epithelial carrier (UAM-MSCs). Through a controlled digestion scheme, we removed part of the DAM matrix to increase its transparency. Concurrently, we inoculated MSCs on their substrate to better mimic the limbal microenvironment. The UAM-MSC-based tissue-engineered corneal epithelium had better transparency, anti-neovascularization, and a closer intercellular connection, closely resembling the natural corneal epithelial tissue phenotype, and could significantly improve the efficacy of keratoplasty in the LSCD animal model. This obvious improvement indicates that UAM-MSCs may be an ideal carrier for constructing tissue-engineered corneal epithelium. However, although most MSC-related animal clinical trials are ongoing and numerous human clinical trials are in the early stages, comprehensive clinical results, including adverse reactions, remain undetermined. Additionally, the quest for clinical safety has spurred the exploration of MSC-derived structures, such as extracellular vesicles, in preclinical and clinical trials76. We will attempt to use MSC derivatives to further improve surgical efficacy. Furthermore, we anticipate the potential utilization of UAM-MSCs to construct other eye tissues based on cell therapy, such as tissue-engineered corneal endothelium and retinal pigment epithelium, to address critical needs in the treatment of vision-threatening eye diseases.
Data availability
Data is provided within the manuscript and supplementary information file.
References
DelMonte, D. W. & Kim, T. Anatomy and physiology of the cornea. J. Cataract Refract. Surg. 37(3), 588–598 (2011).
Schermer, A., Galvin, S. & Sun, T. T. Differentiation-related expression of a major 64K corneal keratin in vivo and in culture suggests limbal location of corneal epithelial stem cells. J. Cell Biol. 103(1), 49–62 (1986).
Lavker, R. M. & Sun, T. T. Epithelial stem cells: The eye provides a vision. Eye 17(8), 937–942 (2003).
Dua, H. S., Shanmuganathan, V. A., Powell-Richards, A. O., Tighe, P. J. & Joseph, A. Limbal epithelial crypts: A novel anatomical structure and a putative limbal stem cell niche. Br. J. Ophthalmol. 89(5), 529–532 (2005).
Tseng, S. C. Concept and application of limbal stem cells. Eye 3(Pt 2), 141–157 (1989).
Li, W., Hayashida, Y., Chen, Y. T. & Tseng, S. C. Niche regulation of corneal epithelial stem cells at the limbus. Cell Res. 17(1), 26–36 (2007).
Dua, H. S., Saini, J. S., Azuara-Blanco, A. & Gupta, P. Limbal stem cell deficiency: concept, aetiology, clinical presentation, diagnosis and management. Indian J. Ophthalmol.. 48(2), 83–92 (2000).
Ahmad, S., Figueiredo, F. & Lako, M. Corneal epithelial stem cells: Characterization, culture and transplantation. Regen. Med. 1(1), 29–44 (2006).
Pellegrini, G. et al. Long-term restoration of damaged corneal surfaces with autologous cultivated corneal epithelium. Lancet 349(9057), 990–993 (1997).
Marchini, G. et al. Long-term effectiveness of autologous cultured limbal stem cell grafts in patients with limbal stem cell deficiency due to chemical burns. Clin. Exp. Ophthalmol. 40(3), 255–267 (2012).
Movahedan, A. et al. Long-term outcomes of ocular surface stem cell allograft transplantation. Am. J. Ophthalmol. 184, 97–107 (2017).
Eslani, M. et al. Late acute rejection after allograft limbal stem cell transplantation: Evidence for long-term donor survival. Cornea 36(1), 26–31 (2017).
Cheung, A. Y., Sarnicola, E. & Holland, E. J. Long-term ocular surface stability in conjunctival limbal autograft donor eyes. Cornea 36(9), 1031–1035 (2017).
Li, W., Hayashida, Y., He, H., Kuo, C. L. & Tseng, S. C. The fate of limbal epithelial progenitor cells during explant culture on intact amniotic membrane. Invest. Ophthalmol. Vis. Sci. 48(2), 605–613 (2007).
Man, R. C. et al. Corneal regeneration by induced human buccal mucosa cultivated on an amniotic membrane following alkaline injury. Mol. Vis. 23, 810–822 (2017).
Sudha, B., Sitalakshmi, G., Iyer, G. K. & Krishnakumar, S. Putative stem cell markers in limbal epithelial cells cultured on intact & denuded human amniotic membrane. Indian J. Med. Res. 128(2), 149–156 (2008).
Zhang, L. et al. An ultra-thin amniotic membrane as carrier in corneal epithelium tissue-engineering. Sci. Rep. 6, 21021 (2016).
Galal, A., Perez-Santonja, J. J., Rodriguez-Prats, J. L., Abad, M. & Alio, J. Human anterior lens capsule as a biologic substrate for the ex vivo expansion of limbal stem cells in ocular surface reconstruction. Cornea 26(4), 473–478 (2007).
Dravida, S. et al. A biomimetic scaffold for culturing limbal stem cells: A promising alternative for clinical transplantation. J. Tissue Eng. Regen. Med. 2(5), 263–271 (2008).
Polisetti, N., Zenkel, M., Menzel-Severing, J., Kruse, F. E. & Schlötzer-Schrehardt, U. Cell adhesion molecules and stem cell-niche-interactions in the limbal stem cell niche. Stem Cells (Dayton, Ohio) 34(1), 203–219 (2016).
Kulkarni, B. B. et al. Comparative transcriptional profiling of the limbal epithelial crypt demonstrates its putative stem cell niche characteristics. BMC Genom. 11, 526 (2010).
Higa, K., Shimmura, S., Miyashita, H., Shimazaki, J. & Tsubota, K. Melanocytes in the corneal limbus interact with K19-positive basal epithelial cells. Exp. Eye Res. 81(2), 218–223 (2005).
Huang, M. et al. Roles of limbal microvascular net and limbal stroma in regulating maintenance of limbal epithelial stem cells. Cell Tissue Res. 359(2), 547–563 (2015).
Chidambaranathan, G. P. et al. In vivo confocal microscopic analysis of limbal stroma in patients with limbal stem cell deficiency. Cornea 34(11), 1478–1486 (2015).
Katikireddy, K. R. & Jurkunas, U. V. Limbal stromal tissue specific stem cells and their differentiation potential to corneal epithelial cells. Methods Mol. Biol. 1341, 437–444 (2016).
Massie, I. et al. Advanced imaging and tissue engineering of the human limbal epithelial stem cell niche. Methods Mol Biol. 1235, 179–202 (2015).
Yamada, K. et al. Mesenchymal-epithelial cell interactions and proteoglycan matrix composition in the presumptive stem cell niche of the rabbit corneal limbus. Mol. Vis. 21, 1328–1339 (2015).
Higa, K. et al. Aquaporin 1-positive stromal niche-like cells directly interact with N-cadherin-positive clusters in the basal limbal epithelium. Stem Cell Res. 10(2), 147–155 (2013).
Xie, H. T., Chen, S. Y., Li, G. G. & Tseng, S. C. Limbal epithelial stem/progenitor cells attract stromal niche cells by SDF-1/CXCR4 signaling to prevent differentiation. Stem Cells 29(11), 1874–1885 (2011).
Han, B., Chen, S. Y., Zhu, Y. T. & Tseng, S. C. Integration of BMP/Wnt signaling to control clonal growth of limbal epithelial progenitor cells by niche cells. Stem Cell Res. 12(2), 562–573 (2014).
Notara, M., Shortt, A. J., Galatowicz, G., Calder, V. & Daniels, J. T. IL6 and the human limbal stem cell niche: A mediator of epithelial-stromal interaction. Stem Cell Res. 5(3), 188–200 (2010).
Lin, N. et al. Nerve growth factor-mediated paracrine regulation of hepatic stellate cells by multipotent mesenchymal stromal cells. Life Sci. 85(7–8), 291–295 (2009).
Fu, S. P. et al. The role and mechanisms of mesenchymal stem cells regulating macrophage plasticity in spinal cord injury. Biomed. Pharmacother. 168, 115632 (2023).
Yao, L. et al. Role of mesenchymal stem cells on cornea wound healing induced by acute alkali burn. PloS One 7(2), e30842 (2012).
Cejkova, J. et al. Suppression of alkali-induced oxidative injury in the cornea by mesenchymal stem cells growing on nanofiber scaffolds and transferred onto the damaged corneal surface. Exp. Eye Res. 116, 312–323 (2013).
Mao, Y. et al. Downregulation of p38 MAPK signaling pathway ameliorates tissue-engineered corneal epithelium. Tissue Eng. A 28(23–24), 977–989 (2022).
Liu, X. et al. Anti-angiogenic and anti-inflammatory effects of SERPINA3K on corneal injury. PLoS One 6(1), e16712 (2011).
DuFunderburghMannSundarRajFunderburgh, Y. M. L. M. M. N. J. L. Multipotent stem cells in human corneal stroma. Stem Cells 23(9), 1266–1275 (2005).
Bajada, S., Mazakova, I., Richardson, J. B. & Ashammakhi, N. Updates on stem cells and their applications in regenerative medicine. J. Tissue Eng. Regen Med. 2(4), 169–183 (2008).
Guillot, P. V., Gotherstrom, C., Chan, J., Kurata, H. & Fisk, N. M. Human first-trimester fetal MSC express pluripotency markers and grow faster and have longer telomeres than adult MSC. Stem Cells 25(3), 646–654 (2007).
Sharma, S. M. et al. Comparative analysis of human-derived feeder layers with 3T3 fibroblasts for the ex vivo expansion of human limbal and oral epithelium. Stem Cell Rev. Rep. 8(3), 696–705 (2012).
Miyashita, H. et al. A novel NIH/3T3 duplex feeder system to engineer corneal epithelial sheets with enhanced cytokeratin 15-positive progenitor populations. Tissue Eng. A 14(7), 1275–1282 (2008).
Kim, J. Y., Djalilian, A. R., Schwartz, G. S. & Holland, E. J. Ocular surface reconstruction: Limbal stem cell transplantation. Ophthalmol. Clin. N. Am. 16(1), 67–77 (2003).
Ramírez, B. E. et al. Stem cell therapy for corneal epithelium regeneration following good manufacturing and clinical procedures. BioMed Res. Int. 2015, 408495 (2015).
Sahu, A., Foulsham, W., Amouzegar, A., Mittal, S. K. & Chauhan, S. K. The therapeutic application of mesenchymal stem cells at the ocular surface. Ocular Surf. 17(2), 198–207 (2019).
Branch, M. J. et al. Mesenchymal stem cells in the human corneal limbal stroma. Invest. Ophthalmol. Vis. Sci. 53(9), 5109–5116 (2012).
Schlötzer-Schrehardt, U. & Kruse, F. E. Identification and characterization of limbal stem cells. Exp. Eye Res. 81(3), 247–264 (2005).
Patel, G. K., Wilson, C. H., Harding, K. G., Finlay, A. Y. & Bowden, P. E. Numerous keratinocyte subtypes involved in wound re-epithelialization. J. Investing. Dermatol. 126(2), 497–502 (2006).
Pitz, S. & Moll, R. Intermediate-filament expression in ocular tissue. Prog. Retinal Eye Res. 21(2), 241–262 (2002).
Ueno, H. et al. Experimental transplantation of corneal epithelium-like cells induced by Pax6 gene transfection of mouse embryonic stem cells. Cornea 26(10), 1220–1227 (2007).
de Paiva, C. S., Chen, Z., Corrales, R. M., Pflugfelder, S. C. & Li, D. Q. ABCG2 transporter identifies a population of clonogenic human limbal epithelial cells. Stem Cells 23(1), 63–73 (2005).
Vazirani, J. et al. Autologous simple limbal epithelial transplantation for unilateral limbal stem cell deficiency: multicentre results. Br. J. ophthalmol. 100(10), 1416–1420 (2016).
Basu, S. et al. Simple limbal epithelial transplantation: Long-term clinical outcomes in 125 cases of unilateral chronic ocular surface burns. Ophthalmology 123(5), 1000–1010 (2016).
Ganger, A., Vanathi, M., Mohanty, S. & Tandon, R. Long-term outcomes of cultivated limbal epithelial transplantation: Evaluation and comparison of results in children and adults. BioMed Res. Int. 2015, 480983 (2015).
Shen, C., Chan, C. C. & Holland, E. J. Limbal stem cell transplantation for soft contact lens wear-related limbal stem cell deficiency. Am. J. Ophthalmol. 160(6), 1142–9.e1 (2015).
Sivaraman, K. R. et al. Superior limbic keratoconjunctivitis-like inflammation in patients with chronic graft-versus-host disease. Ocul. Surf. 14(3), 393–400 (2016).
Jiang, M. et al. Keratinocyte exosomes activate neutrophils and enhance skin inflammation in psoriasis. FASEB J. 33(12), 13241–13253 (2019).
Notara, M. et al. Short-term uvb-irradiation leads to putative limbal stem cell damage and niche cell-mediated upregulation of macrophage recruiting cytokines. Stem Cell Res. 15(3), 643–654 (2015).
Nubile, M. et al. Pathological changes of the anatomical structure and markers of the limbal stem cell niche due to inflammation. Mol. Vis. 19, 516–525 (2013).
Loh, J. T. et al. Mechanism for the attenuation of neutrophil and complement hyperactivity by MSC exosomes. Cytotherapy 24(7), 711–719 (2022).
Nosbaum, A. et al. Cutting edge: Regulatory T cells facilitate cutaneous wound healing. J. Immunol. 196(5), 2010–2014 (2016).
Guo, L. et al. Extracellular vesicles from mesenchymal stem cells prevent contact hypersensitivity through the suppression of Tc1 and Th1 cells and expansion of regulatory T cells. Int. Immunopharmacol. 74, 105663 (2019).
Löbel, M. et al. CCN1: A novel inflammation-regulated biphasic immune cell migration modulator. Cell. Mol. Life Sci. CMLS 69(18), 3101–3113 (2012).
Katikireddy, K. R., Dana, R. & Jurkunas, U. V. Differentiation potential of limbal fibroblasts and bone marrow mesenchymal stem cells to corneal epithelial cells. Stem Cells 32(3), 717–729 (2014).
Thill, M. et al. A novel population of repair cells identified in the stroma of the human cornea. Stem Cells Dev. 16(5), 733–745 (2007).
Coelho, N. M., González-García, C., Salmerón-Sánchez, M. & Altankov, G. Arrangement of type IV collagen and laminin on substrates with controlled density of -OH groups. Tissue Eng. A 17(17–18), 2245–2257 (2011).
LeBleu, V. S., Macdonald, B. & Kalluri, R. Structure and function of basement membranes. Exp. Biol. Med. 232(9), 1121–1129 (2007).
Chang, J. H. et al. Corneal neovascularization: An anti-VEGF therapy review. Surv. Ophthalmol. 57(5), 415–429 (2012).
Han, K. Y., Chang, J. H., Lee, H. & Azar, D. T. Proangiogenic interactions of vascular endothelial MMP14 with VEGF receptor 1 in VEGFA-mediated corneal angiogenesis. Invest. Ophthalmol. Vis. Sci. 57(7), 3313–3322 (2016).
Aggarwal, S. & Pittenger, M. F. Human mesenchymal stem cells modulate allogeneic immune cell responses. Blood 105(4), 1815–1822 (2005).
Liu, B. H. M. et al. TPI1-reduced extracellular vesicles mediated by Rab20 downregulation promotes aerobic glycolysis to drive hepatocarcinogenesis. J. Extracell. Vesicles 10(10), e12135 (2021).
Jiang, H. et al. Triosephosphate isomerase 1 suppresses growth, migration and invasion of hepatocellular carcinoma cells. Biochem. Biophys. Res. Commun. 482(4), 1048–1053 (2017).
Sardesai, V. S., Shafiee, A., Fisk, N. M. & Pelekanos, R. A. Avoidance of maternal cell contamination and overgrowth in isolating fetal chorionic villi mesenchymal stem cells from human term placenta. Stem Cells Transl. Med. 6(4), 1070–1084 (2017).
Wong, R. S. Mesenchymal stem cells: Angels or demons?. J. Biomed. Biotechnol.. 2011, 459510 (2011).
De Miguel, M. P. et al. Immunosuppressive properties of mesenchymal stem cells: Advances and applications. Curr. Mol. Med.. 12(5), 574–591 (2012).
Galieva, L. R., James, V., Mukhamedshina, Y. O. & Rizvanov, A. A. Therapeutic potential of extracellular vesicles for the treatment of nerve disorders. Front. Neurosci. 13, 163 (2019).
Acknowledgements
The authors are grateful to Dr. Wei Li (Xiamen University) for his critical reading and valuable suggestions on the manuscript. Our gratitude is also due to the editor and all peer reviewers who donated their valuable time to assess and help improve the manuscript.
Funding
This work was partly supported by the Provincial Science and Technology Department of Guizhou Province, Qian Kehe Support [2020] (4Y145) for LiYing Zhang, the National Natural Science Foundation of China (82060173) for LiYing Zhang, Fujian Provincial Science Fund for Distinguished Young Scholars: 2023J06053) for Shangkun Ou, Provincial Science and Technology Department of Guizhou Province, Qian Kehe Surport [2022] (Yiban 184) for Hao Gu, and Guizhou Provincial Science and Technology Projects (QKHJC-ZK[2024]ZD043) for Shangkun Ou. The funders had no role in study design, data collection and analysis, decision on publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
Sk. Ou., Ly. Z, and H. G. designed the research; Qr. L. and C. H. performed the research; H. J., S. Z., Ll. Z. and Xe. Z. analyzed the experimental data; and Qr. L. and C. H. wrote the paper.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Long, Q., Huang, C., Zhang, L. et al. A novel tissue-engineered corneal epithelium based on ultra-thin amniotic membrane and mesenchymal stem cells. Sci Rep 14, 17407 (2024). https://doi.org/10.1038/s41598-024-68219-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-68219-8
- Springer Nature Limited