Abstract
This study aimed to investigate the univariate and bivariate effects of ambient temperature and air pollutants on 57,251 inpatients with AECOPD (Acute Exacerbation of Chronic Obstructive Pulmonary Disease) in Ganzhou from January 1, 2016, to December 31, 2019. We categorized the daily mean temperature and air pollutant variables based on the exposure–response curve of the Distributed Lag Non-Linear Model. Poisson regression model was used for interaction and stratification analysis. The Relative Excess Risk due to Interaction (RERI) with 95% confidence intervals (95% CI) between daily mean temperature (Tmean) and air pollutants including NO2, PM2.5, and PM10 were − 0.428 (95% CI − 0.637, − 0.218), -− 0.227 (95% CI − 0.293, − 0.161), and − 0.119 (95% CI − 0.159, − 0.079). Further stratification analysis showed the relative risk (RR) (95% CI) of high NO2 (> 33 μg/m3) at low Tmean (≤ 28 °C) was 1.119 (95% CI 1.096, 1.142). Low temperatures with high PM10 in men and high PM2.5 in women were associated with a higher risk of AECOPD hospitalization. The results indicate a higher risk of hospitalization for AECOPD when there is with high concentrations of air pollution at low temperatures.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Introduction
Chronic obstructive pulmonary disease (COPD) is a prevalent chronic respiratory disease characterized by progressive and irreversible airflow limitation. According to the Global Burden of Disease study, COPD ranks as the third leading cause of death in China, with the mortality rate continuing to rise1. Acute exacerbation of chronic obstructive pulmonary disease (AECOPD) refers to the progressive deterioration of respiratory symptoms in patients with COPD2. AECOPD represents a critical stage in the course of COPD. If left untreated and allowed to deteriorate, it can result in accelerated lung function decline, reduced quality of life, and increased mortality rates3,4.
Currently, most studies primarily focus on analyzing the individual risks associated with ambient temperature or air pollutants on the incidence or mortality of respiratory diseases. For instance, a study conducted in Shenyang, China, found that both air pollution and temperature increase the risk of hospital admissions for AECOPD5. A case-crossover study in Brazil6 revealed a positive correlation between exposure to high temperature environments and the admission rate of COPD. Furthermore, air pollutants such as particulate matter PM2.5 and PM10 have been known to exacerbate respiratory symptoms, leading to hospitalizations and, in severe cases, even fatalities among individuals with respiratory diseases7. In another particular study conducted in Ganzhou City of China, it was observed that air pollution significantly increased the risk of COPD admissions. Specifically, each 10 µg/m3 increase in PM2.5, PM10, NO2, and O3 was associated with a significant elevation of 2.8% (95% CI 1.0–4.7), 1.3% (95%CI 0.3–2.4), 2.8% (95% CI 0.4–5.4), and 1.5% (95% CI 0.2–2.7), respectively, in daily hospital admissions for COPD8.
The effects of air pollution and temperature changes on AECOPD were also analyzed in several regions of Asia. Studies from other Asian regions can offer valuable insights due to the similar topographical and geographic factors. For example, it was found in Korea that particulate matter and air pollution increased the probability of severe AECOPD events, and the association was well analyzed using the comprehensive Air quality index9. Similarly, a follow-up study of patient data in Korea showed that low ambient temperature and air pollution, especially PM10, were associated with the worsening of COPD10. However, the increase of PM10 level caused by seasonal haze in Chiang Mai was significantly associated with the emergency treatment of acute exacerbation of COPD11, and the another study in Taiwan of China found that PM2.5 was significantly correlated with AECOPD hospitalizations in cold seasons12.
However, it is important to note that ambient temperature and air pollutants do not act in isolation when it comes to the occurrence and development of human diseases. In many cases, there was a synergistic effect or interaction between these factors13,14. In a previous study in Athens and surrounding areas, the interaction between air pollution and temperature was investigated. This ecological study utilized multiple linear regression models and found that there was a synergistic effect between air pollution and temperature, resulting in excess mortality in Athens15. A study conducted in Shijiazhuang, China, revealed a significant interaction between PM2.5 and meteorological factors. The findings indicated that high levels of PM2.5 exposure were positively correlated with an increased risk of AECOPD. Moreover, the risk of AECOPD was found to be higher under conditions of low temperature and low humidity16. In 2008, a study was conducted in Wuhan, China, to investigate the interaction between temperature and air pollutants on mortality in the Chinese population17, the study found that during the high temperature period, each 10 µg/m3 increase in PM10 was associated with a 3.02% (95% CI 1.03%–5.04%) increased risk of death from cardiopulmonary diseases.
For AECOPD hospitalization risk, the interaction effects of ambient temperature and air pollution, especially how each different air pollutant interacts with temperature, are inconsistent. In addition, the influence of gender on the interaction of environmental factors is not clear, so it is still important to carefully explore the interaction between ambient temperature and air pollution and analyze the effect of stratification on hospitalization of AECOPD disease.
The main focus of this study was to analyze the effects of PM2.5, PM10, NO2, and ambient temperature, as well as their interactions, on AECOPD hospitalizations in Ganzhou City. By examining the combined effects of ambient temperature and air pollution factors on population health risks, the study aimed to facilitate effective health risk assessments related to ambient temperature and air pollution. The findings have the potential to provide a scientific basis for developing strategies to promote population health in the region.
Methods
Data
Ganzhou City is indeed the prefecture-level city with the largest land area and population in Jiangxi Province, located in southern China (Supplemental Fig. 1). Ganzhou City experiences a typical subtropical monsoon humid climate, with concentrated precipitation occurring in spring and summer. Additionally, the concentration of major pollutants in the air is relatively low, resulting in less polluted air quality. The urbanization rate of permanent residents in Ganzhou City stands at 57.0%18, Ganzhou City appears that while the city is experiencing rapid development, it still lags behind in terms of overall urbanization compared to some other areas. There are three main reasons to choose Ganzhou as the research area: (1) It has typical climatic characteristics. (2) The rapid urbanization process has brought about problems such as climate change and environmental pollution. (3) Its climate, environmental, social and economic data are relatively complete and abundant.
Through the DRGs (Diagnosis Related Groups) platform of Jiangxi Province19, we collected the data of daily AECOPD inpatients in Ganzhou City from January 1, 2016 to December 31, 2019. The case information included hospitalization date, disease diagnosis code (ICD-10), disease diagnosis name, gender, and did not involve patient privacy. The main hospitalization diagnosis was unspecified COPD with acute exacerbation (ICD-10: J44.1), and 57,251 hospitalized cases that matched the disease diagnosis name AECOPD were included in the analysis. This study was conducted according to the guidelines of the Declaration of Helsinki, and all procedures involving human subjects were approved by the ethics committee of Gannan Medical University (Approval No. 2021107), the need to obtain informed consent was waived by the ethics committee of Gannan Medical University.
The meteorological data utilized in this study were obtained from the National Meteorological Data Center (http://data.cma.cn/). The dataset of daily mean temperature (°C) was recorded by four meteorological monitoring stations (Supplemental Fig. 1), and the average values were calculated to derive the daily meteorological data. On the other hand, the air pollutant data employed in this research were sourced from the national urban air quality real-time publishing platform of China environmental monitoring station (https://www.aqistudy.cn/). This dataset included the daily mean concentrations of PM2.5, PM10, and NO2 during the same period. It is important to note that the pollutant data were complete and available for analysis.
Statistical analysis
The statistical description of the daily mean temperature (Tmean), air pollutant concentrations (PM2.5, PM10, NO2), and the number of inpatients with acute exacerbation of chronic obstructive pulmonary disease (AECOPD) was conducted using various measures such as the mean and standard deviation (\(\overline{x }\pm s\)), percentiles (P25, P50, and P75), interquartile range (IQR), and range. To examine the relationship between meteorological variables and pollutant variables, Spearman's correlation analysis was employed.
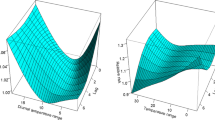
Furthermore, the independent effects of daily mean temperature and air pollutants on AECOPD were estimated using a distributed lag nonlinear model (DLNM). In order to visualize the combined effect of daily mean temperature and air pollutants, a bivariate response surface was utilized. Subsequently, the daily mean temperature and air pollutants were categorized into binary variables based on predetermined pollutant threshold points determined by the cumulative effect curve. The interaction between ambient temperature and air pollution was then estimated using a Poisson regression model. Additionally, subgroup analysis was performed based on gender.
Distributed lag nonlinear model (DLNM)
The DLNM model allows for the consideration of both the nonlinear and lag effects of the exposure variable on the outcome variable by constructing the cross-basis function. This function captures the complex relationship between the exposure variable and the outcome variable, taking into account nonlinearity and potential time lags20. Hence, the assessment of the effects of daily mean temperature and air pollutants on the risk of AECOPD hospitalization can be conducted as follows:
In this assessment, the number of AECOPD hospitalized cases on day t is denoted as \({Y}_{t}\). The intercept is represented by α. The constructed cross-basis function, cb(xt), is applied to capture the relationship between the daily mean temperature or daily pollutant concentration (xt) and the risk of AECOPD hospitalization. Based on previous literature, the maximum lag period considered in this analysis is 14 days. The degrees of freedom (df) in the cross-basis function are determined using the Akaike information criterion (AIC)21. The degree of freedom (df) of the time trend is 7 per year, DOWt is used to control the day of week effect.
Interaction analysis
The Poisson regression model was employed to analyze the interaction between ambient temperature and air pollution on the occurrence of AECOPD22. We categorized the daily mean temperature and air pollutant variables based on the exposure–response curve of the Distributed Lag Non-linear Model (DLNM). The binary classification was determined by selecting the turning point or the value representing the lowest risk effect in the curve. For the daily mean temperature, we defined T = 0 if it was less than or equal to the turning point, and T = 1 if it was greater than the turning point. Similarly, for air pollution, we defined Air Pollution = 0 if the pollutant was less than or equal to the turning point, and Air Pollution = 1 if it exceeded the turning point. The interaction model is then constructed as follows:
From the model, we can obtain the relative risk (RR) values for RR10, RR01, and RR11. These values are used to calculate the interaction relative risk (IRR), as well as the relative excess risk due to interaction (RERI) along with its corresponding 95% confidence interval (CI). These measures are utilized to evaluate the potential interaction effect. The formula for calculating IRR and RERI, along with their 95% CI, is as follows:
A significant interaction is observed when the 95% CI of the IRR does not include 1 or when the 95% CI of the RERI does not include 0. Specifically, if IRR > 1 or RERI > 0, it indicates a synergistic interaction, suggesting that the combined effect of ambient temperature and air pollution is greater than their individual effects alone. On the other hand, if IRR < 1 or RERI < 0, it indicates an antagonistic interaction, implying that the combined effect is lower than what would be expected based on the additive effects of ambient temperature and air pollution individually.
Subgroup analysis
Subgroup analysis was conducted based on gender. Generally, the high-risk group was defined as individuals who are elderly and over 80 years old23. In our study, the individuals with COPD primarily consist of elderly individuals. Therefore, there was no specific analysis conducted to examine age differences. However, it is worth noting that gender is considered a risk factor for COPD and may have an impact on the observed outcomes of this study24, We aim to investigate the influence of gender on environmental factors and their interactions in relation to hospitalizations due to AECOPD.
Sensitive analysis
The exposure response curves of daily mean temperature and air pollutants to AECOPD hospitalization, respectively, were univariate analyses. By controlling for confounding analysis, when analyzing one variable (temperature or air pollution), all the others were taken as confounding control. The difference between before and after was small, as shown in the supplementary material.
Results
Statistical description of meteorological factors, air pollution and AECOPD hospitalization in Ganzhou City
Table 1 presents the data on meteorological factors, air pollutants, and daily hospitalizations due to AECOPD in Ganzhou from 2016 to 2019. Throughout the study period, the average daily temperature in the region was recorded as 20.0 °C. The concentrations of PM2.5, PM10, and NO2 were measured at 39.4 μg/m3, 62.5 μg/m3, and 23.7 μg/m3, respectively. A total of 57,251 AECOPD patients were admitted to hospitals during this time, with 37,087 males and 20,164 females. On average, there were 39 daily hospitalizations and a total of 14,312 hospitalizations per year. The annual hospitalization rate for AECOPD was about 16 per 10,000.
Figure 1 illustrates the temporal variations of daily hospitalizations due to AECOPD and environmental factors from 2016 to 2019. It was evident that there was an observable pattern, with higher AECOPD hospitalizations occurring in December and March each year, while lower numbers were observed between June and September. This distinct seasonal trend indicated that AECOPD hospitalizations were more prevalent during the winter months compared to the summer season.
Correlation analysis
Table 2 presents the Spearman's correlation coefficients between daily mean temperature, air pollution, and the number of hospitalizations due to AECOPD in Ganzhou City from 2016 to 2019. The analysis revealed a significant negative correlation (P < 0.01) between daily mean temperature and various pollutant factors. Specifically, the correlation coefficients between daily mean temperature and PM2.5, PM10, and NO2 were − 0.246, − 0.163, and − 0.465, respectively. Moreover, the number of AECOPD hospitalizations, both for all patients and when stratified by gender, exhibited a negative correlation with daily mean temperature and a positive correlation with NO2 levels.
Distributed lag nonlinear model
Figure 2 illustrates the cumulative exposure–response curve for the risk of daily mean temperature or air pollutants on the overall hospitalized patients with AECOPD using the distributed lag non-linear model (DLNM). The supplemental figures, Supplemental Figs. 2 and 3, present the cumulative exposure–response curve for hospitalized patients with AECOPD based on different genders.
From Fig. 2, the exposure response curve shows that the risk of hospitalization for AECOPD increased significantly as the temperature decreased and the concentration of air pollutants increased. The analysis reveals that the lowest risk point for the nonlinear exposure–response curve of daily mean temperature was observed at 28 °C. Similarly, the turning points for pollutants PM2.5, PM10, and NO2 were determined to be 50 μg/m3, 54 μg/m3, and 33 μg/m3, respectively. In this study, these minimum risk values or turning points were utilized to classify daily mean temperature and pollutants as dichotomous variables.
Interaction analysis
Table 3 presents the interaction between ambient temperature and air pollutants on hospitalizations due to AECOPD. The IRR with corresponding 95% CIs between daily mean temperature and PM2.5, PM10, and NO2 were estimated as 0.684 (95% CI 0.605, 0.774), 0.854 (95% CI 0.810, 0.900), and 0.530 (95% CI 0.334, 0.842), respectively. Furthermore, the RERI values along with their 95% CIs were calculated as − 0.227 (95% CI − 0.293, − 0.161), − 0.119 (95% CI − 0.159, − 0.079), and -0.428 (95% CI − 0.637, − 0.218), indicating an antagonistic interaction between daily mean temperature and air pollutants.
Through stratified analysis based on temperature, it was observed that the RR (95% CI) of high NO2 (> 33 μg/m3) at low Tmean (≤ 28℃) was 1.119 (95% CI: 1.096, 1.142). To visually depict the interaction between ambient temperature and air pollutants on AECOPD hospitalization, bivariate response surface diagrams are provided in Supplemental Figs. 4–6. The sensitivity analysis results of the exposure response curve are shown in Supplementary Fig. 7.
Subgroup analysis
Gender stratification analysis revealed significant antagonistic interactions between daily mean temperature and PM2.5, PM10, and NO2 in both male and female groups. In the male group, the RRs (95% CI) of high NO2 (> 33 μg/m3) and high PM10 (> 54 μg/m3) at low Tmean (≤ 28 ℃) was 1.095 (95% CI 1.067, 1.124) and 1.029 (95% CI 1.007, 1.052), respectively. However, in the female group, the RRs (95% CI) of high NO2 (> 33 μg/m3) and high PM2.5 (> 50 μg/m3) at low Tmean (≤ 28℃) was 1.164 (95% CI 1.124, 1.204) and 1.037 (95% CI 1.004, 1.071), respectively. These findings indicate that there is a significant antagonistic interaction between ambient temperature and air pollution in both gender subgroups, as shown in Table 4.
Discussions
This study investigated the univariate and bivariate effects between ambient temperature and air pollutants among 57,251 AECOPD inpatients in Ganzhou from January 1, 2016 to December 31, 2019. To assess the relationship between ambient temperature, air pollutants, and the number of AECOPD inpatients, we employed a distributed lag nonlinear model. Our findings indicated an antagonistic interaction between ambient temperature and air pollutants among both the total population and gender subgroups. The results indicated a higher risk of hospitalization for AECOPD when low temperature combined with high concentrations of air pollutants, especially NO2, PM2.5, and PM10.
The DLNM model was employed to examine the exposure–response relationship between ambient temperature and AECOPD inpatients. The analysis revealed a significant association between extreme temperature exposure and the risk of AECOPD hospitalization, with low temperatures posing a higher risk for AECOPD inpatients. When individuals with COPD are exposed to colder temperatures, various microorganisms such as bacteria and viruses become crucial factors in inducing respiratory infectious diseases. Moreover, alterations in environmental factors can influence the types, reproduction, and transmission rate of pathogenic microorganisms. Consequently, fluctuations in air temperature and air pollutant concentrations may directly or indirectly heighten the likelihood of exposure to associated risk factors, thereby increasing the susceptibility to respiratory diseases25. In Taiwan, China, the study discovered that for every 1 °C decrease in temperature, there was a 0.8% increase in AECOPD patients. Moreover, when the mean temperature decreased by 5 °C, the long-term impact OR of AECOPD patients was calculated to be 1.106 (with a 95% CI of 1.063 to 1.152)26. In Baltimore, it was observed that there was a higher rate of AECOPD during the winter season, suggesting that the exacerbation of COPD could potentially be attributed to low temperatures27.
Air pollution is recognized as a significant environmental factor that exacerbates COPD. Another study revealed a significant positive correlation between the average exposure to PM2.5 and the mortality rate of respiratory diseases, including COPD and pneumonia. The relative risk (RR) associated with this correlation ranged between 1.10 and 1.2428. For every 10μg/m3 increase in PM2.5, there was an observed 1.61% increase in the number of respiratory hospital admissions (with a 95% CI of 0.87 to 2.3525. Indeed, numerous studies have consistently demonstrated the adverse effects of high pollution levels on COPD. Consistent with individual studies, our study also found that NO2 had the greatest cumulative effect on AECOPD hospitalizations24.
The interaction analysis conducted in this study revealed a significant antagonistic interaction between ambient temperature and air pollutants regarding the risk of AECOPD hospitalization. The results are similar to those of some current studies. For example, another study conducted in Chengdu, China utilized a bivariate response surface model and stratification analysis to investigate the potential interactions between environmental air pollution (including PM2.5, PM10, SO2) and temperature on AECOPD hospitalizations. The findings indicated that the combined effect of low temperature and pollutants had the most substantial impact on the burden of COPD patients. Moreover, subgroup analysis demonstrated that the elderly population and men over 80 years old were more susceptible to being affected by this particular interaction29. The Xi'an study revealed a significant antagonistic effect between temperature and AQI (Air Quality Index) on respiratory mortality. The interaction analysis showed an IRR of 0.805, with a 95% CI ranging from 0.722 to 0.896, indicating a reduced risk. Additionally, the RERI was calculated as -0.235, with a 95% CI of − 0.269 to − 0.163, further confirming the presence of a significant antagonistic effect30. The utilization of the portable vital capacity measurement method for daily respiratory index measurement revealed that long-term exposure to extreme temperatures was associated with an increased incidence of COPD among patients. Furthermore, when temperature is coupled with air pollutants, the relative risk of COPD patients is higher. Specifically, at the 25th percentile (5μg/m3) of indoor PM2.5 concentration, an increase of 0.4 in the BCSS score (indicating a slight increase in symptoms) was observed for every 10°F rise in indoor temperature. Conversely, at the 75th percentile (16 μg/m3) of PM2.5, the BCSS score showed a more substantial increase of 1 (indicating a serious escalation in symptoms)31.
The biological mechanisms that exist for these interactions are discussed below. When COPD patients are exposed to low temperature, it may lead to a variety of unique airway reactions, including nasal stenosis and congestion, airway epithelial injury leading to changes in airway structure and function, and stimulation of airway secretion of mucin to aggravate respiratory symptoms, resulting in exacerbation of COPD5. On the other hand, bacteria, viruses and other microorganisms are important factors that induce respiratory infectious diseases, and changes in environmental factors may affect the types, reproduction and transmission rate of pathogenic microorganisms. Therefore, changes in air temperature and air pollutant concentration may directly or indirectly increase the risk of exposure to related risk factors, resulting in the risk of respiratory diseases25.
In addition, This study found that at low temperatures, high PM10 was associated with a higher risk of AECOPD in men and high PM2.5 in women. The results were similar to those found in the current study. A multi-city study in Korea found that when patients were exposed to air pollution, PM10 would increase the number of hospitalizations for male AECOPD32, while men had more frequent outdoor activities than women and had more opportunities to be exposed to various environments. Therefore, compared with women, male population had a significant effect33. Studies had shown that PM2.5 not only affected the respiratory system and cardiovascular system, but also may cause allergies, immune and oxidative stress reactions. These mechanisms may be more pronounced in women because women have biological characteristics that may make them more susceptible to these mechanisms34.
The potentially significant impact of the interaction between ambient temperature and air pollution exposure on population health should not be underestimated. Generally, air pollution and air temperature interact synergistically and have combined effects on human health. On one hand, air temperature plays a role in influencing the concentration and distribution of atmospheric pollutants. For instance, prolonged periods of high temperatures can facilitate photochemical reactions in the atmosphere, leading to an increased production of pollutants such as O3 and PM2.535. Additionally, sustained low temperatures can also contribute to the generation of more toxic by-products, such as nitrogen dioxide (NO2), which is emitted through the combustion of petroleum products. These lower temperatures can enhance the stability and persistence of NO2 in the atmosphere, further exacerbating air pollution levels. Hence, both high and low temperatures play a role in influencing the production and distribution of various atmospheric pollutants, ultimately impacting human health36. Furthermore, the concentration levels of atmospheric pollutants also impact changes in temperature. For instance, particulate matter can influence atmospheric temperature through the scattering and absorption of light. Additionally, there exists a shared biological mechanism through which temperature and atmospheric pollutants affect human health. Extreme temperatures can intensify inflammatory responses, induce damage to vascular endothelial cells, and trigger a cascade of adverse effects on human health. These combined factors underscore the complex relationship between air temperature, air pollution, and their impacts on both atmospheric conditions and human well-being37,38.
Our research is subject to certain limitations. Firstly, it should be noted that our study design is ecological in nature, relying on environmental variables obtained from monitoring stations. Therefore, the actual exposure levels experienced by individual patients may not be accurately reflected, introducing potential ecological research bias. Secondly, subgroup analysis was only conducted based on gender due to the predominant concentration of AECOPD inpatients among the elderly. Lastly, our findings are derived from a single city, although they are likely applicable to other regions. The study's extended duration, sufficient sample size, and accurate effect estimation provide valuable guidance for other areas of research.
Conclusion
In summary, our findings indicate that in Ganzhou City of China, environmental temperature and air pollutants such as PM2.5, PM10, and NO2 exhibit primarily antagonistic interactions with the risk of AECOPD hospitalizations. Low temperatures with high NO2 for general population, low temperatures with high PM10 in men and high PM2.5 in women were associated with a higher risk of AECOPD hospitalization. The results indicate a higher risk of hospitalization for AECOPD when there is with high concentrations of air pollution at low temperatures. These results underscore the importance for relevant departments to implement targeted prevention and control measures based on meteorological and air pollution conditions. By doing so, we can effectively reduce the hospitalization rate among COPD patients and alleviate the burden of this disease.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Global, regional, and national under-5 mortality, adult mortality, age-specific mortality, and life expectancy, 1970–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet (London, England) 390, 1084–1150 (2017). https://doi.org/10.1016/s0140-6736(17)31833-0
Zwaans, W. A., Mallia, P., van Winden, M. E. & Rohde, G. G. The relevance of respiratory viral infections in the exacerbations of chronic obstructive pulmonary disease—A systematic review. J. Clin. Virol. 61, 181–188. https://doi.org/10.1016/j.jcv.2014.06.025 (2014).
Roberts, C. M. et al. Clinical audit indicators of outcome following admission to hospital with acute exacerbation of chronic obstructive pulmonary disease. Thorax 57, 137–141. https://doi.org/10.1136/thorax.57.2.137 (2002).
Lainscak, M. et al. Body mass index and prognosis in patients hospitalized with acute exacerbation of chronic obstructive pulmonary disease. J. Cachexia Sarcopenia Muscle 2, 81–86. https://doi.org/10.1007/s13539-011-0023-9 (2011).
Chen, C. et al. Risk of temperature, humidity and concentrations of air pollutants on the hospitalization of AECOPD. PLoS One 14, e0225307. https://doi.org/10.1371/journal.pone.0225307 (2019).
Zhao, Q. et al. Ambient heat and hospitalisation for COPD in Brazil: A nationwide case-crossover study. Thorax 74, 1031–1036. https://doi.org/10.1136/thoraxjnl-2019-213486 (2019).
Gao, N. et al. Short-term effects of ambient air pollution on chronic obstructive pulmonary disease admissions in Beijing, China (2013–2017). Int. J. Chron. Obstruct. Pulmon. Dis. 14, 297–309. https://doi.org/10.2147/copd.S188900 (2019).
Zhou, X. et al. Ambient air pollutants relate to hospital admissions for chronic obstructive pulmonary disease in Ganzhou China. Revista saude publica 56, 46. https://doi.org/10.11606/s1518-8787.2022056004324 (2022).
Choi, J. et al. Harmful impact of air pollution on severe acute exacerbation of chronic obstructive pulmonary disease: Particulate matter is hazardous. Int. J. Chron. Obstruct. Pulmon. Dis. 13, 1053–1059. https://doi.org/10.2147/copd.S156617 (2018).
Lee, J. et al. Factors associated with chronic obstructive pulmonary disease exacerbation, based on big data analysis. Sci. Rep. 9, 6679. https://doi.org/10.1038/s41598-019-43167-w (2019).
Pothirat, C., Tosukhowong, A., Chaiwong, W., Liwsrisakun, C. & Inchai, J. Effects of seasonal smog on asthma and COPD exacerbations requiring emergency visits in Chiang Mai, Thailand. Asian Pac. J. Allergy Immunol. 34, 284–289. https://doi.org/10.12932/ap0668 (2016).
Hwang, S. L. et al. Fine particulate matter on hospital admissions for acute exacerbation of chronic obstructive pulmonary disease in southwestern Taiwan during 2006–2012. Int. J. Environ. Health Res. 27, 95–105. https://doi.org/10.1080/09603123.2017.1278748 (2017).
Jin, X. et al. The modification of air particulate matter on the relationship between temperature and childhood asthma hospitalization: An exploration based on different interaction strategies. Environ. Res. 214, 113848. https://doi.org/10.1016/j.envres.2022.113848 (2022).
Fu, S. et al. Interactive effects of high temperature and ozone on COPD deaths in Shanghai. Atmos. Environ. https://doi.org/10.1016/j.atmosenv.2022.119092 (2022).
Katsouyanni, K. et al. Evidence for interaction between air pollution and high temperature in the causation of excess mortality. Arch. Environ. Health 48, 235–242. https://doi.org/10.1080/00039896.1993.9940365 (1993).
Song, B. et al. Effect of high-level fine particulate matter and its interaction with meteorological factors on AECOPD in Shijiazhuang China. Sci. Rep. 12, 8711. https://doi.org/10.1038/s41598-022-12791-4 (2022).
Qian, Z. et al. High temperatures enhanced acute mortality effects of ambient particle pollution in the “oven” city of Wuhan China. Environ. Health Perspect. 116, 1172–1178. https://doi.org/10.1289/ehp.10847 (2008).
Liu, T., Huang, H. & Hu, G. A Time Series Study for Effects of PM(10) on Coronary Heart Disease in Ganzhou China. Int. J. Environ. Res. Public Health https://doi.org/10.3390/ijerph20010086 (2022).
Li, Z., Shi, C., Wang, X., Wang, R. & Hao, Y. Association between daily temperature and hospital admissions for urolithiasis in Ganzhou, China: A time-series analysis. Int. J. Biometeorol. 67, 47–54. https://doi.org/10.1007/s00484-022-02383-2 (2023).
Gasparrini, A., Armstrong, B. & Kenward, M. G. Distributed lag non-linear models. Stat. Med. 29, 2224–2234. https://doi.org/10.1002/sim.3940 (2010).
Zhang, T. P. et al. Exposure to ambient gaseous pollutant and daily hospitalizations for Sjögren’s syndrome in Hefei: A time-series study. Front. Immunol. 13, 1028893. https://doi.org/10.3389/fimmu.2022.1028893 (2022).
Du, Z. et al. Interactions between climate factors and air pollution on daily HFMD cases: A time series study in Guangdong, China. Sci. Total Environ. 656, 1358–1364. https://doi.org/10.1016/j.scitotenv.2018.11.391 (2019).
Zanobetti, A., O’Neill, M. S., Gronlund, C. J. & Schwartz, J. D. Summer temperature variability and long-term survival among elderly people with chronic disease. Proc. Natl. Acad. Sci. U.S.A. 109, 6608–6613. https://doi.org/10.1073/pnas.1113070109 (2012).
Qu, F. et al. The hospitalization attributable burden of acute exacerbations of chronic obstructive pulmonary disease due to ambient air pollution in Shijiazhuang, China. Environ. Sci. Pollut. Res. Int. 26, 30866–30875. https://doi.org/10.1007/s11356-019-06244-1 (2019).
Albahar, S. et al. Air pollution and respiratory hospital admissions in Kuwait: The epidemiological applicability of predicted PM(2.5) in arid regions. Int. J. Environ. Res. Public Health https://doi.org/10.3390/ijerph19105998 (2022).
Tseng, C. M. et al. The effect of cold temperature on increased exacerbation of chronic obstructive pulmonary disease: A nationwide study. PloS one 8, e57066. https://doi.org/10.1371/journal.pone.0057066 (2013).
McCormack, M. C. et al. Colder temperature is associated with increased COPD morbidity. Eur. Respire. J. https://doi.org/10.1183/13993003.01501-2016 (2017).
Pun, V. C., Kazemiparkouhi, F., Manjourides, J. & Suh, H. H. Long-term PM25 exposure and respiratory, cancer, and cardiovascular mortality in older US adults. Am. J. Epidemiol. 186, 961–969. https://doi.org/10.1093/aje/kwx166 (2017).
Qiu, H. et al. The Burden of COPD Morbidity Attributable to the Interaction between Ambient Air Pollution and Temperature in Chengdu China. Int. J. Environ. Res. Public Health https://doi.org/10.3390/ijerph15030492 (2018).
Mokoena, K. K., Ethan, C. J., Yu, Y. & Quachie, A. T. Interaction effects of air pollution and climatic factors on circulatory and respiratory mortality in Xi’an, China between 2014 and 2016. Int. J. Environ. Res. Public Health https://doi.org/10.3390/ijerph17239027 (2020).
McCormack, M. C. et al. Respiratory effects of indoor heat and the interaction with air pollution in chronic obstructive pulmonary disease. Ann. Am. Thorac. Soc. 13, 2125–2131. https://doi.org/10.1513/AnnalsATS.201605-329OC (2016).
Jung, Y. J. et al. Short-term air pollution exposure and risk of acute exacerbation of chronic obstructive pulmonary disease in Korea: A national time-stratified case-crossover study. Int. J. Environ. Res. Public Health https://doi.org/10.3390/ijerph19052823 (2022).
Li, S. & Dong, J. Impact of ambient temperature on hospital admissions for respiratory diseases in suburban rural villages in northwest China. Environ. Sci. Pollut. Res. Int. 29, 66373–66382. https://doi.org/10.1007/s11356-022-20446-0 (2022).
Zhang, J. et al. Sex Differences in cardiovascular risk associated with long-term PM2.5 exposure: A systematic review and meta-analysis of cohort studies. Front. Public Health https://doi.org/10.3389/fpubh.2022.802167 (2022).
Kinney, P. L. Climate change, air quality, and human health. Am. J. Prev. Med. 35, 459–467. https://doi.org/10.1016/j.amepre.2008.08.025 (2008).
Duan, Y. et al. Effect of changes in season and temperature on cardiovascular mortality associated with nitrogen dioxide air pollution in Shenzhen, China. Sci. Total Environ. 697, 134051. https://doi.org/10.1016/j.scitotenv.2019.134051 (2019).
Keatinge, W. R. et al. Increased platelet and red cell counts, blood viscosity, and plasma cholesterol levels during heat stress, and mortality from coronary and cerebral thrombosis. Am. J. Med. 81, 795–800. https://doi.org/10.1016/0002-9343(86)90348-7 (1986).
Gasparrini, A. et al. Mortality risk attributable to high and low ambient temperature: A multicountry observational study. Lancet (London, England) 386, 369–375. https://doi.org/10.1016/s0140-6736(14)62114-0 (2015).
Funding
This work was supported by the National Natural Science Foundation of China (42165012) and Ph.D. Start-up Fund of Gannan Medical University (QD202013).
Author information
Authors and Affiliations
Contributions
Material preparation, analysis, and original draft written by Chenyang Shi. Data collection, guidance, and constructive suggestions provided by Jinyun Zhu and Guoliang Liu. Statistical guidance obtained from Zhicheng Du. Conception, writing, reviewing, editing manuscripts, and financial responsibility handled by Yanbin Hao. All authors have read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Shi, C., Zhu, J., Liu, G. et al. Time series analysis of the interaction between ambient temperature and air pollution on hospitalizations for AECOPD in Ganzhou, China. Sci Rep 14, 17106 (2024). https://doi.org/10.1038/s41598-024-67617-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-67617-2
- Springer Nature Limited