Abstract
Globally one-third of global population are victims of anemia, significantly impacting maternal and infant health and linked to poor cognition, productivity, and mortality risks. We used randomly selected 4040 lactating mothers’ record from nationally representative survey. Descriptive statistics were weighted, and the standard hemoglobin cutoff point (below 12 g/dl) was used. Bivariable and multivariable multilevel binary logistic regression model considering the individual and community-level factors associated with anemia was employed. Crude and adjusted odds ratios with a 95% confidence interval were reported. In Ethiopia, 32.3% (95% CI 30.9–33.7%) of lactating women were anemic, with 23.4% having mild, 7.3% moderate, and 1.2% severe anemia. Pastoral regions (Afar, Somalia, and Oromia region) had higher burden of anemia than the others. The advanced age of the mother above 45 years (AOR = 1.43 (1.11–1.82), unemployment (AOR = 1.19; 95% CI 1.08–1.32), household wealth index (AOR = 0.56; 95% CI 0.50–0.63), extended family size (AOR = 1.20; 95% CI 1.04–1.46), and not using family planning (AOR = 1.70; 95% CI 1.49–1.93) were significant factors associated with anemia. Anemia is a moderate public health problem and associated with location and other factors to be addressed via effective interventions.
Similar content being viewed by others
Introduction
Lactation is one of the most nutrient demanding stages of human development and it is a critical stage, where blood loss and increased nutrient demand predispose them to maternal depletion and increased risk of anemia. Anemia is a reduced hemoglobin level in the blood below the World Health Organization (WHO) cutoff of 12 g/dl for non-pregnant women in reproductive age groups, including lactating women1. Anemia is affects one-third of the global population2,3,4 where the causes are multiple and nutritional causes play a great role. Among these, iron deficiency is the single most important contributor to anemia, contributing to more than 40%5.
Furthermore, anemia is a moderate to severe public health problem in more than 142 countries. An estimated 529 million (29.4%) of women of reproductive age are victims of anemia due to blood loss during menstruation, pregnancy, childbirth and other factors6. Globally, about 40% of children under five years of age, 37% among pregnant women, and 30% of women of reproductive age are affected by anemia7. In Ethiopia, iron deficiency affects about 8% of the population with wide variations among regions (6–48%). Moreover, 13% of women of reproductive age had anemia where the regional variations range from 6 to 40%, making mild to moderate public health problem8.
Anemia is strongly linked to negative growth consequences such as stunting, reduced cognition, morbidity, mortality, and significant economic loss9. Anemia is a huge concern globally, contributing to more than 1 million annual deaths, mainly from Africa and Southeast Asia (70%)3,7,10. Aside from the obvious link to pregnancy complications, it has also been linked to depression, stress, and cognitive functioning in lactating women3.
On the other side, lactation is a period where women are highly susceptible to iron depletion in the presence of an inadequate dietary supply11,12. The maternal iron store is greatly depleted by repeated reproductive burden, blood loss during pregnancy, and childbirth11,13. In addition, the subsequent iron loss through breast milk at the expense of maternal iron store further aggravates the problem9. These problems are more prevalent in Africa, where the fertility rate is higher and dietary intake is poor2,3,14. These is strongly associated with the prevailing occurrence of anemia among this segment of the population that is being further aggravated by multiple dynamic changes happening across the globe.
Ethiopia faces multiple environmental, economic, health and dietary changes influenced by multiple dimensions that could affect nutritional status, anemia specifically15,16. Maternal and child nutrition vulnerability related to anemia arises from widespread iron deficiency anemia, inadequate dietary diversity, and limited healthcare access9. Traditional diets centered around staples and monotonous diets could limit iron intake and bioavailability. Household food security vulnerability is evident during seasonal shortages, affecting many families3. With all these vulnerabilities could further aggravate the existing burden of anemia in Ethiopia17,18.
Much of previous efforts were among pregnant women with a prevalence estimate of above 50%13,16,18,19,20 and yet limited evidence exist among lactating women in Ethiopia. The previous consecutive national reports indicated that 29.9% (2005) and 18.5% (2011) of lactating women had anemia in Ethiopia21. However, lactation is immediate postpartum period where the problem of pregnancy usually continues and is associated with poor maternal and child health2,9. Anemia during this period is of great concern from maternal and newborn perspectives16,22,23. It is linked to poor infant growth24, depression, and adverse maternal and child outcomes25. Comprehensive evidence on anemia could contribute to the sustainable development goals by reducing morbidity and mortality. of women during the lactation period associated with anemia17.
For a better understanding of the contributing factors to anemia among lactating women, a robust analysis of existing large nationally representative datasets is very informative and conclusive as compared to local pocket studies. The DHS gives free access to the country specific survey datasets, enables them to characterize and assess the potential interregional variations and important modifiable risk factors for the prevention of anemia. This paper was to determine the burden, regional distribution, and risk factors of anemia among lactating women in Ethiopia.
Methods
Data sources
The current paper is based on secondary analysis of the 2016 EDHS survey, spanning all regional states and the two federal administrative cities of Ethiopia. Ethiopia is a country that is located in the eastern parts of Africa, within Sub-Saharan Africa. An estimated total population of more than 110 million people resides in the country. The survey was conducted in 2016 from January to June. The data were collected from a nationally representative sample of households in a way that allows national and regional levels estimates of indicators. The results of this analysis targeted all lactating mothers (currently breast-feeding mothers during the data collection period) based on a representative sample of lactating mothers from a randomly selected household. The data nature and coding were reviewed thoroughly to extract important variables and observations. Considering the breast-feeding status during the interview (V404) and the pregnancy status, we extracted 4252 data of lactating women interviewed for the survey. The missing values for the outcome variable was checked, and all cases of the lactating women were included in the analysis (n = 4040) Data was captured from a representative enumeration area and 11 administrative regions of the country.
Variables of the study
The anemia status of the lactating mother was a dependent variable while many socio-demographic, obstetric, diet-related, and other related variables were considered as potential independent variables in the study. Some of the variables included were region, residence, age of the mother, household wealth index, maternal occupation, mother’s educational status, husband’s education, family planning use, marital status, nutritional status of the mother, substance use (alcohol, cigarette and khat chewing).
It is known that different cut-off points are used to diagnose anemia based on the WHO standard anemia (based on hemoglobin measurement) classification adjusted for different life stages (pregnancy, childhood, women of reproductive age and adult males), smoking status, and altitude. Hence, for lactating women who are within women of reproductive age group, hgb concentration value below 12.0 g/dl were classified as anemic. Moreover those with 10–11.9 g/dl as mild, 7–9.9 g/dl as moderately anemic and below 7 g/dl as severely anemic1 (Table 1).
Sampling procedures
A two-stage stratified sampling was employed to include households from a total of 84,915 enumeration areas (EAs) prepared from the 2007 census. An EA is a geographic area covering an average of 181 households per day. Samples were taken from the nine regions and administrative regions of the country. Each primary sampling unit was stratified into urban and rural areas. Then, samples of EAs were selected from the stratum in two stages. Proportional to size sample allocation techniques were maintained at region, zone, and district, where the respective number of enumeration areas were sampled accordingly.
Data collection methods
Data was collected through face-to-face interview and measurements via paper-based and/or tablets. Pretested tool with a translation into local languages was used. Women’s questionnaire that measures socio-demographic characteristics of the mothers, reproductive health, and service use behaviors were included. In addition, biomarkers: anthropometry (body mass index), and anemia testing (hemoglobin) were included. Hemoglobin measurement was done using battery-operated portable HemoCue analyzer for all anemia samples. A 5 ml blood sample was taken after obtaining a written consent from the study subjects26.
A total of 132 individuals were selected as interviewers, 66 as biomarker technicians, 33 as field editors, and 33 as team supervisors, with a four-day field practice being organized. Instruction on how to administer the paper and electronic questionnaires, mock interviews between participants in the classroom, and practice interviews with real respondents in areas outside the survey sample were conducted. In addition, laboratory professionals collected the biomarker data under standard procedures26.
Data analysis
The data was acquired in SPSS format and the analysis was done in SPSS version 20. The data was presented in frequency, percentage, tables, and graphs. The body mass index (kg m−2) was calculated and classified as underweight (less than 18.5 kg m−2), normal (18.5–24.9 kg m−2), and overweight (above 25 kg m−2). The household asset variables were analyzed using a principal component analysis after checking that all assumptions were carried out. Then, the factor score is used to categorize individuals into wealth quintiles (poorest, poorer, middle, rich, and richest). For the present analysis, the wealth index was presented into three groups (poor, middle, and rich) better presentation.
A bivariable and multivariable multilevel binary logistic regression analysis was carried out to identify determinants of anemia. Variables found statistically significant at p-value below 0.25 during bivariable analysis were analyzed in the multivariable logistic regression model. Crude and an adjusted odds ratio with a 95% confidence level was calculated. Statistical significance was declared at a p-value below 0.05. Multicollinearity and effect modifications were evaluated accordingly using variance inflation factor (above 10) and interaction effects.
Ethical approval and consent to participate
The dataset was obtained from the DHS site with a full legal request. The dataset will not be shared with the third party. These are anonymous surveys, which do not allow any potential identification of any single household or individual in the data file. The survey protocol, including biomarker sample collection, was reviewed and approved by the Federal Democratic Republic of Ethiopia's Ministry of Science and Technology and the Institutional Review Board of ICF International. Written informed consent was obtained from all subjects and/or their legal guardian for those aged less than 18 years. The accessed data were used for the purpose of registered research paper. Confidentiality of the data was kept and no effort made to identify any household or individual respondent interviewed in the survey. The data were not passed on to other researchers without the written consent of DHS. The data were fully accessed at www.dhsprogram.com. All methods were carried out in accordance with Declaration of Helsinki.
Results
Socio-demographic and economic characteristics
Out of the total 4252 records, 4040 (95% retrieval rate) records of lactating women were included in the analysis after excluding 67 (1.6%) records due to anemia status not available although sample were collected and 145 (3.4%) were excluded due to maternal refusal or to give blood sample at the start. A total of 800 (18.8%) were from urban areas, and the majority (47.1%) were aged 26–35 years of age. Around 2431 (63.1%) had no education at all (illiterate), and 1683 (43.6%) were Muslims. Almost one-third, or 1439 (33.8%) of lactating women were living in the poorest wealth quintile, while only 559 (13.1%) were from the richest quintile. The majority, 3994 (94%) and 2331 (57.7%), were married and unemployed, respectively. About 648 (15.2%), (13.4%), and (12.3%) were from the Oromia, southern, and Amhara regions of Ethiopia (Fig. 1).
Burden and distribution of anemia
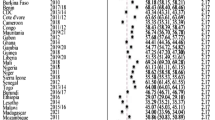
In Ethiopia, 1306 (32.3%; 95% CI 30.9–337%) of lactating women were anemic; 23.4%, 7.3%, and 1.2% had mild, moderate, and severe anemia, respectively. A wide interregional variation in the prevalence of anemia was observed among regions where pastoral regions (Afar, Somalia, and Parts of Oromia regions) had the highest prevalence of anemia (Fig. 2).
Anemia among lactating women was more prevalent among women residing in rural area and in the age group of 26–35 years as compared to counterparts. Women in the lowest socioeconomic class were the most prone to anemia. In addition, the burden of anemia was higher among married and uneducated women (Table 2).
Anemia was highly prevalent in Somalia's regional states (67.2%), followed by Afar (48.6%) and Dire Dawa (43.2%). Specifically severe anemia was higher in Somalia (6.5%) and Afar (2.5%). However, mild anemia was more prevalent across all regional and city administrations. Furthermore, in certain regions like Addis Ababa and Gambelia, no cases of severe anemia were identified (Table 3).
Factors associated with anemia among lactating mothers
In bivariable analysis, the age of the mother, residence, maternal education, household wealth index, household family size, marital status, and alcohol use was associated with anemia in the crude model. Women aged 26 to 35 years (COR = 1.25; 95% CI 1.03–1.52), living in rural areas (COR = 1.80; 95% CI 1.65–1.95), and being married (COR = 1.25; 95% CI 1.2–13) had a 25%, 80%, and 25% higher risk of anemia as compared to counterparts, respectively. Women in a higher the higher wealth quintile (COR = 0.42; 95% CI 0.38–0.48) and had lower risks of anemia compared to lower wealth quintile in the crude model. Women in the higher family size had a 40% increased risk of being anemic (COR = 1.40; 95% CI 1.25–1.60). Concerning substance use, alcohol consumption is associated with reduced risk of anemia (COR = 0.51; 95% CI 0.46–0.55) while association with khat chewing and cigarette smoking did not show statistical significance. In addition, the risk of anemia was found to be higher among undernourished women (COR = 1.29; 95% CI 1.16–1.34) and lower among obese women (COR = 0.66; 95% CI 0.52–0.84) compared to well-nourished mothers in the unadjusted model. Those lactating mothers who never used any family planning methods (COR = 2.36; 95% CI 2.06–2.70) and unemployed mothers (AOR = 1.54; 95% CI 1.34–1.76) had 2.36 and 1.54 times higher odds of anemia compared to counterparts (Table 4).
After adjusting for potential confounders, a stepwise multivariable logistic regression model was fitted (Hosmer–Lemeshow’s p-value = 0.89). The age of the mother, household wealth index, educational status of the women, occupation of the women, household family size, and family planning use were significantly associated with anemia. Women with higher wealth quintile (AOR = 0.56; 95% CI 0.50–0.63) had a lower odd of anemia than women with lower socioeconomic status. Better husband education showed to proportionally decrease the odds of anemia among lactating women as compared to those without formal education (P-value < 0.0001) where those who attended primary (AOR = 0.79; 95% CI 0.70–0.90), secondary (AOR = 0.82; 95% CI 0.72–1.10) and higher education secondary (AOR = 0.75; 95% CI 0.56–1.03) had 21%, 18% and 25% reduced odds of anemia, respectively. Unemployed mothers (AOR = 1.19; 95% CI 1.08–1.32) and women with extended family size (household size) above seven (AOR = 1.20; 95% CI 1.04–1.46) had about 20% higher risks of anemia compared to employed and mothers with smaller household size. Those who did not use family planning (AOR = 1.7; 95% CI 1.49–1.93) was associated with increased risks of anemia among lactating mother (Table 5).
Discussions
The findings of this study showed that 32.3% of lactating women had anemia indicating anemia a moderate public health problem in Ethiopia. Also, the advanced age of the mother above 45 years unemployment, household wealth index, extended family, and not using family planning were significant factors associated with anemia.
The current estimate is slightly higher than the 2005 (29.9%) and 2011 national DHS (18.5%)21. However, a relatively consistent result was found as compared to the study done in Madrid (29%)27. In contrast, studies conducted in India (60–82%)24, Myanmar (60.3%)28, and Vietnam (39.0%)29, showed a higher burden of anemia among lactating women. Sub-national evidence has also showed that anemia affects 43%13 and 28.7% of lactating women in the Northwest and South West Ethiopia, which is above the estimate in Amhara (12.3%) and the Oromia region (15.3%)30. Furthermore, a great inter-regional variation in anemia prevalence was observed12, where anemia is more prevalent in the pastoral and agropastoral regions, which could be linked to many dietary and non-dietary factors. For instance, this might be related to a higher reliance on cow or camel milk, which is a rich source of calcium, affecting iron absorption negatively. In addition, we noted a persistently increasing burden of anemia from 2005 to 2016 in Ethiopia21, which indicates that the existing interventions might not be effective and due attention is not given for lactating women. On the contrary, more recent estimates depicted that 13% of women in reproductive age had anemia with a consistently higher occurrence among women from Somalia (40%) and Dire Dawa30.
This may be associated with differences in socio-economic status and dietary behaviors2,11,13,22. In addition, the current study is based on a country wide large-scale survey, which is inclusive of women from multiple socioeconomic and dietary habits contexts12,29. It is partly explained by the increased blood loss during delivery, coupled with poor dietary habits and prevailing maternal malnutrition further predisposing women to higher risks of anemia9,20,22,23. Hence, anemia during pregnancy which persists while lactation could potentially increase the risks maternal morbidity, mortality, maternal cognition, and poor childhood development, which warrants context-specific interventions addressing anemia like tailored iron and folic acid supplementation schedules Overall, this study indicated that anemia among lactating women is an important public health problem, that needs to be addressed through targeted interventions7,15. Larger family size and not using family planning was found to be associated with higher odds of anemia among lactating women. This is consistent with evidence from India that showed family planning use was preventive for anemia (AOR = 0.68; 95% CI 0.57–0.80)31. Pooled analysis of the 2005 and 2011 EDHS21 also showed that family size and non-use of family planning were significantly associated with increased occurrence of anemia. Other studies conducted in Ethiopia has also showed a similar association13,16,19,32,33. These are mainly explained with the critical link between family size and the issue of maternal depletion syndrome associated with short interpregnancy intervals. Moreover, it could be linked with food insecurity and nutrient loss due to subsequent pregnancy increasing the burden of the mother. Efforts to maintain an optimal birth interval could reduce the risk of maternal depletion and may allow better food and nutrition security for better nutritional status of mothers34. This might be partly explained by the inverse relationship between maternal age and hemoglobin (AOR = 0.8; p = 0.004), which is supported by study done in Southwest Ethiopia (β = − 0.03; 95% CI; 0.04 0.03)13.
In contrast, increased maternal age is associated with repeated pregnancy, expanded family size, and increased maternal depletion. However, it could be linked to being primigravida, which is associated with increased blood loss due to pregnancy complications in the earlier periods2,23. While evidence from Southwest Ethiopia indicated that maternal age had no any significant association with anemia35. While our study indicated that advanced maternal age was associated with a higher burden of anemia. On the other hand, better maternal education reduces the risk of anemia by 75% (AOR = 0.75; 95% CI 0.56–1.03) as compared to illiterates. Those primigravida within the teenager group might have an increased double burden of pregnancy and adolescents. Meeting the iron and vitamin requirements of women during adolescence could contribute to a reduced burden of anemia11. Studies have also showed that adolescents were more at risk for anemia (22%)36,37, which could be associated with the double nutrient burden. This will allow decision maker to target anemia prevention and control strategies focusing on high-risk groups, with enhanced family planning utilization for achieving optimal fertility level and improve nutritional status5,14.
This study showed that women from better economic classes reduced the risk of anemia by half. A study from Myanmar and previous national estimates indicated that better income is associated with a lower risk of anemia which could allow for better food security, educational status, and knowledge of healthy behaviors3,20,31. It may also be linked to having better ANC and post-natal visits and adherence to iron and folic acid supplementation36,37. In this research majority of lactating women’s having anemia had not history of ANC follow up accounts 509 (49%). This emphasizes the need for enhance nutritional counseling and full package delivery during ANC visit could improve the nutrition intake and health behaviors in post-natal period14,38,39,40.
This evidence clearly shows that anemia is a public health problem among lactating women. Little interventions for addressing anemia among lactating women are there in Ethiopia where routine iron and folic acid supplementations are not in place. Hence, little attention is being given to it despite its adverse consequences, which are mainly related to problems with iron intake30,41,42. Intermittent iron supplementation could be an alternative short-term strategy in areas of high anemia burden to supplement existing interventions.
However, the findings of this analysis could be frustrated by many factors. For instance, the old nature of the data could not allow to depict the existing burden of anemia rather it would allow for comparative trends. Hence, the current country insecurity, food security issues and food inflation might have worsened the issue further.
Conclusions
Anemia among lactating women is a moderate public health problem that needs a targeted and effective intervention to address it. Higher age, larger family size, maternal illiteracy, poor socioeconomic class, and not having family planning use history were found to be associated with anemia. There may be a need for country-specific and cost-effective interventions via enhanced family planning, improving food and nutrition security, and intermittent iron supplementation could be a potential strategy to address the current burden of anemia. Thus, interventional studies and pilots could help to further understand the potential feasibility, compliance and effectiveness of such interventions in addressing anemia among lactating women.
Data availability
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
Abbreviations
- ANC:
-
Antenatal care
- AOR:
-
Adjusted odds ratio
- CI:
-
Confidence interval
- COR:
-
Crude odds ratio
- DHS:
-
Demographic and Health Survey
- EA:
-
Enumeration areas
- EDHS:
-
Ethiopia Demographic and Health Survey
- PSU:
-
Primary sampling unit
- WHO:
-
World Health Organization
References
WHO, C. M. Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity. Geneva, Switz World Heal Organ 1–6 (2011).
Bhadra, P. & Deb, A. A review on nutritional anemia. Indian J. Nat. Sci. 10, 18466–18474 (2020).
Chaparro, C. M. & Suchdev, P. S. Anemia epidemiology, pathophysiology, and etiology in low-and middle-income countries. Ann. N. Y. Acad. Sci. 1450, 15–31 (2019).
Organization, W. H. The World Health Report 2002: Reducing Risks, Promoting Healthy Life. (World Health Organization, 2002).
Patterson, A. J., Brown, W. J. & Roberts, D. C. K. Dietary and supplement treatment of iron deficiency results in improvements in general health and fatigue in Australian women of childbearing age. J. Am. Coll. Nutr. 20, 337–342 (2001).
Kinyoki, D., Osgood-Zimmerman, A. E., Bhattacharjee, N. V., Kassebaum, N. J. & Hay, S. I. Anemia prevalence in women of reproductive age in low-and middle-income countries between 2000 and 2018. Nat. Med. 27, 1761–1782 (2021).
World Health Organization (WHO). Anemia. Preprint at (2023).
Woldeyohannes, M. et al. Ethiopia national food and nutrition survey to inform the Ethiopian national food and nutrition strategy: A study protocol. BMJ Open 13, e067641 (2023).
Butwick, A. J. & McDonnell, N. Antepartum and postpartum anemia: A narrative review. Int. J. Obstetr. Anesthesia 47, 102985 (2021).
Garcia-Casal, M. N., Dary, O., Jefferds, M. E. & Pasricha, S. Diagnosing anemia: Challenges selecting methods, addressing underlying causes, and implementing actions at the public health level. Ann. New York Acad. Sci. 1524, 37–50 (2023).
Kominiarek, M. A. & Rajan, P. Nutrition recommendations in pregnancy and lactation. Med. Clin. 100, 1199–1215 (2016).
Mihiretu, A. Factors associated with anemia among lactating mothers in subsistence farming households from selected districts of Jimma zone, south western Ethiopia: A community based cross-sectional study. J. Nutr. Food Sci. 7, (2017).
Feleke, B. E. & Feleke, T. E. Pregnant mothers are more anemic than lactating mothers, a comparative cross-sectional study, Bahir Dar, Ethiopia. BMC Hematol. 18, 1–7 (2018).
Brown, L. R. Women and food security: Roles, constraints, and missed opportunities. Encyclopedia of Life Support Systems: The Role of Food, Agriculture, Forestry and Fisheries in Human Nutrition 316–334 (2011).
Chilot, D. et al. Anaemia among lactating and non-lactating women in low-income and middle-income countries: A comparative cross-sectional study. BMJ Open 13, e069851 (2023).
Correa-Agudelo, E. et al. The epidemiological landscape of anemia in women of reproductive age in sub-Saharan Africa. Sci. Rep. 11, 11955 (2021).
Amaha, N. D. Ethiopian progress towards achieving the global nutrition targets of 2025: Analysis of sub-national trends and progress inequalities. BMC Res. Notes 13, 1–5 (2020).
Kassa, G. M., Muche, A. A., Berhe, A. K. & Fekadu, G. A. Prevalence and determinants of anemia among pregnant women in Ethiopia; a systematic review and meta-analysis. BMC Hematol. 17, 1–9 (2017).
Worku, M. G. et al. Multilevel analysis of determinants of anemia among young women (15–24) in sub-Sahara Africa. Plos One 17, e0268129 (2022).
Kangalgil, M., Sahinler, A., Kırkbir, I. B. & Ozcelik, A. O. Associations of maternal characteristics and dietary factors with anemia and iron-deficiency in pregnancy. J. Gynecol. Obstetr. Human Reproduction 50, 102137 (2021).
Gebremedhin, S. & Enquselassie, F. Correlates of anemia among women of reproductive age in Ethiopia: Evidence from Ethiopian DHS 2005. Ethiop. J. Health Develop. 25, 22–30 (2011).
Georgieff, M. K. Iron deficiency in pregnancy. Am. J. Obstetr. Gynecol. 223, 516–524 (2020).
Naji, T. S., Ali, S. T., Alwan, I. A. & Abbas, M. N. Effect of iron deficient on the pregnant women. BNIHS 140, 845–853 (2022).
Sharif, N., Das, B. & Alam, A. Prevalence of anemia among reproductive women in different social group in India: Cross-sectional study using nationally representative data. Plos One 18, e0281015 (2023).
Hasan, M. M. et al. Anaemia in women of reproductive age in low-and middle-income countries: Progress towards the 2025 global nutrition target. Bull. World Health Organ. 100, 196 (2022).
Central Statistical Agency of Ethiopia. Ethiopia demographic and health survey, 2016: Key indicators report. Central Statistical Agency (CSA, Ethiopia) and ICF (CSA and ICF, Addis Ababa and Rockville, 2016).
Galambosi, P. J., Gissler, M., Kaaja, R. J. & Ulander, V. Incidence and risk factors of venous thromboembolism during postpartum period: a population-based cohort-study. Acta obstetricia et gynecologica Scandinavica 96, 852–861 (2017).
Zhao, A. et al. Prevalence of anemia and its risk factors among lactating mothers in Myanmar. Am. J. Trop. Med. Hygiene 90, 963 (2014).
Dumrongwongsiri, O. et al. Dietary intake and milk micronutrient levels in lactating women with full and partial breastfeeding. Maternal Child Health J. 25, 991–997 (2021).
Ethiopian Public Health Institute (EPHI). Food and Nutrition Stratefy Baseline Report. (2023).
Siddiqui, M. Z. et al. Prevalence of anemia and its determinants among pregnant, lactating, and nonpregnant nonlactating women in India. Sage Open 7, 2158244017725555 (2017).
Zegeye, B. et al. Prevalence of anemia and its associated factors among married women in 19 sub-Saharan African countries. Arch. Public Health 79, 1–12 (2021).
Ba, D. M. et al. Adherence to iron supplementation in 22 sub-Saharan African countries and associated factors among pregnant women: A large population-based study. Curr. Develop. Nutr. 3, nzz120 (2019).
Bellizzi, S. & Ali, M. M. Effect of oral contraception on anemia in 12 low-and middle-income countries. Contraception 97, 236–242 (2018).
Hankey, G., Collaborators, G. B. D. Health effects of dietary risks in 195 countries, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 393, 1958–1972 (2019).
Shaka, M. F. & Wondimagegne, Y. A. Anemia, a moderate public health concern among adolescents in South Ethiopia. PloS One 13, e0191467 (2018).
Hussein, N. A. & Ouda, M. M. A. Life style risk factors of Iron deficiency Anemia among adolescents’ girls. Int. J. Nursing Didactics 8, 18–28 (2018).
Desta, M. et al. Adherence of iron and folic acid supplementation and determinants among pregnant women in Ethiopia: A systematic review and meta-analysis. Reprod. Health 16, 1–14 (2019).
Ikeanyi, E. M. & Ibrahim, A. I. Does antenatal care attendance prevent anemia in pregnancy at term?. Nigerian J. Clin. Practice 18, 323–327 (2015).
Abdel-Aziz, S. B., Hegazy, I. S., Mohamed, D. A., Kasem, M. M. A. A. E. L. & Hagag, S. S. Effect of dietary counseling on preventing excessive weight gain during pregnancy. Public Health 154, 172–181 (2018).
Hess, S. Y. et al. Accelerating action to reduce anemia: Review of causes and risk factors and related data needs. Ann. New York Acad. Sci. 1523, 11–23 (2023).
Anne Bossuyt, A. B. Moving towards nutrition-sensitive agriculture strategies and programming in Ethiopia. in Agriculture for improved nutrition: Seizing the momentum 165–177 (CAB International Wallingford UK, 2019).
Acknowledgements
We are grateful to the Central Statistical Agency of Ethiopia and MEASURE DHS program for granting us permission to download and use the 2016 & 2019 Ethiopia DHS datasets freely for this study.
Funding
No grant was received for this particular study from any funding agency. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
AO and SG: conceptualization of the study; data acquisition; data preparation; formal analysis; methodology; interpretation of the result; and writing: review and editing of the final manuscript. NA, KA, BAM, ID, SA, MS, and AH: involved in the conceptualization, reviewing the manuscript and made intellectual inputs. AO is extensively involved in writing up the manuscript, statistical analysis, constructing tables and charts, reviewing and editing the final version. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Girma, S., Abdureshid, N., Ayele, K. et al. Burden and determinants of anemia among lactating women in Ethiopia: evidence from demographic health survey. Sci Rep 14, 14816 (2024). https://doi.org/10.1038/s41598-024-65583-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-65583-3
- Springer Nature Limited