Abstract
Background
Anemia during pregnancy is one of the most common indirect obstetric cause of maternal mortality in developing countries. It is responsible for poor maternal and fetal outcomes. A limited number of studies were conducted on anemia during pregnancy in Ethiopia, and they present inconsistent findings. Therefore, this review was undertaken to summarize the findings conducted in several parts of the country and present the national level of anemia among pregnant women in Ethiopia.
Methods
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guideline was followed for this systematic review and meta-analysis. The databases used were; PUBMED, Cochrane Library, Google Scholar, CINAHL, and African Journals Online. Search terms used were; anemia, pregnancy related anemia and Ethiopia. Joanna Briggs Institute Meta-Analysis of Statistics Assessment and Review Instrument (JBI-MAStARI) was used for critical appraisal of studies. The meta-analysis was conducted using STATA 14 software. The pooled Meta logistic regression was computed to present the pooled prevalence and relative risks (RRs) of the determinate factors with 95% confidence interval (CI).
Results
Twenty studies were included in the meta-analysis with a total of 10, 281 pregnant women. The pooled prevalence of anemia among pregnant women in Ethiopia was 31.66% (95% CI (26.20, 37.11)). Based on the pooled prevalence of the subgroup analysis result, the lowest prevalence of anemia among pregnant women was observed in Amhara region, 15.89% (95% CI (8.82, 22.96)) and the highest prevalence was in Somali region, 56.80% (95% CI (52.76, 60.84)). Primigravid (RR: 0.61 (95% CI: 0.53, 0.71)) and urban women (RR: 0.73 (95% CI: 0.60, 0.88)) were less likely to develop anemia. On the other hand, mothers with short pregnancy interval (RR: 2.14 (95% CI: 1.67, 2.74)) and malaria infection during pregnancy (RR: 1.94 (95% CI: 1.33, 2.82)) had higher risk to develop anemia.
Conclusions
Almost one-third of pregnant women in Ethiopia were anemic. Statistically significant association was observed between anemia during pregnancy and residence, gravidity, pregnancy interval, and malaria infection during pregnancy. Regions with higher anemia prevalence among pregnant women should be given due emphasis. The concerned body should intervene on the identified factors to reduce the high prevalence of anemia among pregnant women.
Similar content being viewed by others
Background
World health organization (WHO) defines anemia as a low blood hemoglobin concentration. It is one of the major public health problems globally with diverse consequences [1, 2]. It affects the physical health and cognitive development of individual causing low productivity and poor economic development of a country [1, 3]. The problem is also related to high maternal and infant morbidity and mortality especially in developing countries [4, 5].
WHO report showed that anemia affects more than half a billion reproductive age women globally. From this, 38% of the anemic women were pregnant [5]. Anemia is the most common complication related to pregnancy, which affects almost half of pregnant women globally [6,7,8,9,10]. It usually results due to the normal physiological changes of pregnancy resulting in hemoglobin concentration [6, 11]. The problem is more common in developing countries where there is inadequate diet and poor prenatal vitamins and iron and folic acid intake [1, 6, 12]. The most common type of anemia is iron deficiency anemia which mainly affects women of reproductive age group, particularly pregnant women [4, 13].
Several studies have shown that anemia during pregnancy has several adverse effects. Based on the type and severity of anemia, the pregnancy may have poor maternal and fetal outcomes. The most common obstetric problems of anemia include; abortion, prematurity, intrauterine fetal death, low birth weight and perinatal mortality [4, 6, 14,15,16].
Even though studies have been conducted on the magnitude of anemia among pregnant women in Ethiopia, they present inconsistent and inconclusive findings. So, this systematic review and meta-analysis was conducted to determine the prevalence and determinants of anemia among pregnant women in Ethiopia using the available published evidence. The study will be important to design appropriate interventions to reduce the high burden of the disease.
Methods
Study design and search strategy
A systematic review of published studies was used to determine the prevalence of anemia and its determinant factors among pregnant women in Ethiopia. Review of all published studies was done in the following major databases; PubMed, Cochrane Library, Google Scholar, CINAHL, and African Journals Online. The search for published studies was not restricted by time, and all published articles up to January 01/2017 were included into the review. Search of the reference list of already identified studies to retrieve additional articles was done. The search terms used were; “anemia OR anemia during pregnancy OR determinants of anemia AND Ethiopia”. Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guideline was strictly followed when conducting this review [17].
Study selection and eligibility criteria
This review included studies that were conducted and published on anemia among pregnant women in Ethiopia. All studies conducted at the community or health institution level were included. Studies that provide the prevalence of anemia in pregnant women using the WHO definition (hemoglobin level less than 11 g/dl), and published in the English language were included. Studies conducted among pregnant women but who had comorbidities like; like HIV/AIDS, renal disease, and other medical or surgical conditions were excluded from this study. Articles were assessed for inclusion using their title, abstract and then a full review of papers was done before inclusion to the final review.
Outcome of interest
The primary outcome of this study was magnitude of anemia during pregnancy. The WHO defines anemia in pregnany as low blood hemoglobin concentration, below 11 g/dl or hematocrit level less than 33% [1]. The determinant variables included in this review were; residence (urban vs rural), pregnancy interval (less than two years, greater than or equal to two years), malaria infection during pregnancy and total number of pregnancy (primigravida or multigravida). Primigravida refers to women who are pregnant for the first time and multigravida refers to women who are pregnant two or more times [18, 19].
Quality assessment and data collection
Joanna Briggs Institute Meta-Analysis of Statistics Assessment and Review Instrument (JBI-MAStARI) was used for critical appraisal of studies [20]. Two reviewers independently assessed the articles for overall study quality and for inclusion in the review. Any unlear information and disagreement which arises between the reviewers was resolved through discussion and by involving a third reviewer. The researchers developed a data extraction tool. The tool included information on the name of the author/s, publication year, study period, study design, sample size, study area, age of study participants, response rate, mean hemoglobin level, and the prevalence of anemia. Inaddition, the tool contains questions on the prevalence of anemia by residence, number of pregnancy, malaria infection during pregnancy and pregnancy gap.
Publication bias and heterogeneity
Publication bias and heterogeneity were assessed using the Egger’s and Begg’s tests [21, 22]. A p-value less than 0.05 were used to declare statistical significance of publication bias. The heterogeneity of studies was also checked using I 2 test statistics. The I 2 test statistics of 25%, 50%, and 75% was declared as low, moderate and high heterogeneity respectively [23]. A p-value less than 0.05 was used to declare heterogeneity. For the test result which indicates the presence of heterogeneity, random effect model was used as a method of analysis, since it reduces the heterogeneity of studies [23].
Statistical methods and analysis
Data were entered into Microsoft Excel and then exported to STATA 14 software for further analysis. Forest plot was used to present the combined estimate with 95% confidence interval (CI) of the meta-analysis. Subgroup analysis was conducted by regions of the country and type of study design. The effect of selected predictor variables which include; number of pregnancy, malaria infection during pregnancy, pregnancy gap, and residence on the anemia during pregnancy was analyzed using separate categories of meta-analysis. The findings of meta-analysis were presented using forest plot and relative risk (RR) with its 95% CI.
Results
Study selection
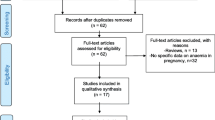
This review included published studies on anemia among pregnant women in Ethiopia. The electronic search was done on several databases, which include; PUBMED, Cochrane Library, Google Scholar, CINAHL, and African Journals Online. The review found a total of 1592 published articles. From this, 86 duplicate records were removed and 1467 records were excluded after screening by title and abstracts. A total of 39 full-text articles were screened for eligibility. From this, 19 articles were excluded since they included non-pregnant women and the outcome variables was not reported. Finally, 20 studies were included in the final quantitative meta-analysis (Fig. 1).
Characteristics of included studies
All included studies were cross-sectional conducted among pregnant women. The minimum sample size was 150 participants in a study conducted in Nekemte [24]. While, the higher sample size was 1678, conducted in Haramaya district of Oromia region [25]. Overall, this meta-analysis included a total of 10, 281 pregnant women. All studies used the WHO definition of anemia during pregnancy [1]. The minimum and maximum age of pregnant women included in this review were 14 years and 42 years respectively. Thirteen, 65% of the included studies were conducted at health institution [24, 26,27,28,29,30,31,32,33,34,35,36,37] and 7(35%) of studies were community-based studies [25, 38,39,40,41,42,43]. Most of the regions in Ethiopia were represented in this review. One of the study was conducted in Addis Ababa, capital city of Ethiopia [34], 3 were from Amhara region [27, 28, 36], 6 from Oromia region [24, 25, 30, 35, 37, 42], 1 from Somali region [38], 5 from SNNPR [29, 32, 33, 40, 43], 2 from Tigray region [26, 31], and 2 were nationwide studies [39, 41] (Table 1).
Prevalence of anemia among pregnant women
The minimum prevalence of anemia was 9.7% observed in a study conducted in North Shoa zone [28]. The highest, 56.8% was observed in a study conducted in Eastern Ethiopia [38]. The I 2 test result showed high heterogeneity (I2 97.7%, p = <0.001). Using the random effect analysis, the pooled prevalence of anemia among pregnant women in Ethiopia was 31.66% (95% CI (26.20, 37.11)) (Fig. 2).
A subgroup analysis by region in Ethiopia was computed to compare the prevalence of anemia acroos different participants characterstics. Based on this analysis, the lowest prevalence of anemia among pregnant women was observed in Amhara region, 15.89% (95% CI (8.82, 22.96)) and the highest prevalence was in Somali region; 56.80%(95% CI (52.76, 60.84)). A higher prevalence (39.49%) of anemia among pregnant women was observed in studies conducted at community level than facility based studies (27.31%) (Table 2).
Association of malaria infection and anemia during pregnancy
Women who had malaria infection during pregnancy were almost two times more likely to develop anemia during pregnancy than women had no such infection, RR: 1.94 (95% CI (1.33, 2.82)). The heterogeneity test showed statistical evidence of heterogeneity, p = <0.001. As a result, weights were calculated using the random-effects analysis. The Begg’s and Egger’s test for publication bias showed no statistical evidence of publication bias, p-value = >0.05 and p-value = 0.543 respectively (Fig. 3).
Association of number of pregnancy with anemia during pregnancy
The meta-analysis showed that premigravida women were 61% less likely to develop anemia during pregnancy compared tomultigravida women, RR: 0.61 (95% CI (0.53, 0.71)). The heterogeneity test showed no statistical evidence of heterogeneity, p = 0.530. The Begg’s and Egger’s test for publication bias also showed no statistical evidence of publication bias, p-value = 0.36 and p-value = 0.397 respectively (see Additional file 1).
Association of short pregnancy interval with anemia during pregnancy
Women who had short pregnancy interval were more than two times more likely to develop anemia during the current pregnancy than women who had more than two years pregnancy interval, RR: 2.14 (95% CI (1.67, 2.74)). The heterogeneity test showed no statistical evidence of heterogeneity, p = 0.108. The Begg’s and Egger’s test for publication bias also showed no statistical evidence of publication bias, p-value = 0.266 and p-value = 0.112 respectively (see Additional file 2).
Association of residence with anemia during pregnancy
Women living in urban areas were 73% less likely to be anemic during pregnancy than women in the rural area, RR: 0.73 (95% CI (0.60, 0.88)). The heterogeneity test showed statistical evidence of heterogeneity, p = 0.003. But, the Begg’s and Egger’s test for publication bias showed no statistical evidence of publication bias, p-value = 0.602 and p-value = 0.581 respectively (see Additional file 3).
Discussion
This review was conducted to determine the pooled prevalence and determinants of anemia among pregnant women in Ethiopia using published studies. Anemia during pregnancy is associated with increased risk of obstetric problems [44]. Studies have shown that anemia is associated with maternal physical and psychological comorbidity, and with an increased risk of perinatal and maternal morbidity and mortality [45,46,47].
The pooled meta-analysis of this review found that the prevalence of anemia among pregnant women in Ethiopia was 31.66% (95%CI: (26.20, 37.11)). The 2016 Ethiopian demographic and health survey (EDHS) report showed a lower (24%) prevalence of anemia among reproductive-aged women, and 29% among pregnant women [48]. This showed a higher prevalence of anemia among pregnant women than non-pregnant reproductive age women. This could be explained by an extra demand of iron by the pregnant women for fetal growth and development during pregnancy. This report is lower than the current finding. The possible explanation for the difference could be related to the sampling and study period. The EDHS was conducted in a nationally representative sample across all regions of the country, while this study included only few regions of the country. The current review also included studies conducted since 2001.
A meta-analysis on global trend of anemia showed that 38% of pregnant women were anemic in 2011 [3]. The review also showed that 36% prevalence of anemia among pregnant women in East Africa and 22% prevalence in high-income regions [3]. The East African finding is relatively higher than the findings of this review. A possible explanation could be the time difference between the two reviews in which the current review also included recent studies and the difference in the sociodemographic characteristics of participants included in the review.
Subgroup analysis based on the regions of the country showed a lower and higher prevalence of anemia in Amhara region (15.89%) and Somali region (56.8%) respectively. The difference in the prevalence between the regions in Ethiopia could be attributed due to the difference in the sociodemographic, socioeconomic, iron-folic acid intake and the difference in the magnitude of the communicable and non-communicable diseases. The difference in the number of studies included in each category of analysis could also be the reason for the difference.
The result of the meta-analysis showed that primigravida women were 61% less likely to develop anemia during pregnancy compared to multigravida women. This could be because of the effect of repeated pregnancy in depleting the iron store of a pregnant woman [49, 50]. A study conducted in Malaysia also found a higher proportion of anemia (66.7%) among grand multigravida women [51].
A shorter interpregnancy interval increases the risk of adverse obstetric outcomes [52]. Short birth interval is associated with preterm births, low birth weight, stillbirth and early neonatal death [52]. The current study also found that pregnant women with short pregnancy interval were more than two times more likely to develop anemia during the current pregnancy than women who had more than two years pregnancy interval. This could be explained by the effect of repeated and short interpregnancy interval and breastfeeding on the overall physiologic status of the mother. The woman will not get enough time to recover from the depleted nutrients [50]. A systematic review of the effect of birth spacing on the maternal and child nutritional status found that short birth intervals are related to maternal anemia [49]. Similar findings were also observed in a study conducted in Tanzania [53].
Pregnant women living in urban areas are 73% less likely to be anemic during pregnancy than women in the rural area. The difference in the socioeconomic status, educational and occupational status of pregnant women, difference in the health service access between rural and urban areas could be the justification for the difference. Additionally, inadequate counselling by health professionals in resolving the wrong beliefs and myths regarding the iron supplementation could contribute to higher prevalence of anemia among pregnant women in rural areas [54, 55]. A study conducted in India also showed that pregnant women from the rural areas are more likely to develop anemia than women from the urban area [54].
WHO recommends early diagnosis and effective treatment of malaria infections and the use of long-lasting insecticidal nets (LLINS) during pregnancy [56]. The result of this meta-analysis showed that women who had malaria attack during pregnancy are almost two times more likely to develop anemia during pregnancy. A review of studies conducted in Sub-Saharan African countries also found that there is a higher (26%) risk of severe anemia in pregnant women secondary to malaria infection. Malaria infection is responsible for one in ten cases of severe anemia in pregnant women [46]. Similar findings was also observed in a study conducted in Kenya [57].
This review used a comprehensive search strategy and more than one reviewer was involved in each step of the review process. PRISMA guideline was strictly followed during the review process. This review has certain limitations. Studies included were cross-sectional and the outcome variable may be affected by other confounding variables. Some studies included in this review didn’t consider respondents’ residential altitude above sea level to define anemia. Studies have shown that there is an increase in the hemoglobin level when people’s live at high altitude [58, 59]. These limitations could affect the overall prevalence of anemia in the country presented in this review.
Conclusions
Almost one-third of pregnant women in Ethiopia were anemic. Statistically significant association was observed between anemia during pregnancy and residence, gravidity, pregnancy interval and malaria infection during their pregnancy. Regions with higher anemia prevalence among pregnant women should be given due attention. Further studies should be conducted to better understand the determinant factors in these regions.
The government and non-governmental organizations should focus on strengthening iron and folic acid supplementation for all pregnant women as part of the routine antenatal care. The use of long-lasting insecticidal nets during pregnancy, early diagnosis and appropriate treatment of malaria in pregnant women, and the use of long-acting family planning methods to prevent short pregnancy intervalsis important and should be stengtehend in areas of higher anemia prevalence in Ethiopia. Health extension workers should be involved in the promotion of antenatal follow-ups and community-based awareness programs, especially in rural areas. Further nationwide studies are needed to understand the determinant factors for anemia in pregnant women.
Abbreviations
- CI:
-
Confidence Interval
- EDHS:
-
Ethiopian Demographic and Health Survey
- LLINS:
-
Long-lasting insecticidal nets
- RR:
-
Relative Risk
- SNNPR:
-
Southern Nations, Nationalities, and Peoples’ Region of Ethiopia
- WHO:
-
World Health Organization
References
WHO. The global prevalence of anaemia in 2011. Geneva: World Health Organization; 2015.
Black RE, Allen LH, Bhutta ZA, Caulfield LE, De Onis M, Ezzati M, Mathers C, Rivera J, Maternal and child undernutrition study group. Maternal and child undernutrition: global and regional exposures and health consequences. The lancet. 2008;371(9608):243–60.
Stevens GA, Finucane MM, De-Regil LM, Paciorek CJ, Flaxman SR, Branca F, et al. Global, regional, and national trends in haemoglobin concentration and prevalence of total and severe anaemia in children and pregnant and non-pregnant women for 1995–2011: a systematic analysis of population-representative data. Lancet Glob Health. 2013;1(1):e16–25.
Huch R. Anemia in pregnancy. Praxis. 1999;88(5):157–63.
WHO. Global nutrition targets 2025: anaemia policy brief (WHO/NMH/NHD/14.4). Geneva: World Health Organization; 2014.
Sifakis S, Pharmakides G. Anemia in pregnancy. Ann N Y Acad Sci. 2000;900:125–36.
Schwartz WJ 3rd, Thurnau GR. Iron deficiency anemia in pregnancy. Clin Obstet Gynecol. 1995;38(3):443–54.
McClure EM, Goldenberg RL, Dent AE, Meshnick SRA. Systematic review of the impact of malaria prevention in pregnancy on low birth weight and maternal anemia. Int J Gynaecol Obstet. 2013;121(2):103–9.
Lee AI, Okam MM. Anemia in pregnancy. Hematol Oncol Clin North Am. 2011;25(2):241–59. vii
Karaoglu L, Pehlivan E, Egri M, Deprem C, Gunes G, Genc MF, et al. The prevalence of nutritional anemia in pregnancy in an east Anatolian province, Turkey. BMC Public Health. 2010;10:329.
Olubukola A, Odunayo A, Adesina O. Anemia in pregnancy at two levels of health care in Ibadan, south west Nigeria. Annals of African medicine. 2011;10(4):272–7.
Ouedraogo S, Koura GK, Bodeau-Livinec F, Accrombessi MM, Massougbodji A, Cot M. Maternal anemia in pregnancy: assessing the effect of routine preventive measures in a malaria-endemic area. The American journal of tropical medicine and hygiene. 2013;88(2):292–300.
Kazmierczak W, Fiegler P, Adamowicz R, Muszer M, Kaminski K. Prevention of iron deficiency anemia--influence on the course of pregnancy, delivery and the infant's status. Wiadomosci lekarskie. 2004;57(Suppl 1):144–7.
Scholl TO, Reilly T. Anemia, iron and pregnancy outcome. J Nutr. 2000;130(2S Suppl):443S–7S.
Lops VR, Hunter LP, Dixon LR. Anemia in pregnancy. Am Fam Physician. 1995;51(5):1189–97.
Kalenga MK, Mutach K, Nsungula K, Odimba FK, Kabyla I. Anemia in pregnancy. Clinical and biological study. Apropos of 463 cases seen in Lubumbashi (Zaire). Revue francaise de gynecologie et d'obstetrique. 1989;84(5):393–9.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–9.
Danish N, Fawad A, Abbasi N. Assessment of pregnancy outcome in primigravida: comparison between booked and un-booked patients. Journal of Ayub Medical College, Abbottabad : JAMC. 2010;22(2):23–5.
Woman to Woman Childbirth Education. Primigravida, primiparous, multigravida. https://womantowomancbe.wordpress.com/. Accessed 29 June 2017.
The Joanna Briggs Institute. Joanna Briggs institute reviewers’ manual: 2008.
Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50(4):1088–101.
Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ: British Medical Journal. 2003;327(7414):557.
Mihiretie H, Fufa M, Mitiku A, Bacha C, Getahun D, Kejela M, Sileshi G, Wakshuma B. Magnitude of anemia and associated factors among pregnant women attending antenatal care in Nekemte health center, Nekemte, Ethiopia. Journal of Medical Microbiology & Diagnosis. 2015;4(3):1–4.
Kedir H, Berhane Y, Worku A. Khat chewing and restrictive dietary behaviors are associated with anemia among pregnant women in high prevalence rural communities in eastern Ethiopia. PLoS One. 2013;8(11):e78601.
Abriha A, Yesuf ME, Wassie MM. Prevalence and associated factors of anemia among pregnant women of Mekelle town: a cross sectional study. BMC research notes. 2014;7(1):1.
Alem M, Enawgaw B, Gelaw A, Kenaw T, Seid M, Olkeba Y. Prevalence of anemia and associated risk factors among pregnant women attending antenatal care in Azezo health center Gondar town, Northwest Ethiopia. Journal of Interdisciplinary Histopathology. 2013;1(3):137–44.
Ayenew F, Abere Y, Timerga G. Pregnancy anaemia prevalence and associated factors among women attending ante Natal Care in north Shoa zone, Ethiopia. Reproductive System & Sexual Disorders. 2014;3(135):1–7.
Bekele A, Tilahun M, Mekuria A. Prevalence of anemia and its associated factors among pregnant women attending antenatal Care in Health Institutions of Arba Minch town, Gamo Gofa zone, Ethiopia: a cross-sectional study. Anemia. 2016;2016:9. doi:10.1155/2016/1073192.
Ejeta E, Alemnew B, Fikadu A, Fikadu M, Tesfaye L, Birhanu T, Nekemte E. Prevalence of anaemia in pregnant womens and associated risk factors in Western Ethiopia. Food Science and Quality Management. 2014;31:82–91.
Gebre A, Mulugeta A. Prevalence of anemia and associated factors among pregnant women in north western zone of Tigray, northern Ethiopia: a cross-sectional study. Journal of nutrition and metabolism. 2015;2015:7. doi:10.1155/2015/165430.
Gedefaw L, Ayele A, Asres Y, Mossie A. Anaemia and associated factors among pregnant women attending antenatal care clinic in Walayita Sodo town, southern Ethiopia. Ethiopian journal of health sciences. 2015;25(2):155–64.
Gies S, Brabin BJ, Yassin MA, Cuevas L. Comparison of screening methods for anaemia in pregnant women in Awassa, Ethiopia. Tropical Med Int Health. 2003;8(4):301–9.
Jufar AH, Zewde T. Prevalence of anemia among pregnant women attending antenatal care at tikur anbessa specialized hospital, Addis Ababa Ethiopia. Journal of Hematology & Thromboembolic. Diseases. 2014;2014:2–125. doi:10.4172/2329-8790.1000125.
Kefiyalew F, Zemene E, Asres Y, Gedefaw L. Anemia among pregnant women in Southeast Ethiopia: prevalence, severity and associated risk factors. BMC research notes. 2014;7(1):1.
Melku M, Addis Z, Alem M, Enawgaw B. Prevalence and predictors of maternal anemia during pregnancy in Gondar, Northwest Ethiopia: an institutional based cross-sectional study. Anemia. 2014;2014:9. doi:10.1155/2014/108593.
Obse N, Mossie A, Gobena T. Magnitude of anemia and associated risk factors among pregnant women attending antenatal care in Shalla Woreda, west Arsi zone, Oromia region, Ethiopia. Ethiopian journal of health sciences. 2013;23(2):165–73.
Addis Alene K, Mohamed Dohe A. Prevalence of anemia and associated factors among pregnant women in an urban area of eastern Ethiopia. Anemia. 2014;2014:7. doi:10.1155/2014/561567.
Alemu T, Umeta M. Reproductive and obstetric factors are key predictors of maternal anemia during pregnancy in Ethiopia: evidence from demographic and health survey (2011). Anemia. 2015;2015:8. doi:10.1155/2015/649815.
Gebremedhin S, Enquselassie F, Umeta M. Prevalence and correlates of maternal anemia in rural Sidama, southern Ethiopia. Afr J Reprod Health. 2014;18(1):44–53.
Gebremedhin S, Samuel A, Mamo G, Moges T, Assefa T. Coverage, compliance and factors associated with utilization of iron supplementation during pregnancy in eight rural districts of Ethiopia: a cross-sectional study. BMC Public Health. 2014;14(1):1.
Getachew M, Yewhalaw D, Tafess K, Getachew Y, Zeynudin A. Anaemia and associated risk factors among pregnant women in Gilgel gibe dam area, Southwest Ethiopia. Parasit Vectors. 2012;5(1):1.
Nega D, Dana D, Tefera T, Eshetu T. Anemia associated with asymptomatic malaria among pregnant women in the rural surroundings of Arba Minch town, South Ethiopia. BMC research notes. 2015;8(1):1.
Central Statistical Agency/Ethiopia, ICF International. Ethiopia demographic and health survey 2011. Addis Ababa, Ethiopia: Central Statistical Agency/Ethiopia and ICF International; 2012.
Shulman CE. Malaria in pregnancy: its relevance to safe-motherhood programmes. Annals of Tropical Medicine & Parasitology. 1999;93(sup1):S59–66.
Guyatt HL, Snow RW. The epidemiology and burden of plasmodium falciparum-related anemia among pregnant women in sub-Saharan Africa. The American journal of tropical medicine and hygiene. 2001;64(1_suppl):36–44.
Desai M, ter Kuile FO, Nosten F, McGready R, Asamoa K, Brabin B, et al. Epidemiology and burden of malaria in pregnancy. Lancet Infect Dis. 2007;7(2):93–104.
Central Statistical Agency (CSA) [Ethiopia] and ICF. Ethiopia demographic and health survey 2016. Addis Ababa, Ethiopia, and Rockville, Maryland, USA: CSA and ICF; 2016.
Dewey KG, Cohen RJ. Does birth spacing affect maternal or child nutritional status? A systematic literature review. Maternal & child nutrition. 2007;3(3):151–73.
Merchant K, Martorell R. Frequent reproductive cycling: does it lead to nutritional depletion of mothers? Progress in food & nutrition science. 1988;12(4):339–69.
Nik Rosmawati N, Mohd Nazri S, Mohd II. The rate and risk factors for anemia among pregnant mothers in Jerteh Terengganu, Malaysia. J Community Med Health Educ. 2012;2(150):2161–0711.1000150.
Wendt A, Gibbs CM, Peters S, Hogue CJ. Impact of increasing inter-pregnancy interval on maternal and infant health. Paediatr Perinat Epidemiol. 2012;26(s1):239–58.
Lilungulu A, Matovelo D, Kihunrwa A, Gumodoka B. Spectrum of maternal and perinatal outcomes among parturient women with preceding short inter-pregnancy interval at Bugando medical Centre, Tanzania. Maternal health, neonatology and perinatology. 2015;1(1):1.
Gowri D, Sakthi D, Palanivel C. Influence of awareness and attitude about anemia and iron supplements on anemic status of pregnant women attending a tertiary care centre in South India. Journal of contraceptive studies. 2017;2:1. doi:10.21767/2471-9749.100026.
Adamu AL, Crampin A, Kayuni N, Amberbir A, Koole O, Phiri A, et al. Prevalence and risk factors for anemia severity and type in Malawian men and women: urban and rural differences. Popul Health Metrics. 2017;15(1):12.
World Health Organization. Malaria in pregnant women. Last update: 25 May 2017. retrived on 29/06/2017, from; http://www.who.int/malaria/areas/high_risk_groups/pregnancy/en/.
Shulman C, Marshall T, Dorman E, Bulmer J, Cutts F, Peshu N, et al. Malaria in pregnancy: adverse effects on haemoglobin levels and birthweight in primigravidae and multigravidae. Tropical Med Int Health. 2001;6(10):770–8.
Dirren H, Logman MH, Barclay DV, Freire WB. Altitude correction for hemoglobin. Eur J Clin Nutr. 1994;48(9):625–32.
Dallman PR, Siimes MA, Stekel A. Iron deficiency in infancy and childhood. Am J Clin Nutr. 1980;33(1):86–118.
Acknowledgements
We would like to acknowledge to authors of studies included in this review.
Funding
No funding was obtained for this study.
Availability of data and materials
All data pertaining to this study are contained and presented in this document.
Author information
Authors and Affiliations
Contributions
GMK involved in the design, selection of articles, data extraction, statistical analysis and manuscript writing. AAM, AKB, and GAF also involved in data extraction, analysis, and manuscript editing. All authors read and approved the final draft of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interest
The authors declare that they have no competing interest.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional files
Additional file 1:
Forest plot displaying the effect of gravidity in a pregnant woman and anemia among pregnant women in Ethiopia. Description of figure: This figure presents the effect of gravdity on anemia during pregnancy. Multigravida women are more likely to develop anemia during pregnancy than primigravida. (DOCX 18 kb)
Additional file 2:
Forest plot displaying the effect of short pregnancy interval and anemia among pregnant women in Ethiopia. Description of figure: This figure presents the effect of short pregnancy interval on anemia during pregnancy. Women who have shorter pregnancy interval are more likely to develop anemia during pregnancy than women with pregnancy interval of more than two years. (DOCX 17 kb)
Additional file 3:
Forest plot displaying the effect residence of pregnant woman and anemia among pregnant women in Ethiopia. Description of figure: This figure presents the effect of residence on anemia during pregnancy. Women who are residing in rural areas are more likely to develop anemia during pregnancy than pregnant women in urban areas. (DOCX 18 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Kassa, G.M., Muche, A.A., Berhe, A.K. et al. Prevalence and determinants of anemia among pregnant women in Ethiopia; a systematic review and meta-analysis. BMC Hematol 17, 17 (2017). https://doi.org/10.1186/s12878-017-0090-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12878-017-0090-z