Abstract
The role of skeletal muscle and adipose tissue in the progression of cancer has been gradually discussed, but it needs further exploration. The objective of this study was to provide an in-depth analysis of skeletal muscle and fat in digestive malignancies and to construct novel predictors for clinical management. This is a retrospective study that includes data from Cancer Center, the First Hospital of Jilin University. Basic characteristic information was analyzed by T tests. Correlation matrices were drawn to explore the relationship between CT-related indicators and other indicators. Cox risk regression analyses were performed to analyze the association between the overall survivals (OS) and various types of indicators. A new indicator body composition score (BCS) was then created and a time-dependent receiver operating characteristic curve was plotted to analyze the efficacy of the BCS. Finally, a nomogram was produced to develop a scored-CT system based on BCS and other indicators. C-index and calibration curve analyses were performed to validate the predictive accuracy of the scored-CT system. A total of 575 participants were enrolled in the study. Cox risk regression model revealed that VFD, L3 SMI and VFA/SFA were associated with prognosis of cancer patients. After adjustment, BCS index based on CT was significantly associated with prognosis, both in all study population and in subgroup analysis according to tumor types (all study population: HR 2.036, P < 0.001; colorectal cancer: HR 2.693, P < 0.001; hepatocellular carcinoma: HR 4.863, P < 0.001; esophageal cancer: HR 4.431, P = 0.008; pancreatic cancer: HR 1.905, P = 0.016; biliary system malignancies: HR 23.829, P = 0.035). The scored-CT system was constructed according to tumor type, stage, KPS, PG-SGA and BCS index, and it was of great predictive validity. This study identified VFD, L3 SMI and VFA/SFA associated with digestive malignancies outcomes. BCS was created and the scored-CT system was established to predict the OS of cancer patients.
Similar content being viewed by others
Introduction
Cancer remains one of the leading threats to human health, with an estimated 19.3 million new cancer cases in 2020, according to the International Agency for Research on Cancer. Among them, there were nearly 6 million cases of digestive system malignancies, which accounted for more than 30% of the total number of new cancer cases worldwide1. Genetic changes are only one part of the development of digestive system malignancies, while lifestyle and dietary habits may have a more significant impact on them, among which, excessive nutrition and obesity lead to many cancers, including esophageal, colorectal, and gastric cancers2,3.
Higher body mass index (BMI) is thought to be associated with more aggressive tumor cells and poorer clinical outcomes for cancer patients, but such claims have been contradicted in multiple studies4,5,6. BMI cannot identify the exact body components that affect health risks, in which case, it cannot directly distinguish between muscle tissue and adipose tissue, nor can it accurately evaluate the distribution of each component, which leads to the inability to identify the hidden obesity of the patients and cannot effectively reflect the real condition of the body. In this context, a series of body composition analysis methods, such as bioelectrical impedance analysis (BIA), are gaining popularity. Cancer patients are in a state of chronic depletion and their body composition is quietly changing. Accurate assessment of a patient's body composition can provide doctors with guidance for individualized and precise treatment. Highly sensitive imaging tools, such as computed tomography (CT) have been recommended to assess muscle quality. It is considered to be the gold standard for evaluating the composition of the body, and by detecting potential changes in the body, it could guide medical decision-makers for timely changes in therapeutic management strategies7.
It is feasible to evaluate the response to antitumor therapy and the prognosis of cancer patients using muscle and fat status8,9,10,11. However, current research is often one-sided, with researchers often exploring the role of only one of these components in depth, ignoring the combined effects of both skeletal muscle and fat. The clinical outcome of patients is the result of a combination of factors, and it is necessary to clarify the specific values of various components considering the important role of body components in cancer patients. The objective of this study was to explore the prognostic value of CT-measured fat and skeletal muscle components in patients with digestive system malignancies and to construct a new indicator for clinical guidance.
Participants and methods
Study participants
This is a retrospective study that screened patients who were admitted to the Cancer Center of the First Hospital of Jilin University from January 1st, 2015 to December 30th, 2021. The inclusion criteria were as follows: (1) Cancer confirmed by pathology with an Eastern Cooperative Oncology Group performance status of 0, 1, or 2; (2) No anti-tumor therapy or related therapy before assessment; (3) No metabolic disease or autoimmune disease; (4) Abdominal CT examination within 1 month before or after the diagnosis of cancer; (5) Age > 18 years old. Meanwhile, the exclusion criteria were as follows: (1) Patients with other types of tumors; (2) History of trauma or surgery within 3 months; (3) Low-quality CT images; (4) Combined with abdominal effusion/pleural effusion; (5) Receive regular hemodialysis; (6) Died within 30 days of admission. The flowchart of study subject inclusion is shown in Fig. 1.
All pathological staging was defined according to the 8th edition of the American Joint Committee on Cancer (AJCC) TNM staging system. The study was approved by the Ethics Committee of the first affiliated hospital of Jilin University (2017-362), and all data in this research was approved by this committee. This study has been performed in accordance with the Declaration of Helsinki and all study participants have filled out written informed consent for participation.
Data collection
The Patient-Generated Subjective Global Assessment (PG-SGA) and Karnofsky Performance Status (KPS) questionnaire were completed within 24 h after admission with professional assistance. According to the PG-SGA score, the nutritional status of patients was assessed. We defined well-nourished as PG-SGA ≤ 2, moderate malnutrition as 3 ≤ PG-SGA ≤ 8, and severe malnutrition as PG-SGA ≥ 912. We used the European Organization for Research and Treatment of Cancer’s Quality of Life Questionnaire Core 30 to assess health-related quality of life (HRQoL)13.
Basic clinical information was recorded, including sex, age, tumor type, tumor stage, smoking history, alcohol history, and previous nutritional therapy. Serological tests were performed in the early morning of the second day after admission, and relevant serological parameters were recorded, including albumin (Alb), C-reactive protein (CRP), neutrophil count, platelet count, lymphocyte count, serum triglycerides (TG), serum total cholesterol (TC), serum high-density lipoprotein cholesterol (HDL-C) and serum low-density lipoprotein cholesterol (LDL-C). Neutrophil to lymphocyte ratio (NLR), platelet to lymphocyte ratio (PLR) and Onodera's prognostic nutritional index (OPNI) were calculated according to the formula: NLR = Neutrophil count (× 109/L)/lymphocyte count (× 109/L); PLR: Platelet count (× 109/L)/lymphocyte count (× 109/L); OPNI = serum albumin level (g/L) + 5 × total number of lymphocytes in peripheral blood (× 109/L)14.
Anthropometric and BIA examinations
Anthropometric and BIA tests were performed within 24 h after admission with professional assistance. In this study, resistance and capacitance were directly measured in ohms at 50 kHz and 800 mA with an Inbody S10 (Biospace Co). Before the measurement, patients voided their bladders, fasted for at least 2 h, and wore a uniform hospital gown; they also avoided physical activity and remained quiet. Patients' relevant indexes were recorded, including height, weight, circumference of the mid-upper arm (MAC), mid-upper arm muscle circumference (MAMC), skinfold thickness (TSF), and the grip strength of the non-dominant hand (HGS). Height and weight were measured to an accuracy of 1 cm and 0.1 kg, respectively. BMI was calculated according to the formula weight (kg)/height2 (m)2. Record appendicular skeletal muscle mass (ASM), extracellular water (ECW) and total body water (TBW). Appendicular skeletal muscle mass index (ASMI) = ASM (kg)/height2 (m2).
Body composition analysis by CT
We quantified data from cross-sectional unenhanced CT scans used to diagnose tumors or tumor staging. All CT scans were exported by radiologists and engineers of the First Hospital of Jilin University and quality control was performed. The final CT images that met the quality control requirements were quantified and analyzed by sliceOmatic (version 5.0; Tomovision, Montreal, Canada) imaging analysis software.
Cross-sectional CT images at the level of the third lumbar (L3) vertebrae for each patient were analyzed. The third lumbar vertebra was set as a landmark, and two consecutive slices were selected to measure the cross-sectional areas of the skeletal muscle. The mean value of two consecutive images was computed for each patient.
Abdominal fat tissue mainly includes subcutaneous fat and visceral fat. Muscle areas included the psoas, erector spinae, quadratus lumborum, transversus abdominis, external and internal obliques, and rectus abdominis muscles. We quantified the cross-sectional areas of subcutaneous fat area (SFA, cm2), visceral fat area (VFA, cm2) and skeletal muscle area of the third lumbar vertebrae (L3 SMA) using standard Hounsfield units (HUs). According to previous research results15,16, we considered a threshold of -190 to -30 HU as subcutaneous fat, -150 to -50 HU as visceral fat and − 29 to 150 HU as skeletal muscle. Total fat area (TFA, cm2) was determined as the sum of the SFA and VFA. In addition, subcutaneous fat density (SFD, HUs), visceral fat density (VFD, HUs) and skeletal muscle density of third lumbar vertebrae (L3 SMD, HUs) were also calculated by the mean attenuation of subcutaneous fat, visceral fat and skeletal muscle using the same CT images, respectively. The ratio of VFA/SFA and VFD/SFD were also recorded. Skeletal muscle index of third lumbar vertebrae (L3 SMI) was calculated according to the formula L3 SMA (cm2)/ height2 (m2). SFA, VFA and TFA were normalized for height2 and reported as SFA index (SFAI, cm2/m2), VFA index (VFAI, cm2/m2) and TFA index (TFAI, cm2/m2)17.
X-tile software to determine the optimal cut-off value
In this study, we used X-tile, a software developed by researchers at Yale University to calculate optimal cut-off values for relevant biological information based on outcomes, to establish appropriate cut-off values for the metrics of interest18. X-tile plots are created by dividing marker data into two populations: low and high. All possible divisions of the marker data are assessed.
Follow-up
All patients were treated with the standard treatment protocol recommended by the guidelines according to tumor type and stage after diagnosis. Participants were regularly followed up by trained persons through telephone interviews or outpatient visits to collect data on survival status and time of events. In this study, we took overall survivals (OS) as the endpoint. Participants were followed from the initial admission until they died or until the end of December 2021.
Statistical analysis
SPSS 26.0 statistical software and R Project for Statistical Computing (version 4.0.5) were used for data analyses. Continuous variables were expressed as the mean ± standard deviation and categorical variables were presented as counts (%). Basic characteristic information of males and females were analyzed by T-tests. The relationship between basic clinical information, anthropometric indicators, serological indicators, BIA data, and CT-related indicators of patients was analyzed using correlation matrices. The optimal cut-off values of CT-related indicators were determined in male and female patients separately using X-tile software and divided into high and low value groups based on the cut-off values. A univariate Cox risk regression model was used to analyze the relationship between OS and CT-related indicators. All statistically significant indicators were included in the multivariate analysis, and the best-fitting Cox risk regression model was constructed using likelihood ratio forward selection (Forward LR). Tumor type and tumor stage were considered as categorical variables. Multicollinearity was tested by linear regression analysis, and variance inflation factor (VIF) > 10 or tolerance < 0.1 was considered as collinearity existence. A new index body composition score (BCS) was constructed based on the results of multivariate Cox. The role of BCS in predicting prognosis was explored in all study participants and in different tumor type subgroups separately, and a time-dependent ROC curve of BCS was plotted. A nomogram was generated to develop the scored-CT system with statistically significant variables of multivariate Cox regression. C-index and calibration curve analyses were performed to validate the predictive accuracy of the scored-CT system.
Ethics approval and consent to participate
The study was approved by the Ethics Committee of the first affiliated hospital of Jilin University (2017-362), and all the patient data in this research was approved by this committee. All study participants have filled out written informed consent for participation.
Results
Baseline characteristic
A total of 575 subjects meeting the criteria were finally enrolled in the study, including 362 males (63.0%) and 213 females (37.0%). The mean age of the overall study population was 59.63 years. Colorectal cancer dominated with 310 cases, accounting for 53.9%, while the rest were patients with gastric cancer, hepatocellular carcinoma, pancreatic cancer, esophageal cancer and biliary system malignant tumors in that order. The majority of patients were stage IV when diagnosed, accounting for 38.1% of the total study subjects (See Table 1). A total of 195 participants died during the follow-up.
Correlation analysis of study indicators
In terms of gender, male and female patients were statistically different in several CT-related indicators (SFA: 98.87 ± 50.06 vs. 144.29 ± 65.98, P < 0.001; SFD: − 88.93 ± 11.30 vs. − 96.10 ± 9.75, P < 0.001; SFAI: 33.75 ± 16.87 vs. 58.20 ± 26.70, P < 0.001; VFA: 110.47 ± 72.22 vs. 87.19 ± 53.55, P < 0.001; L3 SMA: 139.55 ± 25.45 vs. 95.50 ± 16.96, P < 0.001; L3 SMD: 38.44 ± 7.10 vs. 32.66 ± 6.83, P < 0.001; L3 SMI: 47.87 ± 8.56 vs. 38.57 ± 6.30, P < 0.001; TFA: 208.69 ± 115.29 vs. 231.48 ± 108.49, P = 0.036; TFAI: 71.27 ± 39.11 vs. 93.40 ± 44.07, P < 0.001; VFA/SFA: 1.10 ± 0.50 vs. 0.65 ± 0.47, P < 0.001; VFD/SFD: 1.02 ± 0.09 vs. 0.95 ± 0.08, P < 0.001; Males vs. Females, respectively). We observed that although VFD and VFAI were higher in males than those in females, this difference was not statistically significant (See Supplemental Table 1). We then plotted the correlation matrix separately for male and female and could see that CT-related indicators were significantly correlated with several clinical information, anthropometric indicators, serological indicators and BIA indicators (See Fig. 2).
Determination of prognosis-related indicators
The optimal cut-off values for CT-related indices were first determined by X-tile. We calculate the best cut-off values for males and females separately. The final results were obtained as follows: in males, SFA was 92.01 cm2, SFD was -91.61 HUs, SFAI was 28.51 cm2/m2, VFA was 69.20 cm2, VFD was − 87.37 HUs, VFAI was 20.72 cm2/m2, L3 SMA was 125.70 cm2, L3 SMD was 36.50HUs, L3 SMI was 43.11 cm2/m2, TFA was 296.78 cm2, TFAI was 79.53 cm2/m2, VFA/SFA was 0.69 and VFD/SFD was 1.10; in females, SFA was 65.96 cm2, SFD was − 86.45 HUs, SFAI was 26.65 cm2/m2, VFA was 27.06 cm2, VFD was − 81.11 HUs, VFAI was 10.70 cm2/m2, L3 SMA was 89.30 cm2, L3 SMD was 25.48 HUs, L3 SMI was 33.83 cm2/m2, TFA was 81.62 cm2, TFAI was 33.86 cm2/m2, VFA/SFA was 0.69 and VFD/SFD was 1.02 (See Supplemental Fig. 1). We divided the patients into high and low value groups according to the results of the corresponding indicators.
With OS as the observation endpoint, the results of the univariate Cox risk regression model revealed that several indicators correlated with OS (See Table 2). In a further multivariate Cox risk regression model, we fitted a Forward LR approach to form the best model, and the results suggested that among all CT-related indicators, only VFD, L3 SMI, and VFA/SFA were associated with prognosis of cancer patients (HR 2.473, 95% CI of HR 1.716–3.564, P < 0.001; HR 0.580, 95% CI of HR 0.385–0.872, P = 0.009; HR 1.812, 95% CI of HR 1.201–2.733, P = 0.005; See Table 2). In addition, tumor type, stage, surgical resection or not, KPS, PG-SGA and Alb were also associated with OS in cancer patients. Multicollinearity was tested by linear regression analysis, and VIF > 10 or tolerance < 0.1 was considered as collinearity existence. Supplemental Table 2 showed no collinearity existed among these variables, indicating that the multivariate Cox risk regression model by a Forward LR approach was well constructed.
Establishment of body composition score based on CT
We combined VFD, L3 SMI and VFA/SFA to create a new CT-based index body composition score (BCS). According to the Cox results, we defined VFD-High, L3 SMI-Low, VFA/SFA-High as the risk group and assigned a score of 1. The rest were assigned a score of 0. BCS was the sum of the scores of each group (See Supplemental Table 3). A Venn diagram of patients with different CT characteristics was presented (See Supplemental Fig. 2).
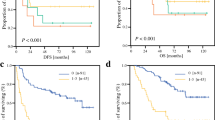
To further clarify the value of BCS, we explored the role of BCS in predicting prognosis in the overall study population, as well as after grouping according to tumor type, respectively. To minimize clinical bias, four different adjustment models were constructed. Model 1: unadjusted; Model 2: adjusted for age, sex, stage, tumor type; Model 3: adjusted for age, sex, stage, tumor type, KPS score, PG-SGA, HRQoL; Model 4: adjusted for age, sex, stage, tumor type, KPS score, PG-SGA, HRQoL, Alb, PLR, OPNI, BMI, MAC, MAMC, HGS, ECW/TBW. In the overall study population, BCS was significantly associated with patient OS (Model 1: HR 2.101, 95% CI of HR 1.721–2.565, P < 0.001; Model 2: HR 2.507, 95% CI of HR 2.000–3.142, P < 0.001; Model 3: HR 2.037, 95% CI of HR 1.647–2.519, P < 0.001; Model 4: HR 2.036, 95% CI of HR 1.644–2.521, P < 0.001; See Table 3). Further subgroup analysis was done according to tumor types, and BCS was a valid prognostic predictor in colorectal cancer, hepatocellular carcinoma, esophageal cancer, pancreatic cancer and biliary system malignancies (HR 2.693, 95% CI of HR 1.755–4.132, P < 0.001; HR 4.863, 95% CI of HR 2.451–9.649, P < 0.001; HR 4.431, 95% CI of HR 1.472–13.335, P = 0.008; HR 1.905, 95% CI of HR 1.127–3.219, P = 0.016; HR 23.829, 95% CI of HR 1.242–457.310, P = 0.035, respectively; See Table 3). In the subgroup analysis of gastric cancer patients, after adjusting by models, we did not find BCS to be statistically significant in prognostic prediction. However, the HR remained greater than 1, representing a trend that higher BCS in patients with gastric cancer still has a poorer prognosis (HR 2.035, 95% CI of HR 0.783–5.290, P = 0.145).
Time-dependent ROC curve of BCS
To test the predictive validity of the BCS in predicting the prognosis of patients with malignancy, we plotted the time-dependent ROC curve of the BCS. It was observed that the predictive validity of BCS remained around 0.70 throughout the follow-up period, indicating the high prognostic validity of BCS (See Fig. 3).
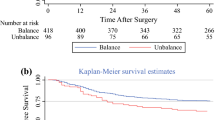
Construction and validation of scored-CT system
A nomogram was constructed according to tumor type, stage, KPS, PG-SGA and BCS to develop a scored-CT system (See Fig. 4). Each subtype within these variables was assigned a score based on a point scale. Each variable site was located on the axis, and then a line was drawn straight upward to the Points axis to determine how many points the patient received from the variables. A scored-CT system to determine the estimated probability of survival at each time point was easily obtained by adding the total score and locating it on the total point scale. To clarify the reliability of the model, we calculated the C-index of the model as 0.813 (95% CI 0.797–0.829). The calibration curves were then plotted for 1, 2, 3, and 5 years (See Fig. 5). It can be seen that the model we constructed predicts the survival rate at 1, 2, 3, and 5 years in high agreement with the actual survival rate of the patients.
The scored-CT system by nomogram used to predict the clinical outcome of patients with digestive system malignancy. Tumor type: 1 = Gastric cancer; 2 = Colorectal cancer; 3 = Hepatocellular carcinoma; 4 = Esophageal cancer; 5 = Pancreatic cancer; 6 = Biliary malignant tumor. Stage: 1 = I; 2 = II; 3 = III; 4 = IV.
Calibration curves of study participants for the nomogram predictions of the 1-, 2-, 3-and 5-year overall survival. (A) Calibration curves of nomogram predictions of the 1-year overall survival; (B) Calibration curves of nomogram predictions of the 2-year overall survival; (C) Calibration curves of nomogram predictions of the 3-year overall survival; (D) Calibration curves of nomogram predictions of the 5-year overall survival.
Discussion
The changes in the body composition of patients with malignant tumors are often dramatic. The prognosis of different individuals in the same disease state or tumor burden condition varies greatly due to differences in body composition19,20. This means that "precision therapy" for human components can help patients achieve better treatment benefits. In this study, we focused on the skeletal muscle and fat status of patients with malignant tumors because they represent the level of individual energy reserves and metabolic status21,22,23, which are of great value to the human body.
We focused on digestive malignancies because abdominal CT is an essential diagnostic and evaluation method for digestive malignancies, which facilitated the acquisition of CT data without increasing the risk of radiation exposure to patients. Skeletal muscle mass at the third lumbar level is significantly associated with the prognosis of various diseases including malignant tumors, which has been confirmed in previous studies11,24,25. Therefore, relevant CT indicators at the third lumbar level are still selected as the object of exploration in this study. It can be seen from the results of the correlation matrix that CT-related indicators are correlated with a variety of biological indicators including PLR, which means that data indicators extracted from CT images have the potential to be used as prognostic biomarkers for cancer patients. We also observed that although BMI was correlated with fat distribution VFA/SFA, the correlation was very low. We believe that this is precisely due to the defects of BMI in the assessment of body composition, which cannot truly reflect the situation of each component and also makes it difficult to detect latent muscle loss in obese patients. Further Cox regression results showed that VFD, L3 SMI and VFA/SFA were CT-related indicators that could significantly affect OS of cancer patients.
It can be seen that for patients with digestive system malignancies, L3 SMI can be used as an important indicator to evaluate their OS. There is a tendency for skeletal muscle mass and function to decline with age, particularly in patients with co-morbid cancers, as prolonged energy depletion results in the forced breakdown of multiple body components involved in metabolism, including increased proteolysis, decreased amino acid transport and regeneration26. When the functional status and quality of skeletal muscle are severely impaired in some patients to a degree that we call sarcopenia, this is associated with poorer clinical outcomes because patients with combined sarcopenia face a greater risk of systemic therapeutic drug toxicity. As we know, platinum-based chemotherapeutic agents are mainly distributed in skeletal muscle tissue for metabolism, and current chemotherapy drug regimens mainly use a body surface area based approach to drug dosing, which may result in high dose levels of systemic chemotherapy drugs given in obese patients with low skeletal muscle mass, causing systemic chemotherapy-related toxicity27. In addition, cancer patients with a combination of sarcopenia are more likely to have postoperative complications and consequently have significantly shorter progression free survivals and OS28,29,30. This could explain the poorer disease prognosis and shorter overall survival time for the L3 SMI-Low patients in our study.
While we acknowledge the value of skeletal muscle in disease and its important role in disease progression, the severe reduction in muscle mass is easily masked by the phenotype of obesity22, potentially misleading clinical decision-makers in their subsequent therapeutic management strategies. Obesity is associated with cardiovascular risk, diabetes, and other diseases, even promoting the development of malignancies and accelerating tumor progression31. However, as we explore obesity more deeply, we find that not all obesity risks are consistent, and the concept of metabolic healthy obesity (MHO) is proposed. Although increased energy storage in the form of triglycerides in the abdominal region, especially in the visceral region, promotes an unhealthy metabolic phenotype, energy storage in the form of triglycerides in subcutaneous adipose tissue of the buttocks and legs is considered beneficial for metabolic health32. So, the distribution of fat directly affects the metabolic status of the whole body. Compared to metabolic unhealthy obesity (MUO), patients with MHO have higher cardiorespiratory fitness and physical activity, higher insulin sensitivity, lower levels of inflammatory markers and normal adipose tissue function. Although the risk of combined cardiovascular disease is lower in MHO patients than that in MUO patients, it is still higher than that in metabolically healthy lean individuals21,33. Therefore, MHO may be a temporary phenotype of MUO, and with further lipid accumulation adipose tissue dysfunction occurs, eventually developing into MUO. Unhealthy fat distribution is a "breeding ground" for many diseases, including cardiovascular disease and cancer34,35,36,37. Because of this, it is not only important to pay attention to changes in the amount of total body fat, but also the distribution of fat.
In our study, we found that patients with VFA/SFA-High had significantly worse prognosis and shorter OS, so we believe that visceral fatty obesity is significantly associated with poor prognosis in patients with digestive system malignancies. Similarly, we also observed that patients with VFD-High had a worse prognosis, again suggesting that the accumulation of abdominal visceral fat promotes the development of cancer. Similarly, adipose distribution promotes the metastasis and further aggressive development of tumor cells to a certain extent, which is related to the fact that adipose accumulation promotes the production of chemokines and also serves as a sufficient energy source for tumor cell proliferation38. Adipose tissue can be described as an endocrine organ distributed throughout the body, but subcutaneous fat is mostly metabolically inactive, whereas visceral adipose tissue is more endocrinologically active. Excessive fat deposition increases adipokine release and leads to adipocyte hypoxia, allowing for increased cytokines and immune cell recruitment, which may lead to higher levels of systemic inflammation21,39. We hypothesize that the level of immune function in cancer patients differs significantly due to the distribution of adipose tissue, which in turn leads to individual differences in response to subsequent treatment and prognosis.
As can be seen from the above, not only skeletal muscle is important for cancer patients, but also fat distribution is an important indicator of prognosis. To better predict the survival of individual patients in clinical work, we combined the muscle and fat conditions of patients with cancer to construct a new BCS index in our study, based on which to reflect both muscle and fat. The time-dependent ROC curve showed that the predictive validity of BCS is stable around 0.70 during the whole follow-up period, which means that our new index BCS was of great predictive validity for patients with gastrointestinal malignancies and is expected to become a new tumor biomarker. We then constructed a prognostic prediction model called the scored-CT system, using the BCS, combined with tumor type, tumor stage, KPS score, and PG-SGA score, which has excellent predictive validity for both short-term survival prognosis and long-term 5-year survival in patients with digestive system malignancies. We did not include Alb in the scored-CT system because it would made clinical data more difficult to obtain, while the improvement in predictive power was not significant.
As determined by the current study, body composition affects the outcome of patients with malignant tumors in many ways, and the main theory is that skeletal muscle is the "buffer" of anti-tumor therapy. Skeletal muscle content is not only related to the toxicity after chemotherapy, but also may be related to the efficacy of chemotherapy, the response to targeted therapy and even the response to immunotherapy40,41. This reflects the interaction among nutrition, inflammation and immunity. Malnutrition is widespread in patients with malignant tumors, and about 25% to 80% of cancer patients have experienced varying degrees of malnutrition42,43. The incidence of malnutrition is significantly higher in patients with digestive system tumors because the tumor location often leads to more serious eating obstruction and dysfunction of nutrient absorption. From an objective perspective, malnutrition not only affects the choice of anti-tumor treatment, reduces response rates to treatment, increases subjective symptoms, and lowers the quality of life, but also increases the incidence of complications and mortality44,45. Therefore, it is necessary to adopt individualized nutritional therapy for cancer patients, which greatly improves clinical outcomes. For malnourished patients, physicians can improve PG-SGA scores through parenteral and enteral nutrition to anticipate a better clinical outcome. For patients with a high risk of death such as VFA/SFA-High and L3 SMI-Low, we can optimize fat distribution and improve skeletal muscle index by dose resistance training, reasonably controlling diet and moderate physical activity46,47,48,49, to control BCS at a lower level and achieve better survival. In short, our study achieved the extraction of the corresponding indicators from CT images, which successfully constructed a new biomarker, BCS, to effectively predict the survival time of patients with digestive system malignant tumors. On this basis, the scored-CT system successfully combined CT indicators, tumor disease status and nutritional status to intervene in the disease process from these three aspects to optimize clinical outcomes.
To some extent, our study comprehensively reflects the overall situation of cancer patients in China, as this is a real-world clinical study in an Asian population with OS, with prognosis as the observation endpoint. We believe that it has the appropriate guidance value for clinical application. Compared with previous studies, our BCS index and scored-CT system comprehensively reflected the interaction of muscle and fat, with corresponding advantages. The corresponding limitation of this study is that our study is a retrospective study, it is difficult to avoid the existence of partial data bias. Secondly, we lack the corresponding external validation data, which may lead to certain shortcomings of this prediction model. In addition, the prediction model in this research was constructed by patients with malignant tumors of the digestive system, which encompasses several tumor types. Due to the sample size limitation, it is difficult to build an accurate prediction model for each type. However, based on the continuous improvement of Investigation on Nutrition Status and its Clinical Outcome of Common Cancers (INSCOC) database construction, we also expect further external data validation in the subsequent research.
Conclusion
In summary, our study acknowledges the value of the role of muscle and adipose tissue in patients with digestive malignancies, and clarifies that CT-based body composition analysis can be used for prognostic prediction. In addition, the prognostic prediction model we constructed has good predictive value and was of good stability. This is a prediction model that both muscle and adipose tissue are used in the construction as proposed for Asian patients. We expect that this model will be applied in clinical practice to provide guidance for cancer patients.
Data availability
Materials described in the manuscript, including all relevant raw data, will be freely available to any scientist wishing to use them for non-commercial purposes, without breaching participant confidentiality. Any investigator interested in viewing raw data may contact us by email: zhengkaiwen1995@163.com.
References
Sung, H. et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 71(3), 209–249 (2021).
Song, M., Garrett, W. S. & Chan, A. T. Nutrients, foods, and colorectal cancer prevention. Gastroenterology 148(6), 1244–60 e16 (2015).
Anand, P. et al. Cancer is a preventable disease that requires major lifestyle changes. Pharm Res 25(9), 2097–2116 (2008).
Matrone, A. et al. Potential impact of BMI on the aggressiveness of presentation and clinical outcome of differentiated thyroid cancer. J. Clin. Endocrinol. Metab. 105(4), e1124–e1134 (2020).
Cantini, L. et al. Body mass index and hormone receptor status influence recurrence risk in HER2-positive early breast cancer patients. Clin. Breast Cancer 20(1), e89–e98 (2020).
Greenlee, H. et al. Association between body mass index and cancer survival in a pooled analysis of 22 clinical trials. Cancer Epidemiol. Biomark. Prev. 26(1), 21–29 (2017).
Cruz-Jentoft, A. J. et al. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 48(4), 601 (2019).
Kim, J. M. et al. Impact of subcutaneous and visceral fat adiposity in patients with colorectal cancer. Clin. Nutr. 40(11), 5631–5638 (2021).
Lee, J. S. et al. Subcutaneous fat distribution is a prognostic biomarker for men with castration resistant prostate cancer. J. Urol. 200(1), 114–120 (2018).
Wada, M. et al. Visceral-to-subcutaneous fat ratio is a possible prognostic factor for type 1 endometrial cancer. Int. J. Clin. Oncol. 27(2), 434–440 (2022).
Fischer, A. et al. Prevalence of low muscle mass in the computed tomography at the third lumbar vertebra level depends on chosen cut-off in 200 hospitalised patients: A prospective observational trial. Nutrients 14(16), 3446 (2022).
Bauer, J., Capra, S. & Ferguson, M. Use of the scored patient-generated subjective global assessment (PG-SGA) as a nutrition assessment tool in patients with cancer. Eur. J. Clin. Nutr. 56(8), 779–785 (2002).
Brundage, M. et al. Patterns of reporting health-related quality of life outcomes in randomized clinical trials: Implications for clinicians and quality of life researchers. Qual. Life Res. 20(5), 653–664 (2011).
Kang, Z. et al. Correlation between L3 skeletal muscle index and prognosis of patients with stage IV gastric cancer. J. Gastrointest. Oncol. 12(5), 2073–2081 (2021).
Kim, H. K. et al. Age-related changes in muscle quality and development of diagnostic cutoff points for myosteatosis in lumbar skeletal muscles measured by CT scan. Clin. Nutr. 40(6), 4022–4028 (2021).
Aubrey, J. et al. Measurement of skeletal muscle radiation attenuation and basis of its biological variation. Acta Physiol. (Oxf.) 210(3), 489–497 (2014).
Martin, L. et al. Assessment of computed tomography (CT)-defined muscle and adipose tissue features in relation to short-term outcomes after elective surgery for colorectal cancer: A multicenter approach. Ann. Surg. Oncol. 25(9), 2669–2680 (2018).
Camp, R. L., Dolled-Filhart, M. & Rimm, D. L. X-tile: A new bio-informatics tool for biomarker assessment and outcome-based cut-point optimization. Clin. Cancer Res. 10(21), 7252–7259 (2004).
Hagens, E. R. C. et al. Influence of body composition and muscle strength on outcomes after multimodal oesophageal cancer treatment. J. Cachexia Sarcopenia Muscle 11(3), 756–767 (2020).
Zhang, Y. et al. Impact of body composition on clinical outcomes in people with gastric cancer undergoing radical gastrectomy after neoadjuvant treatment. Nutrition 85, 111135 (2021).
Blüher, M. Metabolically healthy obesity. Endocr. Rev. 41(3), bnaa004 (2020).
Baracos, V. E. & Arribas, L. Sarcopenic obesity: Hidden muscle wasting and its impact for survival and complications of cancer therapy. Ann. Oncol. 29, ii1–ii9 (2018).
Looijaard, S. et al. Pathophysiological mechanisms explaining poor clinical outcome of older cancer patients with low skeletal muscle mass. Acta Physiol. (Oxf.) 231(1), e13516 (2021).
Bichels, A. V. et al. Muscle mass assessed by computed tomography at the third lumbar vertebra predicts patient survival in chronic kidney disease. J. Ren. Nutr. 31(4), 342–350 (2021).
Liu, X. et al. The correlation between skeletal muscle index of the L3 vertebral body and malnutrition in patients with advanced lung cancer. BMC Cancer 21(1), 1148 (2021).
Argiles, J. M. et al. Cancer cachexia: Understanding the molecular basis. Nat. Rev. Cancer 14(11), 754–762 (2014).
Wendrich, A. W. et al. Low skeletal muscle mass is a predictive factor for chemotherapy dose-limiting toxicity in patients with locally advanced head and neck cancer. Oral Oncol. 71, 26–33 (2017).
Zhuang, C. L. et al. Sarcopenia is an independent predictor of severe postoperative complications and long-term survival after radical gastrectomy for gastric cancer: Analysis from a large-scale cohort. Medicine (Baltimore) 95(13), e3164 (2016).
Chen, F. et al. Impact of preoperative sarcopenia on postoperative complications and prognosis of gastric cancer resection: A meta-analysis of cohort studies. Arch. Gerontol. Geriatr. 98, 104534 (2022).
Halvorsen, T. O. et al. Associations between muscle measures, survival, and toxicity in patients with limited stage small cell lung cancer. J. Cachexia Sarcopenia Muscle 11(5), 1283–1290 (2020).
Park, J. et al. Obesity and cancer–mechanisms underlying tumour progression and recurrence. Nat. Rev. Endocrinol. 10(8), 455–465 (2014).
Stefan, N. Causes, consequences, and treatment of metabolically unhealthy fat distribution. Lancet Diabetes Endocrinol. 8(7), 616–627 (2020).
Bluher, S. & Schwarz, P. Metabolically healthy obesity from childhood to adulthood: Does weight status alone matter?. Metabolism 63(9), 1084–1092 (2014).
Chen, G. C. et al. Association between regional body fat and cardiovascular disease risk among postmenopausal women with normal body mass index. Eur. Heart J. 40(34), 2849–2855 (2019).
Fukuda, T. et al. Sarcopenic obesity assessed using dual energy X-ray absorptiometry (DXA) can predict cardiovascular disease in patients with type 2 diabetes: A retrospective observational study. Cardiovasc. Diabetol. 17(1), 55 (2018).
Hyun, Y. Y. et al. Chronic kidney disease and high eGFR according to body composition phenotype in adults with normal BMI. Nutr. Metab. Cardiovasc. Dis. 26(12), 1088–1095 (2016).
Godziuk, K. et al. The impact of sarcopenic obesity on knee and hip osteoarthritis: A scoping review. BMC Musculoskelet. Disord. 19(1), 271 (2018).
Correa, L. H., Heyn, G. S. & Magalhaes, K. G. The impact of the adipose organ plasticity on inflammation and cancer progression. Cells 8(7), 662 (2019).
Booth, A. et al. Adipose tissue: An endocrine organ playing a role in metabolic regulation. Horm. Mol. Biol. Clin. Investig. 26(1), 25–42 (2016).
Baracos, V. E. & Arribas, L. Sarcopenic obesity: Hidden muscle wasting and its impact for survival and complications of cancer therapy. Ann. Oncol. 29(suppl_2), ii1–ii9 (2018).
Jung, G. H., Kim, J. H. & Chung, M. S. Changes in weight, body composition, and physical activity among patients with breast cancer under adjuvant chemotherapy. Eur. J. Oncol. Nurs. 44, 101680 (2020).
Cederholm, T. et al. GLIM criteria for the diagnosis of malnutrition: A consensus report from the global clinical nutrition community. Clin. Nutr. 38(1), 1–9 (2019).
D’Almeida, C. A. et al. Prevalence of malnutrition in older hospitalized cancer patients: A multicenter and multiregional study. J. Nutr. Health Aging 24(2), 166–171 (2020).
Brown, D. et al. Relationship between global leadership initiative on malnutrition (GLIM) defined malnutrition and survival, length of stay and post-operative complications in people with cancer: A systematic review. Clin. Nutr. 42(3), 255–268 (2023).
Wei, K. et al. Association of frailty and malnutrition with long-term functional and mortality outcomes among community-dwelling older adults: Results from the Singapore longitudinal aging study 1. JAMA Netw. Open 1(3), e180650 (2018).
Scott, J. M. et al. Exercise therapy and cardiovascular toxicity in cancer. Circulation 137(11), 1176–1191 (2018).
Fyfe, J. J., Hamilton, D. L. & Daly, R. M. Minimal-dose resistance training for improving muscle mass, strength, and function: A narrative review of current evidence and practical considerations. Sports Med. 52(3), 463–479 (2022).
Bland, K. A. et al. Exercise-based interventions to counteract skeletal muscle mass loss in people with cancer: Can we overcome the odds?. Sports Med. 52(5), 1009–1027 (2022).
Wedell-Neergaard, A. S. et al. Exercise-induced changes in visceral adipose tissue mass are regulated by IL-6 signaling: A randomized controlled trial. Cell Metab. 29(4), 844-855.e3 (2019).
Acknowledgements
This is a single-center retrospective study carried out by Cancer center, the First Hospital of Jilin University from Changchun, Jilin, China. We thank the patients and physicians who generously donated their time to participate, and radiologists and engineers from radiology department.
Funding
This work was supported by National Key R&D Program of China (2016YFC1303804).
Author information
Authors and Affiliations
Contributions
K.Z.: Conceptualization, Methodology, Formal analysis, Writing—Original Draft & Review & Editing; X.L.: Methodology, Formal analysis, Writing—Review & Editing; Y.L.: Software, Data Curation, Writing—Review & Editing; J.C.: Conceptualization, Writing—Review & Editing, Supervision; W.L.: Conceptualization, Writing—Review & Editing, Supervision.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zheng, K., Liu, X., Li, Y. et al. CT-based muscle and adipose measurements predict prognosis in patients with digestive system malignancy. Sci Rep 14, 13036 (2024). https://doi.org/10.1038/s41598-024-63806-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-63806-1
- Springer Nature Limited