Abstract
Background
Studies have shown that traditional nutrition indicators and body composition indicators are closely related to prognosis after radical gastric cancer (GC) surgery. However, the effect of the combined muscle and adipose composite on the prognosis of GC has not been reported.
Methods
The clinicopathological data of 514 patients with GC were retrospectively analyzed. The skeletal muscle adipose tissue were measured by preoperative CT images to obtain the muscle index and adipose index. X-tile software was used to determine the diagnostic threshold of muscle-adipose imbalance.
Results
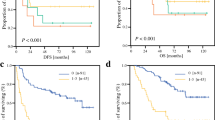
The 5-year OS and RFS of the muscle-adipose imbalanced group were significantly worse than those of the balanced group. Multivariate analysis showed that muscle-adipose imbalance and the CONUT score were independent prognostic factors of OS and RFS (p < 0.05). The nuclear density curve showed that the recurrence risk of the muscle-adipose imbalanced group was higher than that of the balanced group, whereas the nuclear density curve of the CONUT score was confounded. Incorporating the muscle-adipose index into cTNM has the same prognostic performance as the pTNM staging system. Chemotherapy-benefit analysis showed that stage II/III patients in the muscle-adipose balanced group could benefit from adjuvant chemotherapy.
Conclusions
The preoperative muscle-adipose index discovered for the first time is a new independent prognostic factor that affects the prognosis with GC. In addition, the preoperative muscle-adipose index is better than traditional nutrition and body composition indicators in terms of the prognostic evaluation of GC patients and the predictive value of recurrence risk.



Similar content being viewed by others
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424. https://doi.org/10.3322/caac.21492.
Borre M, Dam GA, Knudsen AW, Grønbaek H. Nutritional status and nutritional risk in patients with neuroendocrine tumors. Scand J Gastroenterol. 2018;53(3):284–92. https://doi.org/10.1080/00365521.2018.1430848.
Fujiya K, Kawamura T, Omae K, et al. Impact of malnutrition after gastrectomy for gastric cancer on long-term survival. Ann Surg Oncol. 2018;25(4):974–83. https://doi.org/10.1245/s10434-018-6342-8.
Galizia G, Lieto E, Auricchio A, et al. Naples prognostic score, based on nutritional and inflammatory status, is an independent predictor of long-term outcome in patients undergoing surgery for colorectal cancer. Dis Colon Rectum. 2017;60(12):1273–84. https://doi.org/10.1097/DCR.0000000000000961.
Kuroda D, Sawayama H, Kurashige J, et al. Controlling Nutritional Status (CONUT) score is a prognostic marker for gastric cancer patients after curative resection. Gastric Cancer Off J Int Gastric Cancer Assoc Japanese Gastric Cancer Assoc. 2018;21(2):204–12. https://doi.org/10.1007/s10120-017-0744-3.
Paccagnella A, Morassutti I, Rosti G. Nutritional intervention for improving treatment tolerance in cancer patients. Curr Opin Oncol. 2011;23(4):322–30. https://doi.org/10.1097/CCO.0b013e3283479c66.
Sakurai K, Ohira M, Tamura T, et al. Predictive potential of preoperative nutritional status in long-term outcome projections for patients with gastric cancer. Ann Surg Oncol. 2016;23(2):525–33. https://doi.org/10.1245/s10434-015-4814-7.
Zhao Y, Xu P, Kang H, et al. Prognostic nutritional index as a prognostic biomarker for survival in digestive system carcinomas. Oncotarget. 2016;7(52):86573–83. https://doi.org/10.18632/oncotarget.13472.
Park SH, Lee S, Song JH, et al. Prognostic significance of body mass index and prognostic nutritional index in stage II/III gastric cancer. Eur J Surg Oncol. 2020;46(4 Pt A):620–5. https://doi.org/10.1016/j.ejso.2019.10.024.
Kuroda D, Sawayama H, Kurashige J, Iwatsuki M. Controlling Nutritional Status ( CONUT ) score is a prognostic marker for gastric cancer patients after curative resection. Gastric Cancer. 2017. https://doi.org/10.1007/s10120-017-0744-3.
Zhuang C-L, Huang D-D, Pang W-Y, et al. Sarcopenia is an independent predictor of severe postoperative complications and long-term survival after radical gastrectomy for gastric cancer: analysis from a large-scale cohort. Medicine (Baltimore). 2016;95(13):e3164.
Zheng Z-F, Lu J, Zheng C-H, et al. A novel prognostic scoring system based on preoperative sarcopenia predicts the long-term outcome for patients after r0 resection for gastric cancer: experiences of a high-volume center. Ann Surg Oncol. 2017;24(7):1795–803.
Voron T, Tselikas L, Pietrasz D, et al. Sarcopenia impacts on short- and long-term results of hepatectomy for hepatocellular carcinoma. Ann Surg. 2015;261(6):1173–83.
Malietzis G, Currie AC, Athanasiou T, et al. Influence of body composition profile on outcomes following colorectal cancer surgery. Br J Surg. 2016;103(5):572–80.
Miyamoto Y, Baba Y, Sakamoto Y, et al. Sarcopenia is a negative prognostic factor after curative resection of colorectal cancer. Ann Surg Oncol. 2015;22(8):2663–8.
Amini N, Spolverato G, Gupta R, et al. Impact total psoas volume on short- and long-term outcomes in patients undergoing curative resection for pancreatic adenocarcinoma: a new tool to assess sarcopenia. J Gastrointest Surg. 2015;19(9):1593–602.
Tan BHL, Birdsell LA, Martin L, Baracos VE, Fearon KCH. Sarcopenia in an overweight or obese patient is an adverse prognostic factor in pancreatic cancer. Clin Cancer Res. 2009;15(22):6973–9.
Ting X, Lei L, Ying T, Yan C, Li L. Visceral and subcutaneous fat as new independent predictive factors of survival in locally advanced gastric carcinoma patients treated with neoadjuvant chemotherapy. J Cancer Res Clin Oncol. 2014. https://doi.org/10.1007/s00432-014-1893-y.
Kim JH, Chin HM, Hwang SS, Jun KH. Impact of intra-abdominal fat on surgical outcome and overall survival of patients with gastric cancer. Int J Surg. 2014;12(4):346–52. https://doi.org/10.1016/j.ijsu.2014.01.010.
Agents A. Oncologist. Published online 2011:71–81. https://doi.org/10.1634/theoncologist.2010-0227
Cruz-Jentoft AJ, Baeyens JP, Bauer JM, et al. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing. 2010;39(4):412–23.
Fielding RA, Vellas B, Evans WJ, et al. Sarcopenia: an undiagnosed condition in older adults. Current consensus definition: prevalence, etiology, and consequences. International working group on sarcopenia. J Am Med Dir Assoc. 2011;12(4):249–56.
Tegels JJW, van Vugt JLA, Reisinger KW, et al. Sarcopenia is highly prevalent in patients undergoing surgery for gastric cancer but not associated with worse outcomes. J Surg Oncol. 2015;112(4):403–7.
Ma SWL, Zhou XCD, Li B, Zhen DH, Zhuang XSC. Impact of visceral fat on surgical complications and long-term survival of patients with gastric cancer after radical gastrectomy. Eur J Clin Nutr. 2017. https://doi.org/10.1038/s41430-017-0032-7.
Park HS, Kim HS, Beom SH, Rha SY. Marked loss of muscle, visceral fat, or subcutaneous fat after gastrectomy predicts poor survival in advanced gastric cancer: single-center study from the CLASSIC Trial. Ann Surg Oncol. 2018;25(11):3222–30. https://doi.org/10.1245/s10434-018-6624-1.
Harada K, Baba Y, Ishimoto T, Kosumi K. Low visceral fat content is associated with poor prognosis in a database of 507 upper gastrointestinal cancers. Ann Surg Oncol. 2015;22:3946–53. https://doi.org/10.1245/s10434-015-4432-4.
Guiu B, Petit JM, Bonnetain F, et al. Visceral fat area is an independent predictive biomarker of outcome after first-line bevacizumab- based treatment in metastatic colorectal cancer. Gut. 2010. https://doi.org/10.1136/gut.2009.188946.
Balentine CJ, Enriquez J, Fisher W, Hodges S, Bansal V, Berger DH. Intra-abdominal fat predicts survival in pancreatic cancer. J Gastrointest Surg. 2010. https://doi.org/10.1007/s11605-010-1297-5.
Moon H, Ju Y, Jeong C, et al. Visceral obesity may affect oncologic outcome in patients with colorectal cancer. Ann Surg Oncol. 2008;15(7):1918–22. https://doi.org/10.1245/s10434-008-9891-4.
Wang S-L, Ma L-L, Chen X-Y, et al. Impact of visceral fat on surgical complications and long-term survival of patients with gastric cancer after radical gastrectomy. Eur J Clin Nutr. 2018;72(3):436–45. https://doi.org/10.1038/s41430-017-0032-7.
Onodera T, Goseki N, Kosaki G. Prognostic nutritional index in gastrointestinal surgery of malnourished cancer patients. Nihon Geka Gakkai Zasshi. 1984;85(9):1001–5.
Jiang N, Deng J-Y, Ding X-W, et al. Prognostic nutritional index predicts postoperative complications and long-term outcomes of gastric cancer. World J Gastroenterol. 2014;20(30):10537–44. https://doi.org/10.3748/wjg.v20.i30.10537.
Pecorelli N, Carrara G, de Cobelli F, et al. Effect of sarcopenia and visceral obesity on mortality and pancreatic fistula following pancreatic cancer surgery. Br J Surg. 2016. https://doi.org/10.1002/bjs.10063.
Wang J-B, Xue Z, Lu J, et al. Effect of sarcopenia on short- and long-term outcomes in patients with gastric neuroendocrine neoplasms after radical gastrectomy: results from a large, two-institution series. BMC Cancer. 2020;20(1):1002. https://doi.org/10.1186/s12885-020-07506-9.
Okugawa Y, Toiyama Y, Yamamoto A, et al. Lymphocyte-C-reactive protein ratio as promising new marker for predicting surgical and oncological outcomes in colorectal cancer. Ann Surg. 2020;272(2):342–51. https://doi.org/10.1097/SLA.0000000000003239.
Hacker UT, Hasenclever D, Linder N, et al. Prognostic role of body composition parameters in gastric/gastroesophageal junction cancer patients from the EXPAND trial. J Cachexia Sarcopenia Muscle. 2019. https://doi.org/10.1002/jcsm.12484.
Caan BJ, Meyerhardt JA, Kroenke CH, et al. Explaining the obesity paradox: the association between body composition and colorectal cancer survival ( C-SCANS Study ). Cancer Epidemiol Prevent Biomark. 2017. https://doi.org/10.1158/1055-9965.EPI-17-0200.
Schueneman AJ, Sugar EA, Uram J, et al. Low total lymphocyte count is associated with poor survival in patients with resected pancreatic adenocarcinoma receiving a GM-CSF secreting pancreatic tumor vaccine. Ann Surg Oncol. 2013;20(Suppl 3):S725–30. https://doi.org/10.1245/s10434-013-3262-5.
Shimada H, Takiguchi N, Kainuma O, et al. High preoperative neutrophil-lymphocyte ratio predicts poor survival in patients with gastric cancer. Gastric Cancer. 2010;13(3):170–6. https://doi.org/10.1007/s10120-010-0554-3.
Kang R, Li P, Wang T, et al. Apolipoprotein E epsilon 2 allele and low serum cholesterol as risk factors for gastric cancer in a Chinese Han population. Sci Rep. 2016;6:19930. https://doi.org/10.1038/srep19930.
Suzuki Y, Okabayashi K, Hasegawa H, et al. Comparison of preoperative inflammation-based prognostic scores in patients with colorectal cancer. Ann Surg. 2018;267(3):527–31. https://doi.org/10.1097/SLA.0000000000002115.
Chan JCY, Chan DL, Diakos CI, et al. The lymphocyte-to-monocyte ratio is a superior predictor of overall survival in comparison to established biomarkers of resectable colorectal cancer. Ann Surg. 2017;265(3):539–46. https://doi.org/10.1097/SLA.0000000000001743.
Lien Y-C, Hsieh C-C, Wu Y-C, et al. Preoperative serum albumin level is a prognostic indicator for adenocarcinoma of the gastric cardia. J Gastrointest Surg Off J Soc Surg Aliment Tract. 2004;8(8):1041–8. https://doi.org/10.1016/j.gassur.2004.09.033.
de Ulíbarri Pérez JI, Fernández G, Rodríguez Salvanés F, Díaz López AM. Nutritional screening; control of clinical undernutrition with analytical parameters. Nutr Hosp. 2014;29(4):797–811. https://doi.org/10.3305/nh.2014.29.4.7275.
Cengiz O, Kocer B, Sürmeli S, Santicky M-J, Soran A. Are pretreatment serum albumin and cholesterol levels prognostic tools in patients with colorectal carcinoma? Med Sci Monit Int Med J Exp Clin Res. 2006;12(6):CR240–7.
Dello SAWG, Lodewick TM, van Dam RM, et al. Sarcopenia negatively affects preoperative total functional liver volume in patients undergoing liver resection. HPB (Oxford). 2013;15(3):165–9.
Dindo D, Demartines N, Clavien P-A. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–13.
Ryo S, Kanda M, Ito S, et al. The controlling nutritional status score serves as a predictor of short- and long-term outcomes for patients with stage 2 or 3 gastric cancer: analysis of a multi-institutional data set. Ann Surg Oncol. 2019;26(2):456–64. https://doi.org/10.1245/s10434-018-07121-w.
Mir O, Coriat R, Boudou-Rouquette P, et al. Gemcitabine and oxaliplatin as second-line treatment in patients with hepatocellular carcinoma pre-treated with sorafenib. Med Oncol. 2012;29(4):2793–9. https://doi.org/10.1007/s12032-012-0208-x.
Huillard O, Mir O, Peyromaure M, et al. Sarcopenia and body mass index predict sunitinib-induced early dose-limiting toxicities in renal cancer patients. Br J Cancer. 2013;108(5):1034–41. https://doi.org/10.1038/bjc.2013.58.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Disclosures
All of the authors declare that they have no potential commercial conflicts of interest relevant to this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lu, J., Xue, Z., Xie, Jg. et al. Preoperative Muscle-Adipose Index: A New Prognostic Factor for Gastric Cancer. Ann Surg Oncol 29, 4595–4607 (2022). https://doi.org/10.1245/s10434-022-11509-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-022-11509-0