Abstract
We tested whether alanine aminotransferase/aspartate aminotransferase (ALT/AST), a marker of hepatosteatosis, associates with insulin resistance, β-cell function and postglucose glycemia. We studied 311 young and 148 middle-aged Japanese women, whose BMI averaged < 23.0 kg/m2. Insulinogenic index and Matsuda index were evaluated in 110 young and 65 middle-aged women. In two groups of women, ALT/AST was associated positively with homeostasis model assessment insulin resistance (HOMA-IR) and inversely with Matsuda index. In middle-aged women only, the ratio was also associated positively with fasting and postload glycemia and HbA1c. The ratio showed negative association with disposition index (a product of insulinogenic index and Matsuda index). On multivariate linear regression analysis, HOMA-IR emerged as a single determinant of ALT/AST in young and middle-aged women (standardized β: 0.209, p = 0.003 and 0.372, p = 0.002, respectively). ALT/AST was associated with insulin resistance and β-cell function even in non-obese Japanese women, suggesting a pathophysiologic basis in its prediction of diabetic risk.
Similar content being viewed by others
Introduction
Epidemiologic studies1,2,3,4 have shown that modest elevations of serum liver enzymes, such as alanine aminotransferase (ALT) and aspartate aminotransferase (AST), are associated with an increased risk of subsequently developing type 2 diabetes, which are characterized by insulin resistance and impaired β-cell function. The aminotransferases, particularly ALT, are markers of nonalcoholic fatty liver disease (NAFLD), which are also characterized by insulin resistance5,6. ALT/AST can be used to evaluate the degree of hepatic fat infiltration and hepatic steatosis7,8,9,10,11. For example, in a Framingham study, it was shown that ALT/AST could identify hepatic steatosis more accurately than using ALT or AST alone9. A recent population-based longitudinal study has revealed that the increase in the ALT/AST ratio was closely associated with the risk of new-onset NAFLD in nonobese Chinese individuals12.
Although insulin resistance and impaired β-cell function are hallmarks of type 2 diabetes, studies confirm more severe functional insulin secretory defects in lean individuals compared to the obese phenotype in some Asian countries13. We14 demonstrated that middle-aged Japanese people with prediabetes had reduced glucose-induced insulin secretion and higher circulating orosomucoid, an acute-phase glycoprotein produced mainly in the liver15, in the absence of insulin resistance. However, studies which assessed β-cell function and postglucose glycemia in relation to serum concentrations of liver enzymes are limited as discussed later. We, therefore, investigated whether ALT/AST may be associated with β-cell function and postglucose glycemia in addition to insulin resistance. As described in detail in “Methods”, glucose-induced insulin secretion was evaluated by insulinogenic index (IGI), insulin resistance-corrected insulin secretion (β-cell function) by the oral disposition index (ODI) and insulin resistance/sensitivity by homeostasis model assessment (HOMA-IR) and Matsuda index. These analyses were done in young and middle-aged Japanese women, populations in which confounding factors are so scarce16,17,18. Because liver fat accumulation has been reported to be associated with increased serum orosomucoid in addition to branched chain and aromatic amino acids19, and because orosomucoid and C-reactive protein (CRP) were associated with an increased risk of both type 2 diabetes and cardiovascular disease20, we also studied whether ALT/AST may be associated with serum orosomucoid. Lastly, we examined whether ALT/AST may be associated these variables stronger than ALT alone.
Methods
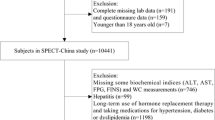
We examined 311 young and 148 middle-aged women as previously reported16,17,18. Among 148 middle-aged women, 137 (92.6%) reported to have regular menstrual cycles (premenopausal). The present study was done between 2004 and 2007 and these women participated as volunteers as previously reported in detail16. Young women were female Japanese students of Department of Food Sciences and Nutrition, Mukogawa Women's University and middle-aged women were their biological mothers of 148 students who participated in the study. Subjects were excluded from the study when they reported to have clinically diagnosed acute or chronic inflammatory diseases, endocrine, cardiovascular, hepatic, renal diseases, hormonal contraception, unusual dietary habits. This research followed the tenets of the Declaration of Helsinki. All participants gave written informed consent after the experimental procedure had been explained.
Blood samples were obtained in the morning after 12-h overnight fast. Oral glucose tolerance test (OGTT) was performed with 75-g glucose administration in 118 female students and 65 mothers. Blood samples were taken at min 0 (fasting), 30, 60 and 120 for glucose and insulin analysis. Plasma glucose was determined by the hexokinase/glucose-6-phosphate dehydrogenase method [interassay coefficient of variation (CV) < 2%]. Serum insulin was measured by an ELISA method with a narrow specificity excluding des-31, des-32, and intact proinsulin (interassay CV < 6%). Insulin resistance/sensitivity was determined by HOMA-IR using fasting plasma glucose and insulin levels21 and Matsuda index using glucose and insulin levels during OGTT22. IGI was calculated as incremental insulin concentrations (μU/mL) divided by incremental glucose concentrations (mg/dL) during the first 30 min of OGTT23. ODI was calculated as the product of IGI and Matsuda index. Area under the glucose and insulin concentration curve during OGTT (AUCg and AUCi, respectively) was calculated using trapezoidal method. Prediabetes and diabetes were diagnosed based on glycemia criteria (fasting and 2-h glucose concentrations) of the American Diabetes Association24.
Serum liver enzymes were measured using an autoanalyzer (AU5232, Olympus, Tokyo, Japan). Highly-sensitivity C-reactive protein (hsCRP) concentrations were measured by an immunoturbidimetric assay with the use of reagents and calibrators from Dade Behring Marburg GmbH (Marburg, Germany, with an interassay CV less than 5%). Orosomucoid concentrations were measured by an immunoturbidimetric method using a commercially available kit (N Antiserum to Human α1-acid Glycoprotein, Siemens Healthcare Diagnostics, Tokyo, Japan) and an autoanalyzer (JCA-BM6010, JEOL, Tokyo, Japan). Intra-assay and interassay CV at 87 mg/dL was 1.4% and 1.7%, respectively.
Body weight, height and waist circumference were measured after an overnight fast with a light cloth and shoes off and BMI was calculated. Weight and height were measured to the nearest 0.1 kg and 0.1 cm, respectively. Whole-body dual-energy X-ray absorptiometry (DXA) (Hologic QDR-2000, software version 7.20D, Waltham, MA) was used to measure lean tissue mass, fat mass, and bone mineral mass for arms, lower-body, trunk and the total body17.
Statistical analysis
Data were presented as mean ± SD unless otherwise stated. Due to deviation from normal distribution, ALT, IGI, ODI and hsCRP were logarithmically transformed for analyses. Bivariate correlations of ALT/AST with anthropometric and metabolic parameters were evaluated by Pearson’s correlation analysis. Stepwise multivariate linear regression analyses were performed to further identify the most significant variables contributing to the variation of ALT/AST. Comparisons between two groups were made with two-sample t-test. Differences among three groups were analyzed using analysis of variance and then Bonferroni's multiple comparison procedure. A two-tailed p < 0.05 was considered statistically significant. All calculations were performed with SPSS system 23 (SPSS Inc, Chicago, IL).
Results
On average, middle-aged mothers and their daughters were nonobese rather slim and had normal mean serum ALT and AST (Table 1). Middle-aged mothers compared with their daughters had higher BMI, percentage body fat, waist circumference and trunk fat and hence higher HbA1c, serum ALT, AST and ALT/AST. However, their BMI, waist and ALT averaged 22 kg/m2, 79 cm and 20 U/L, respectively.
OGTT revealed that prediabetes was found in 7 of 118 young women25 and 11 of 65 middle-aged women14 whereas none had diabetes. Middle-aged women had lower ODI and hence higher glycemia at four time points (Table 1). Matsuda index and HOMA-IR did not differ between two groups.
In young women, there was no significant association of log ALT with variables depicted in Table 1 (data not shown), including fasting insulin (r = 0.08, p = 0.15), HOMA-IR (r = 0.104, p = 0.06) and log HOMA-IR (r = 0.101, p = 0.07). In contrast, ALT/AST showed positive associations with fasting insulin, HOMA-IR and, AUCi and inversely with Matsuda index (Table 2). However, it showed no associations with percentage body fat, percentage trunk fat, and all glycemic variables studied although there was a weak association with BMI.
In middle-aged women, associations of ALT/AST were stronger than those of log ALT (Table 2). ALT/AST was positively associated with BMI, waist, percentage body and trunk fat. The ratio showed positive associations with all glycemic variables studied (glycemia at four time points, AUCg and HbA1c). In addition, the ratio showed significant associations with all markers of insulin resistance/insulin sensitivity studied (fasting and 2-h insulin, AUCi, HOMA-IR, and Matsuda index) (Fig. 1). Further, ALT/AST showed negative association with log ODI although it was not associated with IGI. Associations of ALT/AST with orosomucoid and log hsCRP were significant and tended to be significant, respectively, in middle-aged women.
We have done multivariate analysis for ALT/AST as a dependent variable. The model included HOMA-IR, Matsuda index, log ODI and AUCg as independent variables in young and middle-aged women. HOMA-IR emerged as a single determinant of ALT/AST in both young and middle-aged women (standardized β: 0.209, p = 0.003 and 0.372, p = 0.002, respectively). Including orosomucoid as an additional independent variable did not change the results in middle-aged women.
Young and middle-aged Japanese women were grouped according to tertile of ALT/AST. HOMA-IR increased in two groups of women and log ODI decreased in middle-aged women in a stepwise fashion from the low through median to high tertile (Fig. 2). Matsuda index was lower in the high compared to low and median tertile in middle-aged women. In young women, differences in Masuda index and log ODI were not significant after Bonferroni’s multiple comparison procedure because associations were weak (Table 2).
Homeostasis model assessment-insulin resistance (HOMA-IR), log oral disposition index (ODI) and Matsuda index in young (circles) and middle-aged Japanese women (squares) grouped according to tertile of alanine aminotransferase/aspartate aminotransferase (ALT/AST). Mean ± SD. Means not sharing common letter are significantly different with each other at p < 0.05 or less by Bonferroni’s multiple comparison procedure. Blue, yellow and red symbols represent the low, median and high tertile, respectively. P values: HOMA-IR: young: p = 0.04, middle-aged: p < 0.001 vs. low, p = 0.003 vs. median, log ODI: p = 0.01, Matsuda index: p = 0.004 vs. low, p = 0.003 vs. median.
Discussion
The current study confirmed stronger associations of ALT/AST than those of log ALT and demonstrated an association of ALT/AST, a marker of hepatosteatosis7,8,9,10,11,12, with insulin resistance (higher HOMA-IR) in women in early adult life in addition to midlife. In addition, it was also associated with not only fasting and postglucose glycemia and HbA1c but also serum orosomucoid, a risk factor for type 2 diabetes20, in middle-aged women. Further, the ratio was associated with impaired β-cell function (lower ODI) and hence slower glucose disposal rate during OGTT (higher AUCg).
There is a strong relationship between fat accumulation in the liver and whole-body insulin resistance independent of visceral adiposity, a major regulator of both liver fat and insulin resistance26. An association of ALT/AST, a marker of hepatosteatosis7,8,9,10,11,12, with HOMA-IR, a robust tool for the assessment of insulin resistance, has been demonstrated in studies from Japan27, China28 and Korea29. The present study confirmed this association in middle-aged Japanese women and extended that this association was evident even in Japanese women in early adult life whose waist and ALT averaged 71 cm and 13 U/L, respectively, suggesting minimum abdominal and hepatic lipid accumulation, respectively.
Studies which assessed β-cell function and postglucose glycemia in relation to serum concentrations of liver enzymes are limited. We found a single study which studied associations with β-cell function. Pinnaduwage et al.30 evaluated the association of changes in liver enzymes with changes in insulin sensitivity, β-cell function and glycemia in 336 women with varying degrees of previous gestational glucose metabolic status at 1 and 3 years postpartum. They found that an increase in ALT/AST predicted lower β-cell function, worsening insulin sensitivity and higher fasting glucose at 3 years. In the present study, higher ALT/AST in middle-aged Japanese women was associated with higher insulin resistance and impaired β-cell function (lower ODI) and hence slower glucose disposal rate during OGTT (higher AUCg).
Song et al.31 studied 1128 pregnant women who underwent serum liver enzyme measurements and 75 g OGTT and assessed the relationship of liver enzymes and glycemia during OGTT. They found associations of ALT/AST with fasting and postglucose glycemia in a total of 1128 pregnant women, which were found in 65 middle-aged Japanese women in the present study. They also found that higher ALT/AST as well as triglyceride/high-density lipoprotein cholesterol, a lipid marker of insulin resistance32, was an independent risk factor of gestational diabetes.
An association of ALT/AST with HbA1c in the present study may be related to observations that the severity grades of steatosis evaluated by transient elastography or abdominal ultrasound correlated with HbA1C levels33,34. An association with orosomucoid in the present study may be related to a study19 which showed that already in its early stage liver fat accumulation was associated with increased serum orosomucoid and branched-chain amino, which may be associated with adipose tissue dysfunction. Hepatic orosomucoid expression has recently found to correlate with NAFLD parameters in obese mice with NAFLD induced by high-fat Western diet together with liquid sugar (fructose and sucrose) feeding35.
Associations were stronger in middle aged women than in young women. This may be related to the observation that associations among biomarkers of metabolic syndrome are stronger in obese women than in lean women36, as middle-aged women had greater percentage body fat, waist circumference and trunk fat than did younger women although middle-aged women were not obese.
The strength of this study includes homogeneous study population with scarce confounding factors17,18. Several limitations of this study include the cross-sectional design, relatively small sample size, and a single measurement of biochemical variables. We used many surrogates in the present study, which may be less accurate. Finally, as we studied Japanese women only, results may not be generalized to other sex, races or ethnicities.
In conclusions, ALT/AST, a marker of hepatosteatosis, was associated with insulin resistance, β-cell function and glucose disposal rate even in non-obese Japanese women, suggesting a pathophysiologic basis in its prediction of diabetic risk.
Data availability
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
References
Vozarova, B. et al. High alanine aminotransferase is associated with decreased hepatic insulin sensitivity and predicts the development of type 2 diabetes. Diabetes 51, 1889–1895 (2002).
Doi, Y. et al. Liver enzymes as a predictor for incident diabetes in a Japanese population: The Hisayama study. Obesity 15, 1841–1850 (2007).
Sato, K. K. et al. Liver enzymes compared with alcohol consumption in predicting the risk of type 2 diabetes: The Kansai Healthcare Study. Diabetes Care 31, 1230–1236 (2008).
Kunutsor, S. K., Apekey, T. A. & Walley, J. Liver aminotransferases and risk of incident type 2 diabetes: A systematic review and meta-analysis. Am. J. Epidemiol. 178, 159–171 (2013).
Gastaldelli, A. & Cusi, K. From NASH to diabetes and from diabetes to NASH: Mechanisms and treatment options. JHEP Rep. 1, 312–328 (2019).
Khan, R. S., Bril, F., Cusi, K. & Newsome, P. N. Modulation of insulin resistance in nonalcoholic fatty liver disease. Hepatology 70, 711–724 (2019).
Fuyan, S. et al. Fatty liver disease index: A simple screening tool to facilitate diagnosis of nonalcoholic fatty liver disease in the Chinese population. Dig. Dis. Sci. 58, 3326–3334 (2013).
Lee, J. H. et al. Hepatic steatosis index: A simple screening tool reflecting nonalcoholic fatty liver disease. Dig. Liver Dis. 42, 503–508 (2010).
Long, M. T. et al. Development and validation of the Framingham steatosis index to identify persons with hepatic steatosis. Clin. Gastroenterol. Hepatol. 14, 1172-1180.e2 (2016).
Lu, C. W. et al. Aminotransferase ratio is a useful index for hepatosteatosis in children and adolescents: A cross-sectional observational study. Gastroenterol. Nurs. 42, 486–495 (2019).
Lin, M. S. et al. Serum aminotransferase ratio is independently correlated with hepatosteatosis in patients with HCV: A cross-sectional observational study. BMJ Open 5, e008797. https://doi.org/10.1136/bmjopen-2015-008797 (2015).
Zou, Y., Zhong, L., Hu, C. & Sheng, G. Association between the alanine aminotransferase/aspartate aminotransferase ratio and new-onset non-alcoholic fatty liver disease in a nonobese Chinese population: A population-based longitudinal study. Lipids Health Dis. 19, 245. https://doi.org/10.1186/s12944-020-01419-z (2020).
Olaogun, I., Farag, M. & Hamid, P. The pathophysiology of type 2 diabetes mellitus in non-obese individuals: An overview of the current understanding. Cureus. 12, e7614. https://doi.org/10.7759/cureus.7614 (2020).
Tsuboi, A. et al. Higher circulating orosomucoid, an acute-phase protein, and reduced glucose-induced insulin secretion in middle-aged Japanese people with prediabetes. BMJ Open Diabetes Res. Care. 8, e001392. https://doi.org/10.1136/bmjdrc-2020-001392 (2020).
Luo, Z. et al. Orosomucoid, an acute response protein with multiple modulating activities. J. Physiol. Biochem. 71, 329–340 (2015).
Takeuchi, M. et al. Weight trajectory since birth, current body composition, dietary intake, and glucose tolerance in young underweight Japanese women. Womens Health Rep. 3, 215–221 (2022).
Tanaka, S. et al. Associations of lower-body fat mass with favorable profile of lipoproteins and adipokines in healthy, slim women in early adulthood. J. Atheroscler. Thromb. 18, 365–372 (2011).
Tanaka, M. et al. FTO, abdominal adiposity, fasting hyperglycemia associated with elevated HbA1c in Japanese middle-aged women. J. Atheroscler. Thromb. 19, 633–642 (2012).
Cheng, S. et al. Adipose tissue dysfunction and altered systemic amino acid metabolism are associated with non-alcoholic fatty liver disease. PLoS ONE 10, e0138889. https://doi.org/10.1371/journal.pone.0138889 (2015).
Bao, X. et al. Comparing the inflammatory profiles for incidence of diabetes mellitus and cardiovascular diseases: A prospective study exploring the “common soil” hypothesis. Cardiovasc. Diabetol. 17, 87. https://doi.org/10.1186/s12933-018-0733-9 (2018).
Matthews, D. R. et al. Homeostasis model assessment: Insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28, 412–419 (1985).
Matsuda, M. & DeFronzo, R. A. Insulin sensitivity indices obtained from oral glucose tolerance testing: Comparison with the euglycemic insulin clamp. Diabetes Care 22, 1462–1470 (1999).
Stumvoll, M. et al. Use of the oral glucose tolerance test to assess insulin release and insulin sensitivity. Diabetes Care 23, 295–301 (2000).
American Diabetes Association 2. Classification and diagnosis of diabetes: Standards of medical care in diabetes-2018. Diabetes Care 41, S1327 (2018).
Tsuboi, A. et al. Association of serum orosomucoid with 30-min plasma glucose and glucose excursion during oral glucose tolerance tests in non-obese young Japanese women. BMJ Open Diabetes Res. Care. 6, e000508. https://doi.org/10.1136/bmjdrc-2018-000508 (2018).
Stefan, N., Kantartzis, K. & Häring, H. U. Causes and metabolic consequences of fatty liver. Endocr. Rev. 29, 939–960 (2008).
Kawamoto, R. et al. Alanine aminotransferase/aspartate aminotransferase ratio is the best surrogate marker for insulin resistance in non-obese Japanese adults. Cardiovasc. Diabetol. 11, 117. https://doi.org/10.1186/1475-2840-11-117 (2012).
Zhao, L. et al. Serum alanine aminotransferase/aspartate aminotransferase ratio is one of the best markers of insulin resistance in the Chinese population. Nutr. Metab. 14, 64. https://doi.org/10.1186/s12986-017-0219-x (2017).
Kwon, S. S. & Lee, S. G. A high alanine aminotransferase/aspartate aminotransferase ratio determines insulin resistance and metabolically healthy/unhealthy obesity in a general adult population in Korea: The Korean National Health and Nutritional Examination Survey 2007–2010. Exp. Clin. Endocrinol. Diabetes. 127, 677–684 (2019).
Pinnaduwage, L. et al. Changes over time in hepatic markers predict changes in insulin sensitivity, β-cell function, and glycemia. J. Clin. Endocrinol. Metab. 103, 2651–2659 (2018).
Song, S. et al. ALT/AST as an independent risk factor of gestational diabetes mellitus compared with TG/HDL-C. Int. J. Gen. Med. 15, 115–121 (2022).
Gasevic, D., Frohlich, J., Mancini, G. B. & Lear, S. A. The association between triglyceride to high-density-lipoprotein cholesterol ratio and insulin resistance in a multiethnic primary prevention cohort. Metabolism 61, 583–589 (2012).
Masroor, M. & Haque, Z. HbA1C as a biomarker of non-alcoholic fatty liver disease: Comparison with anthropometric parameters. J. Clin. Transl. Hepatol. 9, 15–21 (2021).
Xie, Y., Kong, W., Wang, X. & Wu, Z. Association of glycated hemoglobin with non-alcoholic fatty liver disease patients and the severity of liver steatosis and fibrosis measured by transient elastography in adults without diabetes. BMC Endocr. Disord. 22, 220. https://doi.org/10.1186/s12902-022-01134-z (2022).
Luo, Y. et al. Role of liquid fructose/sucrose in regulating the hepatic transcriptome in a high-fat Western diet model of NAFLD. J. Nutr. Biochem. 112, 109174. https://doi.org/10.1016/j.jnutbio.2022.109174 (2023).
Abdullah, A. R., Hasan, H. A. & Raigangar, V. L. Analysis of the relationship of leptin, high-sensitivity C-reactive protein, adiponectin, insulin, and uric acid to metabolic syndrome in lean, overweight, and obese young females. Metab. Syndr. Relat. Disord. 7, 17–22 (2009).
Acknowledgements
We thank all participants for their dedicated and conscientious collaboration.
Funding
The study was approved by the Ethics Committees of the Mukogawa Women’s University (No. 07-28 on 19/02/2008).
Author information
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Minato-Inokawa, S., Tsuboi-Kaji, A., Honda, M. et al. Associations of alanine aminotransferase/aspartate aminotransferase with insulin resistance and β-cell function in women. Sci Rep 13, 7853 (2023). https://doi.org/10.1038/s41598-023-35001-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-35001-1
- Springer Nature Limited
This article is cited by
-
Elucidating the role of liver enzymes as markers and regulators in ovarian cancer: a synergistic approach using Mendelian randomization, single-cell analysis, and clinical evidence
Human Genomics (2024)
-
Associations of ALT/AST, a marker of hepatosteatosis, with pulse rate in young women and with blood pressure in middle-aged women independently of abdominal fat accumulation and insulin resistance
Diabetology International (2024)
-
The ratio of high aspartate aminotransferase to alanine aminotransferase: an independent risk factor associated with poor prognosis in IgA nephropathy
Clinical and Experimental Nephrology (2024)