Abstract
Despite remarkable progress in the reduction of under-five mortality; perinatal mortality is the major public health problem in Africa. In Ethiopia, the study findings on perinatal mortality and its predictors were inconsistent. Therefore, this systematic review and meta-analysis estimated the pooled perinatal mortality, and its association with antenatal care visit, maternal tetanus toxoid immunization, and partograph monitoring. International databases like PubMed, SCOPUS, Google Scholar and Science Direct were systematically searched. I squared statistics was used to determine the levels of heterogeneity across studies and the pooled estimate was computed using a random-effect model. The meta-analysis showed that a pooled prevalence of perinatal mortality in Ethiopia was 6.00% (95% CI 5.00%, 7.00%). The highest proportion of perinatal mortality was a stillbirth, 5.00% (95% CI 4.00%, 7.00%). Women who had antenatal care visit [OR = 0.20 (95% CI 0.12, 0.34)], maternal tetanus toxoid immunization [OR = 0.43 (95% CI 0.24, 0.77)] and partograph monitoring [POR = 0.22 (95% CI 0.06, 0.76)] reduced the risk of perinatal mortality. Whereas, previous history of perinatal mortality [POR = 7.95 (95% CI 5.59, 11.30)] and abortion history (POR = 2.02 (95% CI 1.18, 3.46)) significantly increased the risk of perinatal mortality. Therefore, antenatal care visit, maternal tetanus toxoid vaccination uptake, and partograph utilization should be an area of improvements to reduce perinatal mortality.
Similar content being viewed by others
Background
Perinatal mortality consists of stillbirth (pregnancy losses occurring at or after 28 weeks of gestation) and early neonatal deaths (deaths to live births within the first seven days of life)1. According to the recent Global Burden of Disease estimation 4.5 million deaths (2.1 million stillbirths and 2.4 million early neonatal deaths) were occurred in 2015 worldwide2. One million neonatal mortality occurred on the first day and close to one million dying within the first six days3. The burden of perinatal mortality was disproportional across the world. Low and middle-income countries (LMICs), mainly Sub Saharan Africa (SSA) take the lion’s share of the burden4. In developing countries, the risk of death in the perinatal period is much greater than in developed countries5. A systematic review done in SSA showed that the pooled estimate of perinatal mortality was 34.7 per 1000 live births6. The rate of perinatal mortality of Ethiopia is among the highest in SSA, which was 90 per 1000 in a hospital setting and 40 per 1000 live births in the community setting7 and 33 deaths per 1000 live births based on the reports of demographic Health Survey of 20168.
Despite a significant change was made in child health5, the reduction in perinatal mortality reduction is slower which remains a major public health concern in developing countries2. Thus, on current trends, more than 60 countries (including Ethiopia) will miss the Sustainable Developmental Goals (SDGs) target of reducing neonatal mortality by 12 deaths per 1000 live births in 20309. Perinatal mortality is a key indicator for the quality of prenatal, intrapartum and newborn care, considered as basic indicators of a country’s socio-economic situation and quality of life10. Moreover, it is a proxy measure of maternal health status and has enormous economic, social and health implications for families and society11. Evidence also confirmed that perinatal death greatly increased the vulnerability of women to experience negative psychological and social consequences12.
The maternal and perinatal health service such as antenatal care service, maternal immunization status, skilled birth delivery and sociodemographic factors as educational status of women and husband, wealth, residence, and obstetrical factors as obstetric related disorder during pregnancy, history of previous adverse perinatal outcomes, birth preparedness; and neonatal related like preterm birth, low birth weight and neonatal sepsis are associated with perinatal mortality13,14,15,16. While preterm birth, infection, hypertensive disease and intrapartum asphyxia accounted for the most common causes of perinatal mortality in LMICs17. Besides, systematic review done showed that low socioeconomic status, lack of quality health-care services, obstetric complications and lack of antenatal care were the most factors of perinatal mortality18. However, evidence suggests that two-third of perinatal mortality could be prevented using interventions including perinatal care19.
Despite, perinatal mortality can be prevented using simple cost-effective antenatal and intrapartum interventions as antenatal care visit and partograph utilization; the rate of perinatal mortality remains a major challenge in Ethiopia and associated with maternal depression20,21. Thus, to end this, the modifiable factors have to be improved permanently and universally to reduce perinatal mortality. But inconsistent and inconclusive evidence was found on the prevalence of perinatal deaths and its association with antenatal care visit, maternal tetanus vaccination, partograph utilization and poor obstetric history; which cannot be used for policymakers at the national level. Therefore, this systematic review and meta-analysis aimed to estimate the pooled national prevalence of perinatal mortality and its association with antenatal care visit, maternal tetanus vaccination status, partograph monitoring of labour and poor obstetric history. This evidence is essential to inform the health policymakers, program implementers and maternal, neonatal and perinatal health experts to achieve the SDGs target of ending preventable perinatal deaths in 2030.
Methods
Study design, data sources and search strategies
A systemic review and meta-analysis of published studies were conducted to estimate the prevalence of perinatal mortality and its association with antenatal care visit, maternal tetanus toxoid immunization and partograph utilization in Ethiopia. This systematic review and meta-analysis was reported according to the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) 2009 statement checklist22 (Supplementary file 1). All relevant published studies were searched from the major international databases like PubMed, Cochrane Library, Web of science, science direct, and African Journals Online databases. Google Scholar and Google hand searches were also used. Additionally, a search was made for the reference list of studies already identified to retrieve additional articles. Studies identified through the systematic search were retrieved and managed using Endnote X7. The Population, Exposure, Comparison and Outcomes (PECO) search formula was used to retrieve articles.
Population All births from the 28 weeks of gestation till the 7 days’ postpartum period in Ethiopia were the population of interest.
Exposures Predictors of perinatal mortality included antenatal care visit, maternal toxoid injection, partograph monitoring of labour, previous perinatal death and abortion.
Comparisons were defined for each predictor based on the reported reference group for each predictor in each respective variable.
Outcome Perinatal mortality.
For each of the selected components of PECO, electronic databases were searched using the keyword search and the medical subject heading [MeSH] words. Key words like perinatal mortality, stillbirth, predictors, determinants, antenatal care visit, maternal tetanus toxoid injection, partograph monitoring as well as Ethiopia were used. The search terms were combined by the Boolean operators "OR" and "AND.
Study selection and eligibility criteria
All published studies published from 2010 until the end of our search in the English language (7/4/2020) were retrieved to assess eligibility for inclusion in this review and critical assessment. The article selection underwent several steps. Two reviewers (MD and TYA) evaluated the retrieved articles for inclusion using their title, abstract and full-text review. Any disagreement during the selection process between the reviewers was resolved by consensus. Full texts of selected articles were then evaluated using the prior eligibility during the encounter of duplication; only the full-text article was retained. The included studies that were reported perinatal mortality or AND predictors, antenatal care visit, maternal tetanus toxoid injection, partograph monitoring and previous perinatal death. All prospective and retrospective cohort studies, cross-sectional studies, case–control and Demographic and Health Survey (DHS) reports were included in this review. However, this review excluded studies that were case reports of populations, abstracts of conferences, articles without full access and the outcome of interest not reported. Studies that were not fully accessed after at least two email contacts of the principal investigator were excluded.
Outcome variable
The primary outcome of this systematic review and meta-analysis was perinatal mortality in Ethiopia. The secondary outcomes were: the pooled effect of selected predictors on perinatal mortality, antenatal care visit, maternal toxoid injection, partograph monitoring of labour, previous history of perinatal death and abortion.
Poor obstetric history means previous unfavorable fetal outcome in terms of those having at least one of the following two or more consecutive spontaneous abortions, history of intrauterine fetal death, intrauterine growth retardation, stillbirth, early neonatal death, and/or congenital anomalies.
Maternal stress is the exposure of an expectant mother to stress, which can be caused by stressful life events like or by environmental hardships, which resulting changes to the mother's hormonal and immune system may harm the fetus's (and after birth, the infant's) immune function and brain development. Thus, women who endorse life events experienced in the prior 6 months across 11 domains, including financial, legal, relationships, career, safety in the community, safety in the home, medical issues about others, medical issues about self, authority, home issues, and prejudice. Pregnant women who endorsed the event as positive, negative, or neutral. The numbers of domains with at least one negative event were summed to create a negative life events domain score, with higher scores suggesting increased maternal stress23.
Data extraction and quality assessment
Two reviewers (MD and TYA) independently performed data extraction using a predefined eligibility criterion and assessed articles for overall study quality. The standardized data extraction format was prepared using a Microsoft Excel spreadsheet. The data extraction format included primary author, year of publication, and region of the study, sample size, and the reported outcome (perinatal mortality) and the number of cases or live birth who developing the respective outcome, and the selected predictors of perinatal mortality mainly its association with antenatal care visit, maternal tetanus toxoid vaccination, partograph monitoring of labour and previous perinatal history; previous abortion and previous perinatal mortality were extracted.
The quality of included studies was assessed using the Newcastle–Ottawa Scale (NOS) quality assessment tool based on the three components; the selection of the study groups, comparability of the study groups, and ascertainment of exposure or outcome24. The main component of the tool was graded from five stars and mainly emphasized the methodological quality of each primary study. The other component of the tool was graded from two stars and mainly concerned with the comparability of each study and the last component of the tool graded from three stars and was used to evaluate the results and statistical analysis of each original study. The NOS included three categorical criteria with a maximum score of 9 points. The quality of each study was assessed using the following score algorithms: ≥ 7 points were considered as “good”, 4 to 6 points were considered as “moderate” and ≤ 3 points were considered as “poor” quality studies. Consequently, to improve the validity of this systematic review result, only primary studies of fair to good quality have been included.
Heterogeneity and Publication bias
The publication bias was assessed using Egger’s25 and Begg’s26 tests with a p value of less than 0.05. I squared statistic was used to assess heterogeneity across studies and a p value of less than 0.05 was used to detect heterogeneity. As a result of the presence of heterogeneity, a random-effects model was used as a method of analysis27 resulting in the use of a random-effects meta-analysis model to estimate the pooled effect based on the metaprop software by STATA version 14 of the double arcsine transformations28. Because, the proportions contain inadmissible values especially when the statistic is near the boundary and computation of confidence intervals is not possible when the statistic is on the boundary, as the estimated standard error is set to zero and as a consequence, the metan command automatically excludes studies with proportion equal to 0 or 1 from the pooled estimate.
Statistical methods and analysis
The extracted data in Microsoft Excel were exported to Stata version 14 for analysis. Metaprop Stata command with double arcsine transformations was used to estimate the pooled prevalence28. Because, the proportions contain inadmissible values especially when the statistic is near the boundary and computation of confidence intervals is not possible when the statistic is on the boundary, as the estimated standard error is set to zero and as a consequence, the metan command automatically excludes studies with proportion equal to 0 or 1.
Forest plots and Odds Ratios were used to present the pooled estimate with 95% confidence intervals (CI). Subgroup analysis was conducted based on the geographic region, and study design. Besides, a meta-regression model based on sample size, geographic region, study setting, design and year of publication was used to identify the sources of random variations in the included studies. The effect of selected determinant variables was analyzed using separate categories of meta-analysis29. Also, we conducted a sensitivity analysis to assess whether the pooled prevalence estimates were influenced by individual studies.
Results
Study identification and characteristics of included studies
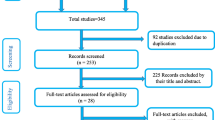
This systematic review and meta-analysis included published studies on the pooled prevalence of perinatal mortality in Ethiopia using international electronic databases. A total of 285 data sources were found in the review. Of these, 87 duplicated records were deleted and 165 articles were excluded by the screening of titles and abstracts. Subsequently, a total of 33 full-text papers were assessed for eligibility based on the inclusion and exclusion criteria. Thus, six studies were excluded due to not report the outcome of interest30,31,32,33,34,35 and the remained two articles excluded due to lack of access to the full text36,37. Finally, 25 studies have been included in the final quantitative meta-analysis (Fig. 1).
Of the 25 studies included in the final quantitative meta-analysis, 16, 13 and 21 studies were used to estimate the overall pooled prevalence of perinatal mortality, early neonatal death and stillbirth with total live birth of 91,370, 49,163 and 71,579 for each outcome respectively. In regards to the design of the included studies, two were surveys38, six prospective studies39,40,41,42,43,44, and twelve cross-sectional and four case–control studies. Of those, 16 (64%) of included studies were community-based studies. The articles were published between 2012 and 2020. The largest sample size was 48,994 of live births in a national level study45 and the smallest sample, 300 live births, from one geographic region were conducted at Southern Nations, Nationalities and Peoples Representative (SNNPR). All studies were conducted in the five geographic regions of Ethiopia. Six studies (24%) were from Amhara, seven (28%) were from SNNPR, four (16%) were from Oromia, three (12%) were from Tigray, two were the national-level studies and the remaining two was at Harar and Addis Ababa (Table 1). The included studies have fair to good qualities based on the NOS assessment tool (Supplement-2).
Meta-analysis of perinatal mortality in Ethiopia
The highest perinatal mortality was reported at the national level survey45 while the lowest was 6 per 580 live births reported from SNNPR51. The meta-analysis of 16 studies showed that the pooled national prevalence of perinatal mortality was 6% (95% CI 5.00, 7.00). A random-effect model was used due to significant heterogeneity (I2 = 97.9%, p value < 0.05) (Fig. 2). There was a publication bias based on the Eggers test with a p value of 0.0002. Due to the presence of significant publication bias, we conducted trimmed and filled analysis. The univariate meta-regression model was also used to identify possible sources of heterogeneity. However, none of these variables was found to be statistically significant, p value > 0.05. Moreover, the sensitivity analysis using a random-effects model showed that no single study had unduly influenced the overall estimate of the perinatal mortality (Supplementary file 2).
The highest cases of early neonatal mortality and stillbirth were 144 per 7367 occurred at Oromia region43 and 588 cases per 7929 live births of cohort study at Harar40. The pooled random-effect meta-analysis of fourteen studies found that the pooled prevalence of early neonatal death among live births was 2% (95% CI 0.01, 0.02). The random-effect model was used due to the presence of significant heterogeneity (I2 = 96.9%, p value < 0.05) (Fig. 3). There is no publication bias with the Eggers and Beggs test (p value of 0.35 and 0.65 respectively). The meta-analysis of twenty-one studies also showed that the pooled prevalence of stillbirth was 5% (95% CI 3.00, 6.00). The random-effect model was used due to the presence of heterogeneity (I2 = 98.7%, p value < 0.05) (Fig. 4). Therefore, to identify the source of heterogeneity a univariate regression was done based on the year of publication, sample size, geographic region, the study design and setting. But, none of the variables was significant. The funnel plot observation also showed that there is a symmetrical distribution and the objective assessment of the egger’s and Begg’s test revealed that there was publication bias with a p value of 0.001 and 0.034. Thus, the Duval and trimmed full analysis were performed to control bias.
Subgroup analysis
The subgroup analysis was conducted based on the region, the study setting and design for perinatal mortality and stillbirth. Therefore, this random effect meta-analysis based on the geographic region revealed that the highest pooled prevalence of perinatal mortality was observed in the Harar, 8.00 (95% CI 7.00, 9.00) followed by SNNPR, 7.00% (95% CI 7.00% (95% CI 4.00, 10.0) and lowest occurred at the national level study, 3.00% (95% CI 2.00, 4.00) respectively (Table 2). Also, the pooled subgroup analysis showed that the perinatal mortality was highest in the facility-based studies, 8.00% (95% CI 6.00, 9.00) and in the cross-sectional studies, 8.00% (95% CI 5.00, 10.0). The subgroup analysis of this meta-analysis showed that the highest pooled prevalence of stillbirth among live births was, 8.00% (95% CI 12.8, 28.63) and the highest prevalence of stillbirth, 7.00% (95% CI 5.00, 9.00) was reported in facility-based studies based on the thirteen studies based on the random-effect model (Table 2).
Impact of antenatal and intrapartum interventions to reduce perinatal mortality
The impact of antenatal interventions (antenatal care visit, maternal immunization) and intrapartum (partograph monitoring of labour) interventions the simplest interventions were assessed and revealed that those interventions are modifiable predictors that reduced the risk of perinatal mortality based on the pooled effect meta-analysis.
The pooled effect of seven studies showed that antenatal care visit utilization was the commonest significant predictor of perinatal mortality among live births in Ethiopia. Thus, women who had antenatal care visit were 80% [POR = 0.20 (95% CI 0.12, 0.34)] less likely to have perinatal mortality than those women haven’t any antenatal care visit during pregnancy. A random-effect model was used due to significant heterogeneity (I2 = 86.7%, p value < 0.05 (Fig. 5). The meta-analysis of three studies revealed that maternal tetanus toxoid immunization uptake was another maternal intervention to reduce the perinatal mortality, women who had utilized the tetanus toxoid immunization were 57% [POR = 0.43 (95% CI 0.24, 0.77)] decreased the odds of perinatal mortality than those women who haven’t utilized tetanus toxoid immunization during pregnancy or postpartum period (Fig. 6).
Also, this systematic review and meta-analysis showed the pooled effect of the most important intrapartum interventions during labour, partograph utilization for monitoring of labour was significantly associated with perinatal mortality; the utilization of partograph for monitoring of labour during the active phase of labour was 78% [POR = 0.22 (95% CI 0.06, 0.76)] less likely to have the chance of perinatal mortality than their counterparts based on the random-effect of a meta-analysis of due to the presence of heterogeneity (I2 = 97.2%, with p value < 0.0001 (Fig. 7). There was no publication bias based on the Eggers and Beggs test with a p value of < 0.05.
Association of poor maternal obstetric history and perinatal mortality
Seven studies were included to assess the effect of poor obstetric history mainly previous perinatal death (based on four studies) and previous abortion history with three studies. Therefore, the pooled effect of the four studies revealed that women who have previous perinatal death were 8 times [OR = 7.95 (95% CI 5.59, 11.30)] more likely to have recent perinatal mortality than those who haven’t any perinatal mortality in previous pregnancy and childbirth. The fixed effect model of meta-analysis was used due to the absence of statistically significant evidence of heterogeneity, I2 = 0% and p = 0.76 (Fig. 8). Egger’s test showed a non-significant publication bias. Moreover, the pooled effect of three studies showed that women who have a previous history of abortion were two [OR = 2.07 (95% CI 1.33, 3.21)] times more likely to the perinatal mortality compared with their counterparts. The fixed effect model of the meta-analysis was used due to the lower or absence of evidence of significant heterogeneity (I2 = 32.5% and p = 0.23) (Fig. 9). There was no publication bias based on egger’s test.
Discussions
The systematic review and meta-analysis found that the pooled estimate prevalence of perinatal mortality was 6% (95% CI 5.00, 7.00); which is higher than the study done in SSA, 3.47%6. The possible justification for this might be due to the variability in the use and quality of maternal health care services provided to pregnant women and their newborns and the study design difference, in that of the SSA the meta-analysis was done based on the demographic health survey of data of 21 countries, and also the higher burden of cesarean delivery in our setting, and home delivery might be also increased the estimate of perinatal mortality. Hence, a systematic review and meta-analysis supported that rate of perinatal deaths following cesarean sections are disproportionately high in LMICs56 and perinatal mortality varies by place of delivery; perinatal mortality is 21% higher for the home compared to facility-based deliveries57. Therefore, proper auditing of cesarean delivery to reduce to the optimal recommended level and improving health facility delivery should be emphasised. This meta-analysis also showed that that the pooled prevalence of stillbirth was, 5% (95% CI 3.00, 6.00) which was comparable with the global network study at LMICs with the epidemiology of stillbirth of 3.2%58. On the other hand, the current pooled estimate of stillbirth was lower than the findings done in Guatemala, 19.9% and 25.3% in India59,60. This variation might be due to the difference in methodology, in the study design and participants included in this systematic review and the countries else.
The findings of this meta-analysis also found that the highest prevalence of perinatal mortality has occurred in Harar and SNNPR and the lowest was at Oromia and Addis Ababa next to the National level. The possible reason for the regional variation in the level of perinatal mortalities in Ethiopia could be explained by the difference in maternal health care service utilization. Hence, a national demographic health survey report in Ethiopia supported that the lowest and highest antenatal care (ANC) service utilization were spatially clustered in Harar (%), SNNPR (39.8%) and Addis Ababa (94%), respectively61. Hence, a systematic review supports that ANC visit significantly increases birth in the health facility, which reduces the risk of perinatal mortality62. Regarding the lower pooled estimate of perinatal mortality at the national level might be explained due to the inclusion of demographic health survey data, intermittent nature of data collection of demographic health survey data, absence of supply chain information and women’s potential of recall bias, substantially underestimate mortality.
This systematic review and meta-analysis revealed that antenatal care visit is the most significant protective factor for the reduction of perinatal mortality. This finding is in line with other studies done in LMICs63, and United States64 found that the odds of perinatal mortality increases among women who have no ANC visit. The possible explanation for this might be due to the fact, those women who have ANC visit might be more likely to increase the maternal literacy, early awareness of pregnancy complications and get the continuum care ; a skilled birth attendant at the health facility and Birth Preparedness and Complication Readiness (BPCR) interventions, getting an antenatal screening of complications, intrapartum, postpartum and neonatal care, associated with an increased likelihood of use of care in the event of newborn illness, and initiation of breastfeeding in the first hour of life, encourages to take decisions before the onset of labour and occurrence of obstetric complications and got the service timely65,66; reduces of perinatal mortality. Hence, a meta-analysis supports that antenatal screening of antenatal syphilis67, gave birth at the health facility57 and BPCR interventions68 are known factors for the reduction of perinatal mortality. Again, those women who had ANC visit might more likely adhere to prenatal maternal nutrition like iron-folic acid supplementations and other micronutrients, which reduces maternal anaemia that increase the risk of perinatal morbidity, preterm births and low birth weight are the leading cause of perinatal mortality69,70. Iron and folic acid and other micronutrients are vital for the development of the fetus, prevents poor birth outcomes. Hence, a meta-analysis revealed that adherence to IFA supplementation and micronutrients is means of reduction of anemia, hemorrhagic newborn disease, congenital anomalies for the fetus, further substantially reduces the risk of perinatal mortality71,72. Thus, there remained activities for the government, researchers and organizations in increasing the ANC visit care based on the WHO recommendations within the national context.
Accordingly, this systematic review and meta-analysis found that the immunization of maternal tetanus toxoid was also another predictor that decreases the chance of perinatal mortality. This can be explained because those women who have got the immunization might be less likely to acquire the infection mainly maternal and neonatal tetanus73. Maternal and neonatal tetanus causes about half of all perinatal deaths and neonatal mortality today, claiming about 180,000 lives worldwide every year mainly in developing countries. However, it is easily prevented by maternal immunization with tetanus toxoid vaccine during antenatal care visit and the interventions to screen and manage infections during pregnancy and intrapartum period are means of reducing those perinatal mortalities attributable to infection74. Despite, the tetanus toxoid vaccination uptake is low, 14.8% to 39%75,76 and the dropout rate of the immunization is increasing up to 72.3%77 Ethiopia. Thus, future strategies to improve the vaccination rate should be emphasised and future prospective studies have to done to assess the effect of the dose of maternal tetanus toxoid immunization on perinatal outcomes.
This meta-analysis also found that partograph monitoring of labour was another intrapartum intervention that significantly reduces the rate of perinatal mortality. This might be since partograph helps the health care provider in identifying the slow progress of labour and provides an early warning system for early referral and may also help to initiate appropriate interventions within a timely manner. Hence, proper partograph utilization improves labour outcomes78,79,80,81. Thus, proper partograph monitoring of labour should be improved at the national level to reduce the rate of perinatal mortality and poor labour outcomes. Therefore, a continuum of care has the potential to scale up to improve the maternal, newborn, and child health (MNCH) by ensuring care for mothers and children, indicates that obstetric care needs still to be strengthened, should include the continuum of care from home to the health facility, make care accessible to all, and reduce delays.
Moreover, the results of this systematic review and meta-analysis investigated that women who had a history of previous perinatal mortality significantly increased the odds of perinatal mortality than their counterparts. This was supported by a meta-analysis done at high-income countries82. Furthermore, this systematic review and meta-analysis found that a previous history of abortion also significantly increased the chance of having perinatal mortality, which was also supported by previous studies done by Brown et al.83 and Saraswat L et al.84. The possible reason for the significant increase of perinatal mortality among those women might be more likely to develop maternal stress associated with the previous exposure. Maternal stress increased the risk of preterm birth85,86 through increased production of proinflammatory cytokines87, cause the production of prostaglandins88, weaken fetal membranes and ripen the cervix89 increases preterm birth, increased the risk of perinatal death. Thus, improving the care provision, integrating mental health with women with previous bad obstetric history is an area of improvements in future studies.
Despite, there was a very extensive systematic search and inclusion of articles without specifying the period of publications, the results of this review should be interpreted with some limitation. The high heterogeneity in between studies might lead to insufficient statistical power to detect significant association. Thus, a meta-regression analysis revealed that there was no variation due to sample size and publication year. This meta-analysis was also unable to assess the association between the doses of maternal tetanus immunizations with perinatal mortality, an area of future research. Also, the studies included in this review were from only five regions and some studies have a small sample size that might reduce its representative for the country. It was impossible to establish the cause-and-effect relationship.
Conclusions
A significant number of live births in Ethiopia are suffering from perinatal mortality. Therefore, the antenatal and intrapartum interventions as antenatal care visit, maternal tetanus toxoid vaccination uptake, monitoring of labour with partograph and identifying of the maternal obstetric history should be an area of improvements to reduce perinatal mortality. The Federal Ministry of Health and other concerned bodies should work towards the reduction of perinatal mortality by emphasizing the identified modifiable factors.
Availability of data and materials
Data will be available from the corresponding author upon reasonable request.
Abbreviations
- ANC:
-
Antenatal care
- BPCR:
-
Birth preparedness and complication readiness
- LMICs:
-
Low and middle-income countries
- NOS:
-
Newcastle-Ottawa scale
- POR:
-
Pooled odds ratio
- SSA:
-
Sub Saharan Africa
References
Organization WH. Neonatal and perinatal mortality: Country, regional and global estimates. World Health Organization (2006).
Wang, H. et al. Global, regional, national, and selected subnational levels of stillbirths, neonatal, infant, and under-5 mortality, 1980–2015: A systematic analysis for the Global Burden of Disease Study 2015. The Lancet 388(10053), 1725–1774 (2016).
WHO: Global health observatory (GHO) dataChild mortality and causes of death. World Health Organization Geneva (2016).
You, D. et al. United Nations Inter-agency Group for Child Mortality Estimation (UN IGME). Global, regional, and national levels and trends in under-5 mortality between 1990 and 2015, with scenario-based projections to 2030: A systematic analysis by the UN Inter-agency Group for Child Mortality Estimation. Lancet 386(10010), 2275–2286 (2015).
WHO: Neonatal and perinatal mortality: country, regional and global estimates (2006).
Akombi, B. J. & Renzaho, A. M. Perinatal mortality in Sub-Saharan Africa: A meta-analysis of demographic and health surveys. Ann. Glob. Health 85(1), 106 (2019).
Berhan, Y. & Berhan, A. Perinatal mortality trends in Ethiopia. Ethiop. J. Health Sci. 24, 29–40 (2014).
FDRE: Ethiopian Demographic and Health Survey (2016).
Unicef: Committing to child survival: a promise renewed. In.: eSocialSciences (2015).
Family Planningf Reproductive Health Indicators Database: New Born Mortality[Internet]. Chapel Hill (NC): MEASURE Evaluation, Carolina Population Center, University of North Carolina at Chapel Hill. In.; (2012).
UNDP: United Nations Development Programme: Measuring Human Development: A Primer. New York: UNDP (2007).
Gausia, K. et al. Psychological and social consequences among mothers suffering from perinatal loss: Perspective from a low income country. BMC Public Health 11(1), 451 (2011).
Mekonnen, Y., Tensou, B., Telake, D. S., Degefie, T. & Bekele, A. Neonatal mortality in Ethiopia: Trends and determinants. BMC Public Health 13(1), 483 (2013).
Orsido, T. T., Asseffa, N. A. & Berheto, T. M. Predictors of Neonatal mortality in Neonatal intensive care unit at referral Hospital in Southern Ethiopia: A retrospective cohort study. BMC Pregnancy Childbirth 19(1), 83 (2019).
Ghorat, F., Ghafarzadeh, R. & Jafarzadeh Esfehani, R. Perinatal mortality and its associated risk factors: A study in the North-East of Iran. Iran. J. Neonatol. IJN 7(1), 47–51 (2016).
Al Kibria, G. M. et al. Determinants of early neonatal mortality in Afghanistan: An analysis of the demographic and health survey. Global Health 14(1), 47 (2018).
Wardlaw, T., You, D., Hug, L., Amouzou, A. & Newby, H. UNICEF Report: Enormous progress in child survival but greater focus on newborns urgently needed. Reprod. Health 11(1), 82 (2014).
Ghimire, P. R. et al. Perinatal mortality in South Asia: Systematic review of observational studies. Int. J. Environ. Res. Public Health 15(7), 1428 (2018).
WHO. WHO recommendations on antenatal care for a positive pregnancy experience. World Health Organization (2016).
Fantahun, A., Cherie, A. & Deribe, L. Prevalence and Factors Associated with Postpartum Depression Among Mothers Attending Public Health Centers of Addis Ababa, Ethiopia, 2016. Clin. Pract. Epidemiol. Ment. Health 14, 196–206 (2018).
Tefera, T. B., Erena, A. N., Kuti, K. A. & Hussen, M. A. Perinatal depression and associated factors among reproductive aged group women at Goba and Robe Town of Bale Zone, Oromia Region, South East Ethiopia. Mater. Health Neonatol. Perinatol. 1(1), 12 (2015).
Moher, D. et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 4(1), 1–9 (2015).
Shalowitz, M. U., Berry, C. A., Rasinski, K. A. & Dannhausen-Brun, C. A. A new measure of contemporary life stress: Development, validation, and reliability of the CRISYS. Health Serv. Res. 33(5 Pt 1), 1381 (1998).
Singer, M. et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA 315(8), 801–810 (2016).
Egger, M. S. G., Schneider, M. & Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 315(7109), 629–634 (1997).
Begg, C. B. M. M. Operating characteristics of a rank correlation testfor publication bias. Biometrics 50(4), 1088–1101 (1994).
Higgins, J. P. T. S., Deeks, J. J. & Altman, D. G. Measuring inconsistency in meta-analyses. BMJ 327(7414), 557 (2003).
Nyaga, V. N., Arbyn, M. & Aerts, M. Metaprop: A Stata command to perform meta-analysis of binomial data. Arch. Public Health 72(1), 39 (2014).
Deeks, J. J., Higgins, J. P. & Altman, D. G. Analysing data and undertaking meta-analyses. In Cochrane Handbook for Systematic Reviews of Interventions (eds Higgins, J. P. et al.) 241–284 (Wiley, Hoboken, 2008).
Gessesse, M. & Nunes Ade, L. Analysis of early neonatal deaths in Yekatit 12 hospital, Addis Ababa. Ethiop. Med. J. 47(4), 255–259 (2009).
Berhan, Y. & Berhan, A. Perinatal mortality trends in Ethiopia. Ethiop. J. Health Sci. 24(Suppl(0 Suppl)), 29–40 (2014).
Welegebriel, T. K., Dadi, T. L. & Mihrete, K. M. Determinants of stillbirth in Bonga general and Mizan Tepi University teaching hospitals southwestern Ethiopia, 2016: A case–control study. BMC Res. Notes 10(1), 713 (2017).
Worede, D. T. & Dagnew, G. W. Determinants of stillbirth in Felege-Hiwot comprehensive specialized referral hospital, North-west, Ethiopia, 2019. BMC Res. Notes 12(1), 579 (2019).
Tilahun, D. & Assefa, T. Incidence and determinants of stillbirth among women who gave birth in Jimma University specialized hospital, Ethiopia. Pan Afr. Med. J. 28(1), 299 (2017).
Tasew, H., Zemicheal, M., Teklay, G. & Mariye, T. Risk factors of stillbirth among mothers delivered in public hospitals of Central Zone, Tigray, Ethiopia. Afr. Health Sci. 19(2), 1930–1937 (2019).
Gaym, A. Perinatal mortality audit at Jimma hospital, South-Western Ethiopia, 1990–1999. Ethiop. J. Health Dev. 14(3), 335–343 (2000).
Bisetegne, D., Hakim, L. Stillbirth at Tikur Anbessa hospital a retrospective study. Ethiop. J. Reprod. Health 2(1) (2008).
Berhie, K. A. & Gebresilassie, H. G. Logistic regression analysis on the determinants of stillbirth in Ethiopia. Mater. Health Neonatol. Perinatol. 2(1), 10 (2016).
Andargie, G., Berhane, Y., Worku, A. & Kebede, Y. Predictors of perinatal mortality in rural population of Northwest Ethiopia: a prospective longitudinal study. BMC Public Health 13(1), 168 (2013).
Tura, A. K. et al. Surviving mothers and lost babies–burden of stillbirths and neonatal deaths among women with maternal near miss in eastern Ethiopia: a prospective cohort study. J. Glob. Health 10(1), 01041310 (2020).
Debelew, G. T., Afework, M. F. & Yalew, A. W. Determinants and causes of neonatal mortality in Jimma zone, southwest Ethiopia: a multilevel analysis of prospective follow up study. PLoS ONE 9(9), e107184 (2014).
Limaso, A. A., Dangisso, M. H. & Hibstu, D. T. Neonatal survival and determinants of mortality in Aroresa district, Southern Ethiopia: A prospective cohort study. BMC Pediatr. 20(1), 33 (2020).
Desta, B. N., Kassa, N. A., Damte, T. D. & Hordofa, L. O. Incidence and risk factors of neonatal mortality in eastern ethiopia, a prospective cohort study in kersa health and demographic surveillance system (Kersa HDSS). Epidemiol. Biostat. Public Health 13(4), 19 (2016).
Assefa, N., Berhane, Y., Worku, A. & Tsui, A. The hazard of pregnancy loss and stillbirth among women in Kersa, East Ethiopia: A follow up study. Sex. Reprod. Healthcare 3(3), 107–112 (2012).
Tessema F, Lakew Y. Trends and causes of neonatal death in Ethiopian, 2010–14. Health and demographic surveillance system of Ethiopian Universities Research Centers’ Network Policy Brief Number (2016).
Woldeamanuel, B. T. & Gelebo, K. K. Statistical analysis of socioeconomic and demographic correlates of perinatal mortality in Tigray region, Ethiopia: a cross sectional study. BMC Public Health 19, 1–10 (2019).
Aragaw, Y. Perinatal mortality and associated factor in Jimma university specialized hospital, South West Ethiopia. Gynecol. Obs. 6, 932–2161 (2016).
Roro, E. M., Sisay, M. M. & Sibley, L. M. Determinants of perinatal mortality among cohorts of pregnant women in three districts of North Showa zone, Oromia Region, Ethiopia: Community based nested case control study. BMC Public Health 18, 1–11 (2018).
Yirgu, R., Molla, M., Sibley, L. & Gebremariam, A. Perinatal mortality magnitude, determinants and causes in west Gojam: population-based nested case-control study. PLoS One 11, e0159390 (2016).
Bayou, G. & Berhan, Y. Perinatal mortality and associated risk factors: a case control study. Ethiop. J. Health Sci. 22, 153–162 (2012).
Tsegaye, B. & Kassa, A. Prevalence of adverse birth outcome and associated factors among women who delivered in Hawassa town governmental health institutions, south Ethiopia, in 2017. Reprod. Health 15(1), 193 (2018).
Lakew, D., Tesfaye, D. & Mekonnen, H. Determinants of stillbirth among women deliveries at Amhara region, Ethiopia. BMC Pregnancy Childbirth 17, 1–7 (2017).
Adane, A. A., Ayele, T. A., Ararsa, L. G., Bitew, B. D. & Zeleke, B. M. Adverse birth outcomes among deliveries at Gondar University hospital, Northwest Ethiopia. BMC Pregnancy Childbirth 14, 1–8 (2014).
Maeruf, H. et al. Advanced maternal age pregnancy and its adverse obstetrical and perinatal outcomes in Ayder comprehensive specialized hospital, Northern Ethiopia, 2017: a comparative cross-sectional study. BMC Pregnancy Childbirth 20, 1,10 (2020).
Zerfu, T. A., Umeta, M. & Baye, K. Dietary diversity during pregnancy is associated with reduced risk of maternal anemia, preterm delivery, and low birth weight in a prospective cohort study in rural Ethiopia. Am. J. Clin. Nutr. 103, 1482–1488 (2016).
Sobhy, S. et al. Maternal and perinatal mortality and complications associated with caesarean section in low-income and middle-income countries: a systematic review and meta-analysis. Lancet 393(10184), 1973–1982 (2019).
Chinkhumba, J., De Allegri, M., Muula, A. S. & Robberstad, B. Maternal and perinatal mortality by place of delivery in sub-Saharan Africa: A meta-analysis of population-based cohort studies. BMC Public Health 14(1), 1014 (2014).
McClure, E. M. et al. Epidemiology of stillbirth in low-middle income countries: A Global Network Study. Acta Obstet. Gynecol. Scand. 90(12), 1379–1385 (2011).
Blencowe, H. C. S. et al. National, regional, and worldwide estimates of stillbirth rates in 2015, with trends from 2000: A systematic analysis. Lancet Glob. Health 4(2), e98-108 (2016).
Saleem, S. T. S. et al. Trends and determinants of stillbirth in developing countries: Results from the global Network’s population-based birth registry. Reprod. Health 15(1), 100 (2018).
Yeneneh, A., Alemu, K., Dadi, A. F. & Alamirrew, A. Spatial distribution of antenatal care utilization and associated factors in Ethiopia: Evidence from Ethiopian demographic health surveys. BMC Pregnancy Childbirth 18(1), 1–12 (2018).
Berhan, Y. & Berhan, A. Antenatal care as a means of increasing birth in the health facility and reducing maternal mortality: a systematic review. Ethiop. J. Health Sci. 24, 93–104 (2014).
Berhan, Y. & Berhan, A. Meta-analysis of selected maternal and fetal factors for perinatal mortality. Ethiop. J. Health Sci. 24, 55–68 (2014).
Getahun, D. A. C. & Kinzler, W. L. Risk factors for antepartum and intrapartum stillbirth: A population-based study. Am. J. Obstet. Gynecol. 196, 499–507 (2007).
Organization, W. H. Working with individuals, families and communities to improve maternal and newborn health (World Health Organization, 2003).
Del Barco, R. Monitoring Birth Preparedness and Complication Readiness. Tools and Indicators for Maternal and Newborn Health (Jhpiego, 2004).
Hawkes, S., Matin, N., Broutet, N. & Low, N. Effectiveness of interventions to improve screening for syphilis in pregnancy: A systematic review and meta-analysis. Lancet Infect. Diseases 11(9), 684–691 (2011).
Soubeiga, D., Gauvin, L., Hatem, M. A. & Johri, M. Birth Preparedness and Complication Readiness (BPCR) interventions to reduce maternal and neonatal mortality in developing countries: Systematic review and meta-analysis. BMC Pregnancy Childbirth 14(1), 129 (2014).
WHO. The global prevalence of anaemia in 2011. World Health Organization, Geneva (2015).
Rahman, M. M. et al. Maternal anemia and risk of adverse birth and health outcomes in low-and middle-income countries: Systematic review and meta-analysis, 2. Am. J. Clin. Nutr. 103(2), 495–504 (2016).
Imdad, A. & Bhutta, Z. A. Routine iron/folate supplementation during pregnancy: Effect on maternal anaemia and birth outcomes. Paediatric Perinatal Epidemiol. 26, 168–177 (2012).
Nisar, Y. B. & Dibley, M. J. Earlier initiation and use of a greater number of iron-folic acid supplements during pregnancy prevents early neonatal deaths in Nepal and Pakistan. PLoS ONE 9(11), e112446 (2014).
Roper, M. H., Vandelaer, J. H. & Gasse, F. L. Maternal and neonatal tetanus. The Lancet 370(9603), 1947–1959 (2007).
Ishaque, S. et al. Effectiveness of interventions to screen and manage infections during pregnancy on reducing stillbirths: A review. BMC Public Health 11(3), S3 (2011).
Gebremedhin, T. S., Welay, F. T., Mengesha, M. B., Assefa, N. E. & Werid, W. M. Tetanus toxoid vaccination uptake and associated factors among mothers who gave birth in the last 12 months in Errer District, Somali Regional State, Eastern Ethiopia. BioMed Res. Int. https://doi.org/10.1155/2020/4023031 (2020).
Anatea, M. D., Mekonnen, T. H. & Dachew, B. A. Determinants and perceptions of the utilization of tetanus toxoid immunization among reproductive-age women in Dukem Town, Eastern Ethiopia: A community-based cross-sectional study. BMC Int. Health Human Rights 18(1), 27 (2018).
Belihu, K., Tesso, F. & Woldetsadik, T. Dropout rate of tetanus toxoid immunization and associated factors among reproductive age group of women in Debrebirhan Town, Amhara Region, Northern Ethiopia. J. Women’s Health Care 6(390), 2167–0420.1000390 (2017).
Lavender, T., Cuthbert, A. & Smyth, R. M. Effect of partograph use on outcomes for women in spontaneous labour at term and their babies. Cochrane Database System. Rev. 8, CD005461 (2018).
Mathai, M. The partograph for the prevention of obstructed labor. Clin. Obstetr. Gynecol. 52(2), 256–269 (2009).
Gans-Lartey, F., O’Brien, B. A., Gyekye, F. O. & Schopflocher, D. The relationship between the use of the partograph and birth outcomes at Korle-Bu teaching hospital. Midwifery 29(5), 461–467 (2013).
Dangal, G. Preventing prolonged labor by using partograph. Int. J. Gynecol. Obstet. 7(1), 1–4 (2006).
Flenady, V. et al. Major risk factors for stillbirth in high-income countries: A systematic review and meta-analysis. The Lancet 377(9774), 1331–1340 (2011).
Brown, J., Adera, T. & Masho, S. Previous abortion and the risk of low birth weight and preterm births. J. Epidemiol. Commun. Health 62(1), 16–22 (2008).
Saraswat, L., Bhattacharya, S., Maheshwari, A. & Bhattacharya, S. Maternal and perinatal outcome in women with threatened miscarriage in the first trimester: A systematic review. BJOG: Int. J. Obstetr. Gynaecol. 117(3), 245–257 (2010).
Lilliecreutz, C., Larén, J., Sydsjö, G. & Josefsson, A. Effect of maternal stress during pregnancy on the risk for preterm birth. BMC Pregnancy Childbirth 16(1), 5 (2016).
Staneva, A., Bogossian, F., Pritchard, M. & Wittkowski, A. The effects of maternal depression, anxiety, and perceived stress during pregnancy on preterm birth: A systematic review. Women Birth: J Austral College Midwives 28(3), 179–193 (2015).
Christian, L. M. Psychoneuroimmunology in pregnancy: Immune pathways linking stress with maternal health, adverse birth outcomes, and fetal development. Neurosci. Biobehav. Rev. 36(1), 350–361 (2012).
Challis, J. R. et al. Inflammation and pregnancy. Reprod. Sci. 16(2), 206–215 (2009).
Snegovskikh, V., Park, J. S. & Norwitz, E. R. Endocrinology of parturition. Endocrinol. Metab. Clin. 35(1), 173–191 (2006).
Funding
No funding sources for this review.
Author information
Authors and Affiliations
Contributions
M.D.: conceived and designed the study protocol, literature review, data extraction, data analysis, interpretation and wrote up the manuscript. T.G.: designed the study protocol, literature review, data extraction, and wrote up the manuscript T.Y.A., Y.M.A., A.S., A.A., Z.T., D.Y., A.A.A., D.B.K., and W.S.S. have reviewed and edit the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Desta, M., Akalu, T.Y., Alamneh, Y.M. et al. Perinatal mortality and its association with antenatal care visit, maternal tetanus toxoid immunization and partograph utilization in Ethiopia: a meta-analysis. Sci Rep 11, 19641 (2021). https://doi.org/10.1038/s41598-021-98996-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-98996-5
- Springer Nature Limited
This article is cited by
-
Contributing factors of birth asphyxia in Thailand: a case–control study
BMC Pregnancy and Childbirth (2023)