Abstract
Mechanisms involved in the acute responses to renal denervation (RDN) have yet to be fully understood. We assessed urinary volume, autonomic control and aorta vascular reactivity after acute RDN. Male normotensive Wistar rats and spontaneously hypertensive rats (SHR) were divided into normotensive + RDN (ND) or sham surgery (NS), and hypertensive + RDN (HD) or sham surgery (HS). Metabolic parameters and hemodynamic measurements were recorded 72h and 4 days after intervention, respectively. Aortic rings were studied 7 days post RDN in an isometric myograph. Concentration–response curves to phenylephrine, sodium nitroprusside and acetylcholine (10–10–10−5 M) were performed. Two-way ANOVA was used for group comparisons and differences reported when p < 0.05. Results are presented as mean ± SEM. Urinary volume was 112% higher in HD vs. HS (HS = 14.94 ± 2.5 mL; HD = 31.69 ± 2.2 mL) and remained unchanged in normotensive rats. Systolic BP was lower in HD rats (HS = 201 ± 12 vs. HD = 172 ± 3 mmHg) without changes in normotensive group. HD group showed increased HF and LF modulation (HS = 5.8 ± 0.7 ms2 vs. HD = 13.4 ± 1.4 ms2; HS = 3.5 ± 0.7 ms2 vs. HD = 10.5 ± 1.7 ms2, respectively). RDN normalized vascular reactivity in HD rats and increased phenylephrine response in ND rats. Acute fall in BP induced by RDN is associated with increased urinary volume, which in turn may also have contributed to functional changes of the aorta.
Similar content being viewed by others
Introduction
It is known that amplitude of the degree of sympathetic nervous system activation is directly related to the magnitude of elevated blood pressure (BP) in the hypertensive patients1. In fact, in hypertension the sympathetic efferent fibers are hyperstimulated and contribute to increased BP2. The ablation of efferent renal nerves leads to a decrease in BP, since it reduces the activity of the renal sympathetic nerve, promoting urinary sodium excretion, whereas afferent renal sympathetic nerve ablation decreases BP by inhibiting central sympathetic flow3. Indeed, studies using experimental models have found that nerve ablation reduces both BP and the target organ damage caused by chronic sympathetic hyperactivity4,5. We have previously demonstrated the key role of renal nerves in cardiovascular homeostasis in hypertension induced by aortic ligation; complete denervation of the ischemic kidney was able to attenuate hypertension, normalize the renin plasma activity and baroreceptor reflex of heart rate 10 days after aortic ligation6.
Catheter-based renal denervation (RDN) has been proposed as a novel treatment in patients with resistant hypertension. Previous studies have shown the effectiveness of this procedure in reducing blood pressure in such patients7,8. Despite the enthusiasm surrounding the procedure, the Symplicity HNT-3 trial (2014), the first to compare renal nerve ablation with a sham procedure, found no significant reduction in the blood pressure. The failure of the trial has been attributed to several possible confounding factors, including issues related to patient selection and medication adherence, suboptimal procedural performance, and operator experience9. The more recent studies, with improved trial design, selection of relevant patient cohorts, and optimized interventional procedures have presented positive outcomes (change in 24-h blood pressure at 2, 3 and 6 months)10,11,12,13.
In light of the controversies still surrounding the effectiveness of this at present, RDN should for now be regarded as alternative approach, to be used only in patients within the context of clinical research and in highly qualified centers14.
Despite the accumulated knowledge gained over all these years of research, the mechanisms underlying BP reduction by RDN have yet to be fully understood. The beneficial effects of this technique on hypertension have been associated with mechanisms such as a progressive decrease in renin release and renal sodium retention15 and attenuation of oxidative stress and inflammation16.
Given the key role of the renal vasculature and the autonomic nervous system in conditions involving increased renal sympathetic nerve activity, such as hypertension and heart failure, the quest for a better understanding of these mechanisms seems to be crucial in proper inform the management and use of renal denervation procedure.
To our knowledge, there are no studies reporting changes in aortic vascular reactivity in renal denervated normotensive and spontaneously hypertensive rats (SHR). In order to have a fuller understanding of the mechanisms underlying RDN, we evaluated aorta response to phenylephrine (Phe), acetylcholine (Ach) and sodium nitroprusside (SNP). Our hypothesis is that renal nerve ablation may be able to improve aorta function. In addition, we assessed heart rate (HR) and blood pressure (BP) variability, along with the reflex control of HR as candidate mechanisms involved in the decrease in BP after denervation.
Therefore, the major aim of this study was to evaluate the autonomic modulation of the circulation of SHR animals after acute renal denervation (7–10 days), as well as the vascular function and morphological alterations of the thoracic descending aorta in these animals.
Results
RDN effects on blood pressure
Although renal denervation was not able to normalize SHR rats blood pressure, hypertensive denervated rats showed lower systolic and diastolic pressures when compared to hypertensive sham group (HS = 201 ± 12 mmHg vs. HD = 172 ± 3 mmHg, and HS = 147 ± 8 mmHg vs. HD = 114 ± 4 mmHg, respectively), resulting in a lower mean pressure (HS = 175 ± 9 mmHg vs. HD = 141 ± 4 mmHg). However, normotensive group pressures remained unchanged, as showed in Fig. 1.
Blood pressure 4 days after intervention. (a) Systolic blood pressure (SBP); (b) diastolic blood pressure (DBP); (c) mean blood pressure (MBP). Data were analyzed by two-way ANOVA followed by Tukey’s post hoc test. Values are mean ± SEM. ANOVA: Interaction factor (I); Blood pressure background factor (P); Denervation factor (D). **p < 0.01; ***p < 0.001 vs. hypertensive sham (HS).
RDN effects on autonomic balance
Figure 2a to f shows RDN effects on autonomic balance. Although RDN did not change heart rate (HR) in normotensive Wistar or hypertensive rats, heart rate variance (HRVar) was higher in hypertensive rats when denervated (HS = 76 ± 9 ms2 vs. HD = 208 ± 8 ms2), while no difference was observed in Wistar rats (NS = 115 ± 10 ms2 vs. ND = 108 ± 12 ms2, Fig. 2a and b).
Autonomic balance 4 days after intervention. (a) Heart rate (HR); (b) heart rate variance (HRVar); (c) square root of the sum of the squares of the consecutive pulse interval differences (RMSSD); (d) high frequency (HF) modulation; (e) low frequency (LF) modulation. (f) Alpha index (AI). Data were analyzed by two-way ANOVA followed by Tukey’s post hoc test. Values are mean ± SEM. ANOVA: Interaction factor (I); Blood pressure background factor (P); Denervation factor (D). *p < 0.05; **p < 0.01; ****p < 0.0001 vs. hypertensive sham (HS).
RMSSD and high frequency (HF) modulation, both involved in parasympathetic modulation, were greater in hypertensive denervated rats when compared to hypertensive sham (HS = 3.5 ± 0.7 ms vs. HD = 5.9 ± 0.5 ms; HS = 5.8 ± 0.7 ms2 vs. HD = 13.4 ± 1.4 ms2 respectively.
Should be emphasized that for these 2 parameters (RMSSD and HF) no differences between Wistar and RDN-treated SHR rats were found, indicating that renal denervation is capable to restore parasympathetic modulation in SHR. Normotensive rats remained unchanged (Fig. 2c and d)
Similarly, low frequency (LF), which reflects sympathetic modulation, was also increased in HD vs. HS (HS = 3.5 ± 0.7 ms2; HD = 10.5 ± 1.7 ms2) while no difference was observed for normotensive rats (NS = 4.5 ± 0.6 ms2; ND = 4.6 ± 0.5 ms2, Fig. 2e).
Alpha index (baroreflex marker) remained unchanged after RDN in both Wistar and SHR rats (Fig. 3f).
Metabolic parameters 72 h after intervention. (a) Water intake; (b) urinary volume; (c) hydric balance. Data were analyzed by two-way ANOVA followed by Tukey’s post hoc test. Values are mean ± SEM. ANOVA: interaction factor (I); blood pressure background factor (P); denervation factor (D). *p < 0.05; **p < 0.01 vs. hypertensive sham.
RDN effects on metabolic parameters
Although hypertensive denervated animals (HD) ingested 46% more water than their control (HS), these same animals showed an urinary volume 112% higher than HS, ensuring greater hydric balance for this group (HS = 38 ± 3% vs. HD = 55 ± 3% ) and demonstrating volume loss in HD animals 72 h after intervention. However, no effects of RDN were observed on normotensive rats in urinary volume, water intake or hydric balance (Fig. 3). Body weight at the end of the experiment was NS = 399 ± 12 g; ND = 337 ± 11 g; HS = 294 ± 22 g and HD = 277 ± 4 g. Other metabolic parameters such as chow intake and feces are presented as supplementary data (see supplementary Fig. S1).
RDN effects on aortic vasorelaxation response
Figure 4a and b represent aorta relaxation when vessel rings were exposed to a concentration–response curve to sodium nitroprusside (endothelium-independent relaxation), and acetylcholine (endothelium-dependent relaxation). When compared to normotensive sham rats (yellow circles), normotensive denervated rats (red squares) exhibited a left-down shift in vasodilator response. This is also observed in half-maximal dose (logED50) which shows a greater sensibility in ND to SNP (Table 1).
Aorta relaxation 7–10 days after renal denervation. (a) Concentration–response curve to sodium nitroprusside; (b) Concentration–response curve to Acetylcholine. NS: normotensive sham (n = 6); ND: denervated normotensive (n = 9), HS: SHR sham (n = 5); HD: denervated SHR (n = 4). Data were analyzed by two-way ANOVA followed by Fisher post hoc test. Values are mean ± SEM. ANOVA: Interaction factor (I); Concentration factor (C); Groups factor (G); Matching (M). #p < 0.05; ##p < 0.01; ####p < 0.0001 NS vs. ND; *p < 0.05 HS vs. HD.
On the other hand, although renal denervation did not change final relaxation to SNP in the hypertensive group, we observed a right up shift in HD group (green up-side down triangles) at lower concentrations when compared to HS (blue triangles). Also, in both SNP and Ach-induced relaxation the curve shifted to control values (green upside-down triangles vs. yellow circles). More importantly is the fact that hypertensive sham rats showed a contractile response in the three last doses of the Ach curve, indicating endothelial dysfunction, which did not occur in hypertension animals undergoing renal denervation. Endothelium-dependent and endothelium-independent relaxation in absolute values are presented as supplementary data (see supplementary Fig. S2).
RDN effects on aortic contractile response
Figure 5 represents aortic contractile response when vessel rings were exposed to a concentration–response curve to phenylephrine (α1-agonist). Yellow circles represent Wistar sham group (control). When denervated (red squares), Wistar rats showed a greater contractile response when compared to control, also represented by a greater maximal response (Emax, Table 1). The same behavior was observed in hypertensive animals; when denervated, SHR showed increased contractile response when compared to their control (blue triangles vs. green upside-down triangles). In summary, RDN increased the contractile response to phenylephrine for both normotensive and hypertensive rats, leading the latter to control values.
Concentration–response curve to phenylephrine. NS: normotensive sham (n = 6); ND: denervated normotensive (n = 9), HS: SHR sham (n = 5); HD: denervated SHR (n = 4). Data were analyzed by two-way ANOVA followed by Fisher post hoc test. Values are mean ± SEM. ANOVA: Interaction factor (I); Concentration factor (C); Groups factor (G); Matching (M). ####p < 0.0001 NS vs. ND; *p < 0.05; ***p < 0.001 HS vs. HD.
RDN effects in aorta tunica media
As shown in Fig. 6, tissue sections showed characteristics of the healthy aortic tunicae (intima, media and adventitia). No histologic abnormalities were observed in the aortic wall, neither fibrosis, nor alteration of the arrangement of elastic lamellae, nor necrotic areas. Furthermore, there was no significant difference in the thickness of aortic tunica media among the experimental groups.
Representative images obtained from picrosirius-stained transverse aortic tissue sections from normotensive rats submitted to sham surgery (NS) or to renal denervation (ND), sham-operated spontaneous hypertensive rats (HS) or spontaneous hypertensive rats undergoing renal denervation (HD). Picrosirius staining demonstrates collagen in red and shows the typical histological organization of a normal aorta in all sections. The tunica media (blue lines) shows thin collagenous fibers interspersed among organized layers of smooth muscle cells and elastic lamellae (arrowheads). The tunica adventitia (asterisks) typically display coarse collagen fibers. Note that there is no difference between the groups for aorta morphology. Scale bars represent 50 µm.
Discussion
Our main findings regarding the effects of bilateral acute renal denervation in spontaneously hypertensive rats were: (1) The Blood pressure was significantly reduced 4 days after renal denervation; (2) Urinary volume was increased 72 h after renal denervation and (3) Aortic vascular function was improved by renal denervation.
Although it has been well documented that renal denervation—induced by different kinds of techniques (e.g. perivascular radiofrequency ablation, chemical ablation)—is able to lower blood pressure in SHR17,18,19,20,21,22, the effects of acutely renal denervation have not previously been fully addressed. While we believe that all measures should be carried out at the same times (simultaneously) of the experiment timeline, this was not always possible from a logistic perspective. However, evidences show that the effects of kidney denervation were extended at all times when such measures were taken17,21. In this way, renal denervation effectiveness has been evaluated by our group by both liquid chromatography technique (HPLC) or BP lowering effects as describe previously23.
Winternitz et al. have reported that 7 days after renal nerve ablation, SHR reaches a systolic blood pressure similar to normotensive animals24. Nevertheless, we found that 4 days after the procedure, renal denervation was already able to reduce SBP in SHR (14.4% of reduction) while BP in normotensive rats remain unchanged. On the other hand, a shorter period of renal denervation (1 h) did not change arterial pressure in SHR, despite the important changes observed in the intrarenal function in the same period—e.g., increase in renal blood flow (RBF), improvement in the dynamic autoregulation of RBF and increase in RBF variability25.
Regarding the effects of renal denervation on renal function, it is well documented that renal denervation produces an increase in sodium and water excretion and a decrease in the renal vascular resistance in some mammalian species15,26,27,28,29. Also, denervation in normal rats does not impact renal hemodynamics30,31,32. However, controversies surround the instant changes in renal hemodynamic and excretory functions following acute renal denervation. In the present study we found that the urinary volume was increased in the first 72 h after renal denervation in hypertensive rats, without changing urine flow in the normotensive animals. It is possible that the renal function of SHR was improved and the intrarenal balance was also modified by renal denervation as already suggested by Dibona and Sawin25. In this sense, we suggest that the acute reduction in the BP induced by renal denervation in the SHR is mediated—at least in part—by the increase in urinary volume. It has been proposed that a number of mechanisms—apart from renal function improvements—may underlie the beneficial effects of renal denervation on attenuation of hypertension. In this way, in our study SHR exhibited: Impaired baroreflex sensitivity33,34, increased renal sympathetic nerve activity35,36, decreased HR variance37 and autonomic imbalance38,39 which may also have been changed by renal denervation.
Heart rate variability (HRV) was the first non-invasive methodology extensively used to evaluate autonomic modulation of the sinus node in normal subjects and in patients with a range cardiac and non-cardiac diseases and to identify patients at increased risk for cardiac mortality40. Spectral analysis allows the identification and quantification of the major oscillations that characterize HRV particularly under resting controlled conditions. Interest in this approach has long been driven by the possibility of correlating short-term spectral components to neural discharge41,42 and of obtaining indirect information on neural modulation of the sinus node. Thus, HRV provides prognostic information to some diseases in which autonomic nervous system is involved43.
In the present study, RDN was able to increase both RMSSD and HF band—which are thought to be representative of cardiac parasympathetic modulation—in SHR rats; suggesting an increase in the vagal modulation induced by renal denervation. Interestingly, LF (sympathetic activity), was also increased in SHR, demonstrating an increase in total heart rate modulation, as confirmed by HRVar. We are aware of other possible mechanisms involved in LF band. One of the most probable confounding factors is the vascular volume change; it has been long acknowledge that volume withdrawal by hemodialysis, for example, may reduce LF modulation44. However, in our study, the HD group presented a higher volume excretion associated with higher LF levels, giving us more confidence about the sympathetic representativity role of LF band in this model. In addition, the RDN did not modify either HF or LF band in normotensive animals, suggesting that the removal of renal nerves is able to alter the autonomic control only in hypertensive animals presenting an impairment in the autonomic system.
Although SHR exhibited impaired baroreflex sensitivity and it has been suggested that it may be improved by autonomic modulation and a lower blood pressure34,45, we found no difference in alpha index, a marker of baroreflex sensitivity after renal denervation.
On the other hand, it has been shown that vascular dysfunction plays an important role in the SHR hypertension state. Endothelial dysfunction is characterized by decreased nitric oxide (NO) bioavailability and consequent impairment of endothelium-dependent relaxation to acetylcholine. Since this neurotransmitter needs an intact endothelium to induce relaxation, any endothelial dysfunction may impair this response46,47,48.
Spontaneously hypertensive rats presents key alterations in endothelial function49,50 along with impaired endothelium-dependent relaxation in aorta, femoral arteries and mesenteric resistance arteries51,52,53,54. Studies involving humans have found that impaired endothelial function may be strongly associated with increased cardiovascular risk and resistant hypertension55. Forearm endothelial dysfunction has been suggested as a marker of future cardiovascular events in patients with essential hypertension56. Furthermore, the severity of hypertension was positively associated with the degree of endothelial function impairment in The Framingham Heart Study57. Taking into account that high activity of sympathetic nerves may impair vascular endothelial function58,59, renal nerve removal may restore this function. Indeed, Yong Wang and colleagues, have demonstrated that RND may improve endothelial dysfunction in a rat model of type 2 diabetes mellitus with insulin resistance60. In the current study, SHR presented an impaired endothelium-dependent relaxation as well as a sustained vasoconstrictor response on the three last Ach concentrations. However, RDN-treated hypertensive rats exhibited proper endothelium-dependent relaxation (not different from the control group, NS), suggesting that renal denervation was able to improve endothelial function in SHR rats 7–10 days after the intervention. Although a left down shift was observed in normotensive RDN-treated rats, no endothelial dysfunction was found, since curve behavior was similar to control, with corresponding final relaxation and no vasoconstriction at any concentration.
Because endothelial function is also highly dependent on nitric oxide (NO) bioavailability61, we challenged aortic rings to a concentration–response curve to SNP (nitric oxide donor that leads to an endothelium-independent relaxation), whose effect is attributed to its direct action on the vascular smooth muscle62. SNP concentration–response curve demonstrated that RDN abolished the difference between hypertensive and normotensive rats, suggesting that renal nerve removal improved NO bioavailability in hypertensive individuals. These findings corroborates a study carried out by Patel et al., who found that renal denervation was able to restore neuronal NO synthase (nNos) down regulation within paraventricular nucleus in rats with heart failure63. They also corroborate an investigation undertaken by Yong Wang et al., who reported significantly NO level increases after RDN in a rat model of type 2 diabetes mellitus with insulin resistance60. All the conditions mentioned above (hypertension, heart failure, type 2 diabetes) are often associated with sympathetic nervous system hyperactivity64,65,66,67,68. In this context, is likely that in the currently study, NO bioavailability is at some level being modulated by sympathetic nervous system. In normotensive denervated rats, not only a left-down shift in the curve was seen, but also a greater sensitivity to SNP, assessed by half-maximal response—logED50 (Table1). Nevertheless, the current study cannot discriminate whether logED50 value is due a greater sensitivity to SNP or due an increase in NO bioavailability. Interestingly, although NO bioavailability may be increased in RDN-treated rats, phenylephrine (α1-receptor agonist) evoked greater contractile response in both Wistar and SHR. It is possible that this increase may be associated with a previously described contractile potential of NO69.
SHR rats have reduced aorta responses to different vasoconstrictors such as norepinephrine77, phenylephrine, angiotensin II, endothelin-1 and urotensin-II70. In the present study, we demonstrated contractile activity induced by phenylephrine, and we found a lower response in hypertensive sham animals compared to Wistar rats. In the other hand, we observed a higher contractility induced by renal denervation in both hypertensive and normotensive animals. Studies have suggested that renal denervation may lead to an augmentation in the expression of α1-adrenoceptors, which in turn increases the response to neural and adrenergic stimuli71,72. The augmented contractile response to phenylephrine in hypertensive RDN-treated rats could be due to the increased sensitivity of these adrenergic receptors against the reduction of peripheral sympathetic activity promoted by renal denervation73. This response is likely to be associated with a different baseline tone between normotensive and hypertensive rats.
Although it has been suggested that aorta from SHR undergo early remodeling that leads to reduced contractility in vitro70, our data do not support this hypothesis, since we observed no difference in aorta tunica media layer thickness among groups.
Hypertensive individuals present vascular fibrosis and increased intima-media relationship, leading to an increased risk of cardiovascular events74. Thus, the degree of artery remodeling has a prognostic value in these individuals. Santos et al. have found outward hypertrophic remodeling and increased elastic fibers content on aortas of 9 month SHR rats75. Honl et al. have shown that renal denervation prevented reduction of aortic distensibility in atherosclerosis prone ApoE‑deficient rats 8 weeks after intervention76. In humans, data from a multi-center trial showed that aortic distensibility is improved 6 months after RDN regardless of the BP response to the intervention77. It should be emphasized that our animal vessels were evaluated 7 days after RDN. As we assessed acute response to renal denervation, a higher degree of remodeling would probably be found in older animals for chronic response.
Conclusion
Spontaneously hypertensive rats had impaired endothelial function, as demonstrated by SNP, Ach and Phe concentration–response curves. Renal denervation normalized either dependent and independent—endothelium vasorelaxation in SHR and improved Phe contraction in both SHR and normotensive rats. The changes found in aorta responses may shed new light on the effects of renal denervation. We suggest that α1-adrenoreceptors and nitric oxide bioavailability may be the key mechanisms involved in this process and they possibly play a critical role in vascular changes after renal nerve removal, but new assessments may clarify this hypothesis.
Finally, acute responses to RDN indicate that the fall in BP is probably associated with the increased urinary volume, which may also have contributed to aortic functional changes. Baroreflex set point shifting may have participating to new BP values adjustments.
Materials and methods
Bioethical statement
We declare that all methods used in this protocol were carried out in accordance with relevant guidelines and regulations. All experiments were carried out after approved by the Ethical Committee for Animal Use from Faculdade de Medicina da Universidade de São Paulo (FMUSP) and the Research Ethics Committee of the Universidade Federal de São Paulo (UNIFESP) under protocol number 125/14 and 9324210514 respectively.
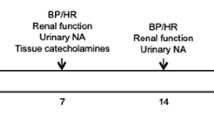
Experimental protocol
To evaluate the autonomic modulation of the circulation after renal nerves ablation, male Wistar and SHR rats were divided in four experimental groups; NS (normotensive + sham surgery), ND (normotensive + RDN surgery), HS (hypertensive + sham surgery), HD (hypertensive + RDN surgery). Metabolic parameters and blood pressure were evaluated 72 h and 4 days after surgery respectively. Blood pressure records were used for hemodynamic measurements and autonomic evaluation, as described below. At the end of the protocol the animals were euthanized through anesthetic overdose and the aorta function assessed using a wire myograph (DMT 620 M). Aortas were collected for histological analysis. The timeline and schedule of the protocol is illustrated in Fig. 7.
Animals
Male Wistar and spontaneously hypertensive rats (300–450 g, aged 12 weeks) were obtained from the Center for the Development of Experimental Models for Biology and Medicine (CEDEME). The animals were kept in individual cages, housed in the Laboratório de Hipertensão Experimental of Instituto do Coração/FMUSP, at room temperature (22–24 °C) and under controlled lighting, in a light/dark cycle (12 h). They were given access to rat chow and water ad libitum. The animals were randomly assigned into 4 (four) experimental groups: Wistar normotensive rats undergoing sham surgery (NS, n = 7); Wistar normotensive rats undergoing bilateral renal denervation (ND, n = 10); spontaneously hypertensive rats undergoing sham surgery (HS, n = 6), and spontaneously hypertensive rats undergoing bilateral renal denervation (HD, n = 8).
Renal denervation (RDN)
The RDN surgical procedure was adapted and validated by Oliveira et al.6. The animals were fasted for eight hours before the procedure and then anesthetized with isoflurane 2.5% in a 0.8 L/min of O2 flow. A trichotomy was performed on the right flank along with the cleansing of the site with 70% ethyl alcohol. The method consisted in placing the animal in the lateral decubitus position and after an incision in the left flank and identification of the kidney, it was folded in such a way as to expose the region of the aorta and renal vein. The section of renal nerves was then removed from the adventitia around the vessels using an iris clamp and ophthalmic scissors, with subsequent general cleansing of the extension—from the abdominal aorta to the kidney—in order to avoid any remaining nerve fibers. The same procedure was performed on the left side. The entire procedure was carried out with the use of magnifying glass and field magnification of 16× (M900, DF Vasconcellos).
The animals undergoing sham surgery had the renal artery and vein region exposed, followed by mild manipulation with a cotton tip. The incision suture was performed in two stages: suture of the muscular layer and skin suture, both using 4.0 nylon thread.
Metabolic parameters
Twenty-four hours after renal denervation, the animals were placed in individual metabolic cages for measuring metabolic parameters, such as water, urinary excretion, chow intake and feces. During the first 24 h, the animals were adapted to the housing conditions, and the data were collected over the previous 24 h.
Catheterization
When removed from metabolic cages, animals were anesthetized with 2.5% isoflurane in a 0.8 L/min of O2 flow and femoral artery and vein were catheterized as previously described78 to allow blood pressure recording and drugs infusion respectively.
Hemodynamic assessments
Heart rate and blood pressure evaluation
BP measurement was performed 24 h after the catheterization procedure (4 days after RDN).
During blood pressure recording, the animals remained awake and allowed to move freely in the cage. BP signals were recorded over a period of 30 min on a microcomputer equipped with a data acquisition system (Windaq, 2KHz, DATAQ Instruments, Akron, OH, USA) to obtain pressure pulses, beat-to-beat (with a sampling frequency of 4000 Hz per channel) for the assessment of systolic blood pressure (SBP), diastolic blood pressure (DBP), mean blood pressure (MBP) and heart rate (HR). HR values were derived from the pulsatile BP signal.
Autonomic balance assessment
Heart rate, blood pressure variability and baroreflex sensitivity
Systolic blood pressure (SBP) and Heart Rate (HR) variability were analyzed in time domain, which involved calculating the mean values of the pulse interval and SBP. Variability of these same variables was quantified by standard deviation, variances and the square root of the sum of the squares of the consecutive pulse interval differences (RMSSD). For analysis in frequency domain, a spectral analysis of the basal registers was performed using the Fast Fourier Transform (FFT) method. Power was obtained using time series derived from pulse interval and blood pressure, with a 512-point Hanning window and 50% overlap (CardioSeries v2.4). The powers for the low frequency bands (LF, 0.20–0.75 Hz, sympathetic modulation) and high frequency (HF, 0.75–3.0 Hz, parasympathetic modulation) were calculated by integrating the power in the bands of interest and presented as absolute values, percentages and were then normalized. For normalization, the potencies of the LF and HF bands were divided by the subtracted power variance in the very low frequency band79. The coupling between pulse interval and systolic blood pressure was estimated by the coherence function. A coherence value (K) greater than 0.5 was considered significant.
Baroreflex sensitivity was measured through alpha index of LF band, calculated by the square root of the ratio between the absolute value of LF PI by the absolute value of LF SBP, correlating the absolute values of LF for the heart with absolute LF for the vessels, when they were consistent with each other80.
Functional evaluation of the descending aorta
In order to evaluate the functional unit of the aorta, vascular reactivity was performed using a wire myograph (DMT 620 M). For this, the animals were euthanized with anesthetic overload (thiopental sodium 80 mg/kg) 7–10 days after RDN or sham surgeries. The thoracic aorta was removed, dissected from the connective tissue and cut into approximately 2 mm length rings, which were carefully transferred to organ baths in the myograph to preserve their endothelial and elastic integrity.
Conductance arteries with an inner diameter of approximately 1200 μm remained one hour at baseline in 5 ml of Krebs solution containing 118.6 mmol L−1 NaCl; 4.7 mmol L−1 KCl; 2.5 mmol L−1 CaCl2; 1.2 mmol L−1 MgSO4; 1.2 mmol L−1 KH2PO4; 25.1 mmol L−1 NaHCO3 and 11.1 mmol L−1 glicose; at 37º C, pH = 7.4 and under constant aeration with carbogenic mixture (95% O2 and 5% CO2). After stabilization period, aortic rings underwent a concentration–response curve to phenylephrine (Phe; 10–10 a 10−5 M), administered cumulatively in the bath to evaluate vasoconstrictor function and then washed with Krebs solution and left for 1 h for a new basal period. Subsequently, acetylcholine (Ach; 10–10 to 10−5 M) concentration–response curve was performed to evaluate endothelium-dependent vasodilation capacity and assess its integrity; vessels were previously contracted with 1 μM/L phenylephrine. Concentration–response curve was also performed on sodium nitroprusside to assess the endothelium-independent vasodilatory capacity; sodium nitroprusside (SNP; 10–10 a 10-5 M) was added to the bath solution on vessels previously contracted with 1 μM/L phenylephrine. All data were recorded by the Powerlab acquisition system and Chart 4.0 software (AD Instruments).
Half-maximal dose (logED50) and maximal response (Emax) to sodium nitroprusside, acetylcholine and phenylephrine were calculated as previously described81,82. The log dose that produced a 50% of maximal response (ED50) reflects sensitivity to the drugs; lower ED50 reflects higher sensitivity, whereas a higher ED50 reflects lower sensitivity.
Perfusion and tissues collection
Animals which were not included in vascular reactivity analysis were euthanized (7–10 days after RDN or sham surgeries) by anesthetic overload (thiopental sodium 80 mg/kg) followed by perfusion with physiological solution and Potassium Chloride (14 mmol/L). The tissues were then perfused with formaldehyde (10%) and the thoracic aorta collected for subsequent histological analysis.
Aorta medial layer thickness
Aorta tissues were stained in Picrossirius red, wich consisted of cutting the tissue using a microtome and then subjecting it to dehydration, whitening and inclusion it in paraffin. The cuts obtained were kept in an oven at 37ºC for 24 h and then the following steps took place: (1) Dewaxing in Xylol baths; (2) Hydration in decreasing alcohol baths (100–50%, followed by distilled water bath); (3) Immersion of tissues in Picrossirius red solution for one hour; (4) Washing under running water to remove excess dye; (5) Dehydration in increasing alcohol baths (50–100%); (6) Blade assembly.
Once the slides were assembled, they were placed under a microscope (Carl Zeiss AxioImager A.1) and observed at 200× magnification. The middle layer thickness of the descending aortas was evaluated by measuring the intima layer until the intersection of the middle layer with the adventitial layer (Quantimed). This measurement was performed at three different points in the vessel and was expressed as the mean of these values in micrometers (μm).
Statistical analysis
The results are presented as mean ± SEM. Two-way ANOVA was used to compare both denervation and blood pressure background factors, followed by Tukey’s post hoc test. For vascular reactivity, two-way ANOVA for repeated measures was performed followed by Fisher post hoc test. Values p < 0.05 were considered statistically significant.
References
Stella, A. & Zanchetti, A. functional role of renal afferents. Phys. Rev. 71, 659–682 (1991).
Schlaich, M. P. et al. renal denervation as a therapeutic approach for hypertension. Hypertension 54, 1195 (2009).
Schlaich, M. P., Sobotka, P. A., Krum, H., Lambert, E. & Esler, M. D. renal sympathetic-nerve ablation for uncontrolled hypertension. N. Engl. J. Med. 361, 932–934. https://doi.org/10.1056/nejmc0904179 (2009).
Dibona, G. F. sympathetic nervous system and the kidney in hypertension. Curr. Opinion Nephrol. Hypertens. 11, 197–200 (2002).
Dibona, G. F. neural control of the kidney: past, present, and future. Hypertension 41, 621–624. https://doi.org/10.1161/01.hyp.0000047205.52509.8a (2003).
Oliveira, V. L., Irigoyen, M. C., Moreira, E. D., Strunz, C. & Krieger, E. M. Renal denervation normalizes pressure and baroreceptor reflex in high renin hypertension in conscious rats. Hypertension 19, ii17-21 (1992).
Krum, H. et al. Percutaneous renal denervation in patients with treatment-resistant hypertension: final 3-year report of the symplicity HTN-1 study. Lancet 383, 622–629. https://doi.org/10.1016/s0140-6736(13)62192-3 (2014).
Esler, M. D. et al. Renal sympathetic denervation in patients with treatment-resistant hypertension (the symplicity htn-2 trial): a randomised controlled trial. Lancet 376, 1903–1909. https://doi.org/10.1016/s0140-6736(10)62039-9 (2010).
Kandzari, D. E. et al. Predictors of blood pressure response in the symplicity htn-3 trial. Eur. Heart J. 36, 219–227. https://doi.org/10.1093/eurheartj/ehu441 (2015).
Azizi, M. et al. Six-month results of treatment-blinded medication titration for hypertension control after randomization to endovascular ultrasound renal denervation or a sham procedure in the radiance-HTN solo trial. Circulation 139, 2542–2553. https://doi.org/10.1161/circulationaha.119.040451 (2019).
Böhm, M. et al. Efficacy of catheter-based renal denervation in the absence of antihypertensive medications (spyral htn-off med pivotal): a multicentre, randomised, sham-controlled trial. Lancet 395, 1444–1451. https://doi.org/10.1016/s0140-6736(20)30554-7 (2020).
Azizi, M. et al. Endovascular ultrasound renal denervation to treat hypertension (radiance-HTN solo): a multicentre, international, single-blind, randomised, sham-controlled trial. Lancet 391, 2335–2345. https://doi.org/10.1016/s0140-6736(18)31082-1 (2018).
Kandzari, D. E. et al. Effect of renal denervation on blood pressure in the presence of antihypertensive drugs: 6-month efficacy and safety results from the spyral htn-on med proof-of-concept randomised trial. Lancet 391, 2346–2355. https://doi.org/10.1016/s0140-6736(18)30951-6 (2018).
Sardar, P. et al. Sham-controlled randomized trials of catheter-based renal denervation in patients with hypertension. J. Am. College Cardiol. 73, 1633. https://doi.org/10.1016/j.jacc.2018.12.082 (2019).
Dibona, G. F. & Esler, M. Translational medicine: the antihypertensive effect of renal denervation. Am. J. Physiol. Regulat. Integrat. Comparat. Physiol. 298, r245-253. https://doi.org/10.1152/ajpregu.00647.2009 (2010).
Nakagawa, T. et al. Renal denervation prevents stroke and brain injury via attenuation of oxidative stress in hypertensive rats. J. Am. Heart Assoc. 2, e000375. https://doi.org/10.1161/jaha.113.000375 (2013).
Gao, J. et al. Sympathoinhibitory effect of radiofrequency renal denervation in spontaneously hypertensive rats with established hypertension. Am. J. Hypertens. 29, 1394–1401. https://doi.org/10.1093/ajh/hpw089 (2016).
Jiang, W. et al. Effect of renal denervation procedure on left ventricular hypertrophy of hypertensive rats and its mechanisms. Acta Cirurg. Bras. 27, 815–820. https://doi.org/10.1590/s0102-86502012001100012 (2012).
Wei, S. et al. Perivascular radiofrequency renal denervation lowers blood pressure and ameliorates cardiorenal fibrosis in spontaneously hypertensive rats. PLoS ONE 12, e0176888. https://doi.org/10.1371/journal.pone.0176888 (2017).
Skrzypecki, J., Gawlak, M., Huc, T., Szulczyk, P. & Ufnal, M. Renal denervation decreases blood pressure and renal tyrosine hydroxylase but does not augment the effect of hypotensive drugs. Clin. Exp. Hypertens. 39, 290–294. https://doi.org/10.1080/10641963.2016.1267191 (2017).
Wang, M. et al. Long-term renal sympathetic denervation ameliorates renal fibrosis and delays the onset of hypertension in spontaneously hypertensive rats. Am. J. Trans. Res. 10, 4042–4053 (2018).
Raikwar, N. et al. Renal denervation and cd161a immune ablation prevent cholinergic hypertension and renal sodium retention. Am. J. Physiol. Heart Circul. Physiol. 317, h517–h530. https://doi.org/10.1152/ajpheart.00234.2019 (2019).
Dagord Schaan, B. et al. Impact of renal denervation on renal content of glut1, albuminuria and urinary tgf-beta1 in streptozotocin-induced diabetic rats. Auton. Neurosci. Basic Clin. 104, 88–94. https://doi.org/10.1016/s1566-0702(02)00295-3 (2003).
Winternitz, S. R., Katholi, R. E. & Oparil, S. Role of the renal sympathetic nerves in the development and maintenance of hypertension in the spontaneously hypertensive rat. J. Clin. Investig. 66, 971–978. https://doi.org/10.1172/jci109966 (1980).
Dibona, G. F. & Sawin, L. L. Effect of renal denervation on dynamic autoregulation of renal blood flow. Am. J. Physiol. Renal Physiol. 286, f1209-1218. https://doi.org/10.1152/ajprenal.00010.2004 (2004).
Bencsáth, P., Bonvalet, J. & De Rouffignac, C. Tubular factors in denervation diuresis and natriuresis.
Bonjour, J. P., Churchill, P. C. & Malvin, R. L. Change of tubular reabsorption of sodium and water after renal denervation in the dog. J. Physiol. 204, 571–582. https://doi.org/10.1113/jphysiol.1969.sp008932 (1969).
Blake, W. D. & Jurf, A. N. Renal sodium reabsorption after acute renal denervation in the rabbit. J. Physiol. 196, 65–73. https://doi.org/10.1113/jphysiol.1968.sp008494 (1968).
Salman, I. et al. Quantification of acute renal denervation diuresis and natriuresis in sprague dawley and spontaneously hypertensive rats. Int. J. Pharmacol. https://doi.org/10.3923/ijp.2009.30.36 (2009).
Hollenberg, N. K. et al. Renal vascular tone in essential and secondary hypertension: hemodynamic and angiographic responses to vasodilators. Medicine 54, 29–44. https://doi.org/10.1097/00005792-197501000-00002 (1975).
Sadowski, J., Kurkus, J. & Gellert, R. Denervated and intact kidney responses to saline load in awake and anesthetized dogs. Am. J. Physiol. 237, f262-267. https://doi.org/10.1152/ajprenal.1979.237.4.f262 (1979).
Luippold, G., Beilharz, M. & Muhlbauer, B. Chronic renal denervation prevents glomerular hyperfiltration in diabetic rats. Nephrol. Dialysis Transpl. 19, 342–347. https://doi.org/10.1093/ndt/gfg584 (2004).
Hayashi, J. et al. Central attenuation of baroreflex by angiotensin ii in normotensive and spontaneously hypertensive rats. Am. J. Hypertens. 1, 15s–22s (1988).
Teng, X. et al. Gabaa receptor, KATP channel and l-type CA2+ channel is associated with facilitation effect of H2S on the baroreceptor reflex in spontaneous hypertensive rats. Pharmacol. Rep. 71, 968–975. https://doi.org/10.1016/j.pharep.2019.05.009 (2019).
Francisco, L. L., Sawin, L. L. & Dibona, G. F. Renal sympathetic nerve activity and the exaggerated natriuresis of the spontaneous hypertensive rat. Hypertension 3, 134–138. https://doi.org/10.1161/01.hyp.3.1.134 (1981).
Zhao, Y. et al. Superoxide anions modulate the performance of apelin in the paraventricular nucleus on sympathetic activity and blood pressure in spontaneously hypertensive rats. Peptides 121, 170051. https://doi.org/10.1016/j.peptides.2018.12.005 (2019).
Zamo, F. S. et al. Hemodynamic, morphometric and autonomic patterns in hypertensive rats-renin-angiotensin system modulation. Clinics (Sao Paulo) 65, 85–92. https://doi.org/10.1590/s1807-59322010000100013 (2010).
Murphy, C. A., Sloan, R. P. & Myers, M. M. Pharmacologic responses and spectral analyses of spontaneous fluctuations in heart rate and blood pressure in SHR rats. J. Auton. Nervous Syst. 36, 237–250. https://doi.org/10.1016/0165-1838(91)90047-7 (1991).
Moreira, T. S., Antunes, V. R., Falquetto, B. & Marina, N. Long-term stimulation of cardiac vagal preganglionic neurons reduces blood pressure in the spontaneously hypertensive rat. J. Hypertens. 36, 2444–2452. https://doi.org/10.1097/hjh.0000000000001871 (2018).
Lombardi, F. Clinical implications of present physiological understanding of hrv components. Cardiac Electrophysiol. Rev. 6, 245–249. https://doi.org/10.1023/a:1016329008921 (2002).
Electrophysiology task force of the european society of cardiology the north american society of, p. Heart rate variability. Circulation 93, 1043–1065, https://doi.org/10.1161/01.cir.93.5.1043 (1996).
Akselrod, S. et al. Power spectrum analysis of heart rate fluctuation: a quantitative probe of beat-to-beat cardiovascular control. Science 213, 220–222. https://doi.org/10.1126/science.6166045 (1981).
Singh, J. P. et al. Reduced heart rate variability and new-onset hypertension. Hypertension 32, 293 (1998).
Ferrario, M. et al. Effects of fluid overload on heart rate variability in chronic kidney disease patients on hemodialysis. BMC Nephrol. 15, 26. https://doi.org/10.1186/1471-2369-15-26 (2014).
Alves, N. F., Porpino, S. K., Monteiro, M. M., Gomes, E. R. & Braga, V. A. Coconut oil supplementation and physical exercise improves baroreflex sensitivity and oxidative stress in hypertensive rats. Appl. Physiol. Nutr. Metab. 40, 393–400. https://doi.org/10.1139/apnm-2014-0351 (2015).
Izzard, A. S., Bund, S. J. & Heagerty, A. M. Myogenic tone in mesenteric arteries from spontaneously hypertensive rats. Am. J. Physiol. 270, h1-6. https://doi.org/10.1152/ajpheart.1996.270.1.h1 (1996).
Furchgott, R. F. & Zawadzki, J. V. The obligatory role of endothelial cells in the relaxation of arterial smooth muscle by acetylcholine. Nature 288, 373–376 (1980).
Watson, T. et al. endothelial progenitor cells, endothelial dysfunction, inflammation, and oxidative stress in hypertension. Antioxidants Redox Signal. 10, 1079–1088. https://doi.org/10.1089/ars.2007.1998 (2008).
Lüscher, T. F. & Vanhoutte, P. M. Endothelium-dependent contractions to acetylcholine in the aorta of the spontaneously hypertensive rat. Hypertension 8, 344–348. https://doi.org/10.1161/01.hyp.8.4.344 (1986).
Yang, D. et al. Oxygen-derived free radicals mediate endothelium-dependent contractions to acetylcholine in aortas from spontaneously hypertensive rats. Br. J. Pharmacol. 136, 104–110. https://doi.org/10.1038/sj.bjp.0704669 (2002).
Bernatova, I. et al. Endothelial dysfunction in spontaneously hypertensive rats: focus on methodological aspects. J. Hypertens. Suppl. 27, s27-31. https://doi.org/10.1097/01.hjh.0000358834.18311.fc (2009).
Mori, Y. et al. Effects of endothelium-derived hyperpolarizing factor and nitric oxide on endothelial function in femoral resistance arteries of spontaneously hypertensive rats. Hypertens. Res. 29, 187–195. https://doi.org/10.1291/hypres.29.187 (2006).
Luscher, T. F., Aarhus, L. L. & Vanhoutte, P. M. Indomethacin improves the impaired endothelium-dependent relaxations in small mesenteric arteries of the spontaneously hypertensive rat. Am. J. Hypertens. 3, 55–58 (1990).
Konishi, M. & Su, C. Role of endothelium in dilator responses of spontaneously hypertensive rat arteries. Hypertension 5, 881–886 (1983).
Quinaglia, T. et al. Non-dipping pattern relates to endothelial dysfunction in patients with uncontrolled resistant hypertension. J. Human Hypertens. 25, 656–664. https://doi.org/10.1038/jhh.2011.43 (2011).
Perticone, F. et al. Prognostic significance of endothelial dysfunction in hypertensive patients. Circulation 104, 191–196. https://doi.org/10.1161/01.cir.104.2.191 (2001).
Benjamin, E. J. et al. Clinical correlates and heritability of flow-mediated dilation in the community: the framingham heart study. Circulation 109, 613–619. https://doi.org/10.1161/01.cir.0000112565.60887.1e (2004).
Joyner, M. J., Charkoudian, N. & Wallin, B. G. A sympathetic view of the sympathetic nervous system and human blood pressure regulation. Exp. Physiol. 93, 715–724. https://doi.org/10.1113/expphysiol.2007.039545 (2008).
Bruno, R. M. et al. Sympathetic regulation of vascular function in health and disease. Front. Physiol. https://doi.org/10.3389/fphys.2012.00284 (2012).
Wang, Y. et al. Renal denervation improves vascular endothelial dysfunction by inducing autophagy via AMPK/MTOR signaling activation in a rat model of type 2 diabetes mellitus with insulin resistance. Acta Diabetol. 57, 1227–1243. https://doi.org/10.1007/s00592-020-01532-6 (2020).
Wilkinson, I. B. et al. Nitric oxide regulates local arterial distensibility in vivo. Circulation 105, 213–217. https://doi.org/10.1161/hc0202.101970 (2002).
Harrison, D. G. & Bates, J. N. The nitrovasodilators. New ideas about old drugs. Circulation 87, 1461–1467. https://doi.org/10.1161/01.cir.87.5.1461 (1993).
Patel, K. P., Xu, B., Liu, X., Sharma, N. M. & Zheng, H. Renal denervation improves exaggerated sympathoexcitation in rats with heart failure: a role for neuronal nitric oxide synthase in the paraventricular nucleus. Hypertension 68, 175–184. https://doi.org/10.1161/hypertensionaha.115.06794 (2016).
Schaan, B. D. et al. Sympathetic modulation of the renal glucose transporter GLUT2 in diabetic rats. Auton. Neurosci. Basic Clin. 117, 54–61. https://doi.org/10.1016/j.autneu.2004.11.001 (2005).
Straznicky, N. E. et al. Neuroadrenergic dysfunction along the diabetes continuum: a comparative study in obese metabolic syndrome subjects. Diabetes 61, 2506–2516. https://doi.org/10.2337/db12-0138 (2012).
Sharp, T. E. 3rd. et al. Renal denervation prevents heart failure progression via inhibition of the renin-angiotensin system. J. Am. College Cardiol. 72, 2609–2621. https://doi.org/10.1016/j.jacc.2018.08.2186 (2018).
Grassi, G. & Ram, V. S. Evidence for a critical role of the sympathetic nervous system in hypertension. J. Am. Soc. Hypertens. 10, 457–466. https://doi.org/10.1016/j.jash.2016.02.015 (2016).
Hill, L. K. & Thayer, J. F. The autonomic nervous system and hypertension: ethnic differences and psychosocial factors. Curr. Cardiol. Rep. 21, 15. https://doi.org/10.1007/s11886-019-1100-5 (2019).
Lefebvre, R. A. & Barthó, L. Mechanism of nitric oxide-induced contraction in the rat isolated small intestine. Br. J. Pharmacol. 120, 975–981. https://doi.org/10.1038/sj.bjp.0700996 (1997).
Gendron, G., Gobeil, F. Jr., Morin, J., Dorleans-Juste, P. & Regoli, D. Contractile responses of aortae from WKY and SHR to vasoconstrictors. Clin. Exp. Hypertens 26, 511–523. https://doi.org/10.1081/ceh-200031826 (2004).
Ramchandra, R., Barrett, C. J., Guild, S. J. & Malpas, S. C. Is the chronically denervated kidney supersensitive to catecholamines?. Am. J. Physiol. Regul Integr. Comparat. Physiol. 282, r603-610. https://doi.org/10.1152/ajpregu.00404.2001 (2002).
Abdulla, M. H. et al. Effect of acute unilateral renal denervation on renal hemodynamics in spontaneously hypertensive rats. Auton. Autacoid Pharmacol. 28, 87–94. https://doi.org/10.1111/j.1474-8673.2008.00421.x (2008).
Khan, A. H., Sattar, M. A., Abdullah, N. A. & Johns, E. J. Influence of cisplatin-induced renal failure on the alpha(1)-adrenoceptor subtype causing vasoconstriction in the kidney of the rat. Eur. J. Pharmacol. 569, 110–118. https://doi.org/10.1016/j.ejphar.2007.04.063 (2007).
Schiffrin, E. L. Resistance arteries as endpoints in hypertension. Blood Pressure Suppl 2, 24–30 (1997).
Fernandes-Santos, C., De Souza Mendonca, L. & Mandarim-De-Lacerda, C. A. Favorable cardiac and aortic remodeling in olmesartan-treated spontaneously hypertensive rats. Heart Vessels 24, 219–227. https://doi.org/10.1007/s00380-008-1104-3 (2009).
Hohl, M. et al. Modulation of the sympathetic nervous system by renal denervation prevents reduction of aortic distensibility in atherosclerosis prone apoe-deficient rats. J. Transl. Med. 14, 167. https://doi.org/10.1186/s12967-016-0914-9 (2016).
Stoiber, L. et al. Renal sympathetic denervation restores aortic distensibility in patients with resistant hypertension: data from a multi-center trial. Clin. Res. Cardiol. 107, 642–652. https://doi.org/10.1007/s00392-018-1229-z (2018).
Dos Santos, F., Moraes-Silva, I. C., Moreira, E. D. & Irigoyen, M. C. The role of the baroreflex and parasympathetic nervous system in fructose-induced cardiac and metabolic alterations. Sci. Rep. 8, 10970. https://doi.org/10.1038/s41598-018-29336-3 (2018).
Soares, P. P. et al. Effects of rat sinoaortic denervation on the vagal responsiveness and expression of muscarinic acetylcholine receptors. J. Cardiovasc. Pharmacol. 47, 331–336. https://doi.org/10.1097/01.fjc.0000205982.67653.26 (2006).
Pagani, M. et al. Changes in autonomic regulation induced by physical training in mild hypertension. Hypertension 12, 600–610. https://doi.org/10.1161/01.hyp.12.6.600 (1988).
Sprick, J. D. et al. Vascular α1-adrenergic sensitivity is enhanced in chronic kidney disease. Am. J. Physiol. Regulat. Integrat. Compar. Physiol. 317, r485–r490. https://doi.org/10.1152/ajpregu.00090.2019 (2019).
Pernomian, L., Gomes, M. & De Oliveira, A. Balloon catheter injury abolishes phenylephrine-induced relaxation in the rat contralateral carotid. Br. J. Pharmacol. 163, 770–781. https://doi.org/10.1111/j.1476-5381.2011.01275.x (2011).
Acknowledgements
This research was jointly funded by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior—CAPES (88882.179920/2018-01), Fundação de Amparo à Pesquisa do Estado de São Paulo—FAPESP (2018/19006-2) and Conselho Nacional de Desenvolvimento Científico e Tecnológico—CNPq (427892/2018-0).
Author information
Authors and Affiliations
Contributions
N.J.D.M. performed the experiments, analyzed the results and wrote the manuscript, F.S. analyzed the hemodynamics measurements, E.D.M. was in charge of the blood pressure records, D.F. contributed to the myograph experiments, L.E.S. performed the renal denervation surgery, M.B.S. performed catheterization surgery, G.S.L and I.C.M.S. improved the manuscript, E.G.C was responsible for aorta histology analyzes and M.C.I designed the protocol, supervised and reviewed the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Moreira, N.J.D., dos Santos, F., Moreira, E.D. et al. Acute renal denervation normalizes aortic function and decreases blood pressure in spontaneously hypertensive rats. Sci Rep 10, 21826 (2020). https://doi.org/10.1038/s41598-020-78674-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-78674-8
- Springer Nature Limited
This article is cited by
-
Advances on the Experimental Research in Resistant Hypertension
Current Hypertension Reports (2024)
-
Possible organ-protective effects of renal denervation: insights from basic studies
Hypertension Research (2023)
-
Enteral administration of the protease inhibitor gabexate mesilate preserves vascular function in experimental trauma/hemorrhagic shock
Scientific Reports (2023)