Abstract
Oxidative stress (OS) is associated with the onset of prostate cancer (PCa). The aims of this study are to examine whether OS biomarkers may be employed as external validating criteria for the diagnosis PCa. This case-control study recruited 204 subjects, 73 patients with PCa, 67 patients with benign prostate hyperplasia (BPH), and 64 healthy controls (HC) and assayed plasma prostate-specific antigen (PSA), protein thiol (−SH) groups, lipid hydroperoxides, carbonyl proteins (PCB), advanced oxidation protein products (AOPP), and total radical-trapping antioxidant parameter (TRAP). -SH groups were significantly and inversely associated with PSA levels. PCa was characterized by lowered -SH groups and red blood cell TRAP levels, and higher PSA, AOPP and PCB levels as compared with BPH and HC. Support vector machine with 10-fold cross-validation showed that PSA values together with -SH groups, PCB and AOPP yielded a cross-validation accuracy of 96.34% for the differentiation of PCa from BPH and HC. The area under the ROC curve using PSA and -SH differentiating PCa from BPH and controls was 0.945. Moreover, lowered -SH, but not PSA, are associated with PCa metastasis and progression. Inflammatory biomarkers were not associated with PCa or BPH. PCa, its progression and metastatic PCa are characterized by lowered antioxidant defenses, especially lowered thiol groups, and increased oxidative stress toxicity, suggesting that these processes play a key role in the pathophysiology of PCa. An algorithm based on -SH and PSA values may be used to differentiate patients with PCa from those with BPH and controls.
Similar content being viewed by others
Introduction
PCa is the second most common malignancy in men and PCa and benign prostatic hyperplasia (BPH) are the most frequent prostatic diseases in aging men. Ageing is the major risk factor for PCa and BPH while also a positive familial history of PCa1, genetic factors2,3, ethnicity4, lifestyle and nutritional factors5, and obesity6 confer risk to PCa. Chronic prostatic inflammation is a possible risk factor that may be associated with PCa and BPH7,8. Metabolic Syndrome (MetS) may be associated with BPH, but not PCa9, and with the more aggressive PCa phenotypes10.
Oxidative stress (OS) toxicity is one of the mechanisms that is associated with the onset of BPH11 and PCa12,13 and progression of the latter. In addition, increased age is also associated with activated OS pathways14. Reactive oxygen species (ROS) are associated with carcinogenesis through structural DNA damage, interaction with oncogenes or tumor suppressor genes and/or immunological mechanisms11,15. In addition, ROS could be responsible for the formation of DNA adducts, for example with malondialdehyde (MDA), a byproduct of the peroxidation of polyunsaturated fatty acids. Oxidative lesions, which are not repaired, can lead to mutations increasing the risk of carcinogenesis16. Some studies found increased levels of MDA in patients with PCa and BPH as compared with controls17,18.
ROS-induced oxidative damage is exacerbated by a decreased efficiency of antioxidant defense mechanisms16. The level of one of these antioxidants namely total thiol (−SH) groups is inversely associated with aging and PCa progression. -SH concentrations are significantly lower in PCa patients while aging is associated with a moderate reduction of -SH in BPH patients19.
In the early stages of PCa, the differential diagnosis between PCa and BPH is not an easy task20. Increased total prostate-specific antigen (tPSA) is the most frequently used laboratorial biomarker to identify prostatic changes21, although tPSA has only a moderate sensitivity to discriminate between PCa and BPH as well as for predicting increased risk of metastasis22. Therefore, it is of paramount importance to delineate novel biomarkers, which could differentiate PCa from BPH and indolent prostate cancer from the more aggressive phenotypes. Moreover, the examination of oxidative stress pathways may delineate the mechanisms that contribute to the pathogenesis or pathophysiology of PCa thereby providing new drug targets to treat PCa. In addition, the side-effects of treatment of indolent tumors may cause increased morbidity as well as worsening of the quality of life without improving overall global survival, whilst treatment delay may lead to incurable disease23.
Thus, the main goal of this study is to identify biomarkers of OS that could differentiate BPH and PCa. The second goal is to delineate the OS biomarkers, which may be used in the clinical practice as predictors of PCa above and beyond the effects of PSA.
Subjects and Methods
This is a case-control study that recruited 204 subjects, 73 patients with PCa (attending the Uro-Oncology Clinic of the Cancer Hospital, Londrina, Brazil), 67 patients with BPH (attending the Urology Clinic of the Evangelical Hospital of Londrina, Brazil), and 64 healthy volunteers (HC). Patients and controls were recruited from the same catchment area namely Londrina, Brazil. The age range of the participants was 35–69 years. The diagnosis PCa was made based on histological evaluation (positive biopsy results). Nine (12%) patients showed metastatic PCa. Moreover, the PCa group was subdivided according to the risk stratification National Comprehensive Cancer Network (NCCN) Guidelines24: AV group1: very low and low risk group; AV group2: favorable and unfavorable intermediate risk group; and AV group3: high and very high risk group. Exclusion criteria for normal controls included a prostate volume >30 cm3 (measured by transabdominal ultrasound) and tPSA >1.5 ng/mL, whereas BPH patients had prostate volume greater than 30 cm3. Exclusion criteria for patients and controls were: (a) treatments with anti-inflammatory drugs (except sporadic use of NSAIDs); (b) use of antioxidant supplements; (c) presence of immune-inflammatory disorders and acute or chronic infections; (d) a prior history of other cancers and; (e) chronic renal insufficiency.
MetS was defined following the Adult Treatment Panel III criteria namely three or more of the following five criteria are present: (1) waist circumference over 94 cm; (2) fasting triglyceride levels greater than or equal to 150 mg/dL; (3) high density lipoprotein (HDL) lower than 40 mg/dL; (4) blood pressure over 130/85 mmHg (or antihypertensive medication use) and; (5) fasting glucose levels greater than or equal to 100 mg/dL or the use of hypoglycemic medication25. Body weight was measured prior to blood collection, using electronic scales accurate to 0.1 kg, with patients wearing light clothing and no shoes; height was measured to a precision of 0.1 cm using a stadiometer. Body mass index (BMI) was calculated as weight (kg) divided by height (m) squared.
Written informed consent was given by all participants of this study. The Human Ethics Committee of the State University of Londrina approved the protocol (CAAE 56182916.7.0000.5231).
Laboratorial analysis
Fasting blood was sampled in the morning hours (8.00 a.m.) and in PCa patients blood was sampled one week before surgery. EDTA collecting tubes with a standard anticoagulant concentration (0.5 mL of EDTA for each 4.5 mL of the blood sample) were used to collect samples for biochemical and OS biomarker assays. Samples were centrifuged at 804 g for 15 min and stored in plasma and serum aliquots at −70 °C until used in laboratory tests.
The assays of total PSA (tPSA), free PSA (fPSA), and ferritin were determined using a chemiluminescent microparticle immunoassay (CMIA; Architect, Abbott Laboratory, Abbott Park, IL, USA). Uric acid (UA) was evaluated by a biochemical auto-analyser (Dimension Dade AR, Dade Behring, Deerfield IL, USA). The quantification of -SH of proteins was performed with spectrophotometry, according to the method described by Hu26. This technique is based on the reaction of the 2,2-dithiobisnitrobenzoic acid (DTNB) with the thiol group of proteins as described by Reznick and Packer27 and the results were expressed in μM. Lipid hydroperoxides (LOOH) were evaluated as described by Flecha et al.28. The results were expressed in relative light units (RLU). Plasma protein carbonyls (PCB) were measured with a spectrophotometric method based on the reaction of 2,4-dinitrophenylhydrazine with the carbonyl group, forming 2,4-dinitrophenylhydrazone, according to27. The results were expressed in nmol/mg of proteins. AOPP was determined according to the method of Witko-Sarsat et al.29. The values were expressed in μM/L of T-chloramine equivalent. TRAP (total radical-trapping antioxidant parameter) was measured using the methodology described by Repetto et al.30. This method detects hydro and liposoluble antioxidants in the plasma and TRAP results are expressed in μM of Trolox. Serum levels of ferritin, fPSA and tPSA were determined using a chemiluminescent microparticle immunoassay (CMIA; Architect, Abbott Laboratory, Abbott Park, IL, USA). Serum levels of C-reactive protein (CRP) were determined by high sensitive turbidimetry (C8000, Abbott Laboratory, Abbott Park, IL, USA). The values of white blood cell (WBC) and hemoglobin (Hb) were obtained using a hematological equipment (BC-6800, Mindray, Shenzhen, China) and erythrocyte sedimentation rate (ESR) was performed using automated equipment (Alifax, Polverara, Itália).
Statistics
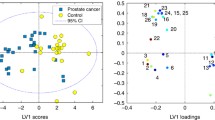
Analysis of variance was used to assess between-group differences in scale variables and analysis of contingency tables (Χ2-test) was used to check associations between nominal variables. We used binary logistic regression analysis to delineate the most significant variables predicting PCa versus controls and or BPH while adjusting for possible confounders (including age, MetS, BMI). Multivariate general linear model (GLM) analysis was used to assess the effects of explanatory variables (including diagnosis) on the biomarkers while controlling for possible confounders. Tests for between-subject effects were used to assess the effects of significant explanatory variables on the separate biomarkers. Model-estimated estimated marginal mean (SE) values were calculated based on the multivariate GLM analysis and protected post hoc analyses were employed to check differences between PCa, BPH and HC. We p-corrected results of multiple comparisons for false discovery rate31. Receiver Operating Characteristics (ROC) analysis was used to compute the area under the ROC curve (AUC ROC). Statistical analyses were performed using IBM SPSS Windows versions 22 and 25. Tests were 2-tailed, and an alpha level of 0.05 indicated a statistically significant effect. Support Vector Machine (SVM) with radial basis kernel function was used to compute the correctly classified PCa and control cases using biomarkers as explanatory variables (The Unscrambler, CAMO) after 10-fold crosss-validation.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
All the participants included in this study provided written informed consent.
Results
Demographic data
Table 1 shows the demographic, clinical and biomarker data in HC, BPH and PCa. BPH and PCa patients were somewhat older than normal controls while there were no significant differences in familial PCa history, BMI, smoking rate, hypertension, and diabetes between the three groups. There were significantly more non-Caucasian people in the PCa group as compared with the BPH and control groups, while BPH was associated with a greater rate of MetS as compared with controls. This table also shows the measurements of PSA and OS biomarkers in the three study groups. Table 1 shows the results of analyses of variance with protected post-hoc comparisons but without any adjustment for the effects of extraneous variables. Therefore, we would suggest to focus on Tables 2 and 3 to interpret the adjusted biomarker data.
The Electronic Supplementary File (ESF), Table 1 shows the measurements of Hb and immune-inflammatory biomarkers namely hsCRP, ESR, leukocytes, and ferritin. However, no significant differences in any of those biomarkers could be found among the three study groups.
Intercorrelation matrix between the variables
The intercorrelation matrix between the biomarkers showed that tPSA was significantly associated with LOOH in red blood cells (LOOHRBC) (r = 0.157, p = 0.028, n = 196), AOPP (r = 0.172, p = 0.014, n = 203), -SH groups (r = −0.527, p < 0.001, n = 204), and TRAPRBC (r = −0.298, p < 0.001, n = 151). Figure 1 shows the strong association between tPSA and -SH groups (r = −0.527, p < 0.001, n = 204). There was a significant correlation between fPSA and tPSA (r = 0.825, p < 0.001, n = 204), -SH groups (r = −0.422, p < 0.001, n = 204) and TRAPRBC (r = −0.243, p = 0.003, p = 151). Uric acid was significantly and positively correlated with TRAP in plasma (TRAPplasma) (r = 0.539, p < 0.001, n = 181), but less with TRAPRBC (r = 0.177, p = 0.030, n = 151). AOPP was significantly correlated with PCB (r = 0.211, p = 0.003, n = 201). There was only a modest correlation between TRAPplasma and RBCs (r = 0.200, p = 0.014, n = 151). tPSA and fPSA were not significantly associated with any of the immune-inflammatory variables (CRP, ferritin, ESR, WBCs). -SH groups were significantly associated with ESR (r = −0.279, p < 0.001, n = 194) and Hb (r = −0.334, p < 0.001, n = 195).
Differences in biomarkers between PCa, BPH and HC
Figure 2 shows the values of PSA/OS biomarkers (all in z values) in HC, BPH and PCa. Table 2 shows the results of multivariate GLM analysis which examines the association between diagnosis and the PSA/OS biomarkers while adjusting for age, BMI and MetS. The TRAP data were assessed separately because TRAP was measured in a subset only (which would yield a considerable lowered number of dfs in the multivariate GLM analyses). Also, the immune-inflammatory markers were entered separately because they reflect another construct.
Total and free PSA levels and oxidative stress biomarkers (all in z values) in healthy controls (HC), patients with Benign Prostate Hyperplasia (BPH), and prostate cancer (PCa). PSA: prostate-specific antigen. -SH: thiol. AOPP: advanced oxidized protein products. PCB: protein carbonyls. LOOH RBC: lipid hydroperoxides in red blood cells. TRAP: total radical-trapping antioxidant parameter.
Multivariate GLM analysis #1 shows that diagnosis was significantly associated with PSA/OS biomarkers with huge effect sizes for tPSA (0.467) and -SH groups (0.375), moderate effect sizes for fPSA (0.189) and AOPP (0.110), and low impact sizes for PCB (0.046), TRAPRBC (0.063) and LOOHRBC (0.034). All differences remained significant after p-correction. There were no significant differences in LOOHplasma, uric acid and TRAPplasma between the study groups.
Table 3 shows the model-generated estimated marginal means (in z scores) of the significant biomarkers as well as the results of post-hoc comparisons. tPSA and fPSA were significantly different between the three subgroups and increased from HC → BPH → PCa. -SH levels were significantly lower in PCa than in HC and BPH, whereas there were no significant differences between BPH and HC. AOPP was significantly increased in BPH and PCa as compared with HC, whereas PCB was higher in PCa than in HC and BPH. LOOHRBC (but not plasma) was significantly higher in both BPH and PCa than in HC while TRAPRBC (but not plasma) was significantly lower in PCa than in HC. There were no significant differences in the immune-inflammatory biomarkers CRP, WBCs, ESR, ferritin and Hb between the three study groups (F = 1.25, df = 10/362, p = 0.258) (see ESF Table 1). The ESF section 1 describes the possible effects of background variables (including the drug state) on the results.
Prediction of PCa using the biomarkers
Table 4 shows the results of binary logistic regression analyses with PCa as dependent variable and either BPH or BPH + HC as reference group. Regression #1 shows that PCa (versus BPH + HC) was significantly predicted using tPSA, -SH groups and age as explanatory variables (X2 = 153.09, df = 3, p < 0.001, Nagelkerke = 0.724; 85.8% of all cases were correctly classified with a sensitivity of 79.5% and a specificity of 89.3%). Without age (regression #2) a similar prediction was established (X2 = 149.47, df = 2, p < 0.001, Nagelkerke = 0.713; whereby 87.3% of all cases were correctly classified with a sensitivity of 82.2% and a specificity of 90.1%).
Regression #3 shows a somewhat better prediction of PCa using tPSA, -SH and PCB (X2 = 144.89, df = 3, p < 0.001, Nagelkerke = 0.761, 91.1% of all cases were correctly classified with a sensitivity of 85.7% and a specificity of 94.0%). The same three variables yielded also a good prediction (regression #4) of PCa versus BPH (X2 = 87.62, df = 3, p < 0.001, Nagelkerke = 0.676, 87.1% of all cases were correctly classified with a sensitivity of 87.3% and a specificity of 86.9%). Regression #5 shows that a familial history of PCa, ethnicity, PCB, SH and tPSA significantly predicted PCa versus BPH + HC (X2 = 162.79, df = 5, p < 0.001, Nagelkerke = 0.762; 89.1% of all cases were correctly classified with a sensitivity of 81.7% and a specificity of 93.1%). Age was not significant in this regression (p = 0.093).
Table 5 shows the results of ROC analyses discriminating PCa from BPH + HC or PCa from BPH. The best separation was obtained for the combination of a familial history of PCa, ethnicity, PCB, -SH and tPSA (area under the ROC curve 0.950), followed by the combined effects of tPSA and -SH (0.945), and tPSA, -SH and PCB (0.945).
Associations among tPSA and -SH groups and other PCa features
Subsequently, we have examined the associations between the biomarkers and other features of PCa, including metastasis, rectal examination, AV groups (risk stratification according to NCCN Guidelines), prostate size and ultrasound. Figure 3 shows the biomarkers in PCa patients with and without metastasis. -SH groups are significantly lower in PCa patients with (mean z score = −2.07 ∀0.24) than without (mean = −0.60 ∀0.10) metastasis (F = 32.57, df = 1/68, p < 0.001, partial eta squared = 0.324), whereas there are no significant differences in any of the other OS biomarkers or tPSA (F = 2.33, df = 1/68, p = 0.131). Moreover, ESR is increased (F = 7.42, df = 1/65, p = 0.008) and Hb decreased (F = 6.72, df = 1/65, p = 0.012) in patients with metastatic PCa. Table 4, regression 6 shows that lowered -SH groups are significantly associated with metastatic PCa versus PCa without metastasis (X2 = 36.42, df = 1, p < 0.001, Nagelkerke = 0.471, and sensitivity of 50.0% and specificity of 98.4).
Differences in total PSA and oxidative stress biomarkers between patients with prostate cancer metastasis (metastatic PCa) versus patients without metastasis (No). PSA: prostate-specific antigen. SH: thiol. AOPP: advanced oxidized protein products. PCB: protein carbonyls. LOOH RBC: lipid hydroperoxides in red blood cells. CRP: high sensitivity C-reactive protein. WBC: white blood cells. ESR: erythrocyte sedimentation rate. Hb: hemoglobin.
Figure 4 shows the biomarkers in subjects (PCa, BPH and HC combined) examining a suspicious digital rectal examination versus a normal examination. tPSA (F = 30.71, df = 1/198, p < 0.001, partial eta squared = 0.134), -SH groups (F = 19.38, df = 1/198, p < 0.001, partial eta squared = 0.126) and AOPP (F = 13.59, df = 1/198, p < 0.001, partial eta squared = 0.065) were significantly associated with a suspicious digital rectal examination. Table 4, Regression #7 shows that -SH groups, tPSA, AOPP and MetS may predict a suspicious digital rectal examination (X2 = 49.56, df = 4, p < 0.001, Nagelkerke = 0.336). However, after bootstrapping (2000 bootstraps) tPSA was no longer significant (p = 0.06), while -SH groups, AOPP and MetS remained significant.
shows the biomarkers in those with a suspicious digital rectal examination versus a normal examination (See Fig. 3 for abbrevations).
Figure 5 shows that the PCa AV risk group3 is accompanied by lower -SH levels as compared with PCa AV risk groups 1 + 2 (F = 16.41, df = 1/68, p < 0.001, partial eta squared = 0.194) while there were no significant differences in tPSA between those groups (F = 0.01, df = 1/68, p = 0.130, partial eta squared = 0.033). Moreover, patients in PCa AV risk group 3 showed lower Hb levels (F = 5.00, df = 1/65, p = 0.029) and higher ESR levels (F = 6.45, df = 1/65, p = 0.014) than patients in PCa AV risk groups 1 + 2.
Shows that AV group 3 (risk group3) is characterized by lowered -SH group values (F = 8.91, df = 1/60, p = 0.004) and higher ESR (F = 9.03, df = 1/60, p = 0.004) than AV groups 1 + 2 (See Fig. 3 for abbreviations).
Table 6 shows the results of multiple regression analysis predicting prostate volume (in cubic centimeter). The best prediction of prostate volume was obtained using age in combination with LOOHRBC explaining 34.0% of the variance (Regression #1), whilst -SH levels were also significant and explained 9.1% of the variance (Regression #2). We found that 15.5% of the variance in ultrasound volume was explained by age and LOOHplasma combined (Regression #3). Regression #4 shows that in PCa patients, tPSA was predicted by lower -SH levels, and increased PCB and prostate volume (27.5% of the variance). Regression #5 shows that in all participants combined, tPSA was significantly predicted by ethnicity, age and familial history of PCa (13.5% of the variance).
Discussion
The main findings of this study are: (a) PCa is characterized by lowered plasma -SH groups and red blood cell TRAP levels and higher plasma AOPP and PCB levels as compared with BPH and control subjects, and (b) OS biomarkers may be used together with tPSA as external validating criterion for PCa. Importantly, 10-fold cross-validation showed that tPSA and fPSA values together with -SH, PCB and AOPP yielded a validation accuracy of 96.34% when differentiating PCa from BPH and HC. Lowered -SH levels show an adequate diagnostic performance for PCa with an AUC ROC of 0.881 (versus controls and BPH) while lowered -SH groups combined with higher tPSA values yielded an area under the ROC curve of 0.945.
Antioxidant Defenses in PCa and BPH
SH-disulphide homeostasis is crucial in several processes such as antioxidant defense, detoxification, cell signaling, transcription, protein regulation and apoptosis32,33. Previous studies reported decreased -SH groups in advanced non-small cell lung cancer34 and advanced gastric adenocarcinoma35. However, a previous study found an increase of non-protein -SH levels (GSH, Reduced Glutathione) in plasma and erythrocytes in PCa patients, mainly in presence of bone metastasis. The authors suggested that the increased levels could be a compensatory mechanism to prevent tissue damage caused by oxidative stress36. In plasma, protein -SH levels are more abundant than glutathione, representing approximately 70% of total intracellular pool of reduced -SH. However, GSH levels in plasma are very low and do not reflect all -SH groups37. Interestingly, in our study there was a strong association between total PSA and -SH levels. One hypothesis is that increased PSA peptidase activity could have induced lowered -SH levels. However, since PSA activity involves serine proteinase and not cysteinases this is less plausible38,39.
Some studies reported decreased antioxidant defenses, other than -SH groups, in PCa and BPH19 including superoxide dismutase (SOD) and catalase in patients with PCa metastasis36,40. However, few reports measured total antioxidant capacity, which reflects the cumulative effects of different antioxidant defenses in plasma thereby providing a more integrated parameter of antioxidant defenses41. In this respect, we found that TRAP in erythrocytes, but not plasma, was decreased in patients with PCa as compared with HC. A previous study demonstrated that antioxidant status, evaluated by TEAC (Trolox Equivalent Antioxidant Capacity), was reduced in plasma of PCa patients when compared with BPH and HC42. Pande et al.13 reported that patients with advanced stages of PCa had lower TEAC, suggesting increased antioxidant consumption.
Lipid and protein oxidation in PCa and BPH
The results of the present study did not show a significant increase in the lipoperoxidation marker LOOH either in plasma or red blood cells. Our data are in agreement with a previous study, which showed no difference in lipoperoxidation between PCa and BPH43. Previous studies on aldehyde formation (which is the consequence of lipid peroxidation) in prostate disease including TBARS (Thiobarbituric Acid Reactive Substances) and MDA yielded controversial results. TBARS in erythrocyte lysates was increased in BPH patients when compared with HC42,44 while MDA levels were higher in BPH patients than HC17,40,45,46 while there was a strong correlation between MDA and tPSA17. However, other studies found no differences in MDA levels in BPH patients as compared with controls47.
Our results showed increased levels of the protein oxidation indices in PCa namely increased PCB in PCa patients versus BPH, and increased AOPP in patients with PCa and BPH versus controls. PCB may be formed by the oxidation of a few amino acid side chains via the addition of aldehydes such as those generated from lipid peroxidation. PCB is an initial and reversible product from protein oxidation whilst AOPP is the final and irreversible product of protein oxidation. Pande et al.13 showed that PCB levels were higher in PCa patients as compared to HC although another case-control study reported no significant associations between PCa risk or aggressiveness and PCB48.
Prostatic inflammation as a result of infection, urine reflux, hormonal and immune dysbalances11,49 may be involved in the pathogenesis and progression of PCa by causing cell and DNA damage and promoting cellular turnover. Prostate tissue damage and oxidative stress generated from inflammation could lead to compensatory cellular proliferation with the resulting hyperplastic growth50. Nevertheless, in the present study, we did not find significant associations between oxidative stress biomarkers and inflammatory biomarkers including ferritin, ESR, and hsCRP. Moreover, these inflammatory biomarkers were not altered in PCa or BPH, suggesting that oxidative stress toxicity may be involved in the physiopathology of PCa independently of immune-inflammatory processes. As such, increased OS and lowered antioxidant defenses, including lowered -SH groups and TRAP as well as protein oxidation may be more important than immune-inflammatory processes in the pathophysiology of PCa.
Oxidative stress and staging of PCa
Interestingly, our study found that there was a significant association between a suspicious rectal examination and lowered levels of -SH groups and AOPP, whereas the association with tPSA was no longer valid after bootstrapping. Also, these findings suggest a pathogenic role of -SH groups and AOPP in PCa. As such, our algorithm comprising -SH groups and tPSA may be used to differentiate BPH from PCa in subjects with suspicious digital rectal exam. Likewise, prostate volume was predicted by pre-surgery values of -SH groups and LOOH in red blood cells, but not tPSA. In this respect, increased levels of tPSA were significantly predicted by lowered -SH groups, increased PCB and prostate volume, indicating that -SH groups and OS processes are involved in BPH, cancer development and increased production of tPSA. Moreover, our results show that lowered -SH groups and Hb, and increased ESR, but not PSA, predict a high-risk phenotype as indicated by the association of -SH with metastatic PCa and AV risk group 3. Previously, it was shown that progressive stages in PCa are associated with a more detrimental redox status13. In addition, it was reported that increased ROS levels are closely linked to the accelerated formation of metastasis51.
Limitations of the study
In the present study, BPH and PCa patients were somewhat older and they showed a higher frequency of MetS, factors that could have influenced the results. Nevertheless, our data were statistically adjusted for possible effects of these and other extraneous variables. Age, BMI and MetS had moderate effects (effect sizes around 0.10) on the biomarkers, whilst diagnosis yielded a huge effect size (0.432). The presence of a greater number of patients with MetS in the BPH group is consistent with findings in the literature that reported associations between the pathophysiology of metabolic imbalance and the predisposition of BPH. However Gacci et al.10 in a meta-analysis comprising 24 studies including 132.589 participants concluded that patients with PCa and MetS have a worse prognosis and a more aggressive phenotype of PCa. This study would have been even more interesting if we had measured biomarkers of oxidative DNA damage. Since antioxidant depletion results in oxidative stress toxicity including DNA damage, oxidative DNA biomarkers could contribute to the diagnostic performance established here. In PCa patients, there were more non-Caucasians as compared with the BPH study group while the levels of -SH groups were lower in Black people than in Caucasians and Asians combined. Therefore, future research should examine whether lowered -SH groups in Black men may explain that the latter are at higher risk of PCa than White and Asian men. Future research should examine whether levels of -SH groups may be used as an adjunctive method for follow up of patients on active surveillance.
Conclusions
This study showed a robust association between -SH groups, OS biomarkers and PCa and its prognosis. -SH levels combined with tPSA may be used as an external validating criterion for PCa and to differentiate PCa from BPH in patients with suspicious digital rectal exam. This is the first study to propose models using oxidative stress biomarkers and clinical and laboratory data to predict prognosis in PCa. If other reports confirm our results, new drugs could be tried with -SH as targets.
References
Lynch, H. T. et al. Screening for familial and hereditary prostate cancer. Int. J. Cancer 138, 2579–2591 (2016).
Cook, M. B. et al. A genome-wide association study of prostate cancer in West African men. Hum. Genet. 133, 509–521 (2014).
Ewing, C. M. et al. Germline Mutations in HOXB13 and Prostate-Cancer Risk. N. Engl. J. Med. 366, 141–149 (2012).
Powell, I. J., Bock, C. H., Ruterbusch, J. J. & Sakr, W. Evidence Supports a Faster Growth Rate and/or Earlier Transformation to Clinically Significant Prostate Cancer in Black Than in White American Men, and Influences Racial Progression and Mortality Disparity. J. Urol. 183, 1792–1797 (2010).
Fleshner, N., Bagnell, P. S., Klotz, L. & Venkateswaran, V. Dietary fat and prostate cancer. J. Urol. 171, S19–24 (2004).
Baillargeon, J. & Rose, D. Obesity, adipokines, and prostate cancer (Review). Int. J. Oncol. https://doi.org/10.3892/ijo.28.3.737 (2006).
De Nunzio, C. et al. The controversial relationship between benign prostatic hyperplasia and prostate cancer: the role of inflammation. Eur. Urol. 60, 106–17 (2011).
Gandaglia, G. et al. The role of prostatic inflammation in the development and progression of benign and malignant diseases. Curr. Opin. Urol. 27, 99–106 (2017).
Zou, C., Gong, D., Fang, N. & Fan, Y. Meta-analysis of metabolic syndrome and benign prostatic hyperplasia in Chinese patients. World J. Urol. 34, 281–289 (2016).
Gacci, M. et al. Meta-analysis of metabolic syndrome and prostate cancer. Prostate Cancer Prostatic Dis. 20, 146–155 (2017).
Udensi, U. K. & Tchounwou, P. B. Oxidative stress in prostate hyperplasia and carcinogenesis. J. Exp. Clin. Cancer Res. 35, 139 (2016).
Shiota, M. et al. Antioxidant therapy alleviates oxidative stress by androgen deprivation and prevents conversion from androgen dependent to castration resistant prostate cancer. J. Urol. 187, 707–14 (2012).
Pande, D. et al. Simultaneous progression of oxidative stress, angiogenesis, and cell proliferation in prostate carcinoma. Urol. Oncol. Semin. Orig. Investig. 31, 1561–1566 (2013).
Ashok, B. T. & Ali, R. The aging paradox: free radical theory of aging. Exp. Gerontol. 34, 293–303 (1999).
Barocas, D. A. et al. Oxidative Stress Measured by Urine F2-Isoprostane Level is Associated With Prostate Cancer. J. Urol. 185, 2102–2107 (2011).
Saha, S. K. et al. Correlation between Oxidative Stress, Nutrition, and Cancer Initiation. Int. J. Mol. Sci. 18, 1544 (2017).
Merendino, R. A. et al. Malondialdehyde in benign prostate hypertrophy: a useful marker? Mediators Inflamm. 12, 127–128 (2003).
Hacer, İ. A. et al. The effect of prostate cancer and antianrogenic therapy on lipid peroxidation and antioxidant systems. Int. Urol. Nephrol. 36, 57–62 (2004).
Cimino, S. et al. Oxidative stress and body composition in prostate cancer and benign prostatic hyperplasia patients. Anticancer Res. 34, 5051–6 (2014).
Armitage, T. G., Cooper, E. H., Newling, D. W. W., Robinson, M. R. G. & Appleyard, I. The Value of the Measurement of Serum Prostate Specific Antigen in Patients with Benign Prostatic Hyperplasia and Untreated Prostate Cancer. Br. J. Urol. 62, 584–589 (1988).
Velonas, V., Woo, H., Remedios, C. & Assinder, S. Current Status of Biomarkers for Prostate Cancer. Int. J. Mol. Sci. 14, 11034–11060 (2013).
Pezaro, C., Woo, H. H. & Davis, I. D. Prostate cancer: measuring PSA. Intern. Med. J. 44, 433–440 (2014).
Alford, A. V. et al. The Use of Biomarkers in Prostate Cancer Screening and Treatment. Rev. Urol. 19, 221–234 (2017).
Network - NCCN, N. C. C. Prostate Cancer Guideline. National Comprehensive Cancer Network (2018). Available at, https://www.nccn.org/professionals/physician_gls/pdf/prostate.pdf. (Accessed: 20th August 2018).
Grundy, S. M. et al. Diagnosis and Management of the Metabolic Syndrome. Circulation 112, 2735–2752 (2005).
Hu, M. L. Measurement of protein thiol groups and glutathione in plasma. Methods Enzymol. 233, 380–5 (1994).
Reznick, A. Z. & Packer, L. Oxidative damage to proteins: Spectrophotometric method for carbonyl assay. In 357–363, https://doi.org/10.1016/S0076-6879(94)33041-7 (1994).
Gonzalez Flecha, B., Llesuy, S. & Boveris, A. Hydroperoxide-initiated chemiluminescence: An assay for oxidative stress in biopsies of heart, liver, and muscle. Free Radic. Biol. Med. 10, 93–100 (1991).
Witko-Sarsat, V. et al. Advanced oxidation protein products as novel mediators of inflammation and monocyte activation in chronic renal failure. J. Immunol. 161, 2524–32 (1998).
Repetto, M. et al. Oxidative stress in blood of HIV infected patients. Clin. Chim. Acta 255, 107–117 (1996).
Benjamini, Y., Drai, D., Elmer, G., Kafkafi, N. & Golani, I. Controlling the false discovery rate in behavior genetics research. Behav. Brain Res. 125, 279–84 (2001).
Rahman, I. & MacNee, W. Regulation of redox glutathione levels and gene transcription in lung inflammation: therapeutic approaches. Free Radic. Biol. Med. 28, 1405–1420 (2000).
Biswas, S., Chida, A. S. & Rahman, I. Redox modifications of protein–thiols: Emerging roles in cell signaling. Biochem. Pharmacol. 71, 551–564 (2006).
Dirican, N. et al. Thiol/disulfide homeostasis: A prognostic biomarker for patients with advanced non-small cell lung cancer? Redox Rep. 21, 197–203 (2016).
Hizal, M. et al. Evaluation of dynamic serum thiol/disulfide homeostasis in locally advanced and metastatic gastric cancer. J. Oncol. Sci. 4, 1–4 (2018).
Battisti, V. et al. Oxidative stress and antioxidant status in prostate cancer patients: Relation to Gleason score, treatment and bone metastasis. Biomed. Pharmacother. 65, 516–524 (2011).
Oliveira, P. V. S. & Laurindo, F. R. M. Implications of plasma thiol redox in disease. Clin. Sci. 132, 1257–1280 (2018).
Malm, J. & Lilja, H. Biochemistry of prostate specific antigen, PSA. Scand. J. Clin. Lab. Invest. 55, 15–22 (1995).
Rawlings, N. D. & Barrett, A. J. Families of serine peptidases. Methods Enzymol. 244, 19–61 (1994).
Arsova-Sarafinovska, Z. et al. Increased oxidative/nitrosative stress and decreased antioxidant enzyme activities in prostate cancer. Clin. Biochem. 42, 1228–35 (2009).
Ghiselli, A., Serafini, M., Natella, F. & Scaccini, C. Total antioxidant capacity as a tool to assess redox status: critical view and experimental data. Free Radic. Biol. Med. 29, 1106–14 (2000).
Aydin, A. et al. Oxidative stress and antioxidant status in non-metastatic prostate cancer and benign prostatic hyperplasia. Clin. Biochem. 39, 176–9 (2006).
Doğru-Abbasoğlu, S., Aykaç-Toker, G., Koçak, T., Unlüer, E. & Uysal, M. Antioxidant enzyme activities and lipid peroxides in the plasma of patients with benign prostatic hyperplasia or prostate cancer are not predictive. J. Cancer Res. Clin. Oncol. 125, 402–4 (1999).
Goswami, K., Nandeesha, H., Koner, B. C. & Nandakumar, D. N. A comparative study of serum protein-bound sialic acid in benign and malignant prostatic growth: possible role of oxidative stress in sialic acid homeostasis. Prostate Cancer Prostatic Dis. 10, 356–9 (2007).
Srivastava, D. S. L. & Mittal, R. D. Free radical injury and antioxidant status in patients with benign prostate hyperplasia and prostate cancer. Indian J. Clin. Biochem. 20, 162–5 (2005).
Aryal, M. et al. Oxidative stress in patients with benign prostate hyperplasia. JNMA. J. Nepal Med. Assoc. 46, 103–6
Almushatat, A. S. K. et al. Vitamin antioxidants, lipid peroxidation and the systemic inflammatory response in patients with prostate cancer. Int. J. cancer 118, 1051–3 (2006).
Hoque, A. et al. Serum oxidized protein and prostate cancer risk within the Prostate Cancer Prevention Trial. Cancer Prev. Res. (Phila). 3, 478–83 (2010).
Gurel, B. et al. Chronic inflammation in benign prostate tissue is associated with high-grade prostate cancer in the placebo arm of the prostate cancer prevention trial. Cancer Epidemiol. Biomarkers Prev. 23, 847–56 (2014).
Crohns, M., Westermarck, T. & Atroshi, F. Prostate Cancer, Inflammation and Antioxidants. In Advances in Prostate Cancer, https://doi.org/10.5772/53296 (InTech, 2013).
Shiota, M., Yokomizo, A. & Naito, S. Oxidative stress and androgen receptor signaling in the development and progression of castration-resistant prostate cancer. Free Radic. Biol. Med. 51, 1320–8 (2011).
Acknowledgements
This study was supported by the Brazilian National Council of Research-CNPq and by Araucária Foundation from the state of Paraná. We thank the University Hospital of State University of Londrina and HU Tec Foundation for technical and administrative supports.
Author information
Authors and Affiliations
Contributions
Alexsandro Koike performed the clinical attendance of participants and wrote the paper. Brunna E. F. Robles, Ana Gabriela Bonacini and Camila Cataldi performed the experiments. Edna M.V. Reiche, Isaias Dichi and Rubens Cecchini designed the study and revised the paper. Michael Maes performed the statistical analysis. Andréa N. C. Simão designed the study, wrote the paper and revised the paper. All authors approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Koike, A., Robles, B.E.F., da Silva Bonacini, A.G. et al. Thiol Groups as a Biomarker for the Diagnosis and Prognosis of Prostate Cancer. Sci Rep 10, 9093 (2020). https://doi.org/10.1038/s41598-020-65918-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-65918-w
- Springer Nature Limited