Abstract
Maternal diet is an important potential factor associated with the risk of preeclampsia. However, it is unclear whether adherence to a Dietary Approaches to Stop Hypertension (DASH)-style diet can reduce the development of preeclampsia. To examine the potential association, we conducted a hospital-based case-control study at the First Affiliated Hospital of Zhengzhou University, China. A total of 449 cases with preeclampsia and 449 controls were studied. Dietary information was collected using a validated food frequency questionnaire (FFQ). DASH scores were calculated according to nutrients/food emphasised or minimised in the DASH diet. The calculated DASH scores ranged from 11 to 38 for all of the participants, and the DASH scores of the cases were significantly lower than those of the controls (23.48 ± 4.58 vs 24.51 ± 4.51; p = 0.001). Participants in the fourth quartile of the DASH score were 45% less likely to have preeclampsia than those in the first quartile in the crude model (Q4 vs Q1, odds ratio [OR]: 0.55; 95% confidence interval [CI]: 0.38, 0.80; ptrend = 0.001). The relationship remained significant in the model adjusted for multiple confounders, especially for major risk factors of preeclampsia (OR: 0.53; 95% CI: 0.36, 0.78; ptrend = 0.001). Our findings suggest an inverse relationship between adherence to a DASH-style diet and the odds of preeclampsia. Further larger-scale cohort studies or randomised controlled trials are warranted to confirm these relationships.
Similar content being viewed by others
Introduction
Preeclampsia is a pregnancy-specific complication that occurs after 20 weeks of gestation and is characterised by hypertension, proteinuria and oedema, with or without multiple organ damage1. It is a major cause of foetal and maternal morbidity and mortality worldwide, and affects 2–8% of all pregnancies2. Currently, the only definitive treatment for preeclampsia is to terminate the pregnancy3. Therefore, primary prevention of preeclampsia is vital.
Evidence indicates that maternal diet is an important potential factor affecting the incidence of preeclampsia4,5. Studies have shown that diets rich in vegetables and fruits or various nutrients such as vitamin D, calcium and zinc are associated with lower levels of oxidative stress and inflammation6,7, which are both recognised pathogenic factors for preeclampsia8. However, individual foods or nutrients are consumed in various characteristic combinations, so nutritional epidemiologists have recommended using overall dietary patterns to find links between diet and diseases9. Recent studies have used factor analysis to explore the relationship between dietary patterns and the risk of preeclampsia10,11,12. However, the dietary patterns obtained in these studies were only appropriate for local residents and the results were not comparable. Universal dietary recommendations for the prevention of preeclampsia remain limited.
The Dietary Approaches to Stop Hypertension (DASH) diet is an established dietary pattern rich in whole grains, fruits, vegetables, low-fat dairy and plant proteins from nuts and legumes, but low in red/processed meat, sweets and sugar-sweetened beverages13. The DASH diet was originally designed and evaluated for lowering blood pressure14, but recent studies have shown its benefits for glioma15, nonalcoholic fatty liver disease16 and other metabolic disorders such as cardiovascular disease17, type 2 diabetes18 and gestational diabetes mellitus (GDM)19. However, so far, no study has assessed the association between the DASH diet and the odds of preeclampsia.
Although preeclampsia is also characterised by hypertension, its mechanism is not quite the same as that of adult hypertension. Therefore, the aim of this study was to explore the association between adherence to a DASH-style diet and the odds of preeclampsia among pregnant women in China. In addition, considering that the DASH diet was previously found to be associated with a decreased risk of GDM19, we performed a sensitivity analysis to exclude the influence of GDM on the results.
Results
Participants
Of the 708 inpatients with preeclampsia seen in the hospital, 162 (22.9%) did not meet the inclusion criteria for this study. Of the 546 eligible subjects, 34 (6.2%) cases were excluded due to incomplete surveys or extreme energy intakes (less than 800 or more than 4200 kcal/d)19, and 63 (11.5%) cases refused to participate. In the end, 449 cases were retained in the analysis, including 389 (86.7%) cases without GDM and 60 (13.3%) cases with GDM. In addition, 449 eligible controls from the same hospital, matched for age, gestation week and GDM, were enrolled.
Basic characteristics and dietary intakes of case and control group
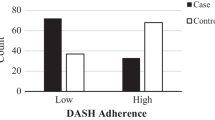
The basic characteristics and dietary intakes of the participants according to case/control status are presented in Table 1. There was no significant difference between the two groups in mean age and gestational age. Mean pre-pregnancy BMI was significantly higher in patients with preeclampsia than in the control group (p < 0.001). Compared with the control group, the cases with preeclampsia had lower total dietary energy and protein intake, consumed significantly less fish, eggs, fruits, vegetables, nuts and legumes, dairy products and red/processed meat. The preeclampsia cases consumed significantly more sodium and were more likely to be nulliparous than the controls. The calculated DASH scores for all participants ranged from 11 to 38, and the cases had significantly lower adherence to the DASH diet than the controls (23.48 ± 4.58 vs 24.51 ± 4.51; p = 0.001).
General characteristics and dietary intakes of the participants by quartiles of DASH score
The general characteristics and dietary intakes of the participants in increasing quartiles of the DASH score are shown in Table 2. The participants in the highest quartiles of the DASH score had higher age and physical activity levels and lower pre-pregnancy BMI than the other quartiles. Adherence to the DASH diet was associated with greater intakes of protein, fish, fruits, vegetables, nuts and legumes, dairy products and red/processed meats. Individuals in the top quartile of the DASH diet had lower intakes of soft drinks and sweets and sodium than those in the bottom quartile. There were no significant differences in consumption of eggs or whole grains and mixed beans between quartiles of the DASH score.
Association between adherence to a DASH-style diet and the odds of preeclampsia
The multivariate adjusted odds ratios (ORs) for preeclampsia across the quartiles of the DASH diet score are shown in Table 3. In the crude model, participants in the top quartile of the DASH diet score were 45% less likely to have preeclampsia (Q4 vs Q1, OR: 0.55; 95% confidence interval [CI]: 0.38, 0.80; ptrend = 0.001). After controlling for age, gestational age and GDM, adherence to the DASH diet was still inversely associated with the odds of preeclampsia (Q4 vs Q1, OR: 0.54; 95% CI: 0.37, 0.79; ptrend = 0.001) (Model 1). Further adjustment for total energy intake, physical activity and nulliparity strengthened the association (Q4 vs Q1, OR: 0.49; 95% CI: 0.34, 0.72; ptrend < 0.001) (Model 2). Additional controlling for pre-pregnancy BMI did not influence the association significantly (Q4 vs Q1, OR: 0.53; 95% CI: 0.36, 0.78; ptrend = 0.001) (Model 3).
Sensitivity analysis
To test the stability of the relationship between adherence to a DASH-style diet and the odds of preeclampsia, we conducted a sensitivity analysis excluding participants with GDM to eliminate the influence of pregnant women with GDM on the results (Table 4). Among 389 pairs of subjects who did not have GDM, participants in the top quartile of the DASH diet score were 39% less likely to have preeclampsia in the crude model (Q4 vs Q1: OR: 0.61; 95% CI: 0.41, 0.90; ptrend = 0.016). In the same way, we adjusted for confounders using the three models mentioned above (except for the confounder of GDM (yes/no)), and found that adherence to the DASH diet was still inversely associated with the odds of preeclampsia.
Discussion
This case-control study demonstrated an inverse association between adherence to a DASH-style diet and the odds of preeclampsia. This significant inverse relationship remained in the model adjusted for multiple confounders, especially for major risk factors of preeclampsia including pre-pregnancy BMI and nulliparity. To the best of our knowledge, this is the first case-control study to explore the association between adherence to a DASH-style diet and the odds of preeclampsia in a Chinese population.
Recent studies have assessed the effects of maternal dietary patterns on the risk of preeclampsia10,12,20. In a prospective longitudinal cohort study in Norway21, four dietary patterns were obtained by factor analysis, of which two were associated with preeclampsia. The dietary pattern characterised by high consumption of vegetables, plant foods and vegetable oils was inversely associated with the odds of developing preeclampsia, while another pattern characterised by processed meat, salty snacks and sweet drinks had the opposite effect10. The above results were consistent with our study in terms of the positive scoring and reverse scoring components of a DASH-style diet.
Furthermore, several previous studies have shown that the components of the DASH diet have different effects on preeclampsia11,21,22,23. A meta-analysis reported that a healthy dietary pattern, rich in vegetables, fruits, legumes and whole grains, was significantly associated with lower odds of preeclampsia11. These components had a large overlap with the characteristics of the DASH diet. Whole grains, as an important positive scoring component of the DASH diet, have been linked to reduced preeclampsia and its risk factors in previous studies, attributed to their nutrients and fibre composition. An observational study of 1538 women in the US found that higher total fibre intake reduced the preeclampsia risk, possibly by attenuating pregnancy-associated dyslipidaemia22. In addition, a DASH-style diet is high in vegetables and fruits, which are rich in natural antioxidants that have been linked to the recognised pathogenic factor of oxidative stress in preeclampsia21. A prospective cohort study in Norway suggested that foods with a high content of added sugar and sugar-sweetened beverages were significantly associated with increased risk of preeclampsia, while foods with natural sugars, such as fresh and dried fruits, were associated with decreased risk of preeclampsia23. A possible explanation is that added sugar provides excess energy intake while foods with a high content of natural sugars are rich in dietary fibre. Red or processed meat and sodium are reverse scoring components of the DASH diet. However, the relationship between these components and preeclampsia and its mechanism has not been reported. More research is needed in the future to uncover the specific mechanism of each component of the DASH diet and the synergistic effects among them.
The Chinese diet is characterised by high consumption of plant foods (grains, vegetables, etc.), lack of high-quality proteins (lean meat, fish, dairy products, etc.) and high oil and salt. The characteristics of high sodium, low calcium and low high-quality protein are the opposite of what the DASH diet recommends and may be important factors in the pathogenesis of preeclampsia. Therefore, for Chinese pregnant women, greater adherence to a DASH-style diet may be associated with decreased odds of preeclampsia. Further studies are also needed in other countries where the diets and foods are naturally different.
This study has many advantages. First, it is the first study to assess the association between adherence to a DASH-style diet and the odds of preeclampsia. Second, our study used a matched case-control design to control for the three major confounders, age, gestational age and GDM. In addition, the relatively large sample size of participants improved the validity, and the sensitivity analysis improved the reliability of the results.
However, some limitations must also be considered when interpreting our findings. First, although we used a validated FFQ to measure dietary intake, there were still inevitable measurement errors and recall bias. Nonetheless, the measurement accuracy benefitted from the employment of trained interviewers who used photographs of food portion sizes to administer the FFQ through face-to-face interviews. Second, considering that patients with preeclampsia have a relatively short time from onset to delivery, we only collected information on the dietary intake of the pregnant women during the final three months before delivery to reduce the recall bias of the FFQ, which may have led to a failure to account for the potential influence of early pregnancy diet on preeclampsia.
In conclusion, our findings suggest an inverse relationship between adherence to a DASH-style diet and the odds of preeclampsia. Further larger-scale cohort studies or randomised controlled trials are needed to confirm the relationship.
Methods
Participants
This hospital-based case-control study was conducted between March 2016 and June 2019 at the First Affiliated Hospital of Zhengzhou University (located in Zhengzhou, a medium-sized city in central China that has been well developed in recent years). Pregnant women of reproductive age (≥18 years) after the 28th week of pregnancy and with single pregnancy were included. The preeclampsia cases were pregnant women who had been diagnosed with preeclampsia by a physician, according to China’s ‘Diagnosis and treatment guideline of hypertensive disorders in pregnancy’ (2015). In this guideline, preeclampsia is defined as systolic blood pressure (SBP) ≥ 140 mmHg or diastolic blood pressure (DBP) ≥ 90 mmHg after 20 weeks of gestation and accompanied by any of the following characteristics: (1) urinary protein ≥ 0.3 g/24 h, or urinary protein/creatinine ratio ≥ 0.3, or random urinary protein ≥ (+) (the test method used when urinary protein cannot be quantified); (2) no proteinuria but accompanied by damage to any of the following organs or systems: heart, lung, liver, kidney and other important organs, or abnormal changes in the blood system, digestive system, nervous system, placental foetus involved, etc. The controls were enrolled among pregnant women from the same hospital without hypertension or proteinuria and were matched with the case group based on age, gestational weeks and GDM.
The exclusion criteria for subjects in both groups were as follows: (1) patients with heart disease, malignancy, hyperthyroidism, immune system diseases, chronic renal insufficiency, and other endocrine system diseases; and (2) patients with epilepsy, depression and other mental or cognitive dysfunction.
Calculation of sample size
On the basis of earlier evidence, we assumed that approximately 30% of the people in the control group would have higher DASH scores, and the estimated OR between the higher DASH scores and preeclampsia odds was 0.6012. With 90% power (β = 0.10), type I error of 0.05 (α = 0.05) and desired CI of 0.95, the minimum required sample size in each group was calculated to be 394, that is, a total of 788 participants. Finally, 449 cases and 449 controls were enrolled in this study.
Assessment of dietary intake
The dietary intake of the study participants during the last three months before delivery was assessed through a valid and reliable semiquantitative food frequency questionnaire (FFQ)24, which included 78 items of foods commonly consumed by Chinese. For each food item, 4 possible frequencies (never, every month, every week and every day) and the amount of consumption each time in grams or millilitres were available. The daily intakes of energy (kcal/d) and key nutrients from each food were calculated according to the Chinese Food Composition Tables25.
Assessment of adherence to a dietary approaches to stop hypertension-style diet
A DASH score was calculated based on the FFQ for each participant. According to Fung’s method26, the DASH score was constructed based on the foods and nutrients emphasised or minimised in the DASH diet, focusing on eight components: high intake of whole grains; fruits; vegetables; nuts and legumes; and low-fat dairy products, and low intake of red/processed meats; sweetened beverages; and sodium26. Because we could not assess the dietary intake of whole grains and low-fat dairy products accurately, we instead calculated whole grains and mixed beans, and dairy products, respectively. Considering that pregnant women consume few sugary drinks, we added sweets to this component.
The scoring criteria and food composition of the DASH-style diet in our study are shown in Table 5. First, the energy-adjusted amounts of components of the DASH-style diet were obtained through the residual method27. Subsequently, quintile cut-off points for each component of the DASH-style diet were obtained in all participants. For the five groups of whole grains and mixed beans, fruits, vegetables, nuts and legumes, and dairy products, those in the highest quintile were given 5 points and those in the lowest quintile received 1 point. In contrast, for the remaining three components, the lowest quintile was given 5 points and the highest received 1 point. An overall DASH score ranging from 8 to 40 was obtained by summing the eight component scores. Individuals with higher DASH scores were more likely to follow the DASH diet.
Assessment of other variables
Information on sociodemographic characteristics, lifestyle habits, pre-pregnancy weight, history of disease, physical activity, menstrual and pregnancy history was obtained through a structured questionnaire. The height and weight of the participants were measured to the nearest 0.1 cm and 0.1 kg, respectively, without shoes and in light clothing. After a rest of ≥10 min, blood pressure was measured at least twice on the left arm with a sphygmomanometer; a third measurement was taken on any occasion when the first two DBP or SBP values differed by more than 3 mmHg or 4 mmHg. At least two measurements were averaged for further analysis. The participants’ physical activity during pregnancy included daily occupational, leisure-time and household-chores, and was expressed as metabolic equivalents (MET) hour/day28. Each individual’s body mass index (BMI) was calculated as weight (kg)/height (m2).
Statistical analysis
The Shapiro-Wilk test and Q-Q plots were used to check the normality of the general characteristics and dietary intakes. The general characteristics of the cases and controls were compared using the chi-square test for categorical variables and independent samples t-test for continuous variables and were described by number and mean ± SD (normal distribution). Considering that the dietary intakes did not show a normal distribution, we used the Mann-Whitney U test to compare the dietary intakes among cases and controls and described the results using M (p25–p75). To assess the association of a DASH-style diet with preeclampsia, the total DASH score was divided into four ascending categories on an ordinal scale. The general characteristics were also compared among quartiles of the DASH score using the chi-square test for categorical variables and one-way ANOVA for continuous variables. The dietary intakes of the participants by quartiles of the DASH score were analysed using analysis of covariance (ANCOVA) adjusted for total energy intake.
The association of the DASH diet with preeclampsia was assessed using binary logistic regression. In addition to the original model, three different models were developed: Model 1 was adjusted for age, gestational age and GDM (yes/no). Model 2 was further adjusted for total energy intake (kcal/d), physical activity (MET) and nulliparity (yes/no). Model 3 comprised Model 2 plus an adjustment for pre-pregnancy BMI. In all models, the first quartile of the DASH score were considered as the reference group. The overall trend of OR across increasing quartiles of the DASH score was examined by considering the median score in each category as a continuous variable15. All probability values below 0.05 were considered statistically significant. All of the statistical analyses were performed using SPSS (version 25.0; SPSS Inc., Chicago, IL).
Ethical approval
This study was approved by the Ethics Committee of Scientific Research and Clinical Trials of the First Affiliated Hospital of Zhengzhou University and written informed consent was obtained from all participants. All of the procedures were performed in accordance with the approved guidelines laid down in the Declaration of Helsinki.
Data availability
Additional data are available from the corresponding author upon reasonable request.
References
Mol, B. W. J. et al. Pre-eclampsia. Lancet 387, 999–1011, https://doi.org/10.1016/s0140-6736(15)00070-7 (2016).
Duley, L. The global impact of pre-eclampsia and eclampsia. Semin. Perinatol. 33, 130–137, https://doi.org/10.1053/j.semperi.2009.02.010 (2009).
Grotegut, C. A. Prevention of preeclampsia. J. Clin. Invest 126, 4396–4398, https://doi.org/10.1172/JCI91300 (2016).
Grum, T., Hintsa, S. & Hagos, G. Dietary factors associated with preeclampsia or eclampsia among women in delivery care services in Addis Ababa, Ethiopia: a case control study. BMC research notes 11, 683, https://doi.org/10.1186/s13104-018-3793-8 (2018).
Oken, E. et al. Diet during pregnancy and risk of preeclampsia or gestational hypertension. Ann. Epidemiol. 17, 663–668, https://doi.org/10.1016/j.annepidem.2007.03.003 (2007).
Achamrah, N. & Ditisheim, A. Nutritional approach to preeclampsia prevention. Curr. Opin. Clin. Nutr. Metab. Care. 21, 168–173, doi:10.1097/MCO.0000000000000462 (2018).
Hillesund, E. R. et al. Associations of adherence to the New Nordic Diet with risk of preeclampsia and preterm delivery in the Norwegian Mother and Child Cohort Study (MoBa). Eur. J. Epidemiol. 29, 753–765, https://doi.org/10.1007/s10654-014-9948-6 (2014).
Jim, B. & Karumanchi, S. A. Preeclampsia: Pathogenesis, Prevention, and Long-Term Complications. Semin. Nephrol. 37, 386–397, https://doi.org/10.1016/j.semnephrol.2017.05.011 (2017).
Hu, F. B. Dietary pattern analysis: a new direction in nutritional epidemiology. Curr. Opin. Lipidol. 13, 3–9, https://doi.org/10.1097/00041433-200202000-00002 (2002).
Ikem, E. et al. Dietary patterns and the risk of pregnancy-associated hypertension in the Danish National Birth Cohort: a prospective longitudinal study. BJOG-An International Journal of Obstetrics and Gynaecology 126, 663–673, https://doi.org/10.1111/1471-0528.15593 (2019).
Kibret, K. T., Chojenta, C., Gresham, E., Tegegne, T. K. & Loxton, D. Maternal dietary patterns and risk of adverse pregnancy (hypertensive disorders of pregnancy and gestational diabetes mellitus) and birth (preterm birth and low birth weight) outcomes: a systematic review and meta-analysis. Public Health Nutrition 22, 506–520, https://doi.org/10.1017/s1368980018002616 (2019).
Schoenaker, D. A., Soedamah-Muthu, S. S., Callaway, L. K. & Mishra, G. D. Prepregnancy dietary patterns and risk of developing hypertensive disorders of pregnancy: results from the Australian Longitudinal Study on Women’s Health. Am. J. Clin. Nutr. 102, 94–101, https://doi.org/10.3945/ajcn.114.102475 (2015).
Vogt, T. M. et al. Dietary Approaches to Stop Hypertension: rationale, design, and methods. DASH Collaborative Research Group. J. Am. Diet. Assoc. 99, S12–18 (1999).
Sacks, F. M. et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N. Engl. J. Med. 344, 3–10, https://doi.org/10.1056/NEJM200101043440101 (2001).
Benisi-Kohansal, S. et al. Adherence to the Dietary Approaches to Stop Hypertension-style diet in relation to glioma: a case-control study. Br. J. Nutr. 115, 1108–1116, https://doi.org/10.1017/S0007114515005504 (2016).
Hekmatdoost, A. et al. Adherence to the Dietary Approaches to Stop Hypertension (DASH) and risk of Nonalcoholic Fatty Liver Disease. International journal of food sciences and nutrition 67, 1024–1029, https://doi.org/10.1080/09637486.2016.1210101 (2016).
Bertoia, M. L. et al. Mediterranean and Dietary Approaches to Stop Hypertension dietary patterns and risk of sudden cardiac death in postmenopausal women. Am. J. Clin. Nutr. 99, 344–351, https://doi.org/10.3945/ajcn.112.056135 (2014).
Liese, A. D., Nichols, M., Sun, X., D’Agostino, R. B. Jr. & Haffner, S. M. Adherence to the DASH Diet is inversely associated with incidence of type 2 diabetes: the insulin resistance atherosclerosis study. Diabetes Care 32, 1434–1436, https://doi.org/10.2337/dc09-0228 (2009).
Izadi, V. et al. Adherence to the DASH and Mediterranean diets is associated with decreased risk for gestational diabetes mellitus. Nutrition 32, 1092–1096, https://doi.org/10.1016/j.nut.2016.03.006 (2016).
Mi, B. et al. Vegetable dietary pattern associated with low risk of preeclampsia possibly through reducing proteinuria. Pregnancy Hypertens 16, 131–138, https://doi.org/10.1016/j.preghy.2019.04.001 (2019).
Brantsaeter, A. L. et al. A dietary pattern characterized by high intake of vegetables, fruits, and vegetable oils is associated with reduced risk of preeclampsia in nulliparous pregnant Norwegian women. J. Nutr. 139, 1162–1168, https://doi.org/10.3945/jn.109.104968 (2009).
Qiu, C., Coughlin, K. B., Frederick, I. O., Sorensen, T. K. & Williams, M. A. Dietary fiber intake in early pregnancy and risk of subsequent preeclampsia. Am. J. Hypertens. 21, 903–909, https://doi.org/10.1038/ajh.2008.209 (2008).
Borgen, I. et al. Maternal sugar consumption and risk of preeclampsia in nulliparous Norwegian women. Eur. J. Clin. Nutr. 66, 920–925, https://doi.org/10.1038/ejcn.2012.61 (2012).
Zhang, C. X. & Ho, S. C. Validity and reproducibility of a food frequency Questionnaire among Chinese women in Guangdong province. Asia Pac. J. Clin. Nutr. 18, 240–250 (2009).
Yang, Y. X., Wang, G. Y. & C., P. X. Chinese Food Composition Table. Second edn, (Peking University Medical Press, 2009).
Fung, T. T. et al. Adherence to a DASH-style diet and risk of coronary heart disease and stroke in women. Arch. Intern. Med. 168, 713–720, https://doi.org/10.1001/archinte.168.7.713 (2008).
Willett, W. C., Howe, G. R. & Kushi, L. H. Adjustment for total energy intake in epidemiologic studies. Am. J. Clin. Nutr. 65, 1220S-1228S; discussion 1229S-1231S, https://doi.org/10.1093/ajcn/65.4.1220S (1997).
Ainsworth, B. E. et al. 2011 Compendium of Physical Activities: a second update of codes and MET values. Med. Sci. Sports. Exerc. 43, 1575–1581, https://doi.org/10.1249/MSS.0b013e31821ece12 (2011).
Acknowledgements
The authors are grateful to the National Natural Science Foundation of China (Grant No. 81602852) for supporting this work.
Author information
Authors and Affiliations
Contributions
Y.L., X.Z. and D.D. designed the research study. Y.C., W.D., D.D. and W.F. performed the research. Y.C., Y.L. and H.C. contributed to analysis of the data. Y.C. and Y.Q. drafted the manuscript. Y.L., Y.B. and Q.L. revised the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cao, Y., Liu, Y., Zhao, X. et al. Adherence to a Dietary Approaches to Stop Hypertension (DASH)-style Diet in Relation to Preeclampsia: A Case-Control Study. Sci Rep 10, 9078 (2020). https://doi.org/10.1038/s41598-020-65912-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-65912-2
- Springer Nature Limited
This article is cited by
-
The association between diet quality index-international and dietary diversity score with preeclampsia: a case–control study
BMC Women's Health (2024)
-
The association between dietary mineral intake and the risk of preeclampsia in Chinese pregnant women: a matched case–control study
Scientific Reports (2023)
-
Dietary carotenoid intake and risk of developing preeclampsia: a hospital-based case–control study
BMC Pregnancy and Childbirth (2022)
-
The association between dietary fatty acid intake and the risk of developing preeclampsia: a matched case–control study
Scientific Reports (2021)