Abstract
Polybrominated diphenyl ethers (PBDEs) are ubiquitous environmental pollutants. Arctic indigenous peoples are exposed to PBDEs through a traditional diet high in marine mammals. PBDEs disrupt thyroid homeostasis. The aim of this study was to assess the relationship between serum PBDEs and thyroid function in a remote population of St. Lawrence Island Yupik. Serum samples were collected from 85 individuals from St. Lawrence Island, Alaska and measured for concentrations of PBDEs, free and total thyroxine (T4), free and total triiodothyronine (T3), and thyroid stimulating hormone (TSH). The relationships between PBDEs and thyroid hormones were assessed using multiple linear regression fit with generalized estimating equations. Serum concentrations of several Penta-BDE congeners (BDE-28/33, 47, and 100) were positively associated with concentrations of TSH and free T3, while serum concentration of BDE-153 was negatively associated with total T3 concentrations. Both BDE-47 and 153 remained significantly associated with thyroid hormones when BDE-47, BDE-153, and BDE-209 were covariates in the same model. There were no significant relationships between serum concentrations of PBDEs and either free or total T4. Individual PBDEs are associated with thyroid hormones in serum from a remote population of Alaska Natives, and directions of effect differ by congener.
Similar content being viewed by others
Introduction
Polybrominated diphenyl ethers (PBDEs) are additive flame retardants still found in numerous products such as urethane foam, electronics and fabrics. Due to their widespread usage and persistence in the environment, PBDEs have become globally ubiquitous environmental contaminants1. In the United States, where most PBDEs were used, they have been voluntarily phased out of production beginning in 20042. All three technical formulations, penta-BDE, octa-BDE, and deca-BDE are globally restricted under the Stockholm Convention on Persistent Organic Pollutants due to evidence of toxicity and bioaccumulation in humans and animals3. Despite recently implemented restrictions, the large reservoir of PBDEs in the environment and products ensures continued exposure to these compounds.
Alaska Natives are exposed to PBDEs through two primary sources: diet and household dust. Characteristic of many arctic indigenous peoples, Alaska Natives are heavily reliant on a subsistence diet. Among the Yupik residents of St. Lawrence Island, Alaska this diet includes high trophic level and/or long lived marine mammals such as bowhead whale (Balaena mysticetus), Pacific walrus (Odobenus rosmarus), and bearded seal (Erignathus barbatus). Bioaccumulation of PBDEs in arctic and sub-arctic marine mammals is well documented4,5,6,7 and thus their dietary consumption represents an important source of PBDE exposure8,9. Residents of St. Lawrence Island are also exposed to PBDEs through the indoor environment; we previously reported that concentrations of PBDEs in house dust from St. Lawrence Island were comparable to those found in the contiguous United States10. The health implications of this exposure for arctic indigenous peoples are unknown and have been poorly studied.
Numerous toxicological studies suggest that PBDE exposure decreases concentrations of circulating thyroid hormones through multiple mechanisms, including displacement from transport proteins, as well increased conjugation, metabolism and excretion of hormones11. However, there is a lack of consistency with regard to the strength and direction of effects reported in epidemiological studies. Some document inverse associations between PBDEs and thyroid hormones, while others report positive associations. A recent prospective study of adult office workers employing repeated measures of both PBDEs and thyroid hormones found significant inverse associations between BDE-47 and 100 and total thyroxine (T4), but no association with thyroid stimulating hormone (TSH)12. This is consistent with the hypothyroxinemic effect predicted by most animal studies13,14. However, positive associations with thyroid hormones have also been reported. In a study of adult male sportfish consumers, BDE-99 and BDE-153 were positively associated with T415. A study of Inuit adults from Canada reported a positive association between BDE-47 and total triiodothyronine (T3)16. Clearly, the relationship between PBDE exposure and thyroid hormones is complex and not fully understood. The aim of the current study was to determine the association between PBDE exposure and thyroid hormones in a remote population of Alaska Natives, including an assessment of potentially differential effects of individual PBDEs on thyroid function.
Methods
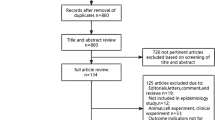
This study was conducted in two Native Villages, Gambell and Savoonga, on St. Lawrence Island. Participants were recruited through flyers posted in public spaces, or directly recruited by bilingual (Yupik-English) community health researchers. Inclusion criteria included being of reproductive age defined as 18–45 years. Community health researchers aimed to recruit one man and one woman from each participating home. A total of 85 individuals from 49 homes were recruited for the study. There were a total of 36 male-female pairs, and an additional 11 unpaired women and 2 unpaired men. This study was approved by the Alaska Area IRB (Indian Health Service IRB00000636) and the Research Ethics Review Board of the Norton Sound Health Corporation. All participants signed an informed consent (administered by bilingual research assistants) before participating in the study. All research was performed in accordance with relevant guidelines and regulations.
Approximately 60 mls of venous blood was drawn into sterile vacutainers (Becton Dickinson, Franklin Lakes, NJ) from individuals who had fasted for at least 8 hours. Blood was allowed to clot at room temperature for one hour, then centrifuged for 15 minutes at 3300 rpm. Serum was then sub-divided for chemical and hormone analyses. For PBDE analysis, serum was transferred to glass vials with PTFE lined caps (Becton Dickinson, Franklin Lakes, NJ), stored at −18 °C, and shipped frozen. Quantification of analytes in serum was carried out by AXYS Analytical (Sydney, British Columbia, Canada). Forty individual PBDEs were quantified using isotope dilution high resolution gas chromatography/high resolution mass spectrometry. Isotopically labeled surrogate standards were used for PBDE analysis. A blank and matrix spike were included in each analytical batch of approximately 13 samples. Analyte recoveries from matrix spikes were never outside of 80–120%. BDE-209 recovery ranged from 60–120%. When blanks contained quantifiable concentrations of analytes, this concentration was subtracted from the other samples in the analytical batch. The limit of detection(LOD) ranged from approximately 0.01 to 1 pg/ml for most congeners, but was higher for BDE-209 ranging from 0.4 to 26 pg/ml. Approximately 2 ml serum aliquots were frozen in the field at −18 °C and shipped overnight to Labcorp (Seattle, Washington) for analysis of thyroid hormones. TSH, T3, free triiodothyronine (fT3), and free thyroxine (fT4) were quantified using an Electro-chemiluminescence immunoassay (ECLIA). Precision was not determined for the samples under study, however method precision is reported as maximum observed coefficients of variation (CV) in human serum reported by Labcorp. T3 had a maximum CV of 5.4%, cross reactivity of <1% for other thyroid hormones, and a LOD of 0.195 ng/mL. fT3 has a maximum CV of 8.2%, cross reactivity of <0.01% for other thyroid hormones, and a LOD of 0.06 ng/dL. fT4 had a maximum CV 7.6%, cross reactivity of ≤0.005% for other thyroid hormones, and a LOD of 0.101 ng/dL. T4 was quantified using a cloned enzyme donor immunoassay (CEDIA) with a maximum CV of 9.2%, cross reactivity of <0.1% for other thyroid hormones, and a LOD of 0.5–20 μg/dL. Total serum lipids were determined by enzymatic measurements of cholesterol, free cholesterol, triglycerides and phospholipids17.
TSH as well as all PBDEs were natural log transformed to better fit a normal distribution. Spearman’s rank correlation was used to assess correlation among PBDEs. PBDE concentrations are reported as percentiles. The associations between PBDEs and circulating thyroid hormones were estimated using multiple linear regression estimated with generalized estimating equations (GEE). GEE was used to account for the correlation of multiple participants from the same home. The wet weight concentrations of individual PBDEs were used as the predictor variables in each of five models with T3, fT3, T4, fT4 and TSH as the dependent variables, adjusting for age, sex, smoking, and serum lipid content. PBDE concentrations were lipid adjusted within the model rather than lipid standardized18. Regression coefficients represent the predicted change in thyroid hormones for a one intra-quartile range increase in PBDE concentration, controlling for covariates. Confounders were identified a priori using a directed acyclic graph19. Additionally, a model was constructed using multiple individual PBDEs as covariates in a single model, for each of five thyroid measures, and adjusted for the same confounders. This model used only BDE-47, BDE-153 and BDE-209. These PBDEs were chosen for several reasons: 1) they had high detection rates and were present at relatively high concentrations, 2) BDE 47 and 209 are good indicators of their respective technical mixtures, 3) BDE 47, 153, and 209 are minimally correlated. For all models, regression coefficients represent the effect of a one intraquartile range (IQR) change in PBDE concentration. Because machine read values were not available, PBDE concentrations that were < LOD were imputed as LOD/√2 for regression analysis20. A sensitivity analysis was conducted in which continuous PBDEs were also modeled with data < LOD imputed as the mean of observed values, a method which produces minimally biased conservative estimates21. The results of these two methods were compared to ensure data < LOD were having a minimal impact on regression estimates (supplemental material). Influential observations were identified using DFBETAS which is a standardized measure of the impact of a single observation on the regression coefficient; in the event a DFBETAS was >1 the observation was removed from the regression, and the regression was re-run. Statistical analysis was conducted in SAS 9.4 (SAS Institute, Cary, NC).
Results
Table 1 presents descriptive statistics for participant characteristics. The median age of participants was 29 years. Age ranges of men and women in the study were comparable (19–45 in men, and 18–45 in women). Tobacco smoke exposure, measured as active smoking or the presence of an active indoor smoker in the home, was slightly more prevalent in women (17%) than men (13%). Detection rates for PBDEs were similar among men and women, but slightly higher in women for BDE-47, BDE-100, and BDE-209. Median concentrations tended to be similar in men and women. A female participant with elevated serum PBDE concentrations skewed the distributions in females, specifically for BDEs 47, 99 and 100. Maximum PBDE concentrations were uniformly higher among women (Table 1). No individuals reported current or former thyroid disease, or current thyroid medication. One individual had a TSH concentration above the reference range. Eight individuals had TSH concentrations below the reference range. One individual had both T3 and fT3 concentrations above the reference ranges. Two individuals had T4 concentrations above the reference range, and one had T4 below the reference range. Unless specified all other hormones in these individuals were within the reference ranges.
Several PBDE congeners were positively associated with serum concentrations of TSH (Table 2). A one IQR increase in BDE-28/33 was positively associated with TSH (β = 0.41; 95% confidence interval (CI) 0.19, 0.63; p < 001), as were BDE 47 (β = 3.87; 95% CI 1.21, 6.57; p < 0.005) and BDE-100 (β = 0.89; 95% CI 0.18, 1.61; p = 0.01).
When modeled individually, no PBDEs were associated with serum concentrations of either f T4 or T4 (Table 2). BDE-99 was marginally associated with T4 after the removal of an influential data point with a high BDE-99 concentration.
A one IQR change in BDE-153 was negatively associated with serum concentrations of T3 (Table 2) (β = −113.14; 95% CI –225.04, −1.14; p = 0.048). Several penta-BDE congeners were positively associated with fT3 concentration. BDE-28/33 was positively associated with fT3 (β = 0.18; 95% CI 0.07, 0.30; p < 0.005), as was BDE-47 (β = 0.2.21; 95% CI 0.46, 3.95; p = 0.01), and BDE-100 (β = 0.39; 95% CI 0.12 0.66; p = 0.005). BDE-209 was not significantly associated with any thyroid hormones.
Table 3 presents the results of models which include a BDE*sex product term to assess effect modification by sex. The table includes the effect of the PBDE in men as well as the joint effect of the PBDE and female sex. The association between BDE-99 and TSH was significantly modified by sex, with a positive association in men (β = 0.75; 95% CI 0.20, 1.30; p = 0.01) and a negative joint effect of BDE-99 and female sex (β = −0.92 95%; CI −1.59, −0.25; p = 0.01). When an influential data point with a high BDE-47 value was removed, sex significantly modified the effect of BDE-47 on T4 (p < 0.001), but this effect was not significant in the full dataset (p = 0.29). Sex also modified the effect of BDE-47 (p = 0.002) and BDE-99 (p = 0.02) on fT4, with a positive effect in women and a negative effect in men. However, no effect modification was detected for any association in the sensitivity analysis (Table S-2).
Table 4 presents the results of models that simultaneously modeled BDE-47, BDE-153 and BDE-209 as predictors, in order to assess the potential for confounding by other PBDEs. BDE-47, 153, and 209 were chosen because they are weakly to moderately inter-correlated and therefore could be simultaneously modeled (Table S-3). BDE-47 remained significantly positively associated with TSH (β 4.57; 95% CI 1.90, 7.24; p < 0.001) for every one IQR change PBDE concentration. BDE-47 appeared significantly associated with T4 (β −9.06; 95% CI −17.73, −0.38; p = 0.04). After adjusting for other PDBEs, a one IQR change in BDE-47 was significantly positively associated with T3 (β = 76.08; 95% CI 23.68, 128.47; p = 0.004) and a one IQR change in BDE-153 remained negatively associated with T3 (β = −153.8; 95% CI −268.85, −38.64; p = 0.009). BDE-47 remained significantly positively associated with fT3 (β = 4.16; 95% CI 2.41, 5.90; p < 0.0001) for every one IQR change in PBDE concentration. Including an influential data point with a high BDE-47 value made this association weaker (β = 3.08) but still significant (p = 0.003). A one IQR change in BDE-153 was negatively associated with fT3 after adjustment for other PBDEs (β = −3.94; 95% CI −6.08, −1.81; p < 0.001).
Discussion
In this study of adult Alaska Natives, BDE-28/33, 47, 99, and 100 were individually and positively associated with TSH. BDE-47 was positively associated with TSH after controlling for the effects of BDE-153 and BDE-209. However, BDE-28/33, 47, 99, and 100 have a high mutual correlation, and it is therefore difficult to partition the effects of these compounds. The overall suggestion is that at least one component congener of penta-BDE is positively associated with TSH. While infrequent, other epidemiological studies have reported positive associations between penta-BDE and TSH. A small study of e-waste workers found higher TSH concentrations among the most highly exposed group22. In a study of young children from the southeastern United States, the sum of penta-BDE was positively associated with TSH23. Multiple PBDEs were positively associated with TSH among late-term pregnant women from California24; however, the opposite association has also been reported in pregnant women from California25. An inverse association between BDE-47 and TSH was reported in a study of males with high fish intake26. Further complicating matters, some studies have reported no association between PBDEs and TSH16,27. There is minimal evidence for PBDEs causing secondary hyperthyroidism, suggesting that any positive associations with TSH may be the result of adaptive TSH increases due to sub-clinical hypothyroidism. However, the hypothyroxinemic effect seen in animal models14 suggests that PBDEs may disrupt thyroid homeostasis in ways other than classic hyperthyroid or hypothyroid effects. In addition, caution should be exercised in inferring physiological explanations for statistical relationships, given the apparent complexity of these relationships.
In the current study we did not find any associations between individual PBDEs and fT4 or T4 when they were modeled individually. Epidemiological studies of adults have documented both inverse associations12 and positive associations15 between PBDEs and T4. In our study of Alaska Natives, removal of a participant with high serum BDE-47 concentration from the models resulted in an apparent departure from additivity of the effect of BDE-47 and female sex on T4. The interaction predicted a significant inverse association in men and positive association in women. However, the relationship was not significant in the sensitivity analysis, thus we cannot rule out the possibility that the interaction resulted from the handling of data <LOD. To the best of our knowledge, effect modification of the BDE-47 and T4 association by sex has not been previously reported. Overall, the results of this study do not suggest a strong interaction between sex and PBDE exposure on thyroid hormone homeostasis. A negative association between BDE-47 and T4 was detected when BDE-153 and BDE-209 were included in the same model.
Several PBDEs were positively associated with fT3 in this population, including BDE-28/33, BDE-47, BDE-100, and a marginally significant association for BDE-99. In contrast, BDE-153 was significantly negatively associated with T3 among participants of this study. No interactive terms were significant for fT3 or T3 models. When BDE-47, 153, and 209 were modeled together, both BDE-47 and BDE-153 were significantly associated with fT3 and T3. Among a large sample of Inuit adults from Canada, serum BDE-47 concentrations were positively associated with T3, however fT3 was not measured16. BDE-153 was also measured, but was not associated with any thyroid hormones among the Canadian Inuit. A study of young children in Atlanta also reported positive associations between penta-BDE congeners and fT323. In a study of adult male sportfish consumers, BDE-47, 99, 100, and 153 were positively associated with reverse T3 (rT3), but BDE-47 and BDE-153 were negatively associated with T315. A non-significant inverse association between BDE-153 and T3 was reported in a cohort study utilizing repeated measures of both exposure and thyroid hormones12. An inverse association between BDE-153 and T3 was also reported in an epidemiological study of pregnant women28. A similar relationship has been reported in cord blood29. However, the generalizability of associations found in pregnant women remains unclear, due to estrogen related changes in thyroid homeostasis30.
The mechanisms which may underlie these associations are not clear. Associations between PBDEs and T3 or rT3 may suggest alterations of deiodinase concentrations or activity. In our study, positive associations with T3 may suggest an increase in deiodination of T4. In human liver cells, both BDE-99 and BDE-209 induce type I deiodinase expression31. However, the opposite effect has been observed. Human glial cells exposed to PBDEs show decreases in type II deiodinase activity32. Research in neonatal rats has also found transient decreases in type I deiodinase expression33. Displacement of T4 from binding proteins has been suggested as a mechanism of PBDE action11. An increase in fT4 could also result in positive associations with T3 if it was efficiently deiodinated into T3. Differences in effects based on species, tissue or individual PBDEs are possible.
Several studies have suggested that the associations between PBDEs and the thyroid hormone axis are modified by other factors. For example, among National Health and Nutrition Examination Survey (NHANES) participants, PBDEs are more strongly associated with thyroid disease in post-menopausal women than in other women34, a result that suggests interplay involving the reproductive axis. Immune function may also modify or mediate the relationship between PBDEs and thyroid homeostasis, as differential effects have been reported in individuals with antibodies to thyroglobulin or thyroperoxidase35. Some authors have speculated that the exposure response relationship between PBDEs and thyroid hormones is non-monotonic36. The hormetic effects of PBDE exposure have been documented in relation to proliferation of cancer cells37,38. Hydroxylated PBDEs (OH-BDEs) were not measured as part of this study, though they may play a role in PBDE related thyroid disruption. Specifically, OH-BDEs are structurally similar to thyroid hormones, and bind to thyroid transport proteins with greater affinity than PBDEs, and OH-BDEs bind the thyroid receptor with different effects (agonist/antagonist) dependent on level of bromination39,40,41,42,43. Collectively, the literature suggests a complex relationship, potentially modified by numerous factors such as age, sex, immune status, iodine sufficiency and exposure to other environmental chemicals. Our results suggest that individual PBDEs may affect thyroid hormone concentrations differently and that different mechanisms or combinations of mechanisms may be at work.
A few individuals had thyroid hormone concentrations outside the laboratory reference ranges, but none showed characteristic patterns associated with disease. For example, several individuals had low TSH with T4 and T3 in the reference range, which could represent sub-clinical hyperthyroidism. Unfortunately, there is great variation in circulating thyroid concentrations in apparently euthyroid individuals and references ranges are inconsistent across studies44,45,46,47. In the absence of more detailed clinical information, it is not possible to identify clinical thyroid disease. While this study cannot make inferences about clinically diagnosed thyroid disease, variation in thyroid hormones in the absence of thyroid disease is associated with morbidities. For example, subclinical hypothyroidism is associated with overweight and obesity48, adverse cardiovascular outcomes49,50, and impaired cognitive function51. Subclinical hyperthyroidism is associated with osteoporosis and abnormal cardiac morphology and function52.
Limitations
The cross-sectional design of this study did not allow an examination of the temporal relationship between exposure and outcome. However, the serum concentration of PBDEs is thought to be an indicator of both past and current exposure, due to relatively long biological half-lives53,54. This was a convenience sample and may not be representative of the population of St. Lawrence Island. However, it is unlikely that participation rates were differential with regard to thyroid function, making any source of bias small for these associations. Given that no participants reported clinically diagnosed thyroid disease, this study cannot provide insight into the role of PBDEs in thyroid disease. The reported prevalence of smoking is low considering the anecdotally high tobacco use in this population. The small sample size limits the statistical power of the study; low power complicates interpretation of null findings, as they may be the result of type II error. PBDEs, especially those found within the same technical mixtures, are often highly correlated in serum samples55. The high mutual correlations among PBDEs make attributing health outcomes to a single compound difficult. BDE-209 is subject to several sources of measurement error, including high risk of sample contamination from the environment, and degradation during analysis56. This non-differential error would bias associations toward the null. There is debate about the role of overweight and obesity in thyroid physiology57. If it is the case that alteration in body mass index (BMI) is secondary to thyroid disruption, then it is not appropriate to include BMI in the models; however, BMI may also alter thyroid physiology. We did not control for BMI in the models. While participants reported fasting for >8 hours, it is possible that length of fast could impact thyroid hormone concentrations, especially if there was poor compliance. Measures of liver function, and specifically liver deiodinase activity, could provide insight into mechanisms of PBDE effects, but were not collected in this study. This study does not correct for multiple statistical tests58, which could increase the probability finding false positive associations.
The residents of St. Lawrence Island are exposed to numerous persistent organic pollutants (POPs) through their traditional diet59; and they have higher levels of certain POPs, including polychlorinated biphenyls (PCBs), than populations of the contiguous United States (Carpenter et al. 2005). The correlation of PBDEs with other POPs may affect the associations found in this study. Associations between PCBs and thyroid hormones have been reported in both epidemiological studies and in animal models60,61. Concurrent exposure to PBDEs and PCBs may have additive or synergistic effects on T4 concentrations62,63. In a study of older adults, PBDEs and PCBs were found to synergistically increase the concentration of serum T3 in women64. Therefore, there may be confounding or interactions with other POPs that were not captured in this study.
Sensitivity analysis suggests that given a small percentage of missing data, the value chosen for data <LOD has a small impact on effect estimates. Given relatively small percentages of missing data, simple imputation can produce minimally biased effect estimates21; however, simple imputation may poorly approximate the variance. This may impact estimates of the standard error and artificially reduce p-values. The empirical (i.e. robust/sandwich) estimator used by GEE provides a reasonable estimate of covariance given an unknown covariance structure65, but may underestimate the true standard error.
Conclusions
Serum concentrations of select PBDEs were associated with serum concentrations of thyroid hormones in this population of Alaska Natives. Several component congeners of the penta-BDE mixture were positively associated with TSH and fT3, while BDE-153 was negatively associated with T3. There was not strong evidence of effect modification by sex. Individual PBDEs appear to have independent, and at times opposite statistical relationships with circulating thyroid hormone concentrations. This may suggest complex and perhaps competing mechanisms of toxicity. No participants reported clinically diagnosed thyroid disease, however sub-clinical alterations in thyroid hormones may have implications for health. The role of PBDE exposure in disruption of thyroid hormone homeostasis, and the clinical significance in adults, remain unclear.
Declarations
Ethics approval and consent to participate
This Study was approved by the Alaska Area IRB (Indian Health Service IRB00000636) and the Research Ethics Review Board of the Norton Sound Health Corporation. All participants provided an informed consent (administered by bilingual research assistants) before participating in the study.
Availability of data and material
The data are not publicly available due to them containing information that could compromise research participant privacy and consent. Data may be available from the authors upon reasonable request and with permission of the St. Lawrence Island working group.
References
Hites, R. A. Polybrominated diphenyl ethers in the environment and in people: a meta-analysis of concentrations. Environ. Sci. Technol. 38, 945–956 (2004).
Abbasi, G., Buser, A. M., Soehl, A., Murray, M. W. & Diamond, M. L. Stocks and flows of PBDEs in products from use to waste in the U.S. and Canada from 1970 to 2020. Environ. Sci. Technol. 49, 1521–1528 (2015).
UNEP. Stockholm Covention on Persistent Organic Pollutants 2256 UNTS 119; 40 ILM 532 (2001).
de Wit, C. A., Herzke, D. & Vorkamp, K. Brominated flame retardants in the Arctic environment–trends and new candidates. Sci. Total Environ. 408, 2885–2918 (2010).
Kannan, K., Yun, S. H. & Evans, T. J. Chlorinated, brominated, and perfluorinated contaminants in livers of polar bears from Alaska. Environ. Sci. Technol. 39, 9057–9063 (2005).
Kelly, B. C., Ikonomou, M. G., Blair, J. D. & Gobas, F. A. Bioaccumulation behaviour of polybrominated diphenyl ethers (PBDEs) in a Canadian Arctic marine food web. Sci. Total Environ. 401, 60–72 (2008).
Rotander, A. et al. Polybrominated diphenyl ethers (PBDEs) in marine mammals from Arctic and North Atlantic regions, 1986–2009. Environ. Int. 40, 102–109 (2012).
Fraser, A. J., Webster, T. F. & McClean, M. D. Diet contributes significantly to the body burden of PBDEs in the general U.S. population. Environ. Health Perspect. 117, 1520–1525 (2009).
Schecter, A. et al. Polybrominated diphenyl ethers (PBDEs) and hexabromocyclodecane (HBCD) in composite U.S. food samples. Environ. Health Perspect. 118, 357–362 (2010).
Byrne, S. et al. Exposure to polybrominated diphenyl ethers and perfluoroalkyl substances in a remote population of Alaska Natives. Environ. Pollut. 231, 387–395 (2017).
Dishaw, L. V., Macaulay, L. J., Roberts, S. C. & Stapleton, H. M. Exposures, mechanisms, and impacts of endocrine-active flame retardants. Curr. Opin. Pharmacol. 19, 125–133 (2014).
Makey, C. M. et al. Polybrominated diphenyl ether exposure and thyroid function tests in North American adults. Environ. Health Perspect. 124, 420–425 (2016).
Hallgren, S., Sinjari, T., Hakansson, H. & Darnerud, P. O. Effects of polybrominated diphenyl ethers (PBDEs) and polychlorinated biphenyls (PCBs) on thyroid hormone and vitamin A levels in rats and mice. Arch. Toxicol. 75, 200–208 (2001).
Zhou, T., Ross, D. G., DeVito, M. J. & Crofton, K. M. Effects of short-term in vivo exposure to polybrominated diphenyl ethers on thyroid hormones and hepatic enzyme activities in weanling rats. Toxicol. Sci. 61, 76–82 (2001).
Turyk, M. E. et al. Hormone disruption by PBDEs in adult male sport fish consumers. Environ. Health Perspect. 116, 1635–1641 (2008).
Dallaire, R., Dewailly, E., Pereg, D., Dery, S. & Ayotte, P. Thyroid function and plasma concentrations of polyhalogenated compounds in Inuit adults. Environ. Health Perspect. 117, 1380–1386 (2009).
Phillips, D. L. et al. Chlorinated hydrocarbon levels in human serum: effects of fasting and feeding. Arch. Environ. Contam. Toxicol. 18, 495–500 (1989).
Schisterman, E. F., Whitcomb, B. W., Buck Louis, G. M. & Louis, T. A. Lipid adjustment in the analysis of environmental contaminants and human health risks. Environ. Health Perspect. 113, 853–857 (2005).
Greenland, S., Pearl, J. & Robins, J. M. Causal diagrams for epidemiologic research. Epidemiology, 37–48 (1999).
Hornung, R. W. & Reed, L. D. Estimation of average concentration in the presence of nondetectable values. Appl. Occup. Environ. Hyg. 5, 46–51 (1990).
Schisterman, E. F., Vexler, A., Whitcomb, B. W. & Liu, A. The limitations due to exposure detection limits for regression models. Am. J. Epidemiol. 163, 374–383 (2006).
Yuan, J. et al. Elevated serum polybrominated diphenyl ethers and thyroid-stimulating hormone associated with lymphocytic micronuclei in Chinese workers from an E-waste dismantling site. Environ. Sci. Technol. 42, 2195–2200 (2008).
Jacobson, M. H. et al. Serum polybrominated diphenyl ether concentrations and thyroid function in young children. Environ. Res. 149, 222–230 (2016).
Zota, A. R. et al. Polybrominated diphenyl ethers, hydroxylated polybrominated diphenyl ethers, and measures of thyroid function in second trimester pregnant women in California. Environ. Sci. Technol. 45, 7896–7905 (2011).
Harley, K. G. et al. PBDE concentrations in women’s serum and fecundability. Environ. Health Perspect. 118, 699–704 (2010).
Hagmar, L., Bjork, J., Sjodin, A., Bergman, A. & Erfurth, E. M. Plasma levels of persistent organohalogens and hormone levels in adult male humans. Arch. Environ. Health 56, 138–143 (2001).
Bloom, M. et al. Environmental exposure to PBDEs and thyroid function among New York anglers. Environ. Toxicol. Pharmacol. 25, 386–392 (2008).
Lignell, S. et al. Maternal body burdens of PCDD/Fs and PBDEs are associated with maternal serum levels of thyroid hormones in early pregnancy: a cross-sectional study. Environ. Health 15, 016–0139 (2016).
Lin, S. M. et al. Negative associations between PBDE levels and thyroid hormones in cord blood. Int. J. Hyg. Environ. Health 214, 115–120 (2011).
Santin, A. P. & Furlanetto, T. W. Role of estrogen in thyroid function and growth regulation. J. Thyroid Res. 2011, 875125 (2011).
Stapleton, H. M., Kelly, S. M., Pei, R., Letcher, R. J. & Gunsch, C. Metabolism of polybrominated diphenyl ethers (PBDEs) by human hepatocytes in vitro. Environ. Health Perspect. 117, 197–202 (2009).
Roberts, S. C., Bianco, A. C. & Stapleton, H. M. Disruption of type 2 iodothyronine deiodinase activity in cultured human glial cells by polybrominated diphenyl ethers. Chem. Res. Toxicol. 28, 1265–1274 (2015).
Szabo, D. T. et al. Effects of perinatal PBDE exposure on hepatic phase I, phase II, phase III, and deiodinase 1 gene expression involved in thyroid hormone metabolism in male rat pups. Toxicol. Sci. 107, 27–39 (2009).
Allen, J. G. et al. PBDE flame retardants, thyroid disease, and menopausal status in U.S. women. Environ. Health 15, 60 (2016).
Vuong, A. M. et al. Maternal polybrominated diphenyl ether (PBDE) exposure and thyroid hormones in maternal and cord sera: the HOME study, Cincinnati, USA. Environ. Health Perspect. 123, 1079 (2015).
Zhao, X. et al. The correlation between polybrominated diphenyl ethers (PBDEs) and thyroid hormones in the general population: a meta-analysis. PLoS One 10, e0126989 (2015).
Wang, L. et al. The hormesis effect of BDE-47 in HepG 2 cells and the potential molecular mechanism. Toxicol. Lett. 209, 193–201 (2012).
Llabjani, V., Trevisan, J., Jones, K. C., Shore, R. F. & Martin, F. L. Derivation by infrared spectroscopy with multivariate analysis of bimodal contaminant-induced dose-response effects in MCF-7 cells. Environ. Sci. Technol. 45, 6129–6135 (2011).
Meerts, I. A. et al. Potent competitive interactions of some brominated flame retardants and related compounds with human transthyretin in vitro. Toxicol. Sci. 56, 95–104 (2000).
Hamers, T. et al. Biotransformation of brominated flame retardants into potentially endocrine-disrupting metabolites, with special attention to 2,2′,4,4′-tetrabromodiphenyl ether (BDE-47). Mol. Nutr. Food Res. 52, 284–298 (2008).
Ren, X. M. & Guo, L. H. Assessment of the binding of hydroxylated polybrominated diphenyl ethers to thyroid hormone transport proteins using a site-specific fluorescence probe. Environ. Sci. Technol. 46, 4633–4640 (2012).
Zheng, X. et al. Accumulation and biotransformation of BDE-47 by zebrafish larvae and teratogenicity and expression of genes along the hypothalamus–pituitary–thyroid axis. Environ. Sci. Technol. 46, 12943–12951 (2012).
Zota, A. R. et al. A temporal comparison of PBDEs, OH-PBDEs, PCBs, and OH-PCBs in the serum of second trimester pregnant women recruited from San Francisco General Hospital, California. Environ. Sci. Technol. 47, 11776–11784 (2013).
Canaris, G. J., Manowitz, N. R., Mayor, G. & Ridgway, E. The Colorado thyroid disease prevalence study. Arch. Intern. Med. 160, 526–534 (2000).
Åsvold, B. O., Bjøro, T., Nilsen, T. I. L. & Vatten, L. J. Association between blood pressure and serum thyroid-stimulating hormone concentration within the reference range: a population-based study. J. Clin. Endocrinol. Metab. 92, 841–845 (2007).
Garber, J. R. et al. Clinical practice guidelines for hypothyroidism in adults: cosponsored by the American Association of Clinical Endocrinologists and the American Thyroid Association. Thyroid 22, 1200–1235 (2012).
Lewandowski, K. Reference ranges for TSH and thyroid hormones. Thyroid Res. 8, A17–A17 (2015).
Biondi, B. Thyroid and obesity: an intriguing relationship. J. Clin. Endocrinol. Metab. 95, 3614–3617 (2010).
Imaizumi, M. et al. Risk for ischemic heart disease and all-cause mortality in subclinical hypothyroidism. J. Clin. Endocrinol. Metab. 89, 3365–3370 (2004).
Rodondi, N. et al. Subclinical hypothyroidism and the risk of heart failure, other cardiovascular events, and death. Arch. Intern. Med. 165, 2460–2466 (2005).
Osterweil, D. et al. Cognitive function in non-demented older adults with hypothyroidism. J. Am. Geriatr. Soc. 40, 325–335 (1992).
Biondi, B. et al. Subclinical hyperthyroidism: clinical features and treatment options. Eur. J. Endocrinol. 152, 1–9 (2005).
Geyer, H. J. et al. Terminal elimination half-lives of the brominated flame retardants TBBPA, HBCD, and lower brominated PBDEs in humans. Organohalogen Compd. 66, 3867–3872 (2004).
Thuresson, K. et al. Apparent half-lives of hepta- to decabrominated diphenyl ethers in human serum as determined in occupationally exposed workers. Environ. Health Perspect. 114, 176–181 (2006).
Sjödin, A. et al. Serum concentrations of polybrominated diphenyl ethers (PBDEs) and polybrominated biphenyl (PBB) in the United States population: 2003–2004. Environ. Sci. Technol. 42, 1377–1384 (2008).
Stapleton, H. M. Instrumental methods and challenges in quantifying polybrominated diphenyl ethers in environmental extracts: a review. Anal. Bioanal. Chem. 386, 807–817 (2006).
Longhi, S. & Radetti, G. Thyroid function and obesity. J. Clin. Res. Pediatr. Endocrinol. 5, 40–44 (2013).
Rothman, K. J. No adjustments are needed for multiple comparisons. Epidemiology 1, 43–46 (1990).
Welfinger-Smith, G. et al. Organochlorine and metal contaminants in traditional foods from St. Lawrence Island, Alaska. J. Toxicol. Environ. Health, A 74, 1195–1214 (2011).
Hallgren, S. & Darnerud, P. O. Polybrominated diphenyl ethers (PBDEs), polychlorinated biphenyls (PCBs) and chlorinated paraffins (CPs) in rats-testing interactions and mechanisms for thyroid hormone effects. Toxicology 177, 227–243 (2002).
Schell, L. M. et al. Relationship of thyroid hormone levels to levels of polychlorinated biphenyls, lead, p,p’- DDE, and other toxicants in Akwesasne Mohawk youth. Environ. Health Perspect. 116, 806–813 (2008).
Crofton, K. M. et al. Thyroid-hormone-disrupting chemicals: evidence for dose-dependent additivity or synergism. Environ. Health Perspect. 113, 1549–1554 (2005).
Miller, V. M., Sanchez-Morrissey, S., Brosch, K. O. & Seegal, R. F. Developmental coexposure to polychlorinated biphenyls and polybrominated diphenyl ethers has additive effects on circulating thyroxine levels in rats. Toxicol. Sci. 127, 76–83 (2012).
Bloom, M. S., Jansing, R. L., Kannan, K., Rej, R. & Fitzgerald, E. F. Thyroid hormones are associated with exposure to persistent organic pollutants in aging residents of upper Hudson River communities. Int J Hyg Environ Health 217, 473–482 (2014).
Zeger, S. L. & Liang, K.-Y. Longitudinal data analysis for discrete and continuous outcomes. Biometrics, 121–130 (1986).
Acknowledgements
The authors would like to thank the many individuals who contributed to accomplishing this research including Jane Kava, Jesse Gologergen, Erika Apatiki, Kristi Apangalook, Tiffany Immingan, Millie Kingeekuk, Susie Booshu, Sharon Campbell-Aningayou, Naomi Madsen, Shelley Klein-Apatiki, Carolyn Kava, Carol Gologergen, Bobby Ungwiluk, Kevin Zweifel, and Heidi Zimmer. The authors also thank Dr. Erin Bell, Dr. Michael Bloom, Dr. Kurunthachalam Kannan, and Dr. Lawrence Schell at the University at Albany for their comments on the manuscript. This study was supported by the National Institute of Environmental Health Sciences (NIH R01ES019620 and 2RO1ES019620).
Author information
Authors and Affiliations
Contributions
S.B. contributed to data collection, data analysis and interpretation, and drafted the manuscript. P.M. contributed to study design, data collection and critically revised the manuscript. S.S.M. contributed to data collection and critically revised the manuscript. V.W. contributed to study design, data collection and critically revised the manuscript. F.v.H. contributed to study design and critically revised the manuscript. C.L.B. contributed to study design and critically revised the manuscript. D.C. contributed to study design and critically revised the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Byrne, S.C., Miller, P., Seguinot-Medina, S. et al. Associations between serum polybrominated diphenyl ethers and thyroid hormones in a cross sectional study of a remote Alaska Native population. Sci Rep 8, 2198 (2018). https://doi.org/10.1038/s41598-018-20443-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-20443-9
- Springer Nature Limited
This article is cited by
-
Polybrominated Diphenyl Ethers (PBDEs) in Marine Fish and Dietary Exposure in Newfoundland
EcoHealth (2022)
-
PFAS and PBDEs in traditional subsistence foods from Sivuqaq, Alaska
Environmental Science and Pollution Research (2022)
-
A Systematic Review of Environmental Health Outcomes in Selected American Indian and Alaska Native Populations
Journal of Racial and Ethnic Health Disparities (2020)
-
Structural studies on the endocrine-disrupting role of polybrominated diphenyl ethers (PBDEs) in thyroid diseases
Environmental Science and Pollution Research (2020)