Abstract
Background
Women have elevated rates of thyroid disease compared to men. Environmental toxicants have been implicated as contributors to this dimorphism, including polybrominated diphenyl ethers (PBDEs), flame retardant chemicals that disrupt thyroid hormone action. PBDEs have also been implicated in the disruption of estrogenic activity, and estrogen levels regulate thyroid hormones. Post-menopausal women may therefore be particularly vulnerable to PBDE induced thyroid effects, given low estrogen reserves. The objective of this study was to test for an association between serum PBDE concentrations and thyroid disease in women from the United States (U.S.), stratified by menopause status.
Methods
Serum PBDE concentrations (BDEs 47, 99, 100 and 153) from the National Health and Examination Survey (NHANES) and reports on thyroid problems were available in the NHANES 2003–2004 cycle. Odds ratios (ORs) were calculated using multivariate logistic regression models accounting for population-weighted survey techniques and controlling for age, body mass index (BMI), education, smoking, alcohol consumption and thyroid medication. Menopause status was obtained by self-reported absence of menstruation in the previous 12 months and declared menopause.
Results
Women in the highest quartile of serum concentrations for BDEs 47, 99, and 100 had increased odds of currently having thyroid disease (ORs: 1.5, 1.8, 1.5, respectively) compared to the reference group (1st and 2nd quartiles combined); stronger associations were observed when the analysis was restricted to postmenopausal women (ORs: 2.2, 3.6, 2.0, respectively).
Conclusion
Exposure to BDEs 47, 99, and 100 is associated with thyroid disease in a national sample of U.S. women, with greater effects observed post-menopause, suggesting that the disruption of thyroid signaling by PBDEs may be enhanced by the altered estrogen levels during menopause.
Similar content being viewed by others
Background
Fire safety standards promulgated in California in the late 1970’s have led to the proliferation of chemical flame retardants (FRs) used in consumer products worldwide [1]. Brominated flame retardant compounds are used as additives in products at up to 20 % by weight of the product [2]. Precisely because they are used as additives, rather than covalently bound to a polymer matrix, these halogenated FRs can and do migrate from their source products into the indoor and outdoor environment [3]. In fact, the global use of one class of environmentally-persistent flame retardant chemicals over a 35-year period, polybrominated diphenyl ethers (PBDEs), has led to their near ubiquitous presence in animals, abiotic matrices and food, as well as in air, dust and surfaces of indoor environments [4–17].
PBDEs share a similar structure to polychlorinated biphenyls (PCBs), polybrominated biphenyls (PBBs), tetrabromobisphenol A (TBBPA), triclosan, and the halogenated-phenyl ring of thyroid hormone thyroxine (T4), with the potential for 209 different congeners based on the number and position of the bromine within the aromatic rings. PBDEs were manufactured in three commercial products—PentaBDE, OctaBDE, DecaBDE—each of which is dominated by one or more congeners (BDEs 47 (2,2′4,4′-tetra-bromodiphenyl ether), 99 (2,2′4,4′5-penta-bromodiphenyl ether), 100 (2,2′,4,4′,6-penta-bromodiphenyl ether); BDE 183 (2,2′,3,4,4′,5′,6-hepta-bromodiphenly ether); BDE 209 (deca-bromodiphenyl ether), respectively). The use of PBDEs as flame retardants have been phased out or banned in some countries, and updated California fire safety standards no longer require PBDEs or other flame retardant chemicals to be used in furniture [18]. However, exposure is expected to continue for several decades because of the reservoir of these chemicals that exist in consumer products that have long durations of use (e.g. couches), and the environmental stability of PBDEs. The most recent data available from NHANES shows that a reduction in PBDEs in serum was not yet observed on a national level following the phase-out of several PBDEs in 2004 [19], although more current biomonitoring data suggest that levels are decreasing [20, 21].
We have known for over 20 years that some PBDEs are carcinogenic. A study by the National Toxicology Program reported in 1986 found that DecaBDE causes thyroid and liver tumors in rats and mice [22]. More recently, a NTP study on PBDEs found that DE71, the major commercial mixture of PentaBDE, is a two-species, two-sex carcinogen [23]. Epidemiological evidence demonstrates that PBDEs are also endocrine-disrupting compounds that interfere with thyroid hormone action [24], reproduction, and neurodevelopment [25–30]. Subtle changes in circulating thyroid hormone concentrations (e.g., free and total T3 (triiodothyronine), T4, TSH (thyroid stimulating hormone)) are associated with many adverse health effects. Thyroid hormones regulate the growth and differentiation of the brain and are therefore critical for neurodevelopment [31]; the developing fetus relies on maternal thyroid hormone until week 11 of gestation [32] before beginning to produce endogenous hormones, and doesn’t produce sufficient hormone for its own needs until approximately week 20 [33]. Further, because the thyroid is a modulator for many of the body’s organs, studies have linked thyroid conditions with other diseases like kidney [34], liver [35], and heart [36].
Thyroid disorders disproportionately impact women [37], and the rates of thyroid cancer are increasing globally, with women having higher rates of thyroid cancer than men, and older women having higher rates than younger women [38]. We know of only one study that evaluated PBDE-associated health effects in a representative U.S. population sample (NHANES) and those researchers found associations with diabetes and metabolic syndrome [39], but did not evaluate thyroid disease as an outcome. Further, we know of no research related to the potential sensitivity of menopausal women to thyroid disease based on PBDE concentration, despite the well-described role of estrogen on thyroid function [40] and the ability of PBDEs to exert estrogenic effects [41]. The objective of our research was to explore the relationship between PBDE exposures in women and thyroid disease using nationally-representative (U.S.) data from the NHANES.
Methods
Exposure Variable—PBDEs
At the time of publication, NHANES reported PBDE concentrations in serum for individuals (i.e., not pooled) for only one NHANES cycle: 2003–2004. We analyzed the data for the four PBDE congeners reported by NHANES (BDEs 47, 99, 100 and 153), all primarily associated with the PentaBDE commercial product; information on BDE 209, the primary congener of the DecaBDE commercial product, has yet to be reported in any NHANES cycle. Other researchers thoroughly describe the NHANES analytical methods for serum PBDE measurements and summary statistics for the population-weighted concentrations [42]. We created exposure categories based on quartiles of lipid-adjusted, sex-specific serum concentrations for each congener as reported by Sjodin et al. [42]. In addition, we generated a variable for total sum of lipid-adjusted PBDE concentrations, which combined the concentrations from the four congeners (ΣBDE).
Outcome variable—thyroid disease
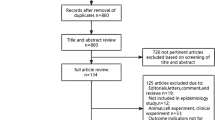
Thyroid hormone measurements are available in NHANES but did not overlap completely with the participants for whom PBDE serum measurements were also available. The NHANES questionnaire administered to all participants in NHANES 2003–2004 included two questions related to thyroid disease: MCQ160m “Has a doctor or other health professional ever told (you/SP) that (you/s/he) . . . had a thyroid problem?” and, MCQ170m “(Do you/Does SP) still . . . have a thyroid problem?”. Responses included: yes, no, don’t know or missing. For our analyses, if a subject responded “don’t know” then the data were considered missing. We used a combination of the thyroid questions to develop an outcome variable ‘current thyroid problem’. We defined having a current thyroid problem as an affirmative answer to ever having a thyroid problem and still have a thyroid problem. The sample size for participants with both PBDE measurements and thyroid disease status available are as follows: BDE 47, n = 1396; BDE 99, n = 1378; BDE 100, n = 1413; BDE 153, n = 1413.
Thyroid disease prevalence
To calculate the survey-weighted prevalence of thyroid problems among the NHANES population, we generated weighted proportions by gender and post-menopause for questions MCQ160m (ever) and MCQ170m (current) according to the NHANES descriptive statistical methodology [43].
Statistical analysis
We performed statistical analyses using STATA statistical software package, version 13.0 (StatCorp, College Station, TX). To estimate odds ratios and 95 % confidence intervals for development of disease accounting for the clustered sampling design in NHANES Control and Prevention (CDC), we used multivariate logistic regression modeling following procedures recommended by the Centers for Disease Control and Prevention [44]. We performed logistic regression analyses in this study using the STATA ‘svy’ commands to account for NHANES strata and cluster variables, and represent population-weighted results. To stratify the analysis to women-only, we assigned men a near zero weight in accordance with NHANES guidance. To stratify for women who were postmenopausal, we created a variable based on women who had not had one menstrual period in the last 12 months (RHQ031) and also indicated the reason for not having a period was post-menopause/hysterectomy (RHD042). Similar to the gender stratification, we assigned near zero weights to all men and women who were not postmenopausal.
We adjusted multivariate models for several potential confounders, using a similar methodology from a recent study examining thyroid effects in the NHANES study [45]. Covariates included in the model, with groupings in parentheses, were: race/ethnicity (Mexican American, other Hispanic, non-Hispanic White, non-Hispanic Black, other race (including multi-racial)); age (continuous variable); body mass index (BMI) (less than 25, 25–30, >30), education (less than high school, high school, more than high school), smoking (ever/never smoked more than 100 cigarettes in lifetime); alcohol consumption (never consume or at least one drink per week); and current hormone use (taking birth control pills now, now using Depo-Provera or injectables, taking estrogen only pills now, taking progestin only pills now, taking estrogen/progestin now, using estrogen-only patches now, using estrogen/progestin patch now).
In the primary models, the first and second quartile exposure groups (Q1 and Q2) were combined to increase statistical power and match the approach necessitated for BDE 99 (for BDE 99, the median serum concentration reported by Sjodin et al. [44] was ‘non-detect’), similar to the approach used by Melzer et al. [45].
Results
In the 2003–4 NHANES survey, the prevalence of women reporting ever being told by a doctor that they had a thyroid problem was five times higher than the prevalence reported by men (16 % v. 3 %; p < 0.05). This was similar to the finding for those reporting a current thyroid problem (13 % v. 2 %; p < 0.05) (Table 1). In comparisons of postmenopausal and premenopausal women, we found that the prevalence of ever having a thyroid problem and the prevalence of currently having a thyroid problem was twice as high for postmenopausal women (ever: 24 % v. 12 %, p < 0.05; current: 18 % v. 10 %, p < 0.10).
In fully-adjusted, survey-weighted logistic regression models we found that women in the highest quartile of serum concentrations for BDE 47, 99, 100 and ΣBDE, had a greater odds of currently having a thyroid problem, compared to women in the lower quartiles of serum concentrations (Table 2); statistically significant associations were observed for BDE 47 (OR: 1.48; 95 % CI: 1.05–2.09), BDE 99 (OR: 1.78; 95 % CI: 1.16–2.75) and ΣBDE (OR: 1.61; 95 % CI: 1.1–2.4), and marginally significant for BDE 100 (OR: 1.50; 95 % CI: 0.97–2.31). The point estimates of the odds ratios for the 3rd quartile were less than unity, although only statistically significant for the ΣBDE variable.
For all PBDE congeners except for BDE 153, the odds ratios for women in the highest exposure category were higher when the analysis was restricted to postmenopausal women. For example, for BDE 47, when all women were included in the analysis, the odds of having a current thyroid problem was 1.5 compared to 2.1 for just postmenopausal women. For BDE 99, this difference was two-fold, with postmenopausal women in the highest exposure category having 3.6 times the odds of having a current thyroid problem (95 % CI: 1.1–11.8), compared to 1.5 times the odds observed for all women (95 % CI: 0.97–2.3). The analysis for a current thyroid problem post-menopause showed odds ratios that were less than unity for the 3rd quartile.
The NHANES dataset did not contain enough men with current thyroid disease for our models to converge in a men-only analysis. In an analysis with all men and women combined, we did not find significant associations between the exposure categories and current thyroid disease (Table 1). Similarly, we originally attempted to explore thyroid cancer specifically, but this NHANES cycle only had nine participants reporting thyroid cancers, precluding us from performing regression analysis.
Discussion
Our study found a positive association between PBDEs in serum and thyroid disease in U.S. women, a finding that suggests that effects of PBDEs on thyroid hormones, documented extensively in toxicological and epidemiological studies, is leading to significant downstream impacts. For example, increased PBDE levels in animals, primarily in mice and rats studies, have been associated with altered T4 and T3 levels [46–50] suggesting thyroid dysregulation in vivo, with several proposed mechanisms of action [51–54]. Associations between thyroid hormone levels and PBDEs have also been observed for animals in the wild, including birds, fish, and polar bears [55–57]. In humans, there are many studies that describe similar findings of associations between PBDE concentrations in serum and thyroid hormone concentrations [21, 25, 26, 29, 58–61].
One possible mechanism accounting for the PBDE-induced reduction in serum T4 is displacement of T4 from the serum binding protein transthyretin (TTR) or thyroxine binding globulin (TBG) [54]—similar to what has been previously observed for polychlorinated biphenyls (PCBs) [62]. (Significantly, a study examining the effects of chemical mixtures observed a potentially synergistic effect on T4 levels with co-exposures to BDE 47 and PCBs [47]). T3 and T4 travel in blood bound to plasma proteins; only 0.04 % of T4 and 0.4 % of T3 are unbound (or “free”), and consequently, available for entry and action in target tissues [32]. The tetra-brominated congeners, BDE 47 in particular, share a similar structure to T4, with both having the diphenyl ether structure and four halogens (iodine for T4; bromine for BDE47). A major difference is that T4 has a hydroxyl group on one of the rings, positioned between the two halogens. However, PBDEs are hydroxylated in vivo and, when this occurs in the meta position, it yields 3-OH-BDE47, which also has the hydroxyl group positioned between two halogens [53].
Along with epidemiological and toxicological evidence showing perturbations in thyroid hormone concentrations, we are now beginning to understand plausible mechanisms by which this disruption is occurring; the similarity of structures of exogenous chemicals to endogenous hormones may be leading to competition for receptor binding sites, causing inhibition or amplification. For thyroid hormones, a study by Cao et al. [52] found that hydroxylated PBDEs bind to transthyretin (TTR) and thyroxine-binding globulin (TBG) at the same sites as the target hormone, T4. Hamers et al. measured binding affinities for PBDEs and metabolites to TTR and reported that the hydroxylated metabolites bound 160–1600 times more avidly than the parent compounds [63]. Further, a study by Butt and Stapleton [51] found that hydroxylated PBDEs are potent inhibitors of thyroid hormone sulfation. Also relevant to our study that focused on menopausal status, hydroxylated PBDEs have been shown to compete with estrogen enzymes. A crystallographic analysis examining the binding affinity of 3-OH-BDE47 to a hormone enzyme, estrogen sulfotransferase, demonstrated that the first phenolic group positions the compound within the enzyme similarly to how 17βestradiol would situate [41]. Further, the authors demonstrated that this positioning creates additional hydrogen bonding via the hydroxyl group, also similar to 17βestradiol, while accommodating the two halogens.
Perhaps the most striking and unique finding in this study is that the odds of having a current thyroid problem associated with PBDEs are so much higher in postmenopausal women. One hypothesis is that this is related to the change in hormone concentrations in postmenopausal women and the affinity of PBDEs to binding sites for both estrogen and thyroid hormones. Menopause is initiated when the ovaries discontinue producing two hormones, estrogen and progesterone. In at least two ways, the strong binding affinity of OH-PBDEs with estrogen sulfotransferase can interfere with the change in estrogen levels that occur during menopause. First, with less estrogen in the system, there may be increased metabolism of PBDEs by this estrogen enzyme [41]. Second, the OH-PBDEs may be competing for these binding sites that are critical for the removal of circulating estrogen produced by other tissues, leading to higher than expected levels of circulating estrogen. This potential interference of the estrogen clearance pathway in the liver via estrogen sulfotransferase, in and of itself, would not explain the higher odds of thyroid problems. However, estrogen (and androgen) can increase the levels of serum thyroxine binding globulin (TBG), interfering with one of the three primary proteins responsible for thyroid hormone transport in serum. In addition to these potential impacts on thyroid hormone via estrogen-mediated pathways, PBDEs can also have a direct impact on thyroid hormones through serum binding proteins outside of the mechanism that involves estrogen; PBDEs show a strong affinity for both TBG and another serum binding protein, transthyretin, and therefore can have a more direct impact on circulating thyroid hormone levels [41, 52]. All of this suggests the disruption of thyroid signaling by PBDEs that may be enhanced by the altered estrogen levels during menopause.
Results from epidemiologic studies on the effects of PBDEs on thyroid hormones are consistent with the toxicological evidence, in that they suggest interference with thyroid hormone regulation. However, in some epidemiologic studies, estimates of PBDE exposure are positively associated with measures of thyroid function, and in others the opposite pattern is observed. For example, in a study of 297 infants, Herbstman et al. observed that cord blood serum PBDE levels were associated with reduced total and free T4 levels [27]. Conversely, Turyk et al. (2008) conducted a study of 405 adult male sport fish consumer and observed a positive trend between free T4 and PBDE serum levels [61]. A more recent study found a positive association between PBDEs in serum of pregnant women and serum total and free T4 and T3 [29].
There are seeming inconsistencies, then, in the epidemiological literature, with some studies showing positive associations with PBDEs and thyroid hormones and others showing negative associations. We note that the PBDE serum concentrations in many of these cohort studies are in different ranges of the concentration distribution found in the U.S. population, with some representing the low-end of exposure and others on the high-end (selected studies; Table 3) [21, 25, 26, 29, 58–60]. Moreover, it seems reasonable to consider the possibility that adults and fetuses have many differences in thyroid physiology that could account for at least some of these differences. However, we hypothesize that a potential explanation of the differences in findings is due to: 1) non-monotonic dose responses to PBDEs, and 2) where on the dose–response range the studies were performed. Within our study using NHANES data, which represents the full range of population exposures in the U.S. and therefore in theory encompasses the ranges found in these other studies, we also observed that the shape of the response curve is non-linear and suggests a non-monotonic dose response curve (NMDRC) may exist (e.g. Q1 + Q2 have higher odds of current thyroid problem relative to Q3; Q4 also has higher odds of current thyroid problem relative to Q3). Vandenberg et al. [64] published a seminal paper evaluating the literature related to endocrine disrupting chemicals and low-dose and nonmonotonic dose responses, with significant implications to our current approach to protecting public health [65]. Vandenberg et al. state that NMDRCs are, “not the exception, but should be expected and perhaps even common,” and that it is no longer acceptable to dismiss NMDRCs based on a lack of mechanism because there are now several potential mechanisms to explain these phenomena [64]. These include cytotoxicity (toxic at high concentrations and biologically active at low concentrations), cell- and tissue-specific receptors and co-factors, receptor sensitivity, and receptor down-regulation and desensitization, among other proposed mechanisms. In our analysis, individuals in the first and last quartiles (Q1 + Q2 and Q4) have higher odds of a thyroid problem, compared to Q3. Results from the other study of PBDEs using NHANES that focused on diabetes and metabolic syndrome were also suggestive of a NMDRC for BDE 99 [39]. It is possible that the existence of a NMDRC for PBDEs may explain the seeming inconsistency across studies examining the relationship between PBDEs and thyroid hormones. The serum concentrations in these studies generally fall within very different ranges of the full distribution of serum concentrations observed in NHANES (Table 3). For example, the central tendency PBDE concentrations in Zota et al. [21] fall within the Q4 of NHANES, and they found that PBDEs were associated lower free T4. In contrast, the central tendency PBDE concentrations in Abdelouahab et al. [25] fall within Q3 of NHANES, and they found that PBDEs were associated with the opposite effect (higher free T4). More research is needed to fully explore this hypothesis.
A limitation of our study is the inability of this analysis to determine causality because the data are cross-sectional; thus, we do not have temporality captured in the data to know if the exposure preceded the outcome. Also, the standard approach to analysis of serum concentrations for lipophilic compounds is to adjust the concentrations based on lipid-content in the serum and report the results as ‘lipid-adjusted’. This approach, however, may have a critical limitation. Thyroid hormones affect lipid metabolism at several points—synthesis, mobilization and degradation [66]. If a person has thyroid disease not caused by PBDE exposure, and the disease increases lipid metabolism leading to lower lipids in the bloodstream, then adjusting PBDEs by this lower lipid concentration yields a higher lipid-adjusted PBDE concentration, creating the appearance of a positive association between thyroid disease and PBDEs. Therefore, it is possible that women who self-report current thyroid disease have elevated lipid-adjusted PBDE concentrations in serum as a result of having thyroid disease. Further, even if serum concentrations are not adjusted for lipid content, the concentration in serum is still impacted by lipid content in the bloodstream, so a simple solution cannot be using serum concentrations that are not lipid-adjusted (we performed an analysis using wet-weight concentrations and found similar results as when we used lipid-normalized concentrations; Additional file 1: Table S1). Considering these points, it is plausible then that the relationship of thyroid dysfunction to PBDEs could be a function of reverse causality, with PBDE concentrations, lipid-adjusted or not, simply an outcome of thyroid dysfunction and altered lipid metabolism.
Another potential limitation of this study is the lack of specificity in the NHANES questionnaire regarding thyroid problems. NHANES is a nationally representative health survey (U.S.) that, due to its breadth, only covers thyroid-related disease with three non-specific questions: 1) Has your doctor ever told you that you have a thyroid problem, 2) Do you still have a thyroid problem, and 3) Do you have thyroid cancer. Yet, ‘thyroid problem’ and ‘thyroid cancer’ encompass a wide range of specific illnesses (e.g., hyperthyroidism, hypothyroidism, nodules, thyroiditis, goiter; papillary thyroid cancer, follicular thyroid cancer, medullary thyroid cancer), each with their own potential etiology (e.g., iodine deficiency, Graves’ disease, Hashimoto’s disease, radiation, environmental chemicals). Despite the lack of specificity in the NHANES questions on the outcome variables, which would likely bias the results toward a null finding, we still observed strong and consistent associations between PBDEs in serum and thyroid problems. Last, the congeners available for analysis in NHANES are also from the same commercial product and are correlated in environmental and body burden samples [5, 42]. Therefore, we cannot rule out that one congener is driving the observed associations seen for several congeners.
Overall, the findings from this analysis of data reported in NHANES provide additional evidence of the impact of PBDEs on the thyroid. We also observed a stronger effect for postmenopausal women. Additional research is warranted to confirm these findings, particularly when the next cycle of NHANES data with PBDE serum concentrations is made available.
Conclusion
We found that women with the highest flame retardant concentrations in their blood were significantly more likely to have a thyroid problem, with stronger associations found for post-menopausal women. Specifically, women with lipid-adjusted serum concentrations of BDE 47, 99 and 100 in the highest quartile of exposure had higher odds of having a current thyroid problem compared to women with lower serum concentrations. These associations were much stronger in an analysis that was restricted to postmenopausal women.
Ethics
This research did not require ethics approval by an Institutional Review Board (IRB) as the data are de-identified data from the National Health and Nutrition Examination Survey (NHANES), a publicly available dataset.
Abbreviations
- ΣBDE:
-
Sum of BDEs 47, 99, 100,183
- BDE 47:
-
2,2′4,4′-tetra-bromodiphenyl ether
- BDE 99:
-
2,2′4,4′5-penta-bromodiphenyl ether
- BDE 100:
-
2,2′,4,4′,6-penta-bromodiphenyl ether
- BDE 183:
-
2,2′,3,4,4′,5′,6-hepta-bromodiphenly ether
- BDE 209:
-
deca-bromodiphenyl ether
- BMI:
-
body mass index
- CDC:
-
Centers for Disease Control and Prevention
- FR:
-
flame retardant
- NHANES:
-
National Health and Nutrition Examination Survey
- NMDRC:
-
non-monotonic dose response curve
- NTP:
-
National Toxicology Program
- OR:
-
odds ratio
- PBB:
-
polybrominated biphenyl
- PBDE:
-
polybrominated diphenyl ether
- PCB:
-
polychlorinated biphenyl
- T3 :
-
triiodothyronine
- T4 :
-
Thyroxine
- TBBPA:
-
Tetrabromobisphenol A
- TBG:
-
thyroxine-binding globulin
- TSH:
-
thyroid stimulating hormone
- TTR:
-
transthyretin
References
State of California. Technical Bulletin 117: Requirements, Test Procedure, and Apparatus for Testing the Flame Retardance of Resilient Filling Materials Used in Upholstered Furniture. North Highlands: Bureau of Home Furnishings and Thermal Insulation; 2000.
Allen JG, McClean MD, Stapleton HM, Webster TF. Linking pbdes in house dust to consumer products using x-ray fluorescence. Environ Sci Technol. 2008;42:4222–8.
Webster TF, Harrad S, Millette J, Holbrook R, Davis J, Stapleton HM, et al. Identifying transfer mechanisms and sources of decabromodiphenyl ether (BDE 209) in indoor environments using environmental forensic microscopy. Environ Sci Technol. 2009; es-2008-03139w.R1.
Allen JG, McClean MD, Stapleton HM, Nelson JW, Webster TF. Personal exposure to polybrominated diphenyl ethers (PBDEs) in residential indoor air. Environ Sci Technol. 2007;41:4574–9.
Allen JG, McClean MD, Stapleton HM, Webster TF. Critical factors in assessing exposure to pbdes via house dust. Environ Int. 2008;34:1085–91.
Allen JG, Stapleton HM, Vallarino J, McNeely E, McClean MD, Harrad SJ, et al. Exposure to flame retardant chemicals on commercial airplanes. Environ Health. 2013;12:17.
Allen JG, Sumner AL, Nishioka MG, Vallarino J, Turner DJ, Saltman HK, et al. Air concentrations of pbdes on in-flight airplanes and assessment of flight crew inhalation exposure. J Expo Sci Environ Epi. 2013;23:337–42.
Chen D, Martin P, Burgess NM, Champoux L, Elliott JE, Forsyth DJ, et al. European starlings (sturnus vulgaris) suggest that landfills are an important source of bioaccumulative flame retardants to canadian terrestrial ecosystems. Environ Sci Technol. 2013;47:12238–47.
Dodson RE, Perovich LJ, Covaci A, Van den Eede N, Ionas AC, Dirtu AC, et al. After the PBDE phase-out: A broad suite of flame retardants in repeat house dust samples from california. Environ Sci Technol. 2012;46:13056–66.
Fraser AJ, Webster TF, McClean MD. Diet contributes significantly to the body burden of PBDEs in the general us population. Environ Health Perspect. 2009;117:1520–5.
Harrad S, Hunter S. Concentrations of polybrominated diphenyl ethers in air and soil on a rural–urban transect across a major uk conurbation. Environ Sci Technol. 2006;40:4548–53.
Lagalante AF, Oswald TD, Calvosa FC. Polybrominated diphenyl ether (PBDE) levels in dust from previously owned automobiles at united states dealerships. Environ Int. 2009;35:539–44.
Letcher RJ, Gebbink WA, Sonne C, Born EW, McKinney MA, Dietz R. Bioaccumulation and biotransformation of brominated and chlorinated contaminants and their metabolites in ringed seals (pusa hispida) and polar bears (ursus maritimus) from east greenland. Environ Int. 2009;35:1118–24.
McKinney MA, Letcher RJ, Aars J, Born EW, Branigan M, Dietz R, et al. Flame retardants and legacy contaminants in polar bears from alaska, canada, east greenland and svalbard, 2005–2008. Environ Int. 2011;37:365–74.
Schecter A, Papke O, Harris TR, Tung KC, Musumba A, Olson J, et al. Polybrominated diphenyl ether (PBDE) levels in an expanded market basket survey of U.S. Food and estimated pbde dietary intake by age and sex. Environ Health Perspect. 2006;114:1515–20.
Watkins DJ, McClean MD, Fraser AJ, Weinberg J, Stapleton HM, Sjodin A, et al. Exposure to PBDEs in the office environment: Evaluating the relationships between dust, handwipes, and serum. Environ Health Perspect. 2011;119:1247–52.
Weschler CJ, Nazaroff WW. SVOC partitioning between the gas phase and settled dust indoors. Atmos Environ. 2010;44:3609–20.
State of California. Technical bulletin 117–2013: Requirements, test procedure, and apparatus for testing the smolder resistance materils used in in upholstered furniture. Sacramento: Department of Consumer Affairs; 2013.
Sjodin A, Jones RS, Caudill SP, Wong LY, Turner WE, Calafat AM. Polybrominated diphenyl ethers, polychlorinated biphenyls, and persistent pesticides in serum from the National Health and Nutrition Examination Survey: 2003–2008. Environ Sci Technol. 2014;48:753–60.
Guo W, Holden A, Smith SC, Gephart R, Petreas M, Park JS. PBDE levels in breast milk are decreasing in California. Chemosphere. 2015. doi:10.1016/j.chemosphere.2015.11.032.
Zota A, Linderholm L, Park JS, Petreas M, Guo T, Privalsky M, et al. Temporal comparison of PBDEs, OH-PBDEs, PCBs, and OH-PCBs in the serum of second trimester pregnant women recruited from San Francisco General Hospital. California Environ Sci Technol. 2013;47(20):11776–84.
National Toxicology Program. Toxicology and carcinogenesis studies of decabromodiphenyl oxide (cas no. 1163-19-5) in f344/n rats and b6c3f1 mice (feed studies).1986. Available from: http://ntp.niehs.nih.gov/results/pubs/longterm/reports/longterm/tr300399/abstracts/tr309/index.html [Accessed 3 February 2016]
National Toxicology Program. TR-589: Pentabromodiphenyl oxide (technical) (de 71): Technical report pathology tables and curves. 2014. Available from: http://ntp.niehs.nih.gov/results/path/tablelistings/longterm/tr500599/tr589/index.html [Accessed 3 February 2016].
Zoeller RT, Bergman A, Becher G, Bjerregaard P, Bornman R, Brandt I, et al. A path forward in the debate over health impacts of endocrine disrupting chemicals. Environ Health. 2014;13:118.
Abdelouahab N, Langlois MF, Lavoie L, Corbin F, Pasquier JC, Takser L. Maternal and cord-blood thyroid hormone levels and exposure to polybrominated diphenyl ethers and polychlorinated biphenyls during early pregnancy. Am J Epi. 2013;178:701–13.
Chevrier J, Harley KG, Bradman A, Gharbi M, Sjodin A, Eskenazi B. Polybrominated diphenyl ether (PBDE) flame retardants and thyroid hormone during pregnancy. Environ Health Perspect. 2010;118:1444–9.
Herbstman JB, Sjodin A, Apelberg BJ, Witter FR, Halden RU, Patterson DG, et al. Birth delivery mode modifies the associations between prenatal polychlorinated biphenyl (PCB) and polybrominated diphenyl ether (PBDE) and neonatal thyroid hormone levels. Environ Health Perspect. 2008;116:1376–82.
Meeker JD, Johnson PI, Camann D, Hauser R. Polybrominated diphenyl ether (PBDE) concentrations in house dust are related to hormone levels in men. Sci Total Environ. 2009;407(10):3425–9. doi:10.1016/j.scitotenv.2009.01.030. Epub 2009 Feb 10.
Stapleton HM, Eagle S, Anthopolos R, Wolkin A, Miranda ML. Associations between polybrominated diphenyl ether (PBDE) flame retardants, phenolic metabolites, and thyroid hormones during pregnancy. Environ Health Perspect. 2011;119(10):1454–9.
Zota AR, Park JS, Wang Y, Petreas M, Zoeller RT, Woodruff TJ. Polybrominated diphenyl ethers, hydroxylated polybrominated diphenyl ethers, and measures of thyroid function in second trimester pregnant women in california. Environ Sci Technol. 2011;45:7896–905.
Haddow JE, Palomaki GE, Allan WC, Williams JR, Knight GJ, Gagnon J, et al. Maternal thyroid deficiency during pregnancy and subsequent neuropsychological development of the child. N Engl J Med. 1999;341:549–55.
Gardner DG, Shoback DM, Greenspan FS. Greenspan's Basic & Clinical Endocrinology. Part 9th. New York: McGraw-Hill Medical; 2011.
Brent GA. Maternal hypothyroidism: Recognition and management. Thyroid: Official Journal of the American Thyroid Association. 1999;9:661–5.
Iglesias P, Diez JJ. Thyroid dysfunction and kidney disease. European Journal of Endocrinology / European Federation of Endocrine Societies. 2009;160:503–15.
Huang MJ, Liaw YF. Clinical associations between thyroid and liver diseases. J Gastroenterol Hepatol. 1995;10:344–50.
Rodondi N, Bauer DC, Cappola AR, Cornuz J, Robbins J, Fried LP, et al. Subclinical thyroid dysfunction, cardiac function, and the risk of heart failure. The cardiovascular health study. J Am Col Cardiol. 2008;52:1152–9.
Canaris GJ, Manowitz NR, Mayor G, Ridgway EC. The colorado thyroid disease prevalence study. Arch Internal Med. 2000;160:526–34.
Pellegriti G, Frasca F, Regalbuto C, Squatrito S, Vigneri R. Worldwide increasing incidence of thyroid cancer: Update on epidemiology and risk factors. J Cancer Epidemiol. 2013;965212.
Lim J-S, Lee D-H, Jacobs DR. Association of brominated flame retardants with diabetes and metabolic syndrome in the U.S. Population, 2003–2004. Diabetes Care. 2008;31:1802–7.
Santin AP, Furlanetto TW. Role of estrogen in thyroid function and growth regulation. J Thyroid Res. 2011;875125.
Gosavi RA, Knudsen GA, Birnbaum LS, Pedersen LC. Mimicking of estradiol binding by flame retardants and their metabolites: A crystallographic analysis. Environ Health Perspect. 2013;121:1194–9.
Sjödin A, Wong L-Y, Jones RS, Park A, Zhang Y, Hodge C, et al. Serum concentrations of polybrominated diphenyl ethers (PBDEs) and polybrominated biphenyl (PBB) in the United States population: 2003–2004. Environ Sci Technol. 2008;42:1377–84.
Centers for Disease Control and Prevention (CDC). Continuous NHANES web tutorial: Descriptive statistics. 2014. Available from: http://www.cdc.gov/nchs/tutorials/NHANES/NHANESAnalyses/descriptivestatistics/descriptive_statistics_intro.htm [Accessed 2 April 2015].
Centers for Disease Control and Prevention (CDC). Continuous NHANES web tutorial: NHANES analyses, logistic regression. 2014. Available from: http://www.cdc.gov/nchs/tutorials/NHANES/NHANESAnalyses/logisticregression/logistic_regression_intro.htm. [Accessed 2 April 2015].
Melzer D, Rice N, Depledge MH, Henley WE, Galloway TS. Association between serum perfluorooctanoic acid (PFOA) and thyroid disease in the U.S. National health and nutrition examination survey. Environ Health Perspect. 2010;118:686–92.
Hallgren S, Sinjari T, Hakansson H, Darnerud PO. Effects of polybrominated diphenyl ethers (PBDEs) and polychlorinated biphenyls (PCBs) on thyroid hormone and vitamin a levels in rats and mice. Arch Toxicol. 2001;75:200–8.
Hallgren S, Darnerud PO. Polybrominated diphenyl ethers (pbdes), polychlorinated biphenyls (PCBs) and chlorinated paraffins (CPs) in rats - testing interactions and mechanisms for thyroid hormone effects. Toxicol. 2002;177:227–43.
Lema SC, Dickey JT, Schultz IR, Swanson P. Dietary exposure to 2,2',4,4'-tetrabromodiphenyl ether (PBDE-47) alters thyroid status and thyroid hormone-regulated gene transcription in the pituitary and brain. Environ Health Perspect. 2008;116:1694–9.
Szabo DT, Richardson VM, Ross DG, Diliberto JJ, Kodavanti PR, Birnbaum LS. Effects of perinatal PBDE exposure on hepatic phase i, phase ii, phase iii, and deiodinase 1 gene expression involved in thyroid hormone metabolism in male rat pups. Toxicol Sci. 2009;107:27–39.
Tseng LH, Li MH, Tsai SS, Lee CW, Pan MH, Yao WJ, et al. Developmental exposure to decabromodiphenyl ether (pbde 209): Effects on thyroid hormone and hepatic enzyme activity in male mouse offspring. Chemosphere. 2008;70:640–7.
Butt CM, Stapleton HM. Inhibition of thyroid hormone sulfotransferase activity by brominated flame retardants and halogenated phenolics. Chem Res Toxicol. 2013;26:1692–702.
Cao J, Lin Y, Guo LH, Zhang AQ, Wei Y, Yang Y. Structure-based investigation on the binding interaction of hydroxylated polybrominated diphenyl ethers with thyroxine transport proteins. Toxicol. 2010;277:20–8.
Feo ML, Gross MS, McGarrigle BP, Eljarrat E, Barcelo D, Aga DS, et al. Biotransformation of BDE-47 to potentially toxic metabolites is predominantly mediated by human cyp2b6. Environ Health Perspect. 2013;121:440–6.
Richardson VM, Staskal DF, Ross DG, Diliberto JJ, DeVito MJ, Birnbaum LS. Possible mechanisms of thyroid hormone disruption in mice by bde 47, a major polybrominated diphenyl ether congener. Toxicol Appl Pharmacol. 2008;226:244–50.
Noyes PD, Hinton DE, Stapleton HM. Accumulation and debromination of decabromodiphenyl ether (bde-209) in juvenile fathead minnows (pimephales promelas) induces thyroid disruption and liver alterations. Toxicol Sci. 2011;122:265–74.
Verreault J, Bech C, Letcher RJ, Ropstad E, Dahl E, Gabrielsen GW. Organohalogen contamination in breeding glaucous gulls from the norwegian arctic: Associations with basal metabolism and circulating thyroid hormones. Environ Pol. 2007;145:138–45.
Villanger GD, Jenssen BM, Fjeldberg RR, Letcher RJ, Muir DC, Kirkegaard M, et al. Exposure to mixtures of organohalogen contaminants and associative interactions with thyroid hormones in east greenland polar bears (ursus maritimus). Environ Int. 2011;37:694–708.
Bloom M, Spliethoff H, Vena J, Shaver S, Addink R, Eadon G. Environmental exposure to PBDEs and thyroid function among new york anglers. Environ Toxicol Pharmacol. 2008;25:386–92.
Dallaire R, Dewailly E, Pereg D, Dery S, Ayotte P. Thyroid function and plasma concentrations of polyhalogenated compounds in inuit adults. Environ Health Perspect. 2009;117:1380–6.
Hagmar L, Bjork J, Sjodin A, Bergman A, Erfurth EM. Plasma levels of persistent organohalogens and hormone levels in adult male humans. Arch Environ Health. 2001;56:138–43.
Turyk ME, Persky VW, Imm P, Knobeloch L, Chatterton R, Anderson HA. Hormone disruption by PBDEs in adult male sport fish consumers. Environ Health Perspect. 2008;116:1635–41.
Lans MC, Klassonwehler E, Willemsen M, Meussen E, Safe S, Brouwer A. Structure-dependent, competitive interaction of hydroxy-polychlorobiphenyls, hydroxy-dibenzo-p-dioxins and hydroxy-dibenzofurans with human transthyretin. Chem Biol Interact. 1993;88:7–21.
Hamers T, Kamstra JH, Sonneveld E, Murk AJ, Visser TJ, Van Velzen MJM, et al. Biotransformation of brominated flame retardants into potentially endocrine-disrupting metabolites, with special attention to 2,2',4,4'-tetrabromodiphenyl ether (BDE-47). Mol Nutr Food Res. 2008;52:284–98.
Vandenberg LN, Colborn T, Hayes TB, Heindel JJ, Jacobs Jr DR, Lee DH, et al. Hormones and endocrine-disrupting chemicals: Low-dose effects and nonmonotonic dose responses. Endocr Rev. 2012;33:378–455.
Birnbaum LS. Environmental chemicals: Evaluating low-dose effects. Environ Health Perspect. 2012;120:A143–144.
Pucci E, Chiovato L, Pinchera A. Thyroid and lipid metabolism. International journal of obesity and related metabolic disorders. J Int Assoc Study of Obesity. 2000;24 Suppl 2:S109–112.
Acknowledgements
This research was supported in part by NIH/NIEHS P30ES000002 and supported in part by the intramural research project of the National Cancer Institute/NIH (Birnbaum). This paper does not reflect NIH policy.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
All authors contributed to the conceptualization of the research, interpretation of the results and preparation of the manuscript. JA conceived the study, performed the initial statistical modeling, and drafted the manuscript; SG performed the final statistical modeling; TZ, LB and JS provided support on the analysis and interpretation of the results and on manuscript preparation; EM contributed to the study design and drafting of the manuscript. All authors read and approved the final manuscript.
Additional file
Additional file 1: Table S1.
Description of Data: Fully-adjusted, survey-weighted associations between serum PBDE concentrations (wet weight) and having a current thyroid problem. (PDF 669 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Allen, J.G., Gale, S., Zoeller, R.T. et al. PBDE flame retardants, thyroid disease, and menopausal status in U.S. women. Environ Health 15, 60 (2016). https://doi.org/10.1186/s12940-016-0141-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12940-016-0141-0