Abstract
Extraintestinal Pathogenic Escherichia coli (ExPEC) pose a significant threat to human and animal health. However, the diversity and antibiotic resistance of animal ExPEC, and their connection to human infections, remain largely unexplored. The study performs large-scale genome sequencing and antibiotic resistance testing of 499 swine-derived ExPEC isolates from China. Results show swine ExPEC are phylogenetically diverse, with over 80% belonging to phylogroups B1 and A. Importantly, 15 swine ExPEC isolates exhibit genetic relatedness to human-origin E. coli strains. Additionally, 49 strains harbor toxins typical of enteric E. coli pathotypes, implying hybrid pathotypes. Notably, 97% of the total strains are multidrug resistant, including resistance to critical human drugs like third- and fourth-generation cephalosporins. Correspondingly, genomic analysis unveils prevalent antibiotic resistance genes (ARGs), often associated with co-transfer mechanisms. Furthermore, analysis of 20 complete genomes illuminates the transmission pathways of ARGs within swine ExPEC and to human pathogens. For example, the transmission of plasmids co-harboring fosA3, blaCTX-M-14, and mcr-1 genes between swine ExPEC and human-origin Salmonella enterica is observed. These findings underscore the importance of monitoring and controlling ExPEC infections in animals, as they can serve as a reservoir of ARGs with the potential to affect human health or even be the origin of pathogens infecting humans.
Similar content being viewed by others
Introduction
Extraintestinal Pathogenic Escherichia coli (ExPEC) cause infections outside the gastrointestinal systems of humans and animals1. In humans, ExPEC are notorious for their contribution to urinary tract infection (UTI), bloodstream infection, neonatal meningitis, intra-abdominal infection, and soft-tissue infection2. About 30% of bacteremia with high mortality are caused by ExPEC3. They can also cause above 50% of the community-acquired UTIs among people with compromised immune systems, leading to substantial morbidity, mortality, and health care costs3. ExPEC strains colonize the intestinal tract but do not cause enteric disease, and differ from intestinal pathogenic E. coli which usually causes gastroenteritis or colitis in the host intestine4. ExPEC strains contain different virulence factors (VFs) from enteric pathogenic E. coli; however, these VFs are widely distributed beyond ExPEC and may contribute to host adaptation of commensal E. coli rather than toxicity of ExPEC5,6.
To explore the diversity and transmission of ExPEC, traditional typing methods and large-scale genomic analysis were conducted. These provided evidence that more than half of the ExPEC strains from humans belonged to the phylogroup B2, which also included intestinal commensal E. coli1,7,8,9. The control of infections by ExPEC has been complicated by the emergence of ARGs, especially extended spectrum beta-lactamases (ESBLs) which can confer resistance to most beta-lactam antibiotics including three-/fourth-generation cephalosporins10. Genomic analysis has shown that most of the widespread ExPEC contained genes that determine resistance to multiple antibiotics7,8. Comparative genomics provided evidence of the crucial contribution of ARGs, especially the ESBLs, to the most wide-distributed ExPEC of ST13111,12.
Animals, including chicken, duck, cattle, cow, swine and some domestic companion animals, are not exempt from the threat posed by ExPEC. For instance, avian pathogenic E. coli (APEC) is known to trigger colibacillosis in poultry, resulting in huge losses in poultry production13,14,15. The purpose of the One Health approach is to balance and optimize the health of people, animals, and ecosystems16,17. The research focused on ExPEC from animals mainly for three important reasons. One is to decipher the diversity and dynamics of ExPEC in animals to reducing the economic loss caused by these organisms18,19. The second is to reveal the relationship between ExPEC from animals and humans to provide more information about the dynamics of ExPEC to control these in humans20,21. Many studies have found that E. coli from animal reservoirs may be a potential source for human ExPEC, especially those from poultry20,21,22,23. Moreover, evidence of the pathogenicity of poultry-derived E. coli strains in causing extraintestinal infections in humans has been demonstrated through in vivo and in vitro experiments24,25. Notably, foodborne E. coli can also cause extraintestinal infections in humans, involving high-risk clones such as ST69, ST95, ST117, ST131, and ST64826,27. The third objective is to unravel the potential transmissions of ARGs from animal microbes to human pathogens, particularly those that can render commonly used and even so-called “last-resort” drugs ineffective28,29. Several plasmids and integrons are crucial in these transmission events28,29,30,31. Moreover, deciphering the transfer of ARGs between bacteria originating from both human and animal hosts is one of the primary missions of the One Health approach, which could provide important information for designing efficient strategies to mitigate resistance32. However, a comprehensive understanding of the contributions of animal ExPEC to human pathogens and their antibiotic resistances is lacking.
Previously, we and other groups found that ExPEC can lead to significant losses in the swine industry18,19,33. Swine ExPEC strains are recognized as significant disease agents, causing conditions such as UTI, meningitis, pneumonia, arthritis, and septicemia34,35. The population structure of swine ExPEC varied slightly across different datasets, primarily comprising the phylogroups A, B1, and D18,33,36. Additionally, uropathogenic E. coli (UPEC) from sows predominantly belonged to phylogroups B1, D, and E35. Furthermore, one study linked the density of industrial hog production to increased UTI rates in nearby human populations, suggesting that intense hog production may elevate UTI incidence in surrounding communities37. This observation was particularly concerning in light of the extensive use of antibiotics in the poultry and livestock industries, as antibiotic resistance has been found to be widespread in strains of E. coli from animal sources38,39. Despite these insights, a comprehensive understanding of the diversity and resistance determinants of swine ExPEC, as well as their relationships and potential spread to human pathogens, remains poorly documented.
In this work, we conduct large-scale genome sequencing and antibiotic resistance tests on 499 ExPEC isolated from disease samples of swine between the years 2011 and 2017 in several provinces of China. We explore the population structure of ExPEC, the relationship between drug resistance phenotype and genotype, and the putative contribution of these ExPEC to human infections.
Results
Swine ExPEC from China exhibit a highly diverse population structure
The ExPEC were isolated from diseased tissues of pigs from different piggeries in China, most of which were located in Central China. To ensure that each strain originated from distinct pigs, we exclusively isolated and preserved one representative ExPEC strain from each pig farm at a given time. In this study, we randomly selected 50-90 isolates for each year from 2011 to 2017 (Supplementary Fig. 1a), resulting in a total collection of 499 E. coli strains from 23 Chinese provinces, mainly from Hubei, Henan and Hunan provinces (Supplementary Data 1). These isolates were obtained from various organs of pigs, with 79.4% originating from the lung (Supplementary Fig. 1b). Each genome of the studied isolates was sequenced, producing approximately 1 Gbp of reads, which were subsequently assembled into contigs for further analysis.
We first performed comparative genomic analysis to gain insight into the diversity and population structure of ExPEC from swine in China. Phylogenetic analysis revealed that over 50% of the isolates belonged to group B1 (54%), with 30% originating from group A, 6.2% from group F, and 5.6% from the recently defined group G (Fig. 1 and Supplementary Data 1). Very few E. coli isolates studied here resided in phylogroups B2, D and E, with proportion for each less than 3%. Based on in silico multilocus sequence typing (MLST), 490 of 499 E. coli could be assigned to 75 sequence types (STs), with 9 strains representing novel STs. The top 5 STs with the most isolates (>5%) including ST410 (14.8%), ST88 (9.2%), ST101 (8.2%), ST117 (5.6%) and ST156 (5.2%), accounting for above 40% of the entire collection (Supplementary Fig. 2a). Among these STs, ST410, ST88, ST101, and ST156 belonged to phylogroup B1, while ST117 was categorized in phylogroup G. The remaining E. coli exhibited a high degree of diversity, with 60 STs, each comprising fewer than 10 members. We also inspected the isolated organs and times of all the E. coli on the basis of phylogenetic analysis. Our findings revealed that strains from a special organ or time point were distributed throughout the whole phylogenetic tree, suggesting an absence of association between the source or time of isolation and the phylogroup or ST. We further assessed the diversity of this E. coli collection by serotype prediction. The high level of diversity was confirmed by the results about H- and O- serotype combinations. Two hundred serotypes were found (Supplementary Data 1 and Supplementary Fig. 2b). The most common serotype was O89:H9, which contained 31 strains accounting for 6.21% of the total collection. The remaining serotypes included less than 20 isolates, and 177 serotypes included less than 5 isolates.
Additionally, to understand the epidemiology of these swine ExPEC strains, we compared them with all E. coli strains present in the EnteroBase database using core genome multi-locus sequence typing (cgMLST). As a result, we identified 39 cases of genetic relatedness between swine ExPEC and isolates collected from different sources, with a maximum separation of 10 alleles (Supplementary Data 2). Among these occurrences, 21 instances involved E. coli strains from the Enterobase database, with explicitly defined host types, including human, swine, and bovine. Human-host instances were the most frequently observed, with a total of 15 swine ExPEC isolates showing genetic relatedness to E. coli from various human body sites, such as blood and rectum. Among these, two strains belonging to ST648 (A71 and A91) and one human blood infection strain (EnteroBase ID, ESC_LA6470AA) differed by only 2 alleles, indicating very closely related genomes. Moreover, swine-derived ExPEC belonging to ST410, ST101, ST131, ST167, or ST744 were also observed to share a common clonal origin with human-derived E. coli. This result underscores evidence of the zoonotic potential of ExPEC strains originating from swine.
Genes encoding virulence factors associated with extraintestinal infections are prevalent in swine ExPEC
Virulence factors (VF) play crucial roles in the interaction between E. coli and their vertebrate hosts. They have been used to define the pathogenicity features of E. coli, including those of different pathovars of intestinal pathogenic E. coli (IPEC) and ExPEC40. To infer the relationship between swine ExPEC and enteric E. coli, the characteristic toxins of enteric E. coli pathotypes were predicted. We found that toxin genes determining enteric diseases were rarely present in these ExPEC strains (Supplementary Fig. 3). Specifically, 49 strains harbored one or more of the following: the Shiga-toxin (STX), heat-labile (LT) enterotoxin, heat-stable (ST) enterotoxin, intimin, and fimbrial adhesins (F4, F5, F18, and F41). These strains mainly belonged to phylogroups F, A, and B1. It is noteworthy that these strains may represent hybrid pathotypes. Therefore, based on these virulence factors, we classified these 49 strains as four hybrid pathotypes, including ExPEC/ETEC, ExPEC/EPEC, ExPEC/EHEC, and ExPEC/EHEC/ETEC (Supplementary Data 3). The most prevalent hybrid pathotype is ExPEC/ETEC, comprising 39 strains in total. Roughly 70% of these strains contain the F5 fimbriae, all of which belonged to ST354/ST457.
We subsequently surveyed the five categories of VFs commonly found in human ExPEC41 within the studied E. coli genome sequences. Regarding adhesins, genes associated with type 1 fimbriae (fim) and curli fibers (csg) were present in approximately 90% of the strains (Supplementary Data 3 and Supplementary Fig. 3). P fimbriae (papC) and antigen 43 (agn43) were identified in 10% and 18% of the strains, respectively, while other genes afa and foc were found in less than 5% of the strains. When considering iron uptake, the iron transport gene (sitA), aerobactin siderophore gene (iutA), and salmochelin siderophore gene (iroN) and were present in 69%, 66%, and 51% of the strains, respectively. While genes involved in yersiniabactin biosynthetic (irp2), heme uptake (chuA), and iron regulation (ireA) were detected in 36%, 16%, and 10% of the strains, respectively. When it comes to serum resistance, genes involved in protecting bacteria from complement-mediated lysis (traT), increased serum survival (iss) and colicin V synthesis (cvaC) were identified in 74%, 69%, and 32% of the genomes, respectively. Additionally, other genes within this category, namely ompA and kpsM, were detected in 11% of the strains. As for the invasins, gene ibeA was found in only 4% of the strains. In terms of toxin genes, those associated with vacuolating autotransporter toxin (vat) and serine protease (pic) were present in 7% and 6% of the genomes, respectively. Other toxin genes such as hly (alpha-hemolysin), cdt (cytolethal distending toxin), and cnf1 (cytotoxic necrotizing factor 1) were detected in less than 3% of the genomes.
About 97% of swine ExPEC are classified as multidrug-resistant (MDR)
In the past decades, antibiotics were heavily used in poultry and livestock industries in China42. It has been reported that E. coli from food animals developed extreme resistance to frequently used antibiotics29,43,44. To assess the antibiotic resistance profiles of this E. coli collection, we conducted susceptibility test of these isolates to 20 antibiotics from 7 different classes, and found that all the isolates showed resistance to at least one of the used antibiotics (Supplementary Data 4). Among the 485 isolates with dependable antibiotic susceptibility outcomes (each test was validated using control strains, and only those passing quality control were considered reliable), MDR (multidrug-resistant, resistance to antibiotics from at least three classes45) strains accounted for up to 97% of the isolates (Fig. 2a). In addition, 239 of the 485 (49.3%) MDR strains were resistant to agents spanning all 7 classes, with strains A376 and A430 exhibiting resistance to 18 antibiotics tested. Notably, among these MDR strains, 46 were hybrid pathotypes, of which 54.3% displayed resistance to agents across all 7 classes (Supplementary Data 4).
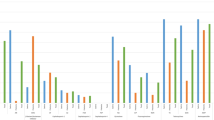
a UpSet plot illustrating the diversity of antibiotic resistance profiles for ExPEC isolates. In the combination matrix at the base of the main bar chart, each column represents a distinct phenotypic profile. A colored dot within a column signifies resistance to at least one antimicrobial within a drug class, with the color corresponding to the respective drug class. The vertical bar chart displays the total number of isolates with specific phenotypic profiles, while the horizontal bar chart depicts the number of isolates resistant to each drug class. Sulfamethoxazole trimethoprim is a combination antibiotic, classified here as encompassing both sulfonamide and trimethoprim. b Histogram illustrating the prevalence of resistance to each test antimicrobial grouped by drug class in ExPEC strains. c The prevalence of antimicrobial resistance in four common STs of ExPEC. Source data are provided as a Source Data file.
When the resistance to each antibiotic was analyzed, we found that most isolates were resistant to tetracycline (95.5%), ampicillin (95.5%), piperacillin (90.1%), sulfamethoxazole trimethoprim (89.9%) and chloramphenicol (85.2%) but only 0.8% of isolates were resistant to meropenem, imipenem, and tazobactam piperacillin (Fig. 2b). For aminoglycosides, about 70% of isolates were resistant to gentamicin and about 15.5% of isolates were resistant to amikacin. More than 65% E. coli showed resistance to each of the three fluoroquinolones, levofloxacin, moxifloxacin and ciprofloxacin. Additionally, resistance was observed in 10% to 60% of isolates for each of the other seven antibiotics within the beta-lactam class. Specifically, 51.8%, 13.4%, and 44.7% exhibited resistance to cefotaxime, ceftazidime, and cefepime, respectively, representing the third and fourth generation cephalosporins.
To assess the commonalities and specificities of antibiotic resistance among strains from different lineages, we analyzed the resistance profiles of strains belonging to the four most prevalent STs (Fig. 2c). We observed similar patterns in the prevalence of resistance to various drugs within each ST. Nonetheless, notable differences were observed, particularly in the prevalence of resistance to three fluoroquinolones and cefepime, which were significantly higher in ST410 compared to other STs. Furthermore, among the four top prevalent STs, only strains belonging to ST410 exhibited resistance to three antibiotics, including tazobactam piperacillin, meropenem, and imipenem.
Swine ExPEC genomes harbor diverse and abundant antibiotic resistance genes
To understand the genetic determinants of antibiotic resistance, we searched all the sequenced genomes for genes and point mutations contributing to antibiotic resistance. We predicted a total of 96 ARGs and point mutations of 3 chromosomal genes (gyrA, parC and parE), which could contribute to resistance to antibiotics belonging to 12 classes (Fig. 3a and Supplementary Data 5). We found that all genomes harbored at least one of these ARGs. Each of the 13 ARGs that determines the resistance to aminoglycosides was contained by more than 5% isolates, among which strA and strB were present in 68% strains. The most frequently occurring sulfonamide resistance gene was sul2, encoded by 85% isolates, which is the highest prevalence among ARGs. Among the 4 phenicol genes, floR had a prevalence of 73%, with others less than 35%. One of the three types of tetracycline resistance protein genes, tet(A), was present in more than 70% of the strains, while both tet(B) and tet(M) were found in less than 35% of the isolates. When genetic determinants contributing to the resistance against fluoroquinolones were considered, we observed that, in addition to the high prevalence of the chromosomal gene mutations, three ARGs were identified, with oqxA and oqxB as the most prevalent one (approximately 45%). Besides, we also found the genes conferring resistance to colistin (mcr-1) and fosfomycin (fosA3) in 23% and 17%, respectively, of the tested isolates. Among the genes encoding β-lactamase, the most prevalent one was blaTEM-1B which was contained by more than 67% isolates. Other beta-lactamase encoding genes had prevalence above 5% include blaCTX-M-14, blaCTX-M-55, blaOXA-1, blaCMY-2, blaCTX-M-65, blaTEM-1A, and blaTEM-141 most of which belong to extended-spectrum β-lactamase (ESBL) genes leading to the resistance to the three-/fourth-generation cephalosporins. When examining all ESBL genes present in our dataset, we found that as many as 262 strains harbored at least one ESBL gene. Moreover, among these, 25 strains were identified as hybrid pathotypes, specifically ExPEC/ETEC and ExPEC/EPEC (Supplementary Data 6). Additionally, 13 out of 15 strains with zoonotic potential also contained ESBL genes (Supplementary Data 2).
a Bar plot showing the percentage of genomes detecting each ARG or point mutation. Genes that contain point mutations leading to antibiotic resistance are marked with an asterisk. The color represents the class of antimicrobials to which genetic determinants confer resistance. The image displays only representative high-prevalence ARGs; you can find all the information in Supplementary Data 5. b Co-occurrence network of ARGs among ExPEC strains. The network was constructed based on the co-occurrence frequency of two-by-two ARGs in 499 genomes. The thickness and color depth of each link (edge) between ARGs (nodes) correspond to how frequently the two genes appeared together within the same genome. The image only visualizes genes that co-occurred together in at least 50 genomes. All connection information is available in Supplementary Data 8. Source data are provided as a Source Data file.
We conducted an additional analysis comparing the prevalence of ARGs of isolates from different STs (Supplementary Fig. 4). We found that the most prevalent ARGs within each class were similar, which is consistent with those for all the isolates. However, there were some over-presented ARGs in each of the four top prevalent STs. In ST410, we detected higher prevalence of ARGs including aph(3’)-Ia, aac(6’)-Ib-cr, rmtB, blaCTX-M-55, blaOXA-1, blaTEM-141, catA1, catB3, oqxA, oqxB, qepA1, and tet(B). In ST88, the prevalence of resistance genes such as aac(3)-IIa, ant(3”)-Ia, blaCTX-M-65, qnsS1, and dfrA1 was higher compared to other STs. Additionally, mcr-1 and dfrA14 were more prevalent in ST101, and blaCTX-M-15 and sul2 were more common in ST117. Here, we further combined the comparative results of antibiotic resistance phenotypes among the four prevalent STs, especially noting that strains belonging to ST410 exhibited the highest resistance to three fluoroquinolones compared to the other STs. Therefore, we analyzed the distribution of genetic determinants responsible for fluoroquinolone resistance, including ARGs and chromosomal point mutations, within the ExPEC population (Supplementary Fig. 5). We observed mutations in three chromosomal genes (gyrA, parC, and parE) present in all ST410 strains, and the prevalence of fluoroquinolone resistance genes in ST410 was higher compared to the other prevalent STs. This could be one of the important genetic factors contributing to the prevalence of ST410. It’s worth noting that all ST410 strains were identified as MDR. Furthermore, a similar pattern was observed in ST354, which presented the hybrid pathotype ExPEC/ETEC, with most strains belonging to this ST type containing ESBL genes.
Highly diverse antibiotic resistance gene co-occurrences contribute to the high prevalence of multidrug-resistant (MDR) ExPEC
To investigate the genetic determinants behind the MDR and XDR (extensively drug-resistant, nonsusceptibility to at least one agent in all but two or fewer antimicrobial categories) E. coli, we examined the compositional profiles of ARGs in each genome. Among the 492 genomes containing at least 2 ARGs, we identified 406 combinations of distinct ARGs (Supplementary Data 7). More than 96% of the combinations were contained by only one or two genomes, with 340 genomes each harboring a unique set of ARGs. Each combination contained an average of 13 ARGs, with the largest one containing up to 28. More than two-thirds of the 406 combinations presented by more than 70% of genomes have over 10 ARGs, including 31 combinations found in 36 genomes containing more than 20 different genes. When drug classes targeted by these ARGs were predicted, we found that the putative MDR isolates accounted for up to 98% of the total, which is consistent with the test results described above. Our findings unveiled a striking diversity in the combinations of ARGs within the majority of the swine ExPEC genomes.
To investigate the simultaneous transfer of multiple ARGs, we conducted co-occurrence network analysis on the entire set of ARGs (Supplementary Data 8). The most prevalent sub-network consisted of sul2, floR, strA, and strB, forming the central core of the entire network, with most of the other ARGs having connections to this sub-network (Fig. 3b). This sub-network was identified in more than 200 of the 499 genomes and had the potential to give rise to MDR E. coli strains resistant to antibiotics from aminoglycoside, chloramphenicol and sulfonamide drug classes. The other highly clustered ARGs included tet(A), blaTEM-1B, oqxA, and oqxB, conferring resistance to tetracyclines, beta-lactams, and fluoroquinolones, respectively. It is crucial to underscore the concurrent existence of ARGs targeting human drugs, such as blaCTX-M-55, blaCTX-M-14, fosA3, and mcr-1, in conjunction with ARGs targeting veterinary drugs. This issue carries notable significance, as the potential dispersal of veterinary drug-related ARGs, stemming from their misuse, indirectly amplifies the proliferation of co-existing ARGs against human drugs. Additionally, we observed that despite mcr-3 being detected in only five genomes (mcr-3.1 in four genomes and mcr-3.5 in one genome), it is noteworthy that two of these genomes concurrently carry both mcr-1 and mcr-3 (Supplementary Data 8).
Both chromosomes and plasmids are vectors of antibiotic resistance genes
To decipher the vectors of ARGs, we chose 20 isolates from all the defined phylogenetic groups to obtain closed genomes. We obtained 62 closed replicons, 20 chromosomes and 42 plasmids, along with one incomplete plasmid sequence (Supplementary Data 9). The plasmids harbor one to four plasmid replicons, including IncFIB (n = 17), IncFIC (n = 14), IncI-gamma/K1 (n = 10), IncFIA (n = 8), and rep_cluster_2244 (n = 8). The average number of the ARGs contained by each chromosome was 2.5, adding up to 50 ARGs across all 20 chromosomes. The tetracycline-associated resistance gene tet(B) was exclusively identified in chromosomes, not in plasmids. Another ARG that exhibited over-representation on chromosomes is blaCMY-2 (Supplementary Data 10). Of the 43 plasmids, thirty-seven harbored at least one ARG, with an average count of 6.2 and the highest observed being 15. AGRs over-presented in plasmid genomes included aac(3)-IId, aadA2, mph(A), dfrA12, oqxA, oqxB, and aph(3’)-Ia. The top prevalent ARGs were all frequently found in both chromosome and plasmid genomes, such as sul1, sul2, floR, tet(A), blaTEM-1B, strA and strB, suggesting potential transfer between plasmids and chromosomes. In particular, we observed that certain ARGs have two copies located on distinct plasmids in the same isolate (Supplementary Data 9). For instance, in strain A430, each of the genes aac(3)-IId, aadA2, blaTEM-1B, dfrA12, and tet(A) was identified with two copies situated on separate plasmids. Additionally, we also identified integrons within the 20 complete genomes. A total of 16 integrons were detected, all of which were located within the plasmid genomes (Supplementary Data 11). Furthermore, we found that these integrons generally contain two ARG cassettes: aadA2/aadA5 and dfrA12/dfrA17. It is noteworthy that we observed these integrons closely associated with IS26 (Fig. 4a). This suggests that the accumulation and dissemination of specific ARGs in swine ExPEC were facilitated by the interplay between integrons and transposons.
a Gene arrow maps illustrating ARGs and their neighboring ISs. The direction of the arrows corresponds to the strand where the genes are situated. Right-pointing arrows represent genes on the forward strand, while left-pointing arrows indicate genes on the reverse strand. Different colors of the arrows signify distinct gene types. The start and end positions of the genes within their respective molecules are visually depicted along the x-axis, measured in kilobase pairs (kbp). Highlighted blue lines emphasize potential co-transfer units of specific significance, while green boxes represent predicted integrons. The labels on the left side denote the names of each vector, and information about the plasmid’s replicon types and mobility (separated by ‘~~~‘) is provided above the dashed box. Gene names and IS elements, which conventionally appear in italics, are displayed in regular font for clarity. A412_chr exhibits only a subset of ARGs and ISs. b The stacked histogram illustrating the distribution ExPEC isolates for various phylogroups harboring genomic islands. c The prevalence of the plasmids in 499 ExPEC genomes. The heatmap illustrates the Jaccard similarity coefficient among pairs of plasmids. The stacked histogram on the left displays the number of genomes for different phylogroups harboring each plasmid. For clusters of highly similar plasmids (such as A333_p0, A430_p0, and A468_p0), we employ the prevalence of the plasmid with the shortest sequence among them as a representative measure for that type of plasmid. Source data are provided as a Source Data file.
When the co-location of the ARGs were considered, we found that the five genes sul2, strA, strB, tet(A), and floR were clustered together on both chromosome and plasmid (Fig. 4a). The ARG cluster on the chromosome is delimited by IS3 and IS1H, forming Genomic Island 1 (GI1), while on the plasmid, it is framed by ISVsa3 and IS26, which are associated with IncI-gamma/K1 plasmid. Moreover, we observed that GI1 was detected in 30 isolates (Fig. 4b), while the Incl-gamma/K1 plasmid was present in 14 isolates (Fig. 4c). It’s worth noting that these isolates were distributed across phylogroups A, B1, D, F, and G. Another ARG cluster located on the chromosome, is consisting of sul2, strA, strB, and blaTME-1B, with IS5075 and IS26 serving as flanking elements, collectively forming Genomic Island 2 (GI2). It was identified in 30 isolates, primarily from phylogroup B1. Regarding plasmids, two similar gene clusters were observed, with both of these gene clusters being associated with IS26. One contains strA, strB, and blaTME-1B (A68_p1, A237_p0, A186_p1), while the other harbors strA, strB, and sul2 (A71_p0). These findings indicate that the transfer of this ARG cluster occurs in a diverse manner, facilitated by transposable elements (TEs) among chromosomes and also by conjugative mobilization through plasmids. Moreover, in addition to the ARG clusters, these conjugative plasmids carried an array of diverse ARGs, including aac(3)-IId, mph(A), cmlA1, sul3, and dfrA17, which confer resistance to antibiotics belonging to aminoglycosides, macrolides, phenicols, sulfonamides, and trimethoprim. These findings highlight the plasticity and heterogeneity of the gene clusters associated with strA and strB, enabling E. coli to combat a broad spectrum of antibiotic agents.
Plasmids carried by swine ExPEC have the potential to transfer ARGs against important antibiotics used in human treatment
We identified potential horizontal gene transfer facilitated by the plasmid by discerning similarities between the plasmids found in ExPEC carrying ARGs and those identified in bacteria from other hosts, especially human (Fig. 5). Among the 20 isolates selected for sequencing of closed genomes, A376 and A382 showed resistance to carbapenems. Two plasmids belonging to IncX3 (A382_p1) and IncFIA/FIC (A376_p2) harbored blaNDM-1 and blaNDM-5, respectively (Fig. 5a). Genomic analysis revealed a high similarity between plasmid A382_p1 and plasmid pNDM_MGR194 found in the human pathogenic bacterium Klebsiella pneumoniae46 (Fig. 5e). The main difference lies in the resistance gene carried by the pNDM_MGR194 and pNDM_MGR194-like plasmids, which is blaNDM-5. However, the insertion sequences on one side of these plasmids are the same. Three strains belonging to phylogroups A and B1 were found to possess plasmid A382_p1 in our swine ExPEC collection (Fig. 5e). Among these isolates, A386 and A499 were found to harbor the antibiotic resistance gene blaNDM-5, consistent with the observations made in pNDM_MGR194. For the blaNDM-5 gene, situated on plasmid A376_p2, it was found to be clustered with other ARGs conferring resistance to beta-lactams, aminoglycosides, sulfonamides, and trimethoprim. These ARGs on the plasmid are flanked by IS26, forming a potentially transposable unit. The plasmid A376_p2 exhibits significant similarity to the plasmid pLZ135-NDM in human E. coli, which contains two copies of this transposable unit. These indicate the potential transmission of blaNDM genes between swine E. coli and human pathogens through plasmids, highlighting the variability of the blaNDM gene on conjugative plasmids in the swine ExPEC.
Gene arrow maps illustrating the presence of ARGs: blaNDM (Panel a), mcr-1 (Panel b), co-existence of fosA3 and ESBLs (Panel c), and co-existence of mcr-1, fosA3, and ESBLs (Panel d). The meaning represented by the depicted elements is similar to that of the elements in Fig. 4a. Black labels for vector names denote plasmids from our study, while each red label corresponds to plasmids from public databases that are most similar to the respective black-labeled plasmid. Information regarding the replicon types, mobility, species name of the strain, and the host of the strain (separated by ‘~~~‘) for public plasmids is provided above the dashed box. A333_chr only shows a partial representation of ARGs and ISs. Panel e: The similarity between plasmids from ExPEC and those from bacteria originating from other hosts, as well as the prevalence of plasmids within the ExPEC context. The meaning represented by the depicted elements is similar to that of the elements in Fig. 4c. Due to partial similarities and some distinctions among plasmids A251_p0, A412_p0, and A329_p0, and in accordance with the principle of plasmid incompatibility, it is not possible for a bacterium to simultaneously possess two such plasmids. Consequently, if the sequencing data of a bacterium mapped to the genomes of these three plasmids, each exhibiting a coverage exceeding 90%, we chose the result with the highest coverage. Source data are provided as a Source Data file.
Seven copies of the colistin resistance gene mcr-1 were identified in the genomes of six isolates, with four copies located on four plasmids (A338_p0, A251_p0, A412_p0, A329_p0) and three copies found on two chromosomes (Fig. 5b and d). In all of these cases, the insertion sequence ISApl1 was found in close proximity to the mcr-1 gene, as reported previously47,48. Plasmid A338_p0 exhibits moderate genomic sequence similarity to plasmid pSCKLB684-mcr from K. pneumoniae. Plasmid A251_p0, A412_p0, and A329_p0 exhibit a high degree of similarity in terms of gene content; however, the latter two are capable of conjugative transfer, while the former is non-mobilizable. Plasmid A412_p0 and A329_p0 share a high level of genomic sequence identity with plasmids pSH15G1450 and pLS61394-MCR, both originating from Salmonella enterica isolated from children with intestinal infections in China49,50. And plasmid A251_p0 is homologous to plasmid pMCR-H8 from ESBL-producing E. coli H8, isolated from the mink farmer in Shandong Province of China51. Importantly, the A251 strain possesses zoonotic potential based on the cgMLST results (Supplementary Data 2). Besides mcr-1, these plasmids harbor a diverse array of additional ARGs conferring resistance to crucially important antibiotics for human treatment, including blaCTX-M-14 (cephalosporin), floR (florfenicol), fosA3 (fosfomycin), and oqxA and oqxB (quinolone). Analysis of plasmid prevalence showed that the conjugative plasmid A412_p0 and A329_p0 were present in 15 and 4 swine ExPEC strains, respectively, whereas the non-mobilizable plasmid A251_p0 could be found in 4 isolates (Fig. 5e).
In addition to the fosA3 genes that co-locate with the mcr-1 genes, we identified an additional four fosA3 genes on the 20 genomes analyzed. Among these, one gene was located on the chromosome, while the remaining three were found on three different plasmids belonging to two distinct families, namely IncFIA and IncI-gamma/K1 (Fig. 5c). Furthermore, we observed that on these plasmids, two ESBL genes (blaCTX-M-15 and blaCTX-M-65) were found in close proximity to fosA3. Additionally, all fosA3 genes and ESBL genes were associated with IS26. Notably, among the three plasmids coexisting with mcr-1, the gene blaCTX-M-14 and fosA constitute a potential co-transfer unit with two IS26 elements serving as flanking sequences (Fig. 5d). Comparative genomic analysis showed that plasmids A163_p1 was highly similar to plasmids pHNHNC02 from a chicken-derived E. coli isolate52 (Fig. 5e). Significantly, plasmids A237_p1 and A68_p0 have a greater diversity of ARGs compared to their closest counterpart, plasmid pHNAH4-1 from a ceftazidime-resistant E. coli strain isolated from chicken feces in China which had no fosfomycin resistance gene53. This finding suggests that these two plasmids represent a novel type carrying both fosA3 and ESBL genes. Taken together, we observed that plasmids carrying the fosA3 gene have a wide host range, being found in different Enterobacteriaceae members of swine, poultry, and human origin.
Discussion
Our large-scale population genomic analysis of 499 swine ExPEC isolates collected from China revealed that more than 80% belonged to phylogroups B1 and A. In pig farms worldwide, encompassing regions such as Australia and Poland, the population structure of E. coli isolated from the feces of healthy pigs was also predominantly characterized by phylogroups B1 and A54,55,56. Moreover, several prevalent STs identified in our dataset coincide with those observed in healthy pig intestinal E. coli57, such as ST10, ST58, ST88, ST101, ST117, and ST744. These findings further support the inference that ExPEC originate from fecal sources and exist asymptomatically within the intestinal tract10. Additionally, these two phylotypes have been reported to be associated with the majority of enterotoxigenic E. coli (ETEC), and many E. coli strains from animals, birds, and the environment have been found to belong to these two groups58,59,60. However, our survey of virulence factors enables us to distinguish these E. coli strains from ETEC, as they exhibit a very low frequency of ETEC toxin genes. Although only a small number of ExPEC strains contain toxins typical of enteric E. coli pathotypes, caution must be exercised regarding these potential hybrid pathotypic strains. For instance, ETEC strains, mainly including F4+ and F18+ E. coli, were often the cause of postweaning diarrhea (PWD), which incurs significant economic costs for the pig industry61. F4-positive ETEC isolates causing PWD commonly belonged to ST100, while F18-positive isolates were assigned to diverse STs, including ST23, ST10, and ST15562. In our study, all three F4-positive ExPEC/ETEC strains belonged to ST100, and one F18-positive ExPEC/ETEC strain belonged to ST155. This caution arises from the potential of hybrid pathotypic E. coli to cause more severe illnesses and exhibit higher levels of resistance compared to non-hybrid pathotypes63,64,65. Furthermore, our investigation illustrated that swine-derived hybrid pathotypic strains displayed heightened antibiotic resistance.
On the other hand, compared to human-derived ExPEC, swine-derived ExPEC displayed a distinct population structure, with human strains often belonging to phylogroups B2 and D7,8,66. The most prevalent STs of human ExPEC, such as ST131, ST69, ST95, ST648, ST73, ST393, and ST121,60, were not commonly found in our dataset. However, a small proportion of swine ExPEC belonged to these ST types, including ST131, ST69, ST95, and ST648. These strains carried ESBL genes, and the majority of them also harbored genetic determinants of fluoroquinolone resistance. A study has indicated that swine E. coli belonging to ST131 posed a potential zoonotic risk67. In our investigation, swine ExPEC belonging to ST131 and ST648 were also found to have zoonotic potential. Additionally, there were several prevalent STs shared by both human and swine ExPEC. The prevalent STs in our collection, including ST410, ST354, ST88, and ST23, were also reported to be among the top 20 human ExPEC STs1. ExPEC strains of ST410, which are resistant to third-generation cephalosporins and carbapenems, have raised significant concerns recently68,69. ST354 represented predominant ST of fluoroquinolone-resistant E. coli originating from canine fecal and extraintestinal infections, with certain strains within this ST type carrying ESBL genes70. In our study, swine ExPEC of ST354 also exhibited similar characteristics: the hybrid pathotype, resistance to fluoroquinolones, and the presence of ESBL genes. Swine ExPEC of the ST10 complex within phylogroup A exhibited a high degree of diversity, including ST774, ST167, ST617, ST10, and several other sequence types (STs) with fewer than 5 members. Among them, ST10, ST167, and ST617 have been reported as major STs associated with human ExPEC infections1. Similarly, our study’s cgMLST analysis revealed that some ExPEC strains in ST167, ST617, or ST744 were sourced from humans. Other STs were once reported to be associated with human ExPEC, including ST117 and ST58. ST117 from phylogroup G has been proposed as an emerging multidrug-resistant foodborne ExPEC71. These findings suggest that, despite differential transmission dynamics of ExPEC between swine and humans, the potential transmission of ExPEC between humans and swine may serve as a significant source of human ExPEC infections. This highlights the importance of understanding and monitoring the dynamics of ExPEC populations in both animal and human settings.
Antibiotic resistance has emerged as a pressing concern in bacteria from animals and their respective environments72,73,74. Our collection of E. coli strains exhibited extensive resistance to various classes of drugs, surpassing the severity of resistance levels reported previously43,44,74. Particularly noteworthy was the heightened prevalence of MDR within swine ExPEC. This phenomenon may be attributed to the enduring use of antibiotics in China’s livestock industry over the preceding decades42. The antibiotic resistance profiles suggested these ExPEC isolates not only have obtained strong resistant abilities to the frequently used veterinary antibiotics, but also have developed resistance to some important clinical antibiotics. Moreover, it is noteworthy that over 50% and 40% of the tested E. coli strains respectively exhibited resistance to third- and fourth-generation cephalosporins, which have been utilized in the treatment of a broad range of severe infectious diseases in humans75,76. In 2020, China implemented a ban on the use of antibiotics in feed additives77, and strict monitoring of the types and quantities of antibiotics used to treat animal diseases is now in place.
The prevalence of unique combinations and the co-transfer of multiple resistance determinants underscores the potential for the emergence and spread of MDR strains. The co-selection of multiple ARGs complicates the transmission and accumulation of these genes, as the presence of one antibiotic is sufficient to sustain (select for) all antibiotic resistance genetic determinants due to their co-location on the plasmid78,79. In our study, the co-occurrence network of ARGs and the genetic contexts of complete plasmids suggested the presence of diverse patterns in the coexistence of ARGs. This information is valuable for preventing the spread of additional ARGs that coexist with genes selected by widely used antibiotics in livestock. Furthermore, we successfully resolved the co-transfer of multiple ARGs with a high co-occurrence frequency and elucidated how these genes achieve widespread presence in this population through the utilization of insertion sequences and conjugative plasmids. Our findings shed light on the mechanisms driving the widespread presence of ARGs in this population, providing a basis for implementing targeted interventions and control measures to uphold antibiotic efficacy and safeguard livestock health.
E. coli has the ability to acquire resistance genes from other bacteria, while also being capable of transferring its own resistance genes to other bacterial strains80. The dynamic exchange of resistance genes underscores the potential for E. coli to play a pivotal role in the dissemination of antibiotic resistance among bacterial populations in both animal and human hosts. Plasmids have been identified as the most crucial vectors of ARGs for the dissemination events28,81,82. Our findings showed the effective transmission of the carbapenemase-encoding gene blaNDM between swine ExPEC, and human pathogens like K. pneumoniae and E. coli through specific plasmid types. Carbapenem-resistant Enterobacterales (CRE) infections have become a major concern in the global effort to combat infections83. In recent years, there has been an increasing global transmission of CRE, and this situation has been further influenced to some extent by the spread of COVID-1984. Our study provided valuable insights that could contribute significantly to CRE prevention and control efforts. Additionally, colistin resistance is a pressing issue globally, primarily because colistin is considered as a last-resort medication for tackling drug-resistant bacterial infections85. Multiple studies have provided compelling evidence of the extensive dissemination of the colistin resistance gene mcr-1 through conjugative plasmids in various settings, including the livestock farms, human populations and natural environment86,87,88. Our study unveiled the combined action of conjugative and non-mobile plasmids in perpetuating mcr-1 prevalence, highlighting the persistent challenge posed by colistin resistance despite regulatory interventions. Colistin resistance genes encompass various types, with mcr-1 and mcr-3 having been disseminated worldwide48,89. It is notable that strains simultaneously carrying both mcr-1 and mcr-3 have been isolated from various sample types, encompassing cattle in Spain and Italy90,91, as well as pigs, poultry, and clinical samples in China92,93,94. Our study describes two swine ExPEC strains concurrently harboring mcr-1 and mcr-3. While this occurrence is not prevalent, vigilance regarding the risk of its accumulation is warranted. The prevalence of extended-spectrum β-lactamases (ESBLs) poses a significant challenge to the utilization of β-lactam antibiotics in human medicine, with CTX-Ms being the predominant ESBL family worldwide95. The limited availability of new antibiotic agents has prompted a re-evaluation of previously used antibiotics, such as fosfomycin, as potential treatment options for multidrug-resistant bacteria, particularly those producing extended-spectrum β-lactamases (ESBLs) and carbapenemases within the Enterobacteriaceae family96. However, several studies have revealed a concerning trend of co-localization of ESBL genes and fosA genes on plasmids, presenting an additional challenge in the treatment of Enterobacteriaceae infections97,98,99. Our investigation revealed the co-localization of fosA3 with multiple ESBL genes on diverse plasmids, aiding in the tracing of the dissemination of these ARGs. In the context of One Health, these findings highlight the need for continued vigilance and comprehensive strategies to monitor and address the potential reservoirs and transmission routes of ARGs, ensuring effective measures are in place to mitigate the risk of their persistence and spread in both animal and human populations.
Methods
ExPEC isolates collection and DNA extraction
The ExPEC isolates were collected from diseased tissue samples of swines exhibiting various extraintestinal infection clinical symptoms by the Animal Disease Diagnostic Laboratory at Huazhong Agricultural University during 2011–2017. Initially, swines suspected of having extraintestinal infections were identified through clinical symptoms such as lying on the side, abdominal breathing, shaking, and lameness. These assessments were conducted by trained veterinarians and animal health professionals. Tissues showing pathological changes from swines that died with these symptoms were collected for further analysis, including lung, liver, brain, and heart. The tissue sampling was conducted using aseptic instruments, with operators wearing personal protective equipment. Samples were collected swiftly, sealed in sterile containers, and refrigerated to preserve their integrity. Detailed records of the diseased tissues, sample collection times, and the geographical locations of the pig farms were documented. The samples, along with the documented records, were transported to the Animal Disease Diagnostic Laboratory at Huazhong Agricultural University. The laboratory was notified in advance of the incoming samples, and a communication channel was established between the field veterinarians and the laboratory personnel to ensure seamless transfer and receipt of the samples. Upon receiving the samples, the laboratory conducted further diagnostic tests to confirm the presence of ExPEC. The results were then reported back to the originating veterinarians and farms for further action.
Given that our study involved isolating E. coli from the tissues of deceased animals, the experiment received ethical approval from the Animal Management and Ethics Committee of Huazhong Agricultural University (No. HZAUSW-2017-006). Moreover, in handling tissues from deceased animals, we strictly adhere to the “Technical Specification for the Harmless Treatment of Dead Animals” issued by the Ministry of Agriculture of the People’s Republic of China (https://www.gov.cn/gongbao/content/2013/content_2547154.htm).
These samples were obtained from pig farms in various regions of China, including the provinces of Hubei, Hunan, Henan, Jiangxi, Anhui, Zhejiang, Guangdong, and Jiangsu. The collected materials were inoculated onto MacConkey agar plates and incubated at 37 °C for 12 hours. Colonies with characteristics indicative of E. coli were selected and subcultured onto a general-purpose agar medium, followed by further incubation at 37 °C for 12 hours to achieve purification. Each E. coli isolate was confirmed using 16 S rRNA gene PCR. Further identification of ExPEC involved PCR utilizing specific oligonucleotide primers to amplify five virulence genes: papA and/or papC (P fimbriae), sfa or foc (S or F1C fimbriae), afa or dra (Dr-antigen-binding adhesins), iutA (aerobactin receptor), and kpsMT II (group 2 capsular polysaccharide units). ExPEC strains were characterized by the presence of at least two of the aforementioned five markers. The primer sequences are provided in Supplementary Data 12.
The ExPEC strains were isolated from diseased pigs sent to our laboratory from various regions across China, forming a comprehensive sample pool. This strain pool served as our sampling frame, which included all ExPEC isolates received from 2011 to 2017. Each year, we selected 50-90 strains for genome sequencing based on practical considerations, including the total number of isolates received annually and the costs associated with sequencing and analysis, resulting in a total collection of 499 strains. A random number generator was used to select isolates from the pool each year, ensuring that each isolate had an equal chance of being included in the study. The genomic DNA was extracted from all ExPEC isolates using a commercial DNA Kit (TIANGEN, Beijing, China). The quality and concentration of the bacterial genomic DNA were assessed through electrophoresis on a 1% agarose gel, and analysis was conducted using a NanoDrop2000 system (Thermo Scientific, Waltham, MA, USA) and a Qubit 4 Fluorometer (Thermo Scientific, Waltham, USA).
Antibiotic susceptibility testing
The MIC values of various antibiotics (Supplementary Data 13) were employed to evaluate the antibiotic susceptibility of ExPEC isolates, and its testing methods and breaking points followed the recommended microbroth dilution protocol (CLSI M100, 28th Edition) of the Clinical & Laboratory Standards Institute (CLSI, United States). The collection of MIC values mainly relied on the BD Phoenix™ 100 automatic microbial identification and susceptibility analysis system. A total of 20 tested antibiotics belonged to six broad categories, including aminoglycoside (amikacin and gentamicin), beta-lactam (penicillin: amoxicillin clavulanic acid, ampicillin, aztreonam, piperacillin, sulbactam ampicillin, and tazobactam piperacillin; first-generation cephalosporin: cefazolin; third- or fourth-generation cephalosporin: cefepime, cefotaxime, and ceftazidime; carbapenem: imipenem and meropenem), chloramphenicol (chloramphenicol), quinolone (ciprofloxacin, levofloxacin, and moxifloxacin), sulfonamide (sulfamethoxazole trimethoprim), tetracycline (tetracycline). Three replicates were set for each antibiotic test. E. coli ATCC 25922 and ATCC 35218 strains were used for quality control.
Short-read assembly and genome annotation
All genomes of the studied E. coli isolates were sequenced through the Illumina HiSeq 2500 platform. Genome assembly and annotation were performed using modules from the comparative genomic analysis platform (PGCGAP)100 developed by us previously. The raw short-reads generated by Illumina platform were initially evaluated using FastQC v0.11.9 (https://www.bioinformatics.babraham.ac.uk/projects/fastqc/) and then processed with Trimmomatic v0.38101 to remove adapters and low-quality reads. The resulting high-quality reads for each strain were assembled using SPAdes v3.14.1102 (parameters: -k 21,33,55,77 --careful). The draft genomes were annotated by Prokka v1.14.6103 with the following parameters: --genus Escherichia --species coli --gram neg --usegenus.
MLST analysis, serotype prediction, VFs and ARGs identification
We employed SRST2 v0.2.0104 to predict sequence type of each strain based on short-read sequences. ExPEC serotype prediction from assembled genome data was performed using ECTyper v1.0.0105. VFs and ARGs were identified based on genome sequences through ABRicate v1.0.1 (https://github.com/tseemann/abricate) using Ecoli_VF database (https://github.com/phac-nml/ecoli_vf) and ResFinder database106, respectively (minimum identity 90%, minimum coverage 80%). Chromosomal point mutations contributing to antibiotic resistance were detected using ResFinder v4.1.5107 with the “--point” parameter, based on the PointFinder database108.
Pangenome analysis and phylogenetic analysis
Pangenome analysis was conducted using Roary v3.13.0109 with the following parameters: -i 85 -e --mafft. This resulted in the creation of a multi-FASTA alignment of 2,241 core genes. Then we used SNP-sites v2.5.1110 to extract the single nucleotide polymorphisms (SNPs) from the core genome alignment, resulting in a total of 208,012 SNPs being identified. The Maximum Likelihood (ML) phylogenetic tree was constructed using RAxML v8.2.12111 with the GTR + GAMMA model and 1000 bootstrap replicates.
cgMLST analysis
We performed cgMLST analysis for each strain using cgMLSTFinder v.1.2.0 (https://bitbucket.org/genomicepidemiology/cgmlstfinder) with the Enterobase Escherichia/Shigella cgMLST v1 scheme. The results provided the closest cgST type along with the number of matching alleles for each strain. Based on this, we further filtered the results with a threshold of ≤10 allele differences compared to the closest cgST type. Consequently, in the filtered results, the ExPEC strains assigned with cgST types shared a common clonal origin with strains in the Enterobase database belonging to the same cgST types. Information regarding the source of public isolates (e.g., bovine, human) was extracted from the “Source Type” and “Source Details” columns in EnteroBase.
Long-read assembly
Twenty representative isolates from different phylogroups and STs were selected to obtain complete genomes. These genomes were sequenced through the Oxford Nanopore Technologies (ONT) MinION sequencer. Guppy v5.0.16 was employ for ONT basecalling, and only reads that passed Guppy’s quality filters were retained (mean_qscore_template ≥7). Subsequently, we utilized Filtlong v0.2.0 (https://github.com/rrwick/Filtlong) to remove the worst 5% of long-reads. Finally, summary statistics of filtered long-reads were evaluated using NanoPlot v1.29.1112. The results indicated that the mean read quality of these samples was around 9, and the mean read length was around 20 kbp (Supplementary Data 14). Additionally, the mean size of each sample yielding filtered data reached 1168 Mbp, with a minimum of 669 Mbp, reflecting a sequencing depth of at least 100x. De novo assembly of filtered long-reads was carried out using Flye v2.8.3-b1695113. The resulting genome sequences underwent two rounds of polishing with Pilon v1.23114, using Illumina reads.
Annotation of complete genomes and comparative analysis of plasmids
The replicon family and transferability of 43 plasmids were predicted using MOB-typer module in the MOB-suite v3.0.3115. Additionally, the ‘mash_nearest_neighbor’ entry in the tool’s results as the basis for the most similar matches to plasmids in public databases, except for plasmid A381_p1. In the case of A381_p1, its closest matches were determined from the literature46, considering gene content and replicons. The annotation of ARGs in the chromosome and plasmid genomes was carried out as previously described. Insertion sequences (ISs) were identified using ABRicate v1.0.1 (https://github.com/tseemann/abricate) with ISfinder database116 (minimum identity 90%, minimum coverage 80%). Integrons were detected using IntegronFinder v2.0.3117 with the following parameters: --local-max --func-annot. The sourmash v3.3.0 program118 was employed, utilizing a k-mer size of 31, to calculate Jaccard indices between pairs of plasmids.
Detection of Genomic Islands on the chromosomes
Detecting complete genomic islands in genomes assembled from short-read data is challenging, as draft genomes exhibit significant fragmentation. Hence, we applied the following criteria to ascertain the existence of a genomic island in a draft genome. First, the presence of all ARGs associated with that genomic island must be confirmed in the genome. Second, for the identification of a partial genomic island—such as for the detection of Genomic Island 1—strB, strA, sul2, IS1H in the draft genome should be located on the same contig. Similarly, for the detection of Genomic Island 2—strB, strA, sul2, IS5075 in the draft genome must be present on the same contig. The above-mentioned process was accomplished using a custom Python script (available at https://github.com/xdli009/Swine_ExPEC_genomes_analysis/tree/main/Detection_Genomic_Islands).
Mapping short reads to plasmid sequences
Mapping short sequence reads from strains that were not subjected to long-read sequencing to complete plasmid sequences was employed to determine the distribution of these plasmids across all ExPECs. We utilized BWA v0.7.17-r1188119 to align short reads from each strain to the plasmid genomes (minimum mapping quality 30) and computed coverage for sequence alignments across each plasmid using bedtools v2.30.0120. To confirm the presence of a specific plasmid within an ExPEC strain, two criteria must be met: firstly, the alignment coverage should be at least 90%, and secondly, the assembled genome’s predicted ARGs must encompass a minimum of 80% of the ARGs present in that plasmid.
Visualization
We employed ggplot2 v3.3.6 (https://ggplot2.tidyverse.org.) and UpSetR v1.4.0121 packages in R (available at https://github.com/xdli009/Swine_ExPEC_genomes_analysis/tree/main/Visualization) to visualize phenotype and genotype data. Phylogenetic trees were visualized by iTOL v5122. The co-occurrence network of ARGs was generated using Cytoscape v3.8.0123. The ARGs and ISs arrow maps for the complete genomes were created using gggenes v0.4.1 (https://github.com/wilkox/gggenes). Heatmaps to visualize Jaccard similarity matrix of plasmid genomes were generated using pheatmap v1.0.12 (https://CRAN.R-project.org/package=pheatmap). We used Adobe Illustrator (http://www.adobe.com/au/products/illustrator.html) for figures retouching.
Statistics & reproducibility
In this study, no statistical analyzes were conducted. Our approach was based on direct observation, descriptive analysis, or other non-statistical methods suitable for the objectives of our research. Biological samples were collected randomly without any prior information about their antibiotic resistance phenotypes. To ensure the reproducibility, each antibiotic susceptibility test was performed in triplicate. Only results that were consistent across all three replicates were considered valid and included in our analysis.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
All clean short-read and long-read sequence data, draft genomes, and complete genomes generated in this study have been deposited in the NCBI under BioProject ID PRJNA1044843. BioSample accession number for each strain are provided in Supplementary Data 1. Source data are provided with this paper.
Code availability
All custom Python and R codes have been uploaded to GitHub: https://github.com/xdli009/Swine_ExPEC_genomes_analysis.git.
References
Manges, A. R. et al. Global extraintestinal pathogenic Escherichia coli (ExPEC) lineages. Clin. Microbiol. Rev. 32, 00135–18 (2019).
Johnson, J. R. & Russo, T. A. Extraintestinal pathogenic Escherichia coli:“the other bad E coli”. J. Lab. Clin. Med. 139, 155–162 (2002).
Martin, G. S., Mannino, D. M., Eaton, S. & Moss, M. The epidemiology of sepsis in the United States from 1979 through 2000. N. Engl. J. Med. 348, 1546–1554 (2003).
Alteri, C. J. & Mobley, H. L. Escherichia coli physiology and metabolism dictates adaptation to diverse host microenvironments. Curr. Opin. Microbiol. 15, 3–9 (2012).
Lindstedt, B.-A., Finton, M. D., Porcellato, D. & Brandal, L. T. High frequency of hybrid Escherichia coli strains with combined Intestinal Pathogenic Escherichia coli (IPEC) and Extraintestinal Pathogenic Escherichia coli (ExPEC) virulence factors isolated from human faecal samples. BMC Infect. Dis. 18, 1–12 (2018).
Dale, A. P. & Woodford, N. Extra-intestinal pathogenic Escherichia coli (ExPEC): disease, carriage and clones. J. Infect. 71, 615–626 (2015).
Kallonen, T. et al. Systematic longitudinal survey of invasive Escherichia coli in England demonstrates a stable population structure only transiently disturbed by the emergence of ST131. Genome Res. 27, 1437–1449 (2017).
Salipante, S. J. et al. Large-scale genomic sequencing of extraintestinal pathogenic Escherichia coli strains. Genome Res 25, 119–128 (2015).
Weissman, S. J. et al. High-resolution two-locus clonal typing of extraintestinal pathogenic Escherichia coli. Appl. Environ. Microbiol. 78, 1353–1360 (2012).
Köhler, C.-D. & Dobrindt, U. What defines extraintestinal pathogenic Escherichia coli? Int. J. Med. Microbiol. 301, 642–647 (2011).
Pitout, J. D. & DeVinney, R. Escherichia coli ST131: a multidrug-resistant clone primed for global domination. F1000Research 6, F1000 Faculty Rev–F1000 Faculty 195 (2017).
Phan, M.-D. et al. Plasmid-mediated ciprofloxacin resistance imparts a selective advantage on Escherichia coli ST131. Antimicrob. Agents Chemother. 66, e02146–21 (2022).
Chen, L. et al. Genetic characterization of extraintestinal Escherichia coli isolates from chicken, cow and swine. AMB Express 8, 1–11 (2018).
Osugui, L., de Castro, A. P., Iovine, R., Irino, K. & Carvalho, V. Virulence genotypes, antibiotic resistance and the phylogenetic background of extraintestinal pathogenic Escherichia coli isolated from urinary tract infections of dogs and cats in Brazil. Vet. Microbiol. 171, 242–247 (2014).
Hu, J. et al. Characteristics, pathogenic mechanism, zoonotic potential, drug resistance, and prevention of avian pathogenic Escherichia coli (APEC). Front. Microbiol. 13, 1049391 (2022).
Rabinowitz, P. & Conti, L. Links among human health, animal health, and ecosystem health. Annu. Rev. Public Health 34, 189–204 (2013).
Larsson, D., Gaze, W., Laxminarayan, R. & Topp, E. AMR, One Health and the environment. Nat. Microbiol. 8, 754–755 (2023).
Tan, C. et al. Serotypes and virulence genes of extraintestinal pathogenic Escherichia coli isolates from diseased pigs in China. Vet. J. 192, 483–488 (2012).
Ma, J. et al. Screening virulence factors of porcine extraintestinal pathogenic Escherichia coli (an emerging pathotype) required for optimal growth in swine blood. Transbound. Emerg. Dis. 68, 2005–2016 (2021).
Singer, R. S. Urinary tract infections attributed to diverse ExPEC strains in food animals: evidence and data gaps. Front. Microbiol. 6, 28 (2015).
Bélanger, L. et al. Escherichia coli from animal reservoirs as a potential source of human extraintestinal pathogenic E. coli. FEMS Immunol. Med. Microbiol. 62, 1–10 (2011).
Mora, A. et al. Poultry as reservoir for extraintestinal pathogenic Escherichia coli O45: K1: H7-B2-ST95 in humans. Vet. Microbiol. 167, 506–512 (2013).
Bergeron, C. R. et al. Chicken as reservoir for extraintestinal pathogenic Escherichia coli in humans. Can. Emerg. Infect. Dis. 18, 415 (2012).
García, V. et al. Genomics, biofilm formation and infection of bladder epithelial cells in potentially uropathogenic Escherichia coli (UPEC) from animal sources and human urinary tract infections (UTIs) further support food-borne transmission. One Health 16, 100558 (2023).
Zhuge, X. et al. Chicken‐source Escherichia coli within phylogroup F shares virulence genotypes and is closely related to extraintestinal pathogenic E. coli causing human infections. Transbound. Emerg. Dis. 68, 880–895 (2021).
Riley, L. W. Extraintestinal foodborne pathogens. Annu. Rev. Food Sci. Technol. 11, 275–294 (2020).
Díaz-Jiménez, D., García-Meniño, I., Herrera, A., Lestón, L. & Mora, A. Microbiological risk assessment of Turkey and chicken meat for consumer: Significant differences regarding multidrug resistance, mcr or presence of hybrid aEPEC/ExPEC pathotypes of E. coli. Food Control 123, 107713 (2021).
Sun, J. et al. Plasmid-encoded tet (X) genes that confer high-level tigecycline resistance in Escherichia coli. Nat. Microbiol. 4, 1457–1464 (2019).
Peng, Z. et al. Antimicrobial resistance and population genomics of multidrug-resistant Escherichia coli in pig farms in mainland China. Nat. Commun. 13, 1116 (2022).
Pitout, J. D. & Chen, L. The significance of epidemic plasmids in the success of multidrug-resistant drug pandemic extraintestinal pathogenic Escherichia coli. Infect. Dis. Ther. 12, 1029–1041 (2023).
Accogli, M. et al. IncI1 plasmids associated with the spread of CMY‐2, CTX‐M‐1 and SHV‐12 in Escherichia coli of animal and human origin. Clin. Microbiol. Infect. 19, E238–E240 (2013).
Despotovic, M., de Nies, L., Busi, S. B. & Wilmes, P. Reservoirs of antimicrobial resistance in the context of One Health. Curr. Opin. Microbiol. 73, 102291 (2023).
Ding, Y. et al. Clonal analysis and virulent traits of pathogenic extraintestinal Escherichia coli isolates from swine in China. BMC Vet. Res. 8, 1–7 (2012).
Zong, B. et al. Characterization of multiple type-VI secretion system (T6SS) VgrG proteins in the pathogenicity and antibacterial activity of porcine extra-intestinal pathogenic Escherichia coli. Virulence 10, 118–132 (2019).
Spindola, M. G. et al. Genetic diversity, virulence genotype and antimicrobial resistance of uropathogenic Escherichia coli (UPEC) isolated from sows. Vet. Q. 38, 79–87 (2018).
Zhu, Y. et al. Characterization and virulence clustering analysis of extraintestinal pathogenic Escherichia coli isolated from swine in China. BMC Vet. Res. 13, 1–10 (2017).
Holcomb, D. A., Quist, A. J. & Engel, L. S. Exposure to industrial hog and poultry operations and urinary tract infections in North Carolina. Usa. Sci. Total Environ. 853, 158749 (2022).
Koch, B. J., Hungate, B. A. & Price, L. B. Food‐animal production and the spread of antibiotic resistance: the role of ecology. Front. Ecol. Environ. 15, 309–318 (2017).
Jiang, H.-X. et al. High prevalence and widespread distribution of multi-resistant Escherichia coli isolates in pigs and poultry in China. Vet. J. 187, 99–103 (2011).
Kaper, J. B., Nataro, J. P. & Mobley, H. L. Pathogenic Escherichia coli. Nat. Rev. Microbiol. 2, 123–140 (2004).
Sora, V. M. et al. Extraintestinal pathogenic Escherichia coli: Virulence factors and antibiotic resistance. Pathogens 10, 1355 (2021).
Shao, Y., Wang, Y., Yuan, Y. & Xie, Y. A systematic review on antibiotics misuse in livestock and aquaculture and regulation implications in China. Sci. Total Environ. 798, 149205 (2021).
Ma, J. et al. Large-scale studies on antimicrobial resistance and molecular characterization of Escherichia coli from food animals in developed areas of eastern China. Microbiol. Spectr. 10, e02015–e02022 (2022).
Zhang, P. et al. Surveillance of antimicrobial resistance among Escherichia coli from chicken and swine, China, 2008–2015. Vet. Microbiol. 203, 49–55 (2017).
Magiorakos, A.-P. et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin. Microbiol. Infect. 18, 268–281 (2012).
Krishnaraju, M. et al. Complete sequencing of an IncX3 plasmid carrying blaNDM-5 allele reveals an early stage in the dissemination of the blaNDM gene. Indian J. Med. Microbiol. 33, 30–38 (2015).
Snesrud, E. et al. A model for transposition of the colistin resistance gene mcr-1 by ISApl1. Antimicrob. Agents Chemother. 60, 6973–6976 (2016).
Wang, R. et al. The global distribution and spread of the mobilized colistin resistance gene mcr-1. Nat. Commun. 9, 1179 (2018).
Lu, X. et al. Epidemiologic and genomic insights on mcr-1-harbouring Salmonella from diarrhoeal outpatients in Shanghai, China, 2006–2016. EBioMedicine 42, 133–144 (2019).
Luo, Q. et al. MDR Salmonella enterica serovar Typhimurium ST34 carrying mcr-1 isolated from cases of bloodstream and intestinal infection in children in China. J. Antimicrob. Chemother. 75, 92–95 (2020).
Zheng, B. et al. Occurrence and genomic characterization of two MCR-1-producing Escherichia coli isolates from the same mink farmer. mSphere 4, e00602–e00619 (2019).
Wang, J. et al. Evolution and comparative genomics of F33: A−: B− plasmids carrying blaCTX-M-55 or blaCTX-M-65 in Escherichia coli and Klebsiella pneumoniae isolated from animals, food products, and humans in China. mSphere 3, 00137–18 (2018).
Liu, L. et al. blaCTX-M-1/9/1 hybrid genes may have been generated from blaCTX-M-15 on an IncI2 plasmid. Antimicrob. Agents Chemother. 59, 4464–4470 (2015).
Bok, E., Kożańska, A., Mazurek-Popczyk, J., Wojciech, M. & Baldy-Chudzik, K. Extended phylogeny and extraintestinal virulence potential of commensal Escherichia coli from piglets and sows. Int. J. Environ. Res. Public Health 17, 366 (2020).
Reid, C. J. et al. Porcine commensal Escherichia coli: a reservoir for class 1 integrons associated with IS26. Microb. Genomics 3, e000143 (2017).
Zingali, T. et al. Whole genome sequencing analysis of porcine faecal commensal Escherichia coli carrying class 1 integrons from sows and their offspring. Microorganisms 8, 843 (2020).
AbuOun, M. et al. Characterizing antimicrobial resistant Escherichia coli and associated risk factors in a cross-sectional study of pig farms in Great Britain. Front. Microbiol. 11, 861 (2020).
von Mentzer, A. et al. Identification of enterotoxigenic Escherichia coli (ETEC) clades with long-term global distribution. Nat. Genet. 46, 1321–1326 (2014).
Muloi, D. M. et al. Population genomics of Escherichia coli in livestock-keeping households across a rapidly developing urban landscape. Nat. Microbiol. 7, 581–589 (2022).
Denamur, E., Clermont, O., Bonacorsi, S. & Gordon, D. The population genetics of pathogenic Escherichia coli. Nat. Rev. Microbiol. 19, 37–54 (2021).
Sun, Y. & Kim, S. W. Intestinal challenge with enterotoxigenic Escherichia coli in pigs, and nutritional intervention to prevent postweaning diarrhea. Anim. Nutr. 3, 322–330 (2017).
García, V. et al. F4-and F18-positive enterotoxigenic Escherichia coli isolates from diarrhea of postweaning pigs: genomic characterization. Appl. Environ. Microbiol. 86, e01913–e01920 (2020).
Rasko, D. A. et al. Origins of the E. coli Strain causing an outbreak of hemolytic-uremic syndrome in Germany. N. Engl. J. Med. 365, 709–717 (2011).
Santos, A. C. D. M., Santos, F. F., Silva, R. M. & Gomes, T. A. T. Diversity of hybrid-and hetero-pathogenic Escherichia coli and their potential implication in more severe diseases. Front. Cell. Infect. Microbiol. 10, 339 (2020).
Kanje, L. E. et al. Short reads-based characterization of pathotype diversity and drug resistance among Escherichia coli isolated from patients attending regional referral hospitals in Tanzania. BMC Med. Genomics 17, 110 (2024).
Royer, G. et al. Phylogroup stability contrasts with high within sequence type complex dynamics of Escherichia coli bloodstream infection isolates over a 12-year period. Genome Med. 13, 77 (2021).
García-Meniño, I. et al. Swine enteric colibacillosis in Spain: pathogenic potential of mcr-1 ST10 and ST131 E. coli isolates. Front. Microbiol. 9, 420699 (2018).
Roer, L. et al. Escherichia coli sequence type 410 is causing new international high-risk clones. mSphere 3, 00337–18 (2018).
Feng, Y. et al. Key evolutionary events in the emergence of a globally disseminated, carbapenem resistant clone in the Escherichia coli ST410 lineage. Commun. Biol. 2, 322 (2019).
Guo, S. et al. Human-associated fluoroquinolone-resistant Escherichia coli clonal lineages, including ST354, isolated from canine feces and extraintestinal infections in Australia. Microbes Infect. 17, 266–274 (2015).
Xia, F. et al. Complete genomic analysis of ST117 lineage extraintestinal pathogenic Escherichia coli (ExPEC) to reveal multiple genetic determinants to drive its global transmission: ST117 E. coli as an emerging multidrug‐resistant foodborne ExPEC with zoonotic potential. Transbound. Emerg. Dis. 69, 3256–3273 (2022).
Zhang, B. et al. Prevalence and antimicrobial susceptibilities of bacterial pathogens in Chinese pig farms from 2013 to 2017. Sci. Rep. 9, 9908 (2019).
Vidovic, N. & Vidovic, S. Antimicrobial resistance and food animals: Influence of livestock environment on the emergence and dissemination of antimicrobial resistance. Antibiotics 9, 52 (2020).
Yassin, A. K. et al. Antimicrobial resistance in clinical Escherichia coli isolates from poultry and livestock, China. PLoS One 12, e0185326 (2017).
Arumugham, V. B., Gujarathi, R. & Cascella, M. Third-Generation Cephalosporins. [Updated 2023 Jun 4]. In: StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK549881/ (2024).
Bui, T. & Preuss, C. V. Cephalosporins. [Updated 2023 Mar 24]. In: StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK551517/ (2024).
Hu, Y. J. & Cowling, B. J. Reducing antibiotic use in livestock. China Bull. W. H. O. 98, 360 (2020).
Cheng, G. et al. Selection and dissemination of antimicrobial resistance in Agri-food production. Antimicrobial Resistance Infect. Control 8, 1–13 (2019).
Sun, H. et al. Co-occurrence of plasmid-mediated resistance genes tet (X4) and blaNDM-5 in a multidrug-resistant Escherichia coli isolate recovered from chicken in China. J. Glob. Antimicrob. Resist. 24, 415–417 (2021).
Puvača, N. & de Llanos Frutos, R. Antimicrobial resistance in Escherichia coli strains isolated from humans and pet animals. Antibiotics 10, 69 (2021).
de Been, M. et al. Dissemination of cephalosporin resistance genes between Escherichia coli strains from farm animals and humans by specific plasmid lineages. PLoS Genet 10, e1004776 (2014).
Ho, P. et al. Dissemination of plasmid‐mediated fosfomycin resistance fosA3 among multidrug‐resistant Escherichia coli from livestock and other animals. J. Appl. Microbiol. 114, 695–702 (2013).
Tacconelli, E. et al. Discovery, research, and development of new antibiotics: the WHO priority list of antibiotic-resistant bacteria and tuberculosis. Lancet Infect. Dis. 18, 318–327 (2018).
Ma, J. et al. Global spread of carbapenem-resistant Enterobacteriaceae: Epidemiological features, resistance mechanisms, detection and therapy. Microbiol. Res. 266, 127249 (2022).
Sharma, J., Sharma, D., Singh, A. & Sunita, K. Colistin resistance and management of drug resistant infections. Can. J. Infect. Dis. Med. Microbiol. 2022 (2022).
Liu, Y.-Y. et al. Emergence of plasmid-mediated colistin resistance mechanism MCR-1 in animals and human beings in China: a microbiological and molecular biological study. Lancet Infect. Dis. 16, 161–168 (2016).
Zhu, L. et al. Comprehensive understanding of the plasmid-mediated colistin resistance gene mcr-1 in aquatic environments. Environ. Sci. Technol. 54, 1603–1613 (2019).
Abozahra, R., Gaballah, A. & Abdelhamid, S. M. Prevalence of the colistin resistance gene MCR-1 in colistin-resistant Klebsiella pneumoniae in Egypt. AIMS Microbiol 9, 177 (2023).
Shen, Y. et al. Prevalence and genetic analysis of mcr-3-positive Aeromonas species from humans, retail meat, and environmental water samples. Antimicrob. Agents Chemother. 62, 00404–00418 (2018).
Hernández, M. et al. Co-occurrence of colistin-resistance genes mcr-1 and mcr-3 among multidrug-resistant Escherichia coli isolated from cattle, Spain, September 2015. Eurosurveillance 22, 30586 (2017).
Alba, P. et al. Molecular epidemiology of mcr-encoded colistin resistance in Enterobacteriaceae from food-producing animals in Italy revealed through the EU harmonized antimicrobial resistance monitoring. Front. Microbiol. 9, 1217 (2018).
Wang, Z. et al. Genetic environment of colistin resistance genes mcr-1 and mcr-3 in Escherichia coli from one pig farm in China. Vet. Microbiol. 230, 56–61 (2019).
Zhang, J. et al. Molecular detection of colistin resistance genes (mcr-1, mcr-2 and mcr-3) in nasal/oropharyngeal and anal/cloacal swabs from pigs and poultry. Sci. Rep. 8, 3705 (2018).
Liu, L., Feng, Y., Zhang, X., McNally, A. & Zong, Z. New variant of mcr-3 in an extensively drug-resistant Escherichia coli clinical isolate carrying mcr-1 and blaNDM-5. Antimicrob. Agents Chemother. 61, 01757–17 (2017).
Castanheira, M., Simner, P. J. & Bradford, P. A. Extended-spectrum β-lactamases: An update on their characteristics, epidemiology and detection. JAC-antimicrobial resistance 3, dlab092 (2021).
Zurfluh, K., Treier, A., Schmitt, K. & Stephan, R. Mobile fosfomycin resistance genes in Enterobacteriaceae—an increasing threat. Microbiologyopen 9, e1135 (2020).
Zhang, Z. et al. Dissemination of IncFII plasmids carrying fosA3 and blaCTX‐M‐55 in clinical isolates of Salmonella enteritidis. Zoonoses Public Health 68, 760–768 (2021).
Palmeira, J. D., Ferreira, H., Madec, J.-Y. & Haenni, M. Pandemic Escherichia coli ST648 isolate harbouring fosA3 and blaCTX-M-8 on an IncI1/ST113 plasmid: A new successful combination for the spread of fosfomycin resistance? J. Glob. Antimicrob. Resist. 15, 254–255 (2018).
Lupo, A., Saras, E., Madec, J.-Y. & Haenni, M. Emergence of blaCTX-M-55 associated with fosA, rmtB and mcr gene variants in Escherichia coli from various animal species in France. J. Antimicrob. Chemother. 73, 867–872 (2018).
Liu, H. et al. Build a bioinformatic analysis platform and apply it to routine analysis of microbial genomics and comparative genomics. Res. Square, PPR485749 (2022).
Bolger, A. M., Lohse, M. & Usadel, B. Trimmomatic: a flexible trimmer for Illumina sequence data. Bioinformatics 30, 2114–2120 (2014).
Bankevich, A. et al. SPAdes: a new genome assembly algorithm and its applications to single-cell sequencing. J. Comput. Biol. 19, 455–477 (2012).
Seemann, T. Prokka: rapid prokaryotic genome annotation. Bioinformatics 30, 2068–2069 (2014).
Inouye, M. et al. SRST2: Rapid genomic surveillance for public health and hospital microbiology labs. Genome Med. 6, 1–16 (2014).
Bessonov, K. et al. ECTyper: in silico Escherichia coli serotype and species prediction from raw and assembled whole-genome sequence data. Microb. Genomics 7, 000728 (2021).
Zankari, E. et al. Identification of acquired antimicrobial resistance genes. J. Antimicrob. Chemother. 67, 2640–2644 (2012).
Bortolaia, V. et al. ResFinder 4.0 for predictions of phenotypes from genotypes. J. Antimicrob. Chemother. 75, 3491–3500 (2020).
Zankari, E. et al. PointFinder: a novel web tool for WGS-based detection of antimicrobial resistance associated with chromosomal point mutations in bacterial pathogens. J. Antimicrob. Chemother. 72, 2764–2768 (2017).
Page, A. J. et al. Roary: rapid large-scale prokaryote pan genome analysis. Bioinformatics 31, 3691–3693 (2015).
Page, A. J. et al. SNP-sites: rapid efficient extraction of SNPs from multi-FASTA alignments. Microb. Genomics 2, e000056 (2016).
Stamatakis, A. RAxML version 8: a tool for phylogenetic analysis and post-analysis of large phylogenies. Bioinformatics 30, 1312–1313 (2014).
De Coster, W., D’hert, S., Schultz, D. T., Cruts, M. & Van Broeckhoven, C. NanoPack: visualizing and processing long-read sequencing data. Bioinformatics 34, 2666–2669 (2018).
Kolmogorov, M., Yuan, J., Lin, Y. & Pevzner, P. A. Assembly of long, error-prone reads using repeat graphs. Nat. Biotechnol. 37, 540–546 (2019).
Walker, B. J. et al. Pilon: an integrated tool for comprehensive microbial variant detection and genome assembly improvement. PLoS One 9, e112963 (2014).
Robertson, J. & Nash, J. H. MOB-suite: software tools for clustering, reconstruction and typing of plasmids from draft assemblies. Microb. Genomics 4, e000206 (2018).
Siguier, P., Pérochon, J., Lestrade, L., Mahillon, J. & Chandler, M. ISfinder: the reference centre for bacterial insertion sequences. Nucleic Acids Res. 34, D32–D36 (2006).
Néron, B. et al. IntegronFinder 2.0: identification and analysis of integrons across bacteria, with a focus on antibiotic resistance in Klebsiella. Microorganisms 10, 700 (2022).
Brown, C. T. & Irber, L. sourmash: a library for MinHash sketching of DNA. J. open source Softw. 1, 27 (2016).
Li, H. Aligning sequence reads, clone sequences and assembly contigs with BWA-MEM. arXiv preprint arXiv:1303.3997, (2013).
Quinlan, A. R. & Hall, I. M. BEDTools: a flexible suite of utilities for comparing genomic features. Bioinformatics 26, 841–842 (2010).
Conway, J. R., Lex, A. & Gehlenborg, N. UpSetR: an R package for the visualization of intersecting sets and their properties. Bioinformatics 33, 2938–2940 (2017).
Letunic, I. & Bork, P. Interactive Tree Of Life (iTOL) v5: an online tool for phylogenetic tree display and annotation. Nucleic Acids Res. 49, W293–W296 (2021).
Shannon, P. et al. Cytoscape: a software environment for integrated models of biomolecular interaction networks. Genome Res. 13, 2498–2504 (2003).
Acknowledgements
This work was funded by the National Key Research and Development Program (2022YFD1800901, 2021YFD1800402), the China Agriculture Research System of MOF and MARA (CARS-35), the Walmart Food Safety Collaboration Center of Walmart Foundation (Project # 61626817), the National Natural Science Foundation of China (31970003). Dr. Michael Gänzle are acknowledged for critical feedback on the manuscript.
Author information
Authors and Affiliations
Contributions
J.Z. and C.T. designed the study; C.T., Y.Z., Y.L., X.W., and Z.P. conducted sample collection and laboratory experiments; X.L., H.H., and T.W. conducted bioinformatic analyzes; X.L. and J.Z. drafted the manuscript; C.T., M.S., and H.C. revised the manuscript. All authors reviewed and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Communications thanks Henrik Christensen, Max Cummins and Azucena Mora for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Source data
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Li, X., Hu, H., Zhu, Y. et al. Population structure and antibiotic resistance of swine extraintestinal pathogenic Escherichia coli from China. Nat Commun 15, 5811 (2024). https://doi.org/10.1038/s41467-024-50268-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41467-024-50268-2
- Springer Nature Limited