Abstract
Background
Neonatal sepsis remains a leading cause of mortality in neonatal units. Neonatologist-performed echocardiography (NPE) offers the potential for early detection of sepsis-associated cardiovascular dysfunction. This review examines available echocardiographic findings in septic neonates.
Methods
Following Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines, we systematically reviewed prospective observational, cross-sectional, case control, and cohort studies on septic newborns with echocardiographic assessments from PubMed, Scopus and Embase. Quality assessment employed the Newcastle–Ottawa Scale, with results analyzed descriptively.
Results
From an initial pool of 1663 papers, 12 studies met inclusion criteria after relevance screening and eliminating duplicates/excluded studies. The review encompassed 438 septic newborns and 232 controls. Septic neonates exhibited either increased risk of pulmonary hypertension or left ventricular diastolic dysfunction, and a warm shock physiology characterized by higher cardiac outputs.
Discussion
The included studies exhibited heterogeneity in sepsis definitions, sepsis severity scores, echocardiographic evaluations, and demographic data of newborns. Limited sample sizes compromised analytical interpretability. Nonetheless, this work establishes a foundation for future high-quality echocardiographic studies.
Conclusion
Our review confirms that septic neonates show significant hemodynamic changes that can be identified using NPE. These findings underscore the need for wider NPE use to tailor hemodynamics-based strategies within this population.
Impact
-
1.
Our study emphasizes the value of neonatologist-performed echocardiography (NPE) as a feasible tool for identifying significant hemodynamic changes in septic neonates.
-
2.
Our study underscores the importance of standardized echocardiographic protocols and frequent monitoring of cardiac function in septic neonates.
-
3.
The impact of the study lies in its potential to increase researchers’ awareness for the need for more high-quality echocardiographic data in future studies. By promoting wider use of NPE, neonatologists can more accurately assess the hemodynamic status of septic newborns and tailor treatment approaches, potentially improving patient outcomes.
Similar content being viewed by others
Introduction
Neonatal sepsis is a leading disease in neonatal intensive care units (NICU) and remains the second cause of death among infants ≤28 days in developing countries.1 Two-thirds of these deaths occur in NICUs, and approximately 31% are considered preventable.1 Cardiac failure is the primary cause of sepsis-related deaths in neonates.2,3 Timely recognition of clinical symptoms, prompt antibiotic administration within one hour of suspicion,4 and timely circulatory support are crucial in reducing neonatal sepsis-related mortality.
Sepsis-related inflammation may lead to severe hemodynamic instability and cardiac dysfunction in both preterm and full-term newborns due to their limited functional reserve. Neonatologist-performed echocardiography (NPE) can provide real-time insights into hemodynamic phenotypes, supporting individualized management of cardiovascular dysfunction. Recent investigations have increased awareness of sepsis-induced myocardial dysfunction,5 however the absolute frequency and the nature of hemodynamic compromise during sepsis in newborns is not widely appreciated.
In this review we conducted a systematic analysis and synthesis of available studies that evaluated echocardiographic findings in septic neonates, aiming to describe echocardiographic parameters currently used in this population.
Sepsis-induced cardiovascular dysfunction
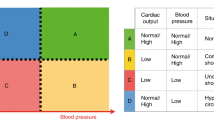
Sepsis-induced cardiovascular dysfunction is traditionally categorized into ‘warm’ shock (hyperdynamic status) and ‘cold’ shock physiology (hypodynamic status).
‘Warm’ shock is characterized by vasodilation, low systemic vascular resistance (SVR), rapid capillary refill time (CRT), and flushed skin. Severe and diffuse vasodilation may cause low systemic venous return and decreased preload with consequent altered left ventricular (LV) and right ventricular (RV) output and compensatory tachycardia.
Conversely, ‘cold’ shock involves general vasoconstriction, resulting in cold extremities, prolonged CRT, and weak peripheral pulses. Peripheral vasoconstriction causes increased afterload with potential LV function impairment, reduced stroke volume, and compromised filling. Despite suboptimal cardiac output, blood pressure often remains within normal ranges, with hypotension becoming a late finding due to severe LV dysfunction.
The origins of hemodynamic compromise in septic patients is multifactorial and a combination of different mechanisms have been studied so far in animal and older human models.
Immune system activation and inflammation may disrupt endothelial integrity,6,7 causing microvascular dysfunction. In some cases, the aberrant systemic inflammatory response syndrome (SIRS) that may develop determines a severe compromise to microcirculatory perfusion and oxygen delivery.8
Animal studies reveal that sepsis-related inflammation directly affects cardiomyocytes, leading to macrophages and mononuclear cells invasion, fibroblast overproliferation and extracellular matrix (ECM) deposition, which impairs cardiac contractility and may progress to heart failure.9 Sepsis also triggers neuroendocrine responses involving catecholamine release,10 reduced vasopressin,11 and corticosteroid reduction,12 impacting vascular tone regulation.13
Clinical assessment of sepsis-related cardiovascular dysfunction
In routine clinical practice, vital parameters traditionally used to diagnose cardiovascular compromise are increased heart rate (HR), low blood pressure, urine output, signs of poor perfusion, clinical appearance, capillary refill time (CRT) > 3 s, raised lactate levels and altered acid-base status. However, clinical assessment of peripheral circulation through these parameters is highly time and patient-dependent and inter-observer variability is still high.14,15
New techniques are therefore needed to improve the continuous monitoring of hemodynamic homeostasis.
Recently, emerging tools such as near-infrared spectroscopy (NIRS)16 and neonatologist-performed echocardiography (NPE)17,18 have improved the clinical assessment of sepsis-related impaired hemodynamic status of critically ill patients.
Echocardiographic modalities to evaluate sepsis-induced myocardial dysfunction
To date, two-dimensional mode (2D mode), motion mode (M-mode), pulsed wave Doppler (PW Doppler), and continuous wave Doppler (CW Doppler) are standard echocardiographic methods employed to evaluate biventricular cardiac function in sepsis in accordance with established guidelines.19,20
Although qualitative assessment of LV systolic function has been largely used, quantitative measures are preferred.20
In particular, left ventricular systolic function can be assessed by geometric linear or volumetric quantification of LV chambers through LV ejection fraction (LVEF) and fractional shortening (FS). The pediatric guidelines suggest calculating FS from 2D parasternal short-axis views, with measurements averaged over three cardiac cycles21 but in newborns FS can be limited by abnormal septal motion and altered ventricular geometry.
LVEF is calculated from the equation EF = (end-diastolic volume - end-systolic volume)/end-diastolic volume and it can be obtained from a standard M-mode tracing or from 2D images providing a value indicative of the percentage of LV volume change during cardiac cycle.
2D echocardiography is also used to assess LV diastolic function through E/A ratio from an apical four-chamber view with the PW Doppler sample volume placed at the mitral valve leaflets tips: this represents the ratio of peak velocity blood flow from left ventricular relaxation in early diastole (the E-wave) to peak velocity flow in late diastole caused by atrial contraction (the A wave).22
Right ventricle (RV) global systolic function is usually assessed through quantitative measurement such as tricuspid annular plane systolic excursion (TAPSE) using M-mode23 and RV fractional area change (FAC).24
A key component of NPE is also the assessment of ductal patency, ductal shunt direction, and ductal pressure gradients. Patent ductus arteriosus (PDA) is usually visualized from the modified left parasternal “ductal” view using both Color Doppler and PW Doppler. Evaluation of volume overload on LV provides additional information about the PDA hemodynamic significance.20
In addition to conventional echocardiographic parameters, Tissue Doppler imaging (TDI) studies have been proposed to obtain additional information about LV and RV function. TDI is an echocardiographic technique that is based on Doppler measurement of myocardial motion velocity. TDI studies are performed from the 4-chamber view, with the Doppler sample volume placed at the lateral and septal segments of the mitral annulus and at lateral segment of the tricuspid annulus. For both ventricle peak systolic (S’), early (e’) and late diastolic (a’) waves can be measured.25
Recently, 2D strain echocardiography (SE) has been applied to assess myocardial function in newborn populations. SE is an innovative technique which assesses biventricular function by tracking tissue deformation as a measure of global and segmental myocardial function. The utility of SE has been previously demonstrated in septic pediatric patients.26,27
A figure illustrating NPE standard views is provided in Fig. 1 and a summary of traditionally used echocardiographic parameters to assess RV function, LV function, pulmonary hypertension, and PDA is provided for the reader in Table 1.
Echocardiographic parameters and poor prognosis in septic newborns
To date, a limited number of studies have investigated the relationship between echocardiographic parameters and outcomes in septic newborns28
Conversely, a larger number of studies in the last decades have identified specific echocardiographic parameters which may be predictive of adverse outcome in the septic adult populations.
In particular, sepsis-induced mortality has been reported to be significantly associated with TDI-derived LV diastolic dysfunction29 but not with systolic function.30
The prognostic value of echocardiography in the septic pediatric population is still largely debated. A recent systematic review and meta-analysis by Sanfilippo and colleagues failed to identify a statistically relevant association between mortality and LV or RV systolic function in the pediatric population.28
However, the authors speculated that LV diastolic dysfunction and increased LV filling pressures may have a prognostic relevance in pediatric septic patients as non-survivors demonstrated lower peak velocity of early diastolic mitral annular motion determined by PW Doppler, albeit not reaching statistical significance.
Data regarding the prognostic value of echocardiography in septic newborn are largely under-evaluated and large prospective studies are required.
Methods
Search strategy and selection criteria
We performed a systematic review following the search method Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.31
Prior to commencing the search, a detailed protocol was agreed to determine search modalities, eligibility criteria, and all methodological details.
We searched for prospective observational, cross-sectional studies, case control and cohort studies conducted on septic newborns that reported echocardiographic parameters indicative of sepsis-induced myocardial dysfunction.
We conducted an extensive search on the following databases (with last update performed on June 1st, 2022): PubMed (https://pubmed.ncbi.nlm.nih.gov/), Scopus (https://www.scopus.com/search/form.uri?display=basic#basic) and Embase (https://www.embase.com/?phase=continueToApp#search) using the following terms: (“echocardiography” AND “sepsis” AND “newborn”) OR (“echocardiography” AND “sepsis” AND “neonate”).
For reliability, two review authors (F.P. and D.U.D.R.) independently analyzed the available literature. Additional studies were identified by authors based on their knowledge in the field, if not already included by literature search.
We have systematically excluded (1) studies not written in English language, (2) studies lacking full-text availability, (3) studies lacking reported data pertaining to echocardiographic analyses, and (4) those involving subjects beyond the neonatal age cohort.
Any disagreement about study eligibility was resolved by discussion with a third reviewer (C.A.) until consensus.
Data extraction
Data were extracted by a systematic evaluation of the abstracts and by reviewing the full text of selected article, excluding those not meeting the eligibility criteria and removing duplicates.
Data from eligible studies were independently extracted by two review authors (F.P. and D.U.D.R.). Pertinent findings from the included studies were tabulated under the following headings: year, study design, sample size, gestational age, presence of a control group or not, sepsis score utilized, late-onset sepsis/early-onset sepsis, timing of echocardiographic studies, who performed echocardiography (neonatologist or cardiologist), echocardiographic modalities used (two-dimensional mode - 2D mode -, motion mode - M-mode -, pulsed wave Doppler – PW Doppler -, continuous wave Doppler – CW Doppler -), key echocardiographic findings, interpretations of results.
We developed a dedicated online data extraction sheet (Excel 16: Microsoft Corporation, Redmond, WA). Data from included records were independently extracted by each investigator using this data extraction sheet and then cross-verified.
Risk of bias assessment
The quality of included cohort studies and the risk of bias using the Newcastle–Ottawa Scale (NOS) were evaluated. The NOS comprises “participant selection”, “comparability of study groups,” and “assessment of outcome or exposure”. A score above 6–7 denotes a reasonable quality. Two review authors (F.P. and D.U.D.R.) independently assessed the risk of bias of included studies.32
Results
Initially, 1663 papers were identified through database search. After removing duplicates, 1060 publications were screened. Following title and abstract review, 31 studies were potentially eligible, and ultimately, 12 studies were included (Fig. 2): of these, 8 were prospective studies.33,34,35,36,37,38,39,40
Studies were conducted in India (6/12: 50%), Egypt (3/12: 25%), Germany (1/12: 8.3%), Netherlands/Australia (1/12: 8.3%) and Saudi Arabia (1/12: 8.3%).
Four studies (33.3%) included only septic neonates,34,36,40,41 whereas a control group of non-septic healthy gestational age-matched and postnatal age-matched neonates was available in the remaining eight studies reviewed (66.6%).33,35,37,38,39,42,43,44
A total of 438 septic newborns and 232 controls were included in the present review.
Five studies (41.7%)37,39,40,41,43 were performed in preterm neonates, while two studies (16.7%) excluded preterm babies33,42 and four studies (33.3%) included both term and preterm babies.34,36,38,44
Diagnostic criteria and severity scores for “sepsis” and “septic shock” were used in 50% of the studies reviewed.33,36,37,39,42,44 Sepsis score and sepsis criteria utilized were: Töllner Sepsis Score,45 Hematologic Scoring System,46 NNF Clinical Practice Guidelines47 and International Pediatric Consensus Conference statement on sepsis and organ dysfunction in Pediatrics.48 Only 3/6 studies (50.0%) used the same score (Töllner septic score).33,36,37
A clear definition of the timing of sepsis onset was missing in 25% of selected issues:34,35,42 eight studies (66.7%) included infants with LOS in the study setting,33,36,37,39,40,41,43,44 whereas in a study (8.3%), performed by Fahmey and colleagues,38 patients with LOS or either early-onset sepsis (EOS) underwent echocardiography.
Definition of LOS as onset after 72 h of life was available in five studies36,37,38,40,41 whereas Hassan and colleagues43 considered onset over 7 days of life.
The timing of echocardiographic studies was reported only in four studies (33.3%).33,36,37,44 The exams were performed at median time of 15.6 h from the time of suspicion of septic episode.
A total of 5 studies (41.7%) provided indications about who performed echocardiographic studies, whereas in the majority of cases (58.3%) this information was not available. The physician who performed echocardiography was a neonatologist trained and experienced in NPE in 4/5 studies (80.0%).34,36,39,41 Beyond standard modalities (used by all authors), two studies (16.7%) included TDI findings,33,38 but none used strain echocardiography to obtain myocardial deformation data.
The main features of included studies are summarized for the reader in Table 2.
Altered Echocardiographic parameters in septic newborns
A limited number of observational studies investigated cardiac function in septic term and preterm infants. These studies indicate that hemodynamic disturbance is a common finding in neonatal sepsis.
A principal finding of our systematic review is that septic newborns are at higher risk of developing pulmonary hypertension (3/12: 25.0%); with septic newborns demonstrating higher mean systolic pulmonary artery pressure (PASP) than controls.34,37,38
Moreover, septic newborns were observed to have a lower E/A ratio across the mitral valve (MV) consistent with LV diastolic dysfunction.35,38,42,44
Although global myocardial performance tends to be impaired,33 septic newborns had a typical warm shock physiology, characterized by lower venous return and higher biventricular cardiac outputs when compared to controls.36,39,40,41,43
Quality of included studies
Most studies including septic newborns had a reasonable quality according to Newcastle–Ottawa Scale, as reported in Table 3.
Discussion
Understanding the underlying physio-pathological mechanisms responsible for impaired hemodynamic dysfunction during sepsis is crucial to individualize therapeutic interventions.
Adequate hemodynamic stabilization is the cornerstone of resuscitation of the critically ill septic newborn and bedside NPE may represent a valid tool to assess septic patients, though it is not yet in routine use for this purpose in NICU settings.
NPE refers to functional echocardiography performed by neonatologists trained in hemodynamic assessment of critically ill neonates: it has been used for cardiac function evaluation in several scenarios49,50,51 and NPE allows frequent re-evaluation and readjustment of management strategies on the basis of the changing clinical and pathophysiological picture.
The main finding of our systematic review is that neonatal sepsis is mostly characterized by a phenotype of warm shock physiology, consisting of higher cardiac outputs, lower venous return and higher inferior vena cava collapsibility36,39,40,41 as well as higher risk of pulmonary hypertension34,37,38 and LV diastolic dysfunction.35,38,42,44
Echocardiographic measures of pulmonary hypertension
Pulmonary arterial pressures are frequently increased during septic episodes.34,37,38
Acute pulmonary hypertension has been previously reported as a complication during neonatal sepsis52,53 but its systematic evaluation is not routinely performed and the use of pulmonary vasodilator medication in the context of sepsis has been rarely described.54
One pathophysiological explanation of this finding may be that sepsis-induced acidosis and hypoxia induce pulmonary vasoconstriction resulting in increased pulmonary vascular resistance and pulmonary arterial pressure, promoting patency of the ductus arteriosus and causing the classical clinical phenotype of persistent pulmonary hypertension of the newborn.
Persistently higher pulmonary pressures may contribute to impairment of right ventricular function and secondary LV failure via ventricular interdependence.55
The mechanisms and clinical significance of pulmonary hypertension in neonatal sepsis therefore remain largely under-evaluated and may deserve more attention in future studies.
Echocardiographic measures of diastolic cardiac function in the left ventricle
Septic newborns also show altered mitral inflow pattern,38,44 larger end-diastolic LV diameter33 and lower LV end-diastolic area42 suggesting an early sepsis-induced LV diastolic dysfunction is a common findings.
Traditional mitral inflow Doppler patterns for assessing left ventricular diastolic function are highly dependent on preload and can change significantly as diastolic dysfunction progresses, whereas TDI (Tissue Doppler Imaging) evaluation is less affected by loading conditions.
Septic newborns display lower TDI-derived mitral and tricuspid e’ velocities, and higher TDI-derived mitral and tricuspid a’ velocities, which may reflect impaired inherent myocardial relaxation during diastole.33
However, the pathophysiology of sepsis-induced diastolic dysfunction has not been fully elucidated.
In early sepsis, an initial hyperdynamic state with excessive proinflammatory cytokines causing increased vascular permeability and vasodilation has been described.5
The associated reduction in relative circulatory volume leads to reduced cardiac preload and stroke volume (SV), despite a normal LV ejection fraction (EF). Ventricular tachycardia is a compensatory response to maintain adequate cardiac output, but may impair LV diastolic function by shortening diastolic filling times and coronary perfusion intervals and worsen LV function via ventricular interdependence.56 Moreover, a sustained proinflammatory state may also lead to myocardial edema directly altering cardiac compliance during diastole.57
Diastolic dysfunction and consequent increased LV filling pressures were noted to have a possible negative prognostic value in pediatric and adult septic cohorts28,29 whereas data on neonatal population are limited.
Echocardiographic measures of systolic cardiac function in the RV and LV
A variety of techniques have been employed to assess systolic ventricular function in neonatal sepsis, but must be interpreted in the context of practical limitations and pathophysiological mechanisms of ventricular dysfunction.
Reductions in tricuspid annular plane systolic excursion (TAPSE) have been observed in limited cohorts and may reflect impaired RV systolic function. However, TAPSE is a load-dependent measure, changes in which may reflect altered preload or afterload, rather than inherent myocardial function per se.
Echocardiographic investigation of biventricular systolic function in septic newborns has also generated contradictory findings.
Alzahrani et al. reported lower systolic RV and LV function in septic patients, with lower LV ejection fraction (EF) and fractional shortening (FS) values albeit still within accepted normal ranges.35 However, other investigators observed no differences in conventional echocardiography parameters of systolic function (EF, FS, and atrioventricular inflow velocity).33,39,44
TDI-derived systolic velocity (S’) of the lateral mitral annulus is indicative of longitudinal LV systolic function and has been demonstrated to be well correlated with of LV ejection fraction.58,59
Though the use of TDI in septic newborns is limited, studies included in our systematic review observed lower atrioventricular annular systolic velocities (S’) indicating early systolic dysfunction in both the RV and LV and RV.33 There are several potential factors contributing to the observed variability in systolic function among septic patients. Firstly, the dynamic nature of sepsis-induced cardiac dysfunction may underlie the heterogeneous responses observed; some patients may exhibit compensatory mechanisms leading to increased cardiac function that results within “normal ranges”, while others may experience an early decline in cardiac function (decompensation) during sepsis. Consequently, analyzing a combined cohort may fail to reveal the individual patient pathophysiology due to these divergent patterns. Secondly, the current echocardiographic measures employed may lack the necessary sensitivity to accurately detect clinical changes in cardiac function. For instance, observer variability in assessing cardiac output measures might be greater than the actual clinical alterations in biventricular output. Understanding these potential reasons is crucial for enhancing the reliability of cardiac function assessment in septic patients.
Additionally, the limited sample size of these studies and the arbitrary timing of echocardiography selection may pose challenges in the interpretation of the results.
When compared with conventional echocardiographic parameters, however, TDI imaging was more sensitive in detecting myocardial dysfunction.33 Since conventional echo parameters (EF and FS) are significantly affected by heart rate and ventricular loading conditions, TDI appears to be a valid technique to assess the global systolic function.
We can therefore conclude that NPE studies should include TDI-derived parameters of myocardial function.
An additional measure of ventricular function employed in neonatal sepsis is the myocardial performance index (MPI or TEI index), a time-interval-based index of global cardiac performance which is independent of ventricular geometry.
From our analysis, results about MPI are equivocal. Abdel-Hady et al.33 demonstrated that TDI-derived RV and LV MPI were significantly higher in septic patients whereas both LV and RV MPI were not different in the study by Alzahrani and collegues.35
MPI has a number of inherent limitations that may explain these findings. MPI is highly load-dependent so may reflect altered loading conditions in studied cohorts. Furthermore, as a composite measure changes in MPI do not discriminate between changes in systolic or diastolic conditions. In addition, the use of different techniques, including Doppler-derived MPI and Tissue Doppler Imaging (TDI) may affect comparison between studies.
Given these considerations, MPI may not be a useful measure of hemodynamic function in septic newborns.
In our review, no studies on septic newborns were performed using strain echocardiography (SE). It has been previously demonstrated that pediatric septic patients may show depressed SE parameters that were not shown by FS and that strain compromission may have a prognostic value since it seems to correlate with severity scores.60
We speculate that SE could be applied also in the neonatal population to grade sepsis severity and eventually drive management.
The available evidence suggests that cardiac depression during sepsis is multifactorial. Septic newborns are likely to suffer from both LV and RV systolic and LV diastolic dysfunction and some echo modalities such as TDI may be more sensitive than conventional echocardiography in detecting myocardial dysfunction.
Early recognition and prompt supportive therapy of sepsis-associated myocardial dysfunction are important to reduce morbidity and mortality among septic newborns61,62 although the prognostic significance of echocardiographic parameter is still poorly investigated and deserves further analysis in this population.
Few and small studies have observed that survivors have higher global myocardial performance and higher LV FS indicating better systolic function33,38,44 but larger prospective and systematic studies are needed to identify a reliable association between mortality and parameters of LV or RV function. In light of the above, although it has been established that NPE significantly impacts clinical management of sick neonates, the specific use of NPE in septic newborns may be an important focus.
Monitoring parameters such as cardiac output, myocardial contractility, and ventricular function can guide clinicians in tailoring interventions, optimizing fluid management, and selecting appropriate therapies (inotropes, lusitropes, vasopressors) to address sepsis-related cardiac alterations.
In this review we have highlighted several critical issues. First of all, there are no standardized echocardiographic protocols for hemodynamic assessment of septic newborns. Moreover, the timing of echocardiography was not available in some studies and when present was not uniform among studies: this may contribute to limit the interpretability of the results.
Furthermore, a unique definition of sepsis was missing for the studies included in the review. The currently accepted definitions for sepsis and septic shock are based on different criteria. Recently, the Society of Critical Care Medicine (SCCM) convened the Pediatric Sepsis Definition Taskforce to develop and validate uniform criteria for the definition of sepsis in pediatric population, including newborns.63 Besides this, a general definition for sepsis, sepsis severity scores and sepsis prediction scores are still missing. Gaining a consensus for sepsis definition is paramount for understanding the impact on short- and long-term outcomes of the disease. In order to develop adequate management and treatment strategies for this condition, concerted efforts are required to the development and acceptance of definitive criteria.
Moreover, the studies included in our final analysis demonstrated significant heterogeneity in terms of echocardiographic modalities as well as demographical data of newborns. The fact that study settings were highly variable and included patients were from economically different area of the world, with diverse underlying conditions and sepsis-management strategies represent an additional limitation.
Lastly, the included studies have limited sample sizes, hampering the interpretability of the analyses.
The previously described issues limit the extrapolation of definitive data for septic newborns who underwent NPE but our aim is to increase researchers awareness for the need for more high-quality echocardiographic data in future studies.
Considering our findings, we propose the adoption of a shared functional echocardiography protocol among centers, which is summarized in the Table 1.
An alternative evolving approach to identifying patterns of hemodynamic dysfunction in neonatal sepsis is the development of Artificial Intelligence (AI) algorithms. These may in the future be able to analyze complex data from multiple sources, detect early cardiovascular abnormalities, identify critical markers of sepsis severity, enable continuous monitoring of several parameters, to augment and support clinical decision-making. While implementation challenges remain, AI has the potential to enhance interventions for septic newborns.64,65
Conclusion
Our review confirmed that significant cardiovascular and hemodynamic changes may occur in septic neonates, that can be identified using a feasible and reliable tool such as NPE.
Our findings support for the need for implementation of a wider use of NPE, shared standardized echocardiographic protocols for septic newborns, assess the prognostic value of echocardiography and monitor frequently cardiac function to customize medications according to hemodynamics.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Jacob, J., Kamitsuka, M., Clark, R. H., Kelleher, A. S. & Spitzer, A. R. Etiologies of NICU deaths. Pediatrics 135, e59–e65 (2015).
Raj, S., Killinger, J. S., Gonzalez, J. A. & Lopez, L. Myocardial dysfunction in pediatric septic shock. J. Pediatr. 164, 72–77.e2 (2014).
Weiss, S. L. et al. The epidemiology of hospital death following pediatric severe sepsis: when, why, and how children with sepsis die*. Pediatr. Crit. Care Med. 18, 823–830 (2017).
Schmatz, M. et al. Surviving sepsis in a referral neonatal intensive care unit: association between time to antibiotic administration and in-hospital outcomes. J. Pediatr. 217, 59–65.e1 (2020).
Kharrat, A. & Jain, A. Hemodynamic dysfunction in neonatal sepsis. Pediatr. Res. 91, 413–424 (2022).
Ince, C. et al. The endothelium in sepsis. Shock 45, 259–270 (2016).
Knuefermann, P. et al. Bacterial DNA induces myocardial inflammation and reduces cardiomyocyte contractility: role of Toll-like receptor 9. Cardiovasc. Res. 78, 26–35 (2008).
Virág, M., Leiner, T., Rottler, M., Ocskay, K. & Molnar, Z. Individualized hemodynamic management in sepsis. J. Pers. Med. 11, 157 (2021).
Cuenca, J., Martín-Sanz, P., Álvarez-Barrientos, A. M., Boscá, L. & Goren, N. Infiltration of inflammatory cells plays an important role in matrix metalloproteinase expression and activation in the heart during sepsis. Am. J. Pathol. 169, 1567–1576 (2006).
Frayn, K. N. Hormonal control of metabolism in trauma and sepsis. Clin. Endocrinol. 24, 577–599 (1986).
Aradhya, A. S. et al. Low vasopressin and progression of neonatal sepsis to septic shock: a prospective cohort study. Eur. J. Pediatr. 179, 1147–1155 (2020).
Khashana, A., Ojaniemi, M., Leskinen, M., Saarela, T. & Hallman, M. Term neonates with infection and shock display high cortisol precursors despite low levels of normal cortisol. Acta Paediatr. 105, 154–158 (2016).
Ni, M. et al. Use of vasopressin in neonatal intensive care unit patients with hypotension. J. Pediatr. Pharmacol. Ther. 22, 430–435 (2017).
LeFlore, J. L. & Engle, W. D. Capillary refill time is an unreliable indicator of cardiovascular status in term neonates. Adv. Neonatal Care 5, 147–154 (2005).
Takci, S., Yigit, S., Korkmaz, A. & Yurdakök, M. Comparison between oscillometric and invasive blood pressure measurements in critically ill premature infants. Acta Paediatr. 101, 132–135 (2012).
Zonnenberg, I. A., van Dijk, J., van den Dungen, F. A. M., Vermeulen, R. J. & van Weissenbruch, M. M. The prognostic value of NIRS in preterm infants with (suspected) late-onset sepsis in relation to long term outcome: a pilot study. PLoS ONE 14, e0220044 (2019).
de Boode, W. P. et al. The role of Neonatologist Performed Echocardiography in the assessment and management of neonatal shock. Pediatr. Res. 84, 57–67 (2018).
Groves, A. M. et al. Introduction to neonatologist-performed echocardiography. Pediatr. Res. 84, 1–12 (2018).
Lai, W. W. et al. Guidelines and standards for performance of a pediatric echocardiogram: a report from the Task Force of the Pediatric Council of the American Society of Echocardiography. J. Am. Soc. Echocardiogr. 19, 1413–1430 (2006).
Mertens, L. et al. Targeted neonatal echocardiography in the neonatal intensive care unit: practice guidelines and recommendations for trainingwriting group of the American Society of Echocardiography (ASE) in collaboration with the European Association of Echocardiography (EAE) and the Association for European Pediatric Cardiologists (AEPC). J. Am. Soc. Echocardiogr. 24, 1057–1058 (2011).
Lopez, L. et al. Recommendations for quantification methods during the performance of a pediatric echocardiogram: a report from the Pediatric Measurements Writing Group of the American Society of Echocardiography Pediatric and Congenital Heart Disease Council. J. Am. Soc. Echocardiogr. 23, 465–495 (2010).
Riggs, T. W. et al. Doppler echocardiographic evaluation of right and left ventricular diastolic function in normal neonates. J. Am. Collage Cardiol. 13, 700–705 (1989).
Koestenberger, M. et al. Systolic right ventricular function in preterm and term neonates: reference values of the tricuspid annular plane systolic excursion (TAPSE) in 258 patients and calculation of Z-score values. Neonatology 100, 85–92 (2011).
Koestenberger, M. et al. Right ventricular function in infants, children and adolescents: reference values of the tricuspid annular plane systolic excursion (TAPSE) in 640 healthy patients and calculation of z score values. J. Am. Soc. Echocardiogr. 22, 715–719 (2009).
Aslan, E. et al. Left and right ventricular function by echocardiography, tissue Doppler imaging, carotid intima-media thickness, and asymmetric dimethyl arginine levels in obese adolescents with metabolic syndrome. Cardiol. Young 29, 310–318 (2019).
Basu, S. et al. Two-dimensional speckle tracking imaging detects impaired myocardial performance in children with septic shock, not recognized by conventional echocardiography*. Pediatr. Crit. Care Med. 13, 259–264 (2012).
Patel, M. D. et al. Cardiac dysfunction identified by strain echocardiography is associated with illness severity in pediatric sepsis. Pediatr. Crit. Care Med. 21, e192–e199 (2020).
Sanfilippo, F. et al. Echocardiographic parameters and mortality in pediatric sepsis: a systematic review and meta-analysis*. Pediatr. Crit. Care Med. 22, 251–261 (2021).
Sanfilippo, F. et al. Tissue Doppler assessment of diastolic function and relationship with mortality in critically ill septic patients: a systematic review and meta-analysis. Br. J. Anaesth. 119, 583–594 (2017).
Sanfilippo, F. et al. Diastolic dysfunction and mortality in septic patients: a systematic review and meta-analysis. Intensive Care Med. 41, 1004–1013 (2015).
Moher, D., Liberati, A., Tetzlaff, J. & Altman, D. G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 6, e1000097 (2009).
Ottawa Hospital Research Institute. https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (2021).
Abdel-Hady, H. E., Matter, M. K. & El-Arman, M. M. Myocardial dysfunction in neonatal sepsis: a tissue Doppler imaging study*. Pediatr. Crit. Care Med. 13, 318–323 (2012).
Ahmed, T., Abqari, S., Firdaus, U., Shahab, T. & Ali, S. M. Status of pulmonary artery pressures on echocardiography among high‑risk newborns. J. Clin. Neonatol. 9, 235–241 (2020).
Alzahrani, A. K. Cardiac function affection in infants with neonatal sepsis. J. Clin. Trial 7, 5 (2017).
Deshpande, S., Suryawanshi, P., Chaudhary, N. & Maheshwari, R. Cardiac output in late onset neonatal sepsis. J. Clin. Diagn. Res. 11, 4 (2017).
Deshpande, S. et al. Pulmonary hypertension in late onset neonatal sepsis using functional echocardiography: a prospective study. J. Ultrasound 25, 233–239 (2021).
Fahmey, S. S., Hodeib, M., Refaat, K. & Mohammed, W. Evaluation of myocardial function in neonatal sepsis using tissue Doppler imaging. J. Matern. Fetal Neonatal Med. 33, 3752–3756 (2020).
Saini, S. S., Kumar, P. & Kumar, R. M. Hemodynamic changes in preterm neonates with septic shock: a prospective observational study*. Pediatr. Crit. Care Med. 15, 443–450 (2014).
Yengkhom, R. et al. Point of care neonatal ultrasound in late-onset neonatal sepsis. J. Neonatol. 35, 59–63 (2021).
de Waal, K. & Evans, N. Hemodynamics in preterm infants with late-onset sepsis. J. Pediatr. 156, 918–922.e1 (2010).
Bandyopadhyay, T., Saili, A., Yadav, D. K. & Kumar, A. Correlation of functional echocardiography and clinical parameters in term neonates with shock. J. Neonatal Perinat. Med. 13, 167–173 (2020).
Hassan, M. et al. PO-0540 changes in haemodynamic and peripheral perfusion in suspected neonatal sepsis. Arch. Dis. Child. 99, A426.2–A426 (2014).
Tomerak, R. H., El-Badawy, A. A., Hussein, G., Kamel, N. R. M. & Razak, A. R. A. Echocardiogram done early in neonatal sepsis: what does it add? J. Investig. Med. 60, 680–684 (2012).
Töllner, U. Early diagnosis of septicemia in the newborn. Clinical studies and sepsis score. Eur. J. Pediatr. 138, 331–337 (1982).
Rodwell, R. L., Leslie, A. L. & Tudehope, D. I. Early diagnosis of neonatal sepsis using a hematologic scoring system. J. Pediatr. 112, 761–767 (1988).
NNF Teaching Aids. Newborn care. Neonatal sepsis. Management of neonatal sepsis. NNF clinical practice guidelines http://www.nnfi.org/assests/upload/usefull-links-pdf/Diagnosis_and_Management_of_Neonatal_Sepsis_NNFI_CPG_Dec2021.pdf (2021).
Goldstein, B., Giroir, B. & Randolph, A., International Consensus Conference on Pediatric Sepsis. International pediatric sepsis consensus conference: definitions for sepsis and organ dysfunction in pediatrics*. Pediatr. Crit. Care Med. 6, 2–8 (2005).
de Boode, W. P. et al. Application of Neonatologist Performed Echocardiography in the assessment and management of persistent pulmonary hypertension of the newborn. Pediatr. Res. 84, 68–77 (2018).
Kluckow, M. Use of ultrasound in the haemodynamic assessment of the sick neonate. Arch. Dis. Child. Fetal Neonatal Ed. 99, F332–F337 (2014).
Kluckow, M., Seri, I. & Evans, N. Functional echocardiography: an emerging clinical tool for the neonatologist. J. Pediatr. 150, 125–130 (2007).
Mohsen, A. A. & Amin, A. Risk factors and outcomes of persistent pulmonary hypertension of the newborn in neonatal intensive care unit of al-minya University Hospital in Egypt. J. Clin. Neonatol. 2, 78–82 (2013).
Verma, B., Daga, S. R. & Mahapankar, A. Persistent pulmonary hypertension among neonates with sepsis. Indian J. Pediatr. 73, 250–251 (2006).
Dempsey, E. & Rabe, H. The use of cardiotonic drugs in neonates. Clin. Perinatol. 46, 273–290 (2019).
Sehgal, A., Athikarisamy, S. E. & Adamopoulos, M. Global myocardial function is compromised in infants with pulmonary hypertension. Acta Paediatr. 101, 410–413 (2012).
Moore, T. D. et al. Ventricular interaction and external constraint account for decreased stroke work during volume loading in CHF. Am. J. Physiol. Heart Circ. Physiol. 281, H2385–H2391 (2001).
Chagnon, F., Bentourkia, M., Lecomte, R., Lessard, M. & Lesur, O. Endotoxin-induced heart dysfunction in rats: assessment of myocardial perfusion and permeability and the role of fluid resuscitation*. Crit. Care Med. 34, 127–133 (2006).
Galiuto, L., Ignone, G. & DeMaria, A. N. Contraction and relaxation velocities of the normal left ventricle using pulsed-wave tissue Doppler echocardiography. Am. J. Cardiol. 81, 609–614 (1998).
Nagueh, S. F., Middleton, K. J., Kopelen, H. A., Zoghbi, W. A. & Quiñones, M. A. Doppler tissue imaging: a noninvasive technique for evaluation of left ventricular relaxation and estimation of filling pressures. J. Am. Collage Cardiol. 30, 1527–1533 (1997).
Haileselassie, B. et al. Strain echocardiography parameters correlate with disease severity in children and infants with sepsis. Pediatr. Crit. Care Med. 17, 383–390 (2016).
Rivers, E. et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N. Engl. J. Med. 345, 1368–1377 (2001).
Nguyen, H. B. et al. Early goal-directed therapy in severe sepsis and septic shock: insights and comparisons to ProCESS, ProMISe, and ARISE. Crit. Care 20, 160 (2016).
Menon, K. et al. Criteria for pediatric sepsis-a systematic review and meta-analysis by the pediatric sepsis definition taskforce. Crit. Care Med. 50, 21–36 (2022).
Sullivan, B. A., Kausch, S. L. & Fairchild, K. D. Artificial and human intelligence for early identification of neonatal sepsis. Pediatr. Res. 93, 350–356 (2023).
Sahu, P. et al. Prediction modelling in the early detection of neonatal sepsis. World J. Pediatr. 18, 160–175 (2022).
Acknowledgements
This work was supported by the Italian Ministry of Health with “Current Research funds”.
Author information
Authors and Affiliations
Contributions
F.P. and C.A. contributed to the study conception and design. Material preparation, data collection, and analysis were performed by F.P. and D.U.D.R. The first draft of the manuscript was written by F.P. and revised by D.U.D.R. N.P., F.K., M.P.R., A.D., P.B., and C.A. critically revised it for important intellectual content. All authors reviewed and approved the final version of the article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pugnaloni, F., De Rose, D.U., Kipfmueller, F. et al. Assessment of hemodynamic dysfunction in septic newborns by functional echocardiography: a systematic review. Pediatr Res 95, 1422–1431 (2024). https://doi.org/10.1038/s41390-024-03045-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-024-03045-2
- Springer Nature America, Inc.