Abstract
Background
Obesity paradox addressing all-cause mortality has been described in several chronic total occlusion (CTO) studies. However, the impact of aging on long-term cardiac events in patients with overweight and obesity with CTO recanalization were less studied.
Methods
A total of 458 patients (64.4 ± 11.3 years, 403 male) with CTO interventions were enrolled. The overweight/obesity group included 311 patients with body mass index (BMI) ≧24 kg/m2 and the non-obesity group included 147. With a median follow-up of 40.0 (17.9–61.4) months, 422 patients with successful true-lumen recanalization were further assessed for target lesion failure [TLF: cardiac death, target vessel myocardial infarction (TVMI), target lesion revascularization (TLR)].
Results
At follow-up, the rates of cardiac death, TVMI, TLR, TLF, and stent thrombosis were 1.9%, 1.9%, 9.2%, 10.7%, and 0.5%, respectively. The TVMI-free survival was borderline better (p = 0.067 by log-rank test) in overweight/obesity than non-obesity group. Among patients <65 years of age, the TVMI-free survival was significantly better in the overweight/obesity group (p = 0.013 compared to non-obesity group by log-rank test). In multivariate Cox regression model, the non-obesity patients younger than 65 years were at a higher risk of TVMI, not only among those <65 years of age (hazard ratio = 11.0, 95% CI = 1.1–106.0) but also among the whole patients (hazard ratio=6.9, 95% CI = 1.4–35.1) with successful CTO recanalization.
Conclusions
For those with true-lumen recanalized CTO, the higher risk of TVMI after successful recanalization was rather evident in patients <65 years of age and without overweight/obesity, suggesting that aging might attenuate prognostic significance of “obesity paradox” for CTO interventions.
Similar content being viewed by others
Introduction
Among the coronary lesion subsets, chronic total occlusion (CTO) remains the most challenging category for percutaneous coronary intervention (PCI) even in the era with much more advances of recanalization devices, techniques [1, 2], and strategies [3,4,5]. The presence of overweight and obesity is accompanied by an increased metabolic burden that could later translate into poorer prognosis due to higher incidences or more severe degree of coronary artery disease or congestive heart failure (CHF) [6, 7]. In the literature, however, most studies evaluating long-term prognosis of CTO-PCI demonstrated a lower rate of all-cause mortality in patients with overweight and obesity, regardless of procedural success [8,9,10]. “Obesity paradox” has been therefore suggested to be present for the outcome of CTO-PCI. On the other hand, a higher incidence of long-term all-cause mortality, cardiac mortality, or cardiac events after PCI or CTO-PCI has been demonstrated in the patients with aging, which was considered to be related to more frailty and comorbidities in this population [11, 12]. Based on the studies of several Asian PCI registries investigating the prognostic impact of body mass index (BMI), nevertheless, an unique trend toward an increasing age with a lowering BMI has been universally shown [13, 14]. Thus the complex relationship between aging and obesity with respect to cardiac outcomes in patients with successful CTO recanalization remained unclear.
Additionally, concerns about the extent of subintima creation should be paid for studying long-term cardiac events after CTO-PCI due to more and more use of “dissection and reentry” devices or techniques during recanalization procedures. Since the severity of subintima was difficult to quantify, the impact of subintimal stenting on outcome studies of CTO-PCI [15, 16] could be uncertain and the results should be cautiously interpretated. In the current study, our CTO-PCI team, as a member of the Taiwan True-Lumen Tracking (TTLT) club [17], aimed to analyze the impact of aging on long-term cardiac events in patients with and without overweight/obesity undergoing CTO-PCI with wiring-based true-lumen recanalization techniques.
Methods
Study Design and Population
According to the definition of Health Promotion Administration, Ministry of Health and Welfare In Taiwan, the criteria for ‘overweight’ and ‘obesity’ states are estimated by the body mass index (BMI), with overweight being ≧24 kg/m2 and obesity ≧27 kg/m2 (https://www.hpa.gov.tw/Pages/List.aspx?nodeid=1757). The TTLT club is initiated by seven high-volume CTO operators from seven independent medical centers in north Taiwan. The concept of true-lumen tracking is to minimize false lumen creation and stenting as much as possible. The criteria of successful “true-lumen tracking” was arbitrarily defined as no loss of antegrade flow for any side-branch ≧1.5 mm of size throughout the entire CTO body including 5 mm before and after the occluded segment on final quantitative coronary angiography (QCA) [17]. The cohort included 458 consecutive patients (64.4 ± 11.3 years, 403 men) with CTO who underwent consecutive coronary interventions in National Taiwan University Hospital between Aug 2014 and March 2022. The overweight/obesity group included 311 patients with a BMI ≧24 kg/m2, and non-obesity group included 147 patients with a BMI < 24 kg/m2. After the interventions, 422 patients with successful true-lumen recanalization were further assessed for target lesion failure (TLF) including cardiac death, target vessel myocardial infarction (MI), and percutaneous or surgical target lesion revascularization (TLR) in the long-term. Chronic kidney disease (CKD) was defined as the estimated glomerular filtration rate (eGFR) < 60 ml/min/1.73m2. CHF was defined as the presence of heart failure signs/symptoms fulfilling the Framingham criteria and left ventricular ejection fraction <50% before the index procedure. The study was conducted according to the Declaration of Helsinki, and was approved by the institutional ethic committee of National Taiwan University Hospital (approval number: 201904023RINC), and the written informed consents were obtained.
Procedures
The definition of multivessel disease was the presence of stenoses ≥50% by QCA in at least two major epicardial coronary arteries. Coronary CTO was defined as the lesions with thrombolysis in MI grade 0 flow for at least 3 months [18, 19]. The J-CTO score was the consensus of two independent operators (Dr. SC Liu and Dr. CL Lee). For CTO procedures, according to the fundamentals of TTLT club, wiring-based antegrade techniques for true-lumen tracking and crossing were attempted first and with effort, regardless of the overall J-CTO score or its individual characteristic. (Fig. 1) The retrograde approach was only used in 38 patients (8%), and the mean time for switching antegrade to retrograde procedures was 71 ± 32 min. When retrograde techniques were necessary during the procedures, true-lumen tracking and direct crossing with a soft (tip load ≦1 gram) retrograde guidewire was the first priority. If not feasible, the retrograde guidewire as the distal landmark for the antegrade guidewire kissing technique was tried. The reverse controlled antegrade and retrograde techniques (CART) and knuckle wire method were considered as the bail-out strategies, but both were not considered as successful true-lumen tracking. During the whole procedure, choices of the guidewires, timing of the parallel wire or retrograde techniques, use of intravascular imaging at any time point were mainly the discretion of the operator. Re-entry devices were not used based on the concept of true-lumen tracking. Besides the criteria of true-lumen recanalization, success of CTO PCI was defined as restoration of thrombolysis in MI grade 3 anterograde flow and postprocedural stenosis <30% during final assessment of angiography. No occurrence of in-hospital major adverse cardiac and/or cerebro-vascular events or any repeat TLR was also necessary for the definition of procedural success. For patients with multi-vessel disease, complete revascularization should be done at the index procedure or within 6 months.
Thirty-eight cases required retrograde techniques back-up. An overall of 33 patients had procedural failure including 23 with pure antegrade wiring failure and 10 with failed hybrid techniques. Among the 425 patients with successful interventions, 2 with reverse CART and one with knuckle wire techniques were excluded for long-term follow-up because of evident subintimal stenting. CTO chronic total occlusion, CART controlled antegrade and retrograde tracking, GW guidewire.
All patients with successful procedures were required to take adequate antiplatelets following the current guidelines.
Follow-up
The 422 patients with successful true-lumen recanalization were further analyzed for long-term cardiac events including target lesion failure (TLF: cardiac death, target vessel MI, and clinically-driven TLR), and stent thrombosis according to the Academic Research Consortium definitions [20]. TLR was any occurrence of restenosis with diameter stenosis ≥50% from 5 mm distal to 5 mm proximal to the occluded segment. All data were collected by regular hospital visit or telephone if necessary. When cardiac related symptoms recurred with/without positive stress tests or restenosis documented by coronary computed tomography angiography, follow-up catheterization was performed.
Statistical analysis
Continuous variables were expressed by mean ± standard deviation, and categorical variables were presented as percentage. The unadjusted comparison in univariate analysis was examined using Wilcoxon rank-sum test, chi-square test, and Fisher’s exact test as appropriate for the data type. Among the 422 patients with successful true-lumen recanalization, event-free survival for the time from the index procedure to follow-up was estimated by the Kaplan-Meier method. Patients lost to follow-up were right-censored at the last follow-up dates. The effect of risk factors on time to cardiac events estimated by the hazard ratio (HR) and 95% CI was analyzed by a multivariate Cox proportional hazards model. For multivariate analyses, factors with p values < 0.10 in univariate analyses were included. All analyses were performed using the IBM SPSS version 25 software package (IBM corp.).
Results
Clinical Features
As shown in Table 1, patients with overweight/obesity were younger than those without [62.4 ± 10.7 versus (vs.) 68.7 ± 11.4 years, p < 0.001], and had a higher percentage of hyperlipidemia (79 vs. 63%, p < 0.001) and smoking (39 vs. 29%, p = 0.031). The incidence of CKD with an eGFR <60 ml/min/1.73m2 was lower in the overweight/obesity group than in the non-obesity group (23 vs. 34%, p = 0.011).
Angiographic and procedural characteristics
Among 458 patients, 412 patients (90%) had multivessel disease. (Table 2) The target vessel of CTO was similar between the groups. All transfemoral access for intervention was borderline less done in the overweight/obesity compared with the non-obesity group (14 vs. 21%, p = 0.076). Although the overall J-CTO score was comparable between the groups (2.3 ± 1.4 vs. 2.3 ± 1.3, p = 0.577), there was less presence of calcification (50 vs. 61%, p = 0.031) and more retry attempts (16 vs. 8%, p = 0.017) in the overweight/obesity than in the non-obesity group. The reference air kerma was much higher in the overweight/obesity than in the non-obesity group (6.8 ± 5.1 vs. 4.1 ± 2.8 gray, p < 0.001), and the retrograde approach for recanalization was borderline more necessary in the overweight/obesity than in the non-obesity group (10 vs. 5%, p = 0.06). With a similar total stent length implanted, the mean stent size was larger in the overweight/obesity than in the non-obesity group (2.8 ± 0.4 vs. 2.7 ± 0.3 mm, p = 0.011). However, the success rate (93 vs. 93%), fluoroscopy time, and total procedure time were not statistically different between the groups.
Long-term cardiac outcomes and the prognostic impact of aging on patients with overweight/obesity versus those without
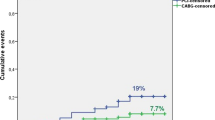
Over a median follow-up of 40.0 (17.9–61.4) months, the long-term cardiac events of all patients (N = 422, Fig. 1), patients with (N = 287) and without (N = 135) overweight/obesity with successful CTO recanalization by true-lumen tracking techniques were shown in Fig. 2. The overall rates of cardiac death, TVMI, TLR, TLF, and stent thrombosis were 1.9%, 1.9%, 9.2%, 10.7%, and 0.5%, respectively. Bothe rates of TLR and TLF were comparable (p > 0.5) between the overweight/obesity and non-obesity group. The Kaplan-Meier curve showed that target vessel MI-free survival was borderline better (p = 0.067 by log-rank test) in the overweight/obesity than in the non-obesity group.
We further tested the effect of aging on outcome analyses. We found that the prognostic impact of overweight/obesity was more pronounced in patients <65 years of age than those with aging (≧65 years of age) (Fig. 3a). Among patients <65 years of age, the target vessel MI-free survival was much better in the overweight/obesity than in the non-obesity group (p = 0.013 by log-rank test). Among the patients ≧65 years of age, the long-term target vessel MI-free survival was similar between the overweight/obesity and non-obesity groups (p = 0.758 by log-rank test). When comparing patients ≧65 years of age with (p = 0.009 by log-rank test) or without (p = 0.036 by log-rank test) overweight/obesity, those <65 years of age and without overweight/obesity still had a worse target vessel MI-free survival after CTO recanalization. The much worse target vessel MI-free survival remained significant when comparing patients <65 years of age and without overweight/obesity to the others (p = 0.001 by log-rank test, Fig. 3b).
Panel (a) showed comparisons of long-term target vessel myocardial infarction-free survival of the patients with and without overweight/obesity stratified by age (65 years). Panel (b) compared long-term target vessel myocardial infarction-free survival between the non-obesity and non-elderly (<65 years) and other patients. BMI body mass index.
In the multivariate Cox proportional hazards model after adjusting potential factors including sex, total stent length, J-CTO score, and intrastent CTO, patients <65 years of age and without overweight/obesity were at a higher risk of target vessel MI than those with overweight/obesity and <65 years of age after successful true-lumen recanalization (HR = 11.0, 95% CI = 1.1–106.0). Even among all patients, those <65 years of age and without overweight/obesity were also rather risky to develop target vessel MI comparing with the others (HR = 6.9, 95% CI = 1.4–35.1) in the long-term.
Discussion
For patients with successful true-lumen recanalized CTO, we showed a higher risk of long-term target vessel MI in patients younger than 65 years of age and without overweight/obesity than their counterparts in the current study. Since the occurrence of MI would lead to a higher rate of mortality in the short- and long-term, this could at least partly contribute to the higher all-cause-mortality as “obesity paradox” in patients without overweight/obesity with CTO-PCI [8,9,10]. However, the higher risk of target vessel MI in patients without overweight/obesity was not seen in the population with aging, suggesting that the impact of aging could possibly attenuate the significance of “obesity paradox” with respect to long-term cardiac events in patients with CTO recanalization.
Several procedural features of CTO-PCI in patients with overweight/obesity were shown in univariate analyses in the present study. For example, when concerning the risk of puncture site complications, both femoral arteries as the access sites are less used in the overweight/obesity group even the retrograde approach was more frequently required. In the OPEN-CTO study [21] with the femoral artery as the main (> 90%) access site in the overweight and obesity groups, the rate of overall access site complications was approximately 5%. To minimize such complication, the use of a slender sheath for a larger guiding catheter made radial arteries as the feasible access for CTO recanalization. We also demonstrated that patients with overweight/obesity with CTO recanalization by true-lumen crossing techniques had a significantly higher radiation dosage than those without overweight/obesity even though the fluoroscopy time was comparable between the two groups. Stähli et al. and Patterson et al. reported a significant difference in procedural radiation between patients with overweight/obesity and normal weight with CTO interventions [8, 21]. Among all CTO-PCI techniques, theoretically, the antegrade and wiring-based true-lumen tracking procedures were thought to be more time-consuming and possibly led to higher radiation exposure. The impact of such kind of technique-related radiation on patients with overweight/obesity must be much more magnified. Due to the risk of developing procedure-related fluoroscopy-induced radiation dermatitis (reference air kerma >7 gray) [22], switching earlier to retrograde approach or devices for “dissection and reentry” to reduce the procedure time and decrease the radiation exposure for patients with overweight/obesity could be recommended according to current CTO-PCI algorithms [3,4,5].
Regarding the evaluation of cardiac outcomes after successful CTO-PCI, whether subintimal stenting would be associated with worse prognosis was still not definitely answered because the impact of subintimal stenting was difficult to quantify. In clinical practice, more complex CTO lesions usually required more use of retrograde techniques or reentry devices [23, 24]. Therefore, longer subintimal stenting would be expected. Fin et al. showed that the presence of subintima tracking clarified by intravascular ultra-sound was correlated with a high J-CTO score, and a higher unadjusted rate of one-year TLF was found in patients with subintima tracking when compared to that with intraplaque tracking [15]. Another study also demonstrated that 4-year TLF increased with the use of the retrograde approach, mostly due to re-occlusion or TLR [16]. Conversely, the recently published CONventional Antegrade vs. Sub-Intimal Synergy sTENTing in Chronic Total Occlusions (CONSISTENT CTO) trial [25] compared clinical outcomes of 109 patients with dissection and reentry techniques plus subintimal stenting to 101 patients with conventional intimal techniques. The study suggested that medium-term major adverse cardiovascular events (MACE) were not adversely affected by use of dissection and reentry techniques with subintimal stenting. However, there seemed to be a trend toward a higher 24-month incidence of MACE in the group with subintimal stenting, when compared to true-lumen stenting (20.8% vs. 13.8%, p = 0.177). To minimize the prognostic effect of subintimal creation and stenting, the current study included only those with successful true-lumen recanalized CTO for long-term follow-up. No significant difference in either TLR or TLF between the overweight/obesity and non-obesity group was seen herein. This finding suggested that the mechanism underlying all-cause mortality as “obesity paradox” demonstrated in prior studies [8,9,10] could be mainly related to the overall risk profile of patients with established coronary artery disease [26], not restricted to the recanalized CTO lesion itself.
Since the presence of overweight/obesity or aging was fundamentally associated with increased burden of coronary atherosclerosis with possibly more cardiac events, the study conversely disclosed a much higher incidence of target vessel MI after true-lumen recanalization for CTO in patients without overweight/obesity, particularly in those < 65 years of age (none-obesity: 8 vs. overweight/obesity: 1%). Besides the significant difference in BMI (22.6 ± 1.0 vs. 28.4 ± 3.2, p < 0.001) between the non-obesity and overweight/obesity group in patients <65 years of age in univariate analysis, the presence of CKD (non-obesity: 29 vs. overweight/obesity: 12%, p = 0.004) could be another causative link of more target vessel MI in patients without overweight/obesity. The relationship between MI and CKD has been reported to be associated with increased oxidative stress, inflammation, endothelial dysfunction, and a disturbed hemostasis towards a prothrombotic state [27,28,29]. Furthermore, although the presence of calcification within the occluded segment was similar between patients with and without overweight/obesity (overweight/obesity: 44 vs. none-obesity: 39%, p = 0.485) among subjects without aging, the highly prevalent overall coronary artery calcification in patients without overweight/obesity but with CKD was still possible and could be related to the higher risk of target vessel MI [30].
Additionally, when comparing to patients with overweight/obesity and ≧65 years of age (Fig. 3a), patients <65 years of age and without overweight/obesity still had a higher risk of target vessel MI after CTO recanalization. Since age has been known to be independently associated with a poorer cardiac prognosis after CTO-PCI [8,9,10] or PCI [11, 12], the worse outcome of patients <65 years of age and without overweight/obesity in the present study further suggested the prognostic impact of “obesity paradox” in patients with CTO recanalization. When all patients with successfully true-lumen recanalized CTO were included, the incidence of target vessel MI remained higher in patients <65 years of age and without overweight/obesity than in others (8% vs. 1%). Besides the lower BMI (non-obesity <65 years of age: 22.6 ± 1.0 vs. the others: 26.6 ± 3.8, p < 0.001), however, the presence of CKD between patients <65 years of age in the non-obesity group and the other patients was no longer different (non-obesity and <65 years of age: 29 vs. the others: 27%, p = 0.826). Moreover, patients <65 years of age and without overweight/obesity had several favorable cardiovascular prognostic features including lower rates of multivessel disease (80 vs. 91%, p = 0.009), hypertension (65 vs. 78%, p = 0.043), hyperlipidemia (61 vs. 75%, p = 0.035), and younger age (58 ± 9 vs. 65 ± 11 years, p < 0.001) than the other patients. Even though several mechanisms have been proposed [31, 32], the causes about the pathophysiology underlying the relationship between overweight/obesity and lower all-cause survival remained mostly speculative [8, 9]. When investigating cardiac events, we demonstrated that patients with a BMI < 24 kg/m2 and age younger than 65 years were independently associated with a significantly higher risk of target vessel MI in the long-term, not only in those < 65 years of age but also in all patients with successfully recanalized CTO. Therefore, beyond the traditional risk factors of MI, future research is warranted to elucidate the crucial link of non-overweight/obesity and a higher rate of target vessel MI in patients <65 years of age with CTO recanalization. Based on the evident correlation between the occurrence of MI and a higher risk of follow-up mortality, this finding could at least partly contribute to the higher all-cause mortality as the “obesity paradox” in patients with CTO interventions.
On the other hand, among patients ≧65 years of age with recanalized CTO, the higher risk of target vessel MI in the non-obesity than overweight/obesity group as that in those <65 years of age was not demonstrated further. For patients without overweight/obesity, the target vessel MI-free survival was even shown to be significantly better in patients with aging than those <65 years of age. Similarly, if taking the adverse aging effect upon the cardiac events after CTO-PCI into consideration, these findings suggested that aging process with its underlying characteristics could play a key role in attenuating the prognostic significance of “obesity paradox” in patients ≧65 years of age.
Study limitations
There were several limitations of the study. First, physical activity and cardiorespiratory fitness have been reported to significantly modify the effect of obesity on long-term mortality or obesity paradox for patients with coronary heart disease [33,34,35]. However, the current study was derived from an interventional registry of CTO recanalization, and the data regarding physical activity were not well recorded and collected. Among the 422 patients with successfully true-lumen recanalized CTO, only 64 patients (15%) had undergone treadmill exercise test after complete revascularization, and a minority of them (15 patients, 15/64 = 23%) were classified as the aging (≧65 years of age) group. Therefore, we did not analyze the cardiorespiratory fitness further due to the limited and potentially biased data. Additionally, the outcome evaluation of the study was mainly focused on target lesion failure after CTO revascularization. Since 90% of patients have multivessel disease in the present study, the prognostic impact of physical activity/cardiorespiratory fitness on the target occluded lesion or single vessel remains less clear and deserves further investigation. Second, the cut-off value of BMI ≧24 kg/m2 for overweight and obesity was following the definition of the study country, which were slightly lower than the commonly used definition (≧25 kg/m2). However, the mean BMI value as 28.0 ± 3.1 kg/m2 of the overweight/obesity group in the study still could be comparable to the majority of patients with overweight/obesity with the worldwide criteria. Third, intravascular imaging was used in 45% of all patients. The judgment of true lumen tracking and crossing was partly based on the operator’s experiences, and therefore, could not be completely confirmed. One study suggested the discordance between presumed and IVUS-confirmed true lumen was 15.8% [25]. In clinical practice, however, it’s nearly impossible for successful wiring if a large and long false lumen was created during the wiring procedure of CTO-PCI. Additionally, successful sizable side-branch preservation defined as true-lumen recanalization herein could further ensure, if any, a limited subintima space created within the CTO segment. Therefore, the rather strict criteria of technical success could decrease the potential discrepancy. Fourth, because of the limited case number, we did not further classify patients with a BMI ≧24 kg/m2 into overweight, obesity, and even severe obesity groups. Whether a U-shaped association between BMI and target vessel MI would exist, as that described between the BMI and survival in patients with severe obesity who have acute coronary syndrome and stable coronary artery disease [36, 37], cannot be answered in the study. Nevertheless, there were too few patients with severe obesity (3.5% of the overweight/obesity group) to compromise the result significantly. Similarly, patients who were ≧ 80 years of age were not further stratified and analyzed due to the limited number of patients (overall 57 patients, 12%). Since extreme aging itself was accompanied by a higher rate of mortality, the outcomes might change if more octogenarians were included. However, the age distribution of the patients in the current study could be comparable to the real-world data because the study was derived from a consecutive registry. Fifth, all CTO interventions were performed by the same true-lumen tracking strategy. Whether the study result can be applied to those with multiple strategies or recanalization techniques is unknown. However, the same strategy would minimize the potential impact of diverse techniques on the outcome evaluation.
Conclusion
In patients with wiring-based true-lumen recanalized CTO, a much higher risk of long-term target vessel MI was rather evident in the non-obesity and non-aging group. However, the higher risk of patients without overweight/obesity was not seen in the population with aging, suggesting that the prognostic impact of “obesity paradox” could be attenuated by the effect of aging.
Data availability
The data will be available upon reasonable request to the corresponding author.
References
Tajti P, Karmpaliotis D, Alaswad K, Jaffer FA, Yeh RW, Patel M, et al. The hybrid approach to chronic total occlusion percutaneous coronary intervention: update from the PROGRESS CTO Registry. J Am Coll Cardiol Interv. 2018;11:1325–35.
Wilson WM, Walsh SJ, Yan AT, Hanratty CG, Bagnall AJ, Egred M, et al. Hybrid approach improves success of chronic total occlusion angioplasty. Heart. 2016;102:1486–93.
Brilakis ES, Grantham JA, Rinfret S, Wyman RM, Burke MN, Karmpaliotis D, et al. A percutaneous treatment algorithm for crossing coronary chronic total occlusions. J Am Coll Cardiol Inter. 2012;5:367–79.
Harding SA, Wu EB, Lo S, Lim ST, Ge L, Chen JY, et al. A new algorithm for crossing chronic total occlusions from the Asia Pacific Chronic Total Occlusion Club. J Am Coll Cardiol Inter. 2017;10:2135–43.
Galassi AR, Werner GS, Boukhris M, Azzalini L, Mashayekhi K, Carlino M, et al. Percutaneous recanalisation of chronic total occlusions: 2019 consensus document from the EuroCTO Club. Eurointervention. 2019;15:198–208.
Eckel RH. Obesity and heart disease: a statement for healthcare professionals from the Nutrition Committee, American heart Association. Circulation. 1997;96:3248–50.
Kenchaiah S, Evans JC, Levy D, Wilson PW, Benjamin EJ, Larson MG, et al. Obesity and the risk of heart failure. N Engl J Med. 2002;347:305–13.
Stähli BE, Gebhard C, Gick M, Herman C, Ferenc M, Mashayekhi K, et al. Impact of body mass index on long-term mortality in women and men undergoing percutaneous coronary intervention for chronic total occlusion. Int J Cardiol. 2016;224:305–9.
Won KB, Yoon HJ, Lee SG, Cho YK, Nam CW, Hur SH, et al. Comparison of long-term mortality according to obesity in patients with successful percutaneous chronic total occlusion interventions using drug-eluting stents. Catheter Cardiovasc Inter. 2018;91:710–6.
Tsai CT, Huang WC, Lu YW, Teng HI, Huang SS, Tsai YL, et al. Obesity paradox in patients with chronic total occlusion of coronary artery. Eur J Clin Invest. 2022;52:e13698.
Lin NH, Ho JS, Djohan AH, Ho VW, Teo YN, Teo YH, et al. Percutaneous coronary intervention in patients aged 80 years old and above: a systematic review and meta-analysis. AsiaIntervention. 2022;8:123–31.
Lateef N, Ahsan MJ, Fazeel HM, Haseeb A, Latif A, Kousa O, et al. Percutaneous coronary intervention for chronic total occlusion in patients aged <75 years versus ≥75 years: a systematic review. Community Hosp Intern Med Perspect. 2020;10:25–31.
Qu Y, Yang J, Zhang F, Li C, Dai Y, Yang H, et al. Relationship between body mass index and outcomes of coronary artery disease in Asian population: Insight from the FOCUS registry. Int J Cardiol. 2020;300:262–7.
Endo H, Dohi T, Shitara J, Wada H, Doi S, Naito R, et al. Impact of body mass index on long-term outcomes in Japanese patients following percutaneous coronary intervention: The Juntendo PCI Registry. J Cardiol. 2018;72:208–14.
Finn MT, Doshi D, Cleman J, Song L, Maehara A, Hatem R, et al. Intravascular ultrasound analysis of intraplaque versus subintimal tracking in percutaneous intervention for coronary chronic total occlusions: one-year outcomes. Catheter Cardiovasc Inter. 2019;93:1048–56.
Kwon O, Lee PH, Lee SW, Lee JY, Kang DY, Ahn JM, et al. Retrograde approach for the percutaneous recanalisation of coronary chronic total occlusions: contribution to clinical practice and long-term outcomes. Eurointervention. 2019;15:e354–61.
Chang CJ, Liu SC, Tsai CT, Cheng JF, Lee CL, Lin CP, et al. Impacts of lesion characteristics on procedures and outcomes of chronic total occlusion recanalization with antegrade guidewire true lumen tracking techniques: a substudy of Taiwan True Lumen Tracking registry. Front Cardiovasc Med. 2022;9:769073.
Galassi A, Tomasello S, Reifart N, Werner GS, Sianos G, Bonnier H, et al. In-hospital outcomes of percutaneous coronary intervention in patients with chronic total occlusion: insights from the ERCTO (European Registry of Chronic Total Occlusion) registry. Eurointervention. 2011;7:472–9.
Olivari Z, Rubartelli P, Piscione F, Ettori F, Fontanelli A, Salemme L, et al. Immediate results and one-year clinical outcome after percutaneous coronary interventions in chronic total occlusions: data from a multicenter, prospective, observational study (TOAST-GISE). J Am Coll Cardiol. 2003;41:1672–8.
Cutlip DE, Windecker S, Mehran R, Boam A, Cohen DJ, van Es GA, et al. Clinical end points in coronary stent trials: a case for standardized definitions. Circulation. 2007;115:2344–51.
Patterson C, Sapontis J, Nicholson WJ, Lombardi W, Karmpaliotis D, Moses J, et al. Impact of body mass index on outcome and health status after chronic total occlusion percutaneous coronary intervention: Insights from the OPEN-CTO study. Catheter Cardiovasc Inter. 2021;97:1186–93.
Ramirez M, Ravichandran S, Ronald L, Pabon-Ramos WM, Smith TP, Kim CY, et al. Recognition and management of dermatologic complications from interventional radiology procedures. Diagn Inter Imaging. 2019;100:659–70.
Syrseloudis D, Secco GG, Barrero EA, Lindsay AC, Ghione M, Kilickesmez K, et al. Increase in J-CTO lesion complexity score explains the disparity between recanalisation success and evolution of chronic total occlusion strategies: insights from a single-centre 10-year experience. Heart. 2013;99:474–9.
Nombela-Franco L, Urena M, Jerez-Valero M, Nguyen CM, Ribeiro HB, Bataille Y, et al. Validation of the J-Chronic Total Occlusion score for chronic total occlusion percutaneous coronary intervention in an independent contemporary cohort. Circ Cardiovasc Inter. 2013;6:635–43.
Walsh SJ, Hanratty CG, McEntegart M, Strange JW, Rigger J, Henriksen PA, et al. Intravascular healing is not affected by approaches in contemporary CTO PCI: the CONSISTENT CTO study. JACC Cardiovasc Interv 2020;13:1448–57.
Romero-Corral A, Montori VM, Somers VK, Korinek J, Thomas RJ, Allison TG, et al. Association of bodyweight with total mortality and with cardiovascular events in coronary artery disease: a systematic review of cohort studies. Lancet. 2006;368:666–78.
Stenvinkel P, Carrero JJ, Axelsson J, Lindholm B, Heimburger O, Massy Z. Emerging biomarkers for evaluating cardiovascular risk in the chronic kidney disease patient: how do new pieces fit into the uremic puzzle? Clin J Am Soc Nephrol. 2008;3:505–21.
Zewinger S, Schumann T, Fliser D, Speer T. Innate immunity in CKD associated vascular diseases. Nephrol Dial Transpl. 2016;31:1813–21.
Mortberg J, Blomback M, Wallen A, He S, Jacobson SH, Spaak J. Increased fibrin formation and impaired fibrinolytic capacity in severe chronic kidney disease. Blood Coagul Fibrinolysis. 2016;27:401–7.
Chen J, Budoff MJ, Reilly MP, Yang W, Rosas SE, Rahman M, et al. Coronary artery calcification and risk of cardiovascular disease and death among patients with chronic kidney disease. JAMA Cardiol. 2017;2:635–43.
Salie R, Huisamen B, Lochner A. High carbohydrate and high fat diets protect the heart against ischaemia/reperfusion injury. Cardiovasc Diabetol. 2014;13:109.
Bastien M, Poirier P, Lemieux I, Després JP. Overview of epidemiology and contribution of obesity to cardiovascular disease. Prog Cardiovasc Dis. 2014;56:369–81.
McAuley PA, Artero EG, Sui X, Lee DC, Church TS, Lavie CJ, et al. The obesity paradox, cardiorespiratory fitness, and coronary heart disease. Mayo Clin Proc. 2012;87:443–51.
Moholdt T, Lavie CJ, Nauman J. Interaction of physical activity and body mass index on mortality in coronary heart disease: Data from the Nord-Trøndelag Health Study. Am J Med. 2017;130:949–57.
Moholdt T, Lavie CJ, Nauman J. Sustained physical activity, not weight loss, associated with improved survival in coronary heart disease. J Am Coll Cardiol. 2018;71:1094–101.
Angeras O, Albertsson P, Karason K, Råmunddal T, Matejka G, James S, et al. Evidence for obesity paradox in patients with acute coronary syndromes: a report from the Swedish Coronary Angiography and Angioplasty Registry. Eur Heart J. 2013;34:345–53.
Steinberg BA, Cannon CP, Hernandez AF, Pan W, Peterson ED, Fonarow GC. Medical therapies and invasive treatments for coronary artery disease by body mass: the “obesity paradox” in the Get With The Guidelines database. Am J Cardiol. 2007;100:1331–5.
Acknowledgements
The study was partly sponsored by the grant from the Taiwan Health Foundation, Taipei, Taiwan.
Author information
Authors and Affiliations
Contributions
J-JH, J-FC, C-LL, J-YC, and Y-CW contributed to the whole interventions and long-term care of these patients. Y-CW, S-CL, C-HH, J-TL, C-JC, C-TT, C-TT, and J-JH contributed to the study conception and design, analysis and interpretation of the data, the drafting of the paper, revising it critically for intellectual content, and the final approval of the version. All authors agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Cheng, JF., Lee, CL., Chiang, JY. et al. Impact of aging on long-term cardiac outcomes of true-lumen recanalized chronic total occlusions in patients with overweight/obesity. Int J Obes (2024). https://doi.org/10.1038/s41366-024-01623-2
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41366-024-01623-2
- Springer Nature Limited