Abstract
Background
There is uncertainty regarding the best revascularization approach—whether coronary artery bypass grafting (CABG) or percutaneous coronary intervention (PCI)—for obese patients suffering from multi-vessel coronary artery disease.
Results
406 patients with low and intermediate SYNTAX scores (SS) underwent PCI with drug-eluting stents (n = 200, 100 with SS ≤ 22, and 100 with SS 23–32) and CABG (n = 206, 100 with SS ≤ 22, and 106 with SS 23–32). Patients were also categorized by body mass index (BMI): normal weight (12%, 48 patients), overweight (41.6%, 169 patients), and obese (46.6%, 189 patients). The follow-up period averaged 9 ± 1.9 years. The endpoints of the study were as follows: major adverse cardiac and cerebrovascular events, a repeat revascularization, diminished left ventricular ejection fraction (LVEF), and high SS (≥ 33) observed over time. When comparing PCI and CABG in overweight individuals, the risk of myocardial infarction (MI) following PCI was greater than after CABG (Hazard Ratio [HR] 2.7, 95% Confidence Interval [CI] 1.1–6.7, p = 0.03). In patients with overweight and Class I obesity, CABG was associated with the risk of coronary atherosclerosis progression (SS ≥ 33) (HR 4.4, 95% CI 1.5–13, p = 0.009 and HR 4.9, 95% CI 1.9–12, p = 0.001, respectively); whereas PCI was connected with the likelihood of repeat revascularization (HR 2.7, 95% CI 1.6–4.55, p < 0.0001 and HR 2, 95% CI 1.3–3.1, p = 0.002, respectively). At the same time, for stented patients, Class III obesity was associated with the risk of repeat revascularization (HR 2.5, 95% CI 1.02–6, p = 0.044).
Conclusion
There were no significant weight-related impacts on long-term outcomes among patients who underwent surgery. Whereas in stented patients, Class III obesity was associated with the risk of repeat revascularization. When comparing PCI and CABG, for overweight and Class I obesity patients, CABG was associated with a likelihood of coronary atherosclerosis progression (SS ≥ 33), while PCI was linked to the risk of repeat revascularization. For overweight patients, CABG outperformed PCI in terms of the risk of MI. For other adverse events in patients of different weight categories, PCI and CABG did not reveal any significant benefits.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Despite the decline in mortality from cardiovascular diseases (CVD) over the past decades, coronary artery disease (CAD) continues to be the primary cause of death globally [1, 2]. Obesity is a strong independent and mediated risk factor for CVD [3, 4] and is also closely associated with coronary atherosclerosis [5, 6]. At the same time, the incidence of obesity has surged to epidemic levels [7]. In this setting, healthcare providers are encountering an increasing number of individuals receiving treatment with distinct clinical characteristics and facing challenges in medical, interventional, and surgical treatments. Historically, studies have shown that coronary artery bypass grafting (CABG) generally surpasses percutaneous coronary intervention (PCI) in various metrics, including survival rates, for patients with multivessel CAD [8,9,10]. It would be logical to assume that surgical treatment of CAD is beneficial for obese patients. Nonetheless, the advent of advanced drug-eluting stents (DES) has brought into question the applicability of earlier findings to present-day practices. Recent large-scale studies have shown minimal differences in outcomes between PCI and CABG [11,12,13]. Also, when choosing a strategy, it is necessary to take into account the anthropometric characteristics of this cohort of patients, the high invasiveness of CABG, in comparison with PCI. At the same time, data on the impact of obesity on the success of PCI and CABG are becoming obsolete [14,15,16], current studies are presented to a greater extent for interventional revascularization than for surgery [17,18,19,20,21]. Therefore, this study's examination of the extended results of PCI using DES compared to CABG in obese patients with multivessel CAD is both pertinent and necessary.
Methods
Study design and patients
This investigation was designed as a longitudinal, retrospective clinical cohort two-central study and was described earlier [22]. Briefly, according to archival data from two hospitals, we identified 406 patients who had stable multivessel CAD exhibiting low to intermediate coronary atherosclerotic damage as per the SYNTAX score (SS) (< 33 points) (https://syntaxscore2020.com) [23, 24]. The selected patients underwent initial PCI with DES (200 patients, 100 with SS ≤ 22, and 100 with SS 23–32) and initial CABG (206 patients, 100 with SS ≤ 22, and 106 with SS 23–32) between 2010 and 2013. SS assessments were not primarily utilized but were subsequently applied to archival angiograms in a retrospective manner. Exclusion criteria included previous stenting or cardiac surgery, single-vessel coronary disease, left main disease, an SS ≥ 33, an acute coronary syndrome with an ST elevation, age over 65, left ventricular aneurysm, severe valvular dysfunction combined with CAD, a left ventricular ejection fraction (LVEF) below 40%, rheumatic or congenital heart defects, and severe chronic renal failure (i.e., a glomerular filtration rate [GFR] < 30 ml/min/1.73 m2 using the Cockcroft-Gault equation). Patients were tracked using the data of clinical electronic databases of centers, data from national electronic polyclinic and inpatient registers (https://pvd.dmed.kz, www.eisz.kz), and up-to-date contact information. The average follow-up spanned 9 ± 1.9 years; with the longest follow-up being 12 years.
Moreover, participants in the study were stratified by weight gradations according to their body mass index (BMI), determined by dividing weight in kilograms by height in meters squared (kg/m2). These categories were classified into normal (BMI = 18.5–24.9), overweight (BMI = 25–29.9), and obese (BMI ≥ 30) as per World Health Organization definitions. Further, obesity was subclassified into Class I (BMI = 30–34.9), Class II (BMI = 35–39.9), and Class III (BMI ≥ 40) [25, 26].
Following the Helsinki Declaration's principles, the study was approved by the ethics committees of the participating centers.
Study endpoints
The clinical outcomes targeted in this study included a combined measure of major adverse cardiac and cerebrovascular events (MACCE) and their individual elements: all-cause mortality, cardiac death, cerebrovascular accidents (CVA), which encompass transient ischemic attacks (TIA) and strokes, myocardial infarction (MI); repeated revascularization, and the development of chronic heart failure (CHF). CHF was assessed in accordance with clinical evaluations, measurement of LVEF; and examination for dilatation of the heart chambers with valvular dysfunction. Additionally, high-grade coronary artery lesions, characterized by a SYNTAX score of ≥ 33 observed over time, were also monitored. Deaths were classified as cardiovascular unless a definitive non-cardiovascular cause could be confirmed.
Statistical analysis
Groups were stratified and evaluated by weight category. The analysis of continuous variables was performed using either univariate analysis of variance (ANOVA) or the Kruskal–Wallis test, contingent upon how the data was distributed. The Chi-square test or the Kendall-Stewart test was used to compare categorical variables, which were expressed as proportions and figures. Evaluation of distant events during the observation period was executed via the Kaplan–Meier method with the log-rank test. The hazard ratio (HR) with a 95% confidence interval (CI) was estimated based on Cox proportional regression. This multivariate analysis aimed to determine whether BMI serves as an independent predictor of adverse outcomes. Relevant covariates included in the Cox model were age, BMI, waist circumference, gender, weight categories, arterial hypertension, diabetes mellitus (DM), previous CVA, atherogenic index, smoking status, previous MI, chronic obstructive pulmonary disease (COPD), type of revascularization (PCI/CABG), persistent/permanent atrial fibrillation (AF), initial LVEF, peripheral vascular disease, Charlson comorbidity index (CCI) (https://www.mdcalc.com/calc/3917/charlson-comorbidity-index-cciprimary) [27, 28], initial SS. The diagnostic significance of BMI was assessed using receiver-operating characteristic (ROC) curves. All calculations were executed using SPSS Statistics software 23.0 (IBM Corporation, Armonk, New York, USA), and the value of p < 0.05 was considered statistically significant.
Results
Baseline characteristics
Our study analyzed 406 patients, categorized based on BMI levels into (1) normal weight (11.8%, n = 48), (2) overweight (41.6%, n = 169), and (3) obese (46.6%, n = 189). There were no patients with a BMI less than 18.5 kg/m2 in our study. The initial characteristics are presented in Table 1. Women (n = 70/17.2%) were more likely to be obese patients (64.3%) than normal (10%) and overweight ones (25.7%) (p = 0.04). On the other hand, overweight (44.9%) and obese (42.9%) male patients outnumbered those who were normal weight (12.2%), at p = 0.04, among men (n = 336/82.8%). The atherogenic index (AI) applied in this study is derived by applying the formula: (total cholesterol minus high-density lipoproteins) divided by high-density lipoproteins. AI was higher in the overweight (3.8 [2.8–4.7]) and obese (3.7 [2.7–5]) groups, compared with patients with normal weight (3.2 [1.8–4]), at p = 0.013. DM and high-grade arterial hypertension (AH) were more prevalent in obese patients than in normal or overweight ones (p < 0.0001 for both indicators). Concerning other initial characteristics, patients with different weight categories did not differ.
Outcomes
Clinical outcomes based on weight gradations are presented in Tables 2 and 3. By employing the weight gradation, overweight patients had a lower risk of cardiac death compared to obese patients (8.3% vs. 15.9%, HR 0.5, CI 0.2–0.96, p = 0.037, respectively). On average, SS were in dynamics, which were higher in patients with obesity and overweight, compared with patients with normal weight (25 [17–33.5], 23 [11.3–32.5], and 16.3 [7.3–26.4], p = 0.026, respectively). When analyzing outcomes among obesity groups (I, II, and III Classes), obese Class I patients had a lower risk of requiring repeated revascularization (HR 0.5, 95% CI 0.25–0.97, p = 0.04), cardiac death (HR 0.32, 95% CI 0.12–0.88, p = 0.028) and MI (HR 0.29, 95% CI 0.11–0.74, p = 0.01), in relation to obese Class III patients. For other events, the groups with different classes of obesity did not have significant differences.
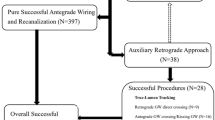
There were no differences between the revascularization outcomes for the normal weight group based on the strategy (Table 4). For overweight patients, the probability of MI development after PCI was higher than after CABG (19% vs. 7.7%, HR 2.7, 95% CI 1.1–6.7, p = 0.03) (Fig. 1). Both overweight and obese patients showed a higher risk of repeated revascularization following PCI as opposed to CABG (59% vs. 23%, HR 2.7, 95% CI 1.6–4.55, p < 0.001; and 67% vs. 33.7%, HR 1.99, 95% CI 1.3–3.1, p = 0.002, respectively); the likelihood of a high degree of coronary artery lesion (SS ≥ 33) after PCI was less than after CABG (9.8% vs. 44.4%, HR 0.23, 95% CI 0.08—0.7, p = 0.009 and 12.8% vs. 49%, HR 0.28, 95% CI 0.14–0.57, p = 0.001, respectively) (Table 4).
Further analysis within obesity classes showed that first-class obesity patients had a higher risk of needing repeated revascularization following PCI as opposed to CABG (74.6% vs. 32.2%, HR 1.93, 95% CI 1.1–3.3, p = 0.02). At the same time, the probability of progression of atherosclerotic lesions of the coronary arteries (SS ≥ 33) after PCI was less than after CABG (11.5% vs. 51.3%, HR 0.2, 95% CI 0.08–0.5, p = 0.001). For patients with second and third classes of obesity, we found no differences in revascularization outcomes depending on the strategy (Table 5).
The development of adverse events was performed using univariate and multivariate Cox regression to find independent predictors. The following indicators were utilized as predictors: gender, age, smoking, type of revascularization (CABG/PCI), BMI, previous CVA, peripheral atherosclerotic vascular disease, hypertension, AF, weight gradations (normal, overweight, and obesity), DM, classes of obesity, initial LVEF, waist circumference, COPD, atherogenic index, previous MI, and initial SS. Consequently, for all revascularized patients BMI was linked to the risk of all-cause mortality (HR 1.05, 95% CI 1.002–1.11, p = 0.04), and cardiac death (HR 1.1, 95% CI 1.02–1.15, p = 0.01). Class III obesity (BMI ≥ 40), compared to normal weight (BMI = 18.5–24.9), was associated with the risk of CHF with reduced LVEF (HR 3.2, 95% CI 1.1–9.3, p = 0.03), and repeated revascularization (HR 2.9, 95% CI 1.4–6.5, p = 0.06). It should be noted that in a multivariate analysis conducted separately for the PCI and CABG groups, Obesity Class III among stented patients was associated with an increased risk of repeat revascularization (HR 2.5, 95% CI 1.02–6, p = 0.044). Additionally, for surgically treated patients, a BMI exceeding 29 kg/m2 was associated with a risk of developing CHF with reduced LVEF (HR 1.06, 95% CI 1.01–1.12, p = 0.015). Yet, BMI did not significantly impact other study endpoints (Table 6).
A Receiver Operating Characteristic (ROC) analysis was performed for evaluating the diagnostic significance, sensitivity, and specificity of BMI. The area under the ROC curve (AUC) demonstrated that BMI had fail predictive capability for all-cause mortality (AUC 0.57, 95% CI 0.49–0.65, p = 0.05). The AUC of the ability of BMI to predict cardiac death reached 0.61 (95% CI 0.52–0.7, p = 0.01), demonstrating poor model quality. Also for patients, who underwent surgery, the AUC of the ability of BMI to predict the development of CHF with reduced LVEF was 0.64 (95% CI 0.55–0.73, p = 0.002), indicating a poor model quality too (Fig. 2).
ROC curves for BMI. Receiver-operating characteristic (ROC) curves for (A) All-cause-Death; (B) Cardiac death; and (C) CHF with reduced LVEF based on the BMI are shown. (A), (B): Overall population; (C): CABG cohort. AUC = Area under curve; BMI = body mass index; CABG = coronary artery bypass grafting; CHF = chronic heart failure; CI = confidence interval; LVEF = left ventricular ejection fraction
Discussion
The body's excessive or abnormal fat or adipose tissue accumulation, referred to as obesity, deteriorates health [26]. The tool used to assess obesity is a BMI ≥ 30 kg/m2 [25, 26]. BMI assessment has limitations due to its inability to describe the relative contribution of adipose tissue, muscle mass, and bone mass [29, 30]. Other indicators of central obesity involve waist-to-hip ratio, waist-to-height ratio, and waist circumference [26, 31]. Due to the retrospective nature of our study, we initially had data only on BMI and waist circumference. Accordingly, we were able to assess changes only in these measurements over time. Other assessments of obesity were not applied in our observation. The measure of waist circumference in our analysis did not show a significant impact on revascularization outcomes.
Obesity is the most important factor in the development of CAD [3, 4]. In the context of the global obesity epidemic, multivessel disease (MVD) is reasonably represented among patients with CAD [7, 32]. Thus, in general, the prevalence of MVD ranges from 30 to 40% of patients with CAD, and among patients with acute coronary syndrome MVD occurs in about 50% of patients [32, 33]. Despite advances in PCI, CABG offers more comprehensive revascularization for more compound multivessel coronary artery disease [34]. It should be noted that surgery is still more invasive treatment method than PCI and it is associated with more pronounced technical difficulties, wound complications and postoperative respiratory problems in this cohort of patients [35]. To objectively compare the outcomes of PCI and CABG, we excluded patients with severe coronary lesions who had clear indications for surgery. Only patients with low and intermediate coronary lesions (SYNTAX score < 33), who were eligible for both PCI and CABG, were included in the analysis. Taking into account the growth of the overweight and obese population, the selection of the optimal revascularization method for this group of patients, and determining the influence of weight categories on the results of PCI and CABG, are of clinical interest and debate.
Despite the existence of a proven causal relationship between morbid obesity and increased cardiovascular morbidity [3, 4], researchers have observed the "obesity paradox," noting that obesity can have a protective effect on postoperative complications and mortality in patients undergoing surgery or interventional treatments [14, 16,17,18, 21]. Even so, some researchers have critically evaluated the "obesity paradox" due to the presence of a selection bias in observations, exclusion of early death cases from long-term studies, lack of proper consideration of unintentional weight loss due to a high level of comorbidity, younger patients with obesity, short-term observation period, insufficient consideration of distorting factors, and association of smoking with lower body weight [30, 36, 37]. In our study, obesity did not express "protective" properties by the main MACCE. Previous long-term studies comparing PCI and CABG outcomes have shown the superiority of surgery in MACCE [8,9,10]. In our study, for overweight patients, CABG also demonstrated superiority over PCI in terms of the risk of developing MI. According to other adverse events, the strategies did not show advantages across all weight categories.
In many other observations, PCI is associated with the likelihood of repeated revascularization [8, 9, 11]. In our study, PCI was also associated with the risk of repeated revascularization among overweight and Class I obese patients (HR 2.7, 95% CI 1.6–4.55, p < 0.0001 and HR 1.9, 95% CI 1.1–3.3, p = 0.017, respectively). In other weight categories, the association between PCI and repeated revascularization was also observed but without statistical significance (Tables 4, 5). It is noteworthy that Obesity Class 3 in stented patients was associated with an increased risk of repeat revascularization, consistent with findings from previous studies [38].
In our observation, for individuals with overweight and Class I obesity, CABG was associated with the risk of coronary atherosclerosis progression (SS > 32) [HR 4.4, 95% CI 1.5–13, p = 0.009 and HR 4.9, 95% CI 1.9–12, p = 0.001, correspondingly]. In other weight categories, high-grade coronary artery lesions (SS > 32) also developed more frequently after CABG than after PCI, but the data were not statistically significant (Tables 4,5). This can likely be attributed to the propensity of grafts, particularly vein grafts, to undergo remodeling, atherosclerosis, and progressive intimal hyperplasia, leading to occlusion or graft stenosis [39, 40]. Graft patency is a critical factor influencing long-term survival and clinical prognosis following CABG [40, 41]. The use of the saphenous vein graft (SVG) is widespread and accounts for more than 80% of CABG cases worldwide [40, 42]. SVG in CABG are characterized by a high incidence of early atherosclerosis, intimal hyperplasia, and thrombosis, resulting in graft failure in 12–20% of cases within a year [40, 43] and 50–60% within a decade [40, 44]. Meanwhile, advances in interventional treatment achieve success in reducing in-stent restenosis. Previous studies indicate that bare-metal stents (BMS) lowered the incidence of restenosis comparing balloon angioplasty from 30–60% to 15–40%, and DES further reduced this rate by up to 15% [45].
Thus, through careful preoperative planning, advanced surgical and interventional techniques, and improved postoperative care, healthcare providers can optimize treatment outcomes for obese patients undergoing coronary revascularization. A detailed understanding of the impact of obesity on PCI and CABG and a personalized approach to patient management can enhance the success of procedures and long-term survival. Addressing specific issues related to different weight categories remains a crucial component of optimizing care for patients undergoing coronary revascularization.
Study limitations
Our results of the study should be considered with the following limitations in mind.
Firstly, the modest sample size may limit the statistical power of this analysis.
Secondly, despite implementing various measures and corrections, the retrospective observational nature of the study introduces the potential for systematic selection bias.
Thirdly, the study's cohort consisted of stable multivessel CAD patients, without left main disease, who had low and intermediate SS and received primary PCI or CABG prior to age 65. As a result, these outcomes are not applicable to other CAD populations.
Fourthly, it is important to note that patients underwent PCI with DES and surgical procedures corresponding to the guidelines from 2010–2013. Thus, our findings may not be fully applicable to modern treatment technologies. Long-term observations, while valuable, are inevitably based on somewhat outdated technologies.
Conclusions
Thus, there were no significant weight-related impacts on long-term outcomes among patients who underwent surgery. Whereas in stented patients, Class III obesity was associated with the risk of repeat revascularization. When comparing PCI and CABG, for overweight and Class I obesity patients, CABG was associated with a likelihood of coronary atherosclerosis progression (SS ≥ 33), while PCI was linked to the risk of repeat revascularization. For overweight patients, CABG outperformed PCI in terms of the risk of MI. For other adverse events in patients of different weight categories, PCI and CABG did not reveal any significant benefits.
Availability of data and materials
Data confirming the results of this study are stored in the databases of the National Research Cardiac Surgery Center (Astana), Pavlodar Regional Cardiology Center, and the national polyclinic and inpatient registers of the Kazakhstan Republican e-Health Center. This data is not publicly available. Nonetheless, acceptable information can be provided by the authors upon reasonable request and with the permission of the directors of these centers.
Abbreviations
- AI:
-
Atherogenic index
- AH:
-
Arterial hypertension
- AF:
-
Atrial fibrillation
- AUC:
-
Area under curve
- BMI:
-
Body mass index
- CAD:
-
Coronary artery disease
- CABG:
-
Coronary artery bypass grafting
- CHF:
-
Chronic heart failure
- CI:
-
Confidence interval
- CCI:
-
Charlson comorbidity index
- CVD:
-
Cardiovascular diseases
- CVA:
-
Cerebrovascular accident
- DES:
-
Drug-eluting stent
- Dg:
-
Degree
- GFR:
-
Glomerular filtration rate
- HR:
-
Hazard ratio
- LVEF:
-
Left ventricular ejection fraction
- MACCE:
-
Major adverse cardiac and cerebrovascular events
- MI:
-
Myocardial infarction
- MVD:
-
Multivessel disease
- PCI:
-
Percutaneous coronary intervention
- RCT:
-
Randomized clinical trials
- ROC:
-
Receiver operating characteristics
- SS:
-
SYNTAX score
- SVG:
-
Saphenous vein graft
- TIA:
-
Transient ischemic attack
References
World Health Organization (11.06.2021) Cardiovascular diseases (CVDs). Fact sheets. Available via DIALOG. https://www.who.int/en/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds). Accessed 15 Jun 2024.
GBD (2021) Causes of Death Collaborators (2024) Global burden of 288 causes of death and life expectancy decomposition in 204 countries and territories and 811 subnational locations, 1990–2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet 403(10440):2100–2132. https://doi.org/10.1016/S0140-6736(24)00367-2
Wilson PW, D’Agostino RB, Sullivan L, Parise H, Kannel WB (2002) Overweight and obesity as determinants of cardiovascular risk: The Framingham experience. Arch Intern Med 162:1867–1872. https://doi.org/10.1001/archinte.162.16.1867
Katta N, Loethen T, Lavie CJ, Alpert MA (2020) Obesity and coronary heart disease: epidemiology, pathology, and coronary artery imaging. Curr Probl Cardiol 46(3):100655. https://doi.org/10.1016/j.cpcardiol.2020.100655
Csige I, Ujvárosy D, Szabó Z, Lőrincz I, Paragh G, Harangi M, Somodi S (2018) The impact of obesity on the cardiovascular system. J Diabetes Res. https://doi.org/10.1155/2018/3407306
Henning RJ (2021) Obesity and obesity-induced inflammatory disease contribute to atherosclerosis: a review of the pathophysiology and treatment of obesity. Am J Cardiovasc Dis 11(4):504–529
World Health Organization (2024) Obesity and overweight. Fact sheets. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight Accessed 15 Jun 2024.
Park SJ, Ahn JM, Kim YH, Park DW, Yun SC, Trial LJYBEST, Investigators, et al (2015) Trial of everolimus-eluting stents or bypass surgery for coronary disease. N Engl J Med 372(13):1204–1212. https://doi.org/10.1056/NEJMoa1415447
Thuijs DJFM, Kappetein AP, Serruys PW, Mohr FW, Morice MC, Mack MJSYNTAX, Investigators ES et al (2019) Percutaneous coronary intervention versus coronary artery bypass grafting in patients with three-vessel or left main coronary artery disease: 10-year follow-up of the multicentre randomised controlled SYNTAX trial. Lancet 394(10206):1325–1334. https://doi.org/10.1016/S0140-6736(19)31997-X
Chew NWS, Koh JH, Ng CH, Tan DJH, Yong JN, Lin C et al (2022) Coronary artery bypass grafting versus percutaneous coronary intervention for multivessel coronary artery disease: a one-stage meta-analysis. Front Cardiovasc Med 9:822228. https://doi.org/10.3389/fcvm.2022.822228
Shaik TA, Chaudhari SS, Haider T, Rukia R, Al Barznji S, Kataria H et al (2022) Comparative effectiveness of coronary artery bypass graft surgery and percutaneous coronary intervention for patients with coronary artery disease: a meta-analysis of randomized clinical trials. Cureus 14(9):e29505. https://doi.org/10.7759/cureus.29505
Biancari F, Gudbjartsson T, Heikkinen J, Anttila V, Mäkikallio T, Jeppsson A et al (2014) Comparison of 30-day and 5-year outcomes of percutaneous coronary intervention versus coronary artery bypass grafting in patients aged≤50 years (the coronary artery disease in young adults study). Am J Cardiol 114(2):198–205. https://doi.org/10.1016/j.amjcard.2014.04.025
Ahn JM, Kang DY, Yun SC, Ho Hur S, Park HJ, Tresukosol D et al. BEST Extended Follow-Up Study Investigators (2022) Everolimus-eluting stents or bypass surgery for multivessel coronary artery disease: extended follow-up outcomes of multicenter randomized controlled BEST trial. Circulation. 146(21):1581–1590. https://doi.org/10.1161/CIRCULATIONAHA.122.062188
Hastie CE, Padmanabhan S, Slack R, Pell AC, Oldroyd KG, Flapan AD et al (2010) Obesity paradox in a cohort of 4880 consecutive patients undergoing percutaneous coronary intervention. Eur Heart J 31(2):222–226. https://doi.org/10.1093/eurheartj/ehp317
Akin I, Tölg R, Hochadel M, Bergmann MW, Khattab AA, Schneider S et al. DES.DE (German Drug-Eluting Stent) Study Group (2012) No evidence of "obesity paradox" after treatment with drug-eluting stents in a routine clinical practice: results from the prospective multicenter German DES.DE (German Drug-Eluting Stent) registry. JACC Cardiovasc Interv 5(2):162–9. https://doi.org/10.1016/j.jcin.2011.09.021
Sharma A, Vallakati A, Einstein AJ, Lavie CJ, Arbab-Zadeh A, Lopez-Jimenez F et al (2014) Relationship of body mass index with total mortality, cardiovascular mortality, and myocardial infarction after coronary revascularization: evidence from a meta-analysis. Mayo Clin Proc 89(8):1080–1100. https://doi.org/10.1016/j.mayocp.2014.04.020
Won KB, Shin ES, Kang J, Yang HM, Park KW, Han KR et al (2023) Body mass index and major adverse events during chronic antiplatelet monotherapy after percutaneous coronary intervention with drug-eluting stents - results from the HOST-EXAM trial. Circ J 87(2):268–276. https://doi.org/10.1253/circj.CJ-22-0344
Mei X, Hu S, Mi L, Zhou Y, Chen T (2021) Body mass index and all-cause mortality in patients with percutaneous coronary intervention: A dose-response meta-analysis of obesity paradox. Obes Rev 22(2):e13107. https://doi.org/10.1111/obr.13107
Wolny R, Maehara A, Liu Y, Zhang Z, Mintz GS, Redfors B et al (2020) The obesity paradox revisited: body mass index and -long-term outcomes after PCI from a large pooled patient-level database. EuroIntervention 15(13):1199–1208. https://doi.org/10.4244/EIJ-D-19-00467
Zhang K, Wang J, Yang Y, An R (2019) Adiposity in relation to readmission and all-cause mortality following coronary artery bypass grafting: A systematic review and meta-analysis. Obes Rev 20(8):1159–1183. https://doi.org/10.1111/obr.12855
Fan Y, Liu J, Jin L, Liu Z, Han L, Wang Y et al (2022) Impacts of metabolic disorders on short- and long-term mortality after coronary artery surgery in the elderly. BMC Cardiovasc Disord 22(1):504. https://doi.org/10.1186/s12872-022-02954-6
Madiyeva MI, Aripov MA, Pya YV, Goncharov AY, Shakirova GN (2023) Long-term results of myocardial revascularization in patients with multivessel disease. Bratisl Lek Listy 124(3):212–220. https://doi.org/10.4149/BLL_2023_034
Sianos G, Morel MA, Kappetein AP, Morice MC, Colombo A, Dawkins K et al (2005) The SYNTAX Score: an angiographic tool grading the complexity of coronary artery disease. EuroIntervention 1(2):219–227
Farooq V, van Klaveren D, Steyerberg EW, Meliga E, Vergouwe Y, Chieffo A et al (2013) Anatomical and clinical characteristics to guide decision making between coronary artery bypass surgery and percutaneous coronary intervention for individual patients: development and validation of SYNTAX score II. Lancet 381(9867):639–650. https://doi.org/10.1016/S0140-6736(13)60108-7
World Health Organization (1995) Physical status: the use and interpretation of anthropometry. Report of a WHO Expert Committee. World Health Organ Tech Rep Ser 854:1–452
Panuganti KK, Nguyen M, Kshirsagar RK (2023) Obesity. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK459357/ Accessed 15 Jun 2024.
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40(5):373–383. https://doi.org/10.1016/0021-9681(87)90171-8
Charlson M, Szatrowski TP, Peterson J, Gold J (1994) Validation of a combined comorbidity index. J Clin Epidemiol 47(11):1245–1251. https://doi.org/10.1016/0895-4356(94)90129-5
Pray R, Riskin S (2023) The history and faults of the body mass index and where to look next: a literature review. Cureus 15(11):e48230. https://doi.org/10.7759/cureus.48230
Donini LM, Pinto A, Giusti AM, Lenzi A, Poggiogalle E (2020) Obesity or BMI paradox? Beneath the tip of the iceberg. Front Nutr 7:53. https://doi.org/10.3389/fnut.2020.00053
World Health Organization (2008) Waist circumference and waist-hip ratio: report of a WHO expert consultation. https://www.who.int/publications/i/item/9789241501491 Accessed 15 Jun 2024
Akbari T, Al-Lamee R (2022) Percutaneous coronary intervention in multi-vessel disease. Cardiovasc Revasc Med 44:80–91. https://doi.org/10.1016/j.carrev.2022.06.254
Faro DC, Laudani C, Agnello FG, Ammirabile N, Finocchiaro S, Legnazzi M et al (2023) Complete percutaneous coronary revascularization in acute coronary syndromes with multivessel coronary disease: a systematic review. JACC Cardiovasc Interv 16(19):2347–2364. https://doi.org/10.1016/j.jcin.2023.07.043
Gu D, Qu J, Zhang H, Zheng Z (2020) Revascularization for coronary artery disease: principle and challenges. Adv Exp Med Biol 1177:75–100. https://doi.org/10.1007/978-981-15-2517-9_3
Bachar BJ, Manna B (2023) Coronary artery bypass graft. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK507836/ Accessed 15 Jun 2024.
Flegal KM, Ioannidis JPA (2018) The obesity paradox: a misleading term that should be abandoned. Obesity (Silver Spring) 26(4):629–630. https://doi.org/10.1002/oby.22140
Tobias DK, Hu FB (2013) Does being overweight really reduce mortality? Obesity (Silver Spring) 21(9):1746–1749. https://doi.org/10.1002/oby.20602
Wang ZJ, Gao F, Cheng WJ, Yang Q, Zhou YJ (2015) Body mass index and repeat revascularization after percutaneous coronary intervention: a meta-analysis. Can J Cardiol 31(6):800–808. https://doi.org/10.1016/j.cjca.2015.01.031
Caliskan E, de Souza DR, Böning A, Liakopoulos OJ, Choi YH, Pepper J et al (2019) Saphenous vein grafts in contemporary coronary artery bypass graft surgery. Nat Rev Cardiol 17(3):155–169. https://doi.org/10.1038/s41569-019-0249-3
Ferrari G, Geijer H, Cao Y, Souza D, Samano N (2021) Percutaneous coronary intervention in saphenous vein grafts after coronary artery bypass grafting: a systematic review and meta-analysis. Scand Cardiovasc J 55(4):245–253. https://doi.org/10.1080/14017431.2021.1900598
Fitzgibbon GM, Kafka HP, Leach AJ, Keon WJ, Hooper GD, Burton JR (1996) Coronary bypass graft fate and patient outcome: angiographic follow-up of 5,065 grafts related to survival and reoperation in 1,388 patients during 25 years. J Am Coll Cardiol 28(3):616–626. https://doi.org/10.1016/0735-1097(96)00206-9
Schwann TA, Tatoulis J, Puskas J, Bonnell M, Taggart D, Kurlansky P et al (2017) Worldwide trends in multi-arterial coronary artery bypass grafting surgery 2004–2014: a tale of 2 continents. Semin Thorac Cardiovasc Surg 29(3):273–280. https://doi.org/10.1053/j.semtcvs.2017.05.018
Motwani JG, Topol EJ (1998) Aortocoronary saphenous vein graft disease: pathogenesis, predisposition, and prevention. Circulation 97(9):916–931. https://doi.org/10.1161/01.cir.97.9.916
Goldman S, Zadina K, Moritz T, Ovitt T, Sethi G, Copeland JG et al.; VA Cooperative Study Group #207/297/364 (2004) Long-term patency of saphenous vein and left internal mammary artery grafts after coronary artery bypass surgery: results from a Department of Veterans Affairs Cooperative Study. J Am Coll Cardiol. 44(11):2149–56. https://doi.org/10.1016/j.jacc.2004.08.064
Spadaccio C, Antoniades C, Nenna A, Chung C, Will R, Chello M et al (2020) Preventing treatment failures in coronary artery disease: what can we learn from the biology of in-stent restenosis, vein graft failure, and internal thoracic arteries? Cardiovasc Res 116(3):505–519. https://doi.org/10.1093/cvr/cvz214
Funding
The authors received no funding to conduct this research or to assist in the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
MMI and AMA have contributed to the study concept and design development, preparation of material, data collection, and analysis. GAY and ZhRY participated in data collection and statistical analysis. The initial draft version of the manuscript was written by MMI, and the other coauthors then made their suggestions and changes to the text of the manuscript. The final version of the manuscript was read and approved by all authors, who agreed to take full responsibility for all aspects of the work related to the accuracy and integrity of any portion of it.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Our retrospective cohort study was conducted in accordance with the principles of the Declaration of Helsinki, and approval for this study was obtained from the Local Ethical Commission of NJSC “Semey Medical University” (minutes no. 2, dated October, 28 2020) and the Committees of the participating centers. Consent to participate is not required due to the retrospective nature of the study that reveals no identifiable private information.
Consent for publication
Not applicable.
Competing interests
All of the authors confirm that they are not affiliated with or involved in any organization with an interest in the material reported in this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Madiyeva, M.I., Aripov, M.A., Goncharov, A.Y. et al. Outcomes of myocardial revascularization in patients with obesity and multivessel coronary artery disease. Egypt Heart J 76, 114 (2024). https://doi.org/10.1186/s43044-024-00548-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43044-024-00548-5