Abstract
The purpose of this review is to report on the perioperative uses of intravenous (IV) ketamine based on literature from the last five years (2018–2022). We searched MEDLINE, Embase and PubMed databases from 1st January 2018 till 15th September 2022. We primarily reviewed randomized control trials and systematic reviews with or without meta-analyses where IV ketamine was used as part of an anesthetic regimen perioperatively for general or regional anesthesia. We included studies with both pediatric and/or adult participants. We did not examine the quality of the randomized controlled trials (RCTs) included in our review. Perioperative IV ketamine consistently reduced postoperative opioid requirement especially in the early postoperative period, however, the duration of this effect was variable in different surgeries and patient populations. This effect was seen in breast, obstetric, bariatric, and orthopedic surgeries. The effect was minimal in pediatric and thoracic surgeries. It has a valuable role in multi-modal analgesic regimen, especially in orthopedic and spine procedures. Considerable heterogeneity was noted with regards to the dosage of IV ketamine. Bolus doses ranged from 0.15 to 1 mg·kg−1 and infusion doses ranged from 2 to 5 ug·kg−1·min−1. Its role in prevention of chronic post-surgical pain is still under investigation. Intravenous ketamine also reduced postoperative depressive symptoms in specific patient populations. It also reduced shivering associated with spinal anesthesia. It has a potential role in prevention of emergence agitation and postoperative delirium. In conclusion, IV ketamine has a versatile range of beneficial clinical effects in perioperative practice. The most widely studied are its analgesic effects which are of variable intensity amongst different surgical specialties and subset of patients. Despite its long history of use, fresh uses of IV ketamine continue to be reported. More trials are needed to better understand ideal dosing and patient subsets that will benefit most from these effects.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
The origin of ketamine dates back to the middle of the twentieth century when lesser psychomimetic analogs of phenyl cyclohexyl piperidone were being developed [1]. It was approved for use as a general anesthetic in 1970 by the Food and Drug Administration in the USA.
With the shift towards multi-modal analgesia to promote enhanced recovery and the occurrence of opioid crisis there has been a renewed interest in ketamine's analgesic potential in both acute and chronic pain management. Its clinical applications have now expanded beyond anesthesia into chronic pain management and neuropsychiatry. Its use in sub-anesthetic doses has also been evaluated for neuro-cognitive and mood outcomes and for treatment of complications such as postoperative shivering [2,3,4,5]. This review highlights evidence from recent literature (2018–2022) on the clinical applications of intravenous (IV) ketamine during the perioperative period.
1.1 Site and mode of action
Ketamine is a non-competitive and high-affinity inhibitor of N-Methyl-D-aspartate (NMDA) receptors. NMDA is a glutamate receptor with key excitatory synaptic transmission in the central nervous system (CNS). Glutamate plays an important role in pain pathways of opioid-induced hyperalgesia and central sensitization and NMDA receptors are involved in the development of opioid tolerance. Ketamine exerts its anti-nociceptive action by antagonism of NMDA receptors not only at the level of the cortex but also at the spinal cord [6]. There is additional evidence that it also interacts with α-Amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA), opioid, cholinergic, and hyperpolarization-activated cyclic nucleotide-gated (HCN) receptors [7].
Molecularly ketamine has two enantiomers R and S ketamine which both have high CNS permeability. S-ketamine has a stronger binding to NMDA receptor, however, in clinical practice and research the racemic mixture is more commonly used [6]. In the present review "ketamine" refers to the racemic mixture (R-ketamine) and "S-ketamine" is written as such, where it is used.
2 Objective
The objective of this review is to report on the current role of perioperative IV ketamine over the last five years (2018–2022).
3 Review methodology
3.1 Search methods
We searched MEDLINE, Embase, and PubMed databases from 1st January 2018 till 15th September 2022. Keywords for conducting the literature search are given below.
((ketamine [MeSH Terms]) OR (ketamine) OR (ketamine hydrochloride)) AND ((period, perioperative [MeSH Terms]) OR (perioperative period) OR (perioperative care) OR (perioperative medicine) OR (perioperative pain management) OR (preoperative care)) OR (preoperative period) OR (preoperative pain management)OR (intraoperative period) OR (intraoperative care) OR (intraoperative pain management) OR (postoperative period) OR (postoperative care) OR (postoperative pain management) OR (pain management)) Filters: from 2018–2022.
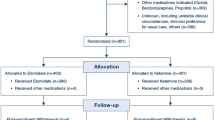
3.2 Selection criteria
We sought randomized controlled trials (RCTs) where IV ketamine was used as part of an anesthetic regimen perioperatively during general or regional anesthesia. IV Ketamine was either compared to a placebo or another drug/technique, either in a bolus dose or infusion or both. RCTs with both adults and children were included. The search was restricted to only English language abstracts. Systematic reviews analyzing RCTs using perioperative IV ketamine were also included.
3.3 Exclusion criteria
We excluded studies where ketamine was given by any other route apart from intravenous or when ketamine was mixed with another medication, e.g., added to local anesthetics or sedative agents. Narrative reviews, editorials, and case series were not considered. RCTs in which ketamine was administered in a nonsurgical setting, were also excluded.
3.4 Data collection
Two authors (Khan Z., Khan F.A.) reviewed all titles and agreed on a list of articles. The third author (Hameed M.) settled any disparity. The abstracts of these articles were then consulted for review. Full articles were accessed for further details. We did not examine the quality of the included RCTs.
4 Results
4.1 Use of perioperative IV ketamine for intra and post-operative analgesia
Analgesic properties of perioperative ketamine have been studied in a variety of surgical populations discussed below.
4.1.1 Anesthesia for breast surgery
Intraoperative ketamine has shown promising results in patients undergoing breast surgery. In a systematic review, Bi et al. investigated the effects of IV ketamine on acute and chronic wound pain in patients undergoing breast surgery. Intravenous ketamine reduced wound pain in the first six hours and decreased opioid requirement for 24 h post-operatively compared to a placebo. In addition perioperative use of ketamine reduced the incidence of post-mastectomy pain syndrome at one, three and six months post-surgery. There was diversity among studies in the mode of administration of ketamine. In five of the studies IV ketamine was administered as an infusion, three studies gave a 0.5 mg·kg−1 bolus before the start of infusion. In one study infusion was continued for 24 h and in another daily infusions were administered for seven days. There were no systematic adverse effects observed [8].
4.1.2 Obstetric anesthesia
A meta-analysis of 20 RCTs evaluated the clinical efficacy of IV ketamine in reducing postoperative pain after anesthesia for Cesarean section (C-section). Patients who received ketamine had lower pain scores, consumed fewer opioid analgesics, and required a longer time interval to the first dose of analgesia postoperatively [9]. Another RCT reported that intravenous ketamine at a dose of 0.25 mg·kg−1 given between neuraxial block and surgical incision in non-elective C-sections decreased opioid requirement till 24 h postoperatively [10].
4.1.3 Anesthesia for bariatric surgery
A number of studies have assessed the use of IV ketamine in bariatric surgeries including abdominoplasty [11], sleeve gastrectomy [12], and laparoscopic gastric bypass [13].
An RCT conducted by Mehta et al. included 54 participants undergoing gastric bypass surgery and observed that ketamine reduced the requirement for postoperative narcotic analgesic in the first 24 h. Intravenous ketamine was administered as a 20 mg bolus followed by an infusion of 5 μg·kg−1·min−1 until the start of wound closure [13].
A meta-analysis of seven RCTs, which included the aforementioned trial, concluded that intravenous ketamine did decrease opioid consumption in the first 24 h after surgery but this was only significant in trials that administered ketamine as a bolus. This review also noted decreased visual analog score up until eight hours after surgery and decreased length of postoperative hospital stay in patients who received ketamine. The risk of post‐operative nausea and vomiting, hallucinations, euphoria, and dizziness was not significantly different amongst the groups [14].
Ketamine as an analgesic adjunct is of particular importance in morbidly obese patients as many of them suffer from obstructive sleep apnea and are sensitive to the respiratory depressant effects of opioids Avoiding or reducing opioid use in these patients may also result in shorter recovery time [14].
4.1.4 Anesthesia for orthopedic and spine surgery
Several systematic reviews and meta-analyses have been published in the last five years on the perioperative use of IV ketamine in orthopedic and spine surgeries.
Xu et al. conducted a systematic review of ten RCTs analyzing the effect of ketamine in total knee and hip arthroplasty. They concluded that IV ketamine administration reduced pain intensity in the early postoperative period i.e. up until eight hours after surgery but not within 8–24 h post-operatively. The cumulative morphine consumption was lower amongst patients who received ketamine till 48 h after surgery. Ketamine use was also observed to be safe and did not increase the risk of gastrointestinal or psychological side effects [15]. One of the trials where ketamine was administered as a bolus followed by continuous infusion for 48 h, demonstrated decreased incidence of chronic pain at 12 months follow-up [15]. Similar results have been observed in other meta-analyses assessing ketamine's role in patients undergoing arthroplasties. They demonstrated lower pain scores beyond the early postoperative period (24–48 h) [16, 17]. Intravenous ketamine when used for pain management in knee arthroplasty also reduced ischemic reperfusion injury [18]. Riddell et al. showed low-dose IV ketamine to be an effective adjunct within a multi-model regimen to decrease pain and opioid requirements across several types of orthopedic surgery in 1271 patients [19].
A meta-analysis of 30 RCTs followed 1865 patients and assessed pain at 12, 24, and 48 h after elective spinal surgery, concluded that patients who received IV ketamine had lower pain scores at rest as well as during mobilization until 48 h post-surgery. The dosages of IV ketamine used in these studies ranged from from a bolus dose of 0.15 to 0.5 mg and infusion rates ranging from 0.3– 10 μg·kg−1·min−1. Sub-group analyses showed that the analgesic effect lasted longer when ketamine was administered both during the intraoperative and the post-operative period. Cumulative opioid consumption after surgery was lower until 48 h. Most of the trials within this meta-analysis administered ketamine as a bolus followed by an infusion although the doses varied considerably. This effect was not observed in pediatric patients [20]. Similar results have been corroborated by other authors evaluating the role of ketamine in the same surgical population [21, 22].
4.1.5 Anesthesia for thoracic surgery
Tseng et al. conducted an RCT comparing low-dose IV ketamine and fentanyl patient-controlled analgesia (IVPCA) with thoracic epidural combined with patient-controlled epidural analgesia (t-PCEA) in acute postoperative pain after Video Assisted Thoracoscopic surgery. In the IVPCA group patient received a continuous infusion containing fentanyl 10 mcg·mL−1 and 0.5 mg·mL−1 ketamine. After a loading dose of 5ml, the background infusion rate was 1 mL−1·h−1 and a 1 mL bolus for a successful trigger every 5 min. They found similar pain control in both groups [23].
An RCT conducted by Borys et al. compared the preemptive administration of ketamine with the continuous paravertebral block (PVB) versus a control group undergoing posterolateral thoracotomy. Acute pain intensity was observed on a visual analog scale (VAS) on post-surgical day one. Acute pain intensity was significantly lower in both ketamine and PVB groups compared to the control group, however, patients who received PVB were more satisfied with pain management compared to the ketamine group [24].
4.1.6 Anesthesia for general surgery
Abdel-Rady et al. conducted a double-blind RCT in patients undergoing intestinal surgery [25]. The intervention group received IV ketamine 1.0 mg·kg−1 followed by an infusion of 0.12 μg·kg−1h−1 till wound closure. Patients were followed for 24 h. This dose regimen resulted in decreased pain scores and lower morphine consumption in the intervention group with no side effects.
Pajina et al. compared IV ketamine 0.25 mg·kg−1, Ilioinguinal nerve block (IINB) using 0.25% bupivacaine 20 ml under ultrasound guidance, and saline placebo, in 75 patients undergoing inguinal hernia repair. VAS scores were recorded at 0, 2, 6, 12, and 24 h post-operatively. Both low-dose IV ketamine and IINB provided effective pain control although IV ketamine showed inferior analgesia reflected by greater opioid consumption compared to IINB [26].
4.1.7 Pediatric anesthesia
Only a few studies have used perioperative IV ketamine as an adjunct analgesic in the pediatric age group, except in spine surgery [20, 21].
Intravenous ketamine 1.0 mg·kg−1 followed by intermittent boluses of 0.5 mg has also been tested in laser photocoagulation in 97 premature infants and compared to IV fentanyl. Both regimes provided inadequate analgesia [27].
4.1.8 Dental anesthesia
A randomized double-blind trial compared IV ketamine and dexmedetomidine in 66 patients undergoing extraction of impacted third molar surgery under general anesthesia. The pain was evaluated before the surgery and postoperatively. Those who received ketamine required less postoperative analgesia in the first 12 h postoperatively [28].
4.1.9 Other surgeries
An RCT included patients undergoing myomectomy and concluded that low-dose ketamine infusion (0.2 mg·kg−1·h−1) following a 0.2 mg.·kg −1 bolus had an opioid-sparing effect and reduced perioperative morphine consumption [29]. In another study IV ketamine administered as 0.15 mg.·kg−1 bolus followed by an infusion of 2 μg·kg−1·min−1 in patients undergoing robotic thyroidectomy decreased pain scores, cough for 24 h, and analgesic requirements without any serious complications [30]. S-ketamine IV has also been assessed for effectiveness and safety for pain relief in a systematic review by Wang et al. Surgeries included abdominal, thoracotomy, gynecological, arthroscopic anterior cruciate ligament repair, cardiac, laparoscopic cholecystectomy, lumbar spinal fusion, radical prostatectomy, and hemorrhoidectomy. S-ketamine reduced resting pain for up to 24 h and opioid consumption till 12 h postoperatively. There was no significant difference beyond this period for both pain and opioid consumption [31].
Perioperative pain management can be challenging in patients who have been using opioids preoperatively. A systematic review evaluated the effect of perioperative IV ketamine for its opioid-sparing effect in patients already consuming opioids. In three of the nine studies ketamine administration was continued till the end of a procedure while in six, ketamine administration lasted for 24 h. Ketamine slightly reduced pain in the 24 h following surgery, however, there was a significant reduction in oral morphine equivalent consumption after 24 h (mean 97.3 mg) and 48 h (mean 186.4 mg) of surgery [32].
A Cochrane review by Brinck et al. evaluated the role of perioperative IV ketamine for acute postoperative pain [33]. The authors noted that ketamine reduced postoperative opioid consumption and pain intensity, particularly after orthopedic, thoracic, and major abdominal surgeries. Moreover, the review also found evidence to suggest that ketamine may be more efficacious in moderate to severe pain and in reducing postoperative hyperalgesia.
4.1.10 Prevention of chronic post-surgical pain
Ketamine effects on AMPA receptors which are implicated in pain processing and chronic pain syndromes [6]. Central sensitization is also an important pathway for the development of chronic pain syndromes and ketamine’s role has been evaluated for this action. However, very few studies have been able to demonstrate the efficacy of ketamine to prevent chronic post-surgical pain. A recent systematic review and meta-analysis assessing multiple drugs including ketamine for the prevention of chronic pain after surgery failed to find any conclusive evidence. [34] A large multi-center trial is currently underway on this topic and its results will further elucidate the role of ketamine in this regard [35].
A summary table on the role of perioperative IV ketamine to manage acute postoperative pain and prevent chronic pain is given in Table 1.
4.2 Use of perioperative IV ketamine to prevent complications associated with neuraxial blocks
Intraoperative ketamine has also been assessed for the prevention of perioperative adverse effects of neuraxial blocks. An RCT investigated the efficacy of prophylactic low-dose ketamine infusion for the prevention of shivering after spinal anesthesia. Patients in the intervention limb were administered a bolus dose of 0.2 mg·kg−1 ketamine followed by an infusion of 0.1 mg·kg−1·h−1. Postoperative shivering was significantly lower in the ketamine group [58.06% in saline versus 13.79% in the ketamine group] compared to the control group who received a saline infusion [3].
4.3 Use of perioperative IV ketamine to reduce post-operative depression
Ketamine has a multitude of pharmacological properties that are not completely understood. The use of low-dose ketamine (0.3–0.5 mg·kg−1) in the intraoperative period has a beneficial effects on mood symptoms in the postoperative period [4]. Symptoms of depression are common among surgical patients and are a major concern contributing to perioperative morbidity [5]. Multiple trials in a systematic review by Li et al. suggest that intraoperative use of ketamine may have a beneficial role in rapidly improving symptoms of depression [36]. Zhou et al. conducted an RCT in patients with major depressive disorder undergoing supratentorial brain tumor resection. The intervention cohort received 0.5 mg·kg−1 of ketamine at the time of dural opening and was compared with the control group who received normal saline. Treatment response, which was defined as a reduction of 50% in symptoms of depression, was assessed by a psychiatrist on postoperative day three using the Montgomery-Asberg Depression Rating Scale. Response in the ketamine group was significantly higher (41.5%) versus the control group (16.3%). The study assessed only the short-term outcome of therapy, i.e., within the hospital stay [37]. Another trial assessed different doses of intravenous S-ketamine in the treatment of depression amongst cervical cancer patients undergoing laparoscopic hysterectomy. The investigators concluded that patients receiving ketamine had a lower Hamilton rating scale for Depression compared to controls. The most pronounced effect was seen in patients who received high dose S-ketamine, i.e., 0.5 mg·kg−1 after one hour of anesthesia induction [38].
There is also substantial evidence to support that administration of intravenous ketamine during the perioperative period of C-section which may help prevent post-partum depression (PPD) [32, 35]. Recently Li et al. in a meta-analysis also reported that ketamine's efficacy as prophylaxis for PPD occurred at a dose of 0.5 mg·kg−1. They also observed that age and body mass index were negatively associated with mood response to ketamine [36]. The authors noted better efficacy of ketamine as prophylaxis to PPD when administered through an analgesic pump continuously for 48 h post-partum instead of an intravenous injection during C-section. In another single-center trial of 375 parturients were administered patient controlled analgesia with S-ketamine, sufentanil and tropisetron and had a reduced incidence of PPD at day 14 compared to parturients who only received sufentanil and tropisetron [39].
A meta-analysis measuring outcomes in breast cancer patients concluded that perioperative intravenous ketamine led to improvement in postoperative depression and its effect persisted beyond one month [8]. Another meta-analysis by Wang et al. concluded that intravenous ketamine administration decreased postoperative depression symptoms till the third postoperative day [40].
There are also trials that have reported negative findings that ketamine does not reduce postoperative depression. Mashour et al. conducted a multicenter trial in patients above 60 years of age with variable pathology and surgical intervention but were unable to prove any beneficial effect on PPD [41]. Similar findings were reported in a meta-analysis evaluating the role of R and S-ketamine to prevent postoperative depression. Though the results were not significant a clinical decreases in the number of patients showing depressive symptoms was noted in the ketamine group [42].
Ketamine’s anti-depressant effects have been hypothesized to be due to multiple molecular pathways. The antagonism of NMDA receptors on post-synaptic neurons inhibits eukaryotic elongation factor 2 kinase leading to the translation of brain-derived neurotrophic factor (BDNF) [7]. BDNF signaling pathway eventually leads to the activation of proteins that are fundamental in synaptogenesis. BDNF can also prevent neuron injury and apoptosis, promote neuron regeneration and differentiation, and maintain the normal physiological function of neurons. It is a marker that is strongly correlated with anti-depressant effects and its levels have been studied as a secondary outcome in research assessing peri-operative ketamine's anti-depressant effect [42]. Evidence also suggests that indirect activation of AMPA receptors by ketamine may also lead to its anti-depressant effects. Interestingly anti-depressants like imipramine and fluoxetine are also associated with AMPA receptor upregulation. Ketamine's action on HCN1 receptors has also been hypothesized to lead to its anti-depressant effects [7].
A sizeable portion of evidence suggests intravenous ketamine has a role in rapidly improving depression in the perioperative setting and preventing PPD, however large-scale studies have failed to find significant association of ketamine to prevent postoperative depression [41, 42]. This may be due to the considerable heterogeneity in the doses and mode of assessment used in the meta-analysis. The multi-center negative trial conducted by Mashour et al. was done in elderly patients (above 60 years) and one of the critique on this study is that the rate of response to anti-depressant decreases with age [42].
The majority of the studies that reported a beneficial effect on depression used intravenous ketamine as a bolus of 0.5 mg.kg.−1 and similar dosing has been utilized in non-surgical settings. However, an important caveat to note is that although currently there is no conclusive evidence that intravenous ketamine may have a role to prevent postoperative depression, it does alleviate symptoms of depression postoperatively especially, amongst patients who suffered from depression preoperatively. The effect is more marked in patients who suffer more severe symptoms preoperatively [37, 38].
4.4 Use of perioperative IV ketamine to reduce emergence excitation, postoperative cognitive dysfunction and postoperative delirium
Recently there has been renewed interest in analyzing the potential neuroprotective effects of intraoperative ketamine. A systematic review assessing the effect of ketamine on emergence agitation (EA) in children revealed that patients receiving intraoperative ketamine had a lower incidence of EA [43].
In adult patients, intraoperative ketamine has been studied for the prevention of delirium and post-operative cognitive dysfunction (POCD). A systematic review on the topic highlighted the potential efficacy of intraoperative bolus of ketamine to reduce the incidence of POCD but not delirium [44]. Due to the paucity of high-quality data, it would be premature to conclude use of ketamine as a neuroprotective agent in the adult population.
A summary list of systematic reviews is provided in Table 2.
5 Conclusion
The majority of the studies in this literature review from the last five years have assessed the role of IV ketamine as an analgesic. The most consistent effect observed was in reducing postoperative opioid requirements. This was seen in breast surgery, C-section, myomectomy, knee arthroplasties, elective spine surgery, intestinal and bariatric surgery. The duration of this outcome measure was variable with some studies reporting the effect lasting for only eight hours postoperatively. There was considerable heterogeneity observed in the dose, timing, and method of administration (i.e., bolus, infusion, or both) of IV ketamine. Its role in the prevention of chronic post-surgical pain is still being defined.
Newer studies continue to define other roles of IV ketamine in perioperative medicine. Several trials suggest its use in decreasing symptoms of postoperative depression. Although promising, these results have only been observed in the early postoperative period. Recent evidence also suggests that IV ketamine may have a role in reducing shivering due to spinal anesthesia in obstetric patients undergoing C-section, and also in reducing postoperative cognitive dysfunction and delirium. There is a need for more robust evidence to be collected regarding its role apart from perioperative analgesia, before any firm conclusions can be drawn.
Availability of data and materials
Not applicable.
Abbreviations
- AMPA:
-
α-Amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid
- BDNF:
-
Brain-derived neurotrophic factor
- CNS:
-
Central nervous system
- C- section:
-
Cesarean section
- EA:
-
Emergence agitation
- HCN:
-
Hyperpolarization-activated cyclic nucleotide-gated
- IINB:
-
Ilioinguinal nerve block
- IV:
-
Intravenous
- IVPCA:
-
Intravenous patient-controlled analgesia
- NMDA:
-
N-Methyl-D-aspartate
- POCD:
-
Post-operative cognitive dysfunction
- PPD:
-
Post-partum depression
- PVB:
-
Paravertebral block
- RCTs:
-
Randomized controlled trials
- VAS:
-
Visual analog scale
References
Hirota K, Lambert DG. Ketamine; history and role in anesthetic pharmacology. Neuropharmacology. 2022;216:109171. https://doi.org/10.1016/j.neuropharm.2022.109171.
Gales A, Maxwell S. Ketamine: recent evidence and current uses. In: WFSA Resource Library [Internet]. 2018. [cited 2023 Jan 22]. Available from: https://resources.wfsahq.org/atotw/ketamine-recent-evidence-and-current-uses/.
Thangavelu R, George SK, Kandasamy R. Prophylactic low dose ketamine infusion for prevention of shivering during spinal anesthesia: a randomized double blind clinical trial. J Anaesthesiol Clin Pharmacol. 2020;36(4):506–10.
Mostafa RH, Khamis AM, Saleh AN, Mekki YMH, Kamal MM, Ibrahim IM, et al. Acute effects of ketamine infusion on postoperative mood scores in patients undergoing dilation and curettage: a randomized double-blind controlled study. Anesthesiol Res Pract. 2021;2021:6674658.
Reinert J, Parmentier BL. Effect of perioperative ketamine on postoperative mood and depression: a review of the literature. Expert Rev Clin Pharmacol. 2021;14(1):25–32.
Doan LV, Wang J. An update on the basic and clinical science of ketamine analgesia. Clin J Pain. 2018;34(11):1077–88. https://doi.org/10.1097/AJP.0000000000000635.
Subramanian S, Haroutounian S, Palanca BJA, Lenze EJ. Ketamine as a therapeutic agent for depression and pain: mechanisms and evidence. J Neurol Sci. 2022;434:120152. https://doi.org/10.1016/j.jns.2022.120152.
Bi Y,Ye Y, Zhu Y, Ma J, Zang X, Liu B.The effect of ketamine on acute and chronic wound pain in patients undergoing breast surgery: a meta-analysis and systematic review. Pain Pract Off J World Inst Pain. 2021;21(3):316–32.
Wang J, Xu Z, Feng Z, Ma R, Zhang X. Impact of ketamine on pain management in cesarean section: a systematic review and meta-analysis. Pain Physician. 2020;23(2):135–48.
Adhikari P, Subedi A, Sah BP, Pokharel K. Analgesic effects of intravenous ketamine after spinal anaesthesia for non-elective caesarean delivery: a randomised controlled trial. BMJ Open. 2021;11(6):e044168.
Ali H, Ismail AA, Wahdan AS. Low-dose ketamine infusion versus morphine infusion during abdominoplasty to change the postoperative pain profile. Anesth Pain Med. 2020;10(6):e108469.
Seman MT, Malan SH, Buras MR, Butterfield RJ, Harold KL, Madura JA, et al. Low-dose ketamine infusion for perioperative pain management in patients undergoing laparoscopic gastric bypass: a prospective randomized controlled trial. Anesthesiol Res and Pract. 2021;2021:5520517.
Mehta SD, Smyth D, Vasilopoulos T, Friedman J, Sappenfield JW, Alex G. Ketamine infusion reduces narcotic requirements following gastric bypass surgery: a randomized controlled trial. Surg Obes Relat Dis. 2021;17(4):737–43.
Chaouch MA, Daghmouri MA, Boutron MC, Ferraz JM, Usai S, Soubrane O, et al. Ketamine as a component of multimodal analgesia for pain management in bariatric surgery: a systematic review and meta-analysis of randomized controlled trials. Ann Med Surg. 2022;78:103783.
Xu B, Wang Y, Zeng C, Wei J, Li J, Wu Z, et al. Analgesic efficacy and safety of ketamine after total knee or hip arthroplasty: a meta-analysis of randomised placebo-controlled studies. BMJ Open. 2019;9(9):e028337.
Wang P, Yang Z, Shan S, Cao Z, Wang Z. Analgesic effect of perioperative ketamine for total hip arthroplasties and total knee arthroplasties: a PRISMA-compliant meta-analysis. Medicine (Baltimore). 2020;99(42):e22809. https://doi.org/10.1097/MD.0000000000022809.
Li Z, Chen Y. Ketamine reduces pain and opioid consumption after total knee arthroplasty: a meta-analysis of randomized controlled studies. Int J Surg. 2019;70:70–83.
Pan L, Shen Y, Ma T, Xue H. The efficacy of ketamine supplementation on pain management for knee arthroscopy: a meta-analysis of randomized controlled trials. Medicine (Baltimore). 2019;98(33):e16918.
Riddell JM, Trummel JM, Onakpoya IJ. Low-dose ketamine in painful orthopaedic surgery: a systematic review and meta-analysis. Br J Anaesth. 2019;123(3):325–34. https://doi.org/10.1016/j.bja.2019.05.043.
Zhou L, Yang H, Hai Y, Cheng Y. Perioperative low-dose ketamine for postoperative pain management in spine surgery: a systematic review and meta-analysis of randomized controlled trials. Pain Res Manag. 2022;2022:1507097.
Park PJ, Makhni MC, Cerpa M, Lehman RA, Lenke LG. The role of perioperative ketamine in postoperative pain control following spinal surgery. J Spine Surg. 2020;6(3):591–7.
Pendi A, Field R, Farhan SD, Eichler M, Bederman SS. Perioperative ketamine for analgesia in spine surgery: a meta-analysis of randomized controlled trials. Spine (Phila Pa 1976). 2018;43(5):E299–307. https://doi.org/10.1097/BRS.0000000000002318.
Tseng WC, Lin WL, Lai HC, Huang TW, Chen PH, Wu ZF. Fentanyl-based intravenous patient-controlled analgesia with low dose of ketamine is not inferior to thoracic epidural analgesia for acute post-thoracotomy pain following video-assisted thoracic surgery: a randomized controlled study. Medicine. 2019;98(28):e16403.
Borys M, Hanych A, Czuczwar M. Paravertebral block versus preemptive ketamine effect on pain intensity after posterolateral thoracotomies: a randomized controlled trial. J Clin Med. 2020;9(3):793.
AbdelRady MM, AboElfadl GM, Othman Mohamed EA, Abdel-rehim MG, Ali AH, Saadimbaby AS, et al. Effect of small dose ketamine on morphine requirement after intestinal surgery: a randomized controlled trial. Egypt J Anaesth. 2021;37(1):302–9.
Pajina B, Tiyaprasertkul W, Thawillarp S, Wisedkarn K, Pokawinpudisnun P. Comparison of low dose ketamine versus ilioinguinal-iliohypogastric nerve block for post-operative pain relief in inguinal hernia repair surgery: a randomized controlled trial. Ambul Surg. 2021;27(1):15–8.
Madathil S, Thomas D, Chandra P, Agarwal R, Sankar MJ, Thukral A, et al. ‘NOPAIN-ROP’trial: Intravenous fentanyl and intravenous ketamine for pain relief during laser photocoagulation for retinopathy of prematurity (ROP) in preterm infants: a randomised trial. BMJ Open. 2021;11(9):e046235.
Gursoytrak B, Kocaturk O, Koparal M, Gulsun B. Comparison of dexmedetomidine and ketamine for managing postoperative symptoms after third-molar surgery. J Maxillofac Surg. 2021;79(3):532–6.
Wahdan AS, Mohamed MM, Helmy NY, Shehata GH, Salama AK. Effects of low-dose ketamine infusion on alleviating the opioid burden for patients undergoing myomectomy surgery. Turk J Anaesthesiol Reanim. 2021;49(1):52–7.
Lee J, Park HP, Jeong MH, Son JD, Kim HC. Efficacy of ketamine for postoperative pain following robotic thyroidectomy: a prospective randomised study. J Int Med Res. 2018;46(3):1109–20.
Wang X, Lin C, Lan L, Liu J. Perioperative intravenous S-ketamine for acute postoperative pain in adults: a systematic review and meta-analysis. J Clin Anesth. 2021;68:110071.
Meyer-Frießem CH, Lipke E, Weibel S, Kranke P, Reichl S, Pogatzki-Zahn EM, et al. Perioperative ketamine for postoperative pain management in patients with preoperative opioid intake: a systematic review and meta-analysis. J Clin Anesth. 2022;78:110652.
Brinck EC, Tiippana E, Heesen M, Bell RF, Straube S, et al. Perioperative intravenous ketamine for acute postoperative pain in adults. Cochrane Database Syst Rev. 2018;12(12):CD012033.
Carley ME, Chaparro LE, Choinière M, Kehlet H, Moore RA, Van Den Kerkhof E, et al. Pharmacotherapy for the prevention of chronic pain after surgery in adults: an updated systematic review and meta-analysis. Anesthesiology. 2021;135(2):304–25. https://doi.org/10.1097/ALN.0000000000003837.
Schug SA, Peyton P. Does perioperative ketamine have a role in the prevention of chronic postsurgical pain: the ROCKet trial. Br J Pain. 2017;11(4):166–8. https://doi.org/10.1177/2049463717736076.
Li Q, Wang S, Mei X. A single intravenous administration of a sub-anesthetic ketamine dose during the perioperative period of cesarean section for preventing postpartum depression: a meta-analysis. Psychiatry Res. 2022;310:114396.
Zhou Y, Sun W, Zhang G, Wang A, Lin S, Chan MTV, et al. Ketamine alleviates depressive symptoms in patients undergoing intracranial tumor resection: a randomized controlled trial. Anesth Analg. 2021;133(6):1588–97.
Wang J, Wang Y, Xu X, Peng S, Xu F, Liu P. Use of Various Doses of S-Ketamine in Treatment of Depression and Pain in Cervical Carcinoma Patients with Mild/Moderate Depression After Laparoscopic Total Hysterectomy. Med Sci Monit Int Med J Exp Clin Res. 2020;26:e9220281–6.
Han Y, Li P, Miao M, Tao Y, Kang X, Zhang J. S-ketamine as an adjuvant in patient-controlled intravenous analgesia for preventing postpartum depression: a randomized controlled trial. BMC Anesthesiol. 2022;22(1):49. https://doi.org/10.1186/s12871-022-01588-7.
Wang J, Sun Y, Ai P, Cui V, Shi H, An D, et al. The effect of intravenous ketamine on depressive symptoms after surgery: a systematic review. J Clin Anesth. 2022;77:110631. https://doi.org/10.1016/j.jclinane.2021.110631.
Mashour GA, Abdallah AB, Pryor KO, El-Gabalawy R, Vlisides PE, Jacobsohn E, Lenze E, Maybrier HR, Veselis RA, Avidan MS, PODCAST Research Group. Intraoperative ketamine for prevention of depressive symptoms after major surgery in older adults: an international, multicentre, double-blind, randomised clinical trial. Br J Anaesth. 2018;121(5):1075–83.
Pang L, Cui M, Dai W, Kong J, Chen H, Wu S. Can intraoperative low-dose r, s-ketamine prevent depressive symptoms after surgery? The first meta-analysis of clinical trials. Front Pharmacol. 2020;19(11):586104. https://doi.org/10.3389/fphar.2020.586104.
Ng KT, Sarode D, Lai YS, Teoh WY, Wang CY. The effect of ketamine on emergence agitation in children: a systematic review and meta-analysis. Pediatr Anesth. 2019;29(12):1163–72.
Hovaguimian F, Tschopp C, Beck-Schimmer B, Puhan M. Intraoperative ketamine administration to prevent delirium or postoperative cognitive dysfunction: a systematic review and meta-analysis. Acta Anaesthesiol Scand. 2018;62(9):1182–93.
Lu Y, Wang Y, Zhou Z, Zhang D, Bao Y, Wu J, Cui Y. Meta-analysis of the efficacy and safety of ketamine on postoperative catheter related bladder discomfort. Front Pharmacol. 2022;13. https://doi.org/10.3389/fphar.2022.816995. Sec Neuropharmacology.
Acknowledgements
Not applicable.
Funding
No funds, grant or other support was received for conducting this review.
Author information
Authors and Affiliations
Contributions
Review concept: Khan, F.A. and Khan, Z. All authors participated in other work to finish this Review including design and protocol, review of abstracts and studies, writing and revision of manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
All authors gave their consent for publication.
Competing interests
Prof. Fauzia Anis Khan is a member of the Editorial Board in Anesthesiology and Perioperative Science and recuses herself from every editorial procedure of this submission including peer-review and academic decisions. All authors have no financial or propriety interests in any material discussed in the article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Khan, Z., Hameed, M. & Khan, F.A. Current role of perioperative intravenous ketamine: a narrative review. APS 1, 36 (2023). https://doi.org/10.1007/s44254-023-00035-1
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s44254-023-00035-1