Abstract
Purpose of Review
Multiple guidelines and recommendations have been written to address the perioperative management of antiplatelet and anticoagulant drugs. In this review, we evaluated the recent guidelines in non-cardiac, cardiac, and regional anesthesia. Furthermore, we focused on unresolved problems and novel approaches for optimized perioperative management.
Recent Findings
Vitamin K antagonists should be stopped 3 to 5 days before surgery. Preoperative laboratory testing is recommended. Bridging therapy does not decrease the perioperative thromboembolic risk and might increase perioperative bleeding risk. In patients on direct-acting oral anticoagulants (DOAC), a discontinuation interval of 24 and 48 h in those scheduled for surgery with low and high bleeding risk, respectively, has been shown to be saved. Several guidelines for regional anesthesia recommend a conservative interruption interval of 72 h for DOACs before neuraxial anesthesia. Finally, aspirin is commonly continued in the perioperative period, whereas potent P2Y12 receptor inhibitors should be stopped, drug-specifically, 3 to 7 days before surgery.
Summary
Many guidelines have been published from various societies. Their applicability is limited in emergent or urgent surgery, where novel approaches might be helpful. However, their evidence is commonly based on small series, case reports, or expert opinions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Antithrombotic drugs are frequently used to prevent or treat various common cardiovascular disorders like acute coronary syndrome (ACS), stroke, peripheral vascular disease, atrial fibrillation (AF), and venous thromboembolism (VTE). Two main classes of oral antithrombotic drugs are on the market: antiplatelet drugs, which prevent or temper inadvertent or inadequate platelet activation and initial clot formation, and anticoagulants, which slow down clot formation by controlling and reducing thrombin generation and formation of stable clots [1]. Aspirin and P2Y12 inhibitors are the most commonly used antiplatelet drugs, either alone or as dual antiplatelet therapy (DAPT) [2•]. Among oral anticoagulants, there are two main drug classes: vitamin K antagonists (VKA) and direct-acting oral anticoagulants (DOAC).
The perioperative management of patients receiving anticoagulant therapy is a frequently encountered clinical scenario, especially with the aging population [3]. Older patients are more likely to be treated with antiplatelets and/or anticoagulants and to require surgeries or invasive procedures than younger patients [3,4]. In addition, anticoagulant use is increasing due to the availability of DOACs, which are easier to handle for the patient than VKA [5]. Thus, it is estimated that in patients with AF, which is the dominant clinical indication for long-term anticoagulant therapy, 10 to 15% will require treatment interruption annually for an elective surgery or invasive procedure [6]. Finally, due to multiple shared risk factors for VTE and arteriosclerotic diseases, combined antiplatelet and anticoagulant therapy is indicated in some patients [1,7]. The combined therapy might be associated with specially increased bleeding risk during surgical intervention.
Despite many years of experience, perioperative management of antiplatelet and anticoagulant drugs in cardiac and non-cardiac surgery remains a dilemma with respect to balancing bleeding versus thrombotic risks. Multiple guidelines and recommendations by various societies have addressed the optimal management of these drugs in different surgical and invasive settings. In this review, we attempt to evaluate the recent guidelines on perioperative management of anticoagulant and antiplatelet agents. Furthermore, we focus on unresolved problems and novel approaches for improved perioperative management in specific patients treated with antiplatelets and anticoagulants.
Search Strategy
An extensive English literature search in PubMed was performed using the following terms: (guidelines) AND (perioperative) AND (anticoagulation). In addition, we searched the homepages of important American and European Societies of cardiac and non-cardiac anesthesiology including but not limited to the American Society of Anesthesiology (ASA), the American Society of Regional Anesthesia (ASRA), the Society of Cardiovascular Anesthesiologists (SCA), the European Society of Anaesthesiology and Intensive Care (ESAIC), and the European Association of Cardiothoracic Anaesthesiology and Intensive Care (EACTAIC) for recent guidelines on this topic. We focused on guidelines published within the last 5 years. Publications with potential importance were critically reviewed and eventually included in this publication.
Perioperative Management of VKA
Vitamin K antagonists, also called coumarins, have been licensed for clinical use since the early 1950s. For many years, VKAs were the only oral medication that could be reliably used for anticoagulation. Despite being largely replaced by DOACs in the United States (US) and Europe, VKAs remain the only approved therapy in patients with mechanical heart valves [8]. For those patients, DOAC therapy is associated with worse outcome compared to VKA therapy [9].
Whereas warfarin is the VKA of choice in the US, phenprocoumon and acenocoumarol are commonly used alternatives in Europe. After oral administration with close to 100% bioavailability, VKAs exert their effects via inhibition of the epoxide reductase enzyme. The latter is required to recycle oxidized vitamin K to a reduced state, which is an essential co-factor in the hepatic production of coagulation factors II, VII, IX, and X. In addition, vitamin K is essential in the hepatic production of protein C and S anticoagulants. Because of this indirect mechanism of action of VKAs, it takes several days to reach onset and offset. The administration of vitamin K can accelerate the synthesis of new coagulation factors II, VII, IX, and X. The specific pharmacologic aspects of VKAs have relevant implications for perioperative management. The half-life is drug specific and spans from about 36 h for warfarin and acenocoumarol to at least 72 h for phenprocoumon. VKAs are highly protein-bound but might be easily displaced by other highly protein-bound drugs. Furthermore, they are almost entirely metabolized in the liver, which exposes them to changed degradation with genetic polymorphism and drug interactions. Additional interactions might occur with food intake. All of these factors result in highly variable half-life and drug effects of VKAs in clinical practice [10].
Non-cardiac Surgery
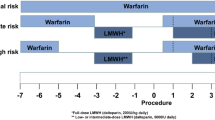
In patients on chronic anticoagulant therapy, VKAs are typically stopped 3 to 5 days prior to surgical or invasive procedures to allow its anticoagulant effect to dissipate. VKA therapy is subsequently resumed within 24 h after the intervention (Table 1, Fig. 1) [11]. Preoperative laboratory testing for recovered coagulation function by prothrombin time (PT) or international normalized ratio (INR) is recommended due to large interindividual variations in recuperation of vitamin K–dependent coagulation factors [11,12]. The value of pre- and postoperative bridging therapy in low-risk patients has been questioned in recent studies [13••, 14••].
Management of oral anticoagulation and antiplatelet therapy in elective patients with and without indication for pre- and/or postoperative bridging (adapted from [15]). Abbreviations: DOAC, direct-acting oral anticoagulants; VKA, vitamin K antagonists.
Cardiac Surgery
Similar recommendations as outlined for non-cardiac surgery are valid for cardiac surgery. According to the recent European and US guidelines on patient blood management in cardiac surgery, VKAs are withheld 3 to 5 days before surgery [15, 16•]. INR testing should be performed before surgery aiming for an INR <1.5 [15]. The safety and efficacy of perioperative bridging therapy in cardiac surgery are scarcely defined [11,17]. Either unfractionated heparin or low molecular weight heparins (LMWH) can be used according to US guidelines, whereas LMWHs are favored in the European guidelines [18,19] The individual thrombotic risk is the main determinant whether to bridge or not before cardiac surgery [11,20].
Regional Anesthesia
In patients planned for regional anesthesia, the timely interruption of VKA therapy 3 to 5 days before intervention is recommended [21•]. PT or INR should be within normal range before initiation of neuraxial anesthesia or deep peripheral nerve blocks (Table 2) [21•]. Furthermore, removal of indwelling neuraxial catheters is generally not recommended when INR is >1.5 [21•]. According to some expert opinions, removal of neuraxial catheters could be performed with caution when INR is between 1.5 and 3. In such cases, neurological status needs to be assessed carefully and regularly until INR has normalized (e.g., <1.5). In case of INR >3.0 and concurrent indwelling neuraxial or deep perineural catheters, VKA should be withheld or at least reduced until INR has dropped [21•]. Superficial nerve blocks can be performed in patients with INR >1.5 with minimal safety concerns [22].
Bridging
Perioperative interruption of VKA relevantly decreases the bleeding risk during and after major surgery. However, patients will be exposed to subtherapeutic anticoagulation for roughly 10–15 days. Given the common postoperative inflammatory and prothrombotic endogenous reaction, such a perioperative interruption raises the question of whether a pre- and post-interventional bridging anticoagulation is warranted to shorten the periods with subtherapeutic anticoagulation. Recently, two large randomized trials have assessed the therapeutic benefits and risks of heparin bridging before and after non-cardiac surgery [13••, 14••]. These studies clarified some uncertainties about “how to bridge” and, even more importantly, “whether or not to bridge.” The putative benefits of heparin bridging with the intention to mitigate the risk of perioperative thromboembolism were not evident in these studies. Furthermore, the Perioperative Anticoagulation Use for Surgery Evaluation (PAUSE) study found significantly more bleeding in the group with heparin bridging [13••]. Of note, these studies mainly included low-risk patients, and the perioperative or peri-interventional bridging therapy might still be indicated in patients with high risk for thromboembolism. In cardiac surgery, bridging-associated increased bleeding risk might be minor threat due to high-dose heparin for CPB and protamine reversal.
The risk of perioperative thrombotic events can be divided into four main pathological groups: (1) mechanical heart valves, (2) AF, (3) thrombophilia with or without history of VTE, and (4) risk of VTE due to surgical intervention. Mechanical valves in the mitral position are always considered as high risk, whereas aortic valves are divided by type: the older caged or tilting disc valves are high risk, whereas newer bi-leaflet valves are low or medium risk depending on additional risk factors [23]. Therefore, bridging might not be absolutely necessary in all mechanical aortic valves. Patients with deficiency of protein C, protein S, or antithrombin, patients with antiphospolipid syndrome, or patients with homozygous factor V Leiden or prothrombin gene mutation are at very high risk for thromboembolic events (annual VTE risk 10%), and perioperative bridging is recommended. Patients with heterozygous factor V Leiden or prothrombin gene mutation are at moderate risk (annual VTE risk 5–10%), similar to most AF patients [24]. Perioperative bridging might not generally be necessary [13••]. Specific thrombophilia testing seems not warranted in most perioperative patients.
Of note, the perioperative thromboembolic risk in patients with AF or history of VTE might be overestimated by 30 to 80% of physicians [25]. The latter might explain the overzealous use of bridging therapy in patients at low risk for VTE [25].
Urgent Surgery
In patients with recent VKA intake scheduled for urgent or emergent surgery, it is recommended to administer vitamin K to accelerate hepatic production of coagulation factors II, VII, IX, and X [26]. However, restoration of adequate levels of these coagulation factor by oral or intravenous administration of high-dose vitamin K takes several hours. If faster reversal is necessary, administration of 4-factor prothrombin complex concentrates (PCC) at a dose of 20–30 U/kg is suggested [27,28]. There is an evident risk of overshooting levels of coagulation factors, especially with high doses of PCC and with coagulation factors with long half-life, such as prothrombin [29]. The use of PCCs might, therefore, be associated with increased risk of thromboembolism. However, the risk of thromboembolic events after administration of PCCs as observed in a large 15-year pharmacovigilance study was generally low [30], and a systematic review on the use of PCCs in cardiac surgery found no additional risks of thromboembolic events or other adverse reactions [31]. Alternatively, FFP might be administered, but high doses of at least 15 ml/kg are required for fast recovery of coagulation factor levels. The latter would be associated with the risk of volume overload in patients with impaired cardiac function [26,32].
What Remains to Be Defined?
There has been a shift away from routine bridging due to mounting evidence suggesting that bridging with heparin confers an increase in both major bleeding and cardiovascular events without an evident decrease in thromboembolic events [13••, 33••]. Instead, decisions to bridge or not to bridge should be considered based on the patient’s individual risk profile for thromboembolism as well as the interventional risk for bleeding. Recent evidence suggests that VKA might not be stopped for procedures with low bleeding risk [34]. Interventions such as gastroscopy, endovascular interventions, cardiac device implantation, cataract surgery, dental extractions, and minor surgery as arthroscopy can be performed while VKA therapy is continued [35]. A recent observational study in major urologic surgery suggested that continued oral anticoagulation was not associated with increased intraoperative bleeding risk [36]. Finally, the unnecessary interruption of VKA has been associated with increased stroke risk within the first week of re-initiation [35]. The latter might be explained by faster inhibition of the endogenous production of anticoagulant proteins C and S, resulting in a relative hypercoagulant state in addition to the postoperative prothrombotic state. Finally, randomized controlled trials are needed to establish safe and optimal dosing of PCC in emergent surgery or bleeding patients [31].
Perioperative Management of DOAC
DOACs are rapidly gaining ground and will probably replace classic VKA therapy in most patients with AF and VTE or at risk for it in the US and Europe. Dabigatran, a direct thrombin inhibitor, was the first of these novel types of oral anticoagulants, which was approved by the FDA in 2010. Today, the market for DOAC is dominated by the factor Xa inhibitors rivaroxaban and apixaban. DOACs have many advantages compared to VKA, including more reliable pharmacokinetics and pharmacodynamics, fewer interactions with other drugs and food, and no need for regular laboratory testing. These beneficial effects might have the potential to outweigh the relevantly higher drug-related costs of DOACs [37,38].
The perioperative handling of DOACs in elective surgery is rather simple. Due to the short half-life, interruption intervals of 24 to 48 h are recommended depending on the invasiveness and the bleeding risk of surgery [33••]. Bridging is not recommended, because the duration necessary for the drug to be withheld before surgery is short and the restoration of clinical effect upon re-initiation is rapid, with no procoagulant effect.
Non-cardiac Surgery
The recently published PAUSE study assessed whether stopping DOACs for 1 to 4 days before surgery is safe [33••]. The authors included more than 3,000 patients treated with either apixaban (42%), rivaroxaban (36%), or dabigatran (22%) for AF, which were scheduled for elective non-cardiac surgery or an invasive procedure. DOACs were omitted for 1 day before a low-bleeding risk procedure and 2 days before a high-bleeding risk procedure. DOACs were resumed 1 day after low-risk procedures and after 2 to 3 days after a high-risk procedure. No perioperative bridging was applied. This study proved that such a simple standardized DOAC interruption was safe with acceptably low rates of perioperative major bleeding and arterial thromboembolism [33••]. Thus, the study supported former recommendations suggesting similar perioperative DOAC interruption regimens [35,39,40,41].
Prolonged discontinuation intervals might be necessary in patients with impaired renal function (creatinine clearance <30 ml/min), with very low body weight, or advanced geriatric age (Table 1). These risk factors have been associated with higher than normal DOAC levels and DOAC levels of 30–50 ng/ml after a discontinuation interval of 48 h [33••]. Importantly, patients with impaired renal function were excluded from the PAUSE study [33••].
Cardiac Surgery
Cardiac surgery is a major surgical intervention with a high bleeding risk. In the recent recommendations from the EACTAIC subcommittee of hemostasis and transfusion [27], a group of European experts stated that most patients on DOAC therapy presenting for elective cardiac surgery can be safely managed in the peri-operative period considering the following recommendations: (1) DOACs should be discontinued two days before elective cardiac surgery; no routine DOAC monitoring is recommended in such cases; (2) in patients with renal or hepatic impairment or additional risk factors for bleeding, pre-operative plasma level of direct oral anticoagulants should be <30 ng/ml; and (3) in similar situations where plasma level monitoring is not feasible (e.g., assay is unavailable), the discontinuation interval should be prolonged to 4 to 5 days, corresponding to 10 elimination half-life.
Regional Anesthesia
Neuraxial anesthesia, such as intrathecal or epidural anesthesia, is viewed as a high-risk intervention with limited outcome benefit in most patients. Furthermore, bleeding complications associated with potentially elevated DOAC levels, especially neuraxial hematoma, could be devastating. Accordingly, recently published guidelines on the perioperative management of DOAC in patients scheduled for neuraxial anesthesia are very conservative [42]. In the 2018 update of the 2010 ASRA guidelines [21•], experts again proposed a conservative strategy in patients receiving DOAC therapy and recommended a discontinuation interval of at least five half-lives. Accordingly, the estimated drug concentration remaining in the system should be <3.1% of blood peak concentration, when neuraxial anesthesia is performed [21•]. Patients treated with rivaroxaban or apixaban should stop their DOAC therapy 72 h before neuraxial anesthesia [21]. Furthermore, the clinician should consider checking the plasma level of anti-Xa inhibitors if the interval is less than 72 h [21•]. Patients prescribed dabigatran with a creatinine clearance >30 ml/min should have neuraxial blocks only 3 to 5 days after the last dose. In those treated with dabigatran with a creatinine clearance <30 ml/min, neuraxial anesthesia should be omitted.
Given the short elimination half-life of DOACs in most patients, a management approach stopping DOACs for 4 to 6 days before surgery might be questioned. Moreover, the longer period without anticoagulation might expose the patient to an increased thromboembolic risk [33••]. Accordingly, European and Scandinavian guidelines have adopted a two half-life interval (48 h) between discontinuation of the drug and neuraxial injection [43].
What Remains to Be Defined?
Based on the PAUSE study [33] and expert opinions [27], DOAC levels <50 ng/ml and <30 ng/ml should be safe for procedures with low and high bleeding risk, respectively. The PAUSE study showed that levels were <50 ng/ml in 91–97% and 99% of patients after interruption intervals of 24 and 48 h, respectively. Applying stricter definitions of critical levels, 90 to 95% of patients were below the threshold of <30 ng/ml after an interruption interval of 48 h [33••].
Despite the proven safety of an interruption period of 24–48 h as evaluated in the PAUSE study [33••], excessive residual anticoagulant level might be present in some patients. Preoperative coagulation testing should be considered in patients with risk factors for persistently high DOAC levels, such as impaired kidney function, very low body weight, or advanced geriatric age. Specific preoperative DOAC level determination in these patients might allow deciding whether a procedure should be delayed or specific DOAC reversal should be applied [27]. However, DOAC-specific coagulation tests are not universally available. Recently, a large French multicenter study showed that the commonly available heparin anti-Xa activity test could be used with adequate accuracy to determine levels of direct anti-Xa inhibitors [44].
Recently, DOAC-specific reversal agents (idarucizumab and andexanet alfa) have been approved for DOAC-associated life-threating or uncontrolled bleeding. A secondary analyses of patients from a large cohort study suggested that idarucizumab should be given without awaiting the laboratory results in patients scheduled for emergent surgery [45]. In contrast, the evidence for administration of andexanet alfa in the perioperative setting is limited to case reports. Of note, the administration of andexanet alfa directly before cardiac or vascular surgery has been discouraged. Both andexanet alfa and heparin might interact with factor Xa and lead to less efficacy of andexanet alfa and/or impaired anticoagulant effect of heparin [46].
Perioperative Management of Antiplatelet Agents
Aspirin (acetylsalicylic acid) is a mainstay therapy in patients with and at risk for most types of cardiovascular disease. After oral or intravenous administration, aspirin exerts its antiplatelet effect via rapid-irreversible inhibition of the cyclooxygenase-1 enzyme, inhibiting the conversion of arachidonic acid to thromboxane A2 (TXA2). TXA2 activates platelets via the thromboxane-prostanoid (TP) receptor. Patients with recent coronary stent implantation are commonly treated with DAPT including aspirin and a P2Y12 receptor inhibitor. DAPT improves stent patency and prevents arterial thromboembolic events, but these drugs increase the risk of perioperative bleeding and the need for transfusion of allogeneic blood products. The efficacy, side effects, and safety of P2Y12 receptor inhibitors are drug specific. Third-generation drugs including prasugrel and ticagrelor have a more rapid and consistent anti-ischemic effect, caused by the stronger platelet inhibition and weaker interactions with the cytochrome P450 system compared to clopidogrel [2•, 47].
Non-cardiac Surgery
The main argument for withholding aspirin is to decrease the risk of major bleeding, but this strategy might increase the risk of perioperative thromboembolic events. In the Perioperative Ischemic Evaluation-2 (POISE-2) trial, discontinuation of aspirin during the perioperative period did not increase the risk of stroke or myocardial infarction in non-cardiac surgery [48]. Of note, the POISE-2 trial suggested an increase in major bleeding in the aspirin compared to placebo group (hazard ratio 1.23; 95% CI 1.01–1.49) [48]. This finding is in disagreement with several former large observational studies suggesting no increased bleeding risk with perioperatively continued aspirin therapy [49•]. Most guidelines recommend the perioperative continuation of aspirin therapy in patients with a history of cardiovascular disease when the potentially increased bleeding risk is acceptable for the surgeon [49•].
The optimal perioperative management of DAPT in patients undergoing non-cardiac surgery is more complicated and is still under debate given the competing risks of bleeding and stent thrombosis [50•]. The 2014 guidelines from the AHA/ACA recommended delaying elective non-cardiac surgery for 1 year after placement of drug-eluting stents (DES) and 30 days after bare-metal stents (BMS) [51]. The 2016 update modified these recommendations by reducing the time to safe surgery from 1 year to 6 months and by considering early surgery after 3 months if the risk of delaying surgery is greater than the risk of stent thrombosis [52]. In addition, DAPT therapy for at least 4–6 weeks after DES stenting was recommended in patients undergoing urgent non-cardiac surgery [52].
Regardless of timing of surgery, ACC/AHA guidelines recommend continuing at least aspirin throughout the perioperative period and ideally continuing DAPT “unless surgery demands discontinuation” [52]. After surgery, the P2Y12 receptor inhibitor should be restarted as soon as possible if stopped preoperatively [52]. However, definitive evidence regarding the optimal perioperative management of antiplatelet therapy is missing due to variable discontinuation intervals between and within studies [50•]. Of note, no study systematically assessed the impact of the cessation time point of antiplatelet therapy on clinical outcomes [50], and the ACC/AHA recommendations were mainly based on expert opinions [50•, 53]. Furthermore, newer generations of DES are thought to have a reduced risk of stent thrombosis, allowing for earlier stopping of DES without relevantly increasing thrombosis risk [52].
In patients with semi-urgent surgery, the decision to prematurely stop one or both antiplatelet agents (at least 5 days pre-operatively) has to be taken in a multidisciplinary consultation, evaluating the individual thrombotic and bleeding risk [54]. Urgently needed surgery has to take place under full antiplatelet therapy despite the increased bleeding risk. In some cases, instead of completely withholding antiplatelet therapy, bridging therapy by substitution with short-acting anticoagulants or an intravenous antiplatelet agents might be considered [50•].
Cardiac Surgery
Most current guidelines suggest continuing aspirin preoperatively to potentially reduce early thromboembolic events and mortality after coronary artery bypass graft (CABG) surgery [15, 55, 56]. These recommendations are in agreement with the findings of a very large meta-analysis evaluating 12 randomized controlled trials including nearly 4,000 patients undergoing CABG surgery and 28 observational studies including nearly 30,000 patients, most of them undergoing CABG surgery [57]. The preoperative continuation of aspirin was associated with reduction in early mortality, acute kidney failure, and myocardial infarction [57]. However, the positive findings were mainly driven by the observational studies. Of note, the largest randomized controlled trial, the Aspirin and Tranexamic Acid for Coronary Artery Surgery (ATACAS) trial including 2,100 CABG patients, found no benefit of continued aspirin administration regarding mortality, myocardial infarction, and stroke within 30 days and 1 year [58,59].
In elective cardiac surgery, it is commonly recommended to stop therapy with a P2Y12 receptor inhibitor 5 to 7 days before surgery [15,55,56]. These recommendations are based on a recent meta-analysis in >22,000 patients undergoing cardiac surgery reporting a potential protection against ischemic events but clearly increased risk of bleeding and higher mortality in patients with continued therapy with P2Y12 receptor inhibitors [60,61,62]. For urgent surgery, evidence is less clear. Postponing cardiac surgery for at least 2 to 3 days might relevantly reduce the risk for massive perioperative bleeding [2•, 63]. The use of platelet function monitoring might help to optimize and potentially reduce the preoperative waiting interval [2•, 64].
Regional Anesthesia
In patients scheduled for neuraxial anesthesia, a discontinuation interval of 7 to 10 days for clopidogrel and prasugrel, and 5 to 7 days for ticagrelor is recommended to reduce the potential risk of bleeding complications [21•]. The same recommendations apply for deep nerve blocks, whereas superficial nerve blocks might be performed without discontinuation of antiplatelet therapy [21•].
What Remains to Be Defined?
Optimal management of antiplatelets in specific situations needs to be defined. Recent data do not support a clear association between continuation and discontinuation of antiplatelet therapy and rates of ischemic events, bleeding complications, and mortality up to 6 months after surgery [54]. Clinical factors, such as indication and urgency of the operation, invasiveness of the procedure, time since stent placement, stent type, functional result of stenting, coronary anatomy, and perioperative control of supply–demand mismatch and bleeding may be more responsible for adverse outcome than antiplatelet management [65].
Similarly, the question of “whether or not to bridge” and “how to bridge” patients with antiplatelet therapy considered as high-risk for thromboembolic events needs to be defined in future studies. Different options have been described including heparin, low molecular weight heparins, glycoprotein IIb/IIIa inhibitors and, most recently, short-acting intravenous P2Y12 receptor inhibitors such as cangrelor. Bridging therapy with cangrelor after timely stopping of the longer acting oral P2Y12 receptor inhibitors might allow for short-term interruption of dual antiplatelet therapy in high-risk patients. The feasibility of such an approach has been described in case reports and a small cohort study [65].
Furthermore, bleeding complications in patients treated with potent antiplatelets might be a major challenge. Whereas the anticoagulant effect of prasugrel can be treated with platelet transfusion, this therapy might not suspend the antiplatelet effects of ticagrelor. Ticagrelor binds reversibly to the platelet ADP receptor, whereas clopidogrel and prasugrel binds irreversibly to this receptor. Therefore, freshly transfused platelet might be immediately blocked by soluble ticagrelor, and platelet transfusion is less efficient up to 24 h after last intake of ticagrelor.
However, recent reports suggest the use of CytoSorb® absorber during cardiopulmonary bypass to reduce ticagrelor levels, thereby reducing postoperative bleeding tendency [2•]. More recently, a phase I study in healthy volunteers evaluating the safety, efficacy, and pharmacokinetic profile of a neutralizing monoclonal antibody fragment that binds ticagrelor and its active circulating metabolite has shown promising results [66]. This drug might present a future opportunity for the anesthesiologist dealing with emergency surgical patients on ticagrelor therapy.
Finally, several whole blood platelet function tests have become commercially available in recent years. Most of them are used as point-of-care (POC) tests [2]. Routine platelet function testing is not recommended [2•, 15], but POC platelet function tests are useful in confirming residual P2Y12 inhibition and adjusting a waiting period before surgery [2•, 67,68,69].
Conclusions
The evidence remains limited for the optimal perioperative or peri-interventional treatment despite the increasing number of patients who are chronically managed with anticoagulants and antiplatelet drugs, especially in urgent or emergent surgery. Published studies involve multiple types of surgery with varying invasiveness, variable timing of discontinuation, and use of bridging agents. These factors insufficiently explain the wide range of major adverse cardiac and thromboembolic or bleeding events from 0 to nearly 25% in a recent systematic review [50•]. Specific patient factors and individual decisions might be more important, but these factors can often not be controlled in cohort studies. Whereas common recommendations (Fig. 1 and Table 1) are valid in many patients, individual decision-making is required in specific patients. New strategies published as case reports or small cohort studies might be helpful. Finally, due to the inherent risk of thromboembolic complications in these patients, early restarting of antiplatelet and anticoagulant agents after surgery is essential.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Bolliger D, Fassl J, Erdoes G. How to manage the perioperative patient on combined anticoagulant and antiplatelet therapy: comments on the 2020 ACC consensus decision pathway. J Cardiothorac Vasc Anesth. 2021;35:1561–4. https://doi.org/10.1053/j.jvca.2021.01.042.
• Bolliger D, Lance MD, Siegemund M. Point-of-Care platelet function monitoring: implications for patients with platelet inhibitors in cardiac surgery. J Cardiothorac Vasc Anesth. 2021;35:1049–59. https://doi.org/10.1053/j.jvca.2020.07.050A recent narrative review on the value of platelet function monitoring in patients scheduled for surgical interventions.
Tschan SL, Bolliger D. Coagulation and aging: implications for the Anesthesiologist. Curr Anesth Rep. 2021;epub ahead. https://doi.org/10.1007/s40140-021-00498-7.
Shah SJ, Singer DE, Fang MC, Reynolds K, Go AS, Eckman MH. Net clinical benefit of oral anticoagulation among older adults with atrial fibrillation. Circ Cardiovasc Qual Outcomes. 2019;12:e006212. https://doi.org/10.1161/CIRCOUTCOMES.119.006212.
Connors JM. Testing and monitoring direct oral anticoagulants. Blood. 2018;132:2009–15. https://doi.org/10.1182/blood-2018-04-791541.
• Tafur A, Douketis J. Perioperative management of anticoagulant and antiplatelet therapy. Heart. 2018;104:1461–7. https://doi.org/10.1136/heartjnl-2016-310581Experts in the perioperative management of anticoagulants and antiplatelet drugs recently summarized the best evidence for perioperative treatment.
Kumbhani DJ, Cannon CP, Beavers CJ, et al. 2020 ACC expert consensus decision pathway for anticoagulant and antiplatelet therapy in patients with atrial fibrillation or venous thromboembolism undergoing percutaneous coronary intervention or with atherosclerotic cardiovascular disease: a report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol. 2021;77:629–58. https://doi.org/10.1016/j.jacc.2020.09.011.
Andrade JG, Meseguer E, Didier R, Dussault C, Weitz JI. Non-vitamin K antagonist oral anticoagulants in atrial fibrillation patients with bioprosthetic valves. Expert Rev Cardiovasc Ther. 2018:1-6. https://doi.org/10.1080/14779072.2018.1475229.
Eikelboom JW, Connolly SJ, Brueckmann M, et al. Dabigatran versus warfarin in patients with mechanical heart valves. N Engl J Med. 2013;369:1206–14. https://doi.org/10.1056/NEJMoa1300615.
Ansell J, Hirsh J, Hylek E, Jacobson A, Crowther M, Palareti G. Pharmacology and management of the vitamin K antagonists: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest. 2008;133:160S–98S. https://doi.org/10.1378/chest.08-0670.
Douketis JD, Spyropoulos AC, Spencer FA, et al. Perioperative management of antithrombotic therapy: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2012;141:e326S–e50S. https://doi.org/10.1378/chest.11-2298.
Soyka MB, Holzmann D. Should we test the prothrombin time in anticoagulated epistaxis patients? Allergy Rhinol (Providence). 2013;4:e52–3. https://doi.org/10.2500/ar.2013.4.0049.
•• Douketis JD, Spyropoulos AC, Kaatz S, et al. Perioperative bridging anticoagulation in patients with atrial fibrillation. N Engl J Med. 2015;373:823–33. https://doi.org/10.1056/NEJMoa1501035The BRIDGE study is an important RCT showing that preoperative bridging in low-risk AF patients did not reduce the risk of thromboembolic events but increased perioperative bleeding risk.
•• Kovacs MJ, Wells PS, Anderson DR, et al. Postoperative low molecular weight heparin bridging treatment for patients at high risk of arterial thromboembolism (PERIOP2): Double blind randomised controlled trial. BMJ. 2021;373:n1205. https://doi.org/10.1136/bmj.n1205The PERIOP2 study is an important RCT showing that postoperative bridging idid not reduce the risk of thromboembolic events.
Boer C, Meesters MI, Milojevic M, et al. 2017 EACTS/EACTA Guidelines on patient blood management for adult cardiac surgery. J Cardiothorac Vasc Anesth. 2018;32:88–120. https://doi.org/10.1053/j.jvca.2017.06.026.
• Tibi P, McClure RS, Huang J, et al. STS/SCA/AmSECT/SABM Update to the clinical practice guidelines on patient blood management. J Cardiothorac Vasc Anesth. 2021;35:2569–91. https://doi.org/10.1053/j.jvca.2021.03.011The most recent guidelines on patient blood management and perioperative anticoagulants in cardiac surgery.
Dunn AS, Turpie AG. Perioperative management of patients receiving oral anticoagulants: a systematic review. Arch Intern Med. 2003;163:901–8. https://doi.org/10.1001/archinte.163.8.901.
Vahanian A, Beyersdorf F, Praz F, et al. 2021 ESC/EACTS Guidelines for the management of valvular heart disease. Eur J Cardiothorac Surg. 2021;60:727–800. https://doi.org/10.1093/ejects/ezab389.
Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guidelines for the management of patients with valvular heart disease: executive summary: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2021;77:450–500. https://doi.org/10.1016/j.jacc.2020.11.035.
Baumann Kreuziger L, Karkouti K, Tweddell J, Massicotte MP. Antithrombotic therapy management of adult and pediatric cardiac surgery patients. J Thromb Haemost. 2018;16:2133–46. https://doi.org/10.1111/jth.14276.
• Horlocker TT, Vandermeuelen E, Kopp SL, Gogarten W, Leffert LR, Benzon HT. Regional anesthesia in the patient receiving antithrombotic or thrombolytic therapy: American Society of Regional Anesthesia and Pain Medicine evidence-based guidelines (Fourth Edition). Reg Anesth Pain Med. 2018;43:263–309. https://doi.org/10.1097/AAP.0000000000000763The most recent but very conservative guidelines on the management with anticoagulants and antiplatelet drugs scheduled for regional anesthesia.
Li J, Halaszynski T. Neuraxial and peripheral nerve blocks in patients taking anticoagulant or thromboprophylactic drugs: challenges and solutions. Local Reg Anesth. 2015;8:21–32. https://doi.org/10.2147/LRA.S55306.
Tan CW, Wall M, Rosengart TK, Ghanta RK. How to bridge? Management of anticoagulation in patients with mechanical heart valves undergoing noncardiac surgical procedures. J Thorac Cardiovasc Surg. 2019;158:200–3. https://doi.org/10.1016/j.jtcvs.2018.06.089.
Bridge Study Investigators. Bridging anticoagulation: Is it needed when warfarin is interrupted around the time of a surgery or procedure? Circulation. 2012;125:e496–8. https://doi.org/10.1161/CIRCULATIONAHA.111.084517.
Moesker MJ, de Groot JF, Damen NL, et al. Guideline compliance for bridging anticoagulation use in vitamin-K antagonist patients; practice variation and factors associated with non-compliance. Thromb J. 2019;17:15. https://doi.org/10.1186/s12959-019-0204-x.
Garcia DA, Crowther MA. Reversal of warfarin: case-based practice recommendations. Circulation. 2012;125:2944–7. https://doi.org/10.1161/CIRCULATIONAHA.111.081489.
Erdoes G, Koster A, Ortmann E, et al. A European consensus statement on the use of four-factor prothrombin complex concentrate for cardiac and non-cardiac surgical patients. Anaesthesia. 2021;76:381–92. https://doi.org/10.1111/anae.15181.
Percy CL, Hartmann R, Jones RM, et al. Correcting thrombin generation ex vivo using different haemostatic agents following cardiac surgery requiring the use of cardiopulmonary bypass. Blood Coagul Fibrinolysis. 2015;26:357–67. https://doi.org/10.1097/MBC.0000000000000243.
Schochl H, Voelckel W, Maegele M, Kirchmair L, Schlimp CJ. Endogenous thrombin potential following hemostatic therapy with 4-factor prothrombin complex concentrate: a 7-day observational study of trauma patients. Crit Care. 2014;18:R147. https://doi.org/10.1186/cc13982.
Hanke AA, Joch C, Gorlinger K. Long-term safety and efficacy of a pasteurized nanofiltrated prothrombin complex concentrate (Beriplex P/N): a pharmacovigilance study. Br J Anaesth. 2013;110:764–72. https://doi.org/10.1093/bja/aes501.
Roman M, Biancari F, Ahmed AB, et al. Prothrombin complex concentrate in cardiac surgery: a systematic review and meta-analysis. Ann Thorac Surg. 2019;107:1275–83. https://doi.org/10.1016/j.athoracsur.2018.10.013.
Refaai MA, Goldstein JN, Lee ML, Durn BL, Milling TJ Jr, Sarode R. Increased risk of volume overload with plasma compared with four-factor prothrombin complex concentrate for urgent vitamin K antagonist reversal. Transfusion. 2015;55:2722–9. https://doi.org/10.1111/trf.13191.
•• Douketis JD, Spyropoulos AC, Duncan J, et al. Perioperative management of patients with atrial fibrillation receiving a direct oral anticoagulant. JAMA Intern Med. 2019;179:1469–78. https://doi.org/10.1001/jamainternmed.2019.2431The PAUSE study is an important and large multicenter cohort study evaluating the safety of commonly suggested interruption intervals in patients treated with direct-acting oral anticoagulants undergoing non-cardiac surgery.
Perry DJ, Noakes TJ, Helliwell PS, British DS. Guidelines for the management of patients on oral anticoagulants requiring dental surgery. Br Dent J. 2007;203:389–93. https://doi.org/10.1038/bdj.2007.892.
Spyropoulos AC, Al-Badri A, Sherwood MW, Douketis JD. Periprocedural management of patients receiving a vitamin K antagonist or a direct oral anticoagulant requiring an elective procedure or surgery. J Thromb Haemost. 2016;14:875–85. https://doi.org/10.1111/jth.13305.
Furrer MA, Abgottspon J, Huber M, et al. Perioperative continuation of aspirin, oral anticoagulants or bridging with therapeutic low-molecular weight heparin does not increase intraoperative blood loss and blood transfusion rate in cystectomy patients: an observational cohort study. Brit J Urolog Int. 2021; epub ahead. https://doi.org/10.1111/bju.15599.
Lorenzoni V, Pirri S, Turchetti G. Cost-effectiveness of direct non-vitamin K oral anticoagulants versus vitamin K antagonists for the management of patients with non-valvular atrial fibrillation based on available “real-world” evidence: The Italian National Health System Perspective. Clin Drug Investig. 2021;41:255–67. https://doi.org/10.1007/s40261-021-01002-z.
Wu Y, Zhang C, Gu ZC. Cost-effectiveness analysis of direct oral anticoagulants vs. vitamin K antagonists in the elderly with atrial fibrillation: insights from the evidence in a real-world setting. Front Cardiovasc Med. 2021;8:675200. https://doi.org/10.3389/fcvm.2021.675200.
Faraoni D, Samama CM, Ranucci M, Dietrich W, Levy JH. Perioperative management of patients receiving new oral anticoagulants: an international survey. Clin Lab Med. 2014;34:637–54. https://doi.org/10.1016/j.cll.2014.06.006.
Raval AN, Cigarroa JE, Chung MK, et al. Management of patients on non-vitamin K antagonist oral anticoagulants in the acute care and periprocedural setting: a scientific statement from the American Heart Association. Circulation. 2017;135:e604–e33. https://doi.org/10.1161/CIR.0000000000000477.
Spyropoulos AC, Douketis JD. How I treat anticoagulated patients undergoing an elective procedure or surgery. Blood. 2012;120:2954–62. https://doi.org/10.1182/blood-2012-06-415943.
McIlmoyle K, Tran H. Perioperative management of oral anticoagulation. BJA Educ. 2018;18:259–64. https://doi.org/10.1016/j.bjae.2018.05.007.
Benzon HT, Avram MJ, Green D, et al. New oral anticaouglants and regional anesthesia. Br J Anaesth. 2013;111:i96–i113. https://doi.org/10.1093/bja/aet401.
Boissier E, Senage T, Babuty A, et al. Heparin anti-Xa activity, a readily available unique test to quantify apixaban, rivaroxaban, fondaparinux, and danaparoid levels. Anesth Analg. 2021;132:707–16. https://doi.org/10.1213/ANE.0000000000005114.
Levy JH, van Ryn J, Sellke FW, et al. Dabigatran reversal with idarucizumab in patients requiring urgent surgery: a subanalysis of the RE-VERSE AD study. Ann Surg. 2021;274:e204–e11. https://doi.org/10.1097/SLA.0000000000003638.
Erdoes G, Birschmann I, Nagler M, Koster A. Andexanet alfa-induced heparin resistance: when anticoagulation really remains reversed. J Cardiothorac Vasc Anesth. 2021;35:908–9. https://doi.org/10.1053/j.jvca2020.11.052.
Sousa-Uva M, Storey R, Huber K, et al. Expert position paper on the management of antiplatelet therapy in patients undergoing coronary artery bypass graft surgery. Eur Heart J. 2014;35:1510–4. https://doi.org/10.1093/eurheartj/ehu158.
Devereaux PJ, Mrkobrada M, Sessler DI, et al. Aspirin in patients undergoing noncardiac surgery. N Engl J Med. 2014;370:1494–503. https://doi.org/10.1056/NEJMoa1401105.
• Gerstein NS, Albrechtsen CL, Mercado N, Cigarroa JE, Schulman PM. A comprehensive update on aspirin management during noncardiac surgery. Anesth Analg. 2020;131:1111–23. https://doi.org/10.1213/ANE.0000000000005064A recent and very complete review on the use of aspirin in non-cardiac surgery.
• Childers CP, Maggard-Gibbons M, Ulloa JG, et al. Perioperative management of antiplatelet therapy in patients undergoing non-cardiac surgery following coronary stent placement: a systematic review. Syst Rev. 2018;7:4. https://doi.org/10.1186/s13643-017-0635-zThis systematic review showed that antiplatelet therapy in patients undergoing non-cardiac surgery is complex and far from standardized.
Fleisher LA, Fleischmann KE, Auerbach AD, et al. 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;130:e278–333. https://doi.org/10.1161/CIR.0000000000000106.
Levine GN, Bates ER, Bittl JA, et al. 2016 ACC/AHA guideline focused update on duration of dual antiplatelet therapy in patients with coronary artery disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2016;134:e123-55. Circulation. 2016;134:e123–55. https://doi.org/10.1161/CIR.0000000000000404.
Levine GN, Bates ER, Blankenship JC, et al. 2015 ACC/AHA/SCAI focused update on primary percutaneous coronary intervention for patients with ST-elevation myocardial infarction. Circulation. 2016;134:e123–55. https://doi.org/10.1161/CIR.0000000000000336.
Mazzeffi MA, Lee K, Taylor B, Tanaka KA. Perioperative management and monitoring of antiplatelet agents: a focused review on aspirin and P2Y12 inhibitors. Korean J Anesthesiol. 2017;70:379–89. https://doi.org/10.4097/kjae.2017.70.4.379.
Kozek-Langenecker SA, Ahmed AB, Afshari A, et al. Management of severe perioperative bleeding: guidelines from the European Society of Anaesthesiology: First update 2016. Eur J Anaesthesiol. 2017;34:332–95. https://doi.org/10.1097/EJA.0000000000000630.
Raphael J, Mazer CD, Subramani S, et al. Society of Cardiovascular Anesthesiologists clinical practice improvement advisory for management of perioperative bleeding and hemostasis in cardiac surgery patients. Anesth Analg. 2019;129:1209–21. https://doi.org/10.1213/ANE.0000000000004355.
Aboul-Hassan SS, Stankowski T, Marczak J, et al. The use of preoperative aspirin in cardiac surgery: a systematic review and meta-analysis. J Card Surg. 2017;32:758–74. https://doi.org/10.1111/jocs.13250.
Myles PS, Smith JA, Forbes A, et al. Stopping vs. continuing aspirin before coronary artery surgery. N Engl J Med. 2016;374:728–37. https://doi.org/10.1056/NEJMoa1507688.
Myles PS, Smith JA, Kasza J, et al. Aspirin in coronary artery surgery: 1-year results of the Aspirin and Tranexamic Acid for Coronary Artery Surgery trial. J Thorac Cardiovasc Surg. 2019;157:633–40. https://doi.org/10.1016/j.jtcvs.2018.08.114.
Morici N, Moja L, Rosato V, et al. Time from adenosine di-phosphate receptor antagonist discontinuation to coronary bypass surgery in patients with acute coronary syndrome: meta-analysis and meta-regression. Int J Cardiol. 2013;168:1955–64. https://doi.org/10.1016/j.ijcard.2012.12.087.
Nijjer SS, Watson G, Athanasiou T, Malik IS. Safety of clopidogrel being continued until the time of coronary artery bypass grafting in patients with acute coronary syndrome: a meta-analysis of 34 studies. Eur Heart J. 2011;32:2970–88. https://doi.org/10.1093/eurheartj/ehr151.
Siller-Matula JM, Petre A, Delle-Karth G, et al. Impact of preoperative use of P2Y12 receptor inhibitors on clinical outcomes in cardiac and non-cardiac surgery: a systematic review and meta-analysis. Eur Heart J Acute Cardiovasc Care. 2017;6:753–70. https://doi.org/10.1177/2048872615585516.
Vuilliomenet T, Gebhard C, Bizzozero C, et al. Discontinuation of dual antiplatelet therapy and bleeding in intensive care in patients undergoing urgent coronary artery bypass grafting: a retrospective analysis. Interact Cardiovasc Thorac Surg. 2019;28:665–73. https://doi.org/10.1093/icvts/ivy330.
Siller-Matula JM, Trenk D, Schror K, et al. How to improve the concept of individualised antiplatelet therapy with P2Y12 receptor inhibitors - is an algorithm the answer? Thromb Haemost. 2015;113:37–52. https://doi.org/10.1160/TH14-03-0238.
Rossini R, Masiero G, Fruttero C, et al. Antiplatelet therapy with cangrelor in patients undergoing surgery after coronary stent implantation: a real-world bridging protocol experience. TH Open. 2020;4:e437–e45. https://doi.org/10.1055/s-0040-1721504.
Bhatt DL, Pollack CV, Weitz JI, et al. Antibody-based ticagrelor reversal agent in healthy volunteers. N Engl J Med. 2019;380:1825–33. https://doi.org/10.1056/NEJMoa1901778.
Mahla E, Suarez TA, Bliden KP, et al. Platelet function measurement-based strategy to reduce bleeding and waiting time in clopidogrel-treated patients undergoing coronary artery bypass graft surgery: The timing based on platelet function strategy to reduce clopidogrel-associated bleeding related to CABG (TARGET-CABG) study. Circ Cardiovasc Interv. 2012;5:261–9. https://doi.org/10.1161/CIRCINTERVENTIONS.111.967208.
Mannacio V, Meier P, Antignano A, Di Tommaso L, De Amicis V, Vosa C. Individualized strategy for clopidogrel suspension in patients undergoing off-pump coronary surgery for acute coronary syndrome: a case-control study. J Thorac Cardiovasc Surg. 2014;148:1299–306. https://doi.org/10.1016/j.jtcvs.2013.12.011.
Williams B, Henderson RA, Reformato VS, Pham T, Taylor BS, Tanaka KA. Hemostasis management of patients undergoing emergency cardiac surgery after ticagrelor loading. J Cardiothorac Vasc Anesth. 2020;34:168–74. https://doi.org/10.1053/j.jvca.2019.06.028.
Acknowledgements
The authors thank Allison Dwileski, B.S., Clinic for Anaesthesiology, Intermediate Care, Prehospital Emergency Medicine, and Pain Therapy, University Hospital Basel, Switzerland, for editorial assistance.
Funding
Open access funding provided by University of Basel.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
There are no conflicts of interest to declare.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Blood Management
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Moster, M., Bolliger, D. Perioperative Guidelines on Antiplatelet and Anticoagulant Agents: 2022 Update. Curr Anesthesiol Rep 12, 286–296 (2022). https://doi.org/10.1007/s40140-021-00511-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40140-021-00511-z