Abstract
This article presents a brief history of the Jefferson Empathy Project, provides a definition of clinical empathy, and describes the Jefferson Scale of Empathy (JSE), the most frequently used instrument for measuring clinical empathy in health professions students and healthcare practitioners. Also, we highlight selected empirical findings from our team and other national and international researchers on correlates of clinical empathy showing significantly positive associations between scores on the JSE and measures of personal qualities that are conducive to relationship building. Findings include group differences on the JSE scores by gender, race/ethnicity, academic background, specialty interest, and clinical competence, as well as empirical findings on erosion and enhancement of clinical empathy in health professions students and practitioners. Additionally, significant associations are reported between physicians’ scores on the JSE, and pertinent/tangible healthcare outcomes in diabetic patients in the U.S. and Italy; plausible explanations are offered for psychosocial and neurobiological mechanisms possibly involved in the link between physician empathy and healthcare outcomes. These findings suggest that empathy must be placed in the realm of evidence-based medicine, considered an essential element of overall professional competence, assessed for admission decisions to medical schools and postgraduate training programs, and incorporated into professional development of all health professionals-in-training and in-practice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
To be understood is a basic human need that can be fulfilled when an empathic connection is formed.
Hojat [2, p. 77].
1 History of the Jefferson Empathy Project
The Jefferson Empathy Project, an offshoot of the Jefferson Longitudinal Study of Medical Education [1] was initiated at the turn of this century in an academic medical center: Asano-Gonnella Center for Research in Medical Education and Health Care, at Sidney Kimmel (formerly Jefferson) Medical College of Thomas Jefferson University. The project initially was supported, in part, by a modest grant (to MH) from Pfizer Medical Humanities Initiative to study personal qualities of physicians-in-training and in-practice that are associated with clinical competence and healthcare outcomes. We did not expect that such a modest grant could lead to such a huge, productive, and influential project in medical education research.
At the initiation of the Jefferson Empathy Project, professionalism in medicine was emerging as a hot topic in medical education and the practice of medicine. Several factors contributed to the shift of attention toward professionalism in medical education and patient care. For example, a concern was growing about over-reliance on computer-based diagnostic and therapeutic technology that could limit students’ and practitioners’ vision of the importance of human connection in patient care [2]. Also, increasing healthcare costs and a trend toward market-driven medical care contributed to the eroding public image of physicians, leading to a benign neglect of the importance of the human factor in patient care. This chain of events led to a trend that prompted a paradigm shift in medical education and the practice of medicine. Training empathic physicians to reclaim the altruistic image of caring doctors of the good old days and regaining the reputation of medicine as a caring profession appeared to gain a renewed momentum along with the emergence of professionalism in medicine.
An extensive review of the literature to learn more about professionalism did not uncover a workable conceptualization of professionalism in medicine; thus, based on our literature review, we conceptualized professionalism as arrays of personal qualities—beyond acquisition of factual and medical knowledge and different from procedural skills—that contribute to physician competence and healthcare outcomes [3]. Also, in our literature search, as we learned more about professionalism in medicine, we noticed that empathy was a frequently mentioned core element of professionalism [3]. However, we were unable to find a workable definition of empathy in the context of patient care. We also could not locate a content-specific and context-relevant instrument to measure empathy in that context. Obviously, no credible empirical research could be undertaken without an operational definition of the concept and a psychometrically sound instrument to measure it. The historical ambiguity associated with the term clinical empathy, the lack of a valid and reliable instrument to measure it, as well as a dearth of empirical research on the topic prompted us to embark on a journey to an uncharted terrain of empathy in the context of patient care (clinical empathy). To fill those needs, we initiated the Jefferson Empathy Project.
2 Purposes of this article
This article was prepared to present a brief history of the Jefferson Empathy Project and summarize our clinical empathy research achievements and accomplishments at national and international levels. We present our definition of clinical empathy and briefly describe the Jefferson Scale of Empathy (JSE), a well-known, valid, and reliable instrument to measure clinical empathy in all health professions students and practitioners. We also present highlights of selected findings from our own research as well as from other national and international researchers on correlates of clinical empathy, group differences on clinical empathy, and healthcare outcomes associated with empathy in patient care. In addition, we report findings from empirical research on erosion of clinical empathy in physicians-in-training, and experimental results of enhancing empathy in physicians in-training and in-practice.
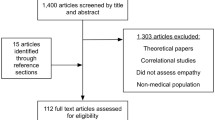
3 Research sources
This article encompasses some of our published findings and those of other national and international researchers, mostly using the JSE as a measure of clinical empathy. We report some of the findings from the nationwide Project in Osteopathic Medical Education and Empathy (POMEE) which is a landmark project in which large national samples of osteopathic medical students in the U.S. participated. The project was supported by national professional medical organizations, such as the American Association of Colleges of Osteopathic Medicine (AACOM), American Osteopathic Association (AOA) in collaboration with the Cleveland Clinic, and Sidney Kimmel Medical College of Thomas Jefferson University. One of us (MH) served as the principal investigator of the project, and our team at Jefferson contributed to the development of the study design, study survey, execution of the project, data analyses, and reports of the results.
The unique features of POMEE included using large national samples of osteopathic medical students (N = 10,751) [4] representing students in all years of medical school education, using a validated measure of clinical empathy (JSE), and providing statistical control for good impression response bias [4,5,6,7,8] to mitigate the social desirability response tendency in self-reported personality tests (respondents’ tendency, intentionally or unintentionally, to show themselves in a socially acceptable light) [9]. To our knowledge, these features of POMEE are unique in medical education research and contributed significantly to improving the internal validity (true relationship among study variables) and external validity (generalizability of the findings). These features add substantially to our confidence about the validity, utility, reproducibility, and generalizability of the findings. Incidentally, one of the publications from the POMEE on national norms for the JSE for osteopathic medical students, [7] was recognized by the American Osteopathic Association House of Delegate as the 2020 recipient of the George W. Northup, DO, Medical Writing Award.
4 Definition of clinical empathy
Clinical empathy is the heart of the art of patient care [4]. It has been described as the most frequently mentioned personal quality of the humanistic physician [10]. Despite a dearth of empirical research, empathy has received considerable attention in public media, academia, national and international politics, business, arts, ethics, and particularly in health professions education and patient care [11, 12]. In particular, attention to clinical empathy has recently increased in the era of the COVID pandemic [13].
Based on our comprehensive review of relevant literature in search of conceptualization of clinical empathy, we adapted the following definition of clinical empathy as:
“a predominantly cognitive (rather than an affective or emotional) attribute (brain mechanism) that involves an understanding (rather than feeling) of the patient’s pain and suffering, combined with a capacity to communicate this understanding (behavioral component), and an intention to help (outcome component)” [2, 4, 5, 14, 15].
The key terms in this definition are shown in italics to underscore their importance in the construct of clinical empathy. In this definition, we deliberately made a distinction between clinical empathy and emotional empathy (synonymous to sympathy, defined as a predominantly an emotional reaction to patient’s pain and suffering) [2, 16] (see Table 1). This distinction is important in patient care because clinical empathy and emotional empathy (sympathy) in our view have different consequences in healthcare outcomes [2, pp. 3–16, 71–81, 16].
A distinction between cognitively defined clinical empathy (most likely processed in the cortical areas of the brain by mechanism of understanding) and emotionally defined empathy or sympathy (most likely processed in the midbrain, limbic system, by mechanism of affect/emotion) may not be as important in social psychology, the bedrock of empathy research, as it is in the context of patient care [2]. In our view, cognitive empathy in abundance, in patient care is always beneficial and can lead to strong trusting relationships; thus, more accurate diagnosis, greater compliance, and consequently more optimal healthcare outcomes [2, 16]. However, because of the affective nature of emotional empathy, its overabundance can be overwhelming and thus, detrimental to patient care, leading to emotional exhaustion and burnout in the clinician and unregulated emotional dependency in both the patient and clinician that could easily interfere with objective clinical decision making [2, 16]. Table 1 depicts some of the differences between cognitive empathy and emotional empathy (sympathy) in patient care.
We maintain that the relationship between emotional empathy and patient outcomes is likely to be curvilinear (e.g., inverted U shape), similar to that between anxiety and performance [2, p.14], meaning that a limited amount of emotional empathy can help; however, overabundance of it can hamper by disrupting rational clinical decision making—the tyranny of emotion over reason!
5 Measurement of clinical empathy
Prior to the development of the JSE, no psychometrically sound instrument was available for measuring clinical empathy in the health professions education and patient care. Several empathy-measuring instruments, including the Interpersonal Reactivity Index [17]; the Empathy Scale [18]; the Emotional Empathy Scale [19], and other instruments were available and used by medical education researchers [2, pp.57–68]. However, these and most other empathy-measuring instruments were developed for administration to the general population. None was specific enough to capture the essence of clinical empathy in the context of health professions education and patient care [2, 20]. These instruments lacked “face” and “content” validity for measuring clinical empathy [2, 21, 22]. There was a need for a content-specific and context-relevant instrument for measuring clinical empathy. In response to that need, the JSE was developed by MH [2, 14, 15].
The JSE is a brief (20-item) instrument developed for administration to not only medical students and physicians, but also to all other health professions students and practitioners. Items are answered on a 7-point Likert-type scale (1 = Strongly Disagree, 7 = Strongly Agree). Half of the items are positively worded and directly scored, and the other half are negatively worded (reverse scored). Such negatively-worded, reversely scored items in self-reported personality tests are used to mitigate the effect of a response pattern known as the “acquiescence” response bias [23]—a tendency to constantly agree or disagree with test items; in the sociopolitical context, individuals with this tendency are called “yea-sayers” or “nay-sayers”. It takes approximately 5 min to complete the JSE.
Three versions of the JSE are available. One version was developed for administration to medical students (S-Version). The second version was developed for administration to all practicing health professionals, including physicians, nurses, dentists, pharmacologists, clinical psychologists, and other clinicians involved with patient care (HP-Version). The third version was developed for administration to all health professions students other than medical students (HPS-Version). All three versions are very similar in content with only minor differences in a few words to make the items more appropriate for the target population [2, pp. 83–127].
The JSE has been recognized as the most researched and widely used instrument in medical education research [24] and as the most frequently used instrument for measuring empathy in medical students [25]. A recent review of research on empathy in health care [26], reported that the JSE is the most frequently used measure of clinical empathy in healthcare research; however, that review article failed to include our key articles on psychometrics of the JSE [5, 14, 15, 27], intervention to enhance empathy in medical students [28] and particularly our findings on physician empathy as predictor of healthcare outcomes [29, 30].
The JSE has been translated into 59 languages, used in more than 88 countries. Abundant evidence has been reported in samples of health professions students and practitioners to support the psychometrics of the JSE by researchers in the U.S. and abroad [2, pp.84–128, 276–286, 5]. National norm tables are available for the U.S. osteopathic medical students by gender and medical school year [5, 7] and tentative norms and cutoff scores are also reported for a large sample of students in allopathic (MD-granting) medical schools [27]. We have assembled a list of 479 publications (as of January 2023) by national and international researchers in peer-reviewed English language journals, (a list of these publications is posted on the following link): https://www.jefferson.edu/content/dam/academic/skmc/crmehc/Bibliography_Natl-Intl%20researchers_4.5.2022.pdf The link below contains 57 articles which were coauthored by MH, where either psychometrics of the JSE were addressed, or the JSE was used: https://www.jefferson.edu/content/dam/academic/skmc/crmehc/Bibliography_Hojat%20et%20al._10.2.20.pdf.
6 Correlates of clinical empathy
Numerous empirical studies have reported associations between scores of the JSE and several pertinent variables, including personal qualities, academic performance, clinical competence, demographics, career interest, and healthcare outcomes.
In the first preliminary study on psychometrics of the JSE in medical students and internal medicine residents published in 2001 [14], we reported statistically significant correlations of moderate magnitude between JSE scores and the following variables: self-reported measures of Compassion and Sympathy [14], scores on the Empathic Concern and Perspective Taking scales of the Interpersonal Reactivity Index, [14, 17] and personality facets of Warmth and Dutifulness of the NEO PI-R [31]. In another study with internal medicine residents [32], significant correlations were found between JSE scores and Perspective Taking, Empathic Concern, and Fantasy scales of the IRI, but not with the Personal Distress scale of the IRI, which is not conceptually relevant to empathy in patient care. Similar findings were reported by Costa and colleagues [33] with samples of medical students from five countries using different translated versions of the JSE.
In a study with medical students in the U.S. [34], higher scores on the JSE were associated with higher scores on a measure of Sociability. Scores of the JSE have also been linked to “Big Five” personality factors such as Agreeableness, Openness to Experience, Conscientiousness, and Extraversion in medical students in Portugal [35]. These findings provide support for criterion-related validity of the JSE.
In a study with third-year medical students in the U.S., positive associations were found between scores of the JSE and measures of optimism and personal accomplishment [36]. In another study with 1805 new matriculants at Sidney Kimmel Medical College, a computerized form of linguistic content analysis was applied to medical school admissions essays [37]. The purpose was to identify the words that were frequently used by medical students in their admissions essays and to examine their associations with students’ scores on the JSE administered at the beginning of medical school education. Results showed that the top three words associated with scores on self-reported clinical empathy were “health,” “patient,” and “care.” The extracted topics from linguistic content analysis consisted of words associated with key features of clinical empathy, such as “empathy,” “understanding,” “compassion,” “caring,” “perspective,” and “trust” [37].
In a study with osteopathic medical students, statistically significant positive correlations were found between scores of the JSE, measures of attitudes toward interprofessional collaboration, and orientation toward an integrative approach to patient care [38]. In a multi-institutional study involving five medical schools in the U.S., students who reported higher exposure to humanities (e.g., engaging in visual arts, singing, playing musical instruments, listening to music, dancing, writing for pleasure, attending theater, visiting museums/galleries) obtained significantly higher scores on the JSE [39].
Empirical research on association between empathy and age is rare. In our own research, we did not find a significant correlation between scores of the JSE and age in health professions students [2, 4], which was also confirmed in studies by some other researchers [40].The lack of significant association between JSE scores and age in health professions students could be an artifact of the “restriction of range” in students’ ages, which does not allow the corresponding correlation to capture its full magnitude [4].
6.1 Clinical empathy and qualities conducive to relationship building
Empirical evidence in studies with health professions students and practitioners showed that scores on a number of personal qualities, conducive to relationship building, were positively correlated with JSE scores, including emotional intelligence [41,42,43]; cooperativeness [44]; desirable professional behavior [45]; positive attitudes toward patient-centered care and orientation toward integrative patient care [38]; patients’ communication experiences with physicians [46]; optimism [36]; and positive social influence measured by peer nomination of students who were recognized by their peers as having positive social influence on classmates in medical school, thus inclined to be potential leaders in medicine [47]. Those students who were recognized by their classmates as excellent in clinical skills and humanistic attributes scored significantly higher on the JSE than those who were not nominated [48]. Furthermore, the peer nomination used in the aforementioned studies holds promise as a robust method of assessment of personal qualities that is free from social desirability response bias, a limitation of self-reported personality tests.
The JSE scores were significantly associated with orientation toward teamwork and interprofessional collaboration in a study with allopathic medical students [49], osteopathic medical students [50], nursing students [51], and pharmacy students [52]. Resiliency against burnout measured by scores on the Personal Accomplishment components in the Maslach Burnout Inventory [53] was positively associated with the JSE scores in medical students [36, 45].
In a study with pharmacy students in Korea [54], a negative correlation was reported between scores on Maslach Burnout Inventory and JSE scores. In that study [54], scores on the JSE were significantly and positively correlated with scores on measures of psychological well-being and satisfaction with psychological needs [54]. Also, in a study by LaNoue and Roter [55], significant associations were found between the JSE scores in third-year medical students and assessments of empathic communication patterns with standardized patients measured by the Roter Interactional Analysis System [56]. In a nationwide study of U.S. osteopathic medical students [8], we found significant correlations between scores of the JSE and positive attitudes toward osteopathic medicine, including the factor of “holistic and integrative care,” a tenet of osteopathic medicine [57, 58].
6.2 Clinical empathy and qualities detrimental to interpersonal relationships and clinician well-being
Conversely, in other studies, scores of the JSE yielded negative correlations with personality attributes that are detrimental to interpersonal relationships, such as measures of aggression-hostility [34, 59]. In a study with Chinese nursing students [60], an inverse relationship was found between the JSE scores and scores of the Neuroticism scale of the Eysenck Personality Questionnaire [61]. A hypothesis that medical students who use psychostimulant drug for non-medical reasons exhibit lower clinical empathy scores than nonusers was not confirmed in a study with medical students [62]; however, psychostimulant drugs users obtained significantly higher average scores on the measure of aggression-hostility of the Zuckerman-Kuhlman Personality Questionnaire [63], which was inversely associated with JSE scores in another study [33]. Also, high scores on indicators of burnout such as Depersonalization and Emotional Exhaustion [53] were associated with lower scores on the JSE [36, 45, 64, 65].
Some researchers, using empathy-measuring instruments other than the JSE reported a positive association between empathy and burnout experiences [66], meaning ironically that higher empathy leads to more experiences of burnout. These studies made no distinction between cognitive and emotional empathy; thus, supporting the unverified assumptions that empathic engagement in patient care can lead to “compassion fatigue,” or a “secondary traumatic stress disorder,” and burnout advanced by Figley [67] who claimed, without presenting empirical evidence, that “Those who have enormous capacity for feeling and expressing tend to be more at risk of compassion stress” [67, p.1]. In his book “Against Empathy” [68], Bloom who also did not acknowledge the consequential differences between cognitive empathy and emotional empathy [16], or between understanding and feeling, oddly concluded that “empathy is a negative in human affairs. It’s sugary soda, tempting and delicious and bad for us” [68, p. 13]. However, based on the finding that the emotional exhaustion factor of burnout [53] is in the opposite pole of the JSE scores factor [35], we expect to find an inverse association between cognitively defined clinical empathy (measured by the JSE) and indicators of burnout experiences, and a positive association between a measure of emotional empathy and burnout. This expectation was indeed confirmed in a study in which it was reported that a cognitive empathy measure, as opposed to emotional empathy, significantly predicted a lower degree of burnout and stronger mental resilience in medical students [69].
7 Academic performance and clinical competence
In a study of third-year medical students [70], a statistically significant association was found between students’ JSE scores and medical school faculty’s global ratings of students’ clinical competence in six core clerkships (family medicine, internal medicine, obstetrics and gynecology, pediatrics, psychiatry, and surgery). Also, significant associations were observed between students’ JSE scores and ratings of clinical competence given by standardized patients in 10 Objective Structured Clinical Examination (OSCE) stations [71, 72].
We must add that we found no significant correlations between scores of the JSE and grades on objective examinations of acquisition of medical knowledge in medical students (e.g., MCAT scores, medical school first- and second-year GPA’s, and scores on medical licensing examinations (Steps 1 and 2 of the USMLE) [70]), indicating that scores on objective examinations of acquisition of knowledge are likely not to be significantly associated with JSE scores.
8 Clinical empathy in contrasted groups
We compared contrasted groups to examine if differences in the JSE scores between the groups are in the expected direction. The expectations are based on previous research, theories, and behavioral inclinations described in the literature [2, p.111]. Indeed, psychometricians use the method of contrasted groups to provide support for the validity of a measuring instrument [2, p. 111].
8.1 Gender difference in clinical empathy
Some have suggested that women’s behavioral style is generally more “empathizing” than men [73]. Indeed, in a majority of studies in the U.S. and abroad, female health professions students and practicing clinicians obtained significantly higher JSE mean scores than their male counterparts [4, 14, 15, 40, 70, 74, 75]. In a large-scale study of 11 entering classes of students at Sidney Kimmel Medical College, women’s JSE mean scores were higher than men’s in all classes, and the gender differences were statistically significant for 10 out of the 11 classes [76]. Several plausible explanations have been given for gender differences in empathy in favor of women, including social learning, genetic predisposition, evolutionary underpinnings, and other factors [2, pp.169–187].
8.2 Race/Ethnic differences in clinical empathy
Empirical research on the association between empathy and race/ethnicity in health professions students and practitioners is scarce. A reason for such limited research may be a lack of sufficient number of students or practitioners from underrepresented minority and ethnic groups in the study samples from single academic institutions to allow meaningful comparisons.
In a study with medical students, an inconsistency was observed between Asian and White students in their JSE scores and standardized patients’ assessments of students’ empathy [71]. In a multi-institutional study with medical students, African-American students, on average, obtained significantly higher scores on the JSE than their White/Caucasian and Asian/Pacific Islander counterparts [72]. However, despite their high scores on the JSE, male African-American students obtained the lowest ratings on the Scale of Patient Perception of Physician Empathy [77], given by standardized patients [72]. The discrepancy between students’ self-reported empathy and ratings of students’ empathy given by standardized patients could raise a question about possible ethnicity bias, or testing fairness in the assessment of African-American students’ clinical skills by standardized patients [72]. By contrast, in a study with nursing students, no significant association was found between race/ethnicity (comparing White, African-American, and Asian students) and scores on the JSE [51].
In our nationwide study of osteopathic medical students (POMEE), the highest JSE mean score was obtained by African-American students, followed by students who identified themselves as Latinx and White/Caucasian, and the lowest JSE mean score was obtained by Asian students [4]. The higher JSE scores in the underrepresented African-American and Latinx groups may be explained by the notion of the “wounded healer effect” [78] which suggests that those who have experienced discrimination and suffering can better understand the suffering of others by sharing common experiences [6].
8.3 Clinical empathy and academic background
Empirical research on clinical empathy and academic background is scarce. The nationwide POMEE research provided a unique opportunity to examine associations between clinical empathy and medical students’ academic background (undergraduate major). Significant differences in the JSE scores were found in favor of those with academic backgrounds in “social and behavioral sciences” and “arts and humanities” in the preclinical phase of medical school education [4]. However, the differences became nonsignificant in the clinical phase of medical school education. The inconsistent pattern of findings on associations between academic background and clinical empathy in the preclinical and clinical phases of medical school education suggests that the effects of academic background on clinical empathy in medical school may last only during the early years of medical school education [4]. In a study with nursing students, no significant association was found between academic background (in humanities, sciences, and business) and scores of the JSE [51].
8.4 Clinical empathy and volunteerism
In a study with medical students, those who volunteered to participate in student-run free clinics to provide healthcare services to indigent and underserved patients were compared with their non-volunteering classmates on their JSE scores. Findings showed that the JSE scores of non-volunteers tend to decline in medical school, but no such erosion in clinical empathy was observed in the volunteer group [79]. Another study observed medical students who volunteered to participate in a program, called “No One Dies Alone” providing compassionate companionship at the bedside of lonely dying patents by simply sitting at the patients’ bedside; holding patients’ hands; rendering therapeutic touch; playing music; and reading books, stories, poetry aloud. Scores on the JSE (administered prior to the experiment) of volunteer students compared to those of non-volunteer classmates, showed that those who volunteered to participate in the program, regardless of whether they had the opportunity to visit a dying patient or not (due to scheduling conflict such as unavailability of patients in students’ free time) obtained higher mean scores on the JSE than their non-volunteering classmates [80]. This suggest that students’ willingness to render compassionate care to terminally ill patients in itself is an indication of empathic inclination in patient care.
8.5 Clinical empathy and career interest
Bailey [81] reported that medical students who planned to pursue a career in specialties requiring extensive and prolonged encounters with patients received significantly higher scores on empathy measured by the IRI [17] than their counterparts who planned to pursue procedure-oriented specialties. Given these findings, we expected that high scorers on the JSE are more inclined to choose specialties that require continuous and prolonged encounters with patients. These specialties are described as “people-oriented,” such as primary care specialties (general internal medicine, family medicine, and pediatrics) and psychiatry. Conversely, we expected that low scorers on the JSE would be more interested in specialties that require less interaction with patients and often involve performing diagnostic or therapeutic procedures. These specialties are described as “technology/procedure-oriented,” such as hospital-based specialties (pathology, radiology, and anesthesiology), urology, surgery, and surgical subspecialties.
The aforementioned expectations were confirmed in a number of studies. For example, physicians in the “people-oriented” specialties scored higher on the JSE compared to others in “technology/procedure-oriented” specialties [15, 82], consistent with findings reported by others researchers in the U.S. and abroad [83,84,85,86].
In other studies by our research team with first-year medical students, we administered the JSE at the beginning of medical school before students were exposed to formal medical education [34, 70]. Findings showed a significant association between JSE scores and specialty interest in favor of those who were planning to pursue “people-oriented” specialties after graduation from medical school. This finding suggests that most medical school matriculants who are interested to pursue “people-oriented” specialties after completing their medical school are more likely than others who expressed an interest to pursue “technology/procedure-oriented” specialties to possess a baseline personality attribute (reflected in their higher JSE scores) that prompts them to choose “people-oriented” specialties before being exposed to formal medical education.
Interestingly, the pattern of malpractice claims for physicians who practice in different specialties is consistent with our research findings on the JSE scores, so that those practicing in “people-oriented” specialties were less likely charged with malpractice litigation than those in the “procedure/technology-oriented” specialties [87]. However, such associations between specialty interest and JSE scores were not observed in osteopathic medical students [50, 88].
9 Erosion of clinical empathy in physicians-in-training
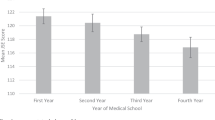
Despite the importance of enhancing clinical empathy in medical education and patient care, our empirical research and some other studies, particularly in the U.S., suggest that empathy tends to erode as students progress through medical school [2, 89,90,91]. Decline in empathy during the clinical phase of medical education was first noticed in a longitudinal study by our team in 2004 [89] in which the JSE was administered at the beginning and the end of the third year of medical school.
A second large-scale longitudinal study of erosion in empathy was also undertaken by our research team in 2009 [90], in which three cohorts of medical students were followed up throughout medical school from orientation to graduation dates, completing the JSE five times during medical school education at the orientation and at the end of each year of medical school. The findings confirmed the erosion of clinical empathy in all three cohorts starting in the third year of medical school when medical education curriculum (in the U.S.) shifts from the pre-clinical to clinical phase of medical school education; ironically at a time when empathy is most needed because of an increase in patient contact [90]. This was aptly reflected in the title of that publication: “Devil is in the third year” [90]. This study received broad media attention. A similar pattern of decline of empathy, using the JSE was also observed in nursing students after experiencing patient encounters [92] and in dentistry school students as they progressed through dental school [93] started when dental students began working with patients.
A few cross-sectional studies on changes in empathy scores in osteopathic medical students have reported no significant decline in empathy by year of schooling [50, 88, 94]. A recent single-institution study with osteopathic medical students by Rizkalla and Henderson [95] reported a decline in JSE scores in the clinical phase of medical school, but the magnitude of decline was negligible. In the nationwide cross-sectional study of decline in empathy in osteopathic medical students in the U.S. (POMEE), a statistically significant decline in the JSE scores was observed in the clinical phase of medical school education; however, the magnitude of the decline was negligible [6]. Comparison of findings with those from allopathic medical schools showed that while the pattern of decline in clinical empathy scores was similar, the magnitude of erosion was less pronounced in osteopathic medical students [6].
Currently, there is an ongoing nationwide longitudinal study of osteopathic medical students in the U.S. (POMEE-Phase II) to examine changes in clinical and emotional empathy (synonymous to sympathy) by following a large cohort of osteopathic students (entering class of 2019) as they progress through medical school from orientation to graduation. Reasons for such changes are also planned to be explored in this large-scale study. Results will be reported in due course.
An interesting finding on decline in empathy was reported in a couple of studies [96, 97], in which decline in empathy was more noticeable when the JSE was used. For example, Smith and colleagues [96] used two empathy-measuring instruments: the JSE, and the Questionnaire of Cognitive and Affective Empathy (QCAE) [98] which is not a content specific-context relevant instrument with regard to patient care. These investigators [96] found significant decline in scores of the JSE but not in scores of the QCAE. We attributed these controversial findings to the sensitivity of the JSE in detecting changes in empathic orientation toward patient care in physicians-in-training and in-practice [22].
Because of differences in the osteopathic and allopathic philosophies and medical education systems, differences in the pattern and magnitude of changes in empathy among osteopathic and allopathic medical students were expected. For example, osteopathic philosophy’s emphasis on provision of holistic care; hands-on approaches to diagnosis and treatment; and patient-centered, integrative and collaborative care [6, 8] could result in a different pattern of development of empathic orientation in patient care in osteopathic compared to allopathic medical students [6, 8, 99]. In addition, one may speculate that the educational goals in osteopathic medical education regarding the importance of developing humanistic behavior, compassionate treatment, altruism, and empathy [8, 58]—which are conducive to empathic orientation—may reveal a different pattern and degree of changes in empathy among osteopathic medical students [6].
A few review articles examined the issue of changes in empathy in physicians-in-training and other health professions students in the U.S. and abroad. For example, Colliver and his colleague [100] reviewed 11 studies (6 with medical students, 1 with dental students, and 4 with residents) and concluded that the decline of empathy during medical education has been greatly exaggerated. However, such a claim was not left unchallenged by us [101].
By contrast, Neumann and colleagues [91] reviewed 18 articles (11 with medical students, and 7 with residents), and concluded that empathy declined during medical education, particularly during clinical phase of medical education. Ferreira-Valente and colleagues [102] reviewed studies published in English, Spanish, Portuguese, and French between 2009 and 2016, and selected 20 studies that met their inclusion criteria. Based on the magnitude of effect size of changes (estimated by the reviewers from published data), they did not report a definitive conclusion about decline in empathy during medical school [102].
10 Enhancement of clinical empathy
Research suggests that clinical empathy can be taught and nurtured by targeted educational programs. Several approaches described elsewhere [2, pp. 217–233] have been used in health professions students and practitioners for enhancing empathy, including improving interpersonal skills; audio recording or visual recording encounters with patients; exposure to positive role models, role playing (such as an aging game); theatrical performances; patient navigator (such as shadowing a patient in hospitals, or emergency rooms, etc.); hospitalization experiences; the study of literature and the arts; exposure to humanities; improving narrative skills and reflective writing; the Balint method (meeting in small groups to discuss difficult cases to enhance understanding of patients’ experiences and concerns which is the backbone of clinical empathy); and other innovative techniques [2, pp.203–234, 103]. For example, we have tried the following approaches to enhance empathy in medical and other health professions students and practitioners:
In a two-phased experiment with medical students at Jefferson [28], medical students in the experimental group participated in a workshop to watch and discuss video clips of patient-physician encounters from commercial movies (e.g., The Doctor, Wit, First Do No Harm), while students in the control group watched a documentary film (phase 1). Ten weeks later in phase 2 of the study, students in the experimental group were divided into two groups; one group attended a lecture by one of us (MH) on empathy in patient care, and the other students in the experimental group, plus all students in the control group watched a biographical film: “Something the Lord Made” about racism. Results of phase 1 experiment showed a statistically significant enhancement on the JSE in the experimental compared to the control group. However, results of phase 2 showed that the improvement in the clinical empathy scores was sustained in the experimental group who attended the empathy lecture, but not in experimental group, who in phase 2, watched the biographical film. It was concluded that additional reinforcement is needed to sustain the improvement resulting from targeted educational program [28].
In another experiment, first-year medical and pharmacy students [104] at Chicago College of Osteopathic Medicine and Chicago College of Pharmacy of Midwestern University participated in a workshop to observe a 10-min play performed by their own classmates who were coached by one of us (MH) to enact problems and concerns faced by elderly people (e.g., aging games). Pretest and posttests comparisons of the JSE scores showed significant increase in clinical empathy scores immediately after the workshop. However, the increased empathy scores were not sustained for a longer time.
A six-year longitudinal study with medical students in Japan found that scores on the JSE improved significantly as a results of participation in a communication skills training program aimed to enhance clinical empathy; however, the improvement was temporary and did not have a sustained effect [105]. In another longitudinal study in Japan, medical students who participated in two programs to improve their interviewing skills by using the Humanitude exercise (a caring approach, involving comprehensive communication, focusing on perception, emotion, and speech) showed significantly improved scores on the JSE after each program. However, neither program showed a sustained effect [106].
In a study, first-year residents in emergency medicine were randomly divided into experimental and control groups [107]. Those in the experimental group were instructed to shadow a patient from triage until discharge, or for a maximum of 6 h, whichever came first. The control group followed a routine schedule without shadowing. Results showed that scores on the JSE did not decline in the experimental group; however, significant erosion of empathy scores was observed in the control group, indicating that erosion of empathy could be prevented by shadowing experiences [107].
In a study by LoSasso and colleagues [108], the effects were examined of an intervention on proper use of electronic medical records for improving medical students’ empathy and reducing communication hurdles in third-year medical students. Research participants were randomly divided into experimental and control groups. The experimental group received a one-hour training session on electronic medical records and specific communication skills. Both groups completed the JSE at the start and end of the clerkship. In addition, faculty and standardized patients rated students’ empathic engagement in standardized patient encounters by completing the Jefferson Scale of Patient Perceptions of Physician Empathy JSPPPE [77]. Ratings given by faculty on the JSPPPE increased significantly, but marginally increased in ratings given by standardized patients (p = 0.07) in the experimental group compared to the control group. Also, scores on the JSE obtained by students in the experimental groups were slightly higher than those in the control group, but the difference was not statistically significant [108]. In a faculty development workshop at the Cleveland Clinic, physicians participated in a narrative medicine workshop engaging in guided reflective writing [109]. Results suggested an improvement in empathy in the experimental group.
11 Health outcomes
The litmus test for the validity and utility of an instrument for measuring clinical empathy is empirical evidence to show significant links between physicians’ scores on clinical empathy and pertinent indicators of healthcare outcomes [21].
One of the earliest studies on empathy and health outcomes was undertaken by Rakel and colleagues [110] who examined physician empathy, as reported by 350 patients with the common cold. Patients completed the Consultation and Relational Empathy (CARE) developed by Mercer and Reynolds [111] for the purpose of assessing physician–patient empathic interactions. Results showed that patients who assigned the highest possible ratings to their physicians on the CARE had a shorter duration and less severity of symptoms.
In more recent empirical studies, our team found significant associations between physicians’ scores on the JSE and objective/tangible health outcomes in two studies, one in the U.S. and the other in Italy. In the U.S. study [29], electronic records of 891 adult patients with type 2 diabetes mellitus treated by one of 29 family physicians were examined, and the results of the most recent tests for hemoglobin A1c and low-density lipoprotein cholesterol (LDL-C) were extracted. Objective/tangible positive healthcare outcomes were considered as indicators of good control of the disease progression reflected in A1c test results (< 7.0%) and LDL-C (< 100). Findings showed that physicians’ scores on the JSE could significantly predict these healthcare outcomes in diabetic patients.
Patients of physicians with high JSE scores (top third scorers, JSE > 128) were significantly more likely to have good control of their disease than patients of physicians with low JSE scores (bottom third scorers, JSE < 117). Results of multiple logistic regression analysis indicated that the associations between physicians’ JSE scores and patients’ healthcare outcomes remained statistically significant after controlling for physicians’ gender and age, as well as for patients’ gender, age, and type of health insurance [29].
Eight years after publication of the above above-mentioned study [29], a group of investigators at the Cleveland Clinic attempted to replicate the study [112], but found no association between physician empathy and health outcomes. However, we challenged their failure to reproduce our findings because of the following reasons: incompatibility in physician sample, differences in the case mix of patients, analytical dissimilarities, and confounding institutional factors [113].
In a second study on physician empathy and healthcare outcomes (at the Local Health Authority of Parma, Italy) [30], electronic records of 20,961 adult patients with types 1 and 2 diabetes mellitus treated by one of 242 primary care physicians were examined, and information on acute metabolic complications (e.g., diabetic ketoacidosis, coma, and hyperosmolar state) that required hospitalization were extracted from patients’ hospital discharge data. Results showed statistically significant associations between physicians’ higher scores on the JSE and lower rates of hospitalization due to the aforementioned acute metabolic complications. The associations remained statistically significant after controlling for physicians’ gender, age, type of practice (solo or group), geographical location of practice, and patients’ gender, age, and duration of time enrolled with the physician [30].
Similarities in the findings of these two studies (in the U.S. and Italy) on associations between physicians’ scores on the JSE and positive healthcare outcomes increase our confidence on generalization of the findings, given cultural differences in the two study samples, variation in medical education, differences between health insurance policies, and differences in the health care systems in the U.S. and Italy. To our knowledge, these two empirical studies on physician empathy and healthcare outcomes were the first published articles using a validated instrument for measuring clinical empathy in physicians, and tangible/objective health outcomes (as opposed to patients’ subjective assessments of their physicians). Both of these studies on physician empathy and healthcare outcomes [29, 30] received broad coverage in public media and posted on a large number of websites.
A more recent study in China [114], using patients with advanced prostate cancer, found that urologists’ clinical empathy scores (measured by the JSE) were negatively correlated with patients’ anxiety and stigma, and positively correlated with patient’s self-efficacy, and with the natural killer cells’ activities. It was concluded that physician empathy, through mediating roles of patients’ anxiety, stigma, and self-efficacy, contributed to improvement of patients’ immune cellular function (i,e., natural killer cells’ activities).
12 Mechanism linking clinical empathy to healthcare outcomes
Our definition of clinical empathy implies that empathic engagement in patient care revolves around communication, reciprocity, and mutual understanding, all of which pave the road to interpersonal attunement. Mechanisms involved in connecting clinical empathy and patient outcomes can be described by psychosocial factors and neurobiological responses that are usually evoked when interpersonal attunement is formed.
At the psychosocial level, interpersonal attunement, resulting from empathic engagement in patient care, lays the foundation for a trusting relationship between the clinician and the patient. Such a trusting relationship will diminish constraints in communication and inhibition in revealing illness narrative without concealment. All these mechanisms lead to achieving a more accurate diagnosis and a greater compliance.
At the neurobiological level, interpersonal attunement in empathic engagement is analogous to a synchronized dance between patient and clinician, which is orchestrated by the tune of neurobiological markers that are described in the “perception–action coupling” model formulated by Preston and deWall [115]. According to this model, perceptions of another person’s cognitive, emotional, and somatosensory states automatically activate representations of those states, unless prohibited [115]. In addition, the neurobiological stimulation in interpersonal attunement that is formed by empathic engagement can activate hormonal changes (e.g., oxytocin, vasopressin) [116] that influence the strength of empathic engagement.
A set of neurons, known as the mirror neuron system, is discharged [117, 118] that may play an important role in understanding of experiences of others which is the key ingredient of empathic engagement in patient care [119]. All of the aforementioned psychosocial and neurobiological activities can provide a plausible explanation of the mechanisms involved in linking empathic engagement in patient care and healthcare outcomes [119]. Figure 1 depicts the aforementioned pathways in connecting patient-clinician empathic engagement and healthcare outcomes. See Hojat [2, pp. 238–244] for more detailed explanations of mechanisms involved in pathways from patient-clinician empathic engagement to healthcare outcomes.
13 Concluding remarks
The empirical evidence presented in this article supports that empathic engagement in patient care is beneficial to the well-being of physicians-in-training, physicians-in-practice, and patients that results in improving healthcare outcomes. Therefore, we propose that clinical empathy must be considered as an essential element of the overall professional competence of clinicians; and in the assessment of applicants to medical schools and postgraduate training programs [120]; that must be integrated into professional development of all healthcare professionals-in-training and in-practice; and that to be placed in the realm of “evidence-based” medicine. We maintain that the assessment, enhancement, and sustaining of empathy in medical education should be considered a mandate that must be acted upon by leaders, faculty, and educators in all academic medical institutions [2].
Because of the importance of empathy in patient care, we suggested elsewhere [120] that for selection of applicants to medical schools (and postgraduate medical education programs), a measure of clinical empathy should be used as a supplementary criterion measure to screen for those who possess a higher propensity for empathic engagement and greater inclination to become caring physicians. Our overarching conclusion is that clinical empathy in patients care is a potent medicine without any adverse effect.
Data availability
Not applicable.
Code availability
Not applicable.
References
Gonnella JS, Callahan CA, Veloski JJ, DeSantis J, Hojat M. Fifty years of findings from the Jefferson Longitudinal Study of Medical Education. Switzerland: Springer; 2022. https://doi.org/10.1007/978-3-030-85379-2.
Hojat, M. Empathy in health professions education and patient care. New York: Springer International Publishing; 2016. www.springer.com/us/book/9783319276243
Veloski JJ, Hojat M. Measuring specific elements of professionalism: empathy, teamwork, and lifelong learning. In: Stern DT, editor. Measuring medical professionalism. Oxford: Oxford University Press; 2006. p. 117–45.
Hojat M, Shannon SC, DeSantis J, Shannon S, Speicher MR, Bragan L, Calabrese LH. Empathy as related to gender, age, race and ethnicity, academic background, and career interest: a nationwide study of osteopathic medical students in the United States. Med Educ. 2020;54:571–81. https://doi.org/10.1111/medu.14138.
Hojat M, DeSantis J, Shannon S, Mortensen LH, Speicher M, Bragan L, LaNoue M, Calabrese LH. The Jefferson Scale of Empathy: a nationwide study of measurement properties, underlying components, latent variable structure, and national norm in medical students. Adv Health Sci Educ Theory Pract. 2018;23:899–920. https://doi.org/10.1007/s10459-018-9839-9.
Hojat M, DeSantis J, Speicher M, Braga L, Calabrese L. Does empathy decline in the Clinical phase of medical education? A nationwide, multi-institutional, cross-sectional study of students at DO-granting medical schools. Acad Med. 2020;95:911–8. https://doi.org/10.1097/acm.0000000000003175.
Hojat M, Shannon S, DeSantis J, Speicher M, Bragan L, Calabrese L. National norms for the Jefferson Scale of Empathy: a nationwide project in osteopathic medical education and empathy (POMEE). J Am Osteopath Assoc. 2019;119:520–32. https://doi.org/10.7556/jaoa.2019.091.
Hojat M, DeSantis J, Cain R, Speicher M, Bragan L, Shannon S, Calabrese L. Attitudes toward osteopathic medicine scale: development, psychometrics. Int J Med Educ. 2021;12:222–32. https://doi.org/10.5116/ijme.615c.2cfa.
Edwards AL. The social desirability variable in personality assessment and research. New York: Dryden; 1957.
Linn LS, DiMatteo MR, Cope DW, Robbins A. Measuring physicians’ humanistic attitudes, values, and behaviors. Med Care. 1987;25:504–15. https://doi.org/10.1097/00005650-198706000-00005.
Coplan A. Understanding empathy: its features and effects. In: Coplan A, Goldie P, editors. Empathy: philosophical and psychological perspectives. New York: Oxford University Press; 2014. p. 3–8.
Matravers D. Empathy as a route to knowledge. In: Coplan A, Goldie P, editors. Empathy: philosophical and psychological perspectives. New York: Oxford University Press; 2014. p. 19–30.
Hojat M. Prepare for mental health aftershock. Philadelphia Inquirer: Monday, June 22, 2020: A9.
Hojat M, Mangione S, Nasca TJ, Cohen MJM, Gonnella JS, Erdmann JB, Veloksi JJ, Magee M. The Jefferson scale of physician empathy: development and preliminary psychometric data. Educ Psychol Meas. 2001;61:349–65. https://doi.org/10.1177/00131640121971158.
Hojat M, Gonnella JS, Nasca TJ, Mangione S, Vergare M, Magee M. Physician empathy: definition, components, measurement, and relationship to gender and specialty. Am J Psychiatry. 2002;159:1563–9. https://doi.org/10.1176/appi.ajp.159.9.1563.
Hojat M, Spandorfer J, Louis DZ, Gonnella JS. Empathic and sympathetic orientations toward patient care: conceptualization, measurement, and psychometrics. Acad Med. 2011;86:989–95. https://doi.org/10.1097/acm.0b013e31822203d8.
Davis MH. Measuring individual differences in empathy: evidence for a multidimensional approach. J Pers Soc Psychol. 1983;44:113–26. https://doi.org/10.1037/0022-3514.44.1.113.
Hogan R. Development of an empathy scale. J Consult Clin Psychol. 1969;33:307–16. https://doi.org/10.1037/h0027580.
Mehrabian A, Epstein NA. A measure of emotional empathy. J Pers. 1972;40:525–43. https://doi.org/10.1111/j.1467-6494.1972.tb00078.x.
Evans BJ, Stanley RO, Burrows GD. Measuring medical students’empathy skills. Br J Med Psychol. 1993;66:121–33. https://doi.org/10.1111/j.2044-8341.1993.tb01735.x.
Hojat M, Gonnella JS. What matters more about the Interpersonal Reactivity Index and the Jefferson Scale of Empathy? Their underlying constructs or their relationships with pertinent measures of clinical competence and patient outcomes [invited commentary]. Acad Med. 2017;92:743–5. https://doi.org/10.1097/acm.0000000000001424.
Hojat M. Changes in empathy in medical school [letter to the editor]. Med Educ. 2018;52:456–7. https://doi.org/10.1111/medu.13497.
Krosnick JA. Survey research. Annu Rev Psychol. 1999;50:537–67. https://doi.org/10.1146/annurev.psych.50.1.537.
Colliver JA, Conlee MJ, Verhulst SJ, Dorsey JK. Rebuttals to critics of studies of the decline on empathy. Acad Med. 2010;85(12):1813–4. https://doi.org/10.1097/acm.0b013e3181fa3576.
Sulzer SH, Feinstein NW, Wendland CL. Assessing empathy development in medical education: a systematic review. Med Educ. 2016;50:300–10. https://doi.org/10.1111/medu.12806.
Nembhard IM, David G, Ezzeddin I, Betts D, Radin J. A systematic review of research on empathy in health care. Health Serv Res. 2022. https://doi.org/10.1111/1475-6773.14016.
Hojat M, LaNoue M. Exploration and confirmation of the latent variable structure of the Jefferson Scale of Empathy. Int J Med Educ. 2014;5:73–81. https://doi.org/10.5116/ijme.533f.0c41.
Hojat M, Axelrod D, Spandorfer J, Mangione S. Enhancing and sustaining empathy in medical students. Med Teach. 2013;35:996–1001. https://doi.org/10.3109/0142159X.2013.802300.
Hojat M, Louis DZ, Markham FW, Wender R, Rabinowitz C, Gonnella JS. Physicians’ empathy and clinical outcomes for diabetic patients. Acad Med. 2011;86:359–64. https://doi.org/10.1097/acm.0b013e3182086fe1.
Del Canale S, Louis DZ, Maio V, Wang X, Rossi G, Hojat M, Gonnella JS. The relationship between physician empathy and disease complications: an empirical study of primary care physicians and their diabetic patients in Parma. Italy Acad Med. 2012;87(9):1243–9. https://doi.org/10.1097/acm.0b013e3182628fbf.
Costa PT, McCrea RB. Revised NEO Personality Inventory (Neo PI-R) and NEO Five Factor Inventory (NEO-FFI): professional manual. Odessa, FL: Psychological Assessment Resources; 1992. https://doi.org/10.4135/9781849200479.n9.
Hojat M, Mangione S, Kane G, Gonnella JS. Relationships between scores of the Jefferson Scale of Physician Empathy (JSPE) and Interpersonal Reactivity Index (IRI). Med Teach. 2005;17:625–8. https://doi.org/10.1080/01421590500069744.
Costa P, de Carvelho-Filho MA, Schweller M, Thiemann P, Salguera A, Benson J, et al. Measuring medical students’ empathy: exploring the underlying constructs of and associations between two widely used self-report instruments in five countries. Acad Med. 2017;92:860–7. https://doi.org/10.1097/acm.0000000000001449.
Hojat M, Zuckerman M, Gonnella JS, Mangione S, Nasca TJ, Vergare M, Magee M. Empathy in medical students as related to specialty interest, personality, and perception of mother and father. Personality Individ Differ. 2005;39:1205–15. https://doi.org/10.1016/j.paid.2005.04.007.
Costa P, Alves R, Neto I, Marvao P, Portela M, Costa MJ. Associations between medical student empathy and personality: a multi-institutional study. PLoS ONE. 2014;9(3):e89254. https://doi.org/10.1371/journal.pone.0089254.
Hojat M, Vergare M, Isenberg G, Cohen M, Spandorfer J. Underlying construct of empathy, optimism, and burnout in medical students. Int J Med Educ. 2015;6:12–6. https://doi.org/10.5116/ijme.54c3.60cd.
Yaden ME, Yaden DB, Buffone AEK, Eichstaedt JC, Crutchley P, Smith LK, Cass JL, Callahan CA, Rosenthal SR, Ungar LH, Schwartz HA, Hojat M. Linguistic analysis of empathy in medical school admission essays. Int J Med Educ. 2020;11:186–90. https://doi.org/10.5116/ijme.5f2d.0359.
Hojat M, Bianco JA, Mann D, Massello D, Calabrese LH. Overlap between empathy, teamwork, and integrative approach to patient care. Med Teach. 2015;2015(37):755–8. https://doi.org/10.3109/0142159X.2014.971722.
Mangione S, Chakraborti C, Staltari G, et al. Medical students’ exposure to humanities correlates with positive personal qualities and reduced burnout: a multi-institutional U.S. Survey. J Gen Intern Med. 2018;33(5):628–34. https://doi.org/10.1007/s11606-017-4275-8.
Park KH, Roh H, Suh DH, Hojat M. Empathy in Korean medical students: findings from a nationwide survey. Med Teach. 2015;37:943–8. https://doi.org/10.3109/0142159X.2014.956058.
Aroa S, Ashrafian H, Davis R, Athanaiou T, Darzi A, Sevdalis N. Emotional intelligence in medicine: a systematic review through the context of the ACGME competencies. Med Educ. 2010;44:749764. https://doi.org/10.1111/j.1365-2923.2010.03709.x.
Austin E, Evans P, Goldwater R, Potter V. A preliminary study of emotional intelligence, empathy, and exam performance in first year medical students. Pers Individ Dif. 2005;39:1395–405. https://doi.org/10.1016/j.paid.2005.04.014.
Kliscz J, Nowicka-Sauer K, Trzeciak B, Nowak P, Sadowska A. Empathy in health care providers—validation study of the Polish version of the Jefferson Scale of Empathy. Adv Med Sci. 2006;51:219-225.42.
Hong M, Bahn GH, Lee WH, Moon SJ. Empathy in Korean psychiatric residents. Asia Pac Psychiatry. 2011;3:83–90. https://doi.org/10.1111/j.1758-5872.2011.00123.x.
Brazeau CMLR, Schroeder R, Rovi S, Boyd L. Relationships between medical student burnout, empathy, and professionalism climate. Acad Med. 2010;85(10):s33–6.
Chaitoff A, Sun B, Windover A, Bokar D, Featherall J, Rotheberg MB, et al. Associations between physician empathy, physician characteristics, and standardized measures of patient experiences. Acad Med. 2017;92:1464–71. https://doi.org/10.1097/ACM0000000000001671.
Hojat M, Michalec B, Veloski J, Tykocinski ML. Can empathy, other personality attributes, and level of positive social influence in medical school identify potential leaders in medicine? Acad Med. 2015;90:505–10. https://doi.org/10.1097/ACM.0000000000000652.
Pohl CA, Hojat M, Arnold L. Peer nominations as related to academic attainment, empathy, and specialty interest. Acad Med. 2011;86:747–51. https://doi.org/10.1097/ACM.0b013e318217e464.
Hojat M, Spandorfer J, Isenberg G, Vergare M, Fassihi R. Psychometrics of the scale of attitudes toward physician-pharmacist collaboration: a study with medical students. Med Teach. 2012;34:e833–7. https://doi.org/10.3109/0142159X.2012.714877.
Calabrese LH, Bianco JA, Mann D, Massello D, Hojat M. Correlates and changes in empathy and attitudes toward interprofessional collaboration in osteopathic medical students. J Am Osteopath Assoc. 2013;113:898–907. https://doi.org/10.7556/jaoa.2013.068.
Ward J, Schaal M, Sullivan J, Bowen ME, Erdmann JB, Hojat M. Reliability and validity of the Jefferson Scale of Empathy in undergraduate nursing students. J Nurs Meas. 2009;17(1):73–88. https://doi.org/10.1891/1061-3749.17.1.73.
Van Winkel LJ, Fjortoft N, Hojat M. Validation of an instrument to measure pharmacy and medical students’ attitudes toward physician-pharmacist collaboration. Am J Pharm Educ. 2011. https://doi.org/10.5688/ajpe759178.
Maslach C. Burnout: a multidimensional perspective. In: Schaufeli WB, Maslach C, Marek FT, editors. Professional burnout: recent developments in theory and research. Washington DC: Taylor & Francis; 1993.
Cho E, Jeon S. The role of empathy and psychological need satisfaction in pharmacy students’ burnout and well-being. BMC Med Educ. 2019;19:43. https://doi.org/10.1186/s12909-019-1477-2.
LaNoue MD, Roter DL. Exploring patient-centeredness: the relationship between self-reported empathy and patient-centered communication in medical trainees. Patient Educ Couns. 2018;101(6):1143–6. https://doi.org/10.1016/j.pec.2018.01.016.
Roter D, Larson S. The Roter interaction analysis system (RIAS): utility and flexibility for analysis of medical interactions. Patient Educ Couns. 2002;46:243–51. https://doi.org/10.1016/S0738-3991(2)00012-5.
Noll DR, Ginsberg T, Elahi A, Cavalieri TA. Effective patient-physician communication based on osteopathic philosophy in caring for elderly patients. J Am Osteopath Assoc. 2016;116(1):42–7. https://doi.org/10.7556/jaoa.2016.005.
National Board of Osteopathic Medical Examiners (NBOME). Fundamental osteopathic medical competency domains. Chicago, IL: National Board of Osteopathic Medical Examiners. June 2011. https://www.nbome.org/docs/NBOME%20Fundamental%20Osteopathic%20Medical%20Compattencies.pdf.
Hasan S, Al-sharquawi N, Dashti F, AbdulAziz M, Abdullah A, Shakkur M, Thalib L. Level of empathy among medical students in Kuwwait University, Kuwait. Med Princ Pract. 2013. https://doi.org/10.1159/000348300.
Xia L, Hongyu S, Xinwei F. Study on correlation between empathy ability and personality characteristics of undergraduate nursing students. Chin Nurs Res. 2011;32:2933–5.
Eysenck HJ, Eysenck SBG. Manual of the Eysenck personality questionnaire (junior and adult). Essex: Hodder & Stoughton.
Bucher JT, Vu DM, Hojat M. Psychostimulant drug abuse and personality factors in medical students. Med Teach. 2013;35:53–7. https://doi.org/10.3109/0142159X.2012.731099.
Zuckerman M. Zuckerman-Kuhlman Personality Questionnaire (ZKPQ): an alternative five-factor model. In: DeRaad B, Perugini MR, editors. Big five assessment. Seattle, WA: Hogrefe & Huber; 2002. p. 377–96.
Lamothe M, Boujut E, Zenasni F, Sultan S. To be or not to be empathic: the combined role of empathic concern and perspective taking in understanding burnout in general practice. MBS Fam Pract. 2014;15:15. https://doi.org/10.1186/1471-2296-15-15.
Zenasni F, Boujut E, de Vaure CB, Catu-Pinault A, Tavani JL, Rigal L, Sultan S. Development of a French-language version of the Jefferson Scale of Physician Empathy and associations with practice characteristics and burnout in a sample of general practitioners. Int J Pers Cent Med. 2012; 2:759–766. http://www.ijpcm.org/index.php/IJPCM/article/view/295.
Williams CA. Empathy and burnout in male and female helping professionals. Res Nurs Health. 1989;12:169–78. https://doi.org/10.1002/nur.4770120307.
Figley CR. Compassion fatigue: copying with secondary traumatic stress disorder in those who treat the traumatized. New York: Brunner/Mazel; 1995.
Bloom P. Against empathy. New York: Harper Collins; 2016.
Wu W, Ma X, Liu Y, Qi Q, Guo Z, Li S, Yu L, Long Q, Chen Y, Teng Z, Li X, Zeng Y. Empathy alleviates the learning burnout of medical college students through enhancing resilience. BMC Med Educ. 2022;22:481. https://doi.org/10.1186/s12909-022-03554-w.
Hojat M, Gonnella JS, Mangione S, Nasca TJ, Veloski JJ, Erdmann JB, Callahan CA, Magee M. Empathy in medical students as related to academic performance, clinical competence and gender. Med Educ. 2002;36:522–7. https://doi.org/10.1046/j.1365-2923.2002.01234.x.
Berg K, Majdan JF, Berg D, Veloski JJ, Hojat M. A comparison of students’ self-reported empathy with simulated patients’ assessment of student empathy. Med Teach. 2011;33:388–91. https://doi.org/10.3109/0142159X.2010.530319.
Berg K, Blatt B, Lopreiato J, et al. Standardized patient assessment of medical student empathy: ethnicity and gender effects in a multi-institutional study. Acad Med. 2015;90:105–11. https://doi.org/10.1097/ACM.0000000000000529.
Baron-Cohen S. The essential difference: the truth about the male and female brain. New York: Basic Books; 2003.
Alcorta-Garza A, Gonzalez-Gurrero JF, Tavitas-Herrera SE, Rodrigues-Lara FJ, Hojat M. validacion de la escala de empatia de Jefferson en estudiantes de medicina Mexicanos. [Validity of the Jefferson Scale of Physician Empathy among Mexican medical students]. Salud Mental [Mental Health]. 2005; 28:57–63.
Fjortoft N, Van Winkle LJ, Hojat M. Measuring empathy in pharmacy students. Am J Pharm Educ. 2011;75(6):109. https://doi.org/10.5688/ajpe756109.
Hojat M, Gonnella JS. Eleven years of data on the Jefferson Scale of Empathy-medical student version (JSE-S): proxy norm data and tentative cutoff scores. Med Princ Pract. 2015;24:344–50. https://doi.org/10.1159/000381954.
Hojat M, DeSantis J, Gonnella JS. Patient perceptions of clinician’s empathy: measurement and psychometrics. J Patient Exp. 2017;4(2):78–83. https://doi.org/10.1177/2374373517699273.
Laskowski C, Pellicore K. The wounded healer archetype: application to palliative care practice. Am J Hosp Palliat Care. 2002;19:403–7. https://doi.org/10.1177/104990910201900611.
Modi A, Fascelli M, Daitch Z, Hojat M. Evaluating the Relationship between participation in student-run free clinics and changes in empathy in medical students. J Prim Care Community Health. 2017;8(3):122–6. https://doi.org/10.1177/2150131916685199.
Hojat M, DeSantis J, Ney D, DeCleene-Do H. Empathy of medical students and compassionate care for dying patients: an assessment of “No One Dies Alone” program. J Patient Exp. 2021;7:164–8. https://doi.org/10.1177/2374373520962605.
Bailey BA. Empathy in medical students: assessment and relationship to specialty choice. Dissertation Abstracts International. 62(6A), 2001.
Hojat M, Gonnella JS, Nasca TJ, Mangione S, Veloski JJ, Magee M. The Jefferson Scale of Physician Empathy: further psychometric data and differences by gender and specialty at item level. Acad Med (supplement). 2002;77:S58–60. https://doi.org/10.1097/00001888-200210001-00019.
Chen DCR, Kirshenbaum DS, Yan J, Kirshenbaum E, Aseltine RH. Characterizing changes in student empathy throughout medical school. Med Teach. 2012;34:305–11. https://doi.org/10.3109/0142159x.2012.644600.
Chen D, Lew R, Hershman W, Orlander J. A cross-sectional measurement of medical student empathy. J Gen Intern Med. 2007;22:1434–8. https://doi.org/10.1007/s11606-007-0298-x.
Kataoka HU, Koide N, Hojat M, Gonnella JS. Measurement and correlates of empathy among female Japanese physicians. BMC Med Educ. 2012. https://doi.org/10.1186/1472-6920-12-48.
Vionescu BI, Szentagoti A, Coogan A. Residents’ clinical empathy: gender and specialty comparisons—a Romanian study. Acta Medica Academica. 2009;38:11–5. https://doi.org/10.5644/ama.v38i1.50.
Taragin MI, Sonnenberg FA, Karns ME, Trout R, Shapiro S, Carson JL. Does physician performance explain interspecialty differences in malpractice claim rates? Med Care. 1994;32:661–7. https://doi.org/10.1097/00005650-199407000-00001.
McTighe AJ, Ditomasso RA, Felgoise S, Hojat M. Effect of medical education on empathy in osteopathic medical students. J Am Osteopath Assoc. 2016;116:668–74. https://doi.org/10.7556/jaoa.2016.131.
Hojat M, Mangione S, Nasca TJ, Rattner S, Erdmann JB, Gonnella JS, Magee M. An empirical study of decline in empathy in medical school. Med Educ. 2004;38:934–41. https://doi.org/10.1111/j.1365-2929.2004.01911.x.
Hojat M, Vergare M, Maxwell K, et al. The devil is in the third year: a longitudinal study of erosion of empathy in medical school. Acad Med. 2009;84:1182–91. https://doi.org/10.1097/ACM.0b013e3181b17e55.
Neumann M, Edelhauser F, Tauschel D, Witz M, Woopen C, Schaffer C. Empathy decline and its reasons: a systematic review of studies with medical students and residents. Acad Med. 2011;86:996–1009. https://doi.org/10.1097/ACM.0b013e318221e615.
Ward J, Cody J, Schaal M, Hojat M. The empathy enigma: an empirical study of decline in empathy among undergraduate nursing students. J Prof Nurs. 2012;28:34–40. https://doi.org/10.1016/j.profnurs.2011.10.007.
Sherman JJ, Cramer A. Measurement of changes in empathy during dental school. J Dent Educ. 2005;69:338–45.
Kimmelman M, Giacobbe J, Faden J, Kumar G, Pinckney CC, Steer R. Empathy in osteopathic medical students: a cross-sectional analysis. JAOA. 2012;112:347–55.
Rizkalla MN, Henderson KK. Empathy and osteopathic manipulative medicine: Is it all in the hands? J Am Osteopath Assoc. 2018;118:573–85. https://doi.org/10.7556/jaoa.2018.131.
Smith KE, Norman GJ, Decety J. The complexity of empathy during medical school training: evidence for positive changes. Med Educ. 2017;51:1146–59. https://doi.org/10.1111/medu.13398.
Spatoula V, Panagopoulou E, Montgomery A. Does empathy change during undergraduate medical education? A meta-analysis. Med Teach. 2019;41:895–904. https://doi.org/10.1080/0142159X.2019.1584275.
Reniers RL, Corcoran R, Drake R, Shryane NM, Vollm BA. The QCAE: a questionnaire of cognitive and affective empathy. J Pers Assess. 2011;93(1):84–95. https://doi.org/10.1080/00223891.2010.528484.
Carey TS, Motyka TM, Garrett JM, Keller RB. Do osteopathic physicians differ in patient interaction from allopathic physicians? Am empirically derived approach. J Am Osteopath Assoc. 2003;103:313–8.
Colliver JA, Conlee MJ, Verhulst SJ, Dorsey JK. Reports of the decline of empathy during medical education are greatly exaggerated: a reexamination of the research. Acad Med. 2010;85:588–93. https://doi.org/10.1097/ACM.0b013e3181d281dc.
Hojat M, Gonnella JS, Veloski JJ. A rebuttal on critics on decline of empathy [letter to the editor]. Acad Med. 2010;85:1812. https://doi.org/10.1097/ACM.0b013e3181fa3576.
Ferreira-Valente A, Monteiro JS, Barbosa RM, Salgueira A, Costa P, Costa MJ. Clarifying changes in student empathy throughout medical school: a scoping review. Adv in Health Sci Educ. 2017;22:1293–313. https://doi.org/10.1007/s10459-016-9704-7.
Ten HM. approaches for enhancing empathy in health and human services cultures. J Health Hum Serv Adm. 2009;31:412–50.
Van Winkle LJ, Fjortoft N, Hojat M. Impact of a workshop about aging on the empathy scores of pharmacy and medical students. Am J Pharm Educ. 2012;76(1):9. https://doi.org/10.5688/ajpe7619.
Kataoka H, Iwase T, Ogawa H, Mahmood S, Sato M, DeSantis J, Hojat M, Gonnella JS. Can communication skills training improve empathy? A six-year longitudinal study of medical students in Japan. Med Teach. 2019;41:195–200. https://doi.org/10.1080/0142159X.2018.1460657.
Fukuyaso Y, Kataoka HU, Hoda M, et al. The effect of humanitude care methodology on improving empathy: a six-year longitudinal study of medical students in Japan. BMC Med Educ. 2021;21:316. https://doi.org/10.1186/s12909-021-02773-x.
Forstater AT, Chauhan N, Allen A, Hojat M, Lopez BL. An emergency department shadowing experience for emergency medicine residents-can it prevent the erosion of empathy [abstract]. Acad Emerg Med. 2011;18(10):2.
LoSasso AA, Lemberton CE, Sammon M, Berg KT, Caruso JW, Cass J, Hojat M. Enhancing student empathetic engagement, history-taking, and communication skills during electronic medical record use in patient care. Acad Med. 2017;92(7):1022–7. https://doi.org/10.1080/0142159x.2018.1460657.
Misra-Hebert AD, Isaacson JH, Kohn M, Hull AL, Hojat M, Papp KK, Calabrese L. Improving empathy of physicians through guided reflective writing. Int J Med Educ. 2012;3:71–7. https://doi.org/10.5116/ijme.4f7e.e332.
Rakel DP, Hoeft TJ, Barrett BP, Chewing BA, Craig BM, Niu M. Practitioner empathy and the duration of the common cold. Fam Med. 2009;41(7):494–501.
Mercer SW, Reynolds WJ. Empathy and quality of care. Br J Gen Pract. 2002;52:S9–12.
Chaitoff A, Rothberg MB, Windover AK, Calabrese L, Misra-Hebert A, Martinez K. Physician empathy is not associated with laboratory outcomes in diabetes: a cross-sectional study. J Gen Intern Med. 2018;34(1):75–81. https://doi.org/10.1007/s11606-018-4731-0.
Hojat M, Maio V, Markham FW, Louis ZL, Gonnella JS. Physician empathy and diabetes outcomes. J Gen Intern Med. 2019;34(10):1966. https://doi.org/10.1007/s11606-019-05187-0.
Yang N, Xiao H, Wang W, Li S, Yan H, Wang Y. Effects of doctors’ empathy abilities on the cellular immunity of patients with advanced prostate cancer treated by orchiectomy: the mediating role of patients’ stigma, self-efficacy, and anxiety. Patient Prefer Adherence. 2018;12:1305–414. https://doi.org/10.2147/PPA.S166460.
Preston SD, de Wall B. Empathy: its ultimate and proximate bases. Behav Brain Sci. 2002;25:1–20. https://doi.org/10.1017/S0140525X02000018.
Heindrichs M, Domes G. Neuropeptides and social behavior: effects of oxytocin and vasopressin in humans. Prog Brain Res. 2008;170:337–50. https://doi.org/10.1016/S0079-6123(08)00428-7.
Rizzolatti G, Fadiga L, Gallese V, Fogassi L. Premotor cortex and the recognition of motor action. Cog Res. 1996;3:131–41. https://doi.org/10.1016/0926-6410(95)00038-0.
Gallese V. The, “shared manifest” hypothesis: from mirror neuron to empathy. J Conscious Stud. 2001;8:33–50.
Hojat M, Louis DZ, Maio V, Gonnella JS. Empathy and health care quality. Am J Med Qual. 2013;28:6–7. https://doi.org/10.1177/1062860612464731.
Hojat M. Assessments of empathy in medical school admissions: what additional evidence is needed [invited editorial]. Int J Med Educ. 2014;5:7–10. https://doi.org/10.5116/ijme.52b7.5294.
Acknowledgements
Mike Magee, M.D., who at the time of initiation of the Jefferson Empathy Project was Director of the Pfizer Medical Humanities Initiative, was instrumental in providing a start-up funding for medical education research that led to the development of the Jefferson Empathy Project. We thank the Noguchi Medical Research Institute in Tokyo, Japan for providing partial support for preparing this article. We thank Pamela Walter for her editorial help and Shira Carroll for her stylistic modifications and formatting of the manuscript.
Funding
Partially funded by the Noguchi Medical Research Institute in Tokyo, Japan.
Author information
Authors and Affiliations
Contributions
MH, VM, CAP, and JSG conceived the idea of the article. MH wrote the first draft of the manuscript. MH, VM, CAP, and JSG critically reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest; however, the Jefferson Scale of Empathy described in this article and in most of the reported citations, was created by Dr. Hojat. His University holds the copyright privilege that generates revenue from others’ use of this instrument. However, Dr. Hojat and other authors of this article derive no financial benefits.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Authors’ note
Journal’s publication charge was waived for this article.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hojat, M., Maio, V., Pohl, C.A. et al. Clinical empathy: definition, measurement, correlates, group differences, erosion, enhancement, and healthcare outcomes. Discov Health Systems 2, 8 (2023). https://doi.org/10.1007/s44250-023-00020-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s44250-023-00020-2