Abstract
Background
Higher EuroSCORE II values are usually associated with increased postoperative morbidity and longer durations of Cardiac intensive care unit (CICU) stay following cardiac surgery.
Aim/Purpose
The aim is to investigate the predictive performance of EuroSCORE II for the Indian population and its relationship with ICU length of stay.
Methods
Prospective, observational study in 250 adult cardiac patients undergoing CABG under general Anaesthesia. Preoperatively values of EuroSCORE II was calculated by an online calculator available on www.euroscore.org. These patients were followed up after surgery for 30 days to note mortality and length of CICU stay.
Results
Of 250 cases studied, 39 (15.6%) had EuroSCORE II less than 1, 163 (65.2%) had EuroSCORE II between 1 and 3, 36 (14.4%) had EuroSCORE II between 3.1 and 5.0 and 12 (4.8%) had EuroSCORE II more than 5 in the study group. Mean EuroSCORE II and length of stay in CICU after surgery was 2.2 ± 1.4 and 4.2 ± 2.5 days respectively. The area under the curve (AUC) for EuroSCORE II as a sole predictor of mortality in the study group based on receiver operating characteristic curve (ROC) analysis was 0.919 (95% CI 0.86–0.97). Based on ROC analysis, AUC is significantly higher for predicting mortality (p < 0.001).
Conclusion
EuroSCORE II in Indian cardiac patients undergoing cardiac surgery is lesser than in European patients (mean 2.2 vs 3.7). Incidence of mortality is higher in patients with higher EuroSCORE II. As per our study patients with higher EuroSCORE II tend to stay longer in ICU.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Perioperative mortality following cardiac surgery is a leading cause of death in developed countries ranging from 2.9 to 6.2% [1]. Therefore, it is desirable to use an accurate predictive tool that can preoperatively discriminate between cardiac patients of high and low risk for surgery. In the past, a number of scores have been developed in European countries and America which tried to accurately stratify the risk for cardiac surgeries. The time-tested preoperative scoring systems were poor predictors of morbidity as assessed by the immediate morbidity [Length of stay (LOS) in ICU] and the intermediate morbidity (LOS in Hospital) [2]. These scores include the Society of thoracic Surgeons (STS), Parsonnet score, sequential organ failure assessment score (SOFA) score and European System for Cardiac Operative Risk Evaluation (EuroSCORE) [3]. EuroSCORE is one of the most well-validated simple predictive models and the most commonly used score for assessing early mortality in cardiac surgery. This predictive model is based on the largest, most complete, and validated databases from 128 surgical centres in eight European countries [4, 5]. In few studies the accumulative method has been found to exaggerate the mortality for patients at the lower end of the risk spectrum while underrate this parameter in the very high-risk patient groups.
In view of the overestimated mortality by EuroSCORE I, EuroSCORE II was introduced as a risk stratification model in 2011 by the EACTS (European Association for Cardiothoracic Surgery) [6]. In the past 10 years, EuroSCORE II has been evaluated and compared in different populations in Europe and Asia but adequate data in comparison to the Indian population is lacking.
The purpose of this research was to study and investigate the predictive performance of EuroSCORE II for the Indian population and the relationship of EuroSCORE II with intensive care unit (ICU) LOS. Several studies in the past have attempted to identify the effect of patient’s factors, treatment and institutional factors that can best explain variation around ICU LOS. However, there is still ambiguity and a lack of concise recommendations which could help us on how resource planning can be improved by monitoring variation in patient management techniques. This is useful in coming to gold standard techniques in managing cardiac patients. There is a need for the development of a multi-institutional risk scoring system for prolonged ICU LOS along with mortality following cardiac surgery. This preoperative predictive model could help in quality assessment, practice improvement, patient counselling, resource allocation and decision making. In resource limited developing countries like India these scores might help label the patient who may need prolonged ICU care and hence resource allocation. Hence here we theorized that higher EuroSCORE II values would be associated with increased postoperative morbidity and therefore longer duration of CICU stay following cardiac surgery.
2 Materials and Methods
This prospective observational study was carried out at a tertiary care center. After clearance from the Armed Forces Medical College, Pune India ethical committee, the study was initiated. Written informed consent was sought from the patients. 250 adult patients of age more than 18 years undergoing CABG (Coronary Artery Bypass Grafting) were included. During the study period, preoperatively patient was evaluated, and Euro SCORE II was calculated by an online calculator available at site [Table 1, Fig. 1].
EuroSCORE II parameters from www.euroscore.org
All patients are monitored according to the American society of anaesthesia (ASA) standard monitoring including Pulmonary arterial pressure monitoring. The post-surgery patient was on invasive monitoring for a duration of 24–48 h depending on haemodynamic and neurological status. Patient’s adverse outcomes were noted in terms of extended ICU stay or mortality (30 days mortality).
2.1 Statistical Analysis
The entire data is statistically analysed using Statistical Package for Social Sciences (SPSS ver 21.0, IBM Corporation, USA) for MS Windows. The data on categorical variables are shown as n (% of cases) and the data on continuous variables is presented as Mean and Standard deviation (SD). The inter-group statistical comparison of continuous variables is done using a one-way analysis of variance (ANOVA—with the significance of linearity trend in the distribution of means). The inter-group statistical comparison of the distribution of categorical variables is done using the Chi-Square test. The underlying normality assumption was tested before subjecting each variable to ANOVA. The proposed diagnostic optimal cut-off is obtained using receiver operating characteristic curve (ROC) analysis. The area under the curve (AUC) along with its 95% CI is used to determine the predictive significance based on ROC analysis.
In the entire study, the p values less than 0.05 are statistically significant. All the hypotheses were formulated using two-tailed alternatives against each null hypothesis (hypothesis of no difference).
3 Results
A predictive tool using Euro SCORE II was used to detect Perioperative mortality and its relationship with ICU and LOS in 250 patients who underwent cardiac surgery under General anaesthesia. Clinical profile and demographic characteristics were comparable between the two groups (Table 2). The average age of patients who had surgery was 64.3 ± 8.6 years. Men are operated on almost three times more often than women (Table 2). Triple vessel disease (SVD) was the most frequent surgery conducted during the study period (Table 2).
Of the 250 cases studied, 163 (65.2%) have EuroSCORE II between 1 and 3 [Table 3]. Mean EuroSCORE II among the group of cases studied was 2.2 ± 1.4 [− 0.50 to 8.70].
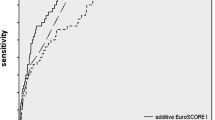
The incidence of mortality in our study group population undergoing cardiac surgery was found to be 5.6%. Mean LOS in ICU after surgery was 4.2 ± 2.5 days. The distribution of AUC for EuroSCORE II as a predictor of mortality in the study group based on ROC analysis was 0.919 with 95% CI (0.861–0.976) and sensitivity of AUC 0.029 [Fig. 2]. Based on ROC analysis, AUC is significantly higher for predicting mortality (p < 0.001). Concerning ROC analysis, the optimal cut-off of EuroSCORE II for the prediction of mortality is 3.70.
The distribution of incidence of mortality is significantly higher among a group of cases with higher EuroSCORE II and vice-versa (p < 0.001). Maximum death (16.7%) was observed in patients EuroSCORE II between 3 and 5 [Table 3].
Distribution of duration of ICU stay in the group of cases with EuroSCORE II below 1, between 1.0 and 3.0, between 3.1 and 5.0 and > 5.0 was 3.72 ± 0.94 days, 3.94 ± 1.90 days, 4.92 ± 3.04 days, and 6.58 ± 4.95 days respectively. The distribution of mean duration of ICU stay is significantly higher among the group of cases that had higher EuroSCORE II (p < 0.001).
Distribution of sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and accuracy of EuroSCORE II (with the optimal cut-off of 3.70) as a predictor of incidence of mortality in the study group was 78.6, 89.8, 31.4, 98.6 and 89.2% respectively.
4 Discussion
In developing countries where resources are limited post-operative morbidity and mortality prediction is of prime importance [7]. Prediction scores will help the treating surgeon and anesthesiologist to take true informed consent for cardiac surgeries and explain the postop morbidity expected on an individual case basis. Quantification of risk accurately will objectify the risk involved in these surgeries and help patient relatives understand the gravity of the situation [8].
In the Indian population, limited literature is available to support the EuroSCORE II model. In some studies mortality was underpredicted and comparing it with other scores like STS (Society of Thoracic Surgeons score) it offered no additional benefit and even overpredicted mortality [9, 10]. In Indian studies where EuroSCORE II was compared with the Parsonnet score, System-97 score and Cleveland score in urban Indian population it was not validated [11]. EuroSCORE II has been studied in previous studies in different countries mostly in Europe. Few Asian studies are also available. As this is still a new topic in risk stratification much research is still going on. Our study is adding a drop to this huge bucket of studies still trying to test EuroSCORE II.
EuroSCORE II on its inception was based on surgical end results and outcomes spotted in vast database which included more than 22,000 patients in hospitals all over the map, mainly in European countries. In the landmark trial, Area under the curve (ROC), the result of EuroSCORE II was 0.81, which was higher as against to the value derived for simple EuroSCORE, which resulted from 0.78 [6]. Comparing EuroSCORE II studies in other countries, The Virginia study revealed to be superior and more realistic than EuroSCORE and STS scores [12]. Among the French population, EuroSCORE II was compared with the previous version in patients more than 80 and less than 80 years. It was found to be better in < 80 years. Age group [13]. In New Zealand score showed strong discriminative ability in CABG but in valvular surgery, it was overestimated [14].
If we collate subjectively the new EuroSCORE II and old EuroSCORE, it has changed the definition of renal function and unstable angina. Also, it went into more details and further subdivided the classification of pulmonary hypertension, urgency, and weight of operation. Most importantly, the new score has also updated the definition of outcome measurement, from a 30-day mortality rate to in-hospital mortality. The main reason was the loss of follow-up data after discharge in many centers, thereby giving rise to poor quality data in the original EuroSCORE. An interesting meta-analysis systematically reviewed the reports related to the relative performance of STS, EuroSCORE II and ACEF performance of discrimination, mortality at 30 days and in consideration of the informed bias [15]. Among the 22 selected studies, containing 33 comparisons showed that scoring systems EuroSCORE II and STS were similar, in terms of their AUC, while it was more than the score of ACEF. The discrimination in results reflect both the design of the EuroSCORE II model and biological variability. Most patients in the original cohort used to originally develop the risk scoring system underwent isolated CABG, and so the model is inherently best powered for this subgroup of procedures.
The identification of potential risk factors preoperatively for perioperative mortality is a key issue in ensuring the complete surgical performance of high quality, and properly allocating resources both clinical and economically. Few independent risk markers of cardiac function like B-type natriuretic peptide (BNP) were evaluated in a few studies in past. They concluded that absolute concentrations of both first- and second-postop day BNP are independent predictors of 12 month, all-cause mortality. When compared to each other, second-postoperative-day BNP is more predictive of 12 month, all-cause mortality [16]. Given its extensive validation and well-recognized standard definitions of risk factors cardiac surgery, EuroSCORE II may represent the base for extensive exploration and study the relationship between preoperative risk factors and mortality in the long run. In patients other than CABG like patients undergoing mitral valve repair for degenerative MR, the EuroSCORE II significantly overestimates the 30 day mortality [17]. Among scores that were developed after EuroSCORE II. Scores like APORTEI risk score when compared with both logistic EuroSCORE and EuroSCORE II shows significantly higher performances in terms of discrimination and calibration compared [18]. Troponin T in combination with EuroSCORE II has proven to be superior to individual scores [19].
4.1 Limitations
Highlighting the few limitations to our study. Firstly, this study is from a single hospital. Our results cannot be simply generalized to the entire population undergoing cardiac surgery in all aspects. EuroSCORE II does not consider the duration of surgery and intraoperative surgical events. These events may also influence mortality and post-op ICU stay in cardiac surgeries. The racial differences between patient and their background makes it difficult to group patients in same set of parameters. In the end, the length of ICU stay is quantifiable only when strict protocols for admission and discharge from ICU are followed in any institute. Any discrepancies can influence the outcome of risk stratification studies like ours.
5 Conclusion
We can conclude that the mean value of EuroSCORE II in Indian patients undergoing cardiac surgery is less than that of European patients (mean 2.2 vs 3.7). Incidence of mortality is higher in patients with higher EuroSCORE II. As per our study patients with higher EuroSCORE II tend to stay longer in ICU.
Data Availability
The data sets used and/or analyzed in the present study are not available.
References
Siregar S, Groenwold RH, de Mol BA, Speekenbrink RG, Versteegh MI, Bravo Bruinsma GJB, et al. Evaluation of cardiac surgery mortality rates: 30-day mortality or longer follow-up. Eur J Cardio-Thoracic Surg. 2013;44:875–83.
Bhukal I, Solanki SL, Ramaswamy S, Yaddanapudi LN, Jain A, Kumar P. Perioperative predictors of morbidity and mortality following cardiac surgery under cardiopulmonary bypass. Saudi J Anaesth. 2012;6:242–7.
Hote M. Cardiac surgery risk scoring systems: In quest for the best. Heart Asia. 2018;10: e011017.
Nashef SA, Roques F, Michel P, Gauducheau E, Lemeshow S, Salamon R. European system for cardiac operative risk evaluation (EuroSCORE). Eur J Cardiothorac Surg. 1999;16:9–13.
Nashef SAM, Roques F, Michel P, Gauducheau E, De Vnicentiis C, Baudet E, et al. Risk factors and outcome in European cardiac surgery: analysis of the EuroSCORE multinational database of 19030 patients. Eur J Cardiothorac Surg. 1999;15:816–22.
Nashef SA, Roques F, Sharples LD, Nilsson J, Smith C, Goldstone AR, Lockowandt U. EuroSCORE II. Eur J Cardiothorac Surg. 2012;41:734–44.
Patel SK, Kacheriwala SM, Duttaroy DD. Audit of Postoperative Surgical Intensive Care Unit Admissions. Indian J Crit Care Med. 2018;22:10–5.
Anand A, Nair RR, Kodamanchili S, Panda R, Bhardwaj KK, Tb G. Communication with Patients on Mechanical Ventilation: A Review of Existing Technologies. Indian J Crit Care Med. 2022;26:756–7.
Almashrafi A, Elmontsri M, Aylin P. Systematic review of factors influencing length of stay in ICU after adult cardiac surgery. BMC Health Serv Res. 2016;16:318.
Messaoudi N, De Cocker J, Stockman B, Bossaert LL, Rodrigus IE. Prediction of prolonged length of stay in the intensive care unit after cardiac surgery: the need for a multi-institutional risk scoring system. J Card Surg. 2009;24:127–33.
Kar P, Geeta K, Gopinath R, Durga P. Mortality prediction in Indian cardiac surgery patients: Validation of European System for Cardiac Operative Risk Evaluation II. Indian J Anaesth. 2017;61:157–62.
Ad N, Holmes SD, Patel J, Pritchard G, Shuman DJ, Halpin L. Comparison of EuroSCORE II, Original EuroSCORE, and The Society of Thoracic Surgeons Risk Score in Cardiac Surgery Patients. Ann Thorac Surg. 2016;102:573–9.
Provenchère S, Chevalier A, Ghodbane W, et al. Is the EuroSCORE II reliable to estimate operative mortality among octogenarians? PLoS ONE. 2017;12: e0187056.
Singh N, Gimpel D, Parkinson G, Conaglen P, Meikle F, Lin Z, et al. Assessment of the EuroSCORE II in a New Zealand Tertiary Centre. Heart Lung Circ. 2019;28:1670–6.
Sullivan PG, Wallach JD, Ioannidis JP. Meta-Analysis Comparing Established Risk Prediction Models (EuroSCORE II, STS Score, and ACEF Score) for Perioperative Mortality During Cardiac Surgery. Am J Cardiol. 2016;118:1574–82.
Mauermann E, Bolliger D, Fassl J, Grapow M, Seeberger EE, Seeberger MD, et al. Absolute Postoperative B-type Natriuretic Peptide Concentrations, but Not Their General Trend, Are Associated With 12-Month, All-Cause Mortality After On-Pump Cardiac Surgery. Anesth Analg. 2017;125:753–61.
Wang TK, Harmos S, Gamble GD, Ramanathan T, Ruygrok PN. Performance of contemporary surgical risk scores for mitral valve surgery. J Card Surg. 2017;32:172–6.
Urso S, Tena MÁ, Horcajada I, Paredes F, González-Barbeito M, Portela F, EME study group. Prediction of surgical risk in patients with endocarditis: Comparison of logistic EuroSCORE, EuroSCORE II and APORTEI score. Enferm Infecc Microbiol Clin (Engl Ed). 2021;39:244–7.
Li X, Shan L, Lv M, et al. Predictive ability of EuroSCORE II integrating cardiac troponin T in patients undergoing OPCABG. BMC Cardiovasc Disord. 2020;20:463.
Funding
No funding was received to assist with the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
KS and SS participated in the design of the study. KS wrote the application for the ethical approval. KS collected the data. NS, SM and TP analyzed the data. SS drafted the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics Approval
Institutional Review Board provided ethical permission for the research (No. EC/OCT/2017). The study is in compliance with the Helsinki Congress and the Declaration of Istanbul.
Consent to Participate
Informed consent taken from all patients.
Consent for Publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kate, S., Shouche, S., Singh, S. et al. EuroSCORE II for Risk Evaluation and Predicting Cardiac Intensive Care Length of Stay in Indian Patients Undergoing Adult Cardiac Surgery. Intensive Care Res 3, 259–264 (2023). https://doi.org/10.1007/s44231-023-00050-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s44231-023-00050-7