Abstract
Background
Preoperative risk evaluation systems are significant and important to the allocation of medical resources and the communication between doctors and patients. The European System for Cardiac Operative Risk Evaluation II (EuroSCORE II) is widely used in clinical practice. Cardiac troponin T (cTnT) can specifically and accurately reflect myocardial injury. Whether EuroSCORE II can improve the predictive power after integrating with cTnT is still unclear. This study was a retrospective single center study designed to assess the predictive ability of EuroSCORE II integrated with cTnT for patients undergoing isolated off-pump coronary artery bypass grafting (OPCABG).
Methods
This retrospective and observational cohort study included 1887 patients who underwent first isolated OPCABG. cTnT was detected within 48 h before operation in each patient. According to myocardial injury, patients were divided by cTnT into 4 stages. A new risk evaluation system was created through logistic regression with EuroSCORE II and myocardial injury classification as covariates. Then the two risk evaluation systems were comparatively assessed by regression analysis, receiver operator characteristic curves, net reclassification index, Bland–Altman plots and decision curve analysis.
Results
There were 43 in-hospital deaths, with a mortality of 2.30% (43/1887). The logistic regression analysis showed that preoperative myocardial injury classification was a significant risk factor for in-hospital mortality in both total cohort (OR 1.491, 95%CI 1.049–2.119) and subsets (OR 1.761, 95%CI 1.102–2.814). The new risk evaluation system has higher calibration and discrimination power than EuroSCORE II, both for overall cohort and subsets. Especially, the new system has obvious advantages in discrimination power in the subset of acute myocardial infarction (AUC 0.813 vs. 0.772, 0.906 vs. 0.841, and 0.715 vs. 0.646, respectively).
Conclusions
Both myocardial injury classification and EuroSCORE II are independent risk factors of in-hospital mortality in OPCABG patients. The new risk evaluation system has higher predictive ability than EuroSCORE II, especially in patients with a recent history of AMI.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
The number of cardiac surgery is increasing rapidly in China following the development of economy and surgical technology [1]. In the past two decades, the proportion of coronary artery bypass grafting (CABG) has been rising fast, more than half of which is off-pump CABG (OPCABG) in mainland China [2]. Preoperative risk evaluation is important and significant and can help surgeons to judge the diagnosis and treatment of potential postoperative complications. The European System for Cardiac Operative Risk Evaluation II (EuroSCOREII) is one of the commonly- and widely-used risk evaluation systems in clinical practice. CABG is a special operation of myocardial revascularization for patients suffering myocardial ischemia injury to different degrees before operation. Myocardial markers, such as cardiac troponin T (cTnT), can specifically and accurately reflect the situation of myocardial injury [3, 4]. However, EuroSCOREII does not include myocardial markers as important variables. Therefore, we suspect whether EuroSCOREII can improve the predictive power after integrating with cTnT for patients undergoing OPCABG. As far as we know, there are only a few reports on this issue [5,6,7]. Hence, this study was aimed to comparatively evaluate the predictive ability of EuroSCOREII integrating with cTnT in OPCABG patients.
Methods
Patients
Between January 2010 and October 2017, 1902 consecutive patients underwent primary isolated OPCABG in our department. Exclusion criteria were preoperative hemodialysis, lack of cTnT before operation, and incomplete medical records. Finally, 1887 patients made up the study database. All included patients, or their legal representatives, signed written informed consents to take part in the study and for all surgical procedures. We reviewed and collected detailed clinical data from medical records and the hospital information system.
Data collection
Venous blood (within 48 h before operation) of each patient was collected and sent to cTnT measurement by standard techniques in the central laboratory of our hospital. Since January 2015, the new-generation high-sensitivity cTnT (hs-cTnT) has been widely used in clinical practice. The detection limits of cTnT and hs-cTnT are 100—2000 and 0—10,000 ng/l, respectively, and their normal ranges are 0—100 and 0—14 ng/l respectively. The risk score of each patient was calculated online according to the EuroSCOREII interactive calculator (https://www.euroscore.org/calcold.html). Myocardial injury classification was divided by the preoperative cTnT into stages 1 to 4, in which the preoperative cTnT is within the normal range, above the upper normal limit (UNL) but less than 10 times of UNL, above 10 times of UNL but less than 20 times of UNL, and above 20 times of UNL respectively.
Research registration
All patients were operated by the same group of surgeons. After operation, treatment and nursing care were performed in accordance with the routine of the department and clinical guidelines. The study was approved by the Ethics committees of the local hospital (ID: 2017–018). The trial was registered at https://www.chictr.org.cn with NO.ChiCTR2000032365.
Creation of new model
Multivariable logistic regression with backward elimination was modeled by using the variables from univariate analysis to identify the independent risk factors associated with in-hospital mortality. All variables with P < 0.15 or clinically considered as risk factors were entered into the multivariate analysis, including gender, age, New York Heart Association (NYHA) stage, cerebrovascular disease, creatinine clearance rate (Ccr), left ventricular ejection fraction (LVEF), peripheral vascular disease, operation status, renal dysfunction, EuroSCORE II, myocardial injury classification, diabetes, valvular disease, body mass index (BMI) and hypertension. After indemnifying EuroSCORE II and myocardial injury classification as independent risk factors for in-hospital mortality, we used these two factors as covariates to create a new risk evaluation system by logistic regression.
Statistical analysis
Continuous data was expressed as mean ± standard deviation or median and interquartile ranges (non-normal distribution), and were compared between groups through Student’s t test or Mann–Whitney U test. Categorical variables were presented as number and percentage and were compared using Fisher’s exact or Chi-square tests.
The new risk evaluation system and EuroSCORE II were calibrated by Hosmer–Lemeshow (H–L) goodness-of-fit statistic. Discrimination ability was measured by receiver’s operating characteristic (ROC) curve. Discrimination power was considered by the area under the curve (AUC) of ROC.
Agreement between the two risk evaluation systems was estimated by Bland–Altman analysis [8]. The predictive in-hospital mortality was calculated by the two systems separately. Figures were plotted by the differences between the two sorts of predictive mortalities and the mean between them. All differences being equal to 0 indicate the two systems fully agree with each other. But certain error always existed in the risk evaluation systems. Patients who died and those who survived were sent to Bland–Altman analysis separately. A better risk evaluation system will give higher predictive mortality in dead patients and lower predictive mortality in surviving patients. The agreement interval was calculated using the mean of differences ± standard deviation. Over 95% of the points fell in the agreement interval, which indicated a good agreement between the two risk evaluation systems.
The net benefits of the two risk evaluation systems for predicting in-hospital mortality were measured by decision curves analysis (DCA). As reported [9], the proportion of all false positive patients was subtracted by DCA from the proportion of true positive patients, and then weighted according to the relative harm of false positive and false negative results.
The consistency of the two evaluation systems in predicting in-hospital mortality was tested by the net reclassification index (NRI). According to Pencina et al. [10], patients were divided into 4 groups by different standards. A change into a higher group means upward movement (up), and a change into a lower group means downward movement (down). The NRI was calculated as follows:
Statistical analysis was performed on SPSS 22.0 for windows (IBM, Chicago, USA). DCA was performed on R software 3.4.0 with the package Decision curve. Two-sided P ≤ 0.05 was considered significant.
Outcome endpoint
The endpoint of this study was in-hospital mortality, which was defined as any death within 30 days after operation or during postoperative hospitalization.
Results
Demographic data
A total of 1887 patients were divided by cTnT into a cTnT group (n = 971) and a hs-cTnT group (n = 916). Baseline clinical characteristics and demographics of the patients were shown in Table 1. Patients in the cTnT group had more frequent preoperative comorbidities, such as hypertension, and unstable angina. Patients in the cTnT group had significantly higher Cr and lower Ccr than the hs-cTnT group (both P < 0.001). The NYHA stage, LVEF and EuroSCORE II were all higher in the cTnT group than the hs-cTnT group.
The degree of myocardial injury significantly differs with the type of coronary heart disease (CAD) [11]. The total cohort was divided by the classification of clinical CAD into 3 subsets, including stable angina, unstable angina, and acute myocardial infarction (AMI). Demographics and perioperative data were revealed in Table 2.
Perioperative outcomes
Totally, 43 patients died in hospital, with a mortality of 2.30% (43/1887). In-hospital mortality rates in total cohort and different subsets were shown in Fig. 1. The in-hospital mortality in the AMI subset was 3.8% (Fig. 1b), and that at myocardial injury stage 4 was up to 9.2% (Fig. 1c).
ROC curve
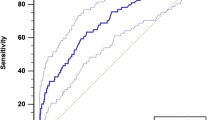
The calibration and discrimination power of EuroSCORE II and the new risk evaluation system (EuroSCORE II integrating with cTnT) were shown in Table 3. In general, the new system outperformed in the total cohort and the subsets (Fig. 2). Especially in the AMI subset, the new system had obvious advantages in discrimination power (AUC 0.813 vs. 0.772, 0.906 vs. 0.841, and 0.715 vs. 0.646, respectively).
The ROC curves of the two risk evaluation systems in total cohort and subsets. a Total cohort and CAD subsets, 1. total cohort, 2. stable angina subset, 3. unstable angina subset, 4. AMI subset. b cTnT group and CAD subsets, 1. cTnT group, 2. stable angina subset, 3. unstable angina subset, 4. AMI subset. c hs-cTnT group and CAD subsets, 1. hs-cTnT group, 2. stable angina subset, 3. unstable angina subset, 4. AMI subset
Net reclassification index
No significant differences in NRI were found in total cohort and the cTnT group (Table 4). It tended to be better NRI for the new system compared to EuroSCORE II. The new system outperformed EuroSCORE II in the hs-cTnT group (P = 0.04). Based on the types of CAD, there was a better NRI for the new system compared to EuroSCORE II in the unstable angina subset. No significant NRI was found in the other two subsets.
Bland–Altman analysis
The agreement between the new risk evaluation system and EuroSCORE II was tested by Bland–Altman analysis (Fig. 3). Results showed the two systems were evaluated as a very good agreement. In the plot of survivors, most of the points were found in the agreement interval (97.9%). Similar result was found in the plot of death group (97.8%). Moreover, the new system reduced 65.7% of predictive mortality in the survivors and increased 65.1% of predictive mortality in the dead patients in hospital.
Logistic regression analysis
The univariate logistic regression analysis showed that preoperative myocardial injury classification was a significant risk factor for in-hospital mortality in the total cohort (OR 2.049, 95%CI 1.542–2.722, P < 0.001). It remained a significant risk factor for in-hospital mortality in the cTnT group and the hs-cTnT group (OR 3.564, 95%CI 2.105–6.035, P < 0.001 and OR 1.963, 95%CI 1.322–2.915, P = 0.001). EuroSCORE II was also an independent risk factor for the postoperative mortality of OPCABG in both the total cohort and the cTnT group (Table 5). In the multivariate logistic regression models, myocardial injury classification and EuroSCORE II were also risk factors for in-hospital mortality (Table 6).
Decision curves analysis
The clinical benefits of EuroSCORE II and the new system in predicting in-hospital mortality were calculated by DCA. The net benefits of the two systems for predicting in-hospital mortality in the total cohort and subsets were shown in Fig. 4. In general, the new system was no worse than EuroSCORE II. Especially in the total cohort, the stable angina subset, the AMI subset, the cTnT group and the cTnT AMI subset, the new risk evaluation system outperformed EuroSCORE II with better net benefits.
DCA for assessing the clinical benefits of the two risk evaluation systems in total cohort and subsets. The gray line represents the net benefits of providing surgery for all patients, assuming that all patients would survive. The black line represents the net benefits of surgery to no patients, assuming that none would survive after operation. The blue and green lines stand for the net benefits of applying surgery to patients according to EuroSCORE II and the new system respectively. a total cohort and CAD subsets. 1. total cohort, 2. stable angina subset, 3. unstable angina subset, 4. AMI subset. b cTnT group and CAD subsets, 1. cTnT group, 2. stable angina subset, 3. unstable angina subset, 4. AMI subset. c hs-cTnT group and CAD subsets, 1. hs-cTnT group, 2. stable angina subset, 3. unstable angina subset, 4. AMI subset
Discussion
Principal findings
Consistent with our hypothesis, the increase of preoperative cTnT or hs-cTnT was an independent risk factor for postoperative mortality in patients undergoing OPCABG. When EuroSCORE II was integrated with the myocardial injury classification, the ability to predict the outcomes after OPCABG can be improved. Especially for patients with preoperative AMI, integration with myocardial injury classification can significantly improve the discrimination power of EuroSCORE II, which is of great clinical significance for high-risk patients. According to our literature review, it is the first time to report the combination of cTnT in improving the prediction ability of EuroSCORE II for OPCABG patients in China.
Cause analysis
EuroSCORE was based on the surgical data of more than 10,000 patients who underwent cardiac surgery in 8 European countries in 1995 [12], and has been used worldwide for decades. With the prolonging of time, EuroSCORE was also advancing and constantly updated. In 2012, the EuroSCORE research team proposed a new system—EuroSCORE II [13]. However, with the continuous advancement of surgical techniques and the increasing amount of cardiac surgery worldwide, EuroSCORE II will overestimate or underestimate the risk of death in patients undergoing cardiac surgery [14,15,16,17,18,19]. The performance of the EuroSCORE II was poor among patients with the lower predicted mortality [20]. Moreover, our previous research considered that EuroSCORE II underestimated the risk of cardiac surgery for the Chinese population, especially for CABG patients [21, 22]. Continuing to use the model may mislead the judgment of clinicians and even will harm the interest of patients. In addition, EuroSCORE II was designed to predict the perioperative mortality [13] and was inappropriate to predict postoperative mid- and long-term risks. Because many factors that can affect the long-term mortality [23, 24], for in-hospital mortality, the predictive ability of EuroSCORE II may be improved theoretically when it integrates with some new risk factors.
cTnT is one of the cardiac calmodulin subunits and a specific marker of myocardial injury [25, 26]. When myocardial cells damaged, with the rupture of cell membrane structure, cTnT quickly enters circulation [27, 28]. The continuous progress of the production technology has continuously improved the detection level of cTnT [29]. Nowadays, the fourth generation of hs-cTnT has been widely used in clinic. Novel highly sensitive assays for hs-cTnT can detect troponin concentration 10 times lower than the standard assays [30].
Literature has confirmed that the increase of cTnT is a strong risk factor of recent adverse cardiovascular events and is also applicable to patients undergoing cardiac intervention and surgery [31,32,33,34]. As reported, cTnT before percutaneous coronary intervention can provide better predictive value for postoperative outcomes [35]. In this study, both univariate and multivariate analyses found that cTnT was an independent risk factor for in-hospital mortality.
EuroSCORE II contains 18 important perioperative risk factors, but does not involve any factor of myocardial injury [13]. Nowadays, cTnT test, a routine in the daily work of CABG [5], is indispensable for patients with myocardial ischemia. Therefore, we tried to integrate preoperative cTnT information into EuroSCORE II and found that its predictive power was improved after integrating with myocardial injury classification.
One of the important functions of risk evaluation systems is to distinguish high-risk patients before operation, which is of great significance and importance to the allocation of medical resources and the communication between doctors and patients’ families. Bland–Altman analysis showed good agreement between the two risk evaluation systems for patients who died or survived after operation. The new risk evaluation system in the surviving patients was scored lower than EuroSCORE II, while was scored higher in the dead patients. These results illustrate the new system can replace EuroSCORE II, and has a higher ability to distinguish high-risk patients. Generally, the risk of operation in AMI patients is higher than of other patients [36]. Subset analysis found the new system significantly improved the predictive power in the AMI subset. The discriminative power of the new system was 0.813, 0.906 and 0.715 respectively. No matter in total cohort or in cTnT group or hs-cTnT group, they all showed the same trends in the AMI patients. In general, after integrating myocardial injury variable, EuroSCORE II could improve the ability to identify high-risk patients before cardiac surgery, which was beneficial to personalized treatment and optimization of medical resources.
Interestingly, the discriminative power of the new risk evaluation system was not as good as EuroSCORE II in the unstable angina subset. The reason may be that the degree of myocardial injury in patients with unstable angina was very different, which affected the contribution of cTnT to the prediction.
Limitations
There are some limitations in our study. Firstly, it was a retrospective observational study in a single medical center, and the sample size was small. Secondly, surgical practice, anesthesia and postoperative care changed over the study period, which can lead to selection bias. Thirdly, considering the influence of renal dysfunction on cTnT [37, 38], we excluded such patients, which may also cause selection bias. Fourthly, we converted cTnT from a continuous variable to a categorical variable, which will lose some information.
Conclusions
Both myocardial injury classification and EuroSCORE II are independent risk factors of in-hospital mortality in OPCABG patients. The inclusion of cTnT can enhance the predictive ability of EuroSCORE II, especially in patients with a recent history of AMI.
Availability of data and materials
If readers need complete original data, they can contact the corresponding author to obtain it.
Abbreviations
- EuroSCORE II:
-
European system for cardiac operative risk evaluation II
- cTnT:
-
Cardiac troponin T
- OPCABG:
-
Off-pump coronary artery bypass grafting
- CABG:
-
Coronary artery bypass grafting
- hs-cTnT:
-
High-sensitivity cardiac troponin T
- UNL:
-
Upper normal limit
- NYHA:
-
New York heart association
- Ccr:
-
Creatinine clearance rate
- LVEF:
-
Left ventricular ejection fraction
- BMI:
-
Body mass index
- H–L:
-
Hosmer–Lemeshow
- ROC:
-
Receiver’s operating characteristic
- DCA:
-
Decision curves analysis
- NRI:
-
Net reclassification index
- CAD:
-
Coronary heart disease
- AMI:
-
Acute myocardial infarction
References
Yuan X, Zhang H, Zheng Z, et al. Trends in mortality and major complications for patients undergoing coronary artery bypass grafting among urban teaching hospitals in China: 2004 to 2013. Eur Heart J Qual Care Clin Outcomes. 2017;3(4):312–8.
Zhou P, Zhu P, Xiao Z, Lin X, Xu R, Zheng S. Meta-analysis of repeat revascularization of off-pump and on-pump coronary artery bypass surgery. Ann Thorac Surg. 2018;106(2):526–31.
Bodor GS. Biochemical markers of myocardial damage. EJIFCC. 2016;27(2):95–111.
Mair J, Lindahl B, Hammarsten O, et al. How is cardiac troponin released from injured myocardium. Eur Heart J Acute Cardiovasc Care. 2018;7(6):553–60.
Fellahi JL, Le Manach Y, Daccache G, Riou B, Gerard JL, Hanouz JL. Combination of EuroSCORE and cardiac troponin I improves the prediction of adverse outcome after cardiac surgery. Anesthesiology. 2011;114(2):330–9.
Petaja L, Rosjo H, Mildh L, et al. Predictive value of high-sensitivity troponin T in addition to EuroSCORE II in cardiac surgery. Interact Cardiovasc Thorac Surg. 2016;23(1):133–41.
Simon C, Capuano F, Roscitano A, Benedetto U, Comito C, Sinatra R. Cardiac troponin I vs EuroSCORE: myocardial infarction and hospital mortality. Asian Cardiovasc Thorac Ann. 2008;16(2):97–102.
Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1(8476):307–10.
Vickers AJ, Elkin EB. Decision curve analysis: a novel method for evaluating prediction models. Med Decis Making. 2006;26(6):565–74.
Pencina MJ, Steyerberg EW, Auid-Oho, Sr DRB. Net reclassification index at event rate: properties and relationships. Stat Med. 2017. 36(28): 4455–4467.
Ibanez B, James S, Agewall S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39(2):119–77.
Nashef SA, Roques F, Michel P, Gauducheau E, Lemeshow S, Salamon R. European system for cardiac operative risk evaluation (EuroSCORE). Eur J Cardiothorac Surg. 1999;16(1):9–13.
Nashef SA, Roques F, Sharples LD, et al. EuroSCORE II. Eur J Cardiothorac Surg. 2012;41(4):734–44.
Ranjan R, Adhikary D, Mandal S, Saha SK, Hasan K, Adhikary AB. Performance of EuroSCORE II and logistic EuroSCORE in Bangladeshi population undergoing off-pump coronary artery bypass surgery: a prospective cohort study. JRSM Cardiovasc Dis. 2019;8:2048004019862125.
Shapira-Daniels A, Blumenfeld O, Korach A, Rudis E, Izhar U, Shapira OM. The American society of thoracic surgery score versus EuroSCORE I and EuroSCORE II in Israeli patients undergoing cardiac surgery. Isr Med Assoc J. 2019;21(10):671–5.
Borracci RA, Rubio M, Baldi J, Giorgini JC, Higa CC. Multicenter prospective validation of the EuroSCORE II in Argentina. Arch Cardiol Mex. 2019;89(4):315–23.
Czub P, Cacko A, Gawalko M, et al. Perioperative risk assessment with Euroscore and Euroscore II in patients with coronary artery or valvular disease. Medicine (Baltimore). 2018;97(50):e13572.
Singh N, Gimpel D, Parkinson G, et al. Assessment of the EuroSCORE II in a New Zealand tertiary centre. Heart Lung Circ. 2019;28(11):1670–6.
Hogervorst EK, Rosseel P, van de Watering L, et al. Prospective validation of the EuroSCORE II risk model in a single Dutch cardiac surgery centre. Neth Heart J. 2018;26(11):540–51.
Knapik P, Cieśla D, Saucha W, et al. Outcome prediction after coronary surgery and redo surgery for bleeding (from the KROK registry). J Cardiothorac Vasc Anesth. 2019;33(11):2930–7.
Shan L, Ge W, Pu Y, et al. Assessment of three risk evaluation systems for patients aged >/=70 in East China: performance of SinoSCORE, EuroSCORE II and the STS risk evaluation system. PeerJ. 2018;6:e4413.
Ma X, Wang Y, Shan L, et al. Validation of SinoSCORE for isolated CABG operation in East China. Sci Rep. 2017;7(1):16806.
Barili F, Pacini D, D’Ovidio M, et al. The impact of EuroSCORE II risk factors on prediction of long-term mortality. Ann Thorac Surg. 2016;102(4):1296–303.
Nezic D. Reliability of EuroSCORE II to predict long-term mortality after isolated aortic valve operations. Ann Thorac Surg. 2016;101(6):2427.
Januzzi JL, Lewandrowski K, MacGillivray TE, et al. A comparison of cardiac troponin T and creatine kinase-MB for patient evaluation after cardiac surgery. J Am Coll Cardiol. 2002;39(9):1518–23.
de Antonio M, Lupon J, Galan A, Vila J, Urrutia A, Bayes-Genis A. Combined use of high-sensitivity cardiac troponin T and N-terminal pro-B type natriuretic peptide improves measurements of performance over established mortality risk factors in chronic heart failure. Am Heart J. 2012;163(5):821–8.
Pokharel Y, Mouhanna F, Schneider A, et al. High-sensitive troponin T, natriuretic peptide, and cognitive change. J Am Geriatr Soc. 2019;67(11):2353–61.
Mueller M, Vafaie M, Biener M, Giannitsis E, Katus HA. Cardiac Troponin T. Circ J. 2013 .
Mehdiani A, Akhyari P, Kamiya H, et al. Prognostic value of the new high sensitive cardiac troponin T assay (hs-cTnT) after coronary artery bypass grafting. Acta Cardiol. 2017;72(3):276–83.
Hashim IA, Vigen R, Fernandez F, et al. Validation and implementation of the fifth-generation high sensitivity Troponin T (hs-TnT) assay at a large teaching county hospital. A laboratory-driven multi-speciality effort. Clin Chim Acta. 2019;495:85–7.
Zachoval CF, Dolscheid-Pommerich R, Graeff I, et al. High-sensitivity troponin T testing: consequences on daily clinical practice and effects on diagnosis of myocardial infarction. J Clin Med. 2020;9(3):775.
Lippi G, Cervellin G. Cardiac troponin T versus cardiac troponin I for mortality risk prediction: Is one biomarker better than the other. Clin Biochem. 2020;78:40–1.
Brynildsen J, Petaja L, Pettila V, et al. The predictive value of NT-proBNP and hs-TnT for risk of death in cardiac surgical patients. Clin Biochem. 2018;53:65–71.
Gillmann HJ, Meinders A, Grohennig A, et al. Perioperative levels and changes of high-sensitivity troponin T are associated with cardiovascular events in vascular surgery patients. Crit Care Med. 2014;42(6):1498–506.
Prasad A, Rihal CS, Lennon RJ, Singh M, Jaffe AS, Holmes DR Jr. Significance of periprocedural myonecrosis on outcomes after percutaneous coronary intervention: an analysis of preintervention and postintervention troponin T levels in 5487 patients. Circ Cardiovasc Interv. 2008;1(1):10–9.
de Lavallaz JDF, Puelacher C, Buse GL, Bolliger D, Germanier D, Hidvegi R, Sazgary L. Daytime variation of perioperative myocardial injury in non-cardiac surgery and effect on outcome. Heart. 2019;105(11):826–33.
Ali SA, Kazmi S, Jalal-Ud-Din M, Qasim MI, Jadoon ZG. Frequency of elevated troponin T in patients of hronic renal failure without clinically suspected acute myocardial infarction. J Ayub Med Coll Abbottabad. 2019;31(3):364–7.
Wrenn K, Blair R, Parl FF, Schleicher R. Calcium-phosphorus product and troponin-T values in renal failure. Am J Emerg Med. 2006;24(7):836–8.
Acknowledgements
Not applicable.
Funding
This study was supported by Shanghai Municipal Natural Science Foundation (20ZR1446100).
Author information
Authors and Affiliations
Contributions
Y.Z. made substantial contributions to conception and design. Y.H., L.S. and M.L. were involved in acquisition of data. Z.L., X.L. and B.L. were responsible for analysis and interpretation of data. X.L., L.S. and M.L. were major contributors in writing and revising the manuscript. B.L., W.G. and Y.Z. gave final approval of the version to be published. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Ethics committees of Shanghai East Hospital (ID: 2017–018). The trial was registered at https://www.chictr.org.cn with NO.ChiCTR2000032365. All patients included in the study, or their legal representatives, signed written informed consents to participate in the study and for all surgical procedures.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Li, X., Shan, L., Lv, M. et al. Predictive ability of EuroSCORE II integrating cardiactroponin T in patients undergoing OPCABG. BMC Cardiovasc Disord 20, 463 (2020). https://doi.org/10.1186/s12872-020-01745-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-020-01745-1