Abstract
Visuospatial ability plays a crucial role in anatomy related study success as studies have shown that students with high scores on a mental rotation test (MRT) perform better on anatomy exams. We hypothesized that segmenting anatomical structures on radiological images might impact students’ visuospatial abilities as measured by MRT scores. Second-year (bio)medical students who participated in a 10-week elective course were recruited for this study. All students completed an MRT questionnaire at the beginning of the elective course and another at the end of the elective course. During the elective course, students manually segmented radiological images (e.g., computed tomography (CT) and magnetic resonance imaging (MRI) data) to construct extended reality models. In total, twenty-eight students (17 males, 25 studied medicine) provided consent to participate in this study. A significant difference in mean pre-test scores (mean: 14.46; SD: ± 4.36) and post-test scores (mean: 17.56; SD: ± 4.57) (paired samples t-test, t(27) = −8.30, P < 0.001) was observed. Males had significantly better MRT scores, both at the pre- and at the post-test MRT. The results from this study should be interpretated with some caution due to the lack of a control group. The use of image segmentation as a teaching method to help (bio)medical students, especially those with low visuospatial insights, should be further investigated In future studies with larger cohorts and using a case–control experimental design.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Anatomy is considered the cornerstone of medical education as it provides a solid foundation on which medical knowledge is built, regardless of medical specialization [1]. Nevertheless, the hours spent on anatomical subjects in medical curricula have been declining for years [2, 3] and, in turn, undergraduate (bio)medical students have reported feeling ill-equipped in terms of anatomical knowledge when commencing their clinical training [4, 5]. To better prepare these students for their medical careers, innovative and novel methods may need to be employed in the teaching of anatomy. One of those methods can be the use of radiological data. Over the past decades, radiology has been increasingly used as a anatomy teaching method and it forms an important component of anatomy teaching programs in many universities [6]. The increasing implementation and use of radiology in anatomy education are propelled by the widespread availability, the increasing quality of radiological images and the ability to visualize human anatomy in great detail. More specifically, visuospatial and sectional anatomy can be taught in detail by use of radiology [7, 8]. In one study, students expressed that the top three preferred teaching formats were anatomy laboratory instruction, interactive sessions in which radiology and anatomy were combined and anatomy lectures. After some training, students also expressed to feel comfortable reviewing radiological images [9]. However, an overlooked possibility with regard to the use of radiological images in anatomy education concerns the use of such images for three dimensional image reconstruction. Using radiology images, 3D models can be created which highlight anatomical structures of interest [10, 11]. For example, in a study of our group, a comprehensive three-dimensional model of the brain was constructed on high-resolution magnetic resonance images [12]. The construction of these 3D models and the use of them in anatomy education can be considered as a new teaching method that warrants proper integration of radiology in anatomy education. Such models can be shown in virtual reality (VR) and augmented reality (AR), which together known as extended reality (XR). Studies have shown that working with AR models does not improve anatomy scores compared to conventional methods, though working with AR models resulted in a lower cognitive load experienced by the students [13], which can improve a learner’s ability to perform and learn [14].
Another important factor for anatomy learning is the student’s visuospatial ability. Visuospatial ability was found to be positively related to the understanding and learning of anatomy with reports showing that students with high visuospatial ability are more likely to score higher on anatomy assessments [15,16,17,18]. Albeit, the reciprocal is also true; learning anatomy enhances the learners’ visuospatial ability [19]. As a result, novel and innovative teaching methods in anatomy education may have the potential to enhance students’ visuospatial capacities.
However, the effect of segmentation of radiological images on students’ visuospatial abilities is still unknown and to date, no studies on this topic exist. However, image segmentation resembles the act of (re)drawing a picture and with that focus, various studies demonstrated the effectiveness of drawing on learning and retention of knowledge [20,21,22]. The theoretical framework of this method concerns the fact that students, when (re-)drawing illustrations, need to select key elements and construct mental representations. This integration step has been described to positively impact learning outcomes and visuospatial abilities [23,24,25]. Whether this also works for segmentation-based learning remains elusive.
Therefore, we investigated the effect of radiological image segmentation as an education method in anatomy education on students’ visuospatial ability. The authors hypothesized that segmentation requires students to closely observe anatomical structures and their surroundings, helping them to convert 2D images into 3D models. Ultimately, this approach may help students to train and improve their visuospatial ability.
2 Materials and methods
2.1 Ethics statement
This study was carried out in agreement with the Statement on the Declaration of Helsinki and the Ethical Conduct of Clinical Studies. Ethical approval was waived (Nederlandse Vereniging voor Medisch Onderwijs (NVMO) ethical review board; registration number NERB 0974) due to the non-invasive character of this study. MRT test moments were implemented during an elective course for (bio)medical students at our university, with the understanding that the test results would not influence course results. For this study, all participants provided written informed consent prior to inclusion.
2.2 Participant recruitment
Second-year bachelor’s students (n = 30) studying either Medicine or Biomedical Sciences enrolled in an elective course regarding radiological anatomy and were eligible to participate in this study on a voluntary basis. Eligible students were provided with an information letter on this study, asking them to contact one of the researchers when they wished to participate.
2.3 Anatomy education in The Netherlands and elective course design
Anatomy is taught as part of the Bachelor’s program of the Medicine and Biomedical Sciences curricula in the Netherlands. Students engaged in various activities, including dissection sessions, small group lectures, and assignments, to study human anatomy. The Bachelor’s curriculum includes a total of 197 h of regular anatomy education, of which the students who participated in this study received 175 h. Students were eligible to enroll when they were enrolled in the second year of the Bachelor’s program. Thereby, students with clinical experience or any relevant experience with the reading of radiological images were excluded from this study. These elements are provided within the curriculum after the second year of the Bachelor’s program.
The elective course was developed at the Faculty of Medical Sciences at Radboud University Medical Center in Nijmegen, the Netherlands. The aim was to teach second-year Medicine and Biomedical Sciences students anatomy through the creation of XR (extended reality) models and 3D prints. The course spanned 10 weeks and students earned 2 ECTS (European Credit Transfer System) points for completing the course. On average, students dedicated 8 h per week. Students worked in pairs and received formal education on XR and 3D printing in anatomy. The course used anonymized radiological Digital Imaging and Communications in Medicine (DICOM) data, such as Computed Tomography (CT) or Magnetic Resonance Imaging (MRI), which students used to create anatomical models. The work process to create such models was detailed in a syllabus which was provided by the teachers.
The syllabus focused on three primary learning goals. First, the syllabus aimed to help students understand the strengths, weaknesses, opportunities, and threats of AR (augmented reality), VR (virtual reality), and 3D printed models in anatomy education. To achieve the first learning goal, students attended lectures on AR, VR, and 3D printing. Also, students were tasked with critical appraisals of scientific papers related to these technologies in anatomy education. After these preparatory assignments, students debated the pros and cons of these techniques in group sessions. Second, the syllabus aimed to give students insights into the possibilities of XR applications to optimize their construction for effective education.
The second learning goal was accomplished through individual assignments and interactive lectures. Students revised their knowledge of radiology imaging acquisition techniques and explored an AR application on brain anatomy to inspire their own creations. In small working group assignments, they discussed their ideas and frameworks for XR applications and 3D models, receiving guidance from teachers on peer-to-peer teaching sessions and how to enhance the use of XR and 3D models.
Third, the syllabus learned students how to create XR applications and 3D printed models for anatomy education from radiological data. This third learning goal involved practical sessions which primarily involved image segmentation sessions. Students used software packages such as ITK-SNAP, MeshLab, 3D Slicer, Spin 3D File Converter Software, and an in-house written software kit. These open-access tools [10, 26] allowed them to segment structures of interest in detail. In total, students spent over 20 h studying and segmenting the radiological images. The segmentation process was closely supervised by various teachers, for a total of 6 h during those 10 weeks. Then, teachers helped students to create 3D digital models, and to convert these models into formats suitable for XR. Exemplary images of the segmentation process and the resulting (virtual) 3D model is provided in Fig. 1. The created 3D models were subsequently used by the same students to teach their peers on the selected anatomy subjects during two 2-h teaching sessions.
2.4 Radiological data collection and processing
Radiological data (CT and MRI data) without structural abnormalities were provided by the department of Medical Imaging. Radiological data was only used if patients had not opted-out for the use for these anonymized data for further academic purposes such as education or research. All data were completely anonymized to protect patient privacy. DIn addition, when applicable, defacing the CT or MRI data was carried out.
After the students collected the DICOM data, manual and/or semi-automatic segmentation of structures of interest was carried out. Together with their teachers, students constructed a list of relevant anatomical structures which needed to be labelled separately. Teachers helped the students to corelate anatomical knowledge and figures in anatomical atlases with the structures as visible on radiological data. Students labelled all the structures to construct a virtual model using ITK-SNAP software (Fig. 2). During this segmentation process, virtual 3D models could be checked to help students to visualize the product of their labour. Feedback from peers and teachers was provided along regular small working group sessions, which helped students to refine their segmentation and, ultimately, their virtual 3D models. When finished, students converted their virtual 3D models from (standard) NifTI files (Neuroimaging Informatics Technology Initiative) into STL files. The STL files were refined during one small working group session. This refinement primarily comprised the smoothing of the model to obtain educational and aesthetic models, suitable for 3D printing, AR and/or VR applications (Fig. 3).
2.5 Visuospatial ability testing
Visuospatial ability of the participants was tested by use of the Mental Rotation Test (MRT) questionnaire. The MRT questionnaire was originally developed by Vandenberg and Kuse and concerns a 24-question test with a target figure and four stimulus figures per question. The four stimulus figures contain two correct figures and two distractors [27]. Peters et al. adapted the MRT questionnaire to be used for research purposes [28]. The MRT questionnaire is standardized and is known as a tool for assessing visuospatial abilities. A sex difference in MRT scores has been well established by others [29,30,31]. The MRT questionnaire was provided during the first week of the elective course, prior to being exposed to radiological images or prior to taking part in the segmentation assignments. Then, the study participants took part in the regular educational activities of the aforementioned described elective course. After 10 weeks, students were asked to complete another MRT. Students were given 2 weeks from the date of their elective course examination to complete the MRT questionnaire. Following the instructions, the questionnaire results were scaled from 0 to 24 points [28]. One point was awarded for correctly identifying the correct two stimulus figures that matched the target figure. A single correct answer did not receive any points.
2.6 Statistical analysis
All statistical analyses were carried out using IBM SPSS software (version 27; IBM Corp., Armonk, NY). Demographic characteristics of the participants, including sex, study direction and study year were noted as co-variables for this study. Descriptive statistical analyses were represented as mean with ± standard deviation (± SD) if normally distributed, or as a median with range (minimum–maximum) if not normally distributed. Cronbach’s alpha test was used to assess the internal consistency of the MRT questionnaire scores. Internal consistency is generally considered acceptable when Cronbach’s alpha ≥ 0.7. The paired samples Students t-test was used to assess differences between the two MRT questionnaires. When data was missing, these participants were excluded from the analyses. Also, a repeated measures ANCOVA was carried out to assess the influence age and sex of the participants on the study outcomes, Statistical significance was assumed when P < 0.05. Cohen’s d value was used to provide insights in the effect size. Interpretation of the d-statistic was carried out using the following categories: < 0.200: no relevant effect size; 0.201–0.500: small effect size; 0.501–0.800 moderate effect size; > 0.800 large effect size.
3 Results
Twenty-eight students (mean age of 20.6 ± 1.1 years) provided consent to participate in this study. Seventeen students were males (60.7%) and 25 studied Medicine (89.3%);the other three studied Biomedical Sciences (10.7%). There was no loss of participants during the study.
Cronbach’s alpha test revealed that baseline MRT questionnaire scores and MRT questionnaire scores after the 10-week elective course had an internal validity of α = 0.878 and α = 0.868.
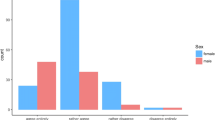
Baseline MRT questionnaire results showed a mean test score of 14.48 points (± 4.36 points) (n = 28). Male students showed a significantly higher baseline MRT questionnaire score (16.02 ± 4.07 points) compared to female students (11.60 ± 3.58 points) at baseline (P = 0.007). Mean MRT questionnaire scores increased significantly to 17.56 points (± 4.6 points) after the 10-week curriculum (P < 0.001; Cohen’s d = 0.801) (n = 28). Again, males showed significant higher MRT questionnaire scores after the 10-week elective course (19.09 ± 4.56 points) compared to female students (14.95 ± 3.38 points)(P = 0.020). Both males and females showed significant improvement of MRT questionnaire results after completion of the 10-week elective course (P < 0.001 for both groups).
Repeated ANCOVA also showed a significant improvement in MRT scores after participating in the here described elective course (F = 6.340; P = 0.013). Student age was not significantly influencing the MRT scores (F = 4.111; P = 0.058), whereas the student’s sex did significantly influence the MRT scores (F = 4.681; P = 0.041).
4 Discussion
Results of this study show that male students had significant better visuospatial insight than their female colleagues, both at baseline and after the 10-week elective course. Although MRT scores improved after finishing a 10-week elective course on segmenting radiological images, causality between improvement in MRT scores and image segmentation cannot be proven with certainty.
To our knowledge, no previous studies have investigated the effects of volumetric radiological image segmentation on spatial abilities. However, a recent study showed that incorporating drawing training into anatomy teaching helped students to improve their anatomy tutorial marks [32]. Unfortunately, this study did not formally investigate the effects of drawing on spatial abilities, but the authors stated that students who liked drawing did not have significantly different MRT scores. Also, there was no statistically significant correlation between using drawing for study and MRT scores. Interestingly, the study of Ritchie et al. demonstrated that students with lower spatial abilities did not underperform in any aspect of anatomy assessment [32]. When focusing on representational drawing and spatial abilities, Chamberlain et al. investigated changes in drawing and spatial skills in art students taking a foundational drawing course. They reported improvements in visuospatial abilities as measured by the MRT questionnaire [33], which is consistent with the results of the present study. This suggests that segmentation of radiological images might be helpful for students with low MRT scores to improve their spatial skills. In anatomy education, it is also generally accepted that spatial abilities training can help students to improve their spatial skill [17]. Due to the lack of a control group in the present study, the authors underscore that causality between image segmentation and improvement in visuospatial abilities cannot be proven. Based on the available evidence, however, we encourage the conduction of future studies which look into these effects.
Improving students’ spatial insight is believed to help them improve their anatomy tutorial marks. Although our study did not aim to find a correlation between segmentation of radiological images and performance on anatomy assessments, previous studies have shown a positive correlation between drawing and anatomy scores [34]. However, a recent study did not report significant differences in anatomy test scores between the drawing group and the control group. To explain this contradictory finding, the authors highlighted the importance of a nuanced understanding of the spatial skills required in anatomy. In their study, there was a significant correlation between MRT score and non-image-based anatomy questions, indicating that the form of testing impacts the outcome of these studies [32]. That the form of testing impacts the outcome was also emphasized in a review, revealing non-significant relationships between spatial abilities tests and anatomy knowledge assessment using essays and non-spatial multiple-choice questions. However, significant relationships were observed between spatial abilities testing and anatomy knowledge assessment using practical examination, three-dimensional synthesis from two-dimensional views, drawing of views, and cross-sections [35]. Relationships between spatial abilities testing and anatomy knowledge assessment using spatial multiple-choice questions, such as those used in the study of Ritchie et al. were unclear [35].
The here reported sex-based differences in MRT scores have been extensively described in the scientific literature [36, 37]. As both males and females improved in MRT scores over time, it is believed that incorporating radiological images in anatomy education might fit the needs of the current generation of students. Millennial students prefer to learn using visuals instead of text [38, 39]. By allowing students to construct their own 3D models based on radiological images, they can observe CT- and MRI-scans while simultaneously training their spatial abilities by turning 2D data into 3D models. This combined effect could fit perfectly in modern day anatomy and/or radiology education. XR models were found to have no significant impact on learning outcomes as compared to traditional teaching methods, whereas various studies reported the beneficiary effects of XR on preventing cognitive overload and increasing students’ motivation (for a review, see [40]).
5 Limitations of the study and future outlooks
The major limitation of the described study is the absence of a control group in a pre- and post-test experimental design. This complicates interpretation of the data as possible confounding effects cannot be ruled out and hinders the drawing of sound conclusions. Other studies have suggested that a test effect may be present when the MRT questionnaire is repeated. Two studies showed a slight increase in MRT questionnaire scores of the control group [8, 19], indicating that students may improve spatial abilities as a function of time regardless of any specific training. However, the improvement described in the control groups of the aforementioned studies [8, 19, 28, 41] was found to have a low to medium effect size, whereas we report a a strong effect size regarding the improvement in MRT scores. Nevertheless, this does not rule out an influence of maturation over time in the results of this experiment and therefore causality between the 10-week elective course and improvement in visuospatial abilities cannot be made. Therefore, this study should be interpretated as a hypothesis generating report in which we provide the groundwork for the hypothesis that segmentation based anatomy learning might help students with poor visuospatial abilities. Nevertheless, this should be further investigated In future studies with larger cohorts and using a case–control experimental design. Furthermore, the studied cohort consisted only of 28 s-year (bio)-medical students, which can be considered a relatively small and specific study cohort. Participants had already received 175 h of anatomy education before following this course, which may have influenced their spatial ability and thus, their MRT scores. However, it is not believed that this impacts the overall improvement of MRT scores between baseline and after the 10-week elective course, as the students received no formal anatomy education other than their segmentation task. Therefore, the true effect of volumetric data segmentation on spatial ability remains partially elusive, and in future, larger studies, a control group should be included in the study-design. In future studies, it would be advisable to include a more diverse group with varying levels of anatomy education to investigate the possible effects of prior education on MRT scores. Furthermore, the study design only allowed for a claim about improvements in spatial ability and not improvements in anatomical knowledge. As literature shows a link between these two, it is postulated that following this course also improved the anatomical knowledge of participants. Still, this needs to be investigated in future studies. The results of the present study warrant further validation in larger cohorts, preferably with a control cohort of students who will not receive segmentation classes. If results are consistent with the pilot data presented in this report, students with low MRT scores could be helped to improve their visuospatial abilities by completing segmentations assignments.
6 Conclusions
This study provides the first groundwork for the hypothesis that implementing image segmentation of radiological images might enhance spatial ability among (bio)medical students. However, this study is limited by the lack of a control cohort, which complicates the ruling out of the so-called maturing effect in which students improve spatial ability over time without any intervention. If the here presented results are validated in studies with a larger sample size with a control group, then these insights could be useful for anatomy educators and education policy makers to help (bio)medical students with low spatial insights.
Data availability
The here presented research data cannot be shared publicly due to individual privacy restrictions. However, data could be anonymized and shared upon reasonable request by contacting the corresponding author.
References
Turney BW. Anatomy in a modern medical curriculum. Ann R Coll Surg Engl. 2007;89(2):104–7. https://doi.org/10.1308/003588407X168244.
McBride JM, Drake RL. National survey on anatomical sciences in medical education. Anat Sci Edu. 2018;11(1):7–14. https://doi.org/10.1002/ase.1760.
Drake RL, McBride JM, Lachman N, Pawlina W. Medical education in the anatomical sciences: the winds of change continue to blow. Anat Sci Educ. 2009;2(6):253–9. https://doi.org/10.1002/ase.117.
Bergman EM, Prince KJAH, Drukker J, Van Der Vleuten CPM, Scherpbier AJJA. How much anatomy is enough? Anat Sci Educ. 2008;1(4):184–8. https://doi.org/10.1002/ase.35.
Custers EJFM, Ten Cate OTJ. Medical students’ attitudes towards and perception of the basic sciences: a comparison between students in the old and the new curriculum at the University Medical Center Utrecht, The Netherlands. Med Educ. 2002;36(12):1142–50. https://doi.org/10.1046/j.1365-2923.2002.01371.x.
Jack A, Burbridge B. The utilisation of radiology for the teaching of anatomy in Canadian medical schools. Can Assoc Radiol J. 2012;63(3):160–4. https://doi.org/10.1016/j.carj.2010.11.005.
Lufler RS, Zumwalt AC, Romney CA, Hoagland TM. Incorporating radiology into medical gross anatomy: does the use of cadaver CT scans improve students’ academic performance in anatomy? Anat Sci Educ. 2010;3(2):56–63. https://doi.org/10.1002/ase.141.
Lufler RS, Zumwalt A, Hoagland TM. Incorporating radiology into medical gross anatomy: a study of its efficacy in learning spatial relationships. Faseb J. 2009. https://doi.org/10.1096/fasebj.23.1_supplement.182.1.
Murphy KP, Crush L, O’Malley E, Daly FE, Twomey M, O’Tuathaigh CMP, et al. Medical student perceptions of radiology use in anatomy teaching. Anat Sci Educ. 2015;8(6):510–7. https://doi.org/10.1002/ase.1502.
Sutherland J, Belec J, Sheikh A, Chepelev L, Althobaity W, Chow BJW, et al. Applying modern virtual and augmented reality technologies to medical images and models. J Digit Imaging. 2019;32(1):38–53. https://doi.org/10.1007/s10278-018-0122-7.
Carvalho LE, Sobieranski AC, von Wangenheim A. 3D Segmentation algorithms for computerized tomographic imaging: a systematic literature review. J Digit Imaging. 2018;31(6):799–850. https://doi.org/10.1007/s10278-018-0101-z.
Henssen DJHA, van den Heuvel L, De Jong G, Vorstenbosch MATM, Van Walsum AMV, Van den Hurk MM, et al. Neuroanatomy learning: augmented reality vs. cross-sections. Anat Sci Educ. 2020;13(3):350–62. https://doi.org/10.1002/ase.1912.
Henssen D, van den Heuvel L, De Jong G, Vorstenbosch M, van CappellenWalsum AM, Van den Hurk MM, et al. Neuroanatomy learning: augmented reality vs. cross-sections. Anat Sci Educ. 2020;13(3):353–65. https://doi.org/10.1002/ase.1912.
Young JQ, Van Merrienboer J, Durning S, Ten Cate O. Cognitive load theory: implications for medical education: AMEE Guide No. 86. Med Teach. 2014;36(5):371–84. https://doi.org/10.3109/0142159x.2014.889290.
Lufler RS, Zumwalt AC, Romney CA, Hoagland TM. Effect of visual-spatial ability on medical students’ performance in a gross anatomy course. Anat Sci Educ. 2012;5(1):3–9. https://doi.org/10.1002/ase.264.
Guillot A, Champely S, Batier C, Thiriet P, Collet C. Relationship between spatial abilities, mental rotation and functional anatomy learning. Adv Health Sci Educ Theory Pract. 2007;12(4):491–507. https://doi.org/10.1007/s10459-006-9021-7.
Langlois J, Bellemare C, Toulouse J, Wells GA. Spatial abilities training in anatomy education: a systematic review. Anat Sci Educ. 2020;13(1):71–9. https://doi.org/10.1002/ase.1873.
Roach VA, Mi M, Mussell J, Van Nuland SE, Lufler RS, DeVeau KM, et al. Correlating spatial ability with anatomy assessment performance: a meta-analysis. Anat Sci Educ. 2021;14(3):317–29. https://doi.org/10.1002/ase.2029.
Vorstenbosch MA, Klaassen TP, Donders AR, Kooloos JG, Bolhuis SM, Laan RF. Learning anatomy enhances spatial ability. Anat Sci Educ. 2013;6(4):257–62. https://doi.org/10.1002/ase.1346.
Pickering JD. Anatomy drawing screencasts: enabling flexible learning for medical students. Anat Sci Educ. 2015;8(3):249–57. https://doi.org/10.1002/ase.1480.
Balemans MC, Kooloos JG, Donders AR, Van der Zee CE. Actual drawing of histological images improves knowledge retention. Anat Sci Educ. 2016;9(1):60–70. https://doi.org/10.1002/ase.1545.
Osório NS, Rodrigues F, Garcia EA, Costa MJ. Drawings as snapshots of student cellular anatomy understanding. Med Educ. 2013;47(11):1120–1. https://doi.org/10.1111/medu.12320.
Van Meter P, Garner J. The promise and practice of learner-generated drawing: literature review and synthesis. Educ Psychol Rev. 2005;17:285–325.
Van Meter P. Drawing construction as a strategy for learning from text. J Educ Psychol. 2001;93(1):129.
Van Meter P, Aleksic M, Schwartz A, Garner J. Learner-generated drawing as a strategy for learning from content area text. Contemp Educ Psychol. 2006;31(2):142–66.
Yushkevich PA, Piven J, Hazlett HC, Smith RG, Ho S, Gee JC, Gerig G. User-guided 3D active contour segmentation of anatomical structures: significantly improved efficiency and reliability. Neuroimage. 2006;31(3):1116–28. https://doi.org/10.1016/j.neuroimage.2006.01.015.
Vandenberg SG, Kuse AR. Mental rotations, a group test of three-dimensional spatial visualization. Percept Mot Skills. 1978;47(2):599–604. https://doi.org/10.2466/pms.1978.47.2.599.
Peters M, Laeng B, Latham K, Jackson M, Zaiyouna R, Richardson C. A redrawn Vandenberg and Kuse mental rotations test - different versions and factors that affect performance. Brain Cognit. 1995;28(1):39–58. https://doi.org/10.1006/brcg.1995.1032.
Masters MS. The gender difference on the Mental Rotations test is not due to performance factors. Mem Cognit. 1998;26(3):444–8. https://doi.org/10.3758/BF03201154.
Halpern DF. Sex differences in cognitive abilities. London: Psychology press; 2000.
Linn MC, Petersen AC. Emergence and characterization of sex differences in spatial ability: a meta-analysis. Child Dev. 1985;56:1479–98.
Ritchie HE, Oakes D, Drury H, Ollerenshaw S, Hegedus E. Can drawing instruction help students with low visuospatial ability in learning anatomy? Anat Sci Educ. 2023;16(2):252–65. https://doi.org/10.1002/ase.2230.
Chamberlain R, Kozbelt A, Drake JE, Wagemans J. Learning to see by learning to draw: a longitudinal analysis of the relationship between representational drawing training and visuospatial skill. Psychol Aesthet Creat Arts. 2021;15(1):76.
Cromley JG, Du Y, Dane AP. Drawing-to-learn: does meta-analysis show differences between technology-based drawing and paper-and-pencil drawing? J Sci Educ Technol. 2020;29(2):216–29. https://doi.org/10.1007/s10956-019-09807-6.
Langlois J, Bellemare C, Toulouse J, Wells GA. Spatial abilities and anatomy knowledge assessment: a systematic review. Anat Sci Educ. 2017;10(3):235–41. https://doi.org/10.1002/ase.1655.
Castro-Alonso JC, Jansen P. Sex differences in visuospatial processing. In: Castro-Alonso JC, editor. Visuospatial processing for education in health and natural sciences. Cham: Springer International Publishing; 2019. p. 81–110.
Peters M. Sex differences and the factor of time in solving Vandenberg and Kuse mental rotation problems. Brain Cogn. 2005;57(2):176–84. https://doi.org/10.1016/j.bandc.2004.08.052.
Slanetz PJ, Kung J, Eisenberg RL. Teaching radiology in the millennial era. Acad Radiol. 2013;20(3):387–9. https://doi.org/10.1016/j.acra.2012.09.022.
Kasprzak T. Technology and radiology education-meeting the needs of millennial learners. Acad Radiol. 2016;23(7):844–7. https://doi.org/10.1016/j.acra.2016.03.003.
Moro C, Birt J, Stromberga Z, Phelps C, Clark J, Glasziou P, Scott AM. Virtual and augmented reality enhancements to medical and science student physiology and anatomy test performance: a systematic review and meta-analysis. Anat Sci Educ. 2021;14(3):368–76. https://doi.org/10.1002/ase.2049.
Hoyek N, Collet C, Rastello O, Fargier P, Thiriet P, Guillot A. Enhancement of mental rotation abilities and its effect on anatomy learning. Teach Learn Med. 2009;21(3):201–6. https://doi.org/10.1080/10401330903014178.
Acknowledgements
None.
Grant source: Dr. Henssen received a Comenius grant (Comenius Program, Netherlands Initiative for Education Research) from the Dutch Ministry of Education, Culture and Science to further investigate the effects of new teaching tools.
Funding
No funding was received.
Author information
Authors and Affiliations
Contributions
DH, LB and TM designed the experiment. DH arranged ethical agreement. JK collected and anonymized the data. DH and JK performed the statistical methods and wrote the first version of the manuscript. LB and TM provided feedback on the first draft of the manuscript. JK revised the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Karstens, J., Boer, L., Maal, T. et al. The possible impact of segmenting radiological images on students’ spatial abilities. Discov Educ 3, 83 (2024). https://doi.org/10.1007/s44217-024-00174-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s44217-024-00174-y