Abstract
Introduction
Type 2 diabetes mellitus is the most common type of diabetes, characterized by varying degrees of insulin resistance and diminishing beta-cell function, which increases the risk of macrovascular and microvascular complications. Dulaglutide is a long-acting glucagon-like peptide-1 receptor agonist that is administered once weekly and approved for treating adults with type 2 diabetes mellitus. It can be used as a monotherapy or in addition to oral hypoglycemic or insulin therapy.
Aim
This study aims to provide information contributing to assessing the efficacy and safety of weekly 1.5 mg dulaglutide therapy in Saudi adult patients with type 2 diabetes mellitus.
Methods
A retrospective single-arm cohort study using a purposive sample to recruit type 2 diabetes mellitus patients on dulaglutide from endocrine and diabetic outpatient clinics in King Saud Medical City (N = 205). Data were collected from participants’ medical profiles and through the phone using interview questionnaires.
Results
Most participants were female and married; approximately 33% had had diabetes for more than 20 years, 41.4% of the sample had third-class obesity, and more than half had used dulaglutide for the last 1–2 years. With therapy, weight, body mass index, hemoglobin A1c, and fasting blood sugar were significantly improved after 6 and 12 months from baseline. The main side effects reported were nausea (52%) and fatigue (28%).
Conclusion
Dulaglutide is a safe and effective therapy that demonstrated favorable glycemic control and weight reduction in obese type 2 diabetes patients of Saudi origin.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Diabetes mellitus (DM) is a group of metabolic diseases resulting in a high blood sugar level over a prolonged period [1]. It is among the most common global chronic health burdens, affecting many people [2]. Type 2 diabetes mellitus (T2DM) is the most dominant type of diabetes, characterized by varying degrees of insulin resistance and diminishing beta-cell function, which will increase the risk of macrovascular complications, including cardiac disease, cerebrovascular accident, and peripheral arterial disease, as well as microvascular complications of chronic kidney disease, neuropathy, and retinopathy [1,2,3].
1.1 Background: Diabetes in Saudi Arabia
In 2017, approximately 462 million individuals were diagnosed with T2DM worldwide. This number is expected to reach 642 million by 2040 [1, 4]. Gulf Cooperation Council (GCC) countries have shown growth in diabetes prevalence over the last two decades. According to the World Health Organization, Saudi Arabia has the second-highest prevalence of diabetes in the Middle East and the seventh highest in the world. The last International Diabetes Federation (IDF) report in 2017 showed that the frequency of diabetes in Gulf countries ranged from 8% to 22%. In 2016, the number of Saudi patients diagnosed with diabetes reached 7,000,000. Another 3,000,000 were diagnosed as prediabetic, with the highest death secondary to diabetes compared to other GCC countries [1, 4].
1.2 Treatment Options
Patients with T2DM can be treated by lifestyle modifications and oral antidiabetic drugs (OADs); because T2DM is a progressive disease, maintenance of glycemic targets in some patients with monotherapy is often possible for a few years, after which combination therapy is needed to achieve optimal glycemic control [5]. In addition to insulin, glucagon-like peptide 1 receptor agonists (GLP-1 RAs) are an injectable method for treating T2DM. According to the American Diabetes Association (ADA, 2022), treatment usually starts with lifestyle modification and metformin if there are no contraindications [6]. Additionally, adding another medication, such as GLP-1 RAs, to metformin is recommended in special circumstances, such as in individuals with an established or high risk of cardiovascular or renal complications [7]. Moreover, GLP-1 RAs are a favored injectable complement to insulin in patients with poor glycemic control with OADs and in obese patients [2, 8].
Glucagon-like peptide 1 (GLP-1) is an incretin hormone that increases glucose load-based insulin secretion, reduces glucagon secretion, delays gastric emptying, and decreases appetite, which leads to more glycemic control. GLP-1 RAs have demonstrated glucose-lowering efficacy with a minimal risk of hypoglycemia and marked body weight reduction in several randomized controlled trials (RCTs) [2]. In addition, treatment with GLP-1 RA has significantly reduced cardiovascular disease risk and mortality and improved renal outcomes [2, 5].
Accordingly, the updated ADA 2022 and European Association for the Study of Diabetes (EASD) guidelines recommend adding a GLP-1RA with proven cardiovascular benefit to metformin for patients with high-risk or established atherosclerotic cardiovascular disease (CVD) regardless of whether hemoglobin A1c (HA1c) is at the target level [9].
Dulaglutide is one of these long-acting GLP1 receptor agonists administered as a once-weekly subcutaneous injection approved for the treatment of adults with T2DM in 2014 and can be used as a monotherapy or in addition to an oral hypoglycemic or insulin therapy [5, 8, 10]. It gradually reaches a maximum concentration within 48 h and has a half-life of approximately 5 days. A pharmacokinetic steady state is reached between the second and fourth doses, supporting that no dose adjustment is required based on age, sex, race, body weight, or injection site [11, 12].
1.3 Study Aim and Objectives
The primary objective of this study was to assess the efficacy of weekly 1.5 mg dulaglutide on improving glycemic control and reducing body weight independently after 6 and 12 months from baseline. Other objectives include assessing the possible effect of weekly 1.5 mg dulaglutide on different parameters, such as blood pressure, lipid profile, aspartate-aminotransferase (AST), alanine-aminotransferase (ALT), alkaline phosphatase (ALP), serum creatinine, and estimated glomerular filtration rate (eGFR) levels after 6 and 12 months from the baseline, and exploring the most common dulaglutide side effects reported by T2DM patients, such as nausea, vomiting, diarrhea, abdominal pain, dyspepsia, local injection reaction, and hypoglycemia. We also hope to assess the incidence of serious side effects that can affect patient safety, such as retinopathy, acute pancreatitis, and gallstones.
Because there have been few studies examining this topic in Saudi Arabia, the rationale for conducting this research is to evaluate the efficacy and safety of dulaglutide among Saudi patients with T2DM. It is our hope that doing so will improve the knowledge base about this medication, which other investigators will find useful in future research about dulaglutide in different Saudi regions, which will help improve medical practice and patient safety in Saudi Arabia and globally.
This study aims to provide information contributing to assessing the efficacy and safety of weekly 1.5 mg injections of dulaglutide in Saudi adult patients with T2DM who have been using it for at least 1 year.
2 Methods
2.1 Design and Setting
The study design is a retrospective single-arm cohort study. It has been conducted in diabetic clinics at King Saud Medical City (KSMC) in Riyadh, Saudi Arabia. This hospital is considered one of the largest Ministry of Health tertiary hospitals that provide health care to registered populations.
2.2 Target Population
Inclusion criteria included all Saudi adult patients aged more than 18 years with T2DM who had been treated weekly with 1.5 mg dulaglutide for at least 1 year and attended the diabetic clinics at King Saud Medical City. Exclusion criteria included patients with type 1 diabetes, positive glutamic acid decarboxylase (GAD), or islet cell antibodies, and patients who used systematic steroid therapy or chemotherapy while using dulaglutide. Investigators also excluded any patients who had undergone bariatric surgery or used weight-loss medications, patients with eGFR < 30, and any women who became pregnant during their year of using dulaglutide.
2.3 Data Collection Methods
Two methods had been used to collect data.
2.3.1 First Interview Questionnaire (Conducted by Phone from May 2023 to August 2023)
To assess dulaglutide safety, the investigators created a new questionnaire to be administered to participants. Data collected after patient consents included personal information, such as age, sex, duration of dulaglutide use, marital status, and education level, along with information about the presence of comorbidities, including hypertension, dyslipidemia (DLP), CVD, and chronic kidney disease (CKD), duration of T2DM, dulaglutide use compliance, common and serious side effects, hypoglycemia events, history of discontinuing use of dulaglutide after 1 year, and if so, the reason for discontinuation.
2.3.2 Then, Review of Participant Medical Records (Retrospectively from July 2019 to August 2023)
We retrospectively reviewed the participants’ medical records to evaluate dulaglutide efficacy. We collected data based on patient usage of insulin and oral antihyperglycemic medication and verified the diagnosis of serious side effects by viewing the clinic or emergency department visits and medical progress notes. The body weight, body mass index (BMI), systolic blood pressure (SBP), diastolic blood pressure (DBP), HbA1c level, and other laboratory results, including fasting plasma glucose (FPG), total cholesterol (TC), triglyceride (TG), low-density lipoprotein-cholesterol (LDL), AST, ALT, ALP, serum creatinine, and eGFR, were reported at baseline, 6 months after dulaglutide initiation, and again 12 months after dulaglutide initiation.
2.4 Data Management Plan
In this study, the STATA-13 statistical program was used for data analysis. Categorical descriptive variables such as sociodemographic data (gender, marital status, educational level. etc.), medical profiles, dulaglutide use, and side effects were presented as frequency (percentage) for the difference between weight, BMI, HbA1c, FBS, systolic blood pressure (SBP) and diastolic blood pressure (DBP), Serum Creatinine, GFR, LDL, TG, AST, ALT, and ALP; the repeated one-way ANOVA analysis was used where the mean in time 1, time 2 and time 3 was presented in addition to the mean difference between baseline and 6 months, baseline and 12 months, and between 6 and 12 months.
The data were considered significant at a p-value lower than 0.05.
3 Results
3.1 Sample Characteristics
In this study, a total of 205 T2DM patients who take a weekly dose of 1.5 mg were included; as Table 1 shows, the sample consisted mainly of females (77.4%) with a mean age of 52 ± 10.88 years, approximately 33% of whom had diabetes for more than 20 years. Moreover, the sample consisted mainly of third-class obese patients (41.44%).
3.2 Medical History
As Table 1 presents, more than half of the participants had hypertension (62.2%), and most of them had DLP (approximately 83%); however, a few of the samples had CVD or CKD (21.5% and 3.4%, respectively).
3.3 Dulaglutide Use
Table 2 presents the use of dulaglutide among the patients; according to the table, more than half of the patients use it in 1–2 years period (64.71%); as for the frequency, around 90.69% reported that they always use it, and only 31.86% discontinue using it, out of this about 46% reported that they discount it due their inability to refill the medication 30.7% due side effects, and around 12% due to reaching glycemic target, and around 10% due to other reasons.
3.4 Medication Profile
The following table (Table 3) presents the medication used by the participants at the time of the study; as it shows, the most taken medication was metformin, which approximately 94% of the participants took; moreover, long- and short-acting insulin were also commonly used by the participants (51.47% and 38.73%, respectively).
3.5 Reported Side Effects of Dulaglutide
Table 4 shows that minor and serious side effects have been reported among the participants, as the table shows; aside from nausea, which was the main side effect reported by approximately half of the participants (52%), most of them describe it as rarely experienced (31%) while 15.27% and about 5% reported that they sometimes and often (respectively) get nausea. Fatigue emerged as the second prevalent side effect reported by participants (28%), with the majority describing it as occurring infrequently. Other GI symptoms, such as vomiting, diarrhea, constipation, abdominal pain, and dyspepsia. were also reported rarely, sometimes, and often, and for Constipation, 1.47% always reported. local injection site reaction and low mode were also reported among the sample, with few reporting that they always get these symptoms.
For the more serious symptoms, approximately 4% (n = 9) of the participants had retinopathy, while 0.49% (n = 1) had pancreatitis, 0.98% reported cholecystitis (n = 2), and 0.49% (n = 1) reported gall bladder stones.
Furthermore, few participants reported hypoglycemia; 7.35% reported occasional mild hypoglycemia, 0.98% reported moderate hypoglycemia, and 0.49% reported occasional severe hypoglycemia.
3.6 Medical Profile Data Differences Over Time
Table 5 presents the effect of dulaglutide use at baseline, after 6 months, and after 12 months in terms of BMI, HA1c, FBS, SBP, DBP, serum creatinine, eGFR, TC, LDL, TG, AST, ALT, and ALP.
As the table shows, there were significant differences in weight, BMI, HA1c, FBS, serum creatinine in females, eGFR, total cholesterol, LDL, and ALP.
At baseline, the mean weight among the participants was 100.94 kg (± 20.44); after 6 months, the average weight was 96.137 kg (± 20.67); and after 12 months, the average weight fell to 93.292 kg (± 20.16). This difference is statistically significant (p-value < 0.001).
BMI showed a significant difference (p-value < 0.001) over time, from the baseline average BMI of 39.38 (± 7.90) kg/m2 to an average BMI of 37.59 (± 7.8) kg/m2 at 6 months, falling to 36.52 (± 7.87) kg/m2 at 12 months.
FBS also shows a significant difference (p-value < 0.001) over time. At baseline, the mean was 10.60 mg/dL (± 4.29); after 6 months, it was 9.146 mg/dL (± 4.097) mg/dL; and at 12 months, it was 8.51 (± 3.58) mg/dL.
Serum creatinine for females also showed a significant difference (p-value < 0.001). There is a steady increase from baseline to 6 months, with the average level rising from 57.6 (± 15.8) μmol/L at baseline to 61.78 (± 19.16) μmol/L at 6 months. However, this level decreased, on average, between 6 and 12 months to an average mean of 60.8 (± 16.12) μmol/L.
The estimated GFR was significantly (p < 0.001) lower after 6 months than at baseline (98.75 ± 20.4 mL/min/1.73 m2 and 101 ± 18.46 mL/min/1.73 m2, respectively). The same goes for TC, which fell from an average total cholesterol of 4.550 (± 1.09) mmol/L at baseline to 4.366 (± 1.071) mmol/L at 6 months.
The difference in LDL was statistically significant (p-value < 0.05) but minor overall, with 2.64 (± 1.12) mmol/L at baseline dropping slightly to 2.383 (± 0.924) mmol/L after 6 months and 2.37 (± 0.935) mmol/L at 12 months.
Finally, for the ALP, it was found to be a statistically significant difference with a noticeable change after 6 months of 87.40 (± 31.16) IU/L.
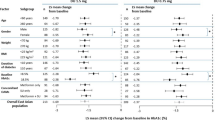
3.7 Differences Within the Group Over Time
Table 6 shows the differences within the group in terms of weight, BMI, HA1c, FBS, eGFR, TC, LDL, and ALT between baseline and after 6 months, between baseline and after 12 months, and between 6 and 12 months. We see a significant difference between weights; it appears that the highest difference was found to be between baseline and after 12 months with a mean difference of 8 kg [95% CI: (6.57, 9.59)] with p-value < 0.001; the difference in mean weight is smaller between 6 and 12 months, with a mean difference of 2.5 kg [95% CI: (1.67, 3.34)].
BMI showed a statistically significant difference at all three points (p-value < 0.05). The mean difference was largest between baseline and 6 months and between baseline and 12 months (mean difference: 2.19 and 3.16 kg/m2, respectively).
The same goes for HA1c; the difference is more prevalent after the first 6 months, where it is 1.12 (95% CI: 0.86, 1.39) lower. However, the level stabilized between 6 and 12 months, with a mean difference of just 0.31 (95% CI: 0.1, 0.52), although it was significant within the group (p-value < 0.05).
The difference in FBS level was significantly lower between baseline and 6 months and between baseline and 12 months only, with p-values < 0.05 (1.18 and 1.83 mg/dL, respectively).
Moreover, the mean difference in eGFR was significantly increased only between baseline and 6 months [mean difference: 2.9 mL/min/1.73 m2 (95% CI:1.2, 4.5)] and between baseline and 12 months [mean difference: 3.17 mL/min/1.73 m2 (95% CI: 1.08, 5.25)], with a p-value < 0.05.
TC only showed a significant change (p-value < 0.05) when viewed in the long term, with a mean difference of 0.26 mmol/L and 95% CI (0.05, 0.47) between baseline and 12 months.
The same goes for LDL and ALT, as the mean difference is significant between baseline and 6 months and between baseline and 12 months only.
4 Discussion
Dulaglutide, an approved long-acting GLP-1 RAs administered weekly, is indicated for treating adults with type 2 diabetes mellitus. Previous trials substantiated its effectiveness in glycemic control and weight reduction in obese patients [2]. Our study affirmed these findings, demonstrating a notable decrease in HA1c, FBS, and weight among patients using dulaglutide for a minimum of one year.
Dulaglutide has been assessed in several phase III trials, known as the global AWARD (Assessment of Weekly Administration of LY2189265 [dulaglutide] in diabetes) studies, showing that dulaglutide is generally an effective medication in maintaining glycemic control as monotherapy or if added to insulin or oral together with sustained weight loss and a low rate of hypoglycemia [5, 9, 13].
The Award 1–5 program, including phase 3 trial studies for dulaglutide, demonstrated mean weight loss ranging between 0.4 and 2.9 kg with a dulaglutide dose of 1.5 mg weekly for 26–52 weeks, either as monotherapy or in comparison with sitagliptin, exenatide or insulin glargine [14, 15]. Similar findings have been shown from several real-world studies regarding the efficacy of dulaglutide in lowering glucose with body weight reduction in patients with T2DM, including high-risk patients such as the elderly, patients with stage 3 or 4 chronic kidney disease, and patients with cardiovascular disease [10]; the most recent study was conducted in 2021 for Korean patients with T2DM and evaluated the glycemic efficacy of dulaglutide as an add-on to oral antidiabetic drugs (OADs) and basal insulin for 6 months [2, 16]. Our study demonstrates similar results in HbA1c reduction and slightly higher weight reduction, with a mean reduction of HbA1c by 1.12 after 6 months and 1.43% after 12 months and a body weight reduction of 5.57 kg after 6 months and approximately 8 kg after 12 months.
The Researching Cardiovascular Events with a Weekly Incretin in Diabetes (REWIND) trial assessed cardiovascular outcomes in diabetic patients on 1.5 mg dulaglutide and showed cardio and renal protection in patients with T2DM who are at high risk of cardiovascular events [13, 17]. As per our study, we did not assess the effect of dulaglutide on cardiovascular and renal protection; however, we observed a significant decrease in estimated glomerular filtration rate (eGFR) after 6 months compared to baseline (98.7 ± 20.4 and 101 ± 18.4 mL/min/1.7 m2, respectively), with a p-value less than 0.001. These findings may be explained by the chronicity of T2DM and its micro- and macrovascular complications. On the other hand, we also reported significant reductions in SBP, TC, and LDL levels in our study after 6 and 12 months. These results support similar findings reported in a post hoc analysis of the AWARD-11 study, conducted for participants who received once-weekly dulaglutide 1.5, 3.0, or 4.5 mg for 52 weeks, and showed that dulaglutide resulted in dose-related decreases in TC (≤ 6.0%) and TG (≤ 21.5%), with little change in LDL. SBP and DBP decreased up to 5.6 and 1.6 mmHg, respectively. These reductions have a positive impact on preventing cardiovascular disease [18]. Furthermore, extensive longitudinal studies must be conducted to assess the cardiovascular and renal benefits among Saudi patients.
Early mild gastrointestinal symptoms, including nausea, diarrhea, and vomiting, were the most reported adverse effects of dulaglutide in most AWARD studies, regardless of the injection doses, with a peak during the first 2 weeks of starting medication and then a rapid decline over the next 4 weeks. Other GI-related events, such as constipation, dyspepsia, and abdominal pain, were also reported [9]. However, the incidence of drug discontinuation due to severe GI events was rare, reaching 1.5% in participants taking 1.5 mg compared to 3.9% in participants taking 4.5 mg, as in the AWARD 2 study [3]. This was confirmed in our study, which showed nausea as the main side effect reported among participants, followed by other GI symptoms; approximately 31.8% of participants discontinued using dulaglutide after 12 months; of these, 30.7% (n = 18) cited side effects as their reason for discontinuing.
Six cases of pancreatitis were confirmed in the Award 2 study, and similar proportions of participants reported adverse events in the gallbladder. However, there were no reports of pancreatic cancer, C-cell hyperplasia, or medullary thyroid carcinoma during the study period in AWARD 2 and 3 [3, 16]. Participants reported a pancreatic carcinoma in the dulaglutide 1.5 mg treatment group in the AWARD 1 study, and one participant reported medullary thyroid carcinoma (MTC) in the dulaglutide 2.0 mg treatment group after approximately 6 months of starting medication in the AWARD 5 study [19]. In our study, one participant only experienced pancreatitis, one experienced gallbladder stones, and two reported cholecystitis; it was not definitively established whether those conditions were related to dulaglutide use. In general, these serious side effects are infrequent.
We found that nine participants experienced retinopathy after starting dulaglutide. The duration of dulaglutide use before retinopathy diagnosis is not precisely known because many diabetic patients are not routinely followed by ophthalmology, and some do not have a baseline retinal examination before starting dulaglutide. By reviewing previous trials, we found that a temporary worsening of diabetic retinopathy was reported in the REWIND study (8.5%) in the participants on dulaglutide, and it was reported in participants with a baseline history of diabetic retinopathy. There is no evidence that the GLP-1RA class has any direct harmful effect on the development or progression of diabetic retinopathy [9].
Multiple studies have also reported injection site reactions with mild symptoms, including pain, pruritus, and rash at the injection site [15]. Among our study population, only 12 participants reported some form of injection site reactions, which were mild and tolerable.
The incidence of documented severe hypoglycemia (i.e., plasma glucose of 54 mg/dL [3.0 mmol/L]) was very low in the comparison studies, reaching 1.3% of events per year in participants on dulaglutide 1.5 mg in the AWARD 2 study; no patient discontinued from the study due to hypoglycemia [9, 20]. In general, hypoglycemia was rarely reported in our findings, and most of those instances (7.35% of the total study population) were mild hypoglycemia, and only one participant reported severe hypoglycemia.
For liver enzymes, we reported a significant reduction only in ALP levels after 6 and 12 months from baseline, with means of 7.25 and 5.53 IU/L, respectively; these reductions were also reported in one meta-analysis study involving 12 studies with GLP-1RA arms and 677 subjects that showed that treatment with GLP-1RA reduced ALT, gamma-glutamyl transferase (GGT), and ALP with no change in AST level, leading to the conclusion that GLP-1RA treatment significantly reduces liver enzymes in patients with NAFLD [21].
There are inherent limitations in our study, as it is a single-arm study without either structured randomization or control groups, which can reduce the validity and significance of the study results. The study duration was short, which limits the strength of the outcome when assessing long-term safety and efficacy. Additionally, a retrospective cohort design can be associated with bias and confounding factors, which must be considered when interpreting findings.
However, despite the study’s limitations in its scope and duration, it achieved its primary objective, which was to assess the efficacy of once-weekly 1.5 mg dulaglutide therapy in improving glycemic control and weight loss in Saudi patients. It also provides practical and significant information to healthcare professionals in Saudi Arabia.
5 Conclusion
Our study has demonstrated that dulaglutide is a safe and effective treatment for improving glycemic control and reducing weight in people with T2DM and obesity of Saudi origin. Most side effects are mild and tolerable and mainly consist of GI symptoms and fatigue. The risk of severe side effects and hypoglycemia is rare, as reported both in our study and in previous real-world trials.
Further large-scale studies—preferably encompassing multiple centers from different cities in Saudi Arabia with larger study cohorts and long durations and assessing cardiovascular effects and cost benefits—are needed to support the utility of dulaglutide in the Saudi population.
Availability of Data and Materials
Original data generated and analyzed during this study are included in this published article.
Abbreviations
- ALT:
-
Alanine aminotransferase
- ALP:
-
Alkaline phosphatase
- AST:
-
Aspartate aminotransferase
- AWARD:
-
Assessment of weekly administration of LY2189265 [dulaglutide] in diabetes
- BMI:
-
Body mass index
- CVD:
-
Cardiovascular disease
- CKD:
-
Chronic kidney disease
- DM:
-
Diabetic mellitus
- DBP:
-
Diastolic blood pressure
- DLP:
-
Dyslipidemia
- eGFR:
-
Estimated glomerular filtration rate
- EASD:
-
European Association for the Study of Diabetes
- FBS :
-
Fasting blood sugar
- GGT:
-
Gamma-glutamyl transferase
- GI:
-
Gastrointestinal
- GLP-1 RAs:
-
Glucagon-like peptide 1 receptor agonists
- GLP-1:
-
Glucagon-like peptide 1
- GAD :
-
Glutamic acid decarboxylase
- GCC:
-
Gulf Cooperation Council
- HA1c:
-
Hemoglobin A1c
- ICA:
-
Islet cell antibodies
- KSMC:
-
King Saud Medical City
- LDL:
-
Low-density lipoprotein-cholesterol
- OADs:
-
Oral antidiabetic drugs
- RCTs.:
-
Randomized controlled trials
- REWIND:
-
Researching cardiovascular events with a weekly incretin in diabetes
- SGLT2:
-
Sodium-glucose transport protein 2
- SBP :
-
Systolic blood pressure
- ADA:
-
The American Diabetes Association
- TC:
-
Total cholesterol
- TG:
-
Triglyceride
- T2DM:
-
Type 2 diabetes mellitus
References
Abdul M, Khan B, Hashim MJ, King JK, Govender RD, Mustafa H, et al. Epidemiology of type 2 diabetes—global burden of disease and forecasted trends. J Epidemiol Glob Health. 2020;10:107–11.
Yoon JH, Hong AR, Choi W, Park JY, Kim HK, Kang HC. Real-world efficacy and safety of dulaglutide in korean patients with type 2 diabetes mellitus: a retrospective study in a tertiary referral center. Chonnam Med J. 2021;57(3):211.
Balducci S, Sacchetti M, Haxhi J, Orlando G, D’Errico V, Fallucca S, Menini S, Pugliese G. Physical exercise as therapy for type II diabetes. Diabetes Metab Res Rev. 2014;32(30):13–23.
Article R. Prevalence and reasons of increased type 2 diabetes in Gulf Cooperation Council Countries. Saudi Med J. 2021;42(5):481–90.
Wang W, Nevárez L, Filippova E, Song KH, Tao B, Gu L, et al. Efficacy and safety of once-weekly dulaglutide versus insulin glargine in mainly Asian patients with type 2 diabetes mellitus on metformin and/or a sulphonylurea: a 52-week open-label, randomized phase III trial. Diabetes Obes Metab. 2019;21(2):234–43.
Alwin Robert A, Abdulaziz Al Dawish M, Braham R, Ali Musallam M, Abdullah Al Hayek A, Hazza Al Kahtany N. Type 2 diabetes mellitus in Saudi Arabia: Major challenges and possible solutions. Curr Diabetes Rev. 2017;13(1):59–64.
Introduction: Standards of medical care in diabetes—2022, vol. 45, diabetes care. American Diabetes Association Inc.; 2022. p. S1–2.
Xu J, Yao DZ, Xia JY. Efficacy and safety of dulaglutide compared with glargine in patients with type 2 diabetes: a systematic review and meta-analysis. J Clin Pharm Ther. 2021;46(5):1245–53.
Macisaac RJ. Dulaglutide and Insulin: how Can the AWARD studies help guide clinical practice? Diabetes Ther [Internet]. 2020;11:1627–38. https://doi.org/10.6084/m9.figshare.12464588.
van den Boom L, Stuecher T, Mader JK. Safe use of a once-a-week glucagon-like peptide-1 receptor agonist in a 16-year-old girl with type 2 diabetes when approved therapy options fail. Clin Case Rep. 2021;9(9):1–6.
Anderson JE, Thieu VT, Boye KS, Hietpas RT, Garcia-Perez LE. Dulaglutide in the treatment of adult type 2 diabetes: a perspective for primary care providers. Postgrad Med. 2016;128(8):810–21. https://doi.org/10.1080/00325481.2016.1218260.
Xu J, Zhang Y, Li Y, Zhao X, et al. Pharmacokinetics, pharmacodynamics, and safety of dulaglutide after single or multiple doses in Chinese healthy subjects and patients with T2DM: a randomized, placebo-controlled, phase I study. Adv Ther. 2022;39(1):488–503. https://doi.org/10.1007/s12325-021-01921-5.
Pharmd DP. Glycaemic and non-glycaemic efficacy of once-weekly GLP-1 receptor agonists in people with type 2 diabetes. J Clin Pharm Ther. 2020;45:28–42.
Jendle J, Grunberger G, Blevins T, Giorgino F, Hietpas RT, Botros FT. Efficacy and safety of dulaglutide in the treatment of type 2 diabetes: a comprehensive review of the dulaglutide clinical data focusing on the AWARD phase 3 clinical trial program. Diabetes Metab Res Rev. 2016;32:776–90.
Umpierrez G, Povedano ST, Manghi FP, Shurzinske L, Pechtner V. Efficacy and safety of dulaglutide monotherapy versus metformin in type 2 diabetes in a randomized controlled trial (AWARD-3). Diabetes Care. 2014;37(8):2168–76.
Terauchi Y, Satoi Y, Takeuchi M, Imaoka T. Monotherapy with the once weekly GLP-1 receptor agonist dulaglutide for 12 weeks in Japanese patients with type 2 diabetes: dose-dependent effects on glycaemic control in a randomised, double-blind, placebo-controlled study. Endocr J. 2014;61(10):949–59.
Gerstein HC, Colhoun HM, Dagenais GR, Diaz R, Lakshmanan M, Pais P, et al. Dulaglutide and cardiovascular outcomes in type 2 diabetes (REWIND): a double-blind, randomised placebo-controlled trial. Lancet. 2019;394(10193):121–30.
Cox DA, Wang H, Nicolay C, Bethel MA. Effect of expanded dulaglutide weekly doses (3.0 mg and 4.5 mg) on cardiovascular disease risk factors in participants with type 2 diabetes at increased cardiovascular disease risk: a post hoc analysis of the AWARD-11 study. Diabetes Obes Metab. 2022;24(9):1770–8. https://doi.org/10.1111/dom.14762.
Frias JP, Bonora E, Ruiz LN, Li YG, Yu Z, Milicevic Z, et al. Efficacy and safety of dulaglutide 3.0 mg and 4.5 mg versus dulaglutide 1.5 mg in metformin-treated patients with type 2 diabetes in a randomized controlled trial (award-11). Diabetes Care. 2021;44(3):765–73.
Terauchi Y, Satoi Y, Takeuchi M, Imaoka T. Monotherapy with the once weekly GLP-1 receptor agonist dulaglutide for 12 weeks in Japanese patients with type 2 diabetes : dose-dependent effects on glycaemic control in a randomised, double-blind, placebo-controlled study. Endocr J. 2014;61(10):949–59.
Rezaei S, Tabrizi R, Nowrouzi-Sohrabi P, Jalali M, Atkin SL, Al-Rasadi K, et al. GLP-1 receptor agonist effects on lipid and liver profiles in patients with nonalcoholic fatty liver disease: systematic review and meta-analysis. Can J Gastroenterol Hepatol. 2021;2021:1–11.
Acknowledgements
The authors thank the Research and Innovation Center and The Adult Endocrine and Diabetic Department at KSMC for their assistance and contribution to this project. They would also like to thank all patients who participated in this study.
Funding
None.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study's conception and design. Material preparation and data collection were performed by M.S.A., R.N.A., and M.A.A. L.O.A. performed data analysis and management. M.S.A. wrote the first draft of the manuscript, and I.A.A. supervised the study. All authors commented on previous versions. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no conflict of interest.
Ethics Approval and Consent to Participate
Ethical approval was obtained from the research ethics committee at KSMC with reference number H1RI-01-Nov22-01, and approval was granted by the endocrinology department chairperson before we called the participants. The study intended not to harm participants, and information was kept confidential; consent was obtained before answering the questionnaire. Participants did not receive any payment for participating in this study, nor were they asked to pay for any procedure related to the study. Participants retained the right to withdraw at any time without mentioning the reasons and were free to refuse to answer any questions.
Consent for Publication
All authors consented to submission for publication.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Albargawi, M.S., Alharbi, R.N., Alajlani, M.A. et al. Efficacy and Safety of Injectable Dulaglutide 1.5 mg Among Type 2 Diabetes Patients in Clinics at King Saud Medical City, Riyadh, Saudi Arabia. J Epidemiol Glob Health (2024). https://doi.org/10.1007/s44197-024-00207-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s44197-024-00207-7