Abstract
Background
Sepsis remains a growing global health concern with soaring mortality and no direct anti-sepsis drug. Although smoking has distinct deleterious effects on chronic inflammatory illnesses and can impair immune function, a comprehensive analysis of the connection between sepsis and smoking is lacking.
Methods
This large-scale longitudinal cohort study retrospectively assessed adults aged ≥ 20 years who underwent national health checkups under the Korean National Health Insurance Service between January and December 2009 (N = 4,234,415) and were followed up for 10 years. Sepsis was identified based on the International Classification of Diseases, 10th Revision codes, and smoking status, including accumulated amount, was collected through a self-administered questionnaire. The Cox proportional hazard regression model was used, adjusting for age, sex, household income, body mass index, drinking, exercise, diabetes, hypertension, dyslipidemia, and chronic renal disease.
Results
After excluding cases with sepsis occurring before follow-up or after ≤ 1 year of follow-up, 3,881,958 participants, including non-smokers (N = 2,342,841), former smokers (N = 539,850), and active smokers (N = 999,267), were included. Compared to non-smokers, all active smokers (adjust hazard ratio: 1.41, 95% confidence interval 1.38–1.44) and former smokers (1.10, 1.07–1.14) with ≥ 20 pack-years exhibited a significantly higher risk of sepsis (p < 0.001). Smoking of ≥ 30 pack-years in former and active smokers groups significantly increased sepsis incidence (adjust hazard ratio [95% confidence interval] 1.34 [1.31–1.38], p < 0.001).
Conclusions
Smoking is closely associated with the incidence of sepsis. Smoking cessation may help in the primary prevention of sepsis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Sepsis is a life-threatening infection incurred by exaggerated and imbalanced inflammation, constituting a substantially important cause of death and morbidities worldwide [1, 2]. Despite advancements in intensive care, including early recolonization and initial resuscitation, the 30-day mortality attributable to sepsis remains high, exceeding 25–30% [3, 4]. Disturbingly, the high short-term mortality for patients with septic shock, which leads to more detrimental outcomes than sepsis, has not been decreasing recently [3]. The challenges of sepsis management originate from the absence of a specific anti-sepsis drug [5, 6]. Therefore, the current international guideline focuses on preventing or rapid recovery of tissue hypoperfusion-induced end-organ damage [1]. However, the protocol-based bundle approaches could not remarkably improve the prognosis of septic shock, and the most optimal therapeutic targets or goals to fundamentally resolve the intricate pathophysiology of sepsis are still lacking [6,7,8,9,10]. Therefore, prevention of hospital-acquired sepsis and modification of risk factors in lifestyle could be personalized countermeasures to reduce the disease burden of sepsis [11, 12].
Cigarette, a notorious carcinogen with widely documented adverse health impacts, has been recognized as being associated with a range of respiratory and cardiovascular diseases [13,14,15]. The global population of tobacco users was estimated to reach 1.3 billion in 2020, with smoking-related illnesses claiming approximately 8 million lives in 2019 [16, 17]. Smoking cessation remains a critical action to prevent medical illnesses, disabilities, and fatalities [18].
Many toxic chemicals in cigarettes can impair heterogeneous components of the innate and adaptive immune systems [19,20,21,22]. Immune dysfunction and immunosenescence from smoking predispose various organs, including the respiratory tract, to infections caused by pathogens [20, 21, 23,24,25]. Moreover, smoking-related chronic hyperinflammation and oxidative stress could increase the risk of developing sepsis-associated organ failure and worsen the outcome of sepsis [26,27,28,29,30]. Contrastingly, some studies reported that active smokers had a significantly lower all-cause in-hospital mortality in pneumonia or sepsis compared to that in non-smokers [22, 31,32,33,34].
Despite the conflicting findings between smoking and infection severity and the considerable social repercussions of smoking on public health, there are few large-scale evaluations to establish a definitive link between smoking and sepsis incidence. This study aimed to provide potential evidence substantiating the association of smoking with sepsis, utilizing a cohort of large community residents in South Korea, where the adult smoking rate was similar to the average of Organization for Economic Co-operation and Development countries [35].
2 Methods
2.1 Study Design and Database Source
This retrospective longitudinal cohort study was based on the healthcare promotion strategy of the Korean National Health Insurance Service (KNHIS), the solitary public insurance system requiring mandatory subscription [36]. The comprehensive system for claims collects medical information encompassing the International Classification of Disease, 10th Revision (ICD-10) diagnostic codes, prescriptions, medical treatments, and procedures in the KNHIS database [36]. The KNHIS provides the health assessment program (HEALS) biennially for individuals aged ≥ 20 years, without additional cost, including anthropometric measurements (height, weight, waist circumference, and blood pressure), a self-administered survey regarding prior/current chronic diseases with medication and health-related behaviors (cigarette smoking, drinking, and exercise), and fasting laboratory tests [37]. The data extraction from the KNHIS–HEALS databases was conducted with anonymized unique identification.
This study was reviewed and approved by the Institutional Review Board of Gangnam Severance Hospital (No. 3-2023-0267) and the National Health Insurance Sharing Service, with a waiver of the requirement for written informed consent. The study was conducted following the principles outlined in the Declaration of Helsinki.
2.2 Cohort Composition
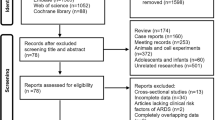
We screened all examinees (N = 4,234,415) in the KNHIS–HEALS databases from January 2009 to December 2009. Time zero was set as the date of health assessment in 2009. Exclusions comprised individuals with missing values (N = 333,176) and those previously diagnosed with sepsis during the wash-out period before time zero (N = 7,932). I addition, we excluded examinees who developed sepsis within one year from time zero (N = 11,349) to evaluate the potential causality between smoking and sepsis. Ultimately, the cohort consisted of 3,881,958 individuals. Follow-up extended from time zero through December 2020, ceasing at the occurrence of the first sepsis or death event; otherwise, it continued (Fig. 1).
2.3 Definitions
Sepsis was identified based on the ICD-10 codes that directly indicate sepsis, similar to those used in other retrospective cohort studies from a large-scale nationwide claims database, except O85 (puerperal sepsis), O88.3 (obstetric pyemic and septic embolism), and P36 (bacterial sepsis of newborn) (Supplementary Table 1) [38]. To further ensure the accuracy of sepsis diagnosis, we considered patients with the ICD-10 codes in the inpatient claims as the sepsis group.
The cigarette smoking behavior was categorized into three groups: non-smokers (participants who have never smoked before time zero), former smokers (participants who smoked but stopped before time zero), and active smokers (participants who continued to smoke at time zero). Total exposure to smoking in former and active smokers was divided into < 10, < 20, < 30, or ≥ 30 pack-years, calculated by multiplying total years by the average daily amount of smoking. The daily number of cigarettes in the self-questionnaire was divided by 20 to convert to pack units (Supplementary Table 2).
The degree of drinking was categorized into abstainers, mild to moderate (< 30 g/day), or heavy drinkers (> 30 g/day) based on the drinking days per week and the amount of alcohol consumed per day [39]. Regular exercise was defined as moderate-intensity physical activities performed ≥ 5 days a week for ≥ 30 min/day or vigorous-intensity physical activities performed ≥ 3 days a week for ≥ 20 min/day [40, 41]. Diabetes mellitus (DM), hypertension, dyslipidemia, and chronic kidney disease were identified based on ICD-10 codes or blood test results in the HEALS applying the diagnostic criteria as of 2009 or medication status at time zero for each disease (Supplementary Table 3). Body mass index (BMI) was subdivided into five levels: underweight (< 18.5 kg/m2), normal (18.5–22.9 kg/m2), overweight (23–24.9 kg/m2), obese I (25–29.9 kg/m2), and obese II (≥ 30 kg/m2) according to the Asia–Pacific standard of the World Health Organization [42]. The lowest quartile group of income status was defined as an annual household income lower than the 25th percentile based on the 2010 population and Housing Census in South Korea.
2.4 Statistical Analysis
Data were expressed as the median with interquartile range or mean ± standard deviation. The incidence rate (IR) of sepsis was calculated per 1000 person-years. A comparison of three groups according to smoking status was performed using the Kruskal–Wallis test for categorical variables and a one-way analysis of variance test for continuous variables. We evaluated the association between smoking and sepsis using the multivariate Cox proportional hazard regression models, expressing hazard ratio (HR) and 95% confidence interval (CI). Along with the unadjusted analysis (Model 1), the HRs of sepsis incidence were adjusted for age and sex in Model 2, or for age, sex, five levels of BMI, lowest income status, alcohol consumption, regular exercise, DM, hypertension, dyslipidemia, and chronic kidney disease in Model 3. Kaplan–Meier curves were generated to compare the cumulative incidence of sepsis by smoking status or accumulated amount, and significance was assessed using log-rank test. In all analyses using the SAS program (version 9.4), a two-tailed p ≤ 0.05 was considered statistically significant.
3 Results
3.1 Basic Characteristics
Our cohort was composed of non-smokers (N = 2,342,841, 60.4%), former smokers (N = 539,850, 13.9%), and active smokers (N = 999,267, 25.7%). Sepsis occurred in 82,061 participants during a median follow-up period of 10.3 years. The cumulative amount of cigarette smoking was 10 (5–20) and 12.5 (6.75–20) pack-years in former and active smokers, respectively. The active smokers had the lowest mean age (42.8 ± 12.5 years) and the highest proportion of people aged < 40 years (44.8%) (all p < 0.001). The proportion of women among ever-smokers was very low (6%). The former smokers group had the highest level of BMI and frequencies of obesity, DM, hypertension, and dyslipidemia (all p < 0.001). In addition to the high rate of metabolic abnormalities, including the highest glucose and total cholesterol values, the participants who exercised regularly were significantly typical in the former smokers compared to that in the non- or active smokers (25.3 vs. 17.0% or 16.3%, p < 0.001). The active smokers had a significantly higher frequency of heavy drinking than that in the non-smokers (17.8 vs. 2.4%, p < 0.001) (Table 1).
3.2 Comparison of Sepsis Incidence in Different Smoking Status and Amount
We observed a progressive increase in the IRs of sepsis with the more cumulative amount of smoking, ranging from 1.25 (< 10 pack-years) to 4.08 (≥ 20 pack-years) in former smokers and from 0.86 (< 10 pack-years) to 3.26/1000 person-years (≥ 20 pack-years) in active smokers. Total active smokers had a significantly higher risk of sepsis in model 2 than that in non-smokers, who were used as the reference (adjusted HR [aHR]: 1.41, 95% CI 1.38–1.44, and p < 0.001) (Table 2). The risk of sepsis in active smokers increased with a higher cumulative amount (aHR = 1.39 and 1.42 in < 10 and ≥ 20 pack-years, respectively) (Table 2). However, the risk of sepsis was significantly higher in former smokers than in non-smokers only if they had smoked ≥ 20 packs in total (aHR [95% CI] 1.07 [1.04–1.10]) or for ≥ 20 years (1.07 [1.04–1.09]), or had a cumulative amount of ≥ 20 pack-years (1.10 [1.07–1.14]) (Table 2 and Supplementary Table 4 and 5).
Analysis of total cumulative amount of smoking until time zero without considering smoking status at the time of starting follow-up showed that ever-smokers exhibited elevated risk of sepsis with greater levels of smoking exposure (aHR [95% CI] in model 2, 1.10 [1.07–1.13] in < 10 pack-years, 1.16 [1.13–1.19] in 10–20 pack-years, 1.19 [1.16–1.23] in 20–30 pack-years, and 1.34 [1.31–1.38] in ≥ 30 pack-years, p < 0.001) (Fig. 2 and Supplementary Table 6).
Effect of lifetime cumulative smoking amount on sepsis incidence regardless of smoking status at the time of health examination. The circles represent the hazard ratio adjusted with age, sex, lowest income status, five categories of body-mass index, regular exercise, alcohol consumption, diabetes mellitus, hypertension, dyslipidemia, chronic kidney disease, and the top and bottom of the bar represent the upper and lower values of the 95% confidence interval, respectively. aPer 1,000 person-years. F/U follow-up, CI confidence interval, HR hazard ratio, IR incidence rate, No number
The Kaplan–Meier curve also showed that the incidence of sepsis at time zero was significantly higher in active smokers than in non-smokers or former smokers, with a larger difference over time (p < 0.001). The incidence probability of sepsis was consistent in the non-smoker and former–smoker groups throughout the follow-up period. In addition, the occurrence of sepsis increased gradationally with the higher cumulative amount regardless of smoking status at the time of examination (p < 0.001) (Fig. 3).
Incidence probability of sepsis incidence according to smoking status or total accumulated amount during the entire observation period. A Smoking status. B Cumulative smoking amount. All incidence probabilities were adjusted by with age, sex, lowest income status, five categories of body-mass index, regular exercise, alcohol consumption, diabetes mellitus, hypertension, dyslipidemia, chronic kidney disease. Ex ex-smoker, PY pack-years
3.3 Risk of Sepsis According to Smoking Amount and Various Variables
The effect of smoking on the incidence of sepsis in women was higher than that in men (aHR [95% CI] in 0–10 pack-years from model 2, 1.50 [1.41–1.60] vs. 1.02 [0.98–1.05], p < 0.001). In the group aged ≥ 65 years with the highest IR of sepsis among all subgroups, smoking was significantly associated with an increased risk of sepsis (aHR [95% CI] in former and active smokers, 1.08 [1.05–1.12] and 1.45 [1.41–1.49], respectively, p < 0.001). However, smoking amount or status in participants aged < 40 years did not increase the risk of sepsis. Non-obese participants with a BMI of < 25 kg/m2 had a significantly higher incidence of sepsis than that observed in the obese participants at the same amount of smoking (Supplementary Fig. 1 and Table 7).
Even in groups that exercised regularly and abstained from alcohol as good health habits, smoking increased the incidence of sepsis (Supplementary Fig. 2 and Table 7). Smokers without DM (p for interaction < 0.001) or hypertension (p for interaction = 0.044) were significantly associated with a higher risk of sepsis than those without DM or hypertension, respectively (Supplementary Fig. 3 and Table 7).
4 Discussion
Our results provide evidence that cigarette smoking is a valid risk factor contributing to sepsis occurrence. Data from models adjusting for sepsis risk factors and subgroup analyses of various variables sufficiently support this conclusion. The association between smoking and increased incidence of sepsis, regardless of chronic illnesses or health behaviors (especially in cases of heavy smoking), suggests that smoking may independently affect sepsis development.
A major findings was that the positive relation between the accumulated amount of smoking and a higher risk of sepsis, even in former smokers. Active smokers with prolonged smoking exhibited a higher hazard than former or non-smokers. The incidence of sepsis was particularly increased among those who smoked ≥ 30 pack-years. However, former smokers who quit smoking with a small amount and/or a short duration had about a 10% lower risk of sepsis compared to non-smokers (aHR [95% CI] 0.90 [0.87–0.94] in < 10 pack-years and 0.93 [0.90–0.97] in 10–20 pack-years) (Table 2 and Supplementary Table 5 and 6). The influence of smoking was evident in older people aged ≥ 65 years, where the risk and poor outcome of sepsis substantially increased. The potential for smoking cessation to prevent critical infections need to be proven through interventional approaches, along with efforts to encourage smoking cessation.
Previous immunologic experiments reported that smoking has been associated with impaired phagocytic function and cytokine expression of T lymphocyte and macrophage in the reparatory tract or peripheral blood [19,20,21,22, 26, 43,44,45,46]. These studies collectively underscore the detrimental impact of smoking on the immune system, which persists even after smoking cessation. In addition, Huttunen et al. highlighted smoking as an independent risk factor for case fatality among 149 patients with bacteremia, with active smokers requiring more frequent intensive care unit care and mechanical ventilation compared to that required by non-smokers [47]. Moreover, the longitudinal cohort of the American National Center for Health Statistics showed that smokers had a larger hazard of death caused by septicemia (A40–A41 of the ICD-10 codes), which was approximately twice as high as those of non-smokers [30]. The report by Kempker et al. [30] aligned with our results, focusing on the risk of developing sepsis from a larger number of patients, including septic shock, and more detailed analyses about smoking duration and cumulative smoking amount.
Strategies to prevent prejudicial outcomes from sepsis include minimizing healthcare facility-associated infections and controlling progression to multi-organ dysfunctions after sepsis [11]. Conventional measures against infection, such as improved sanitation and enhanced herd immunity through vaccination, have been enormously effective as primary prevention for sepsis. However, public efforts to decrease the disease burden of sepsis by managing modifiable risk factors in the population have not received adequate attention. As data accumulates on the relation between smoking and sepsis, the alteration of smoking behavior as a lifestyle habit that aggravates many diseases will be quite cost-effective by blocking the occurrence of sepsis itself from the public health perspective. The negative impact of smoking on severe infection through immune dysfunction may also need to be highlighted to the same extent as in malignancies and cardiovascular diseases.
This study has several limitations. First, extracting sepsis events with diagnostic difficulties from the large database using ICD-10 codes may have resulted in a loss of cases or inclusion imprecision. A large number of events must be included to secure sufficient statistical power; however, prospectively or retrospectively defining sepsis through extensive review by medical staff would make big data analysis virtually unfeasible. Even though the incidence of sepsis can be affected by various factors, sepsis IR in our cohort (211/100,000 person-years) was within the same range as the Korean population-based study (266–453/100,000 person-years) and the meta-analysis of international epidemiology (148–288/100,000 person-years) [48,49,50]. This suggests that our sepsis screening did not deviate significantly from the general assessment. Second, smoking status and amount surveyed through self-questionnaires might not exactly match reality. In addition, the smoking history assessed once at time zero may have changed during the 10-year follow-up. The smoking rate among Korean adult men has steadily decreased from 47.0% in 2009 to 31.3% in 2021 [35]. Therefore, a substantial number of participants among active smokers at health examination may have stopped smoking during follow-up. However, among self-described lifestyle habits, smoking behavior is judged to be the item with a lower probability of being falsely stated. Moreover, dividing the total smoking amount into 10-pack-year intervals could reduce bias due to smoking cessation during follow-up. Despite the possibility of changes in smoking status, our data may have meaningful implications that the cumulative amount of smoking before a certain point can predict an increased risk of sepsis. Third, in line with the characteristics of the Korean population, with the lowest female smoking rate among Organization for Economic Co-operation and Development member nations [35], almost all former or active smokers in our cohort were men. Last, we investigated only cigarettes among various vaporizing tobacco products.
5 Conclusions
This large longitudinal cohort study presents that cigarette smoking status and cumulative smoking amounts are independently associated with a higher incidence of sepsis. The risk of sepsis was higher even for heavy former smokers than for non-smokers. The older smoking population, with basically the highest incidence and worst outcomes of sepsis due to various risk factors, was especially vulnerable to sepsis. With the increasing awareness that sepsis is a public health problem that can be prevented by smoking cessation, these findings suggest that sepsis also needs to be highlighted in public notice and prevention campaigns regarding the adverse health effects of smoking.
Availability of Data and Materials
Not applicable.
References
Evans L, Rhodes A, Alhazzani W, Antonelli M, Coopersmith CM, French C, Machado FR, McIntyre L, Ostermann M, Prescott HC, Schorr C, Simpson S, Wiersinga WJ, Alshamsi F, Angus DC, Arabi Y, Azevedo L, Beale R, Beilman G, Belley-Cote E, Burry L, Cecconi M, Centofanti J, Coz Yataco A, De Waele J, Dellinger RP, Doi K, Du B, Estenssoro E, Ferrer R, Gomersall C, Hodgson C, Moller MH, Iwashyna T, Jacob S, Kleinpell R, Klompas M, Koh Y, Kumar A, Kwizera A, Lobo S, Masur H, McGloughlin S, Mehta S, Mehta Y, Mer M, Nunnally M, Oczkowski S, Osborn T, Papathanassoglou E, Perner A, Puskarich M, Roberts J, Schweickert W, Seckel M, Sevransky J, Sprung CL, Welte T, Zimmerman J, Levy M. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Intensive Care Med. 2021;47:1181–247. https://doi.org/10.1007/s00134-021-06506-y.
Rudd KE, Kissoon N, Limmathurotsakul D, Bory S, Mutahunga B, Seymour CW, Angus DC, West TE. The global burden of sepsis: barriers and potential solutions. Crit Care. 2018;22:232. https://doi.org/10.1186/s13054-018-2157-z.
Bauer M, Gerlach H, Vogelmann T, Preissing F, Stiefel J, Adam D. Mortality in sepsis and septic shock in Europe, North America and Australia between 2009 and 2019- results from a systematic review and meta-analysis. Crit Care. 2020;24:239. https://doi.org/10.1186/s13054-020-02950-2.
Vincent JL, Marshall JC, Namendys-Silva SA, François B, Martin-Loeches I, Lipman J, Reinhart K, Antonelli M, Pickkers P, Njimi H, Jimenez E, Sakr Y. Assessment of the worldwide burden of critical illness: the intensive care over nations (ICON) audit. Lancet Respir Med. 2014;2:380–6. https://doi.org/10.1016/s2213-2600(14)70061-x.
van der Poll T, van de Veerdonk FL, Scicluna BP, Netea MG. The immunopathology of sepsis and potential therapeutic targets. Nat Rev Immunol. 2017;17:407–20. https://doi.org/10.1038/nri.2017.36.
Cohen J, Vincent JL, Adhikari NK, Machado FR, Angus DC, Calandra T, Jaton K, Giulieri S, Delaloye J, Opal S, Tracey K, van der Poll T, Pelfrene E. Sepsis: a roadmap for future research. Lancet Infect Dis. 2015;15:581–614. https://doi.org/10.1016/s1473-3099(15)70112-x.
Osborn TM. Severe sepsis and septic shock trials (ProCESS, ARISE, ProMISe): what is optimal resuscitation? Crit Care Clin. 2017;33:323–44. https://doi.org/10.1016/j.ccc.2016.12.004.
Seymour CW, Gesten F, Prescott HC, Friedrich ME, Iwashyna TJ, Phillips GS, Lemeshow S, Osborn T, Terry KM, Levy MM. Time to treatment and mortality during mandated emergency care for sepsis. N Engl J Med. 2017;376:2235–44. https://doi.org/10.1056/NEJMoa1703058.
Mouncey PR, Osborn TM, Power GS, Harrison DA, Sadique MZ, Grieve RD, Jahan R, Harvey SE, Bell D, Bion JF, Coats TJ, Singer M, Young JD, Rowan KM. Trial of early, goal-directed resuscitation for septic shock. N Engl J Med. 2015;372:1301–11. https://doi.org/10.1056/NEJMoa1500896.
De Backer D, Cecconi M, Lipman J, Machado F, Myatra SN, Ostermann M, Perner A, Teboul JL, Vincent JL, Walley KR. Challenges in the management of septic shock: a narrative review. Intensive Care Med. 2019;45:420–33. https://doi.org/10.1007/s00134-019-05544-x.
Kempker JA, Wang HE, Martin GS. Sepsis is a preventable public health problem. Crit Care. 2018;22:116. https://doi.org/10.1186/s13054-018-2048-3.
Markwart R, Saito H, Harder T, Tomczyk S, Cassini A, Fleischmann-Struzek C, Reichert F, Eckmanns T, Allegranzi B. Epidemiology and burden of sepsis acquired in hospitals and intensive care units: a systematic review and meta-analysis. Intensive Care Med. 2020;46:1536–51. https://doi.org/10.1007/s00134-020-06106-2.
Rigotti NA. Smoking cessation in patients with respiratory disease: existing treatments and future directions. Lancet Respir Med. 2013;1:241–50.
Larsson SC, Burgess S, Michaëlsson K. Smoking and stroke: a Mendelian randomization study. Ann Neurol. 2019;86:468–71. https://doi.org/10.1002/ana.25534.
Larsson SC, Mason AM, Bäck M, Klarin D, Damrauer SM, Michaëlsson K, Burgess S. Genetic predisposition to smoking in relation to 14 cardiovascular diseases. Eur Heart J. 2020;41:3304–10. https://doi.org/10.1093/eurheartj/ehaa193.
World Health Organization. WHO global report on trends in prevalence of tobacco use 2000–2025, fourth edition [Internet]. 2021. Available from: https://www.who.int/publications/i/item/9789240039322. [cited 2023, November 15].
GBD 2019 Risk Factors Collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1223–49. https://doi.org/10.1016/s0140-6736(20)30752-2.
National Center for Chronic Disease Prevention and Health Promotion Office on Smoking and Health. The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General [Internet]. Wiley Online Library; 2014. Available from: https://www.ncbi.nlm.nih.gov/books/NBK179276/. [cited 2023, November 30].
Mehta H, Nazzal K, Sadikot RT. Cigarette smoking and innate immunity. Inflamm Res. 2008;57:497–503. https://doi.org/10.1007/s00011-008-8078-6.
Martos SN, Campbell MR, Lozoya OA, Wang X, Bennett BD, Thompson IJB, Wan M, Pittman GS, Bell DA. Single-cell analyses identify dysfunctional CD16(+) CD8 T cells in smokers. Cell Rep Med. 2020. https://doi.org/10.1016/j.xcrm.2020.100054.
Feldman C, Anderson R. Cigarette smoking and mechanisms of susceptibility to infections of the respiratory tract and other organ systems. J Infect. 2013;67:169–84. https://doi.org/10.1016/j.jinf.2013.05.004.
Stämpfli MR, Anderson GP. How cigarette smoke skews immune responses to promote infection, lung disease and cancer. Nat Rev Immunol. 2009;9:377–84. https://doi.org/10.1038/nri2530.
Nuorti JP, Butler JC, Farley MM, Harrison LH, McGeer A, Kolczak MS, Breiman RF. Cigarette smoking and invasive pneumococcal disease. Active Bacterial Core Surveillance Team. N Engl J Med. 2000;342:681–9. https://doi.org/10.1056/nejm200003093421002.
van Zyl-Smit RN, Richards G, Leone FT. Tobacco smoking and COVID-19 infection. Lancet Respir Med. 2020;8:664–5. https://doi.org/10.1016/S2213-2600(20)30239-3.
Gajalakshmi V, Peto R, Kanaka TS, Jha P. Smoking and mortality from tuberculosis and other diseases in India: retrospective study of 43000 adult male deaths and 35000 controls. Lancet. 2003;362:507–15. https://doi.org/10.1016/s0140-6736(03)14109-8.
Elisia I, Lam V, Cho B, Hay M, Li MY, Yeung M, Bu L, Jia W, Norton N, Lam S, Krystal G. The effect of smoking on chronic inflammation, immune function and blood cell composition. Sci Rep. 2020;10:19480. https://doi.org/10.1038/s41598-020-76556-7.
Zhang N, Liu Y, Yang C, Zeng P, Gong T, Tao L, Li X. Association between smoking and risk of death in patients with sepsis: a systematic review and meta-analysis. Tob Induc Dis. 2022;20:65. https://doi.org/10.18332/tid/150340.
Purkayastha A, Sen C, Garcia G Jr, Langerman J, Shia DW, Meneses LK, Vijayaraj P, Durra A, Koloff CR, Freund DR, Chi J, Rickabaugh TM, Mulay A, Konda B, Sim MS, Stripp BR, Plath K, Arumugaswami V, Gomperts BN. Direct exposure to SARS-CoV-2 and cigarette smoke increases infection severity and alters the stem cell-derived airway repair response. Cell Stem Cell. 2020;27:869-75.e4. https://doi.org/10.1016/j.stem.2020.11.010.
Caliri AW, Tommasi S, Besaratinia A. Relationships among smoking, oxidative stress, inflammation, macromolecular damage, and cancer. Mutat Res Rev Mutat Res. 2021;787: 108365. https://doi.org/10.1016/j.mrrev.2021.108365.
Kempker JA, Kramer MR, Waller LA, Martin GS. Risk factors for septicemia deaths and disparities in a longitudinal US cohort. Open Forum Infect Dis. 2018;5: ofy305. https://doi.org/10.1093/ofid/ofy305.
Beatty JA, Majumdar SR, Tyrrell GJ, Marrie TJ, Eurich DT. Current smoking and reduced mortality in bacteremic pneumococcal pneumonia: a population-based cohort study. Chest. 2016;150:652–60. https://doi.org/10.1016/j.chest.2016.04.020.
Garau J, Baquero F, Pérez-Trallero E, Pérez JL, Martín-Sánchez AM, García-Rey C, Martín-Herrero JE, Dal-Ré R. Factors impacting on length of stay and mortality of community-acquired pneumonia. Clin Microbiol Infect. 2008;14:322–9. https://doi.org/10.1111/j.1469-0691.2007.01915.x.
Fisman DN, Abrutyn E, Spaude KA, Kim A, Kirchner C, Daley J. Prior pneumococcal vaccination is associated with reduced death, complications, and length of stay among hospitalized adults with community-acquired pneumonia. Clin Infect Dis. 2006;42:1093–101. https://doi.org/10.1086/501354.
Marrie TJ, Wu L. Factors influencing in-hospital mortality in community-acquired pneumonia: a prospective study of patients not initially admitted to the ICU. Chest. 2005;127:1260–70. https://doi.org/10.1378/chest.127.4.1260.
OECD. Health at a glance 2023, OECD Indicators [Internet]. Available from: https://www.oecd.org/health/health-at-a-glance/. [cited 2023, November 23].
Cheol Seong S, Kim YY, Khang YH, Heon Park J, Kang HJ, Lee H, Do CH, Song JS, Hyon Bang J, Ha S, Lee EJ, Ae SS. Data resource profile: the National Health Information Database of the National Health Insurance Service in South Korea. Int J Epidemiol. 2017;46:799–800. https://doi.org/10.1093/ije/dyw253.
Seong SC, Kim YY, Park SK, Khang YH, Kim HC, Park JH, Kang HJ, Do CH, Song JS, Lee EJ, Ha S, Shin SA, Jeong SL. Cohort profile: the National Health Insurance Service-National Health Screening Cohort (NHIS-HEALS) in Korea. BMJ Open. 2017;7: e016640. https://doi.org/10.1136/bmjopen-2017-016640.
Tonai M, Shiraishi A, Karumai T, Endo A, Kobayashi H, Fushimi K, Hayashi Y. Hospital-onset sepsis and community-onset sepsis in critical care units in Japan: a retrospective cohort study based on a Japanese administrative claims database. Crit Care. 2022;26:136. https://doi.org/10.1186/s13054-022-04013-0.
Jeon KH, Han K, Jeong SM, Park J, Yoo JE, Yoo J, Lee J, Kim S, Shin DW. Changes in alcohol consumption and risk of dementia in a nationwide cohort in South Korea. JAMA Netw Open. 2023;6: e2254771. https://doi.org/10.1001/jamanetworkopen.2022.54771.
Nam GE, Cho KH, Park YG, Han KD, Choi YS, Kim SM, Lee KS, Ko BJ, Kim YH, Han BD, Kim DH. Socioeconomic status and dyslipidemia in Korean adults: the 2008–2010 Korea National Health and Nutrition Examination Survey. Prev Med. 2013;57:304–9. https://doi.org/10.1016/j.ypmed.2013.06.008.
Södergren M, Sundquist J, Johansson SE, Sundquist K. Physical activity, exercise and self-rated health: a population-based study from Sweden. BMC Public Health. 2008;8:352. https://doi.org/10.1186/1471-2458-8-352.
World Health Organization Western Pacific Region. The Asia-Pacific perspective: Redefining obesity and its treatment [Internet]. 2000. Available from: https://iris.who.int/bitstream/handle/10665/206936/0957708211_eng.pdf. [cited 2023, November 23].
van Zyl-Smit RN, Binder A, Meldau R, Semple PL, Evans A, Smith P, Bateman ED, Dheda K. Cigarette smoke impairs cytokine responses and BCG containment in alveolar macrophages. Thorax. 2014;69:363–70. https://doi.org/10.1136/thoraxjnl-2013-204229.
Ekberg-Jansson A, Andersson B, Avrå E, Nilsson O, Löfdahl CG. The expression of lymphocyte surface antigens in bronchial biopsies, bronchoalveolar lavage cells and blood cells in healthy smoking and never-smoking men, 60 years old. Respir Med. 2000;94:264–72. https://doi.org/10.1053/rmed.1999.0735.
Hagiwara E, Takahashi KI, Okubo T, Ohno S, Ueda A, Aoki A, Odagiri S, Ishigatsubo Y. Cigarette smoking depletes cells spontaneously secreting Th(1) cytokines in the human airway. Cytokine. 2001;14:121–6. https://doi.org/10.1006/cyto.2001.0860.
King TE Jr, Savici D, Campbell PA. Phagocytosis and killing of Listeria monocytogenes by alveolar macrophages: smokers versus nonsmokers. J Infect Dis. 1988;158:1309–16. https://doi.org/10.1093/infdis/158.6.1309.
Huttunen R, Laine J, Lumio J, Vuento R, Syrjanen J. Obesity and smoking are factors associated with poor prognosis in patients with bacteraemia. BMC Infect Dis. 2007;7:13. https://doi.org/10.1186/1471-2334-7-13.
Kim J, Kim K, Lee H, Ahn S. Epidemiology of sepsis in Korea: a population-based study of incidence, mortality, cost and risk factors for death in sepsis. Clin Exp Emerg Med. 2019;6:49–63. https://doi.org/10.15441/ceem.18.007.
Fleischmann-Struzek C, Mellhammar L, Rose N, Cassini A, Rudd KE, Schlattmann P, Allegranzi B, Reinhart K. Incidence and mortality of hospital- and ICU-treated sepsis: results from an updated and expanded systematic review and meta-analysis. Intensive Care Med. 2020;46:1552–62. https://doi.org/10.1007/s00134-020-06151-x.
Fleischmann C, Scherag A, Adhikari NK, Hartog CS, Tsaganos T, Schlattmann P, Angus DC, Reinhart K. Assessment of global incidence and mortality of hospital-treated sepsis. Current estimates and limitations. Am J Respir Crit Care Med. 2016;193:259–72. https://doi.org/10.1164/rccm.201504-0781OC.
Funding
No external funding was received for this study.
Author information
Authors and Affiliations
Contributions
SHH and KDH took responsibility for the integrity of the data and data analysis accuracy. EHL, SHH, and KDH developed the research concept and design. KL and YP performed all processes of acquisition and analysis of data and statistical analyses. EHL and SHH co-drafted the article and produced all figures. All authors contributed to the data interpretation and reviewed the article for important intellectual content. All authors have read and agreed to the final version of the manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
All authors have no conflict of interest in the study.
Ethical approval
The study was reviewed and approved by the Institutional Review Board of Gangnam Severance Hospital (No. 3-2023-0267) and the National Health Insurance Sharing Service, with a waiver of the requirement for written informed consent. This study was conducted following the principles outlined in the Declaration of Helsinki.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lee, E.H., Lee, K.H., Lee, Kn. et al. The Relation Between Cigarette Smoking and Development of Sepsis: A 10-Year Follow-Up Study of Four Million Adults from the National Health Screening Program. J Epidemiol Glob Health 14, 444–452 (2024). https://doi.org/10.1007/s44197-024-00197-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s44197-024-00197-6