Abstract
The widespread occurrence of multi-resistant bacteria is a health problem of global dimension. Infections caused by multi-resistant pathogens are difficult to treat and often associated with high mortality. Therefore, new treatment strategies are of interest, such as the use of differently acting antibacterial concepts. One of these new concepts is the use of antiseptics in combination with the antibacterial photodynamic therapy (aPDT). Currently, no method has yet been established as a standard procedure for investigating combined effects and evaluating them in a generally valid and unambiguous manner. The focus of this study was on how cationic antiseptics benzalkonium chloride (BAC) and chlorhexidine digluconate (CHX) behave in a combined application with aPDT using the photosensitizer TMPyP. For this purpose, BAC and CHX were applied in combination with the aPDT using TMPyP in non-lethal concentrations to the three bacteria Escherichia coli, Staphylococcus aureus, and Enterococcus faecalis. The results of the combination experiments with sublethal concentrations of BAC or CHX with the aPDT showed that the binary application had a lethal effect. Irrespective of the bacteria, the reduction in concentrations in OPECC, compared to individual concentrations, was more than 50% for TMPyP, 23–40% for BAC, and 18–43% for CHX. Furthermore, the optimal effective concentration combinations (OPECCs) could be determined. The latter showed that the combined application allowed the reduction of both concentrations compared to the single application.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Antimicrobial resistance (AMR) has emerged as one of the greatest public health challenges of our time [1, 2]. For instance, AMR was called an overlooked pandemic persisting in the shadows of COVID-19 in a comment on the report of the Antimicrobial Resistance Collaborators group around Christopher Murray that was published 2022 in the Lancet [3]. This report identified AMR as the leading cause of death globally in 2019, with 4.95 million deaths related to AMR and 1.27 million deaths directly caused by AMR [4]. During the COVID-19 pandemic, there was also an increased use of biocides and antiseptics for various applications, such as preprocedural mouthwashes [5], which may have posed the risk of accelerating the spread of AMR by exerting selection pressure and promoting mutations and horizontal gene transfer among microorganisms [6].
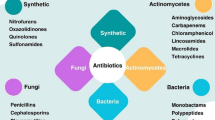
Therefore, there is an urgent need of alternative treatment approaches that are capable of inactivating resistant microorganisms without posing the risk of inducing new resistances in bacteria [7,8,9]. One of these approaches is antimicrobial photodynamic therapy (aPDT), which relies on the combination of an intrinsically non-toxic dye (called a photosensitizer, PS), light of a wavelength (no UV) suitable for exciting the PS, and molecular oxygen to inactivate bacteria through an oxidative process [10]. Upon absorption of a photon, the PS enters an excited state, from which there are two mechanisms to return to the ground state. In type I mechanism, charge is transferred to oxygen or other substrates leading to the generation of reactive oxygen species (ROS) such as superoxide radicals (O2−⋅), hydroxyl radicals (HO⋅), or hydrogen peroxide (H2O2), while in type II mechanism, energy is transferred directly to molecular oxygen leading to generation of high-energy singlet oxygen (1O2) [8, 9]. The ratio of both processes is described by the singlet oxygen quantum yield ΦΔ which is unique for each PS and depends on the respective chemical structure. Particularly, PS that mainly acts according to type II mechanism such as the fourfold positively charged porphyrin derivative TMPyP [5,10,15,20-Tetrakis-(N-methyl-4-pyridyl)-21,23H-porphine tetratosylate)] has shown promising antibacterial efficacy in vitro [11,12,13,14,15].
Due to the continuing spread of AMR, it has also been proposed to combine multiple antimicrobial compounds or approaches as new treatment strategies against infections caused by bacteria resistant to conventional therapeutic regimens [16,17,18]. Evaluating potential “synergistic” effects of binary combinations of antibacterial compounds or approaches can be challenging due to unclear definitions of what “synergism” actually means [19,20,21,22]. Our group recently proposed an extension of the conventional checkerboard method for evaluation of binary combinations of antimicrobials that allows one concentration pair to be determined as an optimal effective concentration combination (OPECC), independent of the various synergy principles [22]. When selecting such binary combinations of antibacterial compounds or approaches, it may be worthwhile to choose some with similar cellular targets in bacteria to potentially achieve “synergistic” effects [22,23,24]. For aPDT, there has been some debate about the actual cellular target structures [25, 26], but recent research suggests that aPDT mainly acts on bacterial cytoplasmic membranes [13, 27,28,29,30]. Cationic biocides and antiseptics such as the quaternary ammonium compound (QAC) benzalkonium chloride (BAC) and the bisbiguanide chlorhexidine digluconate (CHX) also target cytoplasmic membranes by forming hydrophilic domains that impede membrane functions and finally lead to leakage of cytoplasmic components [31, 32].
The aim of the present study was to investigate the effects of binary applications of the antiseptics BAC and CHX with TMPyP-mediated aPDT toward planktonic cultures of Escherichia coli, Staphylococcus aureus, and Enterococcus faecalis. Particularly, we investigated whether it was possible to determine OPECCs for the respective combination treatments and whether the antibacterial efficacy could be influenced by the order of application of antiseptics and aPDT.
2 Materials and methods
2.1 Bacterial strains and culture conditions
Staphylococcus aureus (ATCC 25923), Escherichia coli (ATCC 25922), and Enterococcus faecalis (ATCC 4083) were obtained from DSMZ (Deutsche Sammlung von Mikroorganismen und Zellkulturen, Braunschweig, Germany) and grown on Mueller–Hinton (MH; S. aureus, E. coli) or Brain Heart Infusion (BHI; E. faecalis) agar plates, provided by the Institute for Clinical Microbiology and Hygiene (University Hospital Regensburg, Germany). Single colonies were inoculated in 5 mL MH (Merck, Darmstadt, Germany; S. aureus, E. coli) or BHI (Sigma-Aldrich, St. Louis, MO, USA; E. faecalis) broth, respectively, and incubated as overnight cultures on an orbital shaker (180 rpm) under aerobic conditions at 37 °C. Then, each culture was centrifuged at 2500g for 10 min at 20 °C, and the pellets were resuspended in a phosphate-buffered saline solution (PBS; Dulbecco’s phosphate-buffered saline; Sigma-Aldrich, St. Louis, MO, USA) and adjusted to an optical density (OD) of 0.1 at 600 nm (SPECORD 50 Plus, Analytik Jena, Jena, Germany) to be used for the checkerboard method.
2.2 Test substances and light source
TMPyP [5,10,15,20-Tetrakis-(N-methyl-4-pyridyl)-21,23H-porphine tetratosylate], chlorhexidine digluconate (CHX), and benzalkonium chloride were obtained from Sigma-Aldrich. For irradiation of TMPyP, a gas-discharge lamp (Waldmann UV 236; Waldmann Medizintechnik, Villingen-Schwenningen, Germany; λem 380–600 nm) was used with irradiance adjusted to 18 mW/cm2 at sample level.
2.3 Minimum inhibitory concentrations (MICs)
For each bacterial strain, the minimum inhibitory concentrations (MICs) of the three individual antibacterial approaches BAC, CHX, and TMPyP-mediated aPDT were determined according to the classic method [22, 33]. A 48-well plate was filled with 250 µL each of the compounds (CHX, BAC, TMPyP) in a twofold dilution series and 250 µL of bacterial suspension and then incubated overnight at 37 °C. In case of TMPyP, the wells were either exposed to irradiation for 10 min (light dose: 10.8 J/cm2) and then incubated overnight in the dark or kept in the dark at all (dark control). After overnight incubation, the MICs of each agent were determined visually.
2.4 Checkerboard assay
Based on the MICs determined, the checkerboard method [20, 34, 35] was used in 48-well plates to evaluate the binary combination experiments, according to the method used in our laboratory described in detail earlier [22]. The antiseptics BAC and CHX, respectively, were applied in binary combination with aPDT using the PS TMPyP. Four different experimental conditions with six replicates each were considered for each binary combination against E. coli, S. aureus, and E. faecalis. Sterility and growth controls were included in each experiment. All experiments were performed with (experimental situation) and without (dark control) light exposure. In the binary application, two different sequences of application were examined each. The evaluation was done immediately after application or after 10 min. To identify a potential pattern of antiseptic interactions with aPDT, four experimental conditions were examined and termed 0_0, 0_10, 10_0, and 10_10, whereby the first digit 0 or 10 represents the incubation period in minutes of BAC or CHX, and the second represents the incubation period in minutes of the PS TMPyP. The plates were either irradiated for 10 min or kept in the dark during the same period (dark control).
Each well in the checkerboard system contained a volume of 500 µL, comprising 125 µL of each compound and 250 µL of the respective bacterial suspension. After irradiation for 10 min or keeping in the dark for the same period in case of dark controls, 250 µL was taken from each well and transferred to another 48-well plate each containing 250 µL of pre-loaded culture broth and incubated overnight, protected from light. After this incubation period, each well was visually rated as turbid (growth of bacteria) or not (no growth, i.e., effective eradication of the bacterial sample).
2.5 Optimal effective concentration combinations (OPECCs)
The evaluation of the checkerboard results of the present study was based on the determination of the optimal effective concentration combinations (OPECCs) as introduced recently [22]. In this previous study, OD readings from a checkerboard plate were plotted against the concentration combination pairs and fitted three-dimensionally (TableCurve 3D v 4.0; SYSTAT), resulting in a two-dimensional surface in the three-dimensional Euclidean space. The borderline between no growth and growth was fitted two-dimensionally (TableCurve 2D v 5.01; SYSTAT). From this fit, the inflection point and the corresponding 95% confidence limits in both dimensions were derived and denominated as OPECC [22].
In the present work, the dichotomous results (turbid or not) of each well were determined. From this, the frequency of occurrence of turbidity of the six samples was determined for a given binary combination and normalized to the interval between 0 and 1. These frequencies were then subjected to analysis as briefly described above and detailed in [22] to determine the OPECCs of binary combinations of TMPyP-mediated aPDT with BAC or CHX, respectively. The two-dimensional fitted curves, from which the OPECCs were derived, were further used to determine the marginal concentrations, including the associated confidence intervals, of the single compounds. That is, the concentrations to be used for each of the two substances were determined when the other is zero.
2.6 Statistical analysis
The OPECC was depicted graphically along with its associated 95% confidence limits in both directions [22]. The discriminatory statistics were performed using an extended Tukey interval method. The results of two study groups were assessed as significantly different if the two rectangles that were spanned by the confidence limits in both directions did not overlap. Results of individual substances were statistically evaluated in an analogous manner using the usual 1-dimensional Tukey interval method.
3 Results
The results of the determination of the OPECCs and marginal single concentrations are summarized in Fig. 1. OPECCs were determinable for all experimental conditions (0_0, 0_10, 10_0, and 10_10) of both binary combinations of BAC or CHX with aPDT for all bacteria E. coli, S. mutans, and E. faecalis examined, except for CHX with aPDT against E. coli under condition 0_10. The individual concentrations of all determinable OPECCs were all lower than the respective concentrations in the individual applications (red and blue symbols in Fig. 1, respectively). No pattern of antiseptic interactions with aPDT could be detected with respect to the influence of the four experimental conditions (black symbols in Fig. 1). Only for the experimental condition 0_0 at BAC (open black circles) a tendency was observed that the OPECCs showed the lowest concentrations (TMPyP; BAC): E. coli (7700 µg/mL; 4000 µg/mL), S. aureus (8200 µg/mL; 2500 µg/mL), and E. faecalis (9300 µg/mL; 3900 µg/mL)). Furthermore, all determinable OPECCs were significantly different from the concentrations in each individual application (i.e., results shown in black versus blue or red), except for the binary combination of aPDT with CHX under the conditions 0_10 and 10_0. For all determinable OPECCs, the OPECCs for each pairwise comparison of the four experimental conditions (i.e., the different symbols of the results shown in black against each other) were significantly different from each other. CHX concentrations required as monotherapy were highest for E faecalis (14 µg/mL or higher) compared to the other bacteria (less than 8 µg/mL) tested (red symbols) (Fig. 1). Irrespective of the bacteria, the reduction in concentrations in OPECC, compared to individual concentrations was more than 50% for TMPyP, 23–40% for BAC and 18–43% for CHX. All dark controls showed no antimicrobial effect of the PS TMPyP on the results (data not shown).
OPECCs (see [22]) of the binary application of BAC and CHX with TMPyP-mediated aPDT (left and right columns, respectively) against E. coli, S. aureus, and E. faecalis (top, middle and bottom rows, respectively) with corresponding 95% confidence limits in both directions (black symbols and lines), as well as marginal concentrations with corresponding 95% confidence limits of the compounds (BAC or CHX) or TMPyP-mediated aPDT alone (red or blue symbols and lines, respectively). The confidence limits may be overlaid by the respective symbols. The different symbols of each color indicate the experimental conditions 0_0, 0_10, 10_0, and 10_10, where the first digit 0 or 10 represents the incubation period in minutes of BAC or CHX, and the second represents the incubation period in minutes of TMPyP. The exposure period was 600 s for E. coli and S. aureus, and 1200 s for E. faecalis. The results are based on six independent samples. If a symbol is not plotted in the graph, either no OPECC could be determined in the respective binary application (black symbols) or the marginal concentrations of the application of the single compounds were not derivable (red symbols). In each case, however, at least one limit of the confidence interval could be determined. In general, each individual concentration component of the OPECC (black symbols) was lower than the concentration that would have needed to be used to eradicate the cultures alone (red and blue symbols) for all four experimental conditions
4 Discussion
Combining different antimicrobial approaches may be beneficial for combating AMR. Thus, in the present work, the antibacterial efficacy of binary applications of antiseptics combined with aPDT using the porphyrin-based photosensitizer TMPyP was investigated.
In a previous study by our group, the effect of aPDT with the hematoporphyrin-based PS Photosan was evaluated with or without additional application of EDTA [36]. The combination of EDTA and aPDT with Photosan resulted in biological inactivation of Gram-negative Aggregatibacter actinomycetemcomitans. In contrast, the use of aPDT without EDTA showed no effect [36,37,38]. Pretreatment with EDTA increased the permeability of the bacterial membrane and allowed the PS to penetrate and accumulate in the bacterium [36]. In the current study, BAC and CHX, which are frequently used antiseptics in dentistry, dermatology, and infection control [31, 39,40,41,42], were used in binary combinations with aPDT using the PS TMPyP. BAC and CHX exert their antibacterial effects by bacterial membrane damage [29, 43, 44] and thus potentially increase the diffusion of the PS TMPyP into the bacterial cell. Accumulation inside might improve the efficacy of aPDT compared to attachment of PS to the bacterial membrane alone [25, 26].
TMPyP has been used as PS in numerous in vitro studies [11,12,13, 27, 45], and several studies have also demonstrated the efficacy of aPDT using this PS in single application against the three bacterial species used in the present study [46,47,48]. For E. coli, Preuss et al. demonstrated that the accumulation of the PS on the bacterial cell wall resulted in photodynamic inactivation [48]. For the Gram-positive bacteria S. aureus and E. faecalis, Hanakova et al. concluded that TMPyP was the most effective PS in their studies [46, 47].
In general, there are differences in the effect of antibacterial substances (e.g., antiseptics and antibiotics) against Gram-positive and Gram-negative bacteria. The same applies to aPDT. It was already shown by different research groups that, for example, the number of positive charges and the charge distribution of different photosensitizers seem to have different effects on the photo inactivation of both bacteria species [49,50,51]. Furthermore, since antiseptics and some antibiotics typically target the cell membrane, which is the main difference between Gram-positive and Gram-negative bacteria [52]. Therefore, we have used both Gram-positive and Gram-negative bacteria species. One of the characteristics that set enterococci apart from staphylococci includes their capacity to endure longer on environmental surface [53]. Consequently E. faecalis is even better adapted to extreme living conditions and therefore, a longer irradiation period was needed in the present study to successfully kill E. faecalis compared to S. aureus by the antibacterial photodynamic process.
Binary application of TMPyP-mediated aPDT in combination with BAC or CHX attempts to optimize the concentrations required for antibacterial effects, possibly slowing or even preventing the development of resistance [16,17,18]. BAC and CHX exert their antibacterial effects by creating hydrophilic domains in the lipid bilayers of the bacterial cytoplasmic membrane, finally resulting in leakage of cytoplasmic components [31, 32, 41, 43]. Due to the similar site of action, similar or amplified behavior is expected when using binary combinations of aPDT and BAC or CHX. The primary site of action of aPDT with the PS TMPyP is also assumed to be located at the cell membrane and its antibacterial effect depends on the TMPyP concentration and on the light dose applied [54].
Based on the checkerboard method, the use of binary combinations was evaluated according to the recently introduced OPECC method, i.e., optimal effective concentration combinations were determined [22]. The calculation of an OPECC is based on the determination of the borderline of the shift from non-turbid (showing antibacterial efficacy) to turbid wells. Applying the checkerboard method, the dichotomous results (turbid or not) of each well were determined. In the present work, each checkerboard plate was treated as one sample. From the six samples per study group, the frequency of occurrence of turbidity was determined for each pair of concentrations used and normalized to values between 0 (no turbidity, effective) and 1. This made it possible to apply the procedure to determine OPECCs for the data of this study [22].
In detail, it was investigated whether OPECCs could be determined for the selected combinations of the four experimental conditions (0_0, 0_10, 10_0, 10_10). These four experimental conditions were designed to give an indication on how pre-incubation with BAC or CHX, or pretreatment with aPDT affects antibacterial efficacy. In experimental condition 10_0, BAC and CHX, respectively, are first incubated for 10 min. Subsequently, TMPyP is added and activated by light exposure immediately. In experimental condition 10_10, BAC or CHX and TMPyP are added simultaneously, incubated for 10 min, and subsequently exposed to light. Since the effect of aPDT is limited to the exposure period, similar experimental results are expected as compared to the other experimental conditions [55]. Nevertheless, the experimental results differ. First, this could be attributed to the dark toxicity of TMPyP and second, to a potential "light pollution" in the laboratory. However, in our experiments, dark toxicity can be neglected due to the experimental design, because unexposed dark controls performed in each individual experiment revealed that there was no dark toxicity in the used concentration range of TMPyP. On the other hand, Eckl et al. showed that even a low light intensity is sufficient for activation of the PS TMPyP and can cause antibacterial effects [56]. Therefore, even weak ambient light due to the insufficient darkening of the laboratory rooms may have caused slight antibacterial effects, potentially explaining the observed results.
The combination of BAC and TMPyP revealed OPECCs for all of experimental conditions. This means that for each combined application, regardless of the experimental design, lower concentrations of BAC and TMPyP are required compared to the single application to achieve an effective antibacterial effect. In contrast, OPECC could not be determined for all experimental combinations of CHX and TMPyP. For both antiseptics, the observation of the experimental conditions with pre-incubations did not allow a clear statement about the influence of the conditions. Therefore, it can be assumed that more decided differences in incubation periods or light doses are needed for being able to determine a possible difference. As discussed earlier [22] the process of identifying an OPECC (optimal effective concentration combination) based on the specific organism and substances employed can be expanded to encompass various pathogens, including bacteria, fungi, viruses, and parasites, as well as clinical isolates and their combinations, among other possibilities. In principle, there are no limitations regarding the substances utilized. In addition to traditional antibiotics and antiseptics, a wide array of techniques may be employed, such as antimicrobial photodynamic therapy (aPDT) and cold atmospheric plasma (CAP), among others. In general, any procedure with the objective of eliminating pathogens in the broadest sense can be applied.
5 Conclusions
Here, the optimal effective concentration combination (OPECC) was determined for the first time for the binary use of antiseptics with aPDT, here mediated by the PS TMPyP. The determination of OPECCs is a new method for the evaluation of combinations of different antibacterial compounds and allows the comparison of the lethal concentrations of the combined application with the concentrations for a lethal single application. The results of the combination experiments with sublethal concentrations of BAC and CHX, respectively, with TMPyP-mediated aPDT for the bacteria E. coli, E. faecalis, and S. aureus showed that the binary application had a lethal effect, but an influence of the sequence of the application was not derivable. The combined application allowed the reduction of the concentrations of each substance compared to its single application.
Data availability
The data that support the findings of this study are available on request from the corresponding author [TM].
References
Tacconelli, E., & Pezzani, M. D. (2019). Public health burden of antimicrobial resistance in Europe. The Lancet Infectious Diseases, 19, 4–6. https://doi.org/10.1016/S1473-3099(18)30648-0
O’Neill, J. (2016). Tackling drug-resistant infections globally: final report and recommendations. London.
Laxminarayan, R. (2022). The overlooked pandemic of antimicrobial resistance. The Lancet, 399, 606–607. https://doi.org/10.1016/S0140-6736(22)00087-3
Antimicrobial Resistance Collaborators. (2019). Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. The Lancet, 399(2022), 629–655. https://doi.org/10.1016/S0140-6736(21)02724-0
Cieplik, F., & Jakubovics, N. S. (2022). Preprocedural mouthwashes for reduction of SARS-CoV-2 viral load and infectivity. Journal of Dental Research, 101, 1421–1423. https://doi.org/10.1177/00220345221110444
Lu, J., & Guo, J. (2021). Disinfection spreads antimicrobial resistance. Science, 371, 474. https://doi.org/10.1126/science.abg4380
Czaplewski, L., Bax, R., Clokie, M., Dawson, M., Fairhead, H., Fischetti, V. A., Foster, S., Gilmore, B. F., Hancock, R. E. W., Harper, D., Henderson, I. R., Hilpert, K., Jones, B. V., Kadioglu, A., Knowles, D., Ólafsdóttir, S., Payne, D., Projan, S., Shaunak, S., … Rex, J. H. (2016). Alternatives to antibiotics—A pipeline portfolio review. The Lancet Infectious Diseases, 16, 239–251. https://doi.org/10.1016/S1473-3099(15)00466-1
Wainwright, M., Maisch, T., Nonell, S., Plaetzer, K., Almeida, A., Tegos, G. P., & Hamblin, M. R. (2017). Photoantimicrobials—Are we afraid of the light? The Lancet Infectious Diseases, 17, e49–e55. https://doi.org/10.1016/S1473-3099(16)30268-7
Cieplik, F., Deng, D., Crielaard, W., Buchalla, W., Hellwig, E., Al-Ahmad, A., & Maisch, T. (2018). Antimicrobial photodynamic therapy—What we know and what we don’t. Critical Reviews in Microbiology, 44, 571–589. https://doi.org/10.1080/1040841X.2018.1467876
Denis, T. G. S., & Hamblin, M. (2011). An introduction to photoantimicrobials: photodynamic therapy as a novel method of microbial pathogen eradication. In A. Méndez-Vilas (Ed.), Science against microbial pathogens: communicating current research and technological advances (pp. 675–683). https://api.semanticscholar.org/CorpusID:1866203
Collins, T. L., Markus, E. A., Hassett, D. J., & Robinson, J. B. (2010). The effect of a cationic porphyrin on pseudomonas aeruginosa biofilms. Current Microbiology, 61, 411–416. https://doi.org/10.1007/s00284-010-9629-y
Cieplik, F., Pummer, A., Leibl, C., Regensburger, J., Schmalz, G., Buchalla, W., Hiller, K.-A., & Maisch, T. (2016). Photodynamic inactivation of root canal bacteria by light activation through human dental hard and simulated surrounding tissue. Frontiers in Microbiology, 7, 929. https://doi.org/10.3389/fmicb.2016.00929
Muehler, D., Brandl, E., Hiller, K.-A., Cieplik, F., & Maisch, T. (2022). Membrane damage as mechanism of photodynamic inactivation using methylene blue and TMPyP in Escherichia coli and Staphylococcus aureus. Photochemical & Photobiological Sciences, 21, 209–220. https://doi.org/10.1007/s43630-021-00158-z
Tavares, A., Dias, S. R. S., Carvalho, C. M. B., Faustino, M. A. F., Tomé, J. P. C., Neves, M. G. P. M. S., Tomé, A. C., Cavaleiro, J. A. S., Cunha, Â., Gomes, N. C. M., Alves, E., & Almeida, A. (2011). Mechanisms of photodynamic inactivation of a gram-negative recombinant bioluminescent bacterium by cationic porphyrins. Photochemical and Photobiological Sciences, 10, 1659–1669. https://doi.org/10.1039/c1pp05097d
Branco, T. M., Valério, N. C., Jesus, V. I. R., Dias, C. J., Neves, M. G. P. M. S., Faustino, M. A. F., & Almeida, A. (2018). Single and combined effects of photodynamic therapy and antibiotics to inactivate Staphylococcus aureus on skin. Photodiagnosis and Photodynamic Therapy, 21, 285–293. https://doi.org/10.1016/j.pdpdt.2018.01.001
Choudhary, M. I., Römling, U., Nadeem, F., Bilal, H. M., Zafar, M., Jahan, H., & Ur-Rahman, A. (2022). Innovative strategies to overcome antimicrobial resistance and tolerance. Microorganisms. https://doi.org/10.3390/microorganisms11010016
Schmid, A., Wolfensberger, A., Nemeth, J., Schreiber, P. W., Sax, H., & Kuster, S. P. (2019). Monotherapy versus combination therapy for multidrug-resistant gram-negative infections: Systematic review and meta-analysis. Science and Reports, 9, 15290. https://doi.org/10.1038/s41598-019-51711-x
Feng, Y., CoradiTonon, C., Ashraf, S., & Hasan, T. (2021). Photodynamic and antibiotic therapy in combination against bacterial infections: Efficacy, determinants, mechanisms, and future perspectives. Advanced Drug Delivery Reviews, 177, 113941. https://doi.org/10.1016/j.addr.2021.113941
Wozniak, A., & Grinholc, M. (2018). Combined antimicrobial activity of photodynamic inactivation and antimicrobials-state of the art. Frontiers in Microbiology, 9, 930. https://doi.org/10.3389/fmicb.2018.00930
Botelho, M. (2000). Fractional inhibitory concentration index of combinations of antibacterial agents against cariogenic organisms. Journal of Dentistry, 28, 565–570. https://doi.org/10.1016/s0300-5712(00)00039-7
Berenbaum, M. C. (1978). A method for testing for synergy with any number of agents. Journal of Infectious Diseases, 137, 122–130. https://doi.org/10.1093/infdis/137.2.122
Hiller, K.-A., Wenzl, V., Forster, E.-M., Cieplik, F., & Maisch, T. (2023). The optimal effective concentration combination (OPECC) as a novel method for evaluating the effects of binary application of antibacterial compounds. Microorganisms, 11, 830. https://doi.org/10.3390/microorganisms11040830
Schramm, S., Hiller, K.-A., Cantzler, S., Weilemann, H., Cantzler, M., Zimmermann, J. L., Cieplik, F., & Maisch, T. (2020). The latest time point of retreatment (LTPR) as a novel method to determine antibacterial effects for binary use of cold atmospheric plasma and conventional agents. Frontiers in Microbiology, 11, 576500. https://doi.org/10.3389/fmicb.2020.576500
Iluz, N., Maor, Y., Keller, N., & Malik, Z. (2018). The synergistic effect of PDT and oxacillin on clinical isolates of Staphylococcus aureus. Lasers in Surgery and Medicine, 50, 535–551. https://doi.org/10.1002/lsm.22785
Alves, E., Faustino, M. A. F., Neves, M. G., Cunha, A., Tome, J., & Almeida, A. (2014). An insight on bacterial cellular targets of photodynamic inactivation, Future. Medicinal Chemistry, 6, 141–164. https://doi.org/10.4155/fmc.13.211
Almeida, A., Faustino, M. A. F., & Tomé, J. P. C. (2015). Photodynamic inactivation of bacteria: Finding the effective targets, Future. Medicinal Chemistry, 7, 1221–1224. https://doi.org/10.4155/fmc.15.59
Voit, T., Cieplik, F., Regensburger, J., Hiller, K.-A., Gollmer, A., Buchalla, W., & Maisch, T. (2021). Spatial distribution of a porphyrin-based photosensitizer reveals mechanism of photodynamic inactivation of Candida albicans. Frontiers in Medicine (Lausanne), 8, 641244. https://doi.org/10.3389/fmed.2021.641244
Cieplik, F., Steinwachs, V.-S., Muehler, D., Hiller, K.-A., Thurnheer, T., Belibasakis, G. N., Buchalla, W., & Maisch, T. (2018). Phenalen-1-one-mediated antimicrobial photodynamic therapy: Antimicrobial efficacy in a periodontal biofilm model and flow cytometric evaluation of cytoplasmic membrane damage. Frontiers in Microbiology, 9, 688. https://doi.org/10.3389/fmicb.2018.00688
Muehler, D., Rupp, C. M., Keceli, S., Brochhausen, C., Siegmund, H., Maisch, T., Hiller, K.-A., Buchalla, W., & Cieplik, F. (2020). Insights into mechanisms of antimicrobial photodynamic action toward biofilms using phenalen-1-one derivatives as photosensitizers. Frontiers in Microbiology, 11, 589364. https://doi.org/10.3389/fmicb.2020.589364
Sabino, C. P., Ribeiro, M. S., Wainwright, M., Dos Anjos, C., Sellera, F. P., Dropa, M., Nunes, N. B., Brancini, G. T. P., Braga, G. U. L., Arana-Chavez, V. E., Freitas, R. O., Lincopan, N., & Baptista, M. S. (2023). The biochemical mechanisms of antimicrobial photodynamic therapy†. Photochemistry and Photobiology, 99, 742–750. https://doi.org/10.1111/php.13685
MerchelPiovesan Pereira, B., & Tagkopoulos, I. (2019). Benzalkonium chlorides: Uses, regulatory status, and microbial resistance. Applied and Environmental Microbiology. https://doi.org/10.1128/AEM.00377-19
McDonnell, G., & Russell, A. D. (1999). Antiseptics and disinfectants: Activity, action, and resistance. Clinical microbiology reviews, 12, 147–179. https://doi.org/10.1128/cmr.12.1.147
Andrews, J. M. (2001). Determination of minimum inhibitory concentrations. The Journal of Antimicrobial Chemotherapy, 48(Suppl 1), 5–16. https://doi.org/10.1093/jac/48.suppl_1.5
Ince, D., & Hooper, D. C. (2003). Quinolone resistance due to reduced target enzyme expression. Journal of Bacteriology, 185, 6883–6892. https://doi.org/10.1128/JB.185.23.6883-6892.2003
Jenkins, S. G., & Schuetz, A. N. (2012). Current concepts in laboratory testing to guide antimicrobial therapy. Mayo Clinic Proceedings, 87, 290–308. https://doi.org/10.1016/j.mayocp.2012.01.007
Maisch, T., Wagner, J., Papastamou, V., Nerl, H.-J., Hiller, K.-A., Szeimies, R.-M., & Schmalz, G. (2009). Combination of 10% EDTA, photosan, and a blue light hand-held photopolymerizer to inactivate leading oral bacteria in dentistry in vitro. Journal of Applied Microbiology, 107, 1569–1578. https://doi.org/10.1111/j.1365-2672.2009.04342.x
Vaara, M. (1992). The outer membrane as the penetration barrier against mupirocin in gram-negative enteric bacteria. The Journal of Antimicrobial Chemotherapy, 29, 221–222. https://doi.org/10.1093/jac/29.2.221
Vaara, M., & Vaara, T. (1983). Polycations as outer membrane-disorganizing agents. Antimicrobial Agents and Chemotherapy, 24, 114–122. https://doi.org/10.1128/AAC.24.1.114
Weber, J., Bonn, E. L., Auer, D. L., Kirschneck, C., Buchalla, W., Scholz, K. J., & Cieplik, F. (2023). Preprocedural mouthwashes for infection control in dentistry—An update. Clinical Oral Investigations. https://doi.org/10.1007/s00784-023-04953-z
Bonn, E. L., Rohrhofer, A., Audebert, F. X., Lang, H., Auer, D. L., Scholz, K. J., Schuster, P., Wenzel, J. J., Hiller, K.-A., Buchalla, W., Gottsauner, J. M., Vielsmeier, V., Schmidt, B., & Cieplik, F. (2023). Efficacy of a mouthwash containing CHX and CPC in SARS-CoV-2-positive patients: A randomized controlled clinical trial. Journal of Dental Research. https://doi.org/10.1177/00220345231156415
Cieplik, F., Jakubovics, N. S., Buchalla, W., Maisch, T., Hellwig, E., & Al-Ahmad, A. (2019). Resistance toward chlorhexidine in oral bacteria—Is there cause for concern? Frontiers in Microbiology, 10, 587. https://doi.org/10.3389/fmicb.2019.00587
Meister, T. L., Gottsauner, J.-M., Schmidt, B., Heinen, N., Todt, D., Audebert, F., Buder, F., Lang, H., Gessner, A., Steinmann, E., Vielsmeier, V., Pfaender, S., & Cieplik, F. (2022). Mouthrinses against SARS-CoV-2—High antiviral effectivity by membrane disruption in vitro translates to mild effects in a randomized placebo-controlled clinical trial. Virus Research, 316, 198791. https://doi.org/10.1016/j.virusres.2022.198791
Muehler, D., Sommer, K., Wennige, S., Hiller, K.-A., Cieplik, F., Maisch, T., & Späth, A. (2017). Light-activated phenalen-1-one bactericides: Efficacy, toxicity and mechanism compared with benzalkonium chloride. Future Microbiology, 12, 1297–1310. https://doi.org/10.2217/fmb-2016-0229
Cieplik, F., Kara, E., Muehler, D., Enax, J., Hiller, K.-A., Maisch, T., & Buchalla, W. (2019). Antimicrobial efficacy of alternative compounds for use in oral care toward biofilms from caries-associated bacteria in vitro. Microbiologyopen, 8, e00695. https://doi.org/10.1002/mbo3.695
Eichner, A., Gonzales, F. P., Felgenträger, A., Regensburger, J., Holzmann, T., Schneider-Brachert, W., Bäumler, W., & Maisch, T. (2012). Dirty hands: Photodynamic killing of human pathogens like EHEC, MRSA and Candida within seconds. Photochemical & Photobiological Sciences, 12, 135–147. https://doi.org/10.1039/c2pp25164g
Hanakova, A., Bogdanova, K., Tomankova, K., Binder, S., Bajgar, R., Langova, K., Kolar, M., Mosinger, J., & Kolarova, H. (2014). Study of photodynamic effects on NIH 3T3 cell line and bacteria. Biomedical Paper, 158, 201–207. https://doi.org/10.5507/bp.2012.057
Hanakova, A., Bogdanova, K., Tomankova, K., Pizova, K., Malohlava, J., Binder, S., Bajgar, R., Langova, K., Kolar, M., Mosinger, J., & Kolarova, H. (2014). The application of antimicrobial photodynamic therapy on S. aureus and E. coli using porphyrin photosensitizers bound to cyclodextrin. Microbiological Research, 169, 163–170. https://doi.org/10.1016/j.micres.2013.07.005
Preuss, A., Zeugner, L., Hackbarth, S., Faustino, M. A. F., Neves, M. G. P. M. S., Cavaleiro, J. A. S., & Roeder, B. (2013). Photoinactivation of Escherichia coli (SURE2) without intracellular uptake of the photosensitizer. Journal of Applied Microbiology, 114, 36–43. https://doi.org/10.1111/jam.12018
Alves, E., Costa, L., Carvalho, C. M. B., Tomé, J. P. C., Faustino, M. A. F., Neves, M. G. P. M. S., Tomé, A. C., Cavaleiro, J. A. S., Cunha, A., & Almeida, A. (2009). Charge effect on the photoinactivation of gram-negative and gram-positive bacteria by cationic meso-substituted porphyrins. BMC Microbiology, 9, 70. https://doi.org/10.1186/1471-2180-9-70
Merchat, M., Spikes, J. D., Bertoloni, G., & Jori, G. (1996). Studies on the mechanism of bacteria photosensitization by meso-substituted cationic porphyrins. Journal of Photochemistry and Photobiology B: Biology, 35, 149–157. https://doi.org/10.1016/s1011-1344(96)07321-6
Merchat, M., Bertolini, G., Giacomini, P., Villanueva, A., & Jori, G. (1996). Meso-substituted cationic porphyrins as efficient photosensitizers of gram-positive and gram-negative bacteria. Journal of Photochemistry and Photobiology B: Biology, 32, 153–157. https://doi.org/10.1016/1011-1344(95)07147-4
Poole, K. (2002). Mechanisms of bacterial biocide and antibiotic resistance. Journal of Applied Microbiology, 92(Suppl), 55S-64S.
Neely, A. N., & Maley, M. P. (2000). Survival of enterococci and staphylococci on hospital fabrics and plastic. Journal of Clinical Microbiology, 38, 724–726. https://doi.org/10.1128/JCM.38.2.724-726.2000
de Gao, Agayan, R. R., Xu, H., Philbert, M. A., & Kopelman, R. (2006). Nanoparticles for two-photon photodynamic therapy in living cells. Nano Letters, 6, 2383–2386. https://doi.org/10.1021/nl0617179
Maisch, T., Spannberger, F., Regensburger, J., Felgenträger, A., & Bäumler, W. (2012). Fast and effective: Intense pulse light photodynamic inactivation of bacteria. Journal of Industrial Microbiology and Biotechnology, 39, 1013–1021. https://doi.org/10.1007/s10295-012-1103-3
Eckl, D. B., Dengler, L., Nemmert, M., Eichner, A., Bäumler, W., & Huber, H. (2018). A Closer look at dark toxicity of the photosensitizer TMPyP in bacteria. Photochemistry and Photobiology, 94, 165–172. https://doi.org/10.1111/php.12846
Acknowledgements
This study was funded in part by the Deutsche Forschungsgemeinschaft (grant CI 263/3-1).
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Maisch, T., Scholz, K.J., Forster, EM. et al. Optimal effective concentration combinations (OPECCs) for binary application of membrane-targeting antiseptics and TMPyP-mediated antimicrobial photodynamic therapy. Photochem Photobiol Sci 23, 189–196 (2024). https://doi.org/10.1007/s43630-023-00512-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43630-023-00512-3