Abstract
Purpose
We conducted this study to examine the clinical outcomes of primary total knee arthroplasty (TKA) with autogenous bone graft for a tibial bony defect with a minimum follow-up of 12 months.
Methods
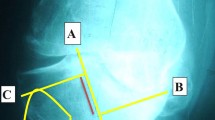
A total of 21 individuals underwent primary TKA with autogenous on-lay bone grafting (ABG) for restoration of posteromedial tibial deformities between January 2016 and November 2021. The patients were clinically assessed using the knee society score (KSS), varus score, and range of motion (ROM) preoperatively and postoperatively to compare using a single sample t test. Postoperative complications were also considered.
Results
KSS before and after surgery was reported to be statistically significant [mean difference = −55.32 (6.81); P < 0.001]. The mean KSS before surgery was 21.14 (7.03) while improved to the mean KSS after surgery of 76.45 (3.05). ROM score before and after surgery was reported to be statistically significant [mean difference = −30.45 (8.99); P < 0.001]. The mean ROM before surgery was 75.45 (6.71) while the improved mean ROM after surgery of 105.91 (5.03). Varus score before and after surgery was reported to be statistically significant [mean difference = 18.45 (3.75); P < 0.001].
Conclusion
The mechanical axis and stability of the knee were effectively restored, with significant differences in preoperative and postoperative results, indicating that this technique is a reasonable and versatile option when reconstructing moderate-to-severe bone loss in TKA.
Graphical Abstract




Similar content being viewed by others
Data availability
The authors attest that the publication and its supplemental materials have the data necessary to support the conclusions of this investigation. Data supporting Figures 1, 2 and 3 and Tables 1, 2 not publicly available in order to protect patient privacy. Repository as part of this record included in https://doi.org/10.1007/s43465-023-00857-y.
References
Stucinskas, J., Robertsson, O., Sirka, A., Lebedev, A., Wingstrand, H., & Tarasevicius, S. (2015). Moderate varus/valgus malalignment after total knee arthroplasty has little effect on knee function or muscle strength: 91 patients assessed after 1 year. Acta Orthopaedica, 86(6), 728–733.
Lei, P. F., Hu, R. Y., & Hu, Y. H. (2019). Bone defects in revision total knee arthroplasty and management. Orthopaedic Surgery, 11(1), 15–24.
Baek, S. W., Kim, C. W., & Choi, C. H. (2013). Management of tibial bony defect with metal block in primary total knee replacement arthroplasty. Knee Surgery & Related Research, 25(1), 7–12.
Chon, J. G., Kang, J. W., Kim, C. U., Jeong, U., & Go, J. (2021). Treatment of 10-mm-deep or greater uncontained tibial bone defects in primary total knee reconstruction without metal augmentation: Autologous oblique structural peg bone and cancellous chip bone grafting. Clinics in Orthopedic Surgery, 13(2), 168.
Ahmed, I., Logan, M., Alipour, F., Dashti, H., & Hadden, W. A. (2008). Autogenous bone grafting of uncontained bony defects of tibia during total knee arthroplasty: A 10-year follow up. Journal of Arthroplasty, 23(5), 744–750.
Luthra, J. S., & Habsi, S. A. (2018). Biological reconstruction of varus deformity in primary total knee replacement using bone graft and description of a new technique. Journal of Orthopaedics, Trauma and Rehabilitation, 25, 69–72.
Hasandoost, L., Rodriguez, O., Alhalawani, A., Zalzal, P., Schemitsch, E. H., Waldman, S. D., Papini, M., & Towler, M. R. (2020). The role of poly (methyl methacrylate) in management of bone loss and infection in revision total knee arthroplasty: A review. Journal of Functional Biomaterials, 11(2), 25.
Liu, S., Wang, S., Wu, T., Fan, Z., Zhang, Y., Rao, Y., & Tan, M. (2017). Short-term effectiveness of bone cement combined with screws for repairing tibial plateau defect in total knee arthroplasty. Zhongguo xiu fu Chong Jian wai ke za zhi = Zhongguo Xiufu Chongjian Waike Zazhi= Chinese Journal of Reparative and Reconstructive Surgery, 31(9), 1055–10588.
Dorr, L. D., Ranawat, C. S., Sculco, T. A., McKaskill, B., & Orisek, B. S. (2006). THE CLASSIC: Bone graft for Tibial defects in total knee arthroplasty. Clinical Orthopaedics and Related Research, 446, 4–9.
Tanwar, Y. S., Kharbanda, Y., Bhargava, H., Attri, K., & Bandil, A. (2019). Mid-term results of impaction bone grafting in tibial bone defects in complex primary knee arthroplasty for severe varus deformity. SICOT-Journal, 5, 2.
Yoon, J. R., Seo, I. W., & Shin, Y. S. (2017). Use of autogenous onlay bone graft for uncontained tibial bone defects in primary total knee arthroplasty. BMC Musculoskeletal Disorders, 18(1), 1–7.
Baek, S. W., & Choi, C. H. (2011). Management of severe tibial bony defects with double metal blocks in knee arthroplasty—A technical note involving 9 cases. Acta Orthopaedica, 82(1), 116–118.
Acknowledgements
We would like to acknowledge Dr. Uzair Yaqoob for his final review and critical appraisal of this manuscript.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
This article was prepared in collaboration between all authors. Authors M.W.K. and I.M.R. did conception and design, acquisition of data, analysis, and interpretation of data. Author M.W.K. drafted the article and did the critical revision. Authors I.M.R., J.Q., and A.Q. did the acquisition of data, analysis, and interpretation of data. All authors gave final approval of the version to be published. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that there is no conflict of interest.
Informed Consent
Informed consent was not sought for the present study because this was a retrospective data collection.
Ethical Approval
Ethical approval for this study was obtained from the Orthopedic Department of Dr. Ruth K. M. Pfau, Civil Hospital, Karachi, Pakistan.
Guarantor
MWK.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Khan, M.W., Rajput, I.M., Qamar, J. et al. Biological Reconstruction of Posteromedial Tibial Defect with Autogenous Bone Graft in Complex Knee Arthroplasty. JOIO 57, 856–862 (2023). https://doi.org/10.1007/s43465-023-00857-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43465-023-00857-y