Abstract
Methotrexate is a chemotherapy medication frequently used to treat various forms of cancer. The purpose of this research was to examine if the administration of Arthrospira platensis (Spirulina) and/or thymoquinone could ameliorate the liver injury resulting from methotrexate. The rats were randomly assigned to seven groups, each containing seven rats. The groups included a control group that received only saline, a group that received A. platensis orally at a dose of 500 mg/kg, a group that received thymoquinone orally at a dose of 10 mg/kg, a group that received a single i.p. dose of 20 mg/kg methotrexate, a group that received both A. platensis and methotrexate, a group that received both thymoquinone and methotrexate, and a group that received A. platensis, thymoquinone, and methotrexate. The injection of methotrexate caused an increase in the levels of alanine aminotransferase, aspartate aminotransferase, alkaline phosphatase, cholesterol, triacylglycerides, and low-density lipoprotein-cholesterol, and a decrease in high-density lipoprotein-cholesterol (HDL-cholesterol). The liver tissues also showed an increase in malondialdehyde and a decrease in reduced glutathione, superoxide dismutase, and catalase, along with pathological lesions and increased expression of TNF-α and caspase-3. However, administration of A. platensis and thymoquinone alone or in combination reduced the toxicity and apoptosis induced by methotrexate.
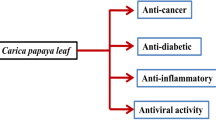
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The liver is responsible for important functions such as metabolism, detoxification, and elimination of harmful substances from the body. Any damage or dysfunction to the liver can result in severe health issues (Ramadori and Cameron 2010).
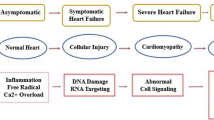
Methotrexate (MTX) is a type of anti-folic acid medication that is derived from aminopterin and can inhibit DNA synthesis and repair (AbdelKader et al. 2023; Aboubakr et al. 2023a). Methotrexate is metabolized and stored in hepatocytes in its polyglutamated form, leading to a longer presence of MTX within the cells, which has been suggested as a possible mechanism for MTX-induced liver damage (Bath et al. 2014; Tag 2015). It is a frequently utilized medication for managing autoimmune disorders, like rheumatoid arthritis and psoriasis (Valerio et al. 2021). It is a highly effective cytotoxic drug that alters cellular metabolism and suppresses cell growth (Aboubakr et al. 2023b). However, the cytotoxic effects of MTX are not limited to cancer cells and can also affect many normal tissues including the brain (Behairy et al. 2023).
Methotrexate-induced hepatotoxicity may occur through the disruption of intestinal barrier functions, leading to the translocation of bacteria to the liver and subsequent liver damage (Cao et al. 2019). In addition, it has been observed that MTX can increase intestinal permeability which has been linked to hepatic inflammation, abnormal liver histological changes such as fibrosis, cirrhosis, and apoptosis of liver cells, and higher levels of hepatic transaminases (Cao et al. 2019). Hepatotoxicity can result from an imbalance in the regulation of oxidative stress, inflammation, endothelial damage, and apoptosis (Abdelaziz et al. 2020; Ezhilarasan 2021; Abd El-Ghafar et al. 2022; Alfwuaires 2022; Morsy et al. 2022; AbdelKader et al. 2023; Wang et al. 2023).
Toxicity in the liver is caused by mechanisms that are triggered when there is an abnormal reduction in antioxidants and an uncontrolled elevation of free radicals in the cells, which is known as oxidative stress (Abd El-Ghafar et al. 2022). Methotrexate, on the other hand, reduces protective antioxidants like glutathione (GSH) and inhibits enzymes that scavenge free radicals, causing the liver to become more susceptible to damage (Goudarzi et al. 2021). In addition, the prolonged buildup of MTX inside liver cells can increase the risk of hepatocyte death and fibrosis by reducing folate levels, disrupting DNA synthesis in hepatocytes, and stimulating collagen production (Morsy et al. 2022).
Herbal remedies or plant-based products have been commonly utilized to treat various illnesses owing to their relatively safer nature and fewer side effects when compared to synthetic drugs (Elsayed et al. 2022; Malayeri et al. 2022).
Arthrospira platensis (Spirulina) is a species of blue-green algae that possesses numerous medicinal uses as a result of its exceptional nutritional content and potent scavengers of free radicals (Ibrahim et al. 2021; Fadl et al. 2022). Spirulina encompasses crucial nutrients such as proteins, lipids, carbohydrates, essential amino acids, essential fatty acids, minerals, vitamins, β-carotene, and C-phycocyanin, which are vital for maintaining human health. Furthermore, spirulina and its primary component, C-phycocyanin, exhibit a range of biological functions, such as liver protection, neuroprotection, anti-inflammatory, immune system modulation, and anticancer effects (Abdelkhalek et al. 2015; Abdel-Daim et al. 2019; Bin-Jumah et al. 2021; Germoush et al. 2022). These compounds have been found to protect against organ toxicities induced by heavy metals and other chemicals, making it a promising therapeutic agent (Ibrahim and Abdel-Daim 2015). Moreover, spirulina has been shown to possess anti-inflammatory, antiapoptotic, antioxidant, and glucose- and lipid-lowering effects (El-Boghdady et al. 2020). Several studies have reported the hepatoprotective effects of spirulina (Abdel-Daim et al. 2018; Khalil et al. 2020; Bin-Jumah et al. 2021). Therefore, spirulina is considered a safe and effective adjuvant therapy for reducing the occurrence of adverse effects caused by MTX.
Spirulina is typically consumed orally in the form of capsules, tablets, or powder. The proteins in spirulina are rich in essential amino acids and are relatively easy to digest and absorb. Some of the vitamins and minerals present in spirulina are also readily absorbed in the gastrointestinal tract. Phycocyanin and other components in spirulina are metabolized by various enzymes in the body. Spirulina is not known to accumulate in the body, and any excess nutrients or compounds not used are typically eliminated through urine or feces (Bortolini et al. 2022). Spirulina is generally considered safe when consumed in appropriate amounts as a dietary supplement or as part of a balanced diet. However, like any substance, including natural supplements, spirulina can have adverse effects if used improperly or excessively and may be contaminated with heavy metals (Al-Dhabi 2013).
Nigella sativa contains thymoquinone (TQ), which is a pharmacologically active component with several biological and pharmaceutical properties (Gökce et al. 2016; Al Aboud et al. 2021; Fadishei et al. 2021). It was able to protect the liver tissue from oxidative stress, inflammation, and cell death (Abdel-Daim et al. 2020a; Abdo et al. 2021; Aboubakr et al. 2021). Thymoquinone possesses the capacity to eliminate free radicals and prevent the process of lipid peroxidation (Farag et al. 2015), and has been reported to possess advantageous effects as an agent against diabetes, hyperlipidemia, inflammation, oxidative stress, and liver damage (Fadishei et al. 2021; Aktaş and Mehmet Gür 2022; Demircigil et al. 2023). Thymoquinone's ability to scavenge free radicals, including superoxide anion, hydroxyl, hydrogen peroxide, and peroxynitrite radicals, as well as its ability to increase the activity of antioxidant enzymes like superoxide dismutase, catalase, and glutathione peroxidase, are responsible for its antioxidant capacity (Hamdy and Taha 2009). Additionally, thymoquinone's ability to prevent cell death through apoptosis has been linked to its promotion of anti-apoptotic proteins and inhibition of pro-apoptotic proteins (Al-Brakati et al. 2019; Al Aboud et al. 2021).
Absorption of TQ in the gastrointestinal tract can be limited due to its relatively low water solubility. It is absorbed more efficiently in the presence of fats or oils. TQ is lipophilic (soluble in fat), which allows it to be distributed throughout the body. Thymoquinone may also accumulate in certain tissues or organs, such as the liver, kidney, and lungs, depending on the route of administration and duration of exposure. Thymoquinone undergoes metabolism in the liver, primarily by cytochrome P450 enzymes and metabolites of TQ are excreted from the body primarily through urine and feces (Goyal et al. 2017). Thymoquinone has been found as an almost safe chemical, LD50 values of 250–794 mg/kg in rats and 300–2400 mg/kg in mice were reported (Mashayekhi-Sardoo et al. 2020).
Numerous studies have shown that MTX and its metabolites can cause harmful effects such as inflammation, oxidative stress, fibrosis, and cell death in liver cells (Chauhan et al. 2020). However, it is still unclear how to protect against these toxic effects. Despite the testing of numerous drugs to alleviate MTX-related adverse effects, none have proven highly effective in clinical studies. Thus, identifying a potential treatment for shielding against MTX-caused liver toxicity has become a crucial area of research. The fundamental aim of this research was to examine if spirulina and/or TQ could decrease the harmful impact of MTX on liver cells. In order to achieve this objective, we examined liver function, oxidative stress, apoptosis, and histological changes in liver tissue.
Materials and Methods
Chemicals
The methotrexate injectable solution (50 mg/5 ml) was obtained from Mina Pharm Pharmaceuticals located in Cairo, Egypt. Sigma Aldrich, based in Saint Louis, MO, USA, supplied the thymoquinone powder with a purity of 98% (Batch NO: MKCB1381V) which dissolved in dimethyl sulfoxide (DMSO). Arthrospira platensis (spirulina) powder (Batch NO: SP72022) was acquired from the Algal Biotechnology unit at the National Research Center in Dokki, Cairo, Egypt. The analytical kits used were provided by the Bio-diagnostics Company located in Giza, Egypt.
Animals and Experimental Design
Forty-nine male Wister Albino rats weighing between 188–222 g were obtained from the Egyptian Organization for Biological Products and Vaccines. The rats were kept in a regulated environment at 25 ± 2 °C and a 12-h light/dark cycle and were provided with a standard pellet diet and free access to water. The rats were allowed to acclimate for 1 week before the experiment started. They were then divided into 7 groups, each consisting of 7 rats. The first group was given saline only as a control, while the second group was given spirulina (500 mg/kg/day p.o. for 21 days) (Khafaga and El-Sayed 2018). The third group was given TQ (10 mg/kg/day p.o. for 21 days) (Abdel-Daim et al. 2020b). The fourth group was given saline, p.o., and a single dose of MTX (20 mg/kg, i.p.) on the 15th day of the study, which served as a toxic control for MTX (Khafaga and El-Sayed 2018). The fifth group received spirulina (500 mg/kg/day p.o. for 21 days) and on the 15th day of the study a single dose of MTX (20 mg/kg) was injected i.p., the sixth group received TQ (10 mg/kg/day p.o. for 21 days) and on the 15th day of the study a single dose of MTX (20 mg/kg) was injected i.p., and the seventh group received spirulina (500 mg/kg/day p.o. for 21 days) + TQ (10 mg/kg/day p.o. for 21 days) and on the 15th day of the study a single dose of MTX (20 mg/kg) was injected i.p.
Blood Sampling and Serum Biochemical Markers
After the experiment was completed, the rats were anesthetized with isoflurane, and blood samples were collected from the retro-orbital plexus. The samples were left to clot at room temperature then centrifuged for 15 min at 1200 × g, and the resulting serum was stored at -20 °C for future biochemical analysis. Liver function tests; including alanine transaminase (AST), alanine transaminase (ALT) (Reitman and Frankel 1957), alkaline phosphatase (ALP) (Belfield and Goldberg 1971), as well as serum cholesterol (Deeg and Ziegenhorn 1983), triacylglycerides (TG) (Fossati and Prencipe 1982), HDL-cholesterol (Burstein et al. 1970), and LDL-cholesterol concentrations (Friedewald et al. 1972) were determined in the serum. The UV–visible spectrophotometer model PharmaSpec 1700 (Shimadzu, Japan) was used to measure biochemical and oxidative stress markers. Finally, all dead rats and remnants of samples were buried in the strict hygienically controlled properly constructed burial pit.
Tissue Sampling and Oxidative Stress Markers
A sample of liver tissue (1 g) was rinsed using a solution containing 50 mM sodium phosphate-buffered saline (100 mM Na2HPO4/NaH2PO4, pH 7.4) and kept on ice. To eliminate red blood cells (RBCs) and clots, 0.1 mM EDTA was added. Next, the tissues were homogenized in a cold saline solution (5 ml per gram of tissue). N-Ethylmaleimide was added directly after homogenization to prevent oxidation of GSH and was subjected to centrifugation at 1200 × g for 10 min at 4 °C. The resulting supernatant was carefully transferred to an Eppendorf tube and stored at -80 °C, enabling spectrophotometric analysis of tissue biomarkers. For the antioxidant markers, GSH was analyzed using the method described by Beutler et al. (1963), which involves the reaction of GSH with 5,5'-dithiobis(2-nitrobenzoic acid) (DTNB) to produce a yellow compound. The absorbance of this compound was measured spectrophotometrically. Superoxide dismutase levels were determined using a method based on the inhibition of the reaction between superoxide radicals, generated by xanthine and xanthine oxidase, and nitroblue tetrazolium (NBT), as described by Nishikimi et al. (1972). Malondialdehyde levels were assessed based on its reaction with thiobarbituric acid (TBA) to form a pink-colored complex, following the protocol of Ohkawa et al. (1979). Lastly, catalase (CAT) activity was gauged by observing the decomposition of hydrogen peroxide and measuring the decrease in absorbance at 240 nm, as per the method of Cohen et al. (1970).
Histopathological Examination
A sample of liver tissue was fixed in a solution of 10% buffer formalin for at least 24 h, processed, and embedded in paraffin using a standard protocol (Feldman and Wolfe 2014). The paraffin-embedded tissue was then sectioned into slices that were 5 µm thick, placed onto glass slides, and deparaffinized. Hematoxylin and eosin (H&E) staining was used to prepare the tissue for examination under a light microscope for histopathological analysis.
Immunohistochemical Analyses of Apoptotic Markers in Hepatic Tissue
To conduct immunohistochemical analysis of TNF-α and caspase-3, liver sections of 4 μm were deparaffinized and boiled using Declere to reveal antigen sites. The sections were then incubated with anti-TNF-α and anti-caspase-3 antibodies in phosphate-buffered saline (PBS) at a dilution of 1:200 for overnight at 4 °C. After removal of the primary antibodies and washing with PBS, the slides were treated with a biotinylated secondary antibody at a dilution of 1:500. Avidin biotinylated peroxidase complex was used to detect bound antibodies. Hematoxylin was used to counterstain the slides. All sections were treated under the same conditions with the same antibody concentration and for the same duration to ensure comparable immunostaining across different experimental groups (Dai et al. 2018).
Statistical Analysis
The mean ± SD was used to express the obtained results. Statistical comparisons were performed using GraphPad Prism 9 software (San Diego, CA, USA) with one-way ANOVA and Tukey’s post hoc test for multiple comparisons. A significance level of p < 0.05 was used.
Results
Methotrexate was found to cause hepatoxicity, as evidenced by an increase in serum levels of liver biomarkers (Fig. 1). Compared to control rats, MTX treatment resulted in substantial increases in AST, ALT, and ALP activities, as well as in the concentration of cholesterol, triacylglycerides, and LDL-cholesterol, and a reduction in the serum concentration of HDL-cholesterol. However, treatment with spirulina, TQ, or a combination of both (spirulina + TQ) significantly reduced these parameters in MTX-treated rats. Furthermore, when MTX-intoxicated rats were treated with both spirulina and TQ, the values were significantly lower than those treated with MTX alone. Therefore, the combination of spirulina and TQ provided better protection against hepatic damage caused by MTX compared to either compound alone. The effect of SP, TQ, and MTX on lipid profile is shown in Fig 2.
The impact of MTX exposure and administration of spirulina, TQ, or their combination on the levels of MDA, reduced glutathione, and antioxidant enzymes in the liver tissues. Co-treatment with spirulina and TQ led to a significant improvement in oxidative damage induced by MTX in liver tissues compared to spirulina or TQ treatment alone (Fig. 3).
The liver tissue of the control group displayed distinct polyhedral-shaped large hepatocytes with well-preserved cytoplasm and rounded euchromatic nucleus with prominent nuclei, forming hepatic cord-like structures (Fig. 4A). The liver sections from the groups treated with spirulina (Fig. 4B) or TQ (Fig. 4C) appeared similar to the normal control group with no significant changes in the hepatic architecture. On the other hand, the liver sections from the MTX-treated group showed several changes such as infiltration of inflammatory cells (Fig. 4D), mitotic activity with hepatocyte nuclei, cytoplasm vacuolation, degeneration (Fig. 4E), hepatocyte necrosis, and nuclei disintegration (Fig. 4F). Compared to MTX-treated rats, the liver sections from the MTX + SP group showed fewer severe alterations. The liver tissue had renewing hepatocytes and fewer signs of inflammation, but moderate degenerating hepatocytes with condensed nuclei and a lack of polygonal-shaped outlines were still observed (Fig. 4G). The MTX + TQ group showed regenerated hepatocytes that appeared more regular as plates and organized, with fewer inflammatory cells than the MTX-treated group (Fig. 4H). The combination of spirulina and TQ administration (MTX + SP + TQ) helped maintain the normal liver structure by preventing cellular inflammation, sinusoidal dilatation, and apoptosis, and only causing mild degeneration and mild congestion. Importantly, the hepatic structure of the liver tissues was nearly similar to that of the control group (Fig. 4I). Table 1 records the histopathological damage scores for the control and MTX-exposed groups with and without SP and/or TQ treatments.
Histological examination of liver sections of control group showed well-preserved hepatocytes with distinct cord-like structures and rounded euchromatic nuclei with prominent nuclei (A). Spirulina (B) or thymoquinone (C) control groups showed typical hepatic architecture similar to the normal control group. MTX-treated group demonstrated infiltration of inflammatory cells (D), mitotic activity, cytoplasm vacuolation, degeneration (E), hepatocyte necrosis, and nuclei disintegration (F). MTX and spirulina showed the presence of renewing hepatocytes and less severe alterations compared to the MTX-only group (G). MTX and thymoquinone showed regenerated hepatocytes that appeared more regular as plates and organized with less inflammatory cells compared to MTX-only group (H). MTX + spiruline + thymoquinone demonstrated nearly normal hepatic structure with mild congestion as well as degeneration (I). Central vein (black arrow), inflammatory cells (black star), degeneration (blue star), and necrobiotic change (red star)
The liver tissue samples from all experimental groups were used to detect TNF-α expression levels through immunohistochemistry, and the results were shown in Fig. 5. The streptavidin–biotin-peroxidase complex method was used, which resulted in brown-colored sediments at the sites where the antigen bound. Treatment with either spirulina (Fig. 5B) or TQ (Fig. 5C) alone did not show any significant changes in the expression levels of TNF-α when compared to the normal control group (Fig. 5A). However, in the liver tissue of rats treated with MTX (Fig. 5D), the expression of TNF-α was increased. Treatment with either spirulina + MTX (Fig. 5E) or TQ + MTX (Fig. 5F) showed a decrease in the intensity of brown staining in the tubules, indicating a decrease in TNF-α expression. The spirulina + MTX + TQ group (Fig. 5G) showed very mild expression of TNF-α. The mean gray value of TNF-α expression was quantified in ten visual fields using Image J software.
Immunostaining analysis performed on liver sections from rats that were treated with spirulina and/or thymoquinone, and its impact on hepatic TNF-α expression. The control group (A) and the groups that received either spirulina (B) or thymoquinone (C) treatment alone showed minimal TNF-α immunopositivity. However, the MTX-intoxicated group exhibited a significant increase in TNF-α expression (D). Conversely, the groups treated with MTX + spirulina (E) or MTX + thymoquinone (F) demonstrated moderate immunopositivity, while the MTX + spirulina + thymoquinone group showed a noticeable reduction in TNF-α expression (G). The semi-quantitative analysis of TNF-α expression revealed a significant difference between the MTX and control groups (H)
In Fig. 6, it is shown that the normal control group (Fig. 6A), spirulina group (Fig. 6B), and TQ group (Fig. 6C) had minimal or no immune-stained cells of caspase-3 in the liver tissues. However, in rats exposed to MTX, there was a significant increase in caspase-3 expression, demonstrated by strongly stained liver cells (Fig. 6D). In contrast, MTX-intoxicated rats treated with either spirulina (Fig. 6E) or TQ (Fig. 6F) showed a significant reduction in the levels of caspase-3 protein expression in liver tissues, with moderately stained hepatic cells compared to those treated with MTX alone. The combination group (MTX + spirulina + TQ) demonstrated the lowest presence of immune-reactive cells in the hepatic tissues, as shown in Fig. 6G.
Immunostaining for liver sections of rats treated with spirulina and/or thymoquinone and their impact on the expression of cleaved caspase-3. Minimal caspase-3 immunopositivity was observed in the control group (A) and the groups treated with spirulina (B) or thymoquinone (C) alone. In contrast, the MTX-intoxicated group exhibited significantly increased caspase-3 expression (D). However, the groups treated with MTX + spirulina (E) or MTX + thymoquinone (F) displayed moderate immunopositivity significance, while the group treated with MTX + spirulina + thymoquinone showed a noticeable reduction in caspase-3 expression (G). Hepatic caspase3 immunopositive (area%) of treated group (H)
Discussion
Methotrexate-induced liver damage is a common and serious side effect of this drug. Many research studies have shown that MTX and its byproducts can lead to inflammatory responses, oxidative stress, fibrosis, and cell death in liver cells (Chauhan et al. 2020; AbdelKader et al. 2023).
The increase in serum levels of ALT, AST, and ALP in rats treated with MTX may be attributed to damage to the plasma membrane of hepatic parenchymal cells. Methotrexate works by binding to the hydrofolic reductase enzyme, which hinders the conversion of folic acid to folinic acid and consequently affects the synthesis of certain amino acids and nucleic acids. This mechanism disrupts the activity of hepatic parenchymal cells by harming their organelles and plasma membrane, which results in the release of hepatic enzymes like ALT and AST into the bloodstream (McGill 2016). An increase in the levels of these enzymes in the bloodstream indicates the severity of the injury (Mehra et al. 2021), this is in line with previous studies (Vardi et al. 2010; Abd El-Ghafar et al. 2022; Alfwuaires 2022; Morsy et al. 2022). ALP is an enzyme that is present in the cells lining the bile ducts and its increase in the bloodstream is often linked to issues with the liver and bile ducts. On the other hand, albumin levels in the blood are indicative of the liver's ability to synthesize this protein (Moghadam et al. 2015).
In addition, the co-administration of spirulina and/or TQ with MTX resulted in a significant reduction in the levels of the three liver enzymes measured in the serum compared to the group treated with MTX alone. These findings align with the investigation conducted by Germoush et al. (2022), which explored the defensive properties of spirulina against microcystin-LR-triggered liver damage in rats. Spirulina administration reduced serum levels of ALT, AST, and ALP in animals exposed to deltamethrin (Abdel-Daim et al. 2013). This could be explained by the antioxidant and safeguarding characteristics of spirulina, which has an abundance of antioxidant substances such as β-carotene, C-phycocyanin, proteins, lipids, essential fatty acids, essential amino acids, carbohydrates, minerals, and vitamins. All of these components possess strong anti-inflammatory and antioxidant attributes (Abdelkhalek et al. 2015). The addition of TQ to the treatment regimen notably enhanced the serum liver function markers in rats with silver nanoparticle-induced toxicity, according to a study by Salama et al. (2023). TQ has the potential to be a beneficial therapeutic agent in mitigating liver damage caused by diabetes, according to Aktaş and Mehmet Gür (2022).
The administration of MTX resulted in a significant increase in the levels of circulating cholesterol, triacylglycerides, and LDL-cholesterol, and a decrease in HDL-cholesterol. These findings are consistent with the results reported by Ghoneum and El-Gerbed (2021) and Sheikha et al. (2022). The liver's function in regulating plasma cholesterol levels is critical, and the impairment of liver function caused by drugs can result in a rise in serum total cholesterol and LDL-cholesterol levels (Atawodi et al. 2014). The liver is accountable for producing triacylglycerides (TG) and transforming TG into very-low-density lipoprotein (VLDL) cholesterol, which is then carried to peripheral tissues. Impairment of VLDL-C production can cause a rise in TG levels (Baratta et al. 2023). Previous research has shown a link between the changes in lipid metabolism caused by MTX and oxidative stress. Increased lipid content may lead to decreased expression of antioxidant enzymes and higher levels of reactive oxygen species (ROS) (Ghoneum and El-Gerbed 2021). Studies have demonstrated that spirulina supplementation can decrease serum levels of cholesterol, LDL-C, and triacylglycerides while increasing HDL-C levels in rats fed a high-fat diet (Yigit et al. 2016). TQ treatment has also been shown to improve the lipid profile in rats fed a high-fat diet, malathion, and in bisphenol A-induced liver injury in rats by reducing plasma LDL cholesterol and total cholesterol levels and increasing plasma HDL cholesterol levels (Abdel-Daim et al. 2020a; Alanazi et al. 2023; Demircigil et al. 2023).
According to previous research, MTX-induced toxicity in multiple organs is primarily caused by oxidative stress (Mahmoud et al. 2017). Studies have indicated that MTX-induced hepatotoxicity is linked to the overproduction of ROS and oxidative/nitrosative stress (Hussein et al. 2020; Abd El-Ghafar et al. 2022; Alfwuaires 2022; AbdelKader et al. 2023). The excessive generation of ROS brought about by MTX administration leads to damage to the cellular enzymatic and non-enzymatic antioxidant defense system (Kolli et al. 2014). Our findings indicate that MTX administration caused a significant increase in MDA levels and a decrease in GSH levels, as well as a decrease in the enzymatic activity of SOD and CAT compared to the control group and the group treated with spirulina and TQ. These results are consistent with previous studies that reported MTX-induced oxidative stress (Dar et al. 2021; Ghoneum and El-Gerbed 2021; Abd El-Ghafar et al. 2022). The reduction in CAT and SOD synthesis or their activity, or excessive ROS formation, may explain the decrease in their activities, and the decrease in cellular GSH may result from NADPH inhibition by MTX (Alfwuaires 2022). Gluthatione is a vital endogenous antioxidant that helps combat free radicals and other oxidants (Ghoneum and El-Gerbed 2021; Sallam et al. 2021; Elsayed et al. 2022).
According to our study, administering spirulina, TQ, or a combination of both along with MTX significantly increased the level of GSH in liver homogenate and improved the activity of key antioxidant enzymes (SOD and CAT). Additionally, these treatments significantly decreased the level of MDA in hepatic tissue when compared to the group treated with MTX alone. These results are similar to those reported in a previous study that found spirulina supplementation inhibited lipid peroxidation and increased the levels of antioxidant enzymes and GSH in hepatic tissues (Wu et al. 2016). Our findings are consistent with a previous study that reported the protective effects of spirulina against deltamethrin-induced oxidative stress, possibly by scavenging free radicals and increasing the activities of SOD and CAT (Abdel-Daim et al. 2013). Other studies have also demonstrated the protective effects of spirulina against hepatic toxicity induced by CCl4 (Kepekçi et al. 2013), acrylamide (Bin-Jumah et al. 2021), and diazinon (Abdel-Daim et al. 2018). The protective effects of spirulina and TQ could be explained by the presence of several antioxidant active components such as C-phycocyanin, vitamins, ß-carotene, and minerals (Grover et al. 2021). Spirulina's antioxidant role was demonstrated by a decrease in MDA concentration, an increase in GSH levels, and enhancement of SOD action in hepatic tissue in previous studies (Karadeniz et al. 2009; Simsek et al. 2009). Similarly, previous research supports the potential of TQ to protect against oxidative stress caused by various hepatotoxic agents, such as aflatoxins (Nili-Ahmadabadi et al. 2011), cisplatin (Al-Malki and Sayed 2014), methotrexate (El-Sheikh et al. 2015), lead (Mabrouk et al. 2016), and arsenic (Alam et al. 2022). Additionally, TQ has been shown to reduce tartrazine-induced hepatotoxicity due to its potent antioxidant and anti-inflammatory properties (Demircigil et al. 2023).
Furthermore, the histological examination of liver tissues stained with H&E supported these findings, showing significant histopathological damage such as hepatocyte vacuolation and disorganization of hepatic cords in the MTX-treated group. These results are consistent with previous studies that reported similar histological damage induced by MTX (Abdelaziz et al. 2020; Mehra et al. 2021; Abd El-Ghafar et al. 2022; Alfwuaires 2022; Morsy et al. 2022; AbdelKader et al. 2023). However, treatment with spirulina and TQ improved the histological architecture of the liver tissues, indicating their protective effect against MTX-induced liver damage.
Methotrexate can increase apoptosis (Horie et al. 2006). Apoptosis can be triggered by lipid peroxidation and the release of free radicals, which can damage DNA and activate the caspase gene (Herman et al. 2005). The current study used immunohistochemical analysis to demonstrate that MTX toxicity in the liver led to increased levels of TNF-α and caspase-3 expressions, which suggests that these factors may contribute to MTX-induced liver damage. Previous studies by Chauhan et al. (2020) and Demiryilmaz et al. (2012) have reported similar results. Previous studies (Abdel-Raheem and Khedr 2014; Ibrahim et al. 2014; Hafez et al. 2015) have reported that TNF-α, a pro-inflammatory mediator, is overexpressed in MTX-induced tissue damage in various models. TNF-α plays a crucial role in liver homeostasis and can activate the pro-apoptotic pathway in liver cells (Liedtke and Trautwein 2012). The activation of TNF-α receptors leads to cellular apoptosis through the activation of different types of caspases (Cubero et al. 2013), including caspase-3, which is frequently activated during apoptosis, including in cases of MTX administration (Chang et al. 2013). In rats that were pretreated with spirulina or TQ, the number of hepatocytes with caspase-3 and immunoreactivity was significantly reduced. This may be due to spirulina's anti-mutagenic effect, which can minimize DNA damage caused by MTX precursors (Ismail et al. 2009). Furthermore, the anti-oxidative properties of spirulina and TQ, as well as their chemical constituents, may also play a role. Previous study has shown that spirulina has an anti-apoptotic role by downregulating caspase-3 (Khafaga and El-Sayed 2018) and TNF-α (Sadek et al. 2017). Similarly, TQ has an anti-apoptotic role by downregulating caspase-3 (Haron et al. 2018) and TNF-α (Aktaş and Mehmet Gür 2022). TQ reduced apoptosis and oxidative stress (Yılmaz et al. 2021).
Conclusions
Overall, the current study suggests that spirulina and TQ may alleviate liver damage caused by MTX in rats. The proposed mechanism of action of involves the antioxidant, and anti-apoptotic properties of spirulina and TQ. Incorporating spirulina and TQ as dietary supplements during MTX treatment may offer protection against MTX-induced hepatic toxicity. However, more laboratory and clinical trials are required to confirm the potential protective effects of spirulina and TQ.
Data Availability
The data presented in this study are available upon request from the first author.
References
Abd El-Ghafar OA, Hassanein EH, Ali FE, Omar ZM, Rashwan EK, Mohammedsaleh ZM, Sayed AM (2022) Hepatoprotective effect of acetovanillone against methotrexate hepatotoxicity: role of Keap-1/Nrf2/ARE, IL6/STAT-3, and NF-κB/AP-1 signaling pathways. Phytother Res 36:488–505. https://doi.org/10.1002/ptr.7355
Abdelaziz RM, Abdelazem AZ, Hashem KS, Attia YA (2020) Protective effects of hesperidin against MTX-induced hepatotoxicity in male albino rats. Naunyn-Schmiedeberg’s Arch Pharmacol 393:1405–1417. https://doi.org/10.1007/s00210-020-01843-z
Abdel-Daim MM, Abuzead SM, Halawa SM (2013) Protective role of Spirulina platensis against acute deltamethrin-induced toxicity in rats. PLoS ONE 8:e72991. https://doi.org/10.1371/journal.pone.0072991
Abdel-Daim MM, Abushouk AI, Alkhalf MI, Toraih EA, Fawzy MS, Ijaz H, Aleya L, Bungau SG (2018) Antagonistic effects of Spirulina platensis on diazinon-induced hemato-biochemical alterations and oxidative stress in rats. Environ Sci Pollut Res 25:27463–27470. https://doi.org/10.1007/s11356-018-2761-0
Abdel-Daim MM, Ahmed A, Ijaz H, Abushouk AI, Ahmed H, Negida A, Aleya L, Bungau SG (2019) Influence of Spirulina platensis and ascorbic acid on amikacin-induced nephrotoxicity in rabbits. Environ Sci Pollut Res 26:8080–8086. https://doi.org/10.1007/s11356-019-04249-4
Abdel-Daim MM, Abo El-Ela FI, Alshahrani FK, Bin-Jumah M, Al-Zharani M, Almutairi B, Alyousif MS, Bungau S, Aleya L, Alkahtani S (2020a) Protective effects of thymoquinone against acrylamide-induced liver, kidney and brain oxidative damage in rats. Environ Sci Pollut Res 27:37709–37717. https://doi.org/10.1007/s11356-020-09516-3
Abdel-Daim MM, Abushouk AI, Bungău SG, Bin-Jumah M, El-Kott AF, Shati AA, Aleya L, Alkahtani S (2020b) Protective effects of thymoquinone and diallyl sulphide against malathion-induced toxicity in rats. Environ Sci Pollut Res 27:10228–10235. https://doi.org/10.1007/s11356-019-07580-y
AbdelKader G, Abdelaziz EZ, Hassan R, Greish SM, Abogresha NM, Sultan BO, Yousef EM, Morsi S, Abdelaziz E, Greish S (2023) Protective Effects of Crocin Against Methotrexate-Induced Hepatotoxicity in Adult Male Albino Rats: Histological, Immunohistochemical, and Biochemical Study. Cureus 15:e34468. https://doi.org/10.7759/cureus.34468
Abdelkhalek NK, Ghazy EW, Abdel-Daim MM (2015) Pharmacodynamic interaction of Spirulina platensis and deltamethrin in freshwater fish Nile tilapia, Oreochromis niloticus: impact on lipid peroxidation and oxidative stress. Environ Sci Pollut Res 22:3023–3031. https://doi.org/10.1007/s11356-014-3578-0
Abdel-Raheem IT, Khedr NF (2014) Renoprotective effects of montelukast, a cysteinyl leukotriene receptor antagonist, against methotrexate-induced kidney damage in rats. Naunyn-Schmiedebergs Arch Pharmacol 387:341–353. https://doi.org/10.1007/s00210-013-0949-x
Abdo W, Elmadawy MA, Abdelhiee EY, Abdel-Kareem MA, Farag A, Aboubakr M, Ghazy E, Fadl SE (2021) Protective effect of thymoquinone against lung intoxication induced by malathion inhalation. Sci Rep 11:2498. https://doi.org/10.1038/s41598-021-82083-w
Aboubakr M, Elshafae SM, Abdelhiee EY, Fadl SE, Soliman A, Abdelkader A, Abdel-Daim MM, Bayoumi KA, Baty RS, Elgendy E, Elalfy A, Baioumy B, Ibrahim SF, Abdeen A (2021) Antioxidant and Anti-Inflammatory Potential of Thymoquinone and Lycopene Mitigate the Chlorpyrifos-Induced Toxic Neuropathy. Pharmaceuticals 14:940. https://doi.org/10.3390/ph14090940
Aboubakr M, Elbadawy M, Ibrahim SS, Khalil E, Darweish M, Farag A, Elfadadny A, Alkafafy M, Soliman A, Elsayed A (2023) Allicin and lycopene possesses a protective effect against methotrexate induced testicular toxicity in rats. Pak Vet J 43:559–566. https://doi.org/10.29261/pakvetj/2023.057
Aboubakr M, Farag A, Elfadadny A, Alkafafy M, Soliman A, Elbadawy M (2023b) Antioxidant and anti-apoptotic potency of allicin and lycopene against methotrexate-induced cardiac injury in rats. Environ Sci Pollut Res 30:88724–88733. https://doi.org/10.1007/s11356-023-28686-4
Aktaş İ, Mehmet Gür F (2022) Hepato-protective effects of thymoquinone and beta-aminoisobutyric acid in streptozocin induced diabetic rats. Biotech Histochem 97:67–76. https://doi.org/10.1080/10520295.2021.1949041
Al Aboud D, Baty RS, Alsharif KF, Hassan KE, Zhery AS, Habotta OA, Elmahallawy EK, Amin HK, Abdel Moneim AE, Kassab RB (2021) Protective efficacy of thymoquinone or ebselen separately against arsenic-induced hepatotoxicity in rat. Environ Sci Pollut Res 28:6195–6206. https://doi.org/10.1007/s11356-020-10955-1
Alam T, Shahid F, Abidi S, Parwez I, Khan F (2022) Thymoquinone supplementation mitigates arsenic-induced cytotoxic and genotoxic alterations in rat liver. J Trace Elem Med Biol 74:127067. https://doi.org/10.1016/j.jtemb.2022.127067
Alanazi S, Alsaqer R, Alsaeed F, Almakhaytah R, Buwashl N, Mohamed M, Younis N (2023) Studying the actions of sage and thymoquinone combination on metabolic syndrome induced by high-fat diet in rats. Eur Rev Med Pharmacol Sci 27:2404–2418. https://doi.org/10.26355/eurrev_202303_31775
Al-Brakati A, Kassab R, Lokman M, Elmahallawy E, Amin H, Abdel Moneim A (2019) Role of thymoquinone and ebselen in the prevention of sodium arsenite–induced nephrotoxicity in female rats. Hum Exp Toxicol 38:482–493. https://doi.org/10.1177/0960327118818246
Al-Dhabi NA (2013) Heavy metal analysis in commercial Spirulina products for human consumption. Saudi J Biol Sci 20:383–388. https://doi.org/10.1016/j.sjbs.2013.04.006
Alfwuaires MA (2022) Galangin mitigates oxidative stress, inflammation, and apoptosis in a rat model of methotrexate hepatotoxicity. Environ Sci Pollut Res 29:20279–20288. https://doi.org/10.1007/s11356-021-16804-z
Al-Malki AL, Sayed AA (2014) Thymoquinone attenuates cisplatin-induced hepatotoxicity via nuclear factor kappa-β. BMC Complement Altern Med 14:282. https://doi.org/10.1186/1472-6882-14-282
Atawodi SE, Yakubu OE, Liman ML, Iliemene DU (2014) Effect of methanolic extract of Tetrapleura tetraptera (Schum and Thonn) Taub leaves on hyperglycemia and indices of diabetic complications in alloxan–induced diabetic rats. Asian Pac J Trop Biomed 4:272–278. https://doi.org/10.12980/APJTB.4.2014C73
Baratta F, Cocomello N, Coronati M, Ferro D, Pastori D, Angelico F, Ben MD (2023) Cholesterol Remnants, Triglyceride-Rich Lipoproteins and Cardiovascular Risk. Int J Mol Sci 24:4268. https://doi.org/10.3390/ijms24054268
Bath RK, Brar NK, Forouhar FA, Wu GY (2014) A review of methotrexate-associated hepatotoxicity. J Dig Dis 15:517–524. https://doi.org/10.1111/1751-2980.12184
Behairy A, Elkomy A, Elsayed F, Gaballa MMS, Soliman A, Aboubakr M (2023) Antioxidant and anti-inflammatory potential of spirulina and thymoquinone mitigate the methotrexate-induced neurotoxicity. Naunyn Schmiedebergs Arch Pharmacol. https://doi.org/10.1007/s00210-023-02739-4
Belfield A, Goldberg D (1971) Colorimetric determination of alkaline phosphatase activity. Enzyme 12:561–568
Beutler E, Duron O, Kelly BM (1963) Improved method for the determination of blood glutathione. J Lab Clin Med 61:882–888
Bin-Jumah MN, Al-Huqail AA, Abdelnaeim N, Kamel M, Fouda MM, Abulmeaty MM, Saadeldin IM, Abdel-Daim MM (2021) Potential protective effects of Spirulina platensis on liver, kidney, and brain acrylamide toxicity in rats. Environ Sci Pollut Res 28:26653–26663. https://doi.org/10.1007/s11356-021-12422-x
Bortolini DG, Maciel GM, Fernandes IAA, Pedro AC, Rubio FTV, Branco IG, Haminiuk CWI (2022) Functional properties of bioactive compounds from Spirulina spp.: current status and future trends. Food Chem 5:100134. https://doi.org/10.1016/j.fochms.2022.100134
Burstein M, Scholnick H, Morfin R (1970) Rapid method for the isolation of lipoproteins from human serum by precipitation with polyanions. J Lipid Res 11:583–595
Cao Y, Shi H, Sun Z, Wu J, Xia Y, Wang Y, Wu Y, Li X, Chen W, Wang A (2019) Protective effects of magnesium glycyrrhizinate on methotrexate-induced hepatotoxicity and intestinal toxicity may be by reducing COX-2. Front Pharmacol 10:119. https://doi.org/10.3389/fphar.2019.00119
Chang CJ, Lin JF, Chang HH, Lee GA, Hung CF (2013) Lutein protects against methotrexate-induced and reactive oxygen species-mediated apoptotic cell injury of IEC-6 cells. PLoS ONE 8:e72553. https://doi.org/10.1371/journal.pone.0072553
Chauhan P, Sharma H, Kumar U, Mayachari A, Sangli G, Singh S (2020) Protective effects of Glycyrrhiza glabra supplementation against methotrexate-induced hepato-renal damage in rats: An experimental approach. J Ethnopharmacol 263:113209. https://doi.org/10.1016/j.jep.2020.113209
Cohen G, Dembiec D, Marcus J (1970) Measurement of catalase activity in tissue extracts. Anal Biochem 34:30–38. https://doi.org/10.1016/0003-2697(70)90083-7
Cubero F, Singh A, Borkham-Kamphorst E, Nevzorova Y, Al Masaoudi M, Haas U, Boekschoten M, Gassler N, Weiskirchen R, Muller M (2013) TNFR1 determines progression of chronic liver injury in the IKKγ/Nemo genetic model. Cell Death Differ 20:1580–1592. https://doi.org/10.1038/cdd.2013.112
Dai C, Xiao X, Li D, Tun S, Wang Y, Velkov T, Tang S (2018) Chloroquine ameliorates carbon tetrachloride-induced acute liver injury in mice via the concomitant inhibition of inflammation and induction of apoptosis. Cell Death Dis 9:1164. https://doi.org/10.1038/s41419-018-1136-2
Dar A, Fehaid A, Alkhatani S, Alarifi S, Alqahtani W, Albasher G, Almeer R, Alfarraj S, Moneim AA (2021) The protective role of luteolin against the methotrexate-induced hepato-renal toxicity via its antioxidative, anti-inflammatory, and anti-apoptotic effects in rats. Hum Exp Toxicol 40:1194–1207. https://doi.org/10.1177/0960327121991905
Deeg R, Ziegenhorn J (1983) Kinetic enzymic method for automated determination of total cholesterol in serum. Clin Chem 29:1798–1802
Demircigil N, Gul M, Gokturk N, Kustepe EK, Bag HG, Erdemli ME (2023) Thymoquinone played a protective role against tartrazine-induced hepatotoxicity. Iran J Basic Med Sci 26:99–106. https://doi.org/10.22038/IJBMS.2022.67341.14763
Demiryilmaz I, Sener E, Cetin N, Altuner D, Suleyman B, Albayrak F, Akcay F, Suleyman H (2012) Biochemically and histopathologically comparative review of thiamine’s and thiamine pyrophosphate’s oxidative stress effects generated with methotrexate in rat liver. Med Sci Monit 18:BR475–BR481. https://doi.org/10.12659/msm.883591
El-Boghdady NA, Kamel MA, El-Shamy RM (2020) Omeprazole and spirulina platensis ameliorate steatohepatitis in experimental nonalcoholic fatty liver disease. Metab Syndr Relat Disord 18:426–434. https://doi.org/10.1089/met.2019.0129
Elsayed A, Elkomy A, Alkafafy M, Elkammar R, Fadl SE, Abdelhiee EY, Abdeen A, Shaheen H, Soliman A, Aboubakr M (2022) Ameliorating effect of lycopene and N-acetylcysteine against cisplatin-induced cardiac injury in rats. Pak Vet J 42:107–111. https://doi.org/10.29261/pakvetj/2021.035
El-Sheikh AA, Morsy MA, Abdalla AM, Hamouda AH, Alhaider IA (2015) Mechanisms of Thymoquinone Hepatorenal Protection in Methotrexate-Induced Toxicity in Rats. Mediators Inflamm 2015:859383. https://doi.org/10.1155/2015/859383
Ezhilarasan D (2021) Hepatotoxic potentials of methotrexate: Understanding the possible toxicological molecular mechanisms. Toxicology 458:152840. https://doi.org/10.1016/j.tox.2021.152840
Fadishei M, Ghasemzadeh Rahbardar M, Imenshahidi M, Mohajeri A, Razavi BM, Hosseinzadeh H (2021) Effects of Nigella sativa oil and thymoquinone against bisphenol A-induced metabolic disorder in rats. Phytother Res 35:2005–2024. https://doi.org/10.1002/ptr.6944
Fadl SE, Elbialy ZI, Abdo W, Saad AH, Aboubakr M, Abdeen A, Elkamshishi MM, Salah AS, El-Mleeh A, Almeer R, Aleya L, Abdel-Daim MM, Najda A, Abdelhiee EY (2022) Ameliorative effect of Spirulina and Saccharomyces cerevisiae against fipronil toxicity in Oreochromis niloticus. Ecotoxicol Environ Saf 242:113899. https://doi.org/10.1016/j.ecoenv.2022.113899
Farag MM, Ahmed GO, Shehata RR, Kazem AH (2015) Thymoquinone improves the kidney and liver changes induced by chronic cyclosporine A treatment and acute renal ischaemia/reperfusion in rats. J Pharm Pharmacol 67:731–739. https://doi.org/10.1111/jphp.12363
Feldman AT, Wolfe D (2014) Tissue processing and hematoxylin and eosin staining. Methods Mol Biol 1180:31–43. https://doi.org/10.1007/978-1-4939-1050-2_3
Fossati P, Prencipe L (1982) Serum triglycerides determined colorimetrically with an enzyme that produces hydrogen peroxide. Clin Chem 28:2077–2080
Friedewald WT, Levy RI, Fredrickson DS (1972) Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem 18:499–502
Germoush MO, Fouda MM, Kamel M, Abdel-Daim MM (2022) Spirulina platensis protects against microcystin-LR-induced toxicity in rats. Environ Sci Pollut Res 29:11320–11331. https://doi.org/10.1007/s11356-021-16481-y
Ghoneum M, El-Gerbed MS (2021) Human placental extract ameliorates methotrexate-induced hepatotoxicity in rats via regulating antioxidative and anti-inflammatory responses. Cancer Chemother Pharmacol 88:961–971. https://doi.org/10.1007/s00280-021-04349-4
Gökce EC, Kahveci R, Gökce A, Cemil B, Aksoy N, Sargon MF, Kısa Ü, Erdoğan B, Güvenç Y, Alagöz F (2016) Neuroprotective effects of thymoquinone against spinal cord ischemia-reperfusion injury by attenuation of inflammation, oxidative stress, and apoptosis. J Neurosurg Spine 4:949–959. https://doi.org/10.3171/2015.10.SPINE15612
Goudarzi M, Kalantar M, Sadeghi E, Karamallah MH, Kalantar H (2021) Protective effects of apigenin on altered lipid peroxidation, inflammation, and antioxidant factors in methotrexate-induced hepatotoxicity. Naunyn Schmiedebergs Arch Pharmacol 394:523–531. https://doi.org/10.1007/s00210-020-01991-2
Goyal SN, Prajapati CP, Gore PR, Patil CR, Mahajan UB, Sharma C, Talla SP, Ojha SK (2017) Therapeutic Potential and Pharmaceutical Development of Thymoquinone: A Multitargeted Molecule of Natural Origin. Front Pharmacol 8:656. https://doi.org/10.3389/fphar.2017.00656
Grover P, Bhatnagar A, Kumari N, Bhatt AN, Nishad DK, Purkayastha J (2021) C-Phycocyanin-a novel protein from Spirulina platensis-In vivo toxicity, antioxidant and immunomodulatory studies. Saudi J Biol Sci 28:1853–1859. https://doi.org/10.1016/j.sjbs.2020.12.037
Hafez HM, Ibrahim MA, Ibrahim SA, Amin EF, Goma W, Abdelrahman AM (2015) Potential protective effect of etanercept and aminoguanidine in methotrexate-induced hepatotoxicity and nephrotoxicity in rats. Eur J Pharmacol 768:1–12. https://doi.org/10.1016/j.ejphar.2015.08.047
Hamdy NM, Taha RA (2009) Effects of Nigella sativa oil and thymoquinone on oxidative stress and neuropathy in streptozotocin-induced diabetic rats. Pharmacology 84:127–134. https://doi.org/10.1159/000234466
Haron AS, Syed Alwi SS, Saiful Yazan L, Abd Razak R, Ong YS, Zakarial Ansar FH, Roshini Alexander H (2018) Cytotoxic effect of thymoquinone-loaded nanostructured lipid carrier (TQ-NLC) on liver cancer cell integrated with hepatitis B genome, Hep3B. Evid Based Complement Alternat Med 2018:1549805. https://doi.org/10.1155/2018/1549805
Herman S, Zurgil N, Deutsch M (2005) Low dose methotrexate induces apoptosis with reactive oxygen species involvement in T lymphocytic cell lines to a greater extent than in monocytic lines. Inflamm Res 54:273–280. https://doi.org/10.1007/s00011-005-1355-8
Horie T, Li T, Ito K, Sumi S, Fuwa T (2006) Aged garlic extract protects against methotrexate-induced apoptotic cell injury of IEC-6 cells. J Nutr 136:861S-863S. https://doi.org/10.1093/jn/136.3.861S
Hussein OE, Hozayen WG, Bin-Jumah MN, Germoush MO, Abd El-Twab SM, Mahmoud AM (2020) Chicoric acid prevents methotrexate hepatotoxicity via attenuation of oxidative stress and inflammation and up-regulation of PPARγ and Nrf2/HO-1 signaling. Environ Sci Pollut Res 27:20725–20735. https://doi.org/10.1007/s11356-020-08557-y
Ibrahim AE, Abdel-Daim MM (2015) Modulating effects of Spirulina platensis against tilmicosin-induced cardiotoxicity in mice. Cell J 17:137–144. https://doi.org/10.22074/cellj.2015.520
Ibrahim MA, El-Sheikh AA, Khalaf HM, Abdelrahman AM (2014) Protective effect of peroxisome proliferator activator receptor (PPAR)-α and-γ ligands against methotrexate-induced nephrotoxicity. Immunopharmacol Immunotoxicol 36:130–137. https://doi.org/10.3109/08923973.2014.884135
Ibrahim SS, Elsabagh R, Allam A, Youssef G, Fadl SE, Abdelhiee EY, Alkafafy M, Soliman A, Aboubakr M (2021) Bioremediation role of Spirulina platensis against deltamethrin-mediated toxicity and its chemical residues in chicken meat. Environ Sci Pollut Res 28:56188–56198. https://doi.org/10.1007/s11356-021-14617-8
Ismail MF, Ali DA, Fernando A, Abdraboh ME, Gaur RL, Ibrahim WM, Raj MH, Ouhtit A (2009) Chemoprevention of rat liver toxicity and carcinogenesis by Spirulina. Int J Biol Sci 5:377–387. https://doi.org/10.7150/ijbs.5.377
Karadeniz A, Cemek M, Simsek N (2009) The effects of Panax ginseng and Spirulina platensis on hepatotoxicity induced by cadmium in rats. Ecotoxicol Environ Saf 72:231–235. https://doi.org/10.1016/j.ecoenv.2008.02.021
Kepekçi RA, Polat S, Çelik A, Bayat N, Saygideger SD (2013) Protective effect of Spirulina platensis enriched in phenolic compounds against hepatotoxicity induced by CCl4. Food Chem 141:1972–1979. https://doi.org/10.1016/j.foodchem.2013.04.107
Khafaga AF, El-Sayed YS (2018) Spirulina ameliorates methotrexate hepatotoxicity via antioxidant, immune stimulation, and proinflammatory cytokines and apoptotic proteins modulation. Life Sci 196:9–17. https://doi.org/10.1016/j.lfs.2018.01.010
Khalil SR, Salem HF, Metwally MM, Emad RM, Elbohi KM, Ali SA (2020) Protective effect of Spirulina platensis against physiological, ultrastructural and cell proliferation damage induced by furan in kidney and liver of rat. Ecotoxicol Environ Saf 192:110256. https://doi.org/10.1016/j.ecoenv.2020.110256
Kolli V, Natarajan K, Isaac B, Selvakumar D, Abraham P (2014) Mitochondrial dysfunction and respiratory chain defects in a rodent model of methotrexate-induced enteritis. Hum Exp Toxicol 33:1051–1065. https://doi.org/10.1177/0960327113515503
Liedtke C, Trautwein C (2012) The role of TNF and Fas dependent signaling in animal models of inflammatory liver injury and liver cancer. Eur J Cell Biol 91:582–589. https://doi.org/10.1016/j.ejcb.2011.10.001
Mabrouk A, Bel Hadj Salah I, Chaieb W, Ben Cheikh H (2016) Protective effect of thymoquinone against lead-induced hepatic toxicity in rats. Environ Sci Pollut Res 23:12206–12215. https://doi.org/10.1007/s11356-016-6419-5
Mahmoud AM, Hussein OE, Hozayen WG, Abd el-Twab SM, (2017) Methotrexate hepatotoxicity is associated with oxidative stress, and down-regulation of PPARγ and Nrf2: Protective effect of 18β-Glycyrrhetinic acid. Chem Biol Interact 270:59–72. https://doi.org/10.1016/j.cbi.2017.04.009
Malayeri A, Badparva R, Mombeini MA, Khorsandi L, Goudarzi M (2022) Naringenin: a potential natural remedy against methotrexate-induced hepatotoxicity in rats. Drug Chem Toxicol 45:491–498. https://doi.org/10.1080/01480545.2020.1719132
Mashayekhi-Sardoo H, Rezaee R, Karimi G (2020) An overview of in vivo toxicological profile of thymoquinone. Toxin Rev 39:115–122
McGill MR (2016) The past and present of serum aminotransferases and the future of liver injury biomarkers. EXCLI J 15:817–828. https://doi.org/10.17179/excli2016-800
Mehra L, Bhattacharya A, Rawat H, Kumar A, Jaimini A, Mittal G (2021) In-vitro and in-vivo functional observation studies to establish therapeutic potential of alpha-ketoglutarate against methotrexate induced liver injury. Biomed J 44:611–619. https://doi.org/10.1016/j.bj.2020.05.012
Moghadam AR, Tutunchi S, Namvaran-Abbas-Abad A, Yazdi M, Bonyadi F, Mohajeri D, Mazani M, Marzban H, Łos MJ, Ghavami S (2015) Pre-administration of turmeric prevents methotrexate-induced liver toxicity and oxidative stress. BMC Complement Altern Med 15:246. https://doi.org/10.1186/s12906-015-0773-6
Morsy MA, Abdel-Latif R, Hafez SMNA, Kandeel M, Abdel-Gaber SA (2022) Paeonol Protects against Methotrexate Hepatotoxicity by Repressing Oxidative Stress, Inflammation, and Apoptosis—The Role of Drug Efflux Transporters. Pharmaceuticals 15:1296. https://doi.org/10.3390/ph15101296
Nili-Ahmadabadi A, Tavakoli F, Hasanzadeh G, Rahimi H, Sabzevari O (2011) Protective effect of pretreatment with thymoquinone against Aflatoxin B(1) induced liver toxicity in mice. Daru 19:282–287
Nishikimi M, Roa N, Yogi K (1972) Measurement of superoxide dismutase. Biochem Biophys Res Commun 46:849–854. https://doi.org/10.1016/s0006-291x(72)80218-3
Ohkawa H, Ohishi N, Yagi K (1979) Assay for lipid peroxides in animal tissues by thiobarbituric acid reaction. Anal Biochem 95:351–358. https://doi.org/10.1016/0003-2697(79)90738-3
Ramadori G, Cameron S (2010) Effects of systemic chemotherapy on the liver. Ann Hepatol 9:133–143
Reitman S, Frankel S (1957) A colorimetric method for the determination of serum glutamic oxalacetic and glutamic pyruvic transaminases. Am J Clin Pathol 28:56–63. https://doi.org/10.1093/ajcp/28.1.56
Sadek KM, Lebda MA, Nasr SM, Shoukry M (2017) Spirulina platensis prevents hyperglycemia in rats by modulating gluconeogenesis and apoptosis via modification of oxidative stress and MAPK-pathways. Biomed Pharmacother 92:1085–1094. https://doi.org/10.1016/j.biopha.2017.06.023
Salama B, Alzahrani KJ, Alghamdi KS, Al-Amer O, Hassan KE, Elhefny MA, Albarakati AJA, Alharthi F, Althagafi HA, Al Sberi H (2023) Silver nanoparticles enhance oxidative stress, inflammation, and apoptosis in liver and kidney tissues: Potential protective role of thymoquinone. Biol Trace Elem Res 201:2942–2954. https://doi.org/10.1007/s12011-022-03399-w
Sallam AO, Rizk HA, Emam MA, Fadl SE, Abdelhiee EY, Khater H, Elkomy A, Aboubakr M (2021) The ameliorative effects of L-carnitine against cisplatin-induced gonadal toxicity in rats. Pakistan Vet J 41:147–151. https://doi.org/10.29261/pakvetj/2020.082
Sheikha M, Soheir N, SyragEldin F (2022) Synthesis, characterization and protection effect of black rice anthocyanins nano-composite against hepatotoxicity induced by methotrexate in rats. Braz J Biol 84:e248726. https://doi.org/10.1590/1519-6984.248726
Simsek N, Karadeniz A, Kalkan Y, Keles ON, Unal B (2009) Spirulina platensis feeding inhibited the anemia-and leucopenia-induced lead and cadmium in rats. J Hazard Mater 164:1304–1309. https://doi.org/10.1016/j.jhazmat.2008.09.041
Tag HM (2015) Hepatoprotective effect of mulberry (Morus nigra) leaves extract against methotrexate induced hepatotoxicity in male albino rat. BMC Complement Altern Med 15:252. https://doi.org/10.1186/s12906-015-0744-y
Valerio V, Kwok M, Loewen H, Winkler J, Mody GM, Scuccimarri R, Meltzer M, Mengistu Y, Feldman CH, Weinblatt ME (2021) Systematic review of recommendations on the use of methotrexate in rheumatoid arthritis. Clin Rheumatol 40:1259–1271. https://doi.org/10.1007/s10067-020-05363-2
Vardi N, Parlakpinar H, Cetin A, Erdogan A, Cetin Ozturk I (2010) Protective effect of β-carotene on methotrexate–induced oxidative liver damage. Toxicol Pathol 38:592–597. https://doi.org/10.1177/0192623310367806
Wang SC, Yi-Chuan H, Hsiao CC, Sheen JM, Huang LT, Lo WS, Hsieh HY, Chen YC (2023) Melatonin protects against methotrexate hepatotoxicity in young rats: Impact of PI3K/Akt/mTOR signaling. J Biochem Mol Toxicol 37:e23323. https://doi.org/10.1002/jbt.23323
Wu Q, Liu L, Miron A, Klímová B, Wan D, Kuča K (2016) The antioxidant, immunomodulatory, and anti-inflammatory activities of Spirulina: an overview. Arch Toxicol 90:1817–1840. https://doi.org/10.1007/s00204-016-1744-5
Yigit F, Gurel-Gurevin E, Isbilen-Basok B, Esener OBB, Bilal T, Keser O, Altiner A, Yilmazer N, Ikitimur-Armutak E (2016) Protective effect of Spirulina platensis against cell damage and apoptosis in hepatic tissue caused by high fat diet. Biotech Histochem 91:182–194. https://doi.org/10.3109/10520295.2015.1114142
Yılmaz O, Yüksek V, Çetin S, Dede S, Tuğrul T (2021) The effects of thymoquinone on DNA damage, apoptosis and oxidative stress in an osteoblast cell line exposed to ionizing radiation. Radiat Eff Defect S 176:575–589. https://doi.org/10.1080/10420150.2021.1898394
Acknowledgements
The authors appreciate the help provided by Dr. Mohamed Elbadawy (Department of Pharmacology, Faculty of Veterinary Medicine, Benha University, Egypt) in performing statistical analysis.
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB). No funding received.
Author information
Authors and Affiliations
Contributions
AB: methodology; AE, MA: designed the experimental protocol; MMSG performed the histopathological and immunohistochemical analyses. MA, FE, AS: original draft preparation, review and editing. All authors read, revised, and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval
The study design was approved by the Research Ethical Committee of the Faculty of Veterinary Medicine, Benha University, Egypt (BUFVTM 11–03-23).
Conflicts of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Behairy, A., Elkomy, A., Elsayed, F. et al. Spirulina and Thymoquinone Protect Against Methotrexate-Induced Hepatic Injury in Rats. Rev. Bras. Farmacogn. 34, 154–167 (2024). https://doi.org/10.1007/s43450-023-00470-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43450-023-00470-y