Abstract
Background
Overwhelming evidence indicates that some naturally occurring coumarins and terpenes are widely used in folk medicine due to their various therapeutic effects affecting the brain. Antiseizure medications (ASMs) are the principal treatment option for epilepsy patients, although some novel strategies based on naturally occurring substances are intensively investigated. This study was aimed at determining the influence of isopimpinellin (ISOP—a coumarin) when administered either separately or in combination with borneol (BOR—a monoterpenoid), on the antiseizure potencies of four classic ASMs (carbamazepine (CBZ), phenytoin (PHT), phenobarbital (PB), and valproate (VPA)) in the mouse model of maximal electroshock-induced (MES) tonic–clonic seizures.
Materials
Tonic–clonic seizures were evoked experimentally in mice after systemic (ip) administration of the respective doses of ISOP, BOR, and classic ASMs. Interactions for two-drug (ISOP + a classic ASM) and three-drug (ISOP + BOR + a classic ASM) mixtures were assessed isobolographically in the mouse MES model.
Results
ISOP (administered alone) had no impact on the anticonvulsant potencies of four classic ASMs. Due to the isobolographic transformation of data, the combination of ISOP + VPA exerted an antagonistic interaction, whereas the two-drug mixtures of ISOP + CBZ, ISOP + PHT, and ISOP + PB produced additive interactions in the mouse MES model. The three-drug combinations of ISOP + BOR with CBZ and PHT produced additive interactions, while the three-drug combinations of ISOP + BOR with PB and VPA exerted synergistic interactions in the mouse MES model.
Conclusions
The most intriguing interaction was that for ISOP + VPA, for which the addition of BOR evoked a transition from antagonism to synergy in the mouse MES model.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Epilepsy as a chronic neurological disorder affects approximately 1% of the world’s population [1, 2]. The principal treatment option for people suffering from epilepsy is monotherapy with a current frontline antiseizure medication (ASM) [3]. If monotherapy fails twice, the patients are on adjunctive treatment as a third option to control their seizures [4]. Despite 25 various ASMs available currently on the pharmaceutical market to treat convulsive and non-convulsive seizures, one-third of epilepsy patients is resistant to the standard ASMs and need more advanced treatment regimens (including dual and triple combinations of ASMs or curative application of novel compounds added to the standard treatment to enhance the anticonvulsant action of the ASMs) so as to properly manage their seizures [5, 6].
Relatively recently, scientific attention has been focused on traditional medicine and curative application of various herbs and medicinal plants in the treatment of patients with epilepsy, due to the confirmed anticonvulsant effects of botanical drugs. The best example of a naturally occurring compound used for ages in traditional medicine in the treatment of epilepsy, which lately became an ASM is cannabidiol (under the tradename of Epidiolex®) [7]. Of course, in traditional medicine, cannabidiol was not used alone as a pure unique drug, but it was given in a mixture of various phytocannabinoids (plant-origin cannabinoids) extracted from leaves of Cannabis sativa spp. There is no doubt that millennial experience in the curative application of some specific herbs and medicinal plants in patients with epilepsy [8, 9], prompted researchers to search for the most active naturally occurring compounds capable of terminating convulsive attacks and/or alleviating seizures [10]. Due to ultra-modern analytical techniques and innovative in vivo assays, it is possible to quickly identify and isolate the bioactive compounds responsible for the anticonvulsant properties of herbal remedies used in traditional medicine [11,12,13]. For instance, some Cannabis sativa L. extracts containing the active ingredients, including Δ9-tetrahydrocannabinol, cannabidiol, and various terpenes (identified qualitatively and quantitatively by ultra-HPLC technique), were investigated with respect to their anticonvulsant properties in an experimental seizure model in mice [14].
At present, a number of botanical drugs containing coumarins are used in traditional medicine for their stomachic, spasmolytic, and sedative effects [15,16,17]. Accumulating evidence indicates that various naturally occurring coumarins (including osthole (OST), imperatorin (IMP), xanthotoxin (XNT), umbelliferone (UMB), and scoparone (SCP)) exerted the anticonvulsant properties in the mouse maximal electroshock-induced seizure (MES) model [18,19,20,21,22,23,24]. Additionally, the mentioned coumarins enhanced the anticonvulsant potencies of some classic ASMs in the mouse MES model [18,19,20,21,22,23,24]. For instance, UMB and SCP significantly potentiated the anticonvulsant action of phenobarbital (PB) and valproate (VPA), but not that of phenytoin (PHT) and carbamazepine (CBZ) [23, 24]. IMP potentiated the antiseizure potencies of CBZ, PHT, and PB, but not that of VPA [21]. XNT enhanced the anticonvulsant action of CBZ and VPA, but not that of PHT and PB [25]. In contrast, OST had no impact on the antiseizure potencies of CBZ, PHT, PB, and VPA [20, 26]. It is worth noting that the MES test in mice corresponds to tonic–clonic seizures and, to a certain extent, to partial convulsions with or without secondary generalization in humans [27].
Accumulating experimental evidence indicates that borneol (BOR—a monoterpenoid) promotes the accumulation of other drugs in brain tissue and increases the brain bioavailability of drugs, including OST [28], and some classic ASMs [24]. BOR inhibits the activity of P-gp in the brain microvascular endothelial cells and reduces the expression of multidrug resistance proteins Mdr1a, Mdr1b, and Mrp1 [29, 30]. Additionally, in the anticonvulsant screening test, BOR itself protected the animals against tonic–clonic seizures in mice subjected to the MES test [31].
In this study, we intended to determine the anticonvulsant profile of isopimpinellin (ISOP)—another naturally occurring coumarin, whose molecular structure is closely related to XNT—a coumarin with confirmed anticonvulsant properties [32]. In the anticonvulsant screening test, ISOP (when administered alone) protected the mice against MES-induced seizures [33]. Additionally, this study was aimed at determining the impact of ISOP (administered alone or in combination with BOR) on the anticonvulsant potencies of four classic ASMs (CBZ, PHT, PB, and VPA) in the mouse model of tonic–clonic seizures in mice.
Materials and methods
Animals and experimental conditions
Male CD-1 outbred mice (8–9 weeks old) were used in this study. Laboratory conditions before and during the experiments were in strict accordance with the EU Directive 2010/63/EU for animal experiments and complied with the ARRIVE guidelines. The animals were housed in a specific pathogen-free facility with a controlled environment and with free access to tap water and food (ad libitum), under standardized housing and laboratory conditions (for more details see [34]). After a week adaptation to laboratory conditions, the mice (weighing 24 ± 3 g) were randomly assigned to experimental groups comprising 8 mice per group. All efforts were made to refine procedures, protect the animals’ welfare, minimize animals’ suffering, and use only the number of animals necessary to produce reliable scientific data according to the 3Rs rule. The experimental protocols and procedures described below were approved by the Local Ethics Committee at the University of Life Sciences in Lublin (License no.: 23/2018 from the 12th February 2018). Total number of mice used in this study was 256.
Drugs
BOR, carbamazepine (CBZ), phenytoin (PHT), phenobarbital (PB), and valproate (VPA) were purchased from Sigma-Aldrich (St. Louis, MO, USA). VPA was dissolved in distilled water while the remaining studied drugs (i.e., BOR, ISOP, CBZ, PHT, and PB) were suspended in a 1% aqueous solution of Tween 80 (Sigma-Aldrich, St. Louis, MO, USA). All the drugs were administered intraperitoneally (ip) as follows: PHT—120 min; PB—60 min; CBZ, ISOP, and VPA—30 min, and BOR—15 min. before the experiments, as reported earlier [24]. ISOP was isolated from dichloromethane extracts obtained from fruits of Pastinaca sativa L. (Apiaceae). From 50 g of dried fruits 7.03 g of crude extract was obtained. The extraction and isolation procedure was similar to this described previously when high-performance counter-current chromatography was used to separate XNT for further ASM studies [35]. Briefly, the 1:1:1:1 n-heptane–ethyl acetate–methanol–water system was used in a reversed-phase system. A portion of the crude extract (200 mg) was dissolved in the biphasic solvent system (6 mL) and injected into a preparative coil of HPCCC Spectrum model (Dynamic Extractions, Slough, UK) multilayer coil-planet J-type centrifuge. The flow rate of the mobile phase was 6 mL/min. Fractions were collected every one minute, then evaporated under reduced pressure, and dissolved in methanol for subsequent purity analysis by HPLC–DAD. The yield of purified ISOP from the injection of crude extract (200 mg) was 3.6 mg with purity of 98%. All of the organic solvents used for extraction and isolation of ISOP were obtained from the Polish Chemical Reagent (Gliwice, Poland) and were of analytical reagent grade. Methanol for HPLC was of chromatographic grade (J.T. Baker Inc., Phillipsburg, NJ, USA), and water used was purified using a Millipore laboratory ultrapure water system (Simplicity TM system, Millipore, Molsheim, France). The standard of ISOP was obtained from Biopurify Phytochemicals Ltd. (Chengdu, Sichuan, China).
Maximal electroshock-induced tonic–clonic seizures in animals
Electroconvulsions (tonic–clonic seizures) in mice were evoked by an alternating current (50 Hz; 500 V; 25 mA) delivered via auricular electrodes. The increasing doses of the classic ASMs were administered and after the respective pretreatment times, the animals were subjected to electroconvulsions. The percent of mice without any seizure activity (i.e., protected from tonic–clonic seizures) along with the respective doses of the ASMs was computed and presented as the median effective dose (ED50) of the ASMs, based on the log-probit method [36]. Each ED50 value corresponds to a dose of the ASM (in mg/kg) predicted to protect half of the animals tested in the MES test. In this study, ISOP was administered in constant doses of 25 and 50 mg/kg; BOR—in a fixed dose of 25 mg/kg; CBZ and PHT—at doses ranging between 6 and 16 mg/kg, PB—at doses ranging between 15 and 35 mg/kg and VPA—at doses ranging between 100 and 350 mg/kg.
Isobolographic transformation of interactions
Doses of all the studied drugs in the mixture (i.e., BOR, ISOP, and classic ASMs) were transformed to the fractions of their ED50 values (from the MES test) and subsequently underwent the isobolographic transformation, as described earlier [37]. Due to the summation of the fractions of all the drugs in the mixture, it was possible to isobolographically characterize the interactions among the tested drugs such as additive, supra-additive (synergistic), or sub-additive (antagonistic) in the mouse MES model. The constant doses of ISOP in the mixture were illustrated graphically as parallel lines to the Y-axis, reflecting these doses, whereas the increasing doses of the ASMs allowed creating the isoboles, as reported earlier [24]. Such a type of transformation takes into account doses of all drugs present in the mixture and their anticonvulsant effects [37].
Statistical analysis
The ED50 values (± SEM) for classic ASMs were calculated from the log-probit method [36], and the method transforming 95% confidence limits to SEM, as described in detail earlier [38]. Statistical comparisons of the respective ED50 values were performed with a one-way ANOVA test followed by the Dunnett’s post hoc test. Statistical comparisons of the respective isobolographic ED50exp and ED50add values for each combination were performed with the unpaired Student’s t-test. GraphPad Prism (version 8.0, San Diego, CA, USA) was used for statistical analysis of all the data (from the MES test and isobolographic transformation). All the isobolograms were drawn in the MS Excel spreadsheet. Differences among the compared values were considered statistically significant if p < 0.05.
Results
Influence of isopimpinellin on the anticonvulsant potency of four classic ASMs in the mouse MES model
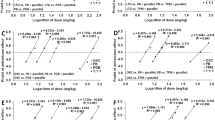
ISOP administered ip at fixed doses of 25 and 50 mg/kg had no impact on the antiseizure effects of CBZ, PHT, PB, and VPA in the mouse MES model (Fig. 1). In the case of CBZ, ISOP at 25 and 50 mg/kg slightly reduced the ED50 value of CBZ in the mouse MES model from 9.52 mg/kg to 8.44 mg/kg (by 11%) and 7.32 mg/kg (by 23%), respectively (Fig. 1a). However, no significant changes among the ED50 values for CBZ were revealed with a one-way ANOVA test (Fig. 1a). ISOP at 25 and 50 mg/kg also reduced the ED50 value of PHT from 8.71 mg/kg to 7.27 mg/kg (by 17%) and 6.13 mg/kg (by 30%), respectively (Fig. 1b), but no significance was observed with a one-way ANOVA test (Fig. 1b). Similarly, ISOP at 25 and 50 mg/kg diminished the ED50 value of PB from 28.85 mg/kg to 26.17 mg/kg (by 9%) and 24.67 mg/kg (by 14%), respectively (Fig. 1c). ISOP administered ip at doses of 25 and 50 mg/kg decreased the ED50 value of VPA from 292 mg/kg to 286 mg/kg (by 2%) and 264 mg/kg (by 10%), respectively (Fig. 1d). In both cases, differences among the ED50 values for PB and VPA were insignificant with a one-way ANOVA test (Fig. 1c and d). ISOP when administered alone protected, in a dose-dependent manner, the animals from MES-induced tonic–clonic seizures, and its ED50 value amounted to 235.7 ± 23.5 mg/kg (results not shown).
Effects of ISOP on the anticonvulsant potency of four classic ASMs in the mouse tonic–clonic seizure model. The columns indicate the ED50 values for CBZ (a), PHT (b), PB (c), and VPA (d) in the mouse MES model. CBZ carbamazepine, ISOP isopimpinellin, PHT phenytoin, PB phenobarbital, VPA valproate. Statistical analysis of data was performed with one-way ANOVA followed by Dunnett’s post hoc test. The total number of animals used for the calculation of ED50 values in this experiment was 192
Isobolographic transformation of interaction between isopimpinellin and four classic ASMs in the mouse MES model
The ED50 values of four classic ASMs (CBZ, PHT, PB, and VPA) along with constant doses of ISOP (25 and 50 mg/kg) were transformed isobolographically so as to classify the exact types of interactions for the studied two-drug combinations (Table 1; Fig. 2a–d). In the case of CBZ, PHT, and PB, no significant difference was observed between the respective ED50exp and ED50add values, confirming the additive nature of interactions among the tested classic ASMs with ISOP (Table 1; Fig. 2a–c). In contrast, the ED50exp value for the mixture of VPA with ISOP (50 mg/kg) considerably differed from the corresponding ED50add value (*p < 0.05; Table 1; Fig. 2d), confirming a sub-additive (antagonistic) interaction between drugs in the mouse MES model (Table 1; Fig. 2d). With isobolographic transformation, it was found that ISOP (25 mg/kg) when combined with VPA produced additive interactions in the mouse MES model (Table 1; Fig. 2d).
Isobolographic transformation of interactions between ISOP and four classic ASMs in the mouse MES model. Interactions between isopimpinellin and carbamazepine (a), phenytoin (b), phenobarbital (c), and valproate (d) are plotted graphically on the system of coordinates. The constant doses of isopimpinellin (25 and 50 mg/kg) in mixtures are plotted as parallel dotted lines to the Y-axis. The diagonal line on each diagram, connecting both X- and Y-axes is the line of additivity, which reflects the theoretically calculated ED50add values. Intersections of the diagonal line with parallel dotted lines illustrate points of additivity (A1 and A2) that correspond to the theoretically calculated ED50add values. Points E1 and E2 reflect the experimentally derived ED50exp values for the two-drug mixtures (ISOP + ASM). *p < 0.05 vs. the respective ED50add value (Student’s t test with Welch’s correction)
Influence of isopimpinellin (ISOP) in combination with borneol (BOR) on the anticonvulsant action of four classic ASMs in the mouse MES model
In the case of CBZ, the combination of ISOP (25 mg/kg) + BOR (25 mg/kg) significantly reduced (by 40%) the ED50 value of CBZ in the mouse MES model from 9.52 mg/kg to 5.73 mg/kg (*p < 0.05; Fig. 3a). The combination of ISOP (25 mg/kg) + BOR (25 mg/kg) also reduced the ED50 value of PHT (by 36%) from 8.71 mg/kg to 5.54 mg/kg (Fig. 3b), but no significance was observed with a one-way ANOVA test (Fig. 3b). In contrast, ISOP (25 mg/kg) + BOR (25 mg/kg) considerably diminished the ED50 value of PB (by 58%) from 28.9 mg/kg to 12.3 mg/kg (****p < 0.0001; Fig. 3c). Similarly, ISOP (25 mg/kg) + BOR (25 mg/kg) significantly decreased the ED50 value of VPA (by 42%) from 292 mg/kg to 169 mg/kg (****p < 0.0001; Fig. 3d).
Effects of isopimpinellin (ISOP) in combination with borneol (BOR) on the anticonvulsant potency of four classic ASMs in the mouse tonic–clonic seizure model. The columns indicate the approx. ED50 values for CBZ (a), PHT (b), PB (c), and VPA (d) in the mouse MES model. CBZ carbamazepine, PHT phenytoin, PB phenobarbital, VEH vehicle, VPA valproate. *p < 0.05 and ****p < 0.0001 vs VEH-treated (control) animals (one-way ANOVA followed by Dunnett’s post hoc test). The total number of animals used for the calculation of ED50 values in this experiment was 256
Isobolographic transformation of interactions for three-drug combinations among borneol (BOR), isopimpinellin (ISOP), and four classic ASMs in the mouse MES model
The three-drug combination of CBZ with ISOP (25 mg/kg) + BOR (25 mg/kg) exerted additive interaction in the mouse MES model with the fraction index value of 0.81 (Table 2). Similarly, the combination of PHT with the constant doses of ISOP and BOR produced additive interaction in the mouse MES model with the fraction index value amounting to 0.85 (Table 2). In the case of the combination of PB with ISOP + BOR, the experimentally derived ED50exp values significantly differed from the additively calculated ED50add values (*p < 0.05), indicating the synergistic interaction among the studied three drugs (Table 2). For the combination of VPA with ISOP + BOR, the synergistic interaction was observed in the mouse MES model because the experimentally derived ED50exp values significantly differed from the additively calculated ED50add values (***p < 0.001; Table 2). For the synergistic interactions, the fraction index values amounted to 0.63 for the combination of PB with ISOP + BOR, and 0.79 for the combination of VPA with ISOP + BOR, respectively (Table 2).
Discussion
The anticonvulsant effects observed for ISOP in combinations with four classic ASMs are quite similar to those reported earlier for osthole (OST). More specifically, OST (simply coumarin) did not affect the anticonvulsant action of CBZ, PHT, PB, or VPA in the mouse MES model [20, 26]. Considering the structural formulas of ISOP, OST, and other coumarins, it is difficult to unequivocally predict the effects of these coumarins on the anticonvulsant activity of classic ASMs. In spite of the structural similarities of ISOP and XNT, their impact on classic ASMs is different. Inversely, the effects produced by ISOP when combined with classic ASMs are identical to those observed for OST, although their structural formulas are not similar. It is worth mentioning that the effects observed for UMB and SCP when combined with classic ASMs are identical (both coumarins potentiated the antiseizure effects of PB and VPA, but not those of CBZ or PHT), and their structural formulas are also quite similar. This fact may suggest the existence of a relationship between the structure of these coumarins (UMB and SCP) and their influence on classic ASMs in the mouse MES model. Unfortunately, such a relationship cannot be ascribed to ISOP and XNT, because the coumarins exerted different effects when combined with classic ASMs in the mouse MES model, albeit their chemical structures are quite similar.
On the other hand, the isobolographic transformation of data revealed that the combinations of ISOP with CBZ, PHT, and PB exerted additive interactions, but the combination of ISOP with VPA produced antagonistic interaction in the mouse MES model. From a pharmacological viewpoint, the antagonistic interaction in terms of seizure suppression is not favorable because ISOP reduced the anticonvulsant potency of VPA in mice subjected to the MES test, as compared to the control (VPA alone-treated) animals. In the case of the combinations of ISOP with CBZ, PHT, and PB, the additive interactions for these two drug mixtures can offer beneficial or neutral effects in terms of seizure suppression in experimental animals. Of note, the isobolographic additivity can be sometimes favorable, especially, if the two-drug mixture offers not only satisfactory seizure suppression but also lesser toxicity, as reported when the drugs are used separately and in higher doses than those when combined in the mixture (for more details, see [39, 40]).
No doubt exists that the isobolographic transformation of data is the best method used in applied pharmacology to classify interactions between drugs, especially, if one of the tested drugs or compounds is not an ASM, but it possesses the anticonvulsant potential [41]. The antagonistic interaction between ISOP and VPA, reported after the isobolographic transformation of data in the mouse MES model, prompted us not to recommend this combination for clinical conditions. A special warning about a potential antagonistic interaction that may occur when combining ISOP with VPA should be addressed to clinicians and potential patients to avoid some potentially harmful effects (i.e., reduction in seizure control) in further polytherapy.
Additionally, we evaluated in this study the influence of BOR in combination with ISOP on the anticonvulsant action of 4 classic ASMs in the mouse MES model. Previously, the effects of BOR (when administered alone) on the anticonvulsant potential of four classic ASMs were assessed in the mouse MES model [24]. Experimental evidence indicated that BOR significantly enhanced the antiseizure effects of PB and VPA in the mouse MES model but, the observed interactions resulted from pharmacokinetic increases in ASMs’ content in the brains of experimental animals [24]. It was reported that BOR significantly elevated total brain contents of PB and VPA, and this fact was the main reason for the significant impact of BOR on the anticonvulsant potentials of classic ASMs in the mouse MES model. Similarly, in this study, we determined the effects of the combinations of ISOP with BOR on the anticonvulsant potential of ASMs. The two-drug mixture of ISOP + BOR did not significantly affect the antiseizure effects of CBZ and PHT, but the mixture of ISOP + BOR enhanced the antiseizure effects of PB and VPA in the mouse MES model.
The isobolographic transformation of data for the three-drug combinations of ISOP + BOR + VPA and ISOP + BOR + PB revealed that the interactions were supra-additive (synergistic) in the mouse MES model, whereas the combinations of ISOP + BOR with CBZ and PHT were additive in nature. It was reported herein that BOR potentiated by itself the anticonvulsant potency of VPA in the mouse MES model, without any collaborative effects of ISOP. In contrast, BOR enhanced the anticonvulsant potency of PB in the mouse MES model offering the synergistic interaction, but only in the presence of ISOP. The lack of ISOP in the mixture makes the combination of BOR with PB only additive in the mouse tonic–clonic seizure model [24], despite an increase in the total brain content of PB after BOR administration.
Of note, a transition from antagonism to synergistic interaction has been demonstrated in this study in the mouse MES model in the case of the combination of ISOP + VPA. BOR seems to be a good candidate drug to increase brain permeability of some classic ASMs, especially PB and VPA.
The superiority of the isobolographic transformation of data over the subthreshold method used in experimental epileptology has been confirmed earlier [42]. Additionally, the isobolographic summation of the anticonvulsant fractions of all the tested drugs in the mixture makes the results more reliable (for more detailed information, see [37, 43]).
Another fact needs a special explanation when extrapolating the results from this preclinical study to further experimental conditions. The anticonvulsant effects produced by the mixture of ISOP + BOR on VPA were substantially higher than those observed for the mixture of VPA with ISOP alone. Adding BOR allowed for exceeding the antagonistic interaction for ISOP + VPA and exerting supra-additive interaction for the three-drug combination of ISOP + BOR + VPA in the mouse MES model. Although, the change in type of interaction from antagonism to synergy was highly likely associated with a significant elevation of total brain VPA concentrations (as reported earlier), this pharmacokinetic nature of interaction among drugs seems to be solely responsible for the observed effects.
This study has also some limitations, which should be mentioned herein, i.e., when translating or extrapolating the results of this study to clinical conditions. First, only some possible pharmacokinetic interactions among BOR and PB or VPA were taken into account because, as reported earlier, BOR elevated the total brain content of PB and VPA in experimental animals. However, neither the total brain content of ISOP and BOR in mice receiving ASMs was verified, nor total brain concentrations of CBZ and PHT were measured. Second, only one animal species (mice) was used. No experiments on rats or zebrafish larvae were conducted to confirm the anticonvulsant activity of ISOP in in vivo studies. Third, only one experimental seizure model (MES test) in mice was used as a model of tonic–clonic seizures. Fourth, the most important limitation is the fact that ISOP and BOR, in contrast to clinical conditions, were tested after their single systemic (ip) administration in the acute seizure model. No chronic (prolonged) oral administration of the tested substances and ASMs was performed. Despite all the above-mentioned limitations, this experimental study provides us with clear-cut information about the anticonvulsant activity of ISOP when administered alone and in combination with classic ASMs and BOR that would be potentially useful in further preclinical or clinical studies.
Conclusions
ISOP when added to the studied classic ASMs (CBZ, PB, and PHT) produced additive interactions, but special attention should be paid to the combination with VPA, which occurred antagonistically in the mouse MES model. BOR added to the mixtures of ISOP with ASMs potentiated the anticonvulsant activity of PB and VPA, exerting synergistic interactions in the mouse MES model. The three-drug mixtures of BOR, ISOP, and CBZ or PHT produced additive interactions in the tonic–clonic seizure model in mice. Unfortunately, BOR significantly increased the total brain concentrations of the tested ASMs, contributing to the pharmacokinetic nature of observed synergistic interactions with VPA and PB in the mouse MES model. BOR in two-drug and three-drug mixtures with CBZ or PHT exerted additive interaction in the mouse MES model.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- ASM:
-
Antiseizure medication
- BOR:
-
Borneol
- CBZ:
-
Carbamazepine
- IMP:
-
Imperatorin
- ISOP:
-
Isopimpinellin
- MES:
-
Maximal electroshock-induced seizures
- OST:
-
Osthole
- PB:
-
Phenobarbital
- PHT:
-
Phenytoin
- SCP:
-
Scoparone
- UMB:
-
Umbelliferone
- VPA:
-
Valproate
- XNT:
-
Xanthotoxin
References
Thijs RD, Surges R, O’Brien TJ, Sander JW. Epilepsy in adults. Lancet. 2019;393:689–701. https://doi.org/10.1016/S0140-6736(18)32596-0.
Citraro R, Leo A. Epilepsy and Related Neuropsychiatric Comorbidities: Basic and Clinical Research. Curr Neuropharmacol. 2023;21:1632–3. https://doi.org/10.2174/1570159X2108230510162504.
Nunes VD, Sawyer L, Neilson J, Sarri G, Cross JH. Diagnosis and management of the epilepsies in adults and children: summary of updated NICE guidance. BMJ. 2012;344: e281. https://doi.org/10.1136/bmj.e281.
Brodie MJ, Sills GJ. Combining antiepileptic drugs–rational polytherapy? Seizure. 2011;20:369–75. https://doi.org/10.1016/j.seizure.2011.01.004.
Stephen LJ, Brodie MJ. Antiepileptic drug monotherapy versus polytherapy: pursuing seizure freedom and tolerability in adults. Curr Opin Neurol. 2012;25:164–72. https://doi.org/10.1097/WCO.0b013e328350ba68.
Tomson T, Zelano J, Dang YL, Perucca P. The pharmacological treatment of epilepsy in adults. Epileptic Disord. 2023. https://doi.org/10.1002/epd2.20093.
Flamini RJ, Comi AM, Bebin EM, Chez MG, Clark G, Devinsky O, et al. Efficacy of cannabidiol in convulsive and nonconvulsive seizure types associated with treatment-resistant epilepsies in the expanded access program. Epilepsia. 2023. https://doi.org/10.1111/epi.17665.
Brillatz T, Jacmin M, Vougogiannopoulou K, Petrakis EA, Kalpoutzakis E, Houriet J, et al. Antiseizure potential of the ancient Greek medicinal plant Helleborus odorus subsp. cyclophyllus and identification of its main active principles. J Ethnopharmacol. 2020;259:112954. https://doi.org/10.1016/j.jep.2020.112954.
Adams M, Schneider S-V, Kluge M, Kessler M, Hamburger M. Epilepsy in the Renaissance: a survey of remedies from 16th and 17th century German herbals. J Ethnopharmacol. 2012;143:1–13. https://doi.org/10.1016/j.jep.2012.06.010.
Challal S, Skiba A, Langlois M, Esguerra CV, Wolfender J-L, Crawford AD, et al. Natural product-derived therapies for treating drug-resistant epilepsies: from ethnopharmacology to evidence-based medicine. J Ethnopharmacol. 2023;317: 116740. https://doi.org/10.1016/j.jep.2023.116740.
Goel RK, Gawande D, Lagunin A, Randhawa P, Mishra A, Poroikov V. Revealing medicinal plants that are useful for the comprehensive management of epilepsy and associated comorbidities through in silico mining of their phytochemical diversity. Planta Med. 2015;81:495–506. https://doi.org/10.1055/s-0035-1545884.
Brillatz T, Jacmin M, Queiroz EF, Marcourt L, Morin H, Shahbazi N, et al. Identification of potential antiseizure agents in boswellia sacra using in vivo zebrafish and mouse epilepsy models. ACS Chem Neurosci. 2021;12:1791–801. https://doi.org/10.1021/acschemneuro.1c00044.
Chipiti T, Viljoen AM, Cordero-Maldonado ML, Veale CGL, Van Heerden FR, Sandasi M, et al. Anti-seizure activity of African medicinal plants: the identification of bioactive alkaloids from the stem bark of Rauvolfia caffra using an in vivo zebrafish model. J Ethnopharmacol. 2021;279: 114282. https://doi.org/10.1016/j.jep.2021.114282.
Costa AM, Senn L, Anceschi L, Brighenti V, Pellati F, Biagini G. Antiseizure effects of fully characterized non-psychoactive Cannabis sativa L. extracts in the repeated 6-Hz corneal stimulation test. Pharmaceuticals. 2021;14(12):1259. https://doi.org/10.3390/ph14121259.
Shi B, Liu J, Zhang Q, Wang S, Jia P, Bian L, et al. Effect of co-administration of Acori Tatarinowii Rhizoma volatile oil on pharmacokinetic fate of xanthotoxol, oxypeucedanin hydrate, and byakangelicin from Angelicae Dahuricae Radix in rat. J Sep Sci. 2020;43:2349–62. https://doi.org/10.1002/jssc.201901250.
Ahmad N, Hui-Yin Y, Makmor-Bakry M. Mechanisms of natural products as potential antiepileptic drugs. Pak J Pharm Sci. 2022;35:1043–53.
Zhu H-L, Wan J-B, Wang Y-T, Li B-C, Xiang C, He J, et al. Medicinal compounds with antiepileptic/anticonvulsant activities. Epilepsia. 2014;55:3–16. https://doi.org/10.1111/epi.12463.
Łuszczki JJ, Marczewski T, Mazurkiewicz LP, Karwan S, Teresińska M, Florek-Łuszczki M, et al. Influence of osthole on the anticonvulsant activity of phenytoin and valproate in the maximal electroshock-induced seizures in mice. Ann Univ Mariae Curie-Sklodowska, Sect DDD Pharm. 2011;24:33–44.
Łuszczki JJ, Wojda E, Andres-Mach M, Cisowski W, Glensk M, Glowniak K, et al. Anticonvulsant and acute neurotoxic effects of imperatorin, osthole and valproate in the maximal electroshock seizure and chimney tests in mice: A comparative study. Epilepsy Res. 2009;85:293–9. https://doi.org/10.1016/j.eplepsyres.2009.03.027.
Łuszczki JJ, Rekas A, Mazurkiewicz LR, Gleńsk M, Ossowska G. Effect of osthole on the protective activity of carbamazepine and phenobarbital against maximal electroshock-induced seizures in mice. Ann Univ Mariae Curie-Sklodowska, Sect DDD Pharm. 2010;23:145–56.
Łuszczki JJ, Wojda E, Raszewski G, Głowniak K, Czuczwar SJ. Influence of imperatorin on the anticonvulsant activity and acute adverse-effect profile of lamotrigine in maximal electroshock-induced seizures and chimney test in mice. Pharmacol Rep. 2008;60:566–73.
Zagaja M, Pyrka D, Skalicka-Wozniak K, Glowniak K, Florek-Luszczki M, Glensk M, et al. Effect of xanthotoxin (8-methoxypsoralen) on the anticonvulsant activity of classical antiepileptic drugs against maximal electroshock-induced seizures in mice. Fitoterapia. 2015;105:1–6. https://doi.org/10.1016/j.fitote.2015.05.020.
Zagaja M, Andres-Mach M, Skalicka-Woźniak K, Rękas AR, Kondrat-Wróbel MW, Gleńsk M, et al. Assessment of the combined treatment with umbelliferone and four classical antiepileptic drugs against maximal electroshock-induced seizures in mice. Pharmacology. 2015;96:175–80. https://doi.org/10.1159/000438704.
Łuszczki JJ, Bojar H, Góralczyk A, Skalicka-Woźniak K. Antiseizure effects of scoparone, borneol and their impact on the anticonvulsant potency of four classic antiseizure medications in the mouse MES model—an isobolographic transformation. Int J Mol Sci. 2023. https://doi.org/10.3390/ijms24021395.
Zagaja M, Andres-Mach M, Patrzylas P, Pyrka D, Szpringer M, Florek-Łuszczki M, et al. Influence of xanthotoxin (8-methoxypsoralen) on the anticonvulsant activity of various novel antiepileptic drugs against maximal electroshock-induced seizures in mice. Fitoterapia. 2016;115:86–91. https://doi.org/10.1016/j.fitote.2016.09.020.
Łuszczki JJ, Andres-Mach M, Cisowski W, Mazol I, Glowniak K, Czuczwar SJ. Osthole suppresses seizures in the mouse maximal electroshock seizure model. Eur J Pharmacol. 2009;607:107–9. https://doi.org/10.1016/j.ejphar.2009.02.022.
Löscher W. Animal models of seizures and epilepsy: past, present, and future role for the discovery of antiseizure drugs. Neurochem Res. 2017;42:1873–88. https://doi.org/10.1007/s11064-017-2222-z.
Luo D-D, Chen X-Y, Zhang Z-B, Sun C-Y, Zheng Y-F, Liu Y-H, et al. Different effects of (+)-borneol and (-)-borneol on the pharmacokinetics of osthole in rats following oral administration. Mol Med Rep. 2017;15:4239–46. https://doi.org/10.3892/mmr.2017.6502.
Yu B, Ruan M, Dong X, Yu Y, Cheng H. The mechanism of the opening of the blood-brain barrier by borneol: a pharmacodynamics and pharmacokinetics combination study. J Ethnopharmacol. 2013;150:1096–108.
Fan X, Chai L, Zhang H, Wang Y, Zhang B, Gao X. Borneol depresses P-glycoprotein function by a NF-κB signaling mediated mechanism in a blood brain barrier in vitro model. Int J Mol Sci. 2015;16:27576–88. https://doi.org/10.3390/ijms161126051.
Skalicka-Woźniak K, Walasek M, Aljarba TM, Stapleton P, Gibbons S, Xiao J, et al. The anticonvulsant and anti-plasmid conjugation potential of thymus vulgaris chemistry: an in vivo murine and in vitro study. Food Chem Toxicol. 2018;120:472–8. https://doi.org/10.1016/j.fct.2018.07.045.
Łuszczki JJ, Andres-Mach M, Gleńsk M, Skalicka-Woźniak K. Anticonvulsant effects of four linear furanocoumarins, bergapten, imperatorin, oxypeucedanin, and xanthotoxin, in the mouse maximal electroshock-induced seizure model: a comparative study. Pharmacol Rep. 2010;62:1231–6. https://doi.org/10.1016/S1734-1140(10)70387-X.
Tosun F, Kızılay ÇA, Erol K, Kılıç FS, Kürkçüoğlu M, Can Başer KH. Anticonvulsant activity of furanocoumarins and the essential oil obtained from the fruits of Heracleum crenatifolium. Food Chem. 2008;107:990–3. https://doi.org/10.1016/j.foodchem.2007.08.085.
Łuszczki JJ, Panasiuk A, Zagaja M, Karwan S, Bojar H, Plewa Z, et al. Polygonogram and isobolographic analysis of interactions between various novel antiepileptic drugs in the 6-Hz corneal stimulation-induced seizure model in mice. PLoS ONE. 2020;15(6): e0234070. https://doi.org/10.1371/journal.pone.0234070.
Skalicka-Woźniak K, Zagaja M, Głowniak K, Łuszczki JJ. Purification and anticonvulsant activity of xanthotoxin (8-methoxypsoralen). Cent Eur J Biol. 2014;9:431–6. https://doi.org/10.2478/s11535-013-0275-9.
Litchfield JT, Wilcoxon F. A simplified method of evaluating dose-effect experiments. J Pharmacol Exp Ther. 1949;96:99–113.
Łuszczki JJ, Danysz W, Czuczwar SJ. Interactions of MRZ 2/576 with felbamate, lamotrigine, oxcarbazepine and topiramate in the mouse maximal electroshock-induced seizure model. Pharmacology. 2008;81:259–65. https://doi.org/10.1159/000114870.
Łuszczki JJ, Ratnaraj N, Patsalos PN, Czuczwar SJ. Isobolographic analysis of interactions between loreclezole and conventional antiepileptic drugs in the mouse maximal electroshock-induced seizure model. Naunyn Schmiedebergs Arch Pharmacol. 2006;373:169–81. https://doi.org/10.1007/s00210-006-0055-4.
Łuszczki JJ, Czuczwar SJ. Interaction between lamotrigine and felbamate in the maximal electroshock-induced seizures in mice: an isobolographic analysis. Eur Neuropsychopharmacol. 2005;15:133–42. https://doi.org/10.1016/j.euroneuro.2004.06.002.
Łuszczki JJ, Zagaja M, Miziak B, Kondrat-Wrobel MW, Zaluska K, Wroblewska-Luczka P, et al. Beneficial combination of lacosamide with retigabine in experimental animals: an isobolographic analysis. Pharmacology. 2018;101:22–8. https://doi.org/10.1159/000480019.
Berenbaum MC. What is synergy? Pharmacol Rev. 1989;41:93–141.
Łuszczki JJ, Czuczwar SJ. Isobolographic and subthreshold methods in the detection of interactions between oxcarbazepine and conventional antiepileptics—a comparative study. Epilepsy Res. 2003;56:27–42. https://doi.org/10.1016/j.eplepsyres.2003.08.003.
Łuszczki JJ, Marzeda P, Gut-Lepiech A, Kondrat-Wróbel MW, Wróblewska-Łuczka P, Karwan S, et al. New derivative of 1,2,4-triazole-3-thione (TP427) potentiates the anticonvulsant action of valproate, but not that of carbamazepine, phenytoin or phenobarbital in the mouse tonic-clonic seizure model. Pharmacol Rep. 2019;71:299–305. https://doi.org/10.1016/j.pharep.2019.01.003.
Funding
This work was supported by the National Science Center, Poland, grant number 2017/27/B/NZ4/00917, Narodowe Centrum Nauki.
Author information
Authors and Affiliations
Contributions
“Conceptualization: JJL, and KS-W; methodology: HB, and MF-Ł; software: JCh; validation: HB, JCh; formal analysis: JJL; investigation: HB, KJ and JJL; resources: KJ, MF-Ł and KS-W; data curation: JCh and HB; writing—original draft preparation: MF-Ł; writing—review and editing: JJL and KS-W; visualization: MF-Ł; supervision: JJL and KS-W; project administration: MF-Ł and KS-W; funding acquisition: KS-W. All authors have read and agreed to the published version of the manuscript.”
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript or in the decision to publish the results.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Łuszczki, J.J., Bojar, H., Jankiewicz, K. et al. Anticonvulsant effects of isopimpinellin and its interactions with classic antiseizure medications and borneol in the mouse tonic–clonic seizure model: an isobolographic transformation. Pharmacol. Rep 75, 1533–1543 (2023). https://doi.org/10.1007/s43440-023-00532-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43440-023-00532-x