Abstract
Introduction
The purpose of this study is to provide a state-of-the-art review regarding risk factors for perioperative complications in adult spinal deformity (ASD) surgery. The review includes levels of evidence for risk factors associated with complications in ASD surgery.
Methods
Using the PubMed database, we searched for complications, risk factors, and adult spinal deformity. The included publications were assessed for level of evidence as described in clinical practice guidelines published by the North American Spine Society, with summary statements generated for each risk factor (Bono et al. in Spine J 9:1046–1051, 2009).
Results
Frailty had good evidence (Grade A) as a risk for complications in ASD patients. Fair evidence (Grade B) was assigned for bone quality, smoking, hyperglycemia and diabetes, nutritional status, immunosuppression/steroid use, cardiovascular disease, pulmonary disease, and renal disease. Indeterminate evidence (Grade I) was assigned for pre-operative cognitive function, mental health, social support, and opioid utilization.
Conclusions
Identification of risk factors for perioperative complications in ASD surgery is a priority for empowering informed choices for patients and surgeons and managing patient expectations. Risk factors with grade A and B evidence should be identified prior to elective surgery and modified to reduce the risk of perioperative complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adult spinal deformity (ASD) has a significant impact on health-related quality of life (HRQOL). The incidence of ASD increases with age and may present in the form of scoliosis, kyphosis, spondylolisthesis, or rotatory subluxation, with accompanying neurological and functional deficits [2, 3]. Questionnaires that quantify HRQOL, including as the Owestry Disability Index (ODI), Scoliosis Research Society score (SRS), and Short Form 36 (SF-36), show that ASD patients have greater functional limitations, greater pain, and poorer mental health than age-matched controls and patients with other chronic medical conditions [3,4,5,6]. Generational decline of HRQOL is substantially higher in ASD patients compared to the general population [7]. Current estimates show that 27.5 million patients in the US are living with ASD, accounting for a significant societal burden that is projected to increase [8].
Surgical intervention for ASD is accompanied by a high incidence of complications (25–52%) [9, 10]. Major perioperative complications of ASD surgery, albeit less common, can include sepsis, adverse cardiac events, and respiratory and renal failure [11,12,13,14]. Both perioperative and late-stage (i.e. non-union) complications can reduce the chance of surgical benefit [15]. Moreover, the costs of ASD surgery can rise by up to 70% with re-admissions, establishing a financial incentive for reducing complications [16].
Knowledge of relevant risk factors for ASD surgery can empower clinicians and patients to gain insight into the expected postoperative course. Understanding which existing risk factors can contribute to complications may enable patients to make more informed choices preoperatively and allow for a better-shared decision-making ability [17]. Moreover, setting realistic expectations with patients prior to surgery can significantly improve patient satisfaction [18].
The purpose of this state-of-the-art review is to summarize and provide a level of evidence for, the association between proposed risk factors and perioperative complications following ASD surgery. The following risk factors will be explored: obesity, bone quality & osteoporosis, frailty, smoking, blood sugar, nutritional status, immunosuppression & steroid use, cardiovascular disease, pulmonary disease, renal disease, pre-cognitive function, mental health, social support, and opioid utilization.
Methods
A literature search was conducted using the PubMed database, with intention of identifying publications pertaining to risk factors of interest and their relation to complications associated with ASD surgery. Keywords including the variables of interest (i.e. “obesity”, “BMI”, “frailty’” etc.) in addition to “adult spinal deformity” and “spine surgery” were used. In cases where the literature specific to ASD was limited, articles with cohorts of patients with spinal surgery beyond ASD were included. The included publications were assessed for level of evidence as described in clinical practice guidelines published by the North American Spine Society, reproduced below [1]:
A: Good evidence—Level I studies with consistent findings for or against recommending a variable as a risk factor.
B: Fair evidence – Level II or III studies with consistent findings for or against recommending a variable as a risk factor.
C: Poor evidence – Level IV or V studies for or against recommending a variable as a risk factor.
I: Insufficient or conflicting evidence not allowing a recommendation for or against intervention.
A summary statement for each specific risk factor was also generated.
Results
Obesity
Several studies have examined the effect of obesity on complications associated with surgical correction of ASD. A retrospective review by Amin et al. of 244 patients found that BMI > 35 was associated with significantly worse perioperative outcomes and higher cost compared to non-obese patients [19]. Brown et al. also found that obesity was associated with increased costs per quality-adjusted life year in patients undergoing ASD surgery [20]. However, other studies have reported no association between obesity and complications. A retrospective review by Soroceanu et al. of 448 patients found that BMI was not a significant risk factor for the development of post-operative medical complications [13]. These results were echoed by Elsamadicy et al. who reported that obesity did not significantly affect surgical outcomes, patient-reported pain scores, and 30-day readmission rates after complex spinal surgery [21]. Yagi et al. conducted a retrospective review of 195 patients who underwent surgical treatment of ASD with the aim of developing a predictive model for major complications at two years after surgery, and while several patient factors were found to be independent predictors of complications, obesity was not one of them [22].
In summary, obesity has been associated with increased complication rates and increased cost of care in spine surgery, but some studies analyzing the relationship between elevated BMI and surgical complications in adult spinal deformity surgery have shown a lack of significant association.
Grade of recommendation – I: There is insufficient evidence that obesity is a risk factor for perioperative complications in ASD surgery.
Bone quality and osteoporosis
Bone quality is an important consideration when planning ASD surgery, and several reports in the literature underscore the value of bone mineral density (BMD) assessment as part of the preoperative medical workup. One retrospective review of 144 patients who underwent ASD surgery found that bone metabolism disorders are highly prevalent in elderly patients scheduled for spinal surgery and strongly recommended preoperative evaluation of BMD [23]. A recent retrospective comparative study found that the GAP score combined with BMI and BMD was better able to predict mechanical complications than the GAP score alone [24]. Another retrospective review of a multi-center ASD database evaluation by Yagi et al. concluded that low BMD was a significant risk factor for proximal junctional failure, recommending that surgeons consider prophylactic treatments when correcting ASD in patients with low BMD [25].
Kuprys et al. recommended that clinical practice guidelines be established on preoperative bone quality assessment for spine patients [26]. Bone quality assessment is typically done with a dual-energy x-ray absorptiometry (DEXA) scan, but it is important to note that in ASD, spine DEXA scans can be inaccurate. Use of DEXA of at least the hip and forearm was recommended for all ASD patients by Gupta et al., as a single scan of the hip can lead to misdiagnosis, which can be costly in the setting of ASD [27].
Grade of recommendation – B: there is fair evidence that osteoporosis is a risk factor for perioperative complications in ASD surgery.
Frailty
Frailty has garnered considerable attention as a potential metric that can be used to predict recovery and postoperative complications after ASD surgery. An international consensus group has defined frailty as, “A medical syndrome with multiple causes and contributors that is characterized by diminished strength, endurance, and reduced physiologic function that increases an individual’s vulnerability for developing increased dependency and/or death” [28]. With respect to ASD, studies have used the Adult Spinal Deformity Frailty Index (ASD-FI), the modified Frailty Index (mFI), and its truncated version, the mFI-5.
Each frailty risk score has been extensively validated. The ASD-FI stratifies patients as not frail (NF) (< 0.3 points), frail (0.3–0.5 points), or severely frail (SF) (> 0.5 points). Retrospective analyses of prospectively maintained multi-center databases have shown that greater patient frailty, as determined by the ASD-FI, is associated with a greater risk of serious complications (i.e. deep wound infection, pseudoarthrosis, proximal junctional kyphosis, wound dehiscence, reoperation) [29,30,31]. Leven et al. reported that mFI scores were also associated with increased rates of complications, reoperations, and mortality in a retrospective review of 1,001 ASD patients acquired from the National Surgical Quality Improvement Program multicenter database [32]. Finally, Yagi et al. utilized the mFI-5 to score patients as 0 (robust), 1 (prefail), or ≥ 2 (frail strata), and concluded that the mFI and the mFI-5 were similarly efficacious at predicting surgical adverse events (SAEs) (weighted Kappa: 0.87) [33]. Despite differing frailty index modalities, the literature agrees with its association with poor clinical outcomes and postoperative complications [34].
Grade of Recommendation – A: There is good evidence that frailty is a risk factor for perioperative complications in adult spinal deformity surgery.
Smoking
The effects of tobacco smoke and ASD surgery are well documented. Soroceanu et al. and Zhang et al. reported that smoking was an independent risk factor for the development of post-operative medical complications, including cardiopulmonary and infectious [13, 35]. A history of smoking was found by Puvanesarajah et al. to be a risk factor for post-operative transfusions [36]. Using data from the SCOLI-RISK-1 Study, Wilson et al. found that a history of smoking significantly increased the risk of excessive intra-op bleeding [37]. Several studies have also found smoking history to be significantly associated with reoperations for ASD patients [38]. Smoking may also be an independent risk factor for mechanical failure, as shown in a series of 76 ASD patients by Inoue et al. [39]. In a study of 1,570 patients from the NSQIP database who underwent instrumentation > 7 levels for ASD, Wade et al. found that a history of smoking was an independent risk factor for surgical delay, and patients experiencing such delay demonstrated an almost sevenfold increase in mortality rate (3.4 vs. 0.5%) [40].
While several studies support smoking as a negative effector of outcomes and complication rates, some have found conflicting results. In a retrospective study, Elsamadicy et al. noted that a history of smoking did not affect 30-day readmission rates in 839 ASD patients [41]. While another study using data from the American College of Surgeon National Surgical Quality Improvement Program (ACS-NSQIP) database reported that smoking was not associated with higher 30-day complication rates or mortality, the authors recommended smoking cessation before spinal fusion given the known negative health effects of smoking.
Grade of Recommendation – B: There is fair evidence that smoking is a risk factor for perioperative complications in adult spinal deformity surgery.
Blood sugar and diabetes
There is a positive association between diabetes and perioperative complications for patients with spinal surgery. Two retrospective reviews of the Healthcare Cost and Utilization Project Nationwide Readmissions Database (HCUP-NRD) have demonstrated diabetes as an independent risk factor for perioperative complications after controlling for other comorbidities [42, 43]. Elasmadicy et al. found that diabetic patients experienced increased readmission rates within 30 days and 90 days post-surgery, with infection being the most prevalent cause (30 days: 18.5%, 31–90 days: 7.4%) [42]. Rubel et al. determined that controlled and uncontrolled diabetes contributed significantly to increased odds of 90-day readmissions (top 3 causes: implant-related complications, disc herniation, postoperative infection) [43]. These findings are supported by a study by Guzman et al. using the Healthcare Cost and Utilization Project Nationwide Inpatient Sample (HCUP-NIS), where inpatient mortality in patients undergoing surgery for degenerative cervical spine pathology was shown to be associated with uncontrolled diabetes [44]. Only one study conducted by Shuman et al. found no association between complications and 90-day readmissions with diabetes, but the study reported an association between diabetes with prolonged length of stay and non-home discharge [45].
An unanswered question is whether the diabetic disease process or absolute blood glucose levels impact operative outcomes. Studies in which serum glucose has been directly measured have demonstrated its strength in predicting health outcomes. In patients without a formal diagnosis of diabetes, the risk of surgical site infection was doubled (2.1 to 4.4%) if perioperative blood glucose measurements were greater than 140 mg/dL (p = 0.01) [46]. Similar results were found in a case–control study by Pennington et al. in which multivariable analysis showed that history of diabetes mellitus, maximum daily glucose variation, and peak postoperative glucose were found to be significant predictors of wound infection [47]. These studies infer that both diabetes and elevated blood glucose levels increase patient risk for post-operative infection.
Grade of Recommendation – B: There is fair evidence that elevated blood sugar is a risk factor for perioperative complications in ASD surgery.
Nutritional status
Several studies have linked malnutrition with post-surgical complications, but there is sparse literature on the association in the context of spine surgery. Serum albumin is widely used as a biomarker of nutritional status within patients undergoing surgical operations, with a value of less than 3.5 g/dL used as the standard marker of malnutrition [48]. Hypoalbuminemia was found to be independently associated with revision surgery for septic reasons and with acute postoperative infections within 30 days of aseptic revisions [49]. In a multivariate logistic regression analysis study of ASD patients, Phan et al. revealed low serum albumin to be an independent risk for 30-day mortality, length of stay greater than 5 days, all complications, pulmonary complications, renal complications, and intra-postoperative red blood cell transfusion [50]. Similar results were observed in a study by Schonfeld et al. in which serum albumin was associated with increased 30-day mortality, major complications, wound infections, and thromboembolic disease [51]. An additional study using the PearlDiver database by Puvanesarajah et al. found that patients with malnutrition had increased odds of 90 day major medical complications, including cerebrovascular accident, pulmonary embolism, pneumonia, myocardial infarction, and acute renal failure [52].
Grade of Recommendation – B: There is fair evidence that nutritional status is a risk factor for perioperative complications in ASD surgery.
Immunosuppression and steroid use
There is a strong positive association between preoperative immunosuppression in patients with ASD and perioperative complications. Two retrospective reviews of the ACS-NSQIP database have shown this relationship for chronic oral steroid use when controlling for patient comorbidities and other potential confounds. White et al. found that oral and parenteral steroid use were associated with perioperative mortality, wound dehiscence, deep vein thrombosis, and blood transfusion [53]. Di Capua et al. showed chronic oral steroid use independently increased the risk of surgical site infection, urinary tract infection, or venous thromboembolism within 30 days of surgery [54]. A single-center study by Tang et al. also demonstrated steroid use for a chronic condition as a predictor of 90-day postoperative complications [55].
The effect of autoimmune disease, independent of immunosuppression, on perioperative complications is less certain. While a Nationwide Inpatient Sample analysis conducted by Bernstein et al. showed an increased risk of total perioperative complications for patients with rheumatoid arthritis (RA) compared to those without (29.9 vs. 24.6%, p < 0.001), it did not control for potential confounding factors, including steroid use, between patients with and without RA [56].
Grade of Recommendation – B: There is fair evidence that immunosuppression and steroid use are risk factors for perioperative complications in ASD surgery.
Cardiovascular disease
The relationship between cardiovascular diseases and perioperative complications following surgery in patients with ASD is likely causal. A large cohort study of 30,330 patients who underwent spine surgery determined that risk factors for the development of cardiac complications within 30 days post-surgery included a history of cardiac disorders and treatments [57]. The development of a cardiac complication before discharge was also associated with a greater length of stay (7.9 versus 2.6 days; p < 0.001). Moreover, both Zhao et al. and Soroceanu et al. found hypertension to be a significant risk factor for postoperative deep venous thrombosis (DVT) [13, 58]. Utilizing registry data of 1,592 adult patients, Guyot et al. determined that previous cardiac history yielded statistically significant risk factors for cardiac complication after spine surgery, especially for patients in age groups 40–46 and > 65 [59].
Grade of Recommendation – B: There is fair evidence that cardiovascular disease is a risk factor for perioperative complications in ASD surgery.
Pulmonary disease
There is an association between pulmonary diseases and perioperative complications following surgery in patients with ASD, with an emphasis on chronic obstructive pulmonary disease (COPD). In a retrospective study of 64,891 patients undergoing lumbar surgical procedures, Murgai et al. found that for patients with prior COPD, incidences of pulmonary collapse (5.6%; RR = 1.64), pneumonia (3.54%; RR = 2.63), and pleural effusion (2.55%; RR = 1.99) were significantly greater compared to patients without the risk factors [60]. Tang et al. also verified that postoperative complications were strongly associated with a history of severe COPD [55]. In a retrospective case–control study of 323 adult patients undergoing posterior spinal instrumentation and fusion for congenital scoliosis, Wu et al. found that the independent risk factors for the development of pulmonary complications included preoperative pulmonary disease [61]. Abnormal pulmonary function test (PFT) results have also yielded associations with pulmonary complications following surgery. In an analysis of 298 patients, Zhang et al. found that as pulmonary function decreased, pulmonary complication incidences increased: 31.6% [forced vital capacity (FVC) < 40%], 7.4% (FVC 40–60%) FVC, and 2.7% (FVC 60–80% FVC) [62].
However, other studies show no significant association between pulmonary risk factors and perioperative complications in ASD surgery. In a retrospective, multi-center, case–control study of 953 ASD patients, Schwab et al. found that cardiopulmonary status and co-morbidities were not significantly associated with major perioperative complications [63]. Liang et al. also found a similar result in a retrospective clinical study of 88 patients with moderate or severe pulmonary dysfunction, indicating that prior respiratory symptoms and FVC play little role in postoperative pulmonary complications [64].
Grade of Recommendation – B: There is fair evidence that pulmonary disease is a risk factor for perioperative complications in ASD surgery.
Renal disease
Multiple studies suggested that patients with chronic kidney disease (CKD) (Stage 3–5) have higher complication rates and increased mortality following adult spinal surgery. A study in 2017 by Bains et al. demonstrated that patients with CKD had a 1.78 odds ratio (OR) of increased mortality following spine surgery compared to patients with normal kidney function [65]. If the patient was on dialysis, that OR increased to 4.18. Another study by Adogwa et al. noted that patients with CKD were more likely to be admitted to the ICU (53 vs 29%), have post-operative delirium (27.8 vs 8.4%), have UTIs (27.8 vs 6.9%), and have DVTs (5.6 vs 0.4%) when compared to those without CKD [66]. A 2012 study by Chikuda et al. found that there was a ten-fold increase in-hospital mortality in patients who were undergoing dialysis compared to patients who were not undergoing dialysis [67].
Grade of Recommendation – B: There is fair evidence that renal disease is a risk factor for perioperative complications in ASD surgery.
Pre-operative cognitive function
Numerous studies suggest that poor preoperative cognition may be a significant risk factor for post-operative delirium. The prevalence of poor preoperative cognition may be high, with Lee et al. finding 38% of patients undergoing lumbar spine surgery to meet diagnosis of cognitive impairment using a Mini-Mental State Exam (MMSE) [68]. In a study by Toombs et al. patients with preoperative dementia and psychotic disorders had more complications than controls in patients undergoing surgery for ASD [69]. Adogwa et al. noted cognitive impairment to be a risk factor for postoperative delirium and concluded that cognitive impairment assessments should be considered in the preoperative evaluation of elderly patients prior to surgery [70]. Although many studies discuss post-operative delirium as a common consequence of preoperative cognitive decline, longer-term outcomes are not conclusive and deserve further investigation.
Grade of Recommendation – I: There is insufficient evidence that pre-operative cognitive function is a risk factor for perioperative complications in ASD surgery.
Mental health
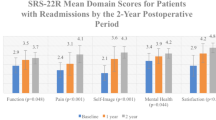
A likely non-causal association has been demonstrated between mental health factors and perioperative complications following surgery in ASD patients. The strongest evidence for this was provided by Shah et al. who noted that depression and anxiety were associated with increased rates of perioperative infection and respiratory complications following surgical correction of ASD after matching patients for sex, age, and Charlson Comorbidity Index (CCI) [71]. While Soroceanu et al. also found an increased rate of medical complications for patients with depression on univariate analysis (RR = 1.6, p = 0.0001), the result did not hold on multivariate analysis [13]. Using the SRS-22r, Watanabe et al. showed that unfavorable mental health scores were associated with perioperative infection, hematoma, DVT, and delirium [72]. These results did not control for potential confounding variables, including comorbidities or preoperative disability, which were greater in patients with worse mental health. Similarly, a NIS analysis performed by Toombs et al. showed increased rates of major complications in the perioperative period for patients with psychotic disorders, but the study also failed to control for potential confounding factors [69]. Finally, many clinical studies have failed to find any relationship between perioperative complications following ASD surgery using metrics such as a preoperative diagnosis of depression, Koenig Depression Scale (KDS), and quantitative scale of psychiatric distress [73,74,75]. Therefore, the most available literature is inconclusive and fails to control for other confounding factors present in patients with mental health illnesses.
Grade of Recommendation – I: There is insufficient evidence that mental health is a risk factor for perioperative complications in ASD surgery.
Social support
Social support is the presence of people and community institutions that can provide supportive behaviors and interventions to help reduce the stress and burden associated with major life events. There is a paucity of data published regarding the impact of social support on outcomes in patients undergoing surgery for ASD. Literature in cardiac surgery and orthopaedic surgery suggest social support may be an important predictive factor of surgical outcomes [76]. For example, Adogwa et al. found that one year after surgery, single patients were observed to have a longer length of stay compared to married patients in 430 patients who underwent elective spine surgery [77]. However, no differences in complications, 30-day readmissions, or patient-reported outcomes were found. To date there have not been any studies evaluating social support in the ASD population, which may be a consequence of the inability to effectively assess social support in large-scale databases and registries [8].
Grade of Recommendation – I: There is insufficient evidence that poor social support is a risk factor for perioperative complications in ASD surgery.
Opioid utilization
There is sparse literature specifically addressing pre-operative opioid use and perioperative complications for ASD. A multicenter retrospective review by Raad et al. found daily preoperative narcotic use independently predicted prolonged hospital length of stay and longer ICU stay [78]. One single-center review by Mesfin et al. found no significant difference in major and minor complications between patients taking opioids and those taking non-opioid analgesics preoperatively [79]. Elsamadicy et al. also found no significant difference in complications between preoperative narcotic users and non-narcotic users for patients receiving five or more level fusion for ASD [80]. Other potentially relevant variables for risk of perioperative complications, such as duration or dosage of opioid utilization, have yet to be assessed.
Grade of Recommendation – I: There is insufficient evidence that preoperative opioid use is a risk factor for perioperative complications in ASD surgery.
Discussion
Table 1 summarizes that patient frailty had the highest grade of evidence for perioperative complications. There is also fair evidence for bone quality, smoking, high blood sugar & diabetes, nutritional status, immunosuppression/steroid use, cardiovascular disease, pulmonary disease, and renal disease as independent risk factors for complications following operative management of ASD.
The strength of evidence for frailty’s association with complications has already been applied clinically. Numerous applications currently utilize frailty as a preoperative risk assessment tool to predict postoperative complications and death for elderly surgical patients outside of spine surgery [81, 82]. Frailty has been used to predict discharge time and mortality after laparoscopic colorectal and liver surgery, with higher scores predicting increases in complications, mortality, and extended length of hospital stay [83, 84]. Similarly, the ASD-FI, mFI, and mFI-5 have been utilized to predict complications in ASD surgery [32, 33]. It is possible that certain frailty indices perform better in predicting perioperative complications. As shown by Burn et al. frailty indexes are typically calculated by summing the number of functional deficits for a specific patient divided by the total number of possible deficits [85]. Those that utilize more deficits to facilitate the calculation could potentially yield better measures but also require greater resources to acquire. Additional studies comparing the predictive validity of different frailty indexes could produce information useful to inform preoperative guidance.
Variables assigned a Grade B: Fair Level of Evidence consisted of most literature supporting an association with perioperative complications, with some variation. For example, while the preponderance of literature suggests that impaired bone quality and bone metabolism compromise surgical outcomes, preoperative bone quality assessment can differ between males and females, and DEXA scans can be inaccurate depending on the scanned region [86, 87]. Future studies that control for patient gender and region of scanning would be of further benefit. A history of smoking, cardiovascular disease, and respiratory disease also presented fair evidence as risk factors for post-operative complications, accompanied by a minority that found conflicting results. Such studies, one being the case–control series by Schwab et al. that failed to find an association between cardiovascular disease and perioperative complications, had less than 10% of patients with complications, citing a necessity for improved matching of additional risk factors [63].
Moreover, smoking, cardiovascular disease, and respiratory disease may predispose patients to long-term complications that are not captured by most available reports. For example, certain studies report that smoking cessation before spinal surgery may improve short-term clinical outcomes, while others report smoking as an independent risk factor for longer-term complications (implant failure, pseudoarthrosis, revisions) [41, 88]. Preoperative pulmonary disease had similar associations with longer-term complications (reoperation) and short-term complications (respiratory failure, prolonged mechanical ventilation) [61]. A single study may be unable to capture the immediate and long-term complications due to certain risk factors, but the literature suggests a trend that such risk factors are indeed associated with either short-term of long-term post-operative complications.
Patient management of risk factors is also an important consideration. For example, it has been generally accepted that uncontrolled high blood sugar predisposes patients to increased cardiovascular, infectious, and additional pathophysiologic diseases [89,90,91]. The studies found in this literature search tended to establish uncontrolled diabetes as an independent risk factor for complications and mortality, while the risks from controlled diabetes ranged from having no association to significant ones with increased infection risk and length of stay. Uncontrolled and controlled diabetes may have different risk profiles, and two patients presenting with diabetes might be predisposed to different complications depending on the disease management. In addition, blood sugar level and diabetes should not be interpreted as binary variables such as “high blood sugar”, “low blood sugar”, “diabetic”, or “not diabetic” when evaluating patients for risk factors. Two of the studies referenced found that doubling blood glucose measurements and increasing daily glucose variation were significant predictors of surgical infections [47, 48]. Measurement of Hemoglobin A1c may present a better method to evaluate the effects of blood sugar on perioperative complications, but few studies have done so in the setting of ASD surgery. In a similar line, the association between renal disease and complications was found to be well-outlined, especially for patients with end-stage renal disease who are dependent on dialysis. However, few studies determined perioperative complications for patients earlier in the disease (i.e. CKD stage 1–3). Future reports on comparisons between patients with preserved eGFR in early-stage CKD and those on dialysis or late-stage CKD could provide additional recommendations.
Few studies discussed the relationship between nutritional status and perioperative complications in ASD surgery. Nevertheless, the fact that low albumin has been associated with infections, vascular complications, and organ dysfunction is in concordance with immune dysregulation from malnutrition [92]. Utilizing prealbumin may be a more accurate biomarker than albumin for nutritional status, given prealbumin’s shorter half-life and reflection of the patient’s most recent nutritional state [93].
The effect of steroid usage on perioperative complications makes intuitive sense but requires additional inquiry. Steroid usage was reported to be significantly associated with perioperative complications in the referenced studies. Large-database studies (> 500,000 patients) reported significantly increased risks of superficial surgical site infections (SSI), deep SSIs, and mortality (4x) with steroid use [94]. Yet, few studies distinguished between complication rates based on the type of steroids and between those who were chronic or intermittent users. Variations in steroid dose may also contribute to complications, as dose can correspond to different levels of immunosuppressive effects [95]. Overall, the literature is convincing that immune dysregulation secondary to steroid use and malnutrition is associated with perioperative surgical complications.
Insufficient evidence was available to link the following variables to complications following ASD operations: obesity, mental health, social support, cognitive function, and opiate use. For risk factors that had significant relationships to complications, such studies failed to control for potential other risk factors. Such variables, however, may still be associated with other predictors of perioperative complications. For example, while obesity, mental health, and social support had insufficient evidence, all three variables are implicated as independent risk factors for cardiovascular disease and can occupy a spectrum that produces varying effects on perioperative complications [96,97,98]. Obesity is typically categorized into Class I (30 < BMI < 35), Class II (35 < BMI < 40), and Class III (BMI > 40), and the rate of complications may increase with a higher class of obesity [99]. A retrospective clinical study conducted by Yokoo et al. determined that BMI > 30 was a risk for blood transfusions, while BMI > 35 increased the risks for unplanned intubation and cardiac events [100]. Clearly, risk profiles can change and become more pronounced with a higher extent of disease. As such, many clinicians use the variables having insufficient evidence for preoperative assessment. For example, Keller et al. showed that patients afflicted with obesity can necessitate adjustments to equipment, altered medication delivery, increased cardiac monitoring, and additional focus on oxygenation and wound healing [99]. A possible reason that certain risk factors had insufficient evidence is that most studies did not stratify BMI, mental health, and social support into sufficient ranges.
The results found by this review should inform the risk factors that should be taken into consideration during the preoperative management of patients undergoing ASD surgery. With knowledge of patient frailty, in conjunction with factors that have fair evidence of risk (cardiovascular, renal, and pulmonary diseases), clinicians may facilitate better-shared decision-making ability regarding the appropriateness of surgery and expected outcomes. Risk factors may be modified to optimize patient health prior to surgery and reduce the chance of complications. Standard Work protocols incorporating modifiable risk factors for deformity patients have been suggested by Burton et al. and Sethi et al. in extensive meta-analysis [101, 102]. Finally, knowledge of risk factors that contribute to complications may help set patient expectations preoperatively.
Applications of Pre-operative medical assessment in quality assessment
The ability of clinicians to stratify patient risk is important for the setting of benchmarks on expected complications [103]. Patients with higher frailty index scores, more medical comorbidities, and greater surgical invasiveness may be more likely to incur complications than those without underlying risk factors. While higher complication rates in the former groups may be expected, equivalent complication rates in the latter group may represent gaps in care. It was vital to understand whether those who incur a complication are high-risk or low-risk. Patients with greater medical comorbidities would have a higher expected benchmark for complications, while patients with fewer risk factors would have a lower expected benchmark. Therefore, the assessment of postoperative outcomes in ASD patients without evaluation of individual patient risk profiles could result in incorrect assumptions about quality of care received.
Limitations
One key limitation was the limited granularity of data available in the literature that could enable the stratification of patients based on specific diagnosis and surgical procedures. In most studies, cohorts consisted of patients with a variety of spinal deformities, with little distinction between types of deformity. Depending on the diagnosis, a different set of risk factors could be less or more predictive of post-operative complications. Due to limitations in both quality and volume of studies pertaining to ASD complications, it was difficult to obtain studies that could unanimously focus on patients with a singular set of ASD diagnosis, procedures, or surgical approaches. While the risk factors assigned a grading of good and fair evidence in this review may be applicable broadly to ASD patients, the applicability may vary depending on the specific patient pathology.
Additionally, certain studies lacked a reliable sample size, some having so few patients with complications that an adequate determination of the association could not be made. Others failed to control for the patients’ full risk profiles. Most importantly, for certain risk factors, including social support and opioid utilization prior to surgery, a limited number of studies discussed the association with complications specifically for ASD patients. While social support and opioid utilization have been identified as risk factors for complications following cardiovascular and shoulder surgery, extrapolating such relationships to ASD is difficult and future studies are needed [104, 105].
Finally, a variety of studies discussed risk factors in the context of long-term complications, such as reoperation and revision surgery [38, 106]. However, such studies may have underestimated complication rates by failing to utilize an appreciable window of time between a patient’s primary surgery and reoperation. As reported by Ahmed et al., revisions for scoliosis can continue past 2-years after the index operation, with a 5-year survivorship of 93.9% [107]. Complications and associated preoperative risk factors are likely underreported in studies with only 2 years of follow-up.
Future directions
Future research focusing on risk factors deemed to have an insufficient level of evidence in association with postoperative complications is needed. Upcoming studies should stratify patients by diagnosis, procedure, and procedural approach (ex. staging, anterior, posterior) in efforts to control for confounding operative variables and focus on preoperative risk factors. Additionally, risk factors that include social support have shown good promise in predicting outcomes following surgery, and future studies could utilize questionnaires [i.e. Risk Assessment and Prediction Tool (RAPT) score] that factor in metrics of community support and in-home assistance [108]. Complications should be classified as peri-operatively, short-term (at 30 days, 90 days, and 1 year post-operatively), and long-term (at 5 years and beyond) to capture revisions, reoperations, and pseudoarthrosis. Classification systems such as the Clavien-Dindo system could divide complications into classes ranging from lower severity (requiring pharmacological intervention) to high severity (morbidity) [109]. The standardization of complications into discrete classes could allow for more comparative studies in the future.
Implications for the development of predictive models
The primary goal of this report was to identify preoperative risk factors that were associated with complications following surgery for ASD. The next step would be to develop predictive models that incorporate and appropriately weigh the pertinent risk factors identified in this study. So far, currently utilized indices and risk scores have variable predictive utility. Specifically, Ondeck et al. demonstrated that numerically tabulated mFI indices and CCI were as predictive of complications after posterior lumbar fusion surgery as the easily obtained demographics and American Society of Anesthesiology (ASA) score [110]. Deogaonkar et al. and Hartin et al. demonstrated that the Fusion Risk Score (FRS), comprised of weighted demographics, comorbidities, surgical approach, levels, and osteotomies, also had a significant association with postoperative medical complications [111, 112]. Evidently, existing risk scores including the mFI and FRS hold promise but require additional validation along with other components of the patient’s risk profile. Future work should ideally utilize machine learning develop to predictive models that incorporate the risk factors identified in this study along with validated risk indices. Development of machine learning models would require large cohorts of patients with granular information in efforts to derive data-driven tools. Such predictive tools would serve to streamline the risk assessment process and enable rapid generation of expected patient outcomes. The relative contribution of each component of the model could be optimized as more patient information becomes available.
Conclusion
Comprehensive preoperative medical assessment decision-making is an important process that involves weighing the risk and benefits of surgery for ASD. The goal of this state-of-the-art review was to summarize the level of evidence for proposed risk factors for perioperative complications following ASD surgery. The included publications were assessed for level of evidence, as previously described in clinical practice guidelines published by the North American Spine Society, and a summary statement was generated using information synthesized from a review of all publications pertaining to each particular risk factor. Of the risk factors identified, frailty had good evidence as an independent risk factor for perioperative complications, while smoking, hyperglycemia, nutritional status, renal disease, cardiovascular disease, pulmonary disease, bone quality, and immunosuppression/steroid use had a fair level of evidence. Insufficient evidence was yielded for obesity, mental health, cognitive function, social support, and opioid use. Overall, we recommend using patient frailty in conjunction with cardiovascular, renal, and pulmonary diseases along with other factors that have fair evidence of risk. Clinicians may utilize important risk factors identified in this study to conduct shared decision-making regarding the appropriateness of spine surgery, to set patient expectations, and to guide preoperative planning.
Data availability
The data used to support the findings of this study are available from the corresponding author upon request.
References
Bono CM, Watters WC 3rd, Heggeness MH et al (2009) An evidence-based clinical guideline for the use of antithrombotic therapies in spine surgery. Spine J 9(12):1046–1051. https://doi.org/10.1016/j.spinee.2009.09.005
Ames CP, Scheer JK, Lafage V et al (2016) Adult spinal deformity: epidemiology, health impact, evaluation, and management. Spine Deform 4(4):310–322. https://doi.org/10.1016/j.jspd.2015.12.009
Bernhardt M, Bridwell KH (1989) Segmental analysis of the sagittal plane alignment of the normal thoracic and lumbar spines and thoracolumbar junction. Spine 14(7):717–721
Berven S, Deviren V, Demir-Deviren S, Hu SS, Bradford DS (2003) Studies in the modified Scoliosis Research Society Outcomes Instrument in adults: validation, reliability, and discriminatory capacity. Spine 28(18):2164–2169
Pellise F, Vila-Casademunt A, Ferrer M et al (2015) Impact on health related quality of life of adult spinal deformity (ASD) compared with other chronic conditions. Eur Spine J 24(1):3–11. https://doi.org/10.1007/s00586-014-3542-1
Theis J, Gerdhem P, Abbott A (2015) Quality of life outcomes in surgically treated adult scoliosis patients: a systematic review. Eur Spine J 24(7):1343–1355. https://doi.org/10.1007/s00586-014-3593-3
Bess S, Line B, Fu KM et al (2016) The health impact of symptomatic adult spinal deformity: comparison of deformity types to united states population norms and chronic diseases. Spine 41(3):224–233
Safaee MM, Scheer JK, Ailon T et al (2018) Predictive Modeling of Length of Hospital Stay Following Adult Spinal Deformity Correction: Analysis of 653 Patients with an Accuracy of 75% within 2 Days. World neurosurg 115:E422–E427. https://doi.org/10.1016/j.wneu.2018.04.064
Campbell PG, Yadla S, Nasser R, Malone J, Maltenfort MG, Ratliff JK (2012) Patient comorbidity score predicting the incidence of perioperative complications: assessing the impact of comorbidities on complications in spine surgery. J Neurosurg Spine 16(1):37–43. https://doi.org/10.3171/2011.9.SPINE11283
Reis RC, de Oliveira MF, Rotta JM, Botelho RV (2015) Risk of complications in spine surgery: a prospective study. Open Orthop J 9:20–25. https://doi.org/10.2174/1874325001509010020
Lee MJ, Konodi MA, Cizik AM, Bransford RJ, Bellabarba C, Chapman JR (2012) Risk factors for medical complication after spine surgery: a multivariate analysis of 1,591 patients. Spine J 12(3):197–206. https://doi.org/10.1016/j.spinee.2011.11.008
Nasser R, Yadla S, Maltenfort MG et al (2010) Complications in spine surgery. J Neurosurg Spine 13(2):144–157. https://doi.org/10.3171/2010.3.SPINE09369
Soroceanu A, Burton DC, Oren JH et al (2016) Medical complications after adult spinal deformity surgery: incidence, risk factors, and clinical impact. Spine 41(22):1718–1723
Weiss HR, Goodall D (2008) Rate of complications in scoliosis surgery - a systematic review of the Pub Med literature. Scoliosis 3:9
Bridwell KH, Berven S, Edwards C, Glassman S, Hamill C, Schwab F (2007) The problems and limitations of applying evidence-based medicine to primary surgical treatment of adult spinal deformity. Spine 32(19 Suppl):S135–S139
McCarthy IM, Hostin RA, Ames CP et al (2014) Total hospital costs of surgical treatment for adult spinal deformity: an extended follow-up study. Spine J 14(10):2326–2333. https://doi.org/10.1016/j.spinee.2014.01.032
Berven SH, Kamper SJ, Germscheid NM et al (2018) An international consensus on the appropriate evaluation and treatment for adults with spinal deformity. Eur Spine J 27(3):585–596. https://doi.org/10.1007/s00586-017-5241-1
Ryu WHA, Platt A, O’Toole JE, Fontes R, Fessler RG (2021) Patient expectations of adult spinal deformity correction surgery. World Neurosurg 146:e931–e939. https://doi.org/10.1016/j.wneu.2020.11.035
Amin RM, Raad M, Jain A, Sandhu KP, Frank SM, Kebaish KM (2018) Increasing body mass index is associated with worse perioperative outcomes and higher costs in adult spinal deformity surgery. Spine 43(10):693–698
Brown AE, Alas H, Pierce KE et al (2020) Obesity negatively affects cost efficiency and outcomes following adult spinal deformity surgery. spine journal 20(4):512–518. https://doi.org/10.1016/j.spinee.2019.12.012
Elsamadicy AA, Camara-Quintana J, Kundishora AJ et al (2019) Reduced impact of obesity on short-term surgical outcomes, patient-reported pain scores, and 30-day readmission rates after complex spinal fusion (>= 7 levels) for adult deformity correction. World neurosurg 127:E108–E113. https://doi.org/10.1016/j.wneu.2019.02.165
Yagi M, King AB, Boachie-Adjei O (2012) Incidence, risk factors, and natural course of proximal junctional kyphosis: surgical outcomes review of adult idiopathic scoliosis Minimum 5 years of follow-up. Spine 37(17):1479–1489
Schmidt T, Ebert K, Rolvien T et al (2018) A retrospective analysis of bone mineral status in patients requiring spinal surgery. BMC Musculoskelet Disord 19(1):53–53. https://doi.org/10.1186/s12891-018-1970-5
Noh SH, Ha Y, Obeid I et al (2020) Modified global alignment and proportion scoring with body mass index and bone mineral density (GAPB) for improving predictions of mechanical complications after adult spinal deformity surgery. spine journal 20(5):776–784. https://doi.org/10.1016/j.spinee.2019.11.006
Yagi M, Fujita N, Tsuji O et al (2018) Low Bone-mineral density is a significant risk for proximal junctional failure after surgical correction of adult spinal deformity. Spine 43(7):485–491
Kuprys TK, Steinmetz LM, Fischer CR et al (2019) Preoperative assessment of bone quality in spine deformity surgery: correlation with clinical practice and published recommendations. Spine 44(12):E735–E741
Gupta A, Upadhyaya S, Patel A et al (2020) DEXA sensitivity analysis in patients with adult spinal deformity. The spine journal 20(2):174–180. https://doi.org/10.1016/j.spinee.2019.08.011
Morley JE, Vellas B, van Kan GA et al (2013) Frailty consensus: a call to action. J Am Med Dir Assoc 14(6):392–397. https://doi.org/10.1016/j.jamda.2013.03.022
Miller EK, Neuman BJ, Jain A et al (2017) An assessment of frailty as a tool for risk stratification in adult spinal deformity surgery. Neurosurg Focus 43(6):E3
Miller EK, Lenke LG, Neuman BJ et al (2018) External Validation of the Adult Spinal Deformity (ASD) Frailty Index (ASD-FI) in the Scoli-RISK-1 Patient Database. Spine 43(20):1426–1431
Miller EK, Vila-Casademunt A, Neuman BJ et al (2018) External validation of the adult spinal deformity (ASD) frailty index (ASD-FI). Eur Spine J 27(9):2331–2338. https://doi.org/10.1007/s00586-018-5575-3
Leven DM, Lee NJ, Kothari P et al (2016) Frailty index is a significant predictor of complications and mortality after surgery for adult spinal deformity. Spine 41(23):E1394–E1401
Yagi M, Michikawa T, Hosogane N et al (2019) The 5-Item modified frailty index is predictive of severe adverse events in patients undergoing surgery for adult spinal deformity. Spine 44(18):E1083–E1091
Yagi M, Michikawa T, Hosogane N et al (2019) Treatment for frailty does not improve complication rates in corrective surgery for adult spinal deformity. Spine 44(10):723–731
Zhang X-N, Sun X-Y, Hai Y, Meng X-L, Wang Y-S (2018) Incidence and risk factors for multiple medical complications in adult degenerative scoliosis long-level fusion. J Clin Neurosci 54:14–19. https://doi.org/10.1016/j.jocn.2018.04.070
Puvanesarajah V, Rao SS, Hassanzadeh H, Kebaish KM (2018) Determinants of perioperative transfusion risk in patients with adult spinal deformity. J Neurosurg Spine 28(4):429–435. https://doi.org/10.3171/2017.10.SPINE17884
Wilson JRF, Jiang F, Badhiwala JH et al (2020) The Effect of Tobacco Smoking on Adverse Events Following Adult Complex Deformity Surgery: Analysis of 270 Patients From the Prospective, Multicenter Scoli-RISK-1 Study. Spine 45(1):32–37
Mok JM, Cloyd JM, Bradford DS et al (2009) Reoperation after primary fusion for adult spinal deformity rate, reason, and timing. Spine 34(8):832–839
Inoue S, Khashan M, Fujimori T, Berven SH (2015) Analysis of mechanical failure associated with reoperation in spinal fusion to the sacrum in adult spinal deformity. J orthopaedic sci 20(4):609–616. https://doi.org/10.1007/s00776-015-0729-1
Wade SM, Fredericks DR, Elsenbeck MJ et al (2020) The Incidence, Risk Factors, and Complications Associated With Surgical Delay in Multilevel Fusion for Adult Spinal Deformity. Global spine j. 12:44–46
Elsamadicy AA, Adogwa O, Sergesketter A et al (2017) Reduced impact of smoking status on 30-day complication and readmission rates after elective spinal fusion (>= 3 levels) for adult spine deformity: a single institutional study of 839 patients. World neurosurg 107:233–238. https://doi.org/10.1016/J.WNEU.2017.07.174
Elsamadicy AA, Ren X, Kemeny H et al (2019) Independent associations with 30- and 90-day unplanned readmissions after elective lumbar spine surgery: a national trend analysis of 144 123 patients. Neurosurgery 84(3):758–767. https://doi.org/10.1093/neuros/nyy215
Rubel NC, Chung AS, Wong M et al (2019) 90-day readmission in elective primary lumbar spine surgery in the inpatient setting: a nationwide readmissions database sample analysis. Spine 44(14):E857–E864
Guzman JZ, Skovrlj B, Shin J et al (2014) The impact of diabetes mellitus on patients undergoing degenerative cervical spine surgery. Spine 39(20):1656–1665
Shuman WH, Neifert SN, Gal JS et al (2020) The Impact of Diabetes on Outcomes and Health Care Costs Following Anterior Cervical Discectomy and Fusion. Global spine j. 12:29–219
Caputo AM, Dobbertien RP, Ferranti JM, Brown CR, Michael KW, Richardson WJ (2013) Risk factors for infection after orthopaedic spine surgery at a high-volume institution. J Surg Orthop Adv Winter 22(4):295–298. https://doi.org/10.3113/jsoa.2013.0295
Pennington Z, Lubelski D, Westbroek EM, Ahmed AK, Passias PG, Sciubba DM (2020) Persistent postoperative hyperglycemia as a risk factor for operative treatment of deep wound infection after spine surgery. Neurosurgery 87(2):211–219. https://doi.org/10.1093/neuros/nyz405
Cross MB, Yi PH, Thomas CF, Garcia J, Della Valle CJ (2014) Evaluation of malnutrition in orthopaedic surgery. J Am Acad Orthop Surg 22(3):193–199. https://doi.org/10.5435/JAAOS-22-03-193
Khanna K, Yi PH, Sing DC, Geiger E, Metz LN (2018) Hypoalbuminemia is associated with septic revisions after primary surgery and postoperative infection after revision surgery. Spine 43(6):454–460
Phan K, Kim JS, Xu J et al (2018) Nutritional Insufficiency as a Predictor for Adverse Outcomes in Adult Spinal Deformity Surgery. Global spine j 8(2):164–171. https://doi.org/10.1177/2192568217708777
Schoenfeld AJMD, Carey PAMD, Cleveland AWMD, Bader JOP, Bono CMMD (2013) Patient factors, comorbidities, and surgical characteristics that increase mortality and complication risk after spinal arthrodesis: a prognostic study based on 5,887 patients. spine j 13(10):1171–1179. https://doi.org/10.1016/j.spinee.2013.02.071
Puvanesarajah V, Jain A, Kebaish K et al (2016) Poor Nutrition Status and Lumbar Spine Fusion Surgery in the Elderly: Readmissions, Complications, and Mortality. Spine 42(13):979–983
White SJW, Ranson WA, Cho B et al (2019) The effects of preoperative steroid therapy on perioperative morbidity and mortality after adult spinal deformity surgery. Spine deformity 7(5):779–787. https://doi.org/10.1016/j.jspd.2018.12.006
Di Capua J, Somani S, Kim JS et al (2017) Hospital-acquired conditions in adult spinal deformity surgery predictors for hospital-acquired conditions and other 30-day postoperative outcomes. Spine 42(8):595–602
Tang H, Zhu J, Ji F, Wang S, Xie Y, Fei H (2014) Risk factors for postoperative complication after spinal fusion and instrumentation in degenerative lumbar scoliosis patients. J Orthop Surg Res 9(1):15–15. https://doi.org/10.1186/1749-799X-9-15
Bernstein DN, Kurucan E, Menga EN, Molinari RW, Rubery PT, Mesfin A (2018) Comparison of adult spinal deformity patients with and without rheumatoid arthritis undergoing primary non-cervical spinal fusion surgery: a nationwide analysis of 52,818 patients. spine j 18(10):1861–1866. https://doi.org/10.1016/j.spinee.2018.03.020
Bovonratwet P, Bohl DD, Malpani R et al (2019) Cardiac complications related to spine surgery: timing, risk factors, and clinical effect. J Am Acad Orthop Surg 27(7):256–263. https://doi.org/10.5435/JAAOS-D-17-00650
Zhao C-M, Zhang Y, Yang S-D et al (2018) Risk factors for lower limb deep vein thrombosis in patients with single-level lumbar fusion: a prospective study of 710 cases. Clin applied thrombosis/hemostasis. 24:157S-162S
Guyot JP, Cizik A, Bransford R, Bellabarba C, Lee MJ (2010) Risk factors for cardiac complications after spine surgery. Evidence-based spine-care j 1(2):18–25. https://doi.org/10.1055/s-0028-1100910
Murgai R, D’Oro A, Heindel P et al (2018) Incidence of respiratory complications following lumbar spine surgery. Inter j spine surg 12(6):718–724. https://doi.org/10.14444/5090
Wu L, Zhang X-n, Wang Y-s, Liu Y-z, Hai Y (2019) Risk factors for pulmonary complications after posterior spinal instrumentation and fusion in the treatment of congenital scoliosis: a case-control study. BMC musculosk disord. 20(1):331–331
Zhang JG, Wang W, Qiu GX et al (2004) The correlation between preoperative pulmonary function and postoperative pulmonary complications in the surgical treatment of scoliosis. Zhonghua Wai Ke Za Zhi 42(21):1296–1298
Schwab FJ, Hawkinson N, Lafage V et al (2012) Risk factors for major peri-operative complications in adult spinal deformity surgery: a multi-center review of 953 consecutive patients. Eur Spine J 21(12):2603–2610. https://doi.org/10.1007/s00586-012-2370-4
Liang J, Qiu G, Shen J et al (2010) Predictive factors of postoperative pulmonary complications in scoliotic patients with moderate or severe pulmonary dysfunction. J Spinal Disord Tech 23(6):388–392. https://doi.org/10.1097/BSD.0b013e3181b55ff4
Bains RS, Kardile M, Mitsunaga L et al (2017) Does chronic kidney disease affect the mortality rate in patients undergoing spine surgery? J Clin Neurosci 43:208–213. https://doi.org/10.1016/j.jocn.2017.05.014
Adogwa O, Elsamadicy AA, Sergesketter A et al (2018) The impact of chronic kidney disease on postoperative outcomes in patients undergoing lumbar decompression and fusion. World neurosurg 110:E266–E270. https://doi.org/10.1016/j.wneu.2017.10.147
Chikuda H, Yasunaga H, Horiguchi H et al (2012) Mortality and morbidity in dialysis-dependent patients undergoing spinal surgery: analysis of a national administrative database in Japan. J Bone Joint Surg Am 94(5):433–438. https://doi.org/10.2106/JBJS.K.00183
Lee Y-S, Kim Y-B, Lee S-H, Park Y-S, Park S-W (2016) The Prevalence of Undiagnosed Presurgical Cognitive Impairment and Its Postsurgical Clinical Impact in Older Patients Undergoing Lumbar Spine Surgery. J Korean Neurosurg Soc 59(3):287–291. https://doi.org/10.3340/jkns.2016.59.3.287
Toombs CS, Paul JC, Lonner BS (2018) Psychosocial factors and surgical outcomes in adult spinal deformity: do dementia patients have more complications? Spine 43(15):1038–1043
Adogwa O, Elsamadicy AA, Vuong VD et al (2018) Association between baseline cognitive impairment and postoperative delirium in elderly patients undergoing surgery for adult spinal deformity. J Neurosurg Spine 28(1):103–108. https://doi.org/10.3171/2017.5.SPINE161244
Shah I, Wang C, Jain N, Formanek B, Buser Z, Wang JC (2019) Postoperative complications in adult spinal deformity patients with a mental illness undergoing reconstructive thoracic or thoracolumbar spine surgery. spine j 19(4):662–669. https://doi.org/10.1016/j.spinee.2018.10.003
Watanabe Y, Yoshida G, Hasegawa T et al (2020) Effect of perioperative mental status on health-related quality of life in patients with adult spinal deformities. Spine 45(2):E76–E82
Scheer JK, Smith JS, Schwab F et al (2017) Development of a preoperative predictive model for major complications following adult spinal deformity surgery. J Neurosurg Spine 26(6):736–743. https://doi.org/10.3171/2016.10.SPINE16197
Adogwa O, Elsamadicy AA, Sergesketter AR et al (2017) Relationship among koenig depression scale and postoperative outcomes, ambulation, and perception of pain in elderly patients (>= 65 years) undergoing elective spinal surgery for adult scoliosis. World neurosurg 107:471–476. https://doi.org/10.1016/j.wneu.2017.07.165
Sikora M, Nemani VM, Winnett RL et al (2020) Helping spine surgeons detect pre-surgical psychological distress in complex spine patients: an observational pilot study. Spine deformity 8(3):413–420. https://doi.org/10.1007/s43390-020-00057-w
Rosenberger PH, Jokl P, Ickovics J (2006) Psychosocial factors and surgical outcomes: An evidence-based literature review. J Am Acad Orthop Surg 14(7):397–405. https://doi.org/10.5435/00124635-200607000-00002
Adogwa O, Elsamadicy AA, Vuong VD et al (2017) Effect of social support and marital status on perceived surgical effectiveness and 30-day hospital readmission. Global spine j 7(8):774–779. https://doi.org/10.1177/2192568217696696
Raad M, Jain A, Neuman BJ et al (2018) Association of Patient-reported Narcotic Use with Short- and Long-term Outcomes After Adult Spinal Deformity Surgery: Multicenter Study of 425 Patients With 2-year Follow-up. Spine 43(19):1340–1346
Mesfin AMD, Lenke LGMD, Bridwell KHMD et al (2014) Does preoperative narcotic use adversely affect outcomes and complications after spinal deformity surgery? A comparison of nonnarcotic- with narcotic-using groups. The spine journal 14(12):2819–2825. https://doi.org/10.1016/j.spinee.2014.03.049
Elsamadicy AA, Drysdale N, Adil SM et al (2019) Association Between Preoperative Narcotic Use with Perioperative Complication Rates, Patient Reported Pain Scores, and Ambulatory Status After Complex Spinal Fusion (>= 5 Levels) for Adult Deformity Correction. World neurosurgery 128:E231–E237. https://doi.org/10.1016/j.wneu.2019.04.107
Amrock LG, Deiner S (2014) The implication of frailty on preoperative risk assessment. Curr Opin Anaesthesiol 27(3):330–335. https://doi.org/10.1097/ACO.0000000000000065
Farhat JS, Velanovich V, Falvo AJ et al (2012) Are the frail destined to fail? Frailty index as predictor of surgical morbidity and mortality in the elderly. j trauma acute care surg 72(6):1526–1531. https://doi.org/10.1097/TA.0b013e3182542fab
Louwers LMD, Schnickel GMD, Rubinfeld IMD (2016) Use of a simplified frailty index to predict Clavien 4 complications and mortality after hepatectomy: analysis of the National Surgical Quality Improvement Project database. Amer j surg 211(6):1071–1076. https://doi.org/10.1016/j.amjsurg.2015.09.015
Keller DS, Bankwitz B, Nobel T, Delaney CP (2014) Using frailty to predict who will fail early discharge after laparoscopic colorectal surgery with an established recovery pathway. Dis Colon Rectum 57(3):337–342. https://doi.org/10.1097/01.dcr.0000442661.76345.f5
Burn R, Hubbard RE, Scrase RJ et al (2018) A frailty index derived from a standardized comprehensive geriatric assessment predicts mortality and aged residential care admission. BMC Geriatr 18(1):319–319. https://doi.org/10.1186/s12877-018-1016-8
El Maghraoui A, Roux C (2008) DXA scanning in clinical practice. j Associat Phys 101(8):605–617. https://doi.org/10.1093/qjmed/hcn022
Naganathan V, Sambrook P (2003) Gender differences in volumetric bone density: a study of opposite-sex twins. Osteoporos Int 14(7):564–569. https://doi.org/10.1007/s00198-003-1422-3
Carlson BB, Burton DC, Jackson RS, Robinson S (2016) recidivism rates after smoking cessation before spinal fusion. Orthopedics 39(2):E318–E322. https://doi.org/10.3928/01477447-20160301-03
Navarro-Perez J, Orozco-Beltran D, Gil-Guillen V et al (2018) Mortality and cardiovascular disease burden of uncontrolled diabetes in a registry-based cohort: the ESCARVAL-risk study. BMC Cardiovasc Disord 18(1):180–180. https://doi.org/10.1186/s12872-018-0914-1
Archuleta S, Gharamti AA, Sillau S et al (2021) Increased mortality associated with uncontrolled diabetes mellitus in patients with pulmonary cryptococcosis: a single US cohort study. Therap adv infect dis 8:204993612110043. https://doi.org/10.1177/20499361211004367
Deshpande AD, Harris-Hayes M, Schootman M (2008) Epidemiology of Diabetes and Diabetes-Related Complications. Phys Ther 88(11):1254–1264. https://doi.org/10.2522/ptj.20080020
Bourke CD, Berkley JA, Prendergast AJ (2016) Immune dysfunction as a cause one consecuence of malnutrition. Trends Immunol 37(6):386–398. https://doi.org/10.1016/j.it.2016.04.003
Keller U (2019) Nutritional laboratory markers in malnutrition. J Clin Med 8(6):775. https://doi.org/10.3390/jcm8060775
Ismael HMD, Horst MMD, Farooq MMD, Jordon JMS, Patton JHMD, Rubinfeld ISMD (2011) Adverse effects of preoperative steroid use on surgical outcomes. Amer j surg 201(3):305–309. https://doi.org/10.1016/j.amjsurg.2010.09.018
Coutinho AE, Chapman KE (2011) The anti-inflammatory and immunosuppressive effects of glucocorticoids, recent developments and mechanistic insights. Mol Cell Endocrinol 335(1):2–13. https://doi.org/10.1016/j.mce.2010.04.005
Cercato C, Fonseca FA (2019) Cardiovascular risk and obesity. Diabetol Metab Syndr 11(1):74–74. https://doi.org/10.1186/s13098-019-0468-0
Chaddha A, Robinson EA, Kline-Rogers E, Alexandris-Souphis T, Rubenfire M (2016) Mental health and cardiovascular disease. Am J Med 129(11):1145–1148. https://doi.org/10.1016/j.amjmed.2016.05.018
Compare A, Zarbo C, Manzoni GM et al (2013) Social support, depression, and heart disease: a ten year literature review. Front Psychol 4:384. https://doi.org/10.3389/fpsyg.2013.00384
Keller C (1999) The obese patient as a surgical risk. Semin Perioper Nurs 8(3):109–117
Yokoo H, Miyata H, Konno H et al (2016) Models predicting the risks of six life-threatening morbidities and bile leakage in 14,970 hepatectomy patients registered in the national clinical database of Japan. Medicine (Baltimore) 95(49):e5466
Burton DC, Sethi RK, Wright AK et al (2019) The Role of Potentially Modifiable Factors in a Standard Work Protocol to Decrease Complications in Adult Spinal Deformity Surgery: A Systematic Review, Part 1. Spine Deform 7(5):669–683. https://doi.org/10.1016/j.jspd.2019.04.003
Sethi RK, Burton DC, Wright AK et al (2019) The Role of Potentially Modifiable Factors in a Standard Work Protocol to Decrease Complications in Adult Spinal Deformity Surgery: A Systematic Review, Part 2. Spine Deform 7(5):684–695. https://doi.org/10.1016/j.jspd.2019.03.001
Spence RT, Mueller JL, Chang DC (2016) A Novel Approach to Global Benchmarking of Risk-Adjusted Surgical Outcomes: Beyond Perioperative Mortality Rate. JAMA Surg 151(6):501–502. https://doi.org/10.1001/jamasurg.2016.0091
Dewan KC, Dewan KS, Idrees JJ et al (2019) Trends and Outcomes of Cardiovascular Surgery in Patients With Opioid Use Disorders. JAMA Surg 154(3):232–240. https://doi.org/10.1001/jamasurg.2018.4608
Khazi ZM, Lu Y, Patel BH, Cancienne JM, Werner B, Forsythe B (2020) Risk factors for opioid use after total shoulder arthroplasty. J Shoulder Elbow Surg 29(2):235–243. https://doi.org/10.1016/j.jse.2019.06.020
Donnally CJ, Sheu JI, Bondar KJ et al (2019) Is There a Correlation Between Preoperative or Postoperative Vitamin D Levels with Pseudarthrosis, Hardware Failure, and Revisions After Lumbar Spine Fusion? World neurosurgery 130:E431–E437. https://doi.org/10.1016/j.wneu.2019.06.109
Ahmed SI, Bastrom TP, Yaszay B, Newton PO (2017) 5-Year Reoperation Risk and Causes for Revision After Idiopathic Scoliosis Surgery. Spine 42(13):999–1005
Glauser G, Piazza M, Berger I et al (2020) The Risk Assessment and Prediction Tool (RAPT) for Discharge Planning in a Posterior Lumbar Fusion Population. Neurosurgery 86(2):E140-e146. https://doi.org/10.1093/neuros/nyz419
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213. https://doi.org/10.1097/01.sla.0000133083.54934.ae
Ondeck NT, Bohl DD, Bovonratwet P et al (2018) Discriminative ability of commonly used indices to predict adverse outcomes after poster lumbar fusion: a comparison of demographics, ASA, the modified Charlson Comorbidity Index, and the modified Frailty Index. Spine J 18(1):44–52. https://doi.org/10.1016/j.spinee.2017.05.028
Deogaonkar K, Mehbod AA, Dawson JM, Transfeldt EE (2018) Validation of the fusion risk score for thoracic and lumbar spine fusion procedures. Clin Spine Surg 31(8):E413–E417. https://doi.org/10.1097/BSD.0000000000000686
Hartin NL, Mehbod AA, Joglekar SB, Transfeldt EE (2013) Fusion risk score: evaluating baseline risk in thoracic and lumbar fusion surgery. Spine 38(25):E1616–E1623
Funding
No funds or financial support were used in support of this study.
Author information
Authors and Affiliations
Contributions
Made substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data; or the creation of new software used in the work AA, DDC, AW, JM, RS, IMN, AAT, PVM, SB. Drafted the work or revised it critically for important intellectual content AA, DDC, AW, JM, RS, IMN, AAT, PVM, SB. Approved the version to be published AA, DDC, AW, JM, RS, IMN, AAT, PVM, SB. Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved AA, DDC, AW, JM, RS, IMN, AAT, PVM, SB.
Corresponding author
Ethics declarations
Conflict of interest
The authors report no study-specific conflict of interest-associated biases in relation to this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Arora, A., Cummins, D.D., Wague, A. et al. Preoperative medical assessment for adult spinal deformity surgery: a state-of-the-art review. Spine Deform 11, 773–785 (2023). https://doi.org/10.1007/s43390-023-00654-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-023-00654-5