Abstract
Purpose
To compare radiographic parameters, and functional and surgical outcomes between lumbar adolescent idiopathic scoliosis (AIS) and lumbar adult idiopathic scoliosis (AdIS).
Methods
A retrospective study was performed to identify Lenke 5c type AIS and AdIS patients from our scoliosis database who had undergone posterior surgical treatment for scoliosis. Preoperative and postoperative radiographic and clinical outcomes were compared between the two groups.
Results
A total of 22 patients were included in AdIS group, and 44 matched patients in AIS group. AdIS group had significantly larger L3 and L4 tilt and translation than AIS group (P < 0.05). AdIS group had larger T10-L2 angle and smaller T5–T12 angle (P < 0.05). AdIS group had higher VAS scores (P < 0.05) and pain domain of SRS-22 scores (P < 0.05) as compared to AIS group. Correlation analysis demonstrated positive relationship between VAS scores and T10-L2 angle (r = 0.492, P < 0.05). AdIS group was fused longer than AIS group (P < 0.05). Cobb angle of TL/L curve was larger and correction ratio was smaller at AdIS group (P < 0.05). AdIS group still had significantly larger L3 and L4 tilt and translation than AIS group (P < 0.05). CT measurements demonstrated larger postoperative vertebral body rotation at apical vertebrae and LIV at AdIS group (P < 0.05). Vertebral correction ratio was smaller at AdIS group (P < 0.05).
Conclusion
Lenke 5c AdIS patients had greater preoperative and postoperative L3 and L4 tilt and translation, as well as less correction of major curve and vertebral body derotation than AIS patients. However, the incidence of adding-on was similar between the two groups.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adolescent Idiopathic Scoliosis (AIS) is an abnormal curvature of the spine exceeding 10 degrees, diagnosed in adolescence and in which the etiology is unknown [1]. According to curve magnitude and maturity of the patients, the main treatment options for scoliosis include observation, bracing, and operation. For the curvature less than 25 degrees, patients can be observed on a 6- to 12-monthly basis with clinical and radiological follow-up [2]. For unmatured patients with curves between 25 and 45°, bracing should be considered [3]. Correction surgery is indicated to patients with curves beyond 45° [4]. However, curves in some patients continued to progress even after skeletal maturity, especially for those who had curves larger than 50° [5]. There are two main approaches to carry out the correction surgery, posterior and anterior, while posterior approach becomes the trend due to the safety and correction outcome. Although anterior surgery can save surgical segments, there are many vessels and organs anteriorly, which affects the safety of the surgery. In addition, back pain was more often seen in adult patients than in adolescent patients, which could be a reason for pursuing corrective surgery [5]. Several studies have compared surgical outcomes between AIS and adult idiopathic scoliosis (AdIS) [6,7,8]. However, most of the studies focused on patients with major thoracic curves (Lenke 1 or 2 types), and there was no study concerning patients with thoracolumbar or lumbar curves (Lenke 5 or 6 types). Different from that of thoracic vertebrae, the stress of lumbar vertebrae is greater and facet joint degeneration is more obvious for adult population [9]. In addition, the key to lumbar correction is vertebral body derotation. The intervertebral disc elasticity of adult scoliosis patients is worse than that of AIS patients, and the correction rates may be different [10]. Finally, the incidence of low back pain in patients with lumbar AdIS is higher than that in thoracic spine [11]. Whether corrective surgery can alleviate low back pain needs to be investigated. It remains to be studied whether corrective surgery for AdIS could achieve the similar radiological or life quality improvement as for AIS. With the increase of the age, intervertebral disc degeneration as well as muscle atrophy would make surgical strategy changed. This study limited the adult age group and curve magnitudes to make the groups comparable to make clear the influence of maturity other than degeneration on surgical strategy. The objectives of this study were to compare radiographic parameters, and functional and surgical outcomes between lumbar AIS and lumbar AdIS underwent posterior procedure to determine the suitable surgical time for idiopathic scoliosis.
Materials and methods
A retrospective study was performed to identify Lenke 5c type AIS and AdIS patients from our scoliosis database who had undergone posterior surgical treatment for scoliosis between May 2006 and September 2017. Inclusion criteria for the AdIS group consisted of age between 25 and 50 years, Cobb angles of the major curve ranging from 45 to 75°, single-stage posterior-only correction and fusion surgery, and at least 2 years of postoperative follow-up. Patients who had other skeletal deformities or had a history of spine surgery or incomplete radiographic data were excluded. From May 2006, posterior approach was the only surgical option to treat scoliosis and all pedicle screw system as well as derotation technique had become standard surgical strategy at our institute. A group of AIS patients aged between 10 and 18 years with complete radiographic, surgical data, and quality-of-life score were selected and were well matched to the AdIS group at a 2:1 ratio in terms of curve pattern, sex, Cobb angle of main curve (within 5°), and length of follow-up (within 6 months). Factors other than these were not considered in the matching process.
All patients in this study had at least 2 years of postoperative follow-up. Preoperative, postoperative, and the last follow-up standing posteroanterior full spine radiographs were acquired. Radiographic parameters were evaluated for coronal and sagittal spinal alignment combined with pelvic parameter: (1) curve angles of major thoracolumbar/lumbar curves and minor thoracic curves; (2) range of thoracolumbar/lumbar curve; (3). L3 and L4 translation: distance between CSVL and vertical line across midpoint of L3 or L4 vertebrae; (4) L3 and L4 tilt: the angle between the inferior endplate of L3 or L4 and the sacrum; (5) sagittal parameters included T5–T12 angle, T10-L2 angle, L1-S1 angle, and SVA; (6) pelvic parameters included pelvic tilt, sacral slope, and pelvic incidence; (7) correction ratio: preoperative Cobb angle–postoperative Cobb angle/preoperative Cobb angle. CT three-dimensional reconstruction was performed pre- and postoperatively. Vertebral body rotation was measured at apical vertebrae and lowest instrumented vertebrae: angle formed between a perpendicular line starting from the posterior central aspect of the spinal canal and a straight line through the posterior central aspect of the spinal canal and the middle of the vertebral body. Preoperative and last follow-up VAS scores and SRS-22 scores were acquired for all the patients. Surgical complications were also recorded. Adding-on was defined as a progressive increase in the number of vertebrae included within the distal curve, with an increase of horizontal translation of LIV + 1 by more than 5 mm.
Statistical analyses
Data were statistically analyzed using IBM SPSS Statistics 23.0 (SPSS Inc., Chicago, IL). Average values were reported as mean (SD). Summary statistics from the analyses of variance calculations were used to provide 95% confidence intervals for the error in measurements. Chi-square test was used in the comparison of the incidence of distal adding-on between the two groups. Independent sample t test was used in the comparison of the difference between the two groups as well as the difference between preoperative and final follow-up. Pearson correlation test was used to detect the correlation between radiographic parameters and VAS scores. The level of significance was set at P < 0.05.
Results
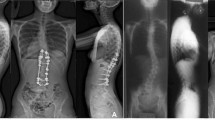
A total of 22 patients with an average age of 37.3 ± 8.7 years (range, 30–48 years) at the time of surgery were included in AdIS group, and 44 matched patients with an average age of 14.7 ± 3.2 years (range, 11–18 yr) at the time of surgery in AIS group. There was no difference between the two groups in terms of main thoracolumbar/lumbar Cobb angle (51.5 ± 6.4 vs. 49.2 ± 7.3°; p = 0.873), sex (p = 0.465), and curve patterns. LIV was at L3 for 8 patients, L4 for 11 patients, and L5 for 3 patients at AdIS group. At AIS group, LIV was at L3 for 28 patients and at L4 for 16 patients. AdIS group was fused longer than AIS group (7.8 ± 2.4 vs. 6.4 ± 1.6 levels; p < 0.05). In the regard of operation data, AdIS group had significant higher operation time (173.6 ± 32.8 vs. 234.2 ± 44.5 min; p < 0.001) and blood loss (578.3 ± 94.7 vs. 739.6 ± 127.3 ml; p < 0.001) than AIS group (Fig. 1).
As to coronal parameters, postoperative Cobb angle of TL/L curve was larger (17.4 ± 8.9 vs. 10.2 ± 7.2°; p = 0.009) and correction ratio was smaller (65.6 ± 15.7 vs. 79.1% ± 13.2%; p = 0.012) at AdIS group than AIS group. AdIS group had significantly larger preoperative L3 tilt (29.4 ± 6.4 vs. 21.7 ± 5.3°; p = 0.027), L4 tilt (23.7 ± 5.7 vs. 15.2 ± 4.6°; p = 0.017), L3 translation (33.4 ± 5.6 vs. 23.1 ± 4.2 mm; p = 0.012), and L4 translation (22.6 ± 5.7 vs. 14.9 ± 5.0 mm; p = 0.021) than AIS group. After the posterior correction surgery, AdIS group still had significantly larger L3 tilt (9.4 ± 4.1 vs. 4.2 ± 3.5°; p < 0.001), L4 tilt (7.2 ± 3.7 vs. 3.8 ± 3.2°; p < 0.001) and L3 translation (22.4 ± 4.3 VS. 15.2 ± 4.6 mm; p = 0.029), L4 translation (16.2 ± 3.9 vs. 11.4 ± 3.2 mm; p = 0.016) than AIS group at final follow-up.
AdIS group had larger preoperative T10-L2 angle (12.6 ± 7.2 vs. 3.2 ± 4.6°; p < 0.001) and smaller T5-T12 angle (18.5 ± 11.5 vs. 24.6 ± 13.3°; p = 0.024). There was no difference as to L1-S1 angle, pelvic tilt, sacral slope, and pelvic incidence (P > 0.05). After the surgery, sagittal parameters have been corrected to normal range and there was no difference as to T10-L2 angle, T5–T12 angle, L1-S1 angle, SVA, pelvic tilt, sacral slope, and pelvic incidence in AdIS and AIS group (P > 0.05) (Fig. 2).
An male patient aged 25 years with 60° left thoracolumbar curve (a, b), showing greater L3 and L4 translation and thoracolumbar kyphosis of 32°. After T10-L4 posterior correction surgery, thoracolumbar curve was corrected to 23°, and thoracolumbar kyphosis was corrected to 8° (c, d); 4 year postoperative radiographs did not show significant correction loss (e, f)
CT measurements demonstrated no difference of vertebral body rotation at apical vertebrae and lowest instrumented vertebrae preoperative (P > 0.05). However, after the derotation operation, AdIS group still had an extent of vertebral body rotation, while these in AIS group had been corrected to normal range. At last follow-up, the vertebral body rotation at apical vertebrae and lowest instrumented vertebrae were significant severe in the AdIS group (17.5 ± 4.2 vs. 10.4 ± 3.7°, p = 0.008 and 14.4 ± 3.4 vs. 9.6 ± 3.6°, p = 0.011).
AdIS group had higher preoperative VAS scores (3.2 ± 0.2 vs. 1.2 ± 0.1; P < 0.001) and higher pain scores of SRS-22 (3.2 ± 0.3 vs. 4.5 ± 0.2; P < 0.001) as compared to AIS group. And there were no significant difference in the rest of the SRS-22 domain (P > 0.05). Immediately after the surgery, six patients in AdIS and ten patients in AIS group reported worse pain, which were relieved at final follow-up. There was no difference of VAS scores and SRS-22 scores between the two groups at final follow-up (P > 0.05).
Correlation analysis demonstrated positive relationship between VAS scores and T10-L2 angle (r = 0.492, P < 0.05). There was no difference of correction loss of major curve between AdIS group and AIS group (2.7 VS. 3.1°, P > 0.05). Adding-on occurred at 5 patients at AdIS group and 9 at AIS group, and the rate of adding-on was similar between the two groups (P > 0.05) (Tables 1, 2 and 3).
Discussion
From classification aspects, AdIS belongs to adult spine deformity (ASD). ASD includes a broad spectrum of spine deformities, and the current classifications of ASD are mostly descriptive rather than decision-making guided [12]. Lenke classification may be the only one offering guidelines of surgical strategies for AIS [13]. Most surgeons refer to Lenke classification when making surgical strategies in the treatment of AdIS. However, AdIS was different from AIS in many aspects. First, AIS patients always seek correction surgery for psychosocial reasons or halting curve progression, while quite a number of AdIS patients receive surgery for the sake of curing back pain. Watanabe investigated the middle-aged patients with non-surgically treated AIS and compared the health-related quality-of-life (HRQOL) status of different curve types. He proposed that when compared patients with structural thoracolumbar/lumbar curves or patients with single main thoracic curve with the healthy controls, the patients with structural thoracolumbar/lumbar curves are more likely to experience greater annual TL/L curve progression and have substantial or worse low back pain-specific HRQOL status than the healthy controls, while patients with single thoracic curve showed no significant difference with the healthy controls [14]. Fekete investigated whether in patients with AIS and notable back pain surgery was associated with significant pain relief and whether age influences outcome, and found that in patients undergoing surgery for correction of AIS, back pain is correlated with age [15]. In our study, AdIS patients had significantly higher incidence and intensity of back pain than AIS patients with posterior approach. One of the origins of back pain could be thoracolumbar junctional kyphosis. We found significantly larger thoracolumbar junctional kyphosis in AdIS patients than in AIS patients. In addition, degrees of thoracolumbar junctional kyphosis were positively correlated to VAS scores in both AIS patients and AdIS patients. An interesting finding was that worsen pain was noted both in AdIS and AIS patients immediately after surgery; however, at last follow-up, pain was significantly reduced in both groups. Immediately worsen pain might be attributed to muscle stretching after scoliosis correction especially in concave side. Long-term follow-up demonstrated helpfulness of correction surgery for pain alleviation for scoliosis patients coinciding with Helenius’s finding that patients who underwent posterior spinal fusion with pedicle screws experienced improved back pain and health-related quality of life compared with patients with untreated AIS [16].
For Lenke 5c AIS, the choosing of touched vertebrae, neutral vertebrae, or stable vertebrae lacks in-depth discussion. We generally choose the most tilt vertebrae as lower end vertebrae. In the long-time follow-up, the effect of this principle is satisfying. Fusion strategy of Lenke 5c AIS adheres to the so-called “cobb-cobb” principle that fuses vertebrae from upper end vertebra to lower end vertebra [17]. However, the premise of using this principle lies in two aspects. First, lower end vertebra is not far from CSVL. Shu found that horizontalization of the LIV and minimizing LIV translation during correction could reduce the risk of distal adding-on [18]. In a meta-analysis, Yang evaluated the incidence, characteristics, and risk factors for "adding-on", and demonstrated that lowest instrumented vertebra (LIV)-center Sacral Vertical Line (CSVL) and deviation of LIV + 1 were found to be significantly associated with "adding-on" [19]. In the present study, AdIS group had greater preoperative L3 and L4 translation than AIS group. AdIS group had more patients instrumented to L4, even at L5. After operation, L3 and L4 translations were still greater in AdIS group. Second, lower end vertebra should be well derotated. Shu also demonstrated that derotation of the presumed LIV on SB films may hint less risk of distal adding-on in Lenke 5c patients [18]. In another word, well derotation could reduce the incidence of adding-on. CT scans showed both similar preoperative rotations of apical vertebra and LIV between the two groups with posterior approach. After operation, AdIS group achieved less derotation than AIS, which could be attributed to degeneration of facet joints and less elicitability of discs. Similarly, correction ratio was also better in AIS group. As has been stated, AdIS patients had significantly larger thoracolumbar junctional kyphosis than AIS patients, which was one of the treatment goals for AdIS. Postoperative radiographs demonstrated good correction of TJK in AdIS group, which was similar to AIS.
Unsurprisingly, AdIS group had longer fusion level, more operation time, and more blood loss than AIS group. AdIS patients always have severer facet joint degeneration, and releasing facet joint would cost more time and produce greater blood loss. In addition, longer fusion level and stronger muscle would also contribute to prolonged operation time and greater blood loss.
Incidence of adding-on was similar between the two groups. Shu reported an incidence of 18.8% of adding-on in Lenke 5c AIS patients [18]. Ilharreborde reported adding-on in 10.3% AIS patients, of which 62.5% had LIV above last touching vertebra. For most Lenke 5c patients, LIV was chosen at either L3 or L4 [20]. AdIS had more incidence of LIV at L4, which limited the room for developing adding-on. Furthermore, depletion of growth potential also permitted low chance of adding-on occurrence, as previous study had demonstrated positive correlation between growth potential and adding-on [21].
The disc degeneration in the distal mobile segments is an issue of concern and related to the back pain over time following surgery. According to the previous study, LIV to L4 had the highest risk of developing significant disc degeneration. Lonner proposed that avoid fusing to L4, maintain the LIV tilt below 5° and LIV translation less than 2 cm could decrease the incidence of disc degeneration [22]. In our study, though AdIS had more incidence of LIV at L4, the disc degeneration showed no significant difference between AdIS and AIS between two groups at final follow-up. The reason for this phenomenon could be insufficient follow-up time and studies with long follow-up time need to be carried out.
In conclusion, Lenke 5c AdIS patients had greater preoperative and postoperative L3 and L4 tilt and translation, as well as less correction of major curve and vertebral body derotation than AIS patients with posterior approach. However, the incidence of adding-on was similar between the two groups.
Data availability
All datasets generated or analyzed during this study are available from the corresponding author on reasonable request.
References
Cheng JC, Castelein RM, Chu WC et al (2015) Adolescent idiopathic scoliosis. Nat Rev Dis Primers 1:15030
Weinstein SL, Dolan LA, Cheng JC et al (2008) Adolescent idiopathic scoliosis. Lancet 371(9623):1527–1537
Negrini S, Minozzi S, Bettany-Saltikov J et al (2016) Braces for idiopathic scoliosis in adolescents. Spine (Phila Pa 1976) 41(23):1813–1825
Bettany-Saltikov J, Weiss HR, Chockalingam N et al (2015) Surgical versus non-surgical interventions in people with adolescent idiopathic scoliosis. Cochrane Database Syst Rev 4:CD010663
Erwin J, Carlson BB, Bunch J et al (2020) Impact of unoperated adolescent idiopathic scoliosis in adulthood: a 10-year analysis. Spine Deform 8(5):1009–1016
Lavelle W, Kurra S, Hu X, Lieberman I (2020) Clinical outcomes of idiopathic scoliosis surgery: is there a difference between young adult patients and adolescent patients? Cureus. 12(5):e8118
Zhu F, Bao H, Yan P et al (2017) Comparison of surgical outcome of adolescent idiopathic scoliosis and young adult idiopathic scoliosis: a match-pair analysis of 160 patients. Spine (Phila Pa 1976) 42(19):E1133–E1139
Charles YP, Ntilikina Y (2020) Scoliosis surgery in adulthood: what challenges for what outcome? Ann Transl Med 8(2):34
Takeda K, Kou I, Hosogane N et al (2019) Association of susceptibility genes for adolescent idiopathic scoliosis and intervertebral disc degeneration with adult spinal deformity. Spine (Phila Pa 1976) 44(23):1623–1629
Langlais T, Vergari C, Pietton R et al (2018) Shear-wave elastography can evaluate annulus fibrosus alteration in adolescent scoliosis. Eur Radiol 28(7):2830–2837
Jackson RP, Simmons EH, Stripinis D (1983) Incidence and severity of back pain in adult idiopathic scoliosis. Spine (Phila Pa 1976) 8(7):749–756
Schwab F, Ungar B, Blondel B et al (2012) Scoliosis Research Society-Schwab adult spinal deformity classification: a validation study. Spine (Phila Pa 1976) 37(12):1077–1082
Lenke LG, Betz RR, Harms J et al (2001) Adolescent idiopathic scoliosis: a new classification to determine extent of spinal arthrodesis. J Bone Joint Surg Am 83(8):1169–1181
Watanabe K, Ohashi M, Hirano T et al (2020) Health-related quality of life in nonoperated patients with adolescent idiopathic scoliosis in the middle years: a mean 25-year follow-up study. Spine (Phila Pa 1976) 45(2):E83–E89
Fekete TF, Mannion AF, Haschtmann D, Loibl M, Kleinstück FS, Jeszenszky DJ (2019) Back pain and its change after surgery in adolescents and young adults with idiopathic scoliosis. Spine Deform 7(5):754–758
Helenius L, Diarbakerli E, Grauers A et al (2019) Back pain and quality of life after surgical treatment for adolescent idiopathic scoliosis at 5-year follow-up: comparison with healthy controls and patients with untreated idiopathic scoliosis [published correction appears in J Bone Joint Surg Am. 2021 Feb 3;103(3):e13]. J Bone Joint Surg Am 101(16):1460–1466
Zhuang Q, Zhang J, Wang S, Yang Y, Lin G (2021) How to select the lowest instrumented vertebra in Lenke type 5 adolescent idiopathic scoliosis patients? Spine J 21(1):141–149
Shu S, Bao H, Zhang Y et al (2020) Selection of distal fusion level for Lenke 5 curve: does the rotation of the presumed lower instrumented vertebra matter? Spine (Phila Pa 1976) 45(12):E688–E693
Yang M, Zhao Y, Yin X et al (2018) Prevalence, risk factors, and characteristics of the “adding-on” phenomenon in idiopathic scoliosis after correction surgery: a systematic review and meta-analysis. Spine (Phila Pa 1976) 43(11):780–790
Ilharreborde B, Ferrero E, Angelliaume A et al (2017) Selective versus hyperselective posterior fusions in Lenke 5 adolescent idiopathic scoliosis: comparison of radiological and clinical outcomes. Eur Spine J 26(6):1739–1747
Qin X, Xia C, Xu L et al (2018) Natural history of postoperative adding-on in adolescent idiopathic scoliosis: what are the risk factors for progressive adding-on? Biomed Res Int 2018:1–8
Lonner BS, Ren Y, Upasani VV et al (2018) Disc degeneration in unfused caudal motion segments ten years following surgery for adolescent idiopathic scoliosis. Spine Deform 6(6):684–690
Funding
No financial or material support was obtained for this study.
Author information
Authors and Affiliations
Contributions
JQ, YQ, and ZZ made substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data; or the creation of new software used in the work. XP, BS, SL, and SM drafted the work or revised it critically for important intellectual content. JQ, ZZ, and YQ approved the version to be published. XP, JQ, ZL, BS, SM, SL, XS, ZZ, and YQ agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no financial or competing interests in relation to this work.
Ethical approval
The study protocol was established and approved by the Clinical Research Ethics Committee of Nanjing Drum Tower hospital. (2021-398-01).
Consent to participate
Written informed consent was obtained from patients.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pan, X., Qiao, J., Liu, Z. et al. Posterior-only correction surgery for idiopathic scoliosis Lenke type 5c: differences of strategies and outcomes between adult patients and adolescent patients. Spine Deform 11, 665–670 (2023). https://doi.org/10.1007/s43390-023-00647-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-023-00647-4