Abstract
With the decreasing proportion of blood donors to patients undergoing transfusion in Japan, optimal blood-product management is becoming increasingly important. Accordingly, we evaluate blood-product inventory management by means of mathematical optimization techniques. Using numerical analyses, we determine the effect of differences in the priority of collections on the units of discarded platelets, and demonstrate the impact of safety-stock levels upon these units. Our results suggest that policymakers should implement the following measures to minimize their disposal rates. Regional-block blood centers with significant fluctuations in demand must generate schedules that minimize both the units of platelets collected, and those interchanged to the maximal extent. Conversely, centers with smaller fluctuations in demand must generate schedules wherein a constant number of platelets is collected every day. Safety-stock levels should be revised in accordance with demands. Furthermore, our policy proposals should be able to mitigate social damage to the blood-supply chain over the course of the COVID-19 pandemic.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
A survey of blood transfusion statuses conducted in Tokyo in 2018 found approximately 86% of patients undergoing transfusion to be over 50 years of age [1]. By contrast, approximately 70% of blood donors are under 50 years of age; that is, younger generations are contributing to a high proportion of a life-saving medical treatment [2]. At present, most blood products (BPs) in Japan are used in life-saving medical treatments for older adults. Furthermore, the national increase in average life expectancy and low birth rate are expected to result in a rapidly aging population. If this trend continues, the proportion of blood donors to patients undergoing transfusion will decrease, and the aforementioned treatments will be seriously compromised. Considering these demographic patterns, maximizing the efficiency of BP usage will become increasingly important [3].
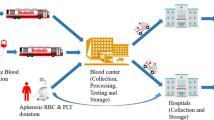
Blood supply operations are the services associated with the collection, processing, and supply of BPs to medical institutions for transfusion patients. The Japanese Red Cross Society (JRCS), an entity approved under the JRCS Act (an organization similar to a corporation), is responsible for blood supply operations throughout Japan. In the management of blood services, blood is collected from donors at donation rooms or bloodmobiles. The collected blood is then transported to one of the seven regional-block blood centers (BCs) distributed throughout the country, where it is screened and processed into BPs. In other words, the stock of a BP in each regional-block BC is replenished by BP processed at its BC from blood collected from donors in each region. Subsequently, the BPs are transported to prefecture-level BCs in the corresponding region. These BCs supply BPs to blood banks at hospitals [4].
Hospitals order specific types and quantities of BPs from the prefecture BCs as required. Two ordering methods are in place, for regular and emergency orders. Regular orders are placed according to stock status and the forecasted use of BPs for transfusion, surgery, and other purposes. Generally, a large-scale hospital places orders on a daily basis. According to the 2013 report by the Saitama Prefectural Joint Committee of Blood Transfusion Therapy, the annual number of emergency orders placed by each small-scale hospital with 19 or less beds is approximately 3.1, whereas that placed by each large-scale hospital with 500 or more beds is approximately 36.3. Conversely, emergency orders constitute a mere 10% of the total number of orders [5].
Schedules for blood collection are regulated by the JRCS. First, the JRCS forecasts demand for BPs for each regional-block BC based on the previous year’s demand. These forecasts are then used to compose annual blood collection schedules for the corresponding BCs. Although each BC is given access to its respective schedule, the JRCS does not publish its forecasted demands and blood collection schedules for public access.
Regional-block BCs in Japan were established in 2012 to provide a stable supply of BPs, and reduce stock bias in prefecture-level BCs. There are seven regional-block BCs: Hokkaido-block BC, Tohoku-block BC, Kanto-Koshinetsu-block BC, Tokai-Hokuriku-block BC, Kinki-block BC, Chugoku-Shikoku-block BC, and Kyushu-block BC; located in Hokkaido, Miyagi, Tokyo, Aichi, Ibaragi, Hiroshima, and Fukuoka, respectively. Each regional-block BC aims to satisfy the blood demands of hospitals in its respective region. Furthermore, BPs can be transferred among regional-block BCs according to their demand and stock. Thus, whenever one regional-block BC is limited in supply, BPs are imported from other BCs.
BPs include plasma, platelets, red blood cells, whole blood, and combinations of these products. Each BP has its own shelf life, and must be discarded past its expiration date. Consequently, the annual disposal rate of platelet BPs in Japan is high. Figure 1 illustrates the annual discarded BPs in units, as well as disposal rates of BPs, from 2007 to 2015. Note that this figure does not encompass whole blood units, as the disposal of these units is generally negligible. For example, only 7 units of whole BPs were discarded in 2015. Conversely, approximately 302,000 platelet units were discarded in 2007. Furthermore, 2013 saw the highest amount of plasma BPs discarded in the 9 years considered in the estimation. This may have been affected by changes in the inventory management system of BPs since 2012. In 2015, 171,675 plasma BPs were discarded, which is exceedingly high. To decrease the waste of BPs, determining the appropriate blood collection schedules that ensure that the amount of collected blood meets the demand is important.
However, demand forecasts significantly vary depending on whether the BPs are subject to inventory management by the hospitals or regional-block BCs. In the former case, not only will the demand for BPs remain uncertain, but the shortage, disposal, procurement, and miscellaneous costs will also highly depend on order quantity. As a result, it is important to account for the uncertainty, and establish an appropriate schedule to minimize the amount of stocks held. However, regional-block BCs need to hold a large amount of stocks to avoid shortages.
The present study is closely related to the field of operations research for health service literature. Since the publication of Van Zyl [6], various topics in the blood industry have been widely researched, and several review papers on the management of BPs have been published [7,8,9,10]. Studies related to the blood industry target individual hospitals, regional BCs, and supply chains. Topics of research include inventory management, blood collection schedules, supply chain management, and distribution scheduling. The methods used in these studies include various analytical methods, such as simulation, dynamic programming, and integer programming (IP). Many studies have analyzed supply chain schemes for BPs [11,12,13,14,15]. Most studies on inventory management focused on blood banks in hospitals [16,17,18,19,20]. Gunpinar and Centeno [16, 17] proposed IP models (deterministic and stochastic models) for inventory management at a hospital to minimize the purchase, waste, and insufficiency costs of BPs. Their stochastic model accounts for uncertainties in patient demand. The inventory management of platelets with a short shelf life has recently become more important [21]. Accordingly, Rajendran and Ravindran proposed a stochastic integer model to determine an ordering policy for a blood supply chain. The proposed model becomes computationally complex with an increase in the number of members of the supply chain; therefore, a variant of the genetic algorithm was proposed for larger problems [22]. Abbaspour et al. [23] attempted to develop a comprehensible method for medical workers, and employed Markov decision processes and simulations to optimize the blood supply chain. However, these models cannot be employed for inventory management of regional-block BCs, as the objective of inventory management in Japan is not to generate profits, but to minimize the units of discarded BPs upon securing an excessively high safety stock level. Dalalah et al. [24] built a simulation-optimization framework to minimize shortage and outdated BPs at hospitals. Our work is somewhat related to Dalalah et al. [24]. The principal difference is that the model of Dalalah et al. [24] does not incorporate the exchange among the regional-block BCs because they address blood inventory in a single hospital.
In this study, we evaluate the effects of the difference in priority of collections and interchanges on the units of discarded platelets through optimal inventory management at regional-block BCs. Additionally, we investigate the impact exerted on platelet disposal by the safety stock levels. The results of these analyses are contrasted with actual Japanese policies regarding BPs, and a discussion of potential future policies is conducted. We also discuss the impact of the pandemic on inventory management policies of platelets. The proposed model for Japanese regional-block BCs extends that developed by Gunpinar and Centeno [16, 17]. This model enables us to obtain an optimal inventory management schedule that minimizes the units of platelets collected and interchanged while maintaining stable supply.
The remainder of this paper is organized as follows: Sect. 2 introduces a method to estimate the daily demand for BPs, and the IP model for inventory management of BPs. Section 3 presents data for inventory management considering the transfer of individual BPs among regional-block BCs, and a numerical analysis of the proposed model. Section 4 discusses policy implications. Section 5 presents concluding remarks along with suggestions for future research.
2 Methods
The following section introduces the estimation formula for the daily demand of BPs, as well as the IP model for regional-block inventory management that collects and transfers the BPs appropriately. First, we propose a formula based on the yearly fluctuation ratio of BPs in regional-block BCs. Next, we present an IP model that minimizes the units of BPs collected and interchanged among regional-block BCs. Our model includes 14 constraints, including the first-in first-out of BPs, supply system on the shortage of a BP, and satisfaction of the minimum safety stock. We solved our model using an IP solver.
2.1 Estimating the Daily Demand for Blood Products
We define A as the set of years. B is defined as the set of regional-block BCs. To estimate the daily demand for BPs, the yearly fluctuation ratio \(r_{ab}\) of year a in regional-block BC b \((\forall a \in A, \forall b \in B)\) is calculated by
where \(D_{ab}\) is the demand for year a in an area of regional-block BC b \((\forall a \in A, \forall b \in B)\). We assume the daily demand \(d_{tb}\) for day t in regional-block BC b to be generated by
where \(\tilde{\xi }_{tb}\) is a random number that follows a normal distribution with mean \(\mu =\mathbb {E}[\sum _{a \in A}r_{ab}]\) and standard deviation, \(\sigma ^2=V[\sum _{a \in A} r_{ab}]\) of \(r_{ab}\), \(\forall b \in B\), i.e., \(\tilde{\xi }_{tb}\) \(\sim\) \(N(\mu , \sigma ^2), \forall b \in B\). Here, the estimation formula includes actual yearly demand, but not actual daily demand. When the actual daily demand is available, it is used to estimate \(\tilde{\xi }_{tb}\). Note that Eq. (2) technically may take a negative value, though the chance of this happening is quite small.
2.2 Integer Programming Model for Inventory Management of Blood Products
We propose an IP model for inventory management and schedule generation pertaining to blood collection and single BP distribution.
The inventory management of a regional-block BC differs from that of a hospital in three major ways. First, the objectives of inventory management in a hospital include both profit maximization and cost minimization. In contrast, the objective of inventory management at a regional-block BC is to minimize the units of discarded BPs. We note that this objective aims to provide a sufficient blood supply for the region, rather than being motivated by profit. Second, hospitals purchase BPs from prefecture-level BCs whenever their supply is limited. This is not the case for regional-block BCs. An insufficient supply of BPs is unacceptable, and safety stocks must be maintained at all times in every regional-block BC. Therefore, we include a constraint that stocks should be equal to or greater than the required level. Finally, hospitals must account for blood types when purchasing BPs, which is not necessary for regional-block BCs. Controlling the ratios of collected blood types for regional-block BCs is difficult as blood donation is voluntary.
We present the notations and constraints used throughout this study.
Notation
Index sets.
- K::
-
set of ages of collected blood (days after collection), \(\vert K \vert\) is shelf life in days.
- T::
-
set of days, \(\vert T \vert\) is scheduling period.
Parameters.
- \(UB_{tb}\) (\(t \in T, b \in B\))::
-
upper bound of units of a BP collected at a regional-block BC b at day t.
- \(d_{tb}\) (\(t \in T, b \in B\))::
-
BP demand in regional-block BC b at day t.
- \(S_b\) (\(b \in B\))::
-
safety stock level at regional-block BC b.
- \(L_{kb}\) (\(k \in K, b \in B\))::
-
initial stock of blood of age k at regional-block BC b.
- \(\alpha\)::
-
weighting factor.
Variables.
- \(m_{tkij}\) (\(t \in T, k \in K, i, j \in B\))::
-
units of a BP of age k transferred from regional-block BC i to regional-block BC j on day t.
- \(y_{tb}\) (\(t \in T, b \in B\))::
-
units of a BP collected at regional-block BC b on day t.
- \(z_{tkb}\) (\(t \in T, k \in K, b \in B\))::
-
1 if a BP of age k is used in regional-block BC b on day t; 0 otherwise.
- \(v_{tkb}\) (\(t \in T, k \in K, b \in B\))::
-
stock of a BP of age k in regional-block BC b on day t.
- \(n_{tkb}\) (\(t \in T, k \in K, b \in B\))::
-
units of an excess of age k in regional-block BC b to be used on day \(t+1\) if all available BPs of age k are not fully used to satisfy the demand on day t (supplementary variable).
Formulation
subject to
Due to the variability of BP use, directly controlling the units of discarded BPs is not possible. To control this quantity indirectly, managers at regional-block BCs determine target values for BP collection and exchange. The objective function (3) comprises two terms with weight parameters \(1-\alpha\) and \(\alpha\). The first term minimizes the units collected, whereas the second term minimizes the units exchanged among the regional-block BCs. The case of \(\alpha =0\) minimizes only the units collected; in other words, BPs continue to be actively transferred. Conversely, the case of \(\alpha =1\) minimizes only the units transferred; in other words, BPs continue to be actively collected. Constraint (4) ensures that the amount of BPs collected at each regional-block BC does not exceed the upper bound of daily blood collection \(UB_{tb}\). Blood collection is subject to resource constraints, such as the numbers of bloodmobiles, blood counters, and blood collectors. Furthermore, the maximum amount of blood collected in a day is fixed.
Constraint (5) ensured that older BPs are used first. Constraint (6) prohibits the use of BPs of age 1. This constraint is necessary any processed BPs should be tested before use. Constraint (7) ensures that whenever the usable stocks of a BP at the regional-block BC fail to meet demand, they are supplemented from other regional-block BCs. Constraint (8) requires the surplus of a regional-block BC to be greater than or equal to the units of a BP transferred to other regional-block BCs. In constraint (9), variables \(z_{tkb}\), \(n_{tkb}\) and \(\sum _{i \in B}m_{tkib}\) are determined from BP demand \(d_{tb}\), which is equal to the difference between the usable stock \(\sum _{k=2}^{E}v_{(t-1)(k-1)b}\) and units of excess \(n_{tkb}\), or the sum of the usable stock \(\sum _{k=2}^{E}v_{(t-1)(k-1)b}\) and units of a BP received \(\sum _{i \in B}m_{tkib}\). Constraint (10) sets the upper limit of \(n_{tkb}\). Constraint (11) defines the initial number of stocks. Constraint (12) states that the units of collected BPs are equal to the units of BPs of age 1. Constraint (13) defines the stock level. If BPs are not used on day t, the stock level does not change, as is the case for \(z_{tkb}=0\): \(v_{tkb}=v_{\left( t-1\right) \left( k-1\right) b}\). If BPs are used or exported to other regional-block BCs on day t, the stock level changes: \(v_{tkb}=\left( 1-z_{t\left( k-1\right) b}\right) \left( n_{tkb}-\sum _{j \in B}m_{tkbj}\right)\). Constraint (14) ensures that the stock level is at or above the safety stock level. Constraint (15) prohibits the transfer of BPs from a regional-block BC to itself. Constraint (16) is a binary constraint. Constraint (17) requires certain variables to be non-negative integers.
3 Numerical Analysis
3.1 Data
From Fig. 1, the disposal rate of platelet BPs is high. Accordingly, we focused on platelet BPs throughout our quantitative experiments. Platelet management is difficult due to the short shelf life of platelet BPs, as well as the challenge of maintaining an appropriate storage temperature [9]. We assumed the actual disposal date of platelet BPs to be \(\vert K \vert =4\) days, for a scheduling period \(\vert T \vert\) of 30 days. Safety stock levels \(S_b\) were assumed to be thrice the average daily forecasted demand, as is the current JRCS standard for safety stocks. Thus, the initial value of stock \(L_{kb}\) is 3 \(\times\) (average demand for a day)/(disposal date). The upper limit of daily blood collection \(UB_{tb}\) does not represent the numerical upper limit, i.e., 2 \(\times\) (average demand for a day). In other words, the value was set appropriately large to eliminate its impact on the solution. For our numerical experiments, the daily demand for platelet BPs was generated using the data from 2007 to 2015 [2] and Eqs. (1) and (2). We generated the parameters \(UB_{tb}\), \(d_{tb}\), \(S_b\) and \(L_{kb}\) on a 1/10 scale to reduce the number of calculations. Although the scaling reduces the number of significant digits by 1, the solution obtained is not different from that prior to scaling, proved in Appendix 2. Thus, the scaling is non-intrusive. Figure 2 illustrates the daily demand for platelet BPs at a regional-block BC \(d_{tb}\). The random number at each regional-block BC follows Hokkaido-block BC \(\tilde{\xi }_{t1}\) \(\sim\) \(N(0.020, 0.001)\), Tohoku-block BC \(\tilde{\xi }_{t2}\) \(\sim\) \(N(0.021, 0.001)\), Kanto-Koshinetsu-block BC \(\tilde{\xi }_{t3}\) \(\sim\) \(N(0.025, 0.000)\), Tokai-Hokuriku-block BC \(\tilde{\xi }_{t4}\) \(\sim\) \(N(0.003, 0.002)\), Kinki-Hokuriku-block BC \(\tilde{\xi }_{t5}\) \(\sim\) \(N(0.021, 0.001)\), Chugoku-Shikoku-block BC \(\tilde{\xi }_{t6}\) \(\sim\) \(N(0.022, 0.002)\) and Kyushu-block BC \(\tilde{\xi }_{t7}\) \(\sim\) \(N(0.024, 0.001)\), i.e., \(\vert B \vert =7\).
3.2 Results
The IP problem was solved using IBM ILOG CPLEX Optimization Studio version 12.6.3. We included some numerical examples for various weighting factors \(\alpha\) of the objective function that range from 0.1 to 0.9, to assess the effects of \(\alpha\) on the optimal solution. We compared the result of the Kanto-Koshinetsu-block BC with that of the Tokai-Hokuriku-block BC. Note that the two blocks exhibit the highest and lowest fluctuation ratios, respectively.
Figure 3 shows the objective function values under different values of \(\alpha\). The function exhibits a minimum at \(\alpha =0.9\), and a maximum at \(\alpha =0.1\). Therefore, for a certain BC, it is desirable to minimize exported units and maximize imported units.
Figure 4 shows the inventory levels of collected platelets at ages 1, 2, 3, and 4 at the Kanto-Koshinetsu-block BC. The number of stocks of platelets of age 1 in regional-block BC b on day t equals the amount of platelets collected in regional-block BC b on day t. As shown in the figure with the labels “\(\alpha =0.1 \& 0.2\)”, “\(\alpha =0.3 \& 0.4\)”, and “\(\alpha =0.7 \& 0.8 \& 0.9\)”, we found the corresponding inventory levels to be equivalent. The proposed formulation generates a schedule that minimizes the units of collected platelets with \(\alpha =0.1\) and \(\alpha =0.2\). The corresponding changes in inventory levels are large because platelets are collected to compensate for demand variations while minimizing the units of collected platelets. In contrast, the changes in inventory levels with \(\alpha =0.3\) are small. In the cases of \(\alpha =0.1\) and \(\alpha =0.2\), the Kanto-Koshinetsu-block BC collects platelets periodically. With regard to the numerical results obtained for the Tokai-Hokuriku-block BC, we found the inventory levels of collected platelets of ages 1, 2, and 3 to be identical for all values of \(\alpha\) (0.1, 0.2, ..., 0.9). Furthermore, no platelets of age 4 were present. From these results, we found inventory levels become less stable with an increase in fluctuation ratio. Figure 5 shows the monthly units of platelets discarded for different values of \(\alpha\). Here, values of \(\alpha =0.1\) and \(\alpha =0.2\) yield the highest amounts of discarded platelets. Conversely, the minimum amount of platelets was discarded for \(\alpha \ge 0.3\). Regional-block BCs must manage their collection of platelets to reduce disposal rates. The results of Figs. 4 and 5 are consistent with those obtained by Clay et al. [25], who found that the reduced fluctuation of inventory levels results in fewer discarded BPs. Figure 6 illustrates the relationship between the collection and exchange of platelets for different values of \(\alpha\). Note that there is a trade-off between the two quantities. For this purpose, regional-block BCs with high variability in demand should minimize both the collection and exchange of platelets. Conversely, regional-block BCs with low variability in demand should collect a specific amount of platelets every day.
Currently, the JRCS assumes safety stocks to be thrice the daily average forecasted demand. We varied the parameter \(S_b\) of safety stock from 2.5 to 3 to investigate its effects on platelet disposal. Figure 7 compares the units of discarded platelets with the monthly safety stocks of each regional-block BC. Here, we found the amount of discarded platelets for an \(S_b\) of 2.5 to be only 1/10 of that for an \(S_b\) of 3. Furthermore, the Kanto-Koshinetsu-block BC exhibited the highest decrease in platelet disposal. These results indicate that safety stock levels exert a significant impact on the amount of discarded platelets. Although these levels are currently fixed at 3 times, the average forecasted demand throughout Japan, by assuming a different value for each block, we demonstrated the possibility of reducing platelet disposal while ensuring safety.
4 Policy Implications and Discussion of COVID-19
The following section compares the results of the present analysis with actual Japanese policy on platelets, and discusses potential future policies. Furthermore, we discuss the impact of outbreaks, such as the COVID-19 pandemic, upon inventory management policies for platelets.
In the present analysis, the disposal rate of platelets was calculated by dividing the units of discarded platelets by the number supplied. This value was 0.0627 for \(\alpha =0.1\) and \(\alpha =0.2\); 0.0322 for \(\alpha =0.3\); and 0.0321 for \(\alpha =0.4\), \(\alpha =0.5\), \(\alpha =0.6\), \(\alpha =0.7\), \(\alpha =0.8\), and \(\alpha =0.9\). 115,671 units of platelets were discarded in Japan in 2015, amounting to an average of approximately 9,639 units per month. Meanwhile, 844,699 units were supplied in 2015, equating to an average of approximately 70,391 per month. The disposal rate for platelets, obtained by dividing the number of units discarded by the number supplied, was 0.139. For every value of \(\alpha\), the disposal rate for the results of the present analysis was smaller.
Based on the present analysis, we recommend policymakers to implement the following policies to minimize the platelet disposal rate.
-
Regional-block BCs that face large fluctuations in demand should not only minimize the units of collected platelets, but also generate inventory management schedules that minimize the units of platelets exchanged.
-
Regional-block BCs with small fluctuations in demand should generate blood-collection schedules wherein a constant amount of platelets is collected every day.
Safety stock levels should be revised. While all-block BCs currently employ a safety stock level thrice the national average of the forecasted demand, regional-block BCs must set different safety stock levels based on the results of the present analysis.
The COVID-19 pandemic has posed an unprecedented challenge for healthcare systems worldwide [26], including shortages of resources such as medical facilities, equipment, and BPs [27]. To resolve this issue, Amin [28] suggests that governments need to provide sufficient resources to healthcare professionals. The pandemic has also affected the inventory management policies of BPs. Because they have a shelf life of only 4 days, platelet BPs are particularly susceptible to shortages due to a decrease in blood donors. The appropriate management of safety stock is therefore important in a pandemic. In the state of Washington, United States, the amount of blood donors dropped significantly during the first week of the COVID-19 pandemic. BCs immediately began messaging news outlets, as well as public health and business leaders, regarding the safety and need for blood donations. They also informed hospitals regarding the current situation, and asked for the immediate implementation of shortage protocols, stringent blood transfusion criteria, and a review of blood transfusion. Consequently, hospitals began triaging blood transfusion, postponed elective surgeries, and prioritized BPs for urgent care. Thus, blood donation started to improve in the second week.
Similarly, in Japan, the amount of blood donors dropped with the suspension of bloodmobiles due to the cancellation of large-scale events and school closures, as well as the increased prevalence of telecommuting. The JRCS called on passersby to donate blood in Tokyo throughout March to maintain a stable supply of blood [2]. Similarly, during the 2009 H1N1 influenza, a virus pandemic, the amount of blood donors also saw a rapid decrease. This amount returned to a normal level in the second week, as e-mail and on-the-street campaigns were used to encourage blood donation [29]. Thus, large-scale disasters such as COVID-19 demand effective management and policies to regulate the blood supply; e.g., upstream and downstream integration of the supply chain.
Gehrie et al. [30] recommended encouraging people to visit blood donation centers that are still open for business, and working overtime to maintain a minimal blood inventory. The World Health Organization (WHO) provided interim guidance on the management of BPs in response to the COVID-19 pandemic [31], and suggested that blood donation numbers should be closely monitored to mitigate the reduced availability. This is particularly critical for platelet BPs, which have a short shelf life. Regarding inventory management policies, the WHO recommended BCs to continually assess their blood stocks in anticipation of uncertainties in the scale of collection. This implies that the quantitative-inventory scheduling and management approaches proposed in this paper are critical for the adequate assessment blood stocks.
During a pandemic, all regional-block BCs face large fluctuations in demand, and the units of platelets collected by and exchanged among BCs are reduced. We recommend policymakers to ensure that regional-block BCs facing large fluctuations in demand generate inventory management schedules that minimize the collection and exchange of platelets, thus minimizing platelet disposal rates. Such a policy could reduce fluctuations in the inventory and backlog (i.e., the bullwhip effect) in the supply chain. Thus, our proposed policy is expected to be particularly useful during pandemics. Large-scale disasters, such as the COVID-19 outbreak, may lead to insufficient health and human resources. However, the social damages and costs of these disasters can be minimized if policymakers implement our proposed policy during ordinary operations as well as disasters.
5 Conclusion
In this study, we evaluated inventory management policies of platelets through quantitative experiments. Using the numerical results, we analyzed the effects of the difference in priority between collections and exchanges, as well as varying safety stock levels, on platelet disposal.
We found that regional-block BCs that face large fluctuations in demand should not only consider minimizing platelet collection, but also generate inventory management schedules that minimize platelet exchange. By contrast, regional-block BCs with small fluctuations in demand should generate inventory management schedules wherein a constant amount of platelets is collected every day. Furthermore, we demonstrated the possibility of reducing platelet disposal while ensuring safety by allowing regional-block BCs to set different safety stock levels. We also discussed the relationship between our proposed model and the response to the COVID-19 pandemic. Our proposed policies are expected to mitigate damages and costs in the blood supply chain during pandemics. This also implies that additional policies and responses would not be required as long as the proposed policy is implemented during ordinary operations. We recommend the Japanese government to implement the aforementioned policies, thus minimizing the disposal rate of platelets.
In this study, we did not account for independent decisions made by hospitals; e.g., timing of the procurement and demand for platelets. Therefore, one objective of future research is to evaluate the inventory management schemes used in Japanese hospitals. Additionally, it may be interesting to examine uncertainties in supply and demand of platelets, along with actual demand, as mentioned in this paper.
References
A survey of blood transfusion status conducted in Tokyo in 2018 [Internet]. Tokyo: Bureau of social welfare and public health. https://www.fukushihoken.metro.tokyo.lg.jp/iryo/k_isyoku/yuketsutyousakekka.files/30gaiyo.pdf, Japanese. Accessed 30 Apr 2020
Japanese Red Cross fears blood shortage due to virus outbreak [Internet]. The Asahi Shimbun. http://www.asahi.com/ajw/articles/13199484. Accessed 23 Jun 2020
Fujiwara Y (2013) Data analysis of health care service focusing on acute care medicine. J Oper Res Soc Japan 58(11):651–656. Japanese
Current status and future of blood services [Internet]. Tokyo: Japanese red cross society. http://www.jrc.or.jp/activity/blood/about/future/, Japanese. Accessed 30 Apr 2020
2013 report by the Saitama prefectural joint committee of blood transfusion therapy [Internet]. Saitama: Saitama prefectural joint committee of blood transfusion therapy. https://www.saitama.bc.jrc.or.jp/godo/forum/6th-YF-bundle_file.pdf, Japanese. Accessed 30 Apr 2020
Van Zyl GJJ (1964) Inventory control for perishable commodities [dissertation]. University of North Carolina Chapel Hill at NC, North Carolina
Beliën J, Force H (2012) Supply chain management of blood products: a literature review. Eur J Oper Res 217(1):1–16
Janssen L, Claus T, Sauer J (2016) Literature review of deteriorating inventory models by key topics from 2012 to 2015. Int J Prod Econ 182:86–112
Pirabán A, Guerrero WJ, Labadie N (2019) Survey on blood supply chain management: models and methods. Comput Oper Res 112:104756
Prastacos GP (1984) Blood inventory management: an overview of theory and practice. Manage Sci 30(7):777–800
Blake JT, Hardy M (2014) A generic modelling framework to evaluate network blood management policies: the Canadian blood services experience. Oper Res Health Care 3(3):116–128
Dalalah D, Alkhaledi KA (2021) Optimization of red blood cell inventory: a blood-type compatibility-preference and emergency model. Int Trans Oper Res 30(1):239–272
Duan Q, Liao TW (2013) A new age-based replenishment policy for supply chain inventory optimization of highly perishable products. Int J Prod Econ 145(2):658–671
Duan Q, Liao TW (2014) Optimization of blood supply chain with shortened shelf lives and ABO compatibility. Int J Prod Econ 153:113–129
Pierskalla WP (2005) Supply chain management of blood banks. Oper Res Health Care 103–145
Gunpinar S, Centeno G (2015) Stochastic integer programming models for reducing wastages and shortages of blood products at hospitals. Comput Oper Res 54:129–141
Gunpinar S, Centeno G (2016) An integer programming approach to the bloodmobile routing problem. Transp Res Part E 86:94–115
Lowalekar H, Ravi RR (2017) Revolutionizing blood bank inventory management using the TOC thinking process: An Indian case study. Int J Prod Econ 186:89–122
Rajendran S, Ravindran AR (2017) Platelet ordering policies at hospitals using stochastic integer programming model and heuristic approaches to reduce wastage. Comput Ind Eng 110:151–164
Zhou D, Leung LC, Pierskalla WP (2011) Inventory management of platelets in hospitals: optimal inventory policy for perishable products with regular and optional expedited replenishments. Manuf Serv Oper Manag 13(4):420–438
Rajendran S, Srinivas S (2019) Hybrid ordering policies for platelet inventory management under demand uncertainty. IISE Trans Healthc Syst Eng 10(2):113–126
Rajendran S, Ravindran AR (2019) Inventory management of platelets along blood supply chain to minimize wastage and shortage. Comput Ind Eng 130:714–730
Abbaspour A, Jahan A, Rezaiee M (2021) A simple empirical model for blood platelet production and inventory management under uncertainty. J Ambient Intell Humaniz Comput 12:1783–1799
Dalalah D, Ojiako U, Chipulu M (2020) On perishable inventory in healthcare: random expiration dates and age discriminated demand. J Simul 16(5):1–22
Clay NM, Abbasi B, Eberhard A, Hearne J (2018) On the volatility of blood inventories. Int Trans Oper Res 25:215–242
Nicola M, Alsafi Z, Sohrabi C, Kerwan A, Al-Jabir A, Iosifidis C, Agha M, Agha R (2020) The socio-economic implications of the coronavirus pandemic (COVID-19): A review. Int J Surg 78:185–193
Islam MM, Rakhi NN, Islam OK, Saha O, Rahaman M (2020) Challenges to be considered to evaluate the COVID-19 preparedness and outcome in Bangladesh. Int J Healthc Manag. https://doi.org/10.1080/20479700.2020.1765120
Amin S (2020) The psychology of coronavirus fear: are healthcare professionals suffering from corona-phobia? Int J Healthc Manag. https://doi.org/10.1080/20479700.2020.1765119
Tsubokura M, Nakada H, Matsumura T, Kodama Y, Narimatsu H, Yamaguchi T, Kami M (2010) The impact of H1N1 influenza A virus pandemic on the blood donations in Hyogo Prefecture. Japan, Transfusion 50:1803–1805
Gehrie EA, Frank SM, Goobie SM (2020) Balancing supply and demand for blood during the COVID-19 pandemic. Anesthesiology 133:16–18
Maintaining a safe and adequate blood supply during the pandemic outbreak of coronavirus disease (COVID-19) [Internet]. World Health Organization. https://www.who.int/publications/i/item/maintaining-a-safe-and-adequate-blood-supply-during-the-pandemic-outbreak-of-coronavirus-disease-(covid-19). Accessed 7 Jul 2020
Funding
Open access funding provided by Kobe University. This work is supported by JSPS KAKENHI (Japan) Grant Number JP21K14371.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no conflicts of interest associated with this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix 1 Linearization of Integer Programming Formulation
Here, we describe the linearization of the nonlinear constraints in our optimization model.
Suppose we have a nonlinear expression \(z=x\times y\), where x is a binary variable and y is a non-negative continuous variable. Then, the nonlinear expression is equivalently expressed as the set of following three linear constraints:
where M is a sufficiently large number. Using this fact, we linearize the nonlinear constraints (9), (10), and (13). More particularly, we replace the product of the binary variable and other variables. \(v_{(t-1)(k-1)b}z_{tkb}\), \(v_{(t-1)(k-1)b}z_{t(k-1)b}\), \(z_{tkb} n_{tkb}\), \(z_{tkb}\sum _{j \in B}m_{tkbj}\), \(z_{t(k-1)b}n_{tkb}\) and \(z_{t(k-1)b}\sum _{j \in B}m_{tkbj}\) with their corresponding linearization variables. We transform constraints (9), (10), and (13) into linearized constraints using the following additional parameter and linearization variables.
Notation
Additional variables.
- \(\gamma _{tkb}\) (\(t \in T, k \in K, b \in B\))::
-
linearization variable for \(v_{(t-1)(k-1)b}z_{tkb}\).
- \(\mu _{t(k-1)b}\) (\(t \in T, k \in K, b \in B\))::
-
linearization variable for \(v_{(t-1)(k-1)b}z_{t(k-1)b}\).
- \(\lambda _{tkb}\) (\(t \in T, k \in K, b \in B\))::
-
linearization variable for \(z_{tkb}n_{tkb}\).
- \(\kappa _{tkb}\) (\(t \in T, k \in K, b \in B\))::
-
linearization variable for \(z_{tkb}\sum _{j \in B}m_{tkbj}\).
- \(\iota _{tkb}\) (\(t \in T, k \in K, b \in B\))::
-
linearization variable for \(z_{t(k-1)b}n_{tkb}\).
- \(\eta _{tkb}\) (\(t \in T, k \in K, b \in B\))::
-
linearization variable for \(z_{t(k-1)b}\sum _{j \in B}m_{tkbj}\).
Additional constraints.
subject to
In constraint (21), \(v_{(t-1)(k-1)b}z_{tkb}\) is replaced with \(\gamma _{tkb}\). In constraint (22), \(v_{(t-1)(k-1)b}z_{tkb}\) is replaced with \(\gamma _{tkb}\), and \(v_{(t-1)(k-1)b}z_{t(k-1)b}\) with \(\mu _{tkb}\). In constraint (23), \(v_{(t-1)(k-1)b}z_{tkb}\) with \(\gamma _{tkb}\), \(z_{tkb}n_{tkb}\) with \(\lambda _{tkb}\), \(z_{tkb}\sum _{j \in B}m_{tkbj}\) with \(\kappa _{tkb}\), \(z_{t(k-1)b}n_{tkb}\) with \(\iota _{tkb}\), and \(z_{t(k-1)b}\sum _{j \in B}m_{tkbj}\) with \(\eta _{tkb}\). The upper and lower bounds of the variables \(\gamma _{tkb}\), \(\mu _{t(k-1)b}\), \(\lambda _{tkb}\), \(\kappa _{tkb}\), \(\iota _{tkb}\), and \(\eta _{tkb}\) are governed by constraints (24)–(26), constraints (27)–(29), constraints (30)–(32), constraints (33)–(35), constraints (36)–(38), and constraints (39)–(41), respectively. Constraint (42) is used to set the upper bound of M. Constraint (43) requires certain variables to be non-negative integers. We then obtain a linear integer programming model (3)–(8), (11), (12), (14)–(17) and (21)–(43) for the inventory management and scheduling of BPs.
The upper bound of large number M can be determined from the relationship between \(v_{(t-1)(k-1)b}\), \(z_{tkb}\), and \(\sum _{j \in B}m_{tkbj}\). Formulation (13) is obtained as follows:
Using formulations (5) and (10), \(v_{tkb}=v_{(t-1)(k-1)b}\) when \(z_{tkb}=0 \wedge z_{t(k-1)b}=0\), \(\forall t, k, b\), and \(v_{tkb}=n_{tkb}-\sum _{j \in B}m_{tkbj}\) when \(z_{tkb}=1 \wedge z_{t(k-1)b}=0\), \(\forall t, k, b\), and \(v_{tkb}=0\) when \(z_{tkb}=1 \wedge z_{t(k-1)b}=1\), \(\forall t, k, b\).
The upper bound of \(v_{tkb}\) is either \(v_{(t-1)(k-1)b}\) or \(n_{tkb}- \sum _{j \in B}m_{tkbj}\). The magnitude of the relationship between \(v_{(t-1)(k-1)b}\) and \(n_{tkb}- \sum _{j \in B}m_{tkbj}\) is unclear. The rough upper bound is determined using the following formulation:
Using formulation (10), \(0 \ge n_{tkb}\) when \(z_{tkb}=0 \wedge z_{t(k-1)b}=0, \forall {t,k,b}\), and \(v_{(t-1)(k-1)b}\ge n_{tkb}\) when \(z_{tkb}=1 \wedge z_{t(k-1)b}=0, \forall {t,k,b}\), i.e., \(v_{(t-1)(k-1)b}\ge n_{tkb}\). From Table 1, the upper bound of \(v_{(t-1)(k-1)b}\) is \(L_{kb} \vee y_{tb}\). The upper bound of \(y_{tb}\) is \(UB_{tb}\) according to formulation (4). The upper bound \(UB_{tb}\) of \(y_{tb}\) is that of \(v_{(t-1)(k-1)b}\), that is,
Using formulation (6), the upper bound of \(\sum _{j \in B}m_{tkbj}\)
i.e.,
Therefore, the upper bound of \(v_{tkb}\) is \(v_{tkb} \le v_{(t-1)(k-1)b}+n_{tkb}-\sum _{j \in B}m_{tkbj}\),
The third term of the above formulation is \(-UB_{(t-1)b}\). There is no upper bound of \(v_{tkb}\) when the upper bound of \(\sum _{j \in B}m_{tkbj}\) is negative. Therefore, the third term of the above formulation is not considered here, that is, the upper bound of the rough is
Appendix 2 Scaling of Data
We improved the solver by changing to Gurobi Optimizer Ver. 9.5.2 to solve the problem for the original data, which was ten times the data in Section 3.1. The numerical analysis resulted in an objective function value of 15695, which is ten times the objective function value of 1/10 data. We confirmed the effectiveness of the scaling in the above numerical experiment.
Appendix 3 Units of Platelets Transferred and Received
Figure 8 shows the units of platelets transferred over 10 days at the Kanto-Koshinetsu-block BC for different values of \(\alpha\), \(m_{tk3j}\). From the results with \(\alpha =0.1 \& 0.2\), we know that 15 platelets were transferred from the Kanto-Koshinetsu-block BC to the Kinki-block BC. In the case of \(\alpha =0.4\), the Kanto-Koshinetsu-block BC transferred 1 platelet each to the Kinki-block BC and the Kyushu-block BC. In the case of \(\alpha =0.5\), the Kanto-Koshinetsu-block BC transferred 5 platelets to the Kyushu-block BC. In the cases of \(\alpha =0.6, 0.7, 0.8\), and 0.9, the Kanto-Koshinetsu-block BC satisfied their own stock. The Tokai-Hokuriku-block BC transferred 1 platelet each to the Kanto-Koshinetsu-block BC and the Tohoku-block BC. The Tokai-Hokuriku-block BC transferred 2 platelets each to the Kinki-block BC and the Kyushu-block BC.
Figure 9 shows the units of platelets received over 10 days at the Kanto-Koshinetsu-block BC for different values of \(\alpha\), \(m_{tki3}\). From the results with \(\alpha =0.1 \& 0.2\), we know that the highest numbers of platelets were received on days 15, 18, and 20. The Tokai-Hokuriku-block BC did not receive any platelets over the 10 days.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ito, M., Takashima, R. Evaluating Inventory Management Policies of Platelets at Regional-Block Blood Centers in Japan. Oper. Res. Forum 4, 57 (2023). https://doi.org/10.1007/s43069-023-00235-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s43069-023-00235-2