Abstract
Objective
The purpose of the present study was to investigate the association between cardiorespiratory fitness (CRF) measured as peak oxygen uptake (VO2peak, expressed in mL/min) and body mass index (BMI) in a large cohort of apparently healthy subjects.
Methods
BMI and VO2peak were measured in a cross-sectional study of 8470 apparently healthy adults. VO2peak (mL/min) was determined by an incremental cycle ergometer test to exhaustion. Linear regression analyses were performed to identify predictors of CRF.
Results
There was no difference in CRF between adults with a normal weight (BMI between 18.5–24.9 kg/m2) and those who were overweight (BMI 25.0–29.9 kg/m2). Subjects who were underweight (BMI < 18.5 kg/m2) as well as females who were obese (BMI ≥ 30.0 kg/m2) showed a reduced CRF compared to the normal and overweight groups. Age, height, and gender were significant predictors of CRF (R2 = 0.467, P < 0.0001); BMI did not add significantly to this relationship.
Conclusion
Our findings indicate that BMI was not associated with CRF in addition to age, height, and gender. In subjects with a BMI < 18.5 kg/m2, CRF was lower compared to subjects with a BMI between 18.5 and 29.9 kg/m2. In obese subjects, CRF was only lower in females compared to females with a BMI between 18.5 and 29.9 kg/m2. Correcting CRF for BMI may be beneficial for subjects with a low BMI, and females with a BMI ≥ 30.0 kg/m2. The outcome of this study might help to improve the interpretation of exercise testing results in individuals with a low or high BMI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cardiorespiratory fitness (CRF) plays an increasingly important role in treatment and prevention of diseases. A low level of CRF is associated with metabolic dysfunction [13, 23], cardiovascular disease [1], and an independent predictor for cardiovascular events [18]. In fact, individuals with a CRF rating in the lowest quartile of the general population are at a 2–5 times greater risk of all-cause mortality [14].
The gold standard for determining cardiorespiratory fitness is the measurement of peak oxygen uptake (VO2peak) during a maximal cardiopulmonary exercise test (CPET) [14, 25]. CRF is related to sex, age, anthropometric characteristics, and level of habitual physical activity [15, 24, 30]. According to guidelines for CPET, reference values regarding CRF should be adjusted for height, weight, or BMI [4].
Overweight or obese persons are often expected to have lower levels of CRF compared to normal weight peers because of deconditioning [3]. However, the literature is inconsistent in this regard. Some studies have indicated that individuals with an increased BMI have a normal CRF and others have suggested a lower CRF [9, 11, 20].
The excess body mass might be accompanied by an increased skeletal muscle mass [17], and increased cardiac stroke volume resulting from an expanded blood volume. However, obese subjects can develop left ventricular dysfunction, which might reduce the cardiac ejection fraction, thus might negatively affect the cardiac output in individuals with a high BMI [2]. In addition a smaller arterio-venous oxygen difference in the overweight and obese population impacts the oxygen transport negatively [28, 29].
Obesity and low cardiorespiratory fitness (CRF) have been shown to independently increase the risk of cardiovascular diseases (CVD) and mortality [8]. The relationship between BMI and CRF was investigated in male Indian [19], Finnish [25], Brazilian [6], and female Israeli [7] populations, and a negative association between BMI and CRF was found. However, CRF was expressed relative to body mass in the above-mentioned studies. This would result in an “artificially” lowered CRF because of the excessive body mass in subjects with a high BMI [16]. A high CRF per kilogram body mass is important for the performance of weight bearing physical activities. A high absolute CRF might be important for health purposes as well as for assessing change following an intervention.
In the current study we aim to investigate the relationship between BMI and CRF among a large group of apparently healthy subjects with a large range of BMI categories.
Methods
Study Design
This study was conducted using data from the Low-Lands Fitness Registry. This database contains currently cross-sectional “open source” exercise testing data from 11 centers, in the Netherlands and Belgium (Isala Hospital Zwolle, Diving Medical Center Den Helder, In2Motion Sports Bureau, Erasmus Medical Center Rotterdam, Ministry of Defense Testing Center, Soesterberg, University of Applied Science Utrecht, St Anna Hospital Geldrop, InspanningLoont Center Utrecht, Maxima Medical Center Veldhoven, Hospital Jan Portaels Vilvoorde, Radboud UMC Nijmegen). This study was approved by the Medical Ethics Committee of the UMC Utrecht, the Netherlands (Protocol 16/167).
Study Population
The study population comprised 6914 males and 1556 females in the age group of 18–94 years. Inclusion criteria were a minimum age of 18 years, apparently healthy subjects, and measurement of VO2peak that was performed on a bicycle ergometer.
Testing Protocol
Only CPETs performed on an electromagnetically braked cycle ergometer were used for this analysis. These ergometers came from distinctive manufacturers, including Lode BV, Groningen, the Netherlands and Ergoline, Bitz, Germany [22]. Individually adjusted step-wise incremental protocols to volitional exhaustion were employed, after the incremental phase a cooldown period was employed. The aim of the protocol was to exhaust the subjects within 8–12 min of exercise. Verbal encouragements were provided throughout the CPET. Tests were performed in a temperature-controlled room (20–23 °C). The VO2peak was defined as the highest amount of oxygen uptake during maximum effort of the CPET and was expressed in ml/min. Peak values were averaged over 30–60 s, based on the preference of the institution.
The VO2peak was measured with a calibrated respiratory gas-analysis system as described previously [21]. These systems were also from distinctive manufacturers, in particular from Cortex Metalyzer, Leipzig, Germany; Carefusion, Hoghberg, Germany; Geratherm, Bad Kissingen, Germany; Cosmed, Rome, Italy; and Medisoft, Sorrines, Belgium.
Measurements
In order to study the association between BMI and CRF, the following variables were used: VO2peak (in mL/min), Heart Rate (HR) and Respiratory Exchange Ratio (RER = VCO2/VO2), height, and weight. HR was measured using a standard exercise electrocardiogram (XECG).
Height and weight were measured with an accuracy of 1 cm and 0.1 kg, respectively. BMI was calculated as body weight divided by square of height (kg/m2). BMI was classified into four groups: (1) underweight < 18.5 kg/m2, (2) normal weight 18.5–24.9 kg/m2, (3) overweight 25.0–29.9 kg/m2, (4) obese ≥ 30.0 kg/m2.
All tests were performed at room temperature at sea level. Data were obtained by qualified and experienced health care providers.
Statistical Analysis
The baseline characteristics of the study population were calculated using descriptive statistics. One-way ANOVA test was performed to test differences in CRF between BMI categories. P-values adjustment for multiple post hoc tests was done using the Bonferroni method. Furthermore, a multiple linear regression analysis using the backward mode was carried out to study the relationship between age, gender, BMI, and VO2peak.
Statistical significance was defined as a P value < 0.05 (2 tailed). SPSS software (version 21.0) was used to perform all statistical analyses.
Results
Baseline characteristics of all study participants are presented in Table 1. In males, 50 subjects were classified as underweight (BMI < 18.5 kg/m2), 3745 subjects had a normal or healthy weight (BMI between 18.5 and 24.9 kg/m2), 2759 subjects were classified as overweight (BMI 25.0–29.9 kg/m2), and 360 male subjects were classified as obese (BMI ≥ 30.0 kg/m2). In females 27 subjects were classified as underweight (BMI < 18.5 kg/m2), 1024 subjects had a normal or healthy weight (BMI between 18.5 and 24.9 kg/m2), 378 subjects were classified as overweight (BMI between 25.0– 29.9 kg/m2), and 127 subjects were obese (BMI ≥ 30.0 kg/m2).
The CRF results are displayed in Table 2.
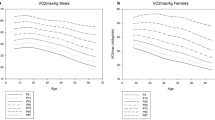
The differences between CRF in the BMI classes are shown in Fig. 1 for females and males (Males: ANOVA F = 29.87, df = 3.00, P < 0.0001; Females: ANOVA F = 17.329, df = 3.00, P < 0.0001). When BMI was between 18.5 kg/m2 and 29.9 kg/m2, no statistically significant differences in CRF were apparent between the BMI categories.
However, in males and females who are underweight (BMI < 18.5 kg/m2) or in females who are obese a statistically significantly lower VO2peak compared to their normal weight peers was observed (P < 0.0001, P = 0.0017, P= 0.0013, respectively). As expected, the VO2peak was lower in females compared in males with the same BMI status.
Table 3 presents the multivariable linear regression models for predicting VO2peak. Age was negatively associated with VO2peak, males had a higher VO2peak compared to females, and height was positively associated with VO2peak. BMI was excluded from the regression model since it did not add significantly to the explained variance next to age and gender (R2: 0.354); age, gender, and height (R2: 0.467); and age, gender, and BMI (R2: 0.365).
Discussion
The primary aim of this study was to determine the association of weight status expressed as BMI with CRF in a large cohort of apparently healthy subjects. Our findings indicated that CRF was negatively related in males and females who are underweight (BMI < 18.5 kg/m2). Further, there was a small difference in CRF between the normal weight, overweight, and obese male subjects, of which the difference between normal weight and overweight reached statistical significance.
In females the underweight and obese groups scored lower than the normal weight and overweight groups. This indicates that the CRF is independent of weight status, when BMI is between 18.5 and 29.9 kg/m2. CRF was only lower in obese females, but not in obese males. This gender difference might be related to the fact that our female subjects in the obese group were smaller and older compared to the normal weight group.
Care should be taken when CRF is interpreted in terms of VO2peak related to body mass. Our data found that CRF expressed in absolute values (mL/min) is independent of BMI in subjects with a BMI between 18.5 and 30.0 kg/m2. However, when CRF is divided by body mass in case of overweight or obesity, it will be “artificially” lowered because of the excess in fat mass. This finding was also reported in children by Goran et al., who observed that fat mass did not have any effect on VO2peak; however, they found that absolute VO2peak was significantly higher in obese children compared to lean children [10]. Moreover, Hansen et al. reported a higher than predicted absolute VO2peak in obese adult subjects [12].
We did not observe a higher VO2peak in our adult subjects who were overweight or obese. In their classic study Buskirk and Taylor stated that the presence of fat does not interfere with the maximal cardiovascular-respiratory performance of a subject [5]. This in also in accord with the results of our regression analysis. BMI did not add to the explained variance in the relation between VO2peak and age, gender and height.
Based on our findings, we recommend to express CRF in absolute values (mL/min or L/min), as well as in relative values (mL/kg/min) in persons who are overweight or obese. Males and females with a low BMI had a lower absolute VO2peak value compared to peers with a normal BMI. Females with a low BMI have comparable relative VO2peak values compared to females with a normal BMI. This can be (partially) explained by the fact that the females with a low BMI were taller than the females with a normal BMI.
However, males with a low BMI have higher relative VO2peak values compared to peers with a normal BMI. The latter is described as the “fallacy of the per weight ratio” [26]. Subjects with a higher body mass are penalized when VO2peak is related to body mass [27]. However, from a performance viewpoint, relative VO2peak is important for capacity to perform weight bearing activities, such as walking, running, or uphill cycling [5].
The results from our regression analyses confirm the findings of Debeaumont et al. [9]. They observed that next to gender, age and height were the best predictors of VO2peak in the obese population. Our regression model was able to explain almost 50% of the variance in VO2peak among the subjects.
A change in absolute CRF would be helpful when interpreting the effectiveness interventions, particularly lifestyle interventions, such as exercise training [31]
Strengths and Limitations
A primary merit of the current study is the large sample size used to analyze the association between body composition expressed in BMI and CRF. Another strength of this study is its multicenter design and the direct measurement of VO2peak which provided accurate data about CRF. On the other hand, there are some limitations that should be addressed. Firstly, the number of subjects with a BMI < 18.5 kg/m2 was relatively small. The groups contained of 49 male and 27 female subjects. Secondly, the participants included in the current study were regarded as apparently healthy. However, this was self-reported by the subjects. Also, body composition data (fat mass and fat free mass) were not available.
Recommendations for Future Research
A larger number of females, more participants older than 70 years, smoking, BMI < 18.0 kg/m2 and > 35.0 kg/m2, body composition (fat free mass), and physical activity level should be taken into consideration in a future study. Extensive research on this topic would offer more insight into the influence of excess body weight on CRF.
Clinical Relevance
Our findings indicate that adjustment of the absolute value of VO2peak in overweight and obese individuals is not necessarily in males, as well as in obese females. Adjustments for CRF in individuals with a BMI < 18.5 kg/m2 are also required.
Conclusion
Our findings indicate that BMI was not associated with CRF in addition to age, gender, and height. In subjects with a BMI < 18.5 kg/m2, CRF was lower compared to subjects with a BMI between 18.5 and 29.9 kg/m2. In obese subjects, CRF was only lower in females compared to females with a BMI between 18.5 and 29.9 kg/m2. Correcting CRF for BMI may be beneficial for subjects with a low BMI, and females with a BMI ≥ 30.0 kg/m2. The outcome of this study might help improve the interpretation of exercise testing results in individuals with a low or high BMI.
Availability of Data and Material
Not applicable.
Code Availability
Not applicable.
Abbreviations
- BMI:
-
Body Mass Index
- CPET:
-
Cardiopulmonary exercise testing
- CRF:
-
Cardiorespiratory fitness
- CVD:
-
Cardiovascular diseases
- HRpeak :
-
Peak heart rate
- RERpeak :
-
Peak respiratory exchange ratio
- VO2 peak :
-
Peak oxygen uptake
References
Al-Mallah MH, Sakr S, Al-Qunaibet A. Cardiorespiratory fitness and cardiovascular disease prevention: an update. Curr Atheroscler Rep. 2018;20(1):1–9. https://doi.org/10.1007/s11883-018-0711-4.
Alpert MA, Omran J, Bostick BP. Effects of obesity on cardiovascular hemodynamics, cardiac morphology, and ventricular function. Curr Obes Rep. 2016;5(4):424–34. https://doi.org/10.1007/s13679-016-0235-6.
Argo CK, Stine JG, Henry ZH, Lackner C, Patrie JT, Weltman AL, Caldwell SH. Physical deconditioning is the common denominator in both obese and overweight subjects with nonalcoholic steatohepatitis. Aliment Pharmacol Ther. 2018;48(3):290–9. https://doi.org/10.1111/apt.14803.
ATS/ACCP. ATS/ACCP statement on cardiopulmonary exercise testing. Am J Respir Crit Care Med. 2003;167(2):211–77. https://doi.org/10.1164/rccm.167.2.211.
Buskirk E, Taylor HL. Maximal oxygen intake and its relation to body composition, with special reference to chronic physical activity and obesity. J Appl Physiol. 1957;11(1):72–8. https://doi.org/10.1152/jappl.1957.11.1.72.
Carvalho LP, Di Thommazo-Luporini LD, Aubertin-Leheudre M, Bonjorno Junior JC, de Oliveira CR, Luporini RL, Mendes RG, Zangrando KTL, Trimer R, Arena R, Borghi-Silva A. Prediction of cardiorespiratory fitness by the six-minute step test and its association with muscle strength and power in sedentary obese and lean young women: a cross-sectional study. PLoS ONE. 2015;10(12): e0145960. https://doi.org/10.1371/journal.pone.0145960.
Dagan SS, Segev S, Novikov I, Dankner R. Waist circumference vs body mass index in association with cardiorespiratory fitness in healthy men and women: a cross sectional analysis of 403 subjects. Nutr J. 2013;12:12. https://doi.org/10.1186/1475-2891-12-12.
Davison K, Bircher S, Hill A, Coates AM, Howe PRC, Buckley JD. Relationships between Obesity, Cardiorespiratory Fitness, and Cardiovascular Function. Journal of obesity. 2010;2010: 191253. https://doi.org/10.1155/2010/191253.
Debeaumont D, Tardif C, Folope V, Castres I, Lemaitre F, Tourny C, Dechelotte P, Thill C, Darmon A, Coquart JB. A specific prediction equation is necessary to estimate peak oxygen uptake in obese patients with metabolic syndrome. J Endocrinol Invest. 2016;39(6):635–42. https://doi.org/10.1007/s40618-015-0411-7.
Goran M, Fields D, Hunter GR, Herd SL, Weinsier RL. Total body fat does not influence maximal aerobic capacity. Int J Obes Relat Metab Disord. 2000;24(7):841–8. https://doi.org/10.1038/sj.ijo.0801241.
Hansen D, Marinus N, Remans M, Courtois I, Cools F, Calsius J, Massa G, Takken T. Exercise tolerance in obese vs. lean adolescents: a systematic review and meta-analysis. Obes Rev. 2014;15(11):894–904. https://doi.org/10.1111/obr.12202.
Hansen JE, Sue DY, Wasserman K. Predicted values for clinical exercise testing. Am Rev Respir Dis. 1984;129(2 Pt 2):S49-55. https://doi.org/10.1164/arrd.1984.129.2P2.S49.
Hassinen M, Lakka TA, Hakola L, Savonen K, Komulainen P, Litmanen H, Kiviniemi V, Kouki R, Heikkilá H, Rauramaa R. Cardiorespiratory fitness and metabolic syndrome in older men and women: the dose responses to Exercise Training (DR’s EXTRA) study. Diabetes Care. 2010;33(7):1655–7. https://doi.org/10.2337/dc10-0124.
Kaminsky LA, Imboden MT, Arena R, Myers J. Reference standards for cardiorespiratory fitness measured with cardiopulmonary exercise testing using cycle ergometry: data from the Fitness Registry and the Importance of Exercise National Database (FRIEND) Registry. Mayo Clin Proc. 2017;92(2):228–33. https://doi.org/10.1016/j.mayocp.2016.10.003.
Koch B, Schäper C, Ittermann T, Spielhagen T, Dörr M, Völzke H, Opitz CF, Ewert R, Gläser S. Reference values for cardiopulmonary exercise testing in healthy volunteers: the SHIP study. Eur Respir J. 2009;33(2):389–97. https://doi.org/10.1183/09031936.00074208.
Konigstein K, Klenk C, Rossmeissl A, Baumann S, Infanger D, Hafner B, Hinrichs T, Hanssen H, Schmidt-Trucksäss A. The obesity factor: how cardiorespiratory fitness is estimated more accurately in people with obesity. Obesity. 2018;26(2):291–8. https://doi.org/10.1002/oby.22078.
Krachler B, Savonen K, Komulainen P, Hassinen M, Lakka TA, Rauramaa R. Cardiopulmonary fitness is a function of lean mass, not total body weight: the DR’s EXTRA study. Eur J Prev Cardiol. 2015;22(9):1171–9. https://doi.org/10.1177/2047487314557962.
Laukkanen JA, Kurl S, Salonen R, Rauramaa R, Salonen JT. The predictive value of cardiorespiratory fitness for cardiovascular events in men with various risk profiles: a prospective population-based cohort study. Eur Heart J. 2004;25(16):1428–37. https://doi.org/10.1016/j.ehj.2004.06.013.
Laxmi CC, Udaya IB, Vinutha SS. Effect of body mass index on cardiorespiratory fitness in young healthy males. Int J Sci Res Publ. 2014;4(2):1–4.
Lorenzo S, Babb TG. Quantification of cardiorespiratory fitness in healthy nonobese and obese men and women. Chest. 2012;141(4):1031–9. https://doi.org/10.1378/chest.11-1147.
Mylius CF, Krijnen WP, van der Schans CP, Takken T. Peak oxygen uptake reference values for cycle ergometry for the healthy Dutch population: data from the LowLands Fitness Registry. ERJ Open Res. 2019;5(2):00056–2018. https://doi.org/10.1183/23120541.00056-2018.
Van de Poppe DJ, Hulzebos E, Takken T, Low-Land Fitness Registry Study G. Reference values for maximum work rate in apparently healthy Dutch/Flemish adults: data from the LowLands fitness registry. Acta Cardiol. 2019;74(3):223–30. https://doi.org/10.1080/00015385.2018.1478763.
Sabag A, Keating SE, Way KL, Sultana RN, Lanting SM, Twigg SM, Johnson NA. The association between cardiorespiratory fitness, liver fat and insulin resistance in adults with or without type 2 diabetes: a cross-sectional analysis. BMC Sports Sci Med Rehabil. 2021;13(1):40. https://doi.org/10.1186/s13102-021-00261-9.
Takken T, Mylius CF, Paap D, Broeders W, Hulzebos HJ, Van Brussel M, Bongers BC. Reference values for cardiopulmonary exercise testing in healthy subjects - an updated systematic review. Expert Rev Cardiovasc Ther. 2019;17(6):413–26. https://doi.org/10.1080/14779072.2019.1627874.
Tammelin T, Näyhä S, Rintamäki H. Cardiorespiratory fitness of males and females of northern Finland birth cohort of 1966 at age 31. Int J Sports Med. 2004;25(7):547–52. https://doi.org/10.1055/s-2004-820949.
Tanner JM. Fallacy of per-weight and per surface area standards, and their relation to spurius correlation. J Appl Physiol. 1949;2(1):1–15. http://doi.org/10.1152/jappl.1949.2.1.1.
Vanderburgh PM, Katch FI. Ratio scaling of VO2max penalizes women with larger percent body fat, not lean body mass. Med Sci Sports Exerc. 1996;28(9):1204–8. https://doi.org/10.1097/00005768-199609000-00019.
Vella CA, Paul DR, Bader J. Cardiac response to exercise in normal-weight and obese, Hispanic men and women: implications for exercise prescription. Acta Physiol. 2012;205(1):113–23. https://doi.org/10.1111/j.1748-1716.2011.02371.x.
Vella CA, Zubia RY, Burns SF, Ontiveros D. Cardiac response to exercise in young, normal weight and overweight men and women. Eur J Appl Physiol. 2009;105(3):411–9. https://doi.org/10.1007/s00421-008-0918-0.
Wasserman K, Hansen JE, Sue DY, Stringer W, Whipp BJ. Principles of exercise testing and interpretation: including pathophysiology and clinical applications. 4th ed. Philadelphia: Lippincott Williams & Wilkins; 2005.
Zouhal H, Ben Abderrahman A, Khodamoradi A, Saeidi A, Jayavel A, Hackney AC, Laher I, Algotar AM, Jabbour G. Effects of physical training on anthropometrics, physical and physiological capacities in individuals with obesity: a systematic review. Obes Rev. 2020;21(9): e13039. https://doi.org/10.1111/obr.13039.
Acknowledgements
The Low-Lands Fitness Registry Study Group consists of the following contributors: Harriet Wittink PhD, Marcel Schmitz MSc, Pieter-Jan van Ooi MD, Geert van Beek MSc, Leendert van Galen MSc, Jeroen Molinger MSc, Robert Rozenberg MD, Marieke van den Oord PhD, Yvonne Hartman PhD, Nicolle Verbaarschot MSc, Aernout Snoek MD, Jaap Stomphorst MD, Joep van Kesteren MSc.
Funding
Not applicable.
Author information
Authors and Affiliations
Consortia
Contributions
(1) Made substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data; or the creation of new software used in the work; (2) drafted the work or revised it critically for important intellectual content; (3) approved the version to be published; and (4) agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no confict of interest.
Ethical approval
Not applicable.
Additional information
The members of the Low-Lands Fitness Registry are mentioned “Acknowledgments section”.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Takken, T., Hulzebos, H.J. & Low-Lands Fitness Registry Study Group. Is BMI Associated with Cardiorespiratory Fitness? A Cross-Sectional Analysis Among 8470 Apparently Healthy Subjects Aged 18–94 Years from the Low-Lands Fitness Registry. J. of SCI. IN SPORT AND EXERCISE 4, 283–289 (2022). https://doi.org/10.1007/s42978-021-00143-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42978-021-00143-z