Abstract
Aims
To explore the neural mechanism of white matter related cognitive dysfunction in patients with type 2 diabetes mellitus.
Methods
This prospective study between 2016 and 2018 included 55 patients with type 2 diabetes mellitus and 40 participants without type 2 diabetes mellitus. Detailed neuropsychological assessment, clinical and biochemical information, diffusion tensor imaging and resting-state functional MRI were collected. The fractional anisotropy (FA), mean diffusivity (MD) and amplitude of low-frequency fluctuation (ALFF) in white matter were compared between the two groups and then extracted for correlation and mediation analysis with clinical parameters and cognitive assessments.
Results
The current research showed that three parameters changed in several white matter areas of patients with type 2 diabetes mellitus. Meanwhile, FA in the corpus callosum mediated the effect of insulin resistance on executive function in both two groups. In the group without type 2 diabetes mellitus, ALFF moderated the effect of FA on executive function.
Conclusion
Patients with type 2 diabetes mellitus showed alterations in structural integrity and activation of white matter, which played a mediating and regulating role in the cognitive impairment caused by insulin resistance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Approximately 537 million adults aged 20–79 years suffered from diabetes in 2021 [1], which makes diabetes-associated health issues a concern. Epidemiological studies have confirmed the close correlation and interaction between diabetes and cognitive impairment [2], including poor performance in cognitive tasks, rapid cognitive decline, and high risk of dementia [3]. However, the key central nervous system mechanisms of diabetes-associated cognitive impairment still need to be determined.
Although many studies have reported functional network of grey matter, most fMRI studies ignored a major part of the brain, the white matter. It is increasingly recognized that white matter is strongly associated with baseline cognitive performance and risk of prevalent mild cognitive impairment or dementia [4]. Recent studies have shown that white matter microstructural integrity can predict improvements in cognitive function in patients with cognitive-related diseases after cognitive training [5, 6], which indicated that changes in white matter integrity may become an important target for the prediction and treatment of cognitive decline. Therefore, this study focused on the changes in white matter in patients with type 2 diabetes mellitus to expand the understanding of the mechanisms of diabetes-associated cognitive impairment.
Magnetic resonance imaging provides non-invasive indicators for assessing white matter structure and function. Diffusion tensor imaging (DTI) sequences using fractional anisotropy (FA) and mean diffusivity (MD) as detection parameters can be used to evaluate the microstructure of white matter [7]. In studies of diabetes-associated cognitive impairment, extensive white matter integrity changes were observed in multiple brain regions, including the corpus callosum, hippocampus, and frontal and temporal lobes [8]. Recently, functional magnetic resonance imaging (fMRI), which provides the blood oxygenation level-dependent (BOLD) signal, has been recognized to contain rich functional information regarding white matter. Poorer white matter microstructure integrity was associated with weakened BOLD modulation [9]. The amplitude of low-frequency fluctuation (ALFF) has been proposed as a meaningful and direct indicator for detecting activation [10] and the functional networks within white matter [11].
Therefore, the purpose of the current study was to introduce BOLD fluctuations in white matter in resting-state fMRI as a complement to DTI parameters for detecting microstructural and functional disorders of white matter in patients with type 2 diabetes mellitus. In addition, detailed cognitive assessment for general cognition and various cognitive subdomains, as well as clinical variables such as insulin resistance (IR), were taken into consideration for a comprehensive correlation and mediation analysis to identify mechanisms of diabetes-associated cognitive impairment.
Materials and methods
Participants
The current study was approved by the Ethics Committee of the Nanjing Drum Tower Hospital and registered at Clinicaltrails.gov (NCT 02738671). Written informed consent was obtained from all participants after an elaborate description of the study.
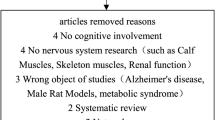
The study included 60 patients with type 2 diabetes mellitus and 40 participants without type 2 diabetes mellitus. Five patients with type 2 diabetes mellitus were excluded for diagnosis with pre-diabetes, image artefacts and excessive head movement (> 2 mm shift or > 2° rotation). A total of 55 patients with type 2 diabetes mellitus (30 men and 25 women; mean age 53.2 years; range 37.0–66.0 years) and 40 participants without type 2 diabetes mellitus (17 men and 23 women; mean age, mean age 51.9 years; range 37.0–65.0 years) matched for age, sex and educational level were finally included in the data analysis.
Inclusion criteria for all participants were age ranging from 35 to 75 years; right handedness; 6 or more years of education. The diagnostic criteria for type 2 diabetes mellitus were based on the World Health Organization/International Diabetes Federation criteria. The exclusion criteria included (a) a Mini-Mental State Examination (MMSE) score < 27; (b) a history of cardiovascular disease or mental and neurological disease; (c) a self-reported history of alcohol or substance abuse; and (d) unsuitability for MRI scanning.
Clinical features, laboratory features and cognitive assessment
All subjects participated in the standardized questionnaire survey, during which clinical information and anthropometric features were recorded, including lifestyle and habits, heredity and disease history, and body weight and height. All control subjects had a 2-h oral glucose tolerance test, while patients with type 2 diabetes mellitus had a steamed bread meal test. Blood glucose, glycated haemoglobin (HbA1c), insulin and C-peptide levels were assessed. IR was calculated using the HOMA2-IR (Homeostatic Model Assessment) calculator v2.2.3 [12]. Blood pressure was averaged across three time points in one day. Total cholesterol, triglyceride, low-density lipoprotein level, high-density lipoprotein level, creatinine and estimated glomerular filtration rate (Modification of Diet in Renal Disease Study) [eGFR (MDRD)] were provided by standard laboratory examination. All subjects received the same neuropsychological tests assessing global cognition and cognitive subdomains, as shown in Table 1. All cognitive assessments were performed by neurologists blinded to the clinical and imaging information.
MRI acquisition and image processing
MRI data were acquired on a 3.0 T clinical MR scanner (Achieva TX, Philips Medical Systems, Eindhoven, The Netherlands) using an 8-channel head coil. The scan parameters for DTI, resting-state fMRI and structural imaging are provided in the supplementary materials. The preprocessing of the DTI data was implemented using a pipeline toolbox for analysing brain diffusion images (PANDA) [13] to obtain the FA and MD, while the preprocessing of the resting-state fMRI data was performed using Data Processing and Analysis for (Resting-State) Brain Imaging (DPABI) [14]. The specific steps of preprocessing are provided in the supplementary materials.
ALFF analysis was also performed using DPABI software with the following steps: (a) transformed to a frequency domain with a fast Fourier transform and obtained the power spectrum; (b) calculated the square root at each frequency and averaged at each voxel; and (c) used the ALFF values after z transformation to measure the amplitude of regional activity in each subject.
Statistical analysis
Statistics for the demographic information, clinical indicators and cognitive scores were performed using SPSS software (version 20.0; SPSS, Chicago, IL, United States). In continuous variables, an independent sample t test was used for inter-group comparisons if the data confirm to a normal distribution, and intra-group statistics were reported as the mean ± standard deviation; a nonparametric t test was used for inter-group comparisons if the data do not confirm to a normal distribution, and intra-group statistics were reported as the median (first quartile, third quartile). While Pearson’s χ2 test was used for categorical variables (p < 0.05 considered statistically significant).
The DPABI software was used for statistical analysis of the FA, MD and ALFF images. A voxel-based independent sample t test was used for the comparison of FA, MD and ALFF images between patients and controls with age, sex, education and waist-hip ratio (WHR) as covariates. The group-level white matter mask (cluster size = 21,289) was used in the comparison of FA and MD images. The intersecting regions showing significant differences in FA and MD were extracted as masks (cluster size = 730) for the group analysis of the ALFF images. Then, the regions showing significant differences in ALFF were extracted as regions of interest (ROI) for the subsequent correlation analyses. Multiple comparison correction was performed using GRF correction (voxel p value < 0.001, cluster p value < 0.05).
The mean FA, MD and ALFF values of the ROIs were extracted for each individual. The episodic memory, working memory, word fluency, processing speed and executive function scores were separately added and standardized to z scores. Meanwhile, partial correlation analyses with age, sex, education and WHR controlled for were conducted to assess whether the structural and functional changes in the brain were associated with diabetes-related characteristics and different cognitive domains [with false discovery rate (FDR) correction].
Moderation and mediation factor analyses were performed using bootstrapped mediation procedures included in the PROCESS SPSS macro [15] to examine the interrelations among white matter structure and activation, cognitive function, and diabetes-related characteristics. Age, sex, education and WHR were used as covariates. Confidence intervals (CI) were set as 95%, and the number of bootstrap samples was set as 5000. p < 0.05 was considered statistically significant.
Results
Demographics, clinical variables and cognitive assessment
The demographic, clinical variables and cognitive assessment of type 2 diabetes mellitus and the control group are summarized in Table 1. No significant differences were observed in age, sex, education level, tobacco and alcohol habits, diastolic blood pressure, and total cholesterol, triglyceride, low-density lipoprotein, fasting insulin, fasting C-peptide levels, creatinine and eGFR (MDRD). Patients with type 2 diabetes mellitus had higher HbA1c, fasting and 2-h plasma glucose, 2 h postprandial glucose, 2 h postprandial insulin, body mass index (BMI), WHR, and systolic blood pressure levels, and lower high-density lipoprotein (HDL) levels than the controls. There were no significant differences between the two groups in global cognition, total scores for visual attention and task switching, or word fluency. In contrast, patients with type 2 diabetes mellitus had lower scores on the episodic and working memory tests and used longer times on the executive function test than the controls, all of which indicated worse performance.
Lower FA and higher MD in extensive white matter regions
Between-group analyses corrected for age, sex, education and WHR showed lower FA in the corpus callosum, bilateral frontal lobes, left cingulate gyrus and left temporal lobe (Fig. 1a and Table 2) and higher MD in the bilateral frontal lobes, right cingulate gyrus and right parietal lobe (Fig. 1b and Table 2) in patients with type 2 diabetes mellitus compared with the controls (voxel p value < 0.001, cluster p value < 0.05, with GRF correction).
Voxel-based independent sample t tests corrected for age, sex, education and WHR indicated altered FA, MD and ALFF in patients with type 2 diabetes compared with non-diabetic controls [with Gaussian random field (GRF) correction, voxel-level p < 0.001, cluster-level p < 0.05]. FA was observed to be lower in the corpus callosum, bilateral frontal lobes, left cingulate gyrus and left temporal lobe (a). MD was observed to be higher in the bilateral frontal lobes, right cingulate gyrus and right parietal lobe (b). Between-group analysis in white matter regions with significant differences in FA or MD (the regions of the purple coil in c) corrected for age, sex, education and WHR showed higher ALFF in the corpus callosum in patients with type 2 diabetes compared with the control group. ALFF was higher in the corpus callosum (c). L left, R right, ALFF amplitude of low-frequency fluctuation, FA fractional anisotropy, MD mean diffusivity, WHR waist-hip ratio
Higher ALFF in white matter regions
Between-group analysis in white matter regions with significant differences in FA or MD corrected for age, sex, education and WHR showed higher ALFF in the genu of the corpus callosum in patients with type 2 diabetes mellitus compared with the controls (voxel p value < 0.001, cluster p value < 0.05, with GRF correction) (Fig. 1c and Table 2).
Associations of white matter parameters in the genu of the corpus callosum with diabetes-related characteristics and cognitive assessments
White matter parameters with significant differences in the corpus callosum were extracted. As shown in Table 3, within the control group, ALFF was observed to be significantly positively correlated with fasting C-peptide levels (r = 0.474, p = 0.004), HOMA2-IR (r = 0.477, p = 0.003), and executive function (r = 0.655, p = 0.001). FA was observed to be significantly negatively correlated with executive function (r = − 0.587, p = 0.001). Within the patients with type 2 diabetes mellitus, FA was observed to be significantly negatively correlated with fasting C-peptide levels (r = − 0.386, p = 0.005) and executive function (r = − 0.372, p = 0.007).
Mediation and moderation models for the associations among cognition, white matter and diabetes-related characteristics
Mediation analyses were performed to determine whether white matter alterations acted as a moderation or mediation factor between executive function and IR. Figure 2 demonstrates that FA mediated the effect of HOMA2-IR on executive function in both patients with type 2 diabetes mellitus (β = 0.0907, 95% bootstrap CI [0.00081, 0.2261]) and participants without type 2 diabetes mellitus (β = 0.3124, 95% bootstrap CI [0.0040, 0.6468]) groups. While ALFF moderated the effect of FA on executive function (β = − 0.3025, p = 0.0163) only in the non-diabetic control group.
Moderation and mediation factor analyses for the associations among HOMA2-IR, FA and ALFF in the corpus callosum and executive function. Standardized β-coefficients were derived from the mediation models controlling for age, sex, education and WHR. FA mediated the effect of HOMA2-IR on executive function in both diabetic and non-diabetic control groups. While ALFF moderated the effect of FA on executive function only in the non-diabetic control group. ALFF amplitude of low-frequency fluctuation, FA fractional anisotropy, HOMA2-IR homeostatic model assessment 2 of insulin resistance, WHR waist-hip ratio
Discussion
In the current study, we observed that the microstructural integrity of white matter was disrupted in the corpus callosum, bilateral frontal lobes, bilateral cingulate gyrus, left temporal lobe and right parietal lobe in patients with type 2 diabetes mellitus. It was also found that the activation of the genu of the corpus callosum was altered in these damaged white matter regions. In addition, mediation and moderation factor analyses supported the existence of detrimental pathways linking insulin resistance to worse executive function through lower FA and higher ALFF in the genu of the corpus callosum.
Decreased memory and executive function were observed in patients with type 2 diabetes mellitus in our study, which was consistent with previous studies [16, 17], indicating vulnerable cognitive subdomains that deserve more attention to discover mechanisms related to changes in cognition. Furthermore, impaired executive function and working memory can in turn affect self-regulation behaviour and diabetes care management and ultimately lead to worse disease control [18]. Numerous studies reported an extensive decrease in FA in the white matter of patients with type 2 diabetes mellitus [19], which indicated damage of microstructures related to cognitive impairment [20]. Executive function was not only closely associated with the frontal lobes but also predicted by the parameter of white matter integrity in the corpus callosum and cingulate gyrus [21]. In addition, disruption of white matter in the temporal lobe can lead to decreased memory performance.
This study was the first to use the parameter ALFF, a BOLD fluctuation parameter, to detect white matter activation in the study of diabetes-related cognitive impairment, and verified a relationship between FA and fMRI BOLD response, which was consistent with the previous study [22]. BOLD fMRI activation in white matter was reported to be detectable and meaningful, and was confirmed highly correlated to resting-state grey matter networks, highlighting their functional role [11]. The corpus callosum serves as a crucial organization for understanding the information integration between the two hemispheres. Several studies, paying more attention to the corpus callosum, suggest strongly that task-induced and resting state signals in white matter appear to reflect hemodynamic changes associated with neural activity [23]. Compared with DTI, the low-frequency amplitude signal of fMRI is more sensitive to the changes of white matter function and ALFF can indicate the specific microstructure changes of involved in white matter efficiency such as internal capsule and corpus callosum [24]. The current study report alterations in ALFF in the corpus callosum in patients with type 2 diabetes mellitus, a measure that can become a supplement to DTI parameters, and potential evidence for the progression of white matter damage.
In addition, the current study used mediation and moderation factor analyses to explore the role of white matter microstructural integrity and activation in the development of cognitive impairment in patients with type 2 diabetes mellitus. It was observed that in the process of IR affecting cognition, FA, which reflected the structural integrity of the white matter, played a mediating role in this influence in both patients and controls. In addition, ALFF moderated the effect of white matter integrity damage on executive function in the controls. However, this regulatory effect was not observed in patients with type 2 diabetes mellitus, which may have reflected the compensation for regional white matter integrity alterations in controls and the functional decompensation in patients with type 2 diabetes mellitus.
Recent studies have emphasized a close relationship between IR and executive function, confirmed that IR predicted cognitive decline [25], suggested that controlling the level of IR has substantial benefits for cognitive preservation and restoring insulin responsiveness may help reverse cognitive impairment [26]. Although previous studies have reported the correlation between IR and changes in white matter parameters, especially in the corpus callosum [27], the specific mechanism of how white matter integrity mediates the effect of IR on cognition has not been determined. Associations were observed between inflammatory factors and white matter injury [28]. White matter FA changes associated with IR might be due to neuro inflammation, a condition frequently caused by IR, and lead to neurodegenerative diseases. In addition, a recent study suggested that IR induced changes in cholesterol metabolism may be the mechanism by which IR and insulin affect white matter myelination and lead to cognitive decline or susceptibility to neurodegenerative diseases [29].
There are still some limitations in this study. First, although white matter BOLD fluctuation parameters such as ALFF have been indicated to have physiological value, the specific mechanisms of the white matter damage observed here have not been clearly demonstrated. Second, the design of the current study was cross-sectional and thus cannot address issues of causality related to future cognitive decline due to diabetes. Longitudinal studies are needed to observe the dynamic relationship between diabetic parameters and white matter parameters and to explore whether the control of diabetes can help to repair the structural and functional impairments in white matter and cognitive function.
In conclusion, our findings demonstrated that patients with type 2 diabetes mellitus showed a mild impairment in several cognitive subdomains and alterations in white matter; these findings can be considered early indicators of cognitive impairment before the decline in general cognition. The current study highlighted the significance of IR in the progression of diabetic-related cognitive impairment and proposed the structural and functional alteration of white matter as a significant intermediate link, which may provide new ideas for further research.
Data availability statement
The datasets generated during and/or analysed during the current study are not publicly available due privacy ethical but are available from the corresponding author on reasonable request.
Abbreviations
- DTI:
-
Diffusion tensor imaging
- FA:
-
Fractional anisotropy
- MD:
-
Mean diffusivity
- fMRI:
-
Functional magnetic resonance imaging
- BOLD:
-
Blood oxygenation level-dependent
- ALFF:
-
Amplitude of low-frequency fluctuation
- IR:
-
Insulin resistance
- HOMA2-IR:
-
Homeostatic model assessment 2—insulin resistance
- eGFR (MDRD):
-
Estimated glomerular filtration rate (Modification of Diet in Renal Disease Study
References
Sun H, Saeedi P, Karuranga S, Pinkepank M, Ogurtsova K, et al. IDF diabetes Atlas: global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract. 2021. https://doi.org/10.1016/j.diabres.2021.109119.
Xue M, Xu W, Ou YN, Cao XP, Tan MS, Tan L, et al. Diabetes mellitus and risks of cognitive impairment and dementia: a systematic review and meta-analysis of 144 prospective studies. Ageing Res Rev. 2019;55: 100944. https://doi.org/10.1016/j.arr.2019.100944.
Koekkoek PS, Kappelle LJ, van den Berg E, Rutten GE, Biessels GJ. Cognitive function in patients with diabetes mellitus: guidance for daily care. Lancet Neurol. 2015;14(3):329–40. https://doi.org/10.1016/S1474-4422(14)70249-2.
Power MC, Su D, Wu A, Reid RI, Jack CR, Knopman DS, et al. Association of white matter microstructural integrity with cognition and dementia. Neurobiol Aging. 2019;83:63–72. https://doi.org/10.1016/j.neurobiolaging.2019.08.021.
de Lange AG, Brathen AC, Grydeland H, Sexton C, Johansen-Berg H, Andersson JL, et al. White matter integrity as a marker for cognitive plasticity in aging. Neurobiol Aging. 2016;47:74–82. https://doi.org/10.1016/j.neurobiolaging.2016.07.007.
Subramaniam K, Gill J, Fisher M, Mukherjee P, Nagarajan S, Vinogradov S. White matter microstructure predicts cognitive training-induced improvements in attention and executive functioning in schizophrenia. Schizophr Res. 2018;193:276–83. https://doi.org/10.1016/j.schres.2017.06.062.
Walhovd KB, Johansen-Berg H, Karadottir RT. Unraveling the secrets of white matter—bridging the gap between cellular, animal and human imaging studies. Neuroscience. 2014;276:2–13. https://doi.org/10.1016/j.neuroscience.2014.06.058.
Biessels GJ, Reijmer YD. Brain changes underlying cognitive dysfunction in diabetes: what can we learn from MRI? Diabetes. 2014;63(7):2244–52. https://doi.org/10.2337/db14-0348.
Webb CE, Rodrigue KM, Hoagey DA, Foster CM, Kennedy KM. Contributions of white matter connectivity and BOLD modulation to cognitive aging: a lifespan structure–function association study. Cereb Cortex. 2020;30(3):1649–61. https://doi.org/10.1093/cercor/bhz193.
Ji G-J, Liao W, Chen F-F, Zhang L, Wang K. Low-frequency blood oxygen level-dependent fluctuations in the brain white matter: more than just noise. Sci Bull. 2017;62(9):656–7. https://doi.org/10.1016/j.scib.2017.03.021.
Peer M, Nitzan M, Bick AS, Levin N, Arzy S. Evidence for functional networks within the human brain’s white matter. J Neurosci. 2017;37(27):6394–407. https://doi.org/10.1523/JNEUROSCI.3872-16.2017.
Levy JC, Matthews DR, Hermans MP. Correct homeostasis model assessment (HOMA) evaluation uses the computer program. Diabetes Care. 1998;21(12):2191–2. https://doi.org/10.2337/diacare.21.12.2191.
Cui Z, Zhong S, Xu P, He Y, Gong G. PANDA: a pipeline toolbox for analyzing brain diffusion images. Front Hum Neurosci. 2013;7:42. https://doi.org/10.3389/fnhum.2013.00042.
Yan CG, Wang XD, Zuo XN, Zang YF. DPABI: data processing and analysis for (resting-state) brain imaging. Neuroinformatics. 2016;14(3):339–51. https://doi.org/10.1007/s12021-016-9299-4.
Hayes AJJOEM. Introduction to mediation, moderation, and conditional process analysis. J Educ Meas. 2013;51(3):335–7. https://doi.org/10.1111/jedm.12050.
Sanjari Moghaddam H, Ghazi Sherbaf F, Aarabi MH. Brain microstructural abnormalities in type 2 diabetes mellitus: a systematic review of diffusion tensor imaging studies. Front Neuroendocrinol. 2019;55: 100782. https://doi.org/10.1016/j.yfrne.2019.100782.
Alotaibi A, Tench C, Stevenson R, Felmban G, Altokhis A, Aldhebaib A, et al. Investigating brain microstructural alterations in type 1 and type 2 diabetes using diffusion tensor imaging: a systematic review. Brain Sci. 2021. https://doi.org/10.3390/brainsci11020140.
Black S, Kraemer K, Shah A, Simpson G, Scogin F, Smith A. Diabetes, depression, and cognition: a recursive cycle of cognitive dysfunction and glycemic dysregulation. Curr Diab Rep. 2018;18(11):118. https://doi.org/10.1007/s11892-018-1079-0.
Zhou C, Li J, Dong M, Ping L, Lin H, Wang Y, et al. Altered white matter microstructures in type 2 diabetes mellitus: a coordinate-based meta-analysis of diffusion tensor imaging studies. Front Endocrinol (Lausanne). 2021;12: 658198. https://doi.org/10.3389/fendo.2021.658198.
Gao S, Chen Y, Sang F, Yang Y, Xia J, Li X, et al. White matter microstructural change contributes to worse cognitive function in patients with type 2 diabetes. Diabetes. 2019;68(11):2085–94. https://doi.org/10.2337/db19-0233.
Bettcher BM, Mungas D, Patel N, Elofson J, Dutt S, Wynn M, et al. Neuroanatomical substrates of executive functions: beyond prefrontal structures. Neuropsychologia. 2016;85:100–9. https://doi.org/10.1016/j.neuropsychologia.2016.03.001.
Warbrick T, Rosenberg J, Shah NJ. The relationship between BOLD fMRI response and the underlying white matter as measured by fractional anisotropy (FA): a systematic review. Neuroimage. 2017;153:369–81. https://doi.org/10.1016/j.neuroimage.2016.12.075.
Gore JC, Li M, Gao Y, Wu TL, Schilling KG, Huang Y, et al. Functional MRI and resting state connectivity in white matter—a mini-review. Magn Reson Imaging. 2019;63:1–11. https://doi.org/10.1016/j.mri.2019.07.017.
Frizzell TO, Phull E, Khan M, Song X, Grajauskas LA, Gawryluk J, et al. Imaging functional neuroplasticity in human white matter tracts. Brain Struct Funct. 2022;227(1):381–92. https://doi.org/10.1007/s00429-021-02407-4.
Ekblad LL, Rinne JO, Puukka P, Laine H, Ahtiluoto S, Sulkava R, et al. Insulin resistance predicts cognitive decline: an 11-year follow-up of a nationally representative adult population sample. Diabetes Care. 2017;40(6):751–8. https://doi.org/10.2337/dc16-2001.
Arnold SE, Arvanitakis Z, Macauley-Rambach SL, et al. Brain insulin resistance in type 2 diabetes and Alzheimer disease: concepts and conundrums. Nat Rev Neurol. 2018;14(3):168–81. https://doi.org/10.1038/nrneurol.2017.185.
Ryu SY, Coutu JP, Rosas HD, Salat DH. Effects of insulin resistance on white matter microstructure in middle-aged and older adults. Neurology. 2014;82(21):1862–70. https://doi.org/10.1212/WNL.0000000000000452.
Sun J, Xu B, Zhang X, He Z, Liu Z, Liu R, et al. The mechanisms of type 2 diabetes-related white matter intensities: a review. Front Public Health. 2020;8: 498056. https://doi.org/10.3389/fpubh.2020.498056.
O’Grady JP, Dean DC 3rd, Yang KL, Canda CM, Hoscheidt SM, Starks EJ, et al. Elevated insulin and insulin resistance are associated with altered myelin in cognitively unimpaired middle-aged adults. Obesity (Silver Spring). 2019;27(9):1464–71. https://doi.org/10.1002/oby.22558.
Acknowledgements
This work was supported by the National Natural Science Foundation of China (81720108022, 91649116, 81571040); the social development project of science and technology project in Jiangsu Province (BE2016605, BE2017707); key medical talents of the Jiangsu province, the “13th Five-Year” health promotion project of the Jiangsu province (B.Z.2016-2020); Jiangsu Provincial Key Medical Discipline (Laboratory) (ZDXKA2016020); the project of the sixth peak of talented people (WSN-138, BZ). The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare they have no conflict of interest.
Ethical approval
This study was approved by the ethical committee of the Affiliated Drum Tower Hospital of Nanjing University Medical School. The study complied with the Declaration of Helsinki. Oral and informed consent was obtained from all volunteers.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wang, X., Bi, Y., Zhang, Z. et al. White matter microstructural integrity and BOLD fluctuation alterations mediated the effects of insulin resistance on cognitive function in patients with type 2 diabetes mellitus. Chin J Acad Radiol 5, 122–131 (2022). https://doi.org/10.1007/s42058-022-00093-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42058-022-00093-7