Key summary points
This study is the first to explore the risk factors of frailty in chronic obstructive pulmonary disease (COPD) patients.
AbstractSection FindingsThe estimated prevalence of frailty in patients with COPD was 36%.
AbstractSection MessageAge, education level, income level and CAT score are risk factors for frailty in COPD patients.
Abstract
Objective
To systematically review the prevalence and risk factors for frailty in patients with chronic obstructive pulmonary disease (COPD).
Methods
A systematic review and meta-analysis were conducted, and a search of the PubMed, Embase and Web of Science databases was carried out to collect Chinese and English studies on frailty and COPD published up to September 5, 2022.
Results
A total of 38 articles were included for the quantitative analysis after the collected literature was either included or omitted based on pertinent criteria. The results indicated that the estimated overall pooled prevalence of frailty was 36% (95% confidence interval [CI] = 31–41%), and the estimated pre-frailty was 43% (95% CI = 37–49%). A higher age (odds ratio [OR] = 1.04; 95% CI = 1.01–1.06) and higher COPD assessment test (CAT) score (OR = 1.19; 95% CI = 1.12–1.27) were associated with a significantly increased likelihood of frailty in patients with COPD. However, a higher educational attainment (OR = 0.55; 95% CI = 0.43–0.69) and higher income (OR = 0.63; 95% CI = 0.45–0.88) were associated with a significantly reduced risk of frailty in patients with COPD. A total of 17 other risk factors for frailty were identified via qualitative synthesis.
Conclusion
The incidence of frailty in patients with COPD is high, and there are many influencing factors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Frailty is a syndrome occurring in the older people that is defined as a state of increased vulnerability due to an age-related decline in function and reserves, which results in a decline in the ability to cope with daily or acute stressors [1, 2]. Once stressors strike, patients with frailty are likely to experience adverse consequences, such as prolonged hospital stays, decreased activity, occurrence of a disability attack, increased mortality and adverse drug reactions [3]. In addition, the presence of frailty is often observed in patients with chronic morbidities, and its prevalence is positively related to age [4,5,6]. Aging (in patients aged ≥ 65 years) and chronic diseases can promote health deterioration and increase the risk and severity of frailty [7,8,9].
Chronic obstructive pulmonary disease (COPD) has become a major challenge for public health worldwide. It is a common disease with high global morbidity and mortality rates [10], and is expected to rank fifth in terms of global disease burden and fourth in terms of mortality by 2030 [11]. According to current knowledge, COPD and frailty have certain overlapping risk factors, including aging, smoking, neuroendocrine abnormality, impaired immune system, chronic inflammation, lack of exercise and decreased exercise ability [5, 9]. Moreover, COPD is the most frequently studied chronic respiratory disease associated with frailty [12]. Compared to participants without COPD, patients with the disease have a higher likelihood of frailty [9]. In previous studies, the prevalence of frailty ranged from 9 to 28%, while the prevalence of pre-frailty ranged from 48 to 64%, depending on the setting [9]. Compared to patients without frailty, patients with both this condition and lung disease tend to have a worse prognosis, including a higher prevalence of hospitalization and readmission, prolonged hospital stay, disability and self-reported adverse endpoints [13].
As a dynamic state, frailty can be improved by a targeted treatment strategy; however, if left untreated, it can become worse, with a greater risk of adverse outcomes. Understanding the risk factors that contribute to frailty in patients with COPD is critical and could facilitate early identification of patients at high risk of frailty, as well as highlight new targets for interventions to prevent or improve the condition. To date, the associated risk factors of frailty in patients with COPD have not been systematically explored, thus hindering a reliable implementation of effective frailty interventions. Therefore, the present study quantitatively synthesizes the existing evidence on the prevalence and risk factors for frailty with COPD by performing a systematic review and meta-analysis, with the aim of highlighting areas for future research.
Methods
The meta-analysis followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Statement (PRISMA) guidelines. The protocol used for the present study is available from the International Prospective Register of Systematic Reviews (PROSPERO) database (https://www.crd.york.ac.uk/PROSPERO/).
Literature and data acquisition
Three databases (PubMed, Embase and Web of Science) were independently searched by two authors (L.C.Y. and X.Y.W.) from database inception to September 5, 2022. The medical subject heading terms and free words associated with frailty and COPD were used as keywords (e.g., chronic obstructive lung disease, chronic obstructive pulmonary diseases, chronic obstructive airway disease, chronic obstructive pulmonary disease, airflow obstruction, chronic, airflow obstructions, chronic, chronic airflow obstructions, chronic airflow obstruction and frailties, frailness, frailty syndrome, debility, and debilities). The entries were searched independently by the two authors, and other potential records were manually obtained from the references contained in related reviews and articles.
Inclusion and exclusion criteria
All observational studies investigating the associations between frailty and COPD were included. The inclusion criteria were as follows: (1) articles in English; (2) cross-sectional, case–control or cohort studies; (3) adult studies (≥ 18 years of age); and (4) articles reporting the prevalence rate data and prevalence rate or those that provide sufficient data for calculating the frailty prevalence rate in patients with COPD.
The exclusion criteria were as follows: (1) non-original articles (e.g., reviews, editorial letters or conference abstracts); (2) articles without an explicit definition of frailty; (3) articles with a single symptom used to define frailty; (4) articles with combined serious illness (e.g., human immunodeficiency virus); and (5) duplicates.
In addition, in the COPD frailty prevalence meta-analysis, only the frailty prevalence pertaining to COPD in the baseline data was reported due to the limitations of the original data.
Study selection and data extraction
After storing all relevant records, the two reviewers independently screened the literature using endnote software (Clarivate Analytics, the United States). First, the duplicates were deleted before the articles were checked by title and summary and the full text that met the inclusion and exclusion criteria was finally determined. A third reviewer became involved in the case of any disagreement.
The two reviewers independently extracted variables from the included articles, which included the following: (1) the basic information (author, country, year of publication, study design, sample size and setting); (2) exposure variables (prevalence of frailty and pre-frailty); (3) sociodemographic variables (percentage of males, age); (4) and the frailty assessment scale. A third reviewer approved the final version if there was no dispute at the time.
Related definitions
COPD: COPD is a common disease that can be prevented and treated, characterized by persistent respiratory symptoms and airflow limitations, usually associated with airway and/or alveolar abnormalities caused by significant exposure to harmful particles or gases [14].
Frailty: frailty is a medical syndrome with multiple causes, characterized by a decline in strength, endurance, and physiological function that increases an individual's progressive dependence and/or susceptibility to death [15].
Pre-frailty: pre-frailty refers to the intermediate state between health and frailty. Pre-frailty can be reversed to a healthy state, and some frailty states can also be reversed to pre-frailty [16].
Methodological quality assessment
The methodological quality was evaluated by two investigators using the Joanna Briggs Institute's critical appraisal checklist, which is widely applied in previous reports on prevalence [17]. In total, this checklist includes nine items, and the total score is positively related to the quality of the included studies. The studies were classified as high quality (≤ 49%), medium quality (50–69%) or low quality (≥ 70%) according to the percentage of ‘no’ answers [17, 18].
Statistical analysis
Data on the prevalence and impact of frailty in patients with COPD were extracted by two independent reviewers using Microsoft Excel. The meta-analysis was performed using Review Manager version 5.4 and Stata version 15.0 software. The I2 statistical test was used to assess the heterogeneity of the included studies. When there was heterogeneity in the study (I2 > 50% or P < 0.05), the results were combined using the random-effect model, with a fixed-effect model used in all other cases. Combined odds ratios (ORs) with a corresponding 95% confidence interval (CI) were calculated using a fixed-effect or random-effect model to compare the risk factors for the prevalence of frailty, with the significance determined using a Z test. When the P value was < 0.05, the results were considered statistically significant. Sensitivity analysis was performed by omitting individual studies and then comparing the P values of the combined ORs. When there was no substantial difference in the corresponding P value of the combined ORs (P < 0.05), the results were considered reliable. Publication bias was assessed using Begg’s test and funnel plot analysis [19, 20]. When the P value was < 0.05, the results were regarded as statistically significant.
Results
Search results
In total, 1687 relevant articles were identified from the PubMed (n = 138), Embase (n = 817) and Web of Science (n = 731) databases, with one article identified through other sources. After identifying any duplicate articles and any records marked as ineligible by the automation tools, 1570 articles were excluded. Following this, two reviewers screened the literature for highly relevant articles based on the titles and abstracts, with 117 considered for eligibility. After reviewing the full-text articles, 38 studies were finally determined to be eligible for the meta-analysis according to the inclusion criteria. The reasons for exclusion are detailed in Fig. 1.
Data extraction
The characteristics of the included studies are presented in Table 1. These studies were published between 2011 and 2022, and 24 of them were cross-sectional studies [6, 7, 19, 21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41], 8 of which were longitudinal studies [17, 42,43,44,45,46,47,48] and the remaining 6 cohort studies [12, 49,50,51,52,53]. In total, 19,362 participants from 13 countries were included in the analysis, with the main geographic locations in the United States (eight studies) [28, 38, 40, 44,45,46, 49, 50]. The qualified studies involved 30 studies pertaining to hospitals. The mean age of the included participants ranged from 61 to 86 years, while in 31 of the studies, more than half of the participants were men. The prevalence of frailty in these studies ranged from 6 to 83%. The Fried frailty phenotype definition of frailty was used in 16 studies, the Kihon checklist was used in 4 studies [7, 24, 44, 47], the FRAIL scale was used in two studies [27, 37] and the frailty index was also used in two studies [4, 29].
Prevalence of frailty in patients with chronic obstructive pulmonary disease
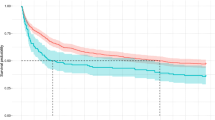
In total, 36 studies reported the prevalence of frailty in patients with COPD. The estimated overall pooled prevalence of frailty was 36% (95% CI = 31%–40%). There was significant heterogeneity (I2 = 98.6%, P < 0.001) among these studies (Fig. 2), and sensitivity analysis was thus conducted to explore the impact of a single study on the results of the meta-analysis. The analysis results indicated that the sensitivity was stable (Fig. 3). The funnel plot presented a largely asymmetric pattern (Fig. 4), which indicated the presence of publication bias.
Prevalence of pre-frailty in patients with chronic obstructive pulmonary disease
Of the 38 included studies, only 17 reported the prevalence of pre-frailty in patients with COPD. The estimated overall pooled prevalence of pre-frailty was 43% (95% CI = 37–49%), with a high heterogeneity (I2 = 96.0%, P < 0.001) (Fig. 5).
Meta-analysis of the risk factors for frailty in patients with chronic obstructive pulmonary disease
A total of six studies reported the risk factors for frailty in patients with COPD [24, 27, 32, 33, 37, 40]. Multivariate meta-analyses were performed in terms of nine risk factors (Table 2), with the most relevant detailed below.
Age
The meta-analysis of five studies [26, 32, 33, 37, 40] revealed that age was a risk factor for frailty in COPD (OR = 1.04; 95% CI = 1.01–1.06) (Supplemental File 1).
Educational attainment
The meta-analysis of three studies [26, 33, 40] revealed an association between educational attainment and the risk of frailty in patients with COPD. The results indicated that patients with a higher education were less likely to develop frailty (OR = 0.55; 95% CI = 0.43–0.69) (Supplemental File 2).
Income level
The meta-analysis of two studies [33, 40] revealed that a higher income (OR = 0.63; 95% CI = 0.45–0.88) was associated with a significantly reduced risk of frailty in patients with COPD (Supplemental File 3).
Assessment test score
A total of seven studies [17, 23, 24, 30, 31, 33, 35] investigated the relationship between the COPD CAT score and the risk of frailty in patients with COPD; however, most were unsuitable for extracting data and the meta-analysis could only be performed in terms of two of these studies [24, 33]. The results suggested that the CAT score was an indicator for frailty in patients with COPD (OR = 1.19; 95% CI = 1.12–1.27) (Supplemental File 4).
Narrative synthesis of the other risk factors for frailty in patients with chronic obstructive pulmonary disease
In addition to the above factors, 17 studies examined the other risk factors for frailty in patients with COPD and identified 17 significant risk factors for the condition. Among these factors, two pertained to the sociodemographic domain, seven pertained to clinical performance, seven were health-related and one pertained to the social domain (Table 3). These studies results indicated that the number of exacerbations within a year (6 studies), comorbidities (5 studies), gender (5 studies), Global Chronic Obstructive Pulmonary Disease (GOLD) Symptom Initiative (4 studies), modified Medical Research Council (mMRC) score (3 studies), drug quantity (3 studies), smoking status (2 studies), and depression (2 studies) were risk factors for frailty in COPD patients. Inconsistent associations with frailty were observed for gender and body mass index (BMI). In one study, men were associated with a higher risk, while in four studies, women were associated with a higher risk. In one study, a higher BMI (> 26 kg/m2) was associated with a higher risk, while in another, a BMI of < 21 kg/m2 was associated with a higher risk. Previous frailty, depression, a high mMRC score, GOLD B&D status, active smoking status and a higher number of comorbidities, exacerbations and drugs used were consistently found to be correlated with an increased risk of frailty. Other risk factors were only investigated in a single study.
Discussion
The present study provides a comprehensive review of the existing evidence on frailty prevalence and risk factors in patients with COPD. The analysis indicated that the estimated frailty prevalence proportion among the patients with COPD was 36% (95% CI = 31–40%) and that the estimated pre-frailty prevalence proportion was 43% (95% CI = 37–49%).
The studies included in our meta-analysis largely report various sociodemographic variables as risk factors, and the results of the meta-analysis indicated that age, educational attainment, income level and CAT score were associated with a higher prevalence of frailty. In terms of the risk factors for frailty, a further 17 factors were found in the eligible studies. A prior study found that COPD and frailty share certain risk factors, including age and smoking [54, 55]. In fact, frailty is considered to be a geriatric syndrome [56], with its prevalence increasing with age. Older COPD patients are often accompanied by multiple diseases [57]. When multiple diseases coexist, various chronic diseases interact and have a synergistic effect on vascular endothelial cell damage, thereby exacerbating cerebral ischemia and hypoxia and forming a vicious cycle, further reducing cognitive function [57]. In addition, the coexistence of multiple diseases can accelerate the decline of organ function, leading to a decrease in physiological reserves of multiple systems. Patients are in a chronic state of depletion, resulting in a decrease in tolerance and resistance, leading to frailty [58]. Furthermore, in the case of smoking, systemic inflammation can be demonstrated by increased levels of inflammatory markers, such as high-sensitivity C-reactive protein and interleukin-6 [56, 59]. In fact, interleukin-6 is associated with sarcopenia, which is regarded as the main cause of physical frailty [59]. Most studies indicate that among patients with COPD, women are more prone to frailty than men, with research demonstrating that the bone mass loss caused by hormone-related changes associated with the menopause may be the mechanism behind the high vulnerability risk among older women [60].
The present study found that patients with COPD who had a poorer respiratory performance (e.g., first–second forced expiratory volume percentage declined, higher CAT and mMRC scores) and depression had a higher chance of developing frailty than those without these issues. It is well known that individuals with poor lung function have breathing difficulties and one possible reason for this is that individuals with dyspnea are more inclined to a sedentary lifestyle and are more likely to develop more muscle strength, mass and quality defects than other individuals [61, 62]. As the degree of difficulty in breathing increases, the patient's physical activity decreases, resulting in muscle atrophy and decreased muscle strength, which further leads to a decrease in activity tolerance and a vicious cycle. Exercise training is an important cornerstone in lung rehabilitation, as evidenced by multiple studies [63, 64] which have shown that reasonable exercise training can effectively improve exercise tolerance, delay muscle atrophy and muscle strength decline in COPD patients, and help delay or reverse the delay. In addition to respiratory symptoms and muscle frailty, patients with COPD may also suffer from anorexia and weight loss, which leads to malnutrition [9]. A study by Beek et al. indicated that malnutrition substantially (40%) coexists with frailty since energy and protein intake, as well as other key nutrients, play a fundamental role in muscle function and fatigue [19].
Furthermore, disease-related pain tends to increase the chances of patients with COPD taking multiple drugs [65, 66]. Changes associated with aging can affect specific pharmacokinetics, such as a decreased drug clearance and increased drug accumulation, while they may also increase the patient’s pain [67]. This may increase the risk of drug-related side effects, such as poor mobility and malnutrition [68] and could increase the risk of frailty. Therefore, it is recommended to carefully evaluate the risks of multiple drug use, optimize medication regimens for the older people, and reduce the damage caused by adverse drug reactions [15]. In the future, further exploration can be made to reduce the impact of multiple drug use on the development of frailty.
Finally, the prevalence of COPD is higher among populations with low socioeconomic status and low social support [69]. The present study revealed a high prevalence of frailty in patients with a low socioeconomic status (e.g., education and income) and social support. These social-network background aspects can be a factor in alleviating the defects accumulated in the older people over time by providing help in terms of daily activities, cognitive stimulation, love, friendship, suggestions for specific needs and/or financial and material goods or services. New insight into the prevention and the management of the onset of frailty could also be provided. However, it is unclear how these environmental factors affect the relationship between frailty and COPD and further research is needed to ascertain whether specific social factors can clarify this relationship.
The present study adopted a rigorous methodology following PRISMA guidelines and quantitatively synthesized the prevalence and risk factors for frailty with COPD, further expanding the knowledge in this field. This may help doctors make risk-informed decisions in clinical management.
However, the study involves a number of limitations. In general, the data pertaining to study-level variables, such as identification and vulnerability factors, tend to be inconsistent, which may have led to a certain degree of heterogeneity among the included studies, thus undermining the robustness of the results. In addition, the risk factors for frailty in patients with COPD were identified mainly based on limited studies and univariate analyses. These deficiencies were primarily due to the inconsistent risk factors reported in the original studies. Finally, due to the limited resources, the meta-analysis did not include any studies that were not published in English-language journals.
Furthermore, while strict retrieval strategies and inclusion and exclusion criteria were developed in this study, the following limitations must be acknowledged: (1) due to the lack of relevant research data, only the survival data from 38 original studies could be used for the meta-analysis, which may have reduced the statistical power of the study results; (2) the included literature was all from the PubMed, Embase or Web of Science databases, and all the relevant literature could not be collected; (3) the 38 included studies mostly used intermediate indicators (e.g., age, education level and income level) to observe the risk factors of frailty in patients with COPD and lacked specific hard-end points, such as the quality of the life score, mortality and other clinically relevant long-term follow-up outcomes, while they also did not determine the long-term risk factors.
Conclusion
This systematic review and meta-analysis revealed that frailty substantially (36%) coexists with COPD. Older age, low socioeconomic status, poorer respiratory performance, a high number of comorbidities, exacerbations and drugs used, smoking, depression, poorer physical performance, malnutrition, a high number of hospitalizations and low social support are associated with the increased prevalence of frailty among patients with COPD. However, given the high heterogeneity among the included studies, which could have undermined the robustness of the results, further higher quality studies with a larger sample size must be conducted to validate the results.
Data availability
All data generated or analyzed during this study are included in this published article.
References
Proietti M, Cesari M (2021) Describing the relationship between atrial fibrillation and frailty: clinical implications and open research questions. Exp Gerontol 152:111455. https://doi.org/10.1016/j.exger.2021.111455
Zhang Y (2021) Prediction model of fattening in elderly inpatients with cardiovascular disease based on decision tree. Shantou University
Zheng JR, Yang SL (2020) Minnan region of Fujian province present endowment the elderly quality of life that occupy the home under the weak condition. J Occup Health 4(19):2669–2672
Zhao J, Ding JH, Wei LZ et al (2022) Cluster analysis of self-management types and characteristics in elderly patients with COPD. J Nurs 37(3):88–92
Antoniu SA, Boiculese LV, Prunoiu V (2021) Frailty, a dimension of impaired functional status in advanced COPD: utility and clinical applicability. Medicina (Kaunas) 57(5):474
Gephine S, Mucci P, Grosbois JM et al (2021) Physical frailty in COPD patients with chronic respiratory failure. Int J Chron Obstruct Pulmon Dis 16:1381–1392
Dias LS, Ferreira ACG, da Silva Junior JLR et al (2020) Prevalence of frailty and evaluation of associated variables among COPD patients. Int J Chron Obstruct Pulmon Dis 15:1349–1356
Veronese N, Sigeirsdottir K, Eiriksdottir G et al (2017) Frailty and risk of cardiovascular diseases in older persons: the age, gene/environment susceptibility-Reykjavik study. Rejuvenation Res 20(6):517–524. https://doi.org/10.1089/rej.2016.1905
Marengoni A, Vetrano DL, Manes-Gravina E et al (2018) The relationship between COPD and frailty: a systematic review and meta-analysis of observational studies. Chest 154(1):21–40
Rabe KF, Watz H (2017) Chronic obstructive pulmonary disease. Lancet 389(10082):1931–1940
Collins PF, Yang IA, Chang YC et al (2019) Nutritional support in chronic obstructive pulmonary disease (COPD): an evidence update. J Thorac Dis 11(Suppl 17):S2230–S2237
Lee SY, Nyunt MSZ, Gao Q et al (2022) Co-occurrence of physical frailty and COPD and association with disability and mortality: singapore longitudinal ageing study. Chest 161(5):1225–1238. https://doi.org/10.1016/j.chest.2021.12.633
Koons B, Greenland JR, Diamond JM et al (2020) Pathobiology of frailty in lung disease. Transl Res 221:1–22
Halpin DMG, Criner GJ, Papi A et al (2021) Global initiative for the diagnosis, management, and prevention of chronic obstructive lung disease. The 2020 GOLD science committee report on COVID-19 and chronic obstructive pulmonary disease. Am J Respir Crit Care Med 203(1):24–36
Morley JE, Vellas B, van Kan GA et al (2013) Frailty consensus: a call to action. J Am Med Dir Assoc 14(6):392–397
Yu J-Y (2019) Preliminary construction of a risk prediction model for frailty and pre-frailty in older adults in Chengdu community. Chengdu University of Traditional Chinese Medicine
Bernabeu-Mora R, Oliveira-Sousa SL, Sánchez-Martínez MP et al (2020) Frailty transitions and associated clinical outcomes in patients with stable COPD: a longitudinal study. PLoS One 15(4):e0230116
Xu Y, Jia Y, Zhang Q et al (2021) Prevalence and risk factors for postoperative venous thromboembolism in patients with ovarian cancer: Systematic review and meta-analysis. Gynecol Oncol 160(2):610–618
Ter Beek L, van der Vaart H, Wempe JB et al (2020) Coexistence of malnutrition, frailty, physical frailty and disability in patients with COPD starting a pulmonary rehabilitation program. Clin Nutr 39(8):2557–2563
Weng S, Wang W, Wei Q et al (2019) Effect of tranexamic acid in patients with traumatic brain injury: a systematic review and meta-analysis. World Neurosurg 123:128–135. https://doi.org/10.1016/j.wneu.2018.11.214
Bozkurt C, Yildirim Y, Senuzun AF (2021) The effect of frailty level on acceptance of illness in older people with chronic obstructive pulmonary disease. Turk J Geriatr 4(2):244–254
Kagiali S, Inal-Ince D, Cakmak A et al (2022) Daily living activities, exercise capacity, cognition, and balance in COPD patients with and without frailty. Ir J Med Sci 191(2):817–824
Luo J, Zhang D, Tang W et al (2021) Impact of frailty on the risk of exacerbations and all-cause mortality in elderly patients with stable chronic obstructive pulmonary disease. Clin Interv Aging 16:593–601
Naval E, González MC, Giraldós S, Calatayud J, Jornet M, Lluch I, Meseguer M, Cubillan JJR, Viña J, Tarazona-Santabalbina FJ (2021) Frailty Assessment in a stable COPD cohort: is there a COPD-frail phenotype? COPD 18(5):525–532
Nishimura K, Nakayasu K, Mori M et al (2021) Are fatigue and pain overlooked in subjects with stable chronic obstructive pulmonary disease? Diagnostics (Basel) 11(11):2029
Park SK (2021) Frailty in Korean patients with chronic obstructive pulmonary disease, using data from the Korea national health and nutrition examination survey, 2015 and 2016. Appl Nurs Res 59:151417
Takahashi S, Hirano T, Yasuda K et al (2021) Impact of frailty on hippocampal volume in patients with chronic obstructive pulmonary disease. Biomedicines 9(9):1103
Witt LJ, Spacht WA, Carey KA et al (2021) Weak handgrip at index admission for acute exacerbation of COPD predicts all-cause 30-day readmission. Front Med (Lausanne) 8:611989
Chin M, Voduc N, Huang S et al (2020) Practical lessons in implementing frailty assessments for hospitalised patients with COPD. BMJ Open Qual 9(1):e000782
Oishi K, Matsunaga K, Harada M et al (2020) A new dyspnea evaluation system focusing on patients’ perceptions of dyspnea and their living disabilities: the linkage between COPD and frailty. J Clin Med 9(11):3580
Talay MB, Tas GS, Birtekocak F et al (2020) Factors affecting frailty syndrome in elderly chronic obstructive pulmonary disease patients and its relationship with systemic inflammation. Turk J Geriatr 23(4):446–454
Ierodiakonou D, Kampouraki M, Poulonirakis I et al (2019) Determinants of frailty in primary care patients with COPD: the Greek UNLOCK study. BMC Pulm Med 19(1):63
Chen PJ, Yang KY, Perng WC et al (2018) Effect of dyspnea on frailty stages and related factors in Taiwanese men with COPD. Int J Chron Obstruct Pulmon Dis 13:2463–2469
Gale NS, Albarrati AM, Munnery MM et al (2018) Frailty: a global measure of the multisystem impact of COPD. Chron Respir Dis 15(4):347–355
Medina-Mirapeix F, Bernabeu-Mora R, Giménez-Giménez LM et al (2018) Physical frailty characteristics have a differential impact on symptoms as measured by the CAT score: an observational study. Health Qual Life Outcomes 16(1):140
Kusunose M, Oga T, Nakamura S et al (2017) Frailty and patient-reported outcomes in subjects with chronic obstructive pulmonary disease: are they independent entities? BMJ Open Respir Res 4(1):e000196
Limpawattana P, Putraveephong S, Inthasuwan P et al (2017) Frailty syndrome in ambulatory patients with COPD. Int J Chron Obstruct Pulmon Dis 12:1193–1198
Mittal N, Raj R, Islam EA et al (2016) The frequency of frailty in ambulatory patients with chronic lung diseases. J Prim Care Community Health 7(1):10–15
Valenza MC, Torres-Sánchez I, Cabrera-Martos I et al (2016) Physical activity as a predictor of absence of frailty in subjects with stable COPD and COPD exacerbation. Respir Care 61(2):212–219
Park SK, Richardson CR, Holleman RG et al (2013) Frailty in people with COPD, using the national health and nutrition evaluation survey dataset (2003–2006). Heart Lung 42(3):163–170
Galizia G, Cacciatore F, Testa G, Della-Morte D, Mazzella F, Langellotto A, Raucci C, Gargiulo G, Ferrara N, Rengo F, Abete P (2011) Role of clinical frailty on long-term mortality of elderly subjects with and without chronic obstructive pulmonary disease. Aging Clin Exp Res 23(2):118–125. https://doi.org/10.1007/BF03351076. (PMID: 21743290)
Hanlon P, Lewsey J, Quint JK et al (2022) Frailty in COPD: an analysis of prevalence and clinical impact using UK Biobank. BMJ Open Respir Res 9(1):e001314
Zhang D, Tang W, Dou LY et al (2022) Four different frailty models predict health outcomes in older patients with stable chronic obstructive pulmonary disease. BMC Geriatr 22(1):57
Scarlata S, Finamore P, Laudisio A et al (2021) Association between frailty index, lung function, and major clinical determinants in chronic obstructive pulmonary disease. Aging Clin Exp Res 33(8):2165–2173
Yee N, Locke ER, Pike KC et al (2020) Frailty in chronic obstructive pulmonary disease and risk of exacerbations and hospitalizations. Int J Chron Obstruct Pulmon Dis 15:1967–1976
Ehsani H, Mohler MJ, Golden T et al (2018) Upper-extremity function prospectively predicts adverse discharge and all-cause COPD readmissions: a pilot study. Int J Chron Obstruct Pulmon Dis 14:39–49
Bernabeu-Mora R, García-Guillamón G, Valera-Novella E et al (2017) Frailty is a predictive factor of readmission within 90 days of hospitalization for acute exacerbations of chronic obstructive pulmonary disease: a longitudinal study. Ther Adv Respir Dis 11(10):383–392
Medina-Mirapeix F, Bernabeu-Mora R, García-Guillamón G et al (2016) Patterns, trajectories, and predictors of functional decline after hospitalization for acute exacerbations in men with moderate to severe chronic obstructive pulmonary disease: a longitudinal study. PLoS One 11(6):e0157377
Roberts MH, Mapel DW, Ganvir N et al (2022) Frailty among older individuals with and without COPD: a cohort study of prevalence and association with adverse outcomes. Int J Chron Obstruct Pulmon Dis 17:701–717
Kennedy CC, Novotny PJ, LeBrasseur NK et al (2019) Frailty and clinical outcomes in chronic obstructive pulmonary disease. Ann Am Thorac Soc 16(2):217–224
Ushida K, Shimizu A, Hori S, Yamamoto Y, Momosaki R (2022) Hospital frailty risk score predicts outcomes in chronic obstructive pulmonary disease exacerbations. Arch Gerontol Geriatr 100:104658 (published correction appears in Arch Gerontol Geriatr. 2022 Jul 21;103:104780)
Maddocks M, Kon SS, Canavan JL et al (2016) Physical frailty and pulmonary rehabilitation in COPD: a prospective cohort study. Thorax 71(11):988–995
Lahousse L, Ziere G, Verlinden VJ et al (2016) Risk of frailty in elderly With COPD: a population-based study. J Gerontol A Biol Sci Med Sci 71(5):689–695
Kojima G, Iliffe S, Walters K (2015) Smoking as a predictor of frailty: a systematic review. BMC Geriatr 15(1):131
Finamore P, Scarlata S, Delussu AS et al (2021) Frailty impact during and after pulmonary rehabilitation. COPD 18(5):518–524
Wang Z, Hu X, Dai Q (2020) Is it possible to reverse frailty in patients with chronic obstructive pulmonary disease? Clinics (Sao Paulo) 75:e1778
Jingxue P, Liqun C, Jingli W et al (2021) Investigation on cognitive function of elderly patients with chronic diseases in community. Chin J Nurs 56(01):109–115
Xiaolin H, Jing G, Chenxi W et al (2018) Current status and analysis of frailty in elderly people in nursing institutions. Chin J Nurs 53(1):88–93
Provinciali M, Cardelli M, Marchegiani F (2011) Inflammation, chronic obstructive pulmonary disease and aging. Curr Opin Pulm Med 17(Suppl 1):S3-10
Barriga S, Rodrigues F, Bárbara C (2014) Factors that influence physical activity in the daily life of male patients with chronic obstructive pulmonary disease. Rev Port Pneumol 20(3):131–137
Tanabe N, Sato S (2021) Narrative review of current COPD status in Japan. J Thorac Dis 13(6):3878–3887
Brighton LJ, Evans CJ, Farquhar M et al (2021) Integrating comprehensive geriatric assessment for people with COPD and frailty starting pulmonary rehabilitation: the Breathe Plus feasibility trial protocol. ERJ Open Res 7(1):00717–02020
Liao CD, Chen HC, Huang SW et al (2019) The role of muscle mass gain following protein supplementation plus exercise therapy in older adults with sarcopenia and frailty risks: a systematic review and meta-regression analysis of randomized trials. Nutrients 11(8):1713
Angulo J, El Assar M, Álvarez-Bustos A et al (2020) Physical activity and exercise: strategies to manage frailty. Redox Biol 35:101513
Jyrkkä J, Enlund H, Korhonen MJ, Sulkava R, Hartikainen S (2009) Patterns of drug use and factors associated with polypharmacy and excessive polypharmacy in elderly persons. Drugs Aging 26(6):493–503
Mangoni AA, Jackson SH (2004) Age-related changes in pharmacokinetics and pharmacodynamics: basic principles and practical applications. Br J Clin Pharmacol 57(1):6–14
Ali B, Choi EE, Barlas V et al (2022) Modified Frailty Index (mFI) predicts 30-day complications after microsurgical breast reconstruction. J Plast Surg Hand Surg 56(4):229–235
Naharci MI, Tasci I (2020) Frailty status and increased risk for falls: The role of anticholinergic burden. Arch Gerontol Geriatr 90:104136
Atassi M, Kavav ACF, Nejjari C et al (2020) Association between chronic airflow obstruction and socio-economic position in Morocco: BOLD results. Int J Tuberc Lung Dis 24(2):202–206
Funding
Key R & D projects in Ningxia Hui Autonomous Region (No.2021BEG03116) and The General Hospital of Ningxia Medical University “new master training” and Ningxia Medical University university-level project (MX2022055).
Author information
Authors and Affiliations
Contributions
Conception and design of the research: H-YL and L-CY. Acquisition of data: L-CY, X-YW, and GX. Analysis and interpretation of the data: X-YW, YC, and PY. Statistical analysis: L-CY, GX, H-YL, PY, and BW. Obtaining financing: none. Writing of the manuscript: L-CY and H-YL. Critical revision of the manuscript for intellectual content: H-YL.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflicts of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yan, LC., Lu, HY., Wang, XY. et al. Prevalence and risk factors of frailty in patients with chronic obstructive pulmonary disease: systematic review and meta-analysis. Eur Geriatr Med 14, 789–802 (2023). https://doi.org/10.1007/s41999-023-00800-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41999-023-00800-2