Key summary points
To summarise the existing knowledge on fall risk associated with benzodiazepines (BZDs) and Z-drugs in older people with focus on appropriate prescribing, including deprescribing.
AbstractSection FindingsDifferent mechanisms contribute to increased BZD/Z-drug-related fall risk: orthostatic hypotension, dizziness and/or imbalance, sedation, muscular weakness, ataxia, etc. BZDs and Z-drugs have shown their effectiveness for the short-term symptomatic treatment of insomnia and anxiety in older people. However, prolonged use has been associated with several adverse effects, whereby the risks outweigh the benefits. Different strategies are described to increase the appropriate use of BZDs and Z-drugs including deprescribing initiatives.
AbstractSection MessageBZDs and Z-drugs should be used with caution in older people. A multifaceted approach including non-pharmacological interventions, comprehensive medication reviews, shared decision-making and close interprofessional communication and collaboration is warranted.
Abstract
Purpose
The aim of this clinical review was to summarise the existing knowledge on fall risk associated with benzodiazepines (BZDs) and Z-drugs in older people with focus on appropriate prescribing, including deprescribing.
Methods
We conducted a literature search in June 2021 in PubMed and Embase with citation and reference checking. Personal reference libraries and international websites were also used. Keywords for the searches included “benzodiazepines”, “Z-drugs”, “falls”, “deprescribing”, “fall-risk-increasing-drugs”, “inappropriate prescribing”, “older people” and matching synonyms. We discuss use of BZDs and Z-drugs, potential fall-related adverse reactions, alternatives for and deprescribing of BZDs and Z-drugs in older persons.
Results
BZDs and Z-drugs differ in fall-related adverse effect profile. They contribute to fall risk through orthostatic hypotension, dizziness and/or imbalance, sedation, muscular weakness, ataxia, etc. Fall incidents contribute significantly to mortality and morbidity. Therefore, there is a need for appropriate prescribing and use of BZDs and Z-drugs in older people. In practice, this means pertaining to a strict indication, strongly consider to non-pharmacological alternatives, limit use to the lowest dose and the shortest duration possible. Judicious deprescribing should be considered and encouraged as well. Practical resources, tools and algorithms are available to guide and assist clinicians in deprescribing BZDs and Z-drugs.
Conclusions
Prescribing BZDs and Z-drugs should be done in a well-considered way in fall-prone older people. A good overview and insight in the fall-related adverse effects of these drugs, as well as the availability of different strategies to increase the appropriate use, including deprescribing initiatives, can assist clinicians in clinical decision-making.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Falls are, after road traffic injuries, the second leading cause of injury-related deaths worldwide. Each year, an estimated number of 684,000 individuals die from injurious falls globally [1]. Older age is one of the key risk factors for falls and falls and fall-related injuries are a common problem in older people. In Western Europe, 54,504 older adults died due to falls in 2017. However, death rates varied widely between countries (from 29 to 153 per 100 000) [2]. About one-third of older people (≥ 65 years) fall at least once a year, and this occurs even more frequently in the very old (≥ 80 years), frail and institutionalised patients [3, 4]. Fall incidents in older people are often associated with serious injuries, such as fractures, increased rate of emergency department visits and hospital admissions, leading to increased healthcare expenditures. In addition, falls may lead to loss of independence, loss of self-confidence, increased risk of institutionalisation and decreased quality of life [3, 5].
A multifactorial falls risk assessment is required to identify the individual modifiable risk factors as they may differ between patients [5]. One of the most prominent and also modifiable risk factors is the use of fall-risk-increasing drugs (FRIDs) [6,7,8]. Fall prevention guidelines recommend performing a medication review to identify the inappropriate use of FRIDs as part of the multifactorial fall prevention strategy [7]. Until recently, there was no consensus about which medications are to be considered as FRIDs. In 2020, a European expert group developed the STOPPFall tool, an explicit screening tool and deprescribing aid in older adults with high fall risk. This tool was created using an expert Delphi consensus process and consists of 14 medication classes [8].
Psychotropic medications, and especially benzodiazepines (BZDs) and Z-drugs (zolpidem, zopiclone, zaleplon), have consistently been reported to increase the risk of falls [6]. A systematic review and meta-analysis by Seppala et al. showed an odds ratio (OR) of 1.42 for BZD-related fall risk [6]. Psychotropic drugs are widely used in older people, both in primary and secondary care [9,10,11]. BZDs and the related Z-drugs are among the world’s most widely prescribed psychotropic drugs in older people. The use of these drugs among community-dwelling older people shows a large variability, ranging from 13.8% to 25.4% in international studies in individual countries, depending on the methodology used. The prevalence is especially high among institutionalised older people [12]. Importantly, their use is associated with multiple potential adverse effects to which older people are more vulnerable due to age-related changes in pharmacodynamics and pharmacokinetics, multimorbidity and drug–drug interactions related to polypharmacy. For example, the altered pharmacodynamics of the ageing brain leads to higher sensitivity to centrally acting agents.
Allosterically binding of BZDs and Z-drugs to the gamma-amino butyric acid (GABA)–benzodiazepine receptor/ion channel complex modulates its activity and thus facilitates GABA-ergic neurotransmission. The GABA–benzodiazepine receptor complex consists of 5 subunits (2 α, 2 β and 1 γ subunits). Each receptor has several isoforms of these subunits. Depending on the affinity of the BZDs for the different isoforms, they have a different pharmacological effect, as schematically illustrated by Griffin et al. and Cheng et al. [13, 14]. For example, a BZD that has a high affinity for the α2 subunit will have anxiolytic effects. A BZD with a high affinity for the α1 subunit is more likely to cause sedation, amnesia, and antiepileptic effects [13]. There are two central receptors (BZ1 and BZ2) and one peripheral receptor. BZ1 receptors, containing the α1 isoform, are predominantly located in the cerebellum, mediating the anxiolytic and hypnosedative actions. BZ2 receptors, containing the α2 subunit, are located predominantly in the spinal cord and striatum and are involved in mediating the muscle relaxant actions of BZDs. Zolpidem and zaleplon, in contrast to most BZDs and zopiclone, have a high selectivity for the BZ1 receptor. They both exhibit sedative effects similar to those of the BZDs, but with a lower probability of undesirable side effects as memory loss and abuse potential [13, 15].
BZDs and Z-drugs are only indicated for the short-term pharmacological management of acute insomnia and for severe and disabling anxiety, the latter as an alternative for selective serotonin reuptake inhibitors (SSRIs) [9, 15]. In older people, about 20–58% suffer from insomnia and the prevalence increases with age [16]. This partially explains the wide use of these drugs in this population. However, the benefits are only marginal and adverse reactions are common. Importantly, the effectiveness on sleep quality diminishes after 4 weeks, while adverse effects persist [17]. A meta-analysis performed by Glass and colleagues revealed that the number needed to harm (i.e., for any adverse reaction) was only six. They concluded that the risks of short-term treatment with BZDs and Z-drugs in older people with insomnia outweigh the potential benefits, especially in patients with high risk for falls [18].
Given the potentially harmful consequences of BZD and Z-drug use, such as falls, there is need for appropriate prescribing and use in older people: pertaining to a strict indication, attention to non-pharmacological alternatives, limitation to the lowest dose and the shortest duration of use possible. Judicious deprescribing should be considered and encouraged as well [19]. It has been reported that deprescribing can be performed safely in older people. To support healthcare professionals in their decision making, the European Geriatric Medicine Society (EuGMS) Task and Finish Group on FRIDs developed a practical deprescribing tool, including FRID drug class specific deprescribing recommendations [7].
In this clinical review, an overview of the current literature regarding use of BZDs and Z-drugs, their fall-related adverse reactions and deprescribing recommendations is provided. This clinical review was informed by a literature search conducted in June 2021 in PubMed and Embase with citation and reference checking. Personal reference libraries and international websites were also used. Keywords for the searches included “benzodiazepines”, “Z-drugs”, “falls”, “deprescribing”, “FRIDs”, “inappropriate prescribing”, “older people” and matching synonyms.
Fall-related adverse effects of benzodiazepines and Z-drugs
Different risk factors contribute to a higher fall-risk, as illustrated in Fig. 1. These factors can be categorised in age-, disease- and drug-related risk factors. Some risk factors are unmodifiable (demographics, diseases), others are potentially modifiable (health and functional conditions, including FRIDs) and should, therefore, be targeted. BZDs and Z-drugs (drug-related risk factor) are associated with falls [4, 6,7,8, 20, 21], but the underlying reasons for prescribing them (insomnia and anxiety) are also associated with increased fall risk [22]. Therefore, we should be aware for possible confounding by indication in studies addressing the association between use of FRID and fall risk. Three meta-analyses exploring the association between drug use and falls in older people have reported concordant results, with pooled OR for the association between BZDs use and falls ranging from 1.39 (95% confidence interval (CI) 1.24–1.54) to 1.57 (95% CI 1.43–1.72) [23]. BZDs are also strongly associated with hip fractures [18, 24], where approximately one-third of patients with a hip fracture die within a year. Even when falls do not result in fractures, they are associated with fear of subsequent falls, limitation of activities of daily living and consequently decreased quality of life [24]. Z-drugs are often perceived as safer than BZDs. However, use of Z-drugs is also associated with a statistically significant increased risk for fractures (OR = 1.63, 95% CI 1.42–1.87) [25].
Different characteristics of BZDs and Z-drugs may contribute to the risk of falls, such as the elimination half-life, dose and exposure duration. BZDs and Z-drugs are often classified into groups according to elimination half-life (Table 1): long-acting agents (half-life > 20 h), such as diazepam, flurazepam, and nitrazepam; intermediate acting agents (half-life between 10 and 20 h), such as lorazepam, bromazepam, and alprazolam; and short-acting agents (half-life < 10 h), such as lormetazepam, oxazepam and zolpidem [26]. Short-acting BZDs were positively associated with falls during hospital stays in contrast to long-acting BZDs [27, 28]. This is in line with other studies in which the use of short-acting BZDs or Z-drugs was significantly associated with frequent falls [20, 29,30,31]. In contrast, a prospective cohort study demonstrated that patients using long-acting diazepam were over three times more likely to have a fall in the previous 90 days compared with non-users and all other BZD users. Zolpidem significantly increased the risk of inpatient falls [32]. A possible mechanism to account for the differences in falls risk between different BZDs may include age-related changes in pharmacokinetics and pharmacodynamics in older people which may increase the risk for adverse outcomes caused by BZDs. The changes in pharmacokinetics include changes in body composition, serum albumin, total body water, and hepatic and renal functions [33]. Body fat increases and this can affect the distribution of lipophilic drugs, such as diazepam. Changes in activity of cytochrome P450 (CYP) enzymes, as well as a decrease in albumin plasma levels influence the free fractions of BZDs [34]. Studies reported also an effect on the dose strength on fall risk. BZDs doses > 1 mg/day in diazepam equivalents was significantly associated with falls among hospitalised older people. Accidental falls leading to hospitalisation for femur fractures were more common in patients taking higher doses of BZDs [31, 35]. The study by Ballokova et al., however, did not identify any significant relationship between a history of falls and different doses of BZDs [34]. But, we have to acknowledge the limitation that these self-reported data on past falls may have been biased due to retrospective recall, which would more likely lead to under-estimation rather than over-estimation. Conversely, in a population-based study, Yu et al. observed that all dose levels of BZDs and high dose levels of Z-drugs significantly increased the risk of fall-related injuries requiring hospitalisation [20]. This was also confirmed in a study among nursing home residents with dementia. Higher fall risk was already present at low doses and increased further with increasing doses [36]. There might be a dose-dependent relationship, but this needs further investigation. Studies have also evaluated the association between duration of BZDs use and falls. Some studies demonstrated that the risk of falls is higher in the first weeks after BZD treatment initiation [21, 37,38,39,40] as well as with long-term use (> 28 days) [40]. The study of Carrier et al. showed that occasional BZDs use was not associated with increased risk of fall-related fractures. Chronic BZD users had a higher risk of fractures than non-users [21]. However, polypharmacy and the use of multiple types of BZDs and/or Z-drugs or other psychotropics significantly increased the risk of falls [20]. Altogether, it is important to remind the patient that the treatment duration must be limited in time (e.g., < 4 weeks). Therefore, is it useful to indicate a tentative stop date already at initiation of the treatment.
The therapeutic window for sedative and anxiolytic effects of BZDs and Z-drugs is narrow, and these drugs increase the risk of falls by inducing different mechanisms: sedation and delirium, (orthostatic) hypotension (OH) and dizziness, movement disorders (muscular weakness, extrapyramidal symptoms) and visual disorders [21, 24, 41, 42]. The adverse reaction profile and tolerability is different between BZDs and Z-drugs, but there are also differences within these two classes (Table 2). In clinical practice, selecting a BZD or Z-drug in older people should be individualised, taking into account the adverse reaction profile and tolerability of the drug and patient characteristics. In the following paragraphs, a summary of the literature is provided on effects that might contribute to fall risk caused by BZDs and Z-drugs.
Sedation (drowsiness, sleepiness or somnolence)
Sedation is defined as subjective feelings of drowsiness and sleepiness, but also as decreased psychomotor functioning, which can be measured in objective tests [43]. In a meta-analysis of 8 studies, BZDs were more likely than placebo to be associated with complaints of daytime drowsiness [9]. Long-acting BZDs are associated with significant daytime hangover effect, confusion, dizziness, impaired motor coordination, increased risk of falls resulting in fractures, and increased risk of motor vehicle crashes [44]. Sleep inertia, also referred to as sleep drunkenness, is characterised by impaired performance upon awakening from sleep. Such impairments may have implications for fall risk [22]. This can be explained by the decreased metabolism of long-acting BZDs in older people [24] but also by the age-related changes in pharmacodynamics (decreased number of synapses in the brain and their binding function and downward receptor signalling, etc. [45].
Delirium
BZDs are known to worsen delirium states, especially in older people. The reported prevalence of delirium among older hospitalised patients ranges from 14% to 56%, and almost one-third appeared to be drug-induced [41]. On the other hand, we have to keep in mind, once again, that confounding by indication could be present as BZDs also have their place in treatment guidelines of delirium and acute agitation. The updated Beers [46] and STOPP/START [47] criteria for potentially inappropriate medication use in older people, strongly advise against prolonged BZDs in older people due to increased risk of confusion, delirium, falls, fractures, and motor vehicle crashes.
Effects on balance
BZDs and Z-drugs exhibit a dose and time-dependent deleterious effect on stability and balance [48]. As balance forms a major fall-risk factor, this supports the hypothesis that balance is the major pathophysiological pathway for BZDs-related fall risk [49]. The effect of BZDs and Z-drugs on balance is most prominent within the first few hours after intake. The impact on balance is more pronounced with higher doses, a shorter time between intake and waking up, or after concomitant use with alcohol or other sedative drugs [50]. Holbrook et al. found a significant increase in adverse events with BZD use. The increase in psychomotor-type adverse reactions found with sedative use in the study of Glass et al. (OR 2.61) is similar to the increase in reports of dizziness and light-headedness found in the Holbrook meta-analysis after BZD use (OR 2.6, 0.7 to 10.3) [9, 18]. Zolpidem binds preferentially with the γ5 subunit of the BZ1 receptor as an agonist and does not interfere with muscle coordination (BZ2 effect). Zolpidem is also rapid metabolised via CYP3A4 and CYP2C9, resulting in negligible (if any) residual effects even 9 h after intake. Since zolpidem is renally cleared and renal function is reduced in many older people, peak concentrations can be increased [48]. In the same way as for BZD, a trend toward greater fall risk in the early treatment period and with increasing doses has been shown for Z-drugs [49].
Effects on orthostatic hypotension and postural instability
OH is defined as a reduction in SBP of at least 20 mmHg or DBP of at least 10 mmHg within 3 min of standing up from the supine position, or a similar fall in blood pressure within 3 min of upright tilt table testing to at least 60 degrees [51]. There is an increase in OH prevalence from 15% to 26% with advancing age resulting in more falls, partly due to a decline in autonomic functioning. Aging is also associated with generalised neuronal loss, fewer beta receptors with decreased functionality and a weaker response to catecholamines—all of which are factors contributing to the development of OH [52]. Orthostatic hypotension may play a role in the association between BZDs and falls, since cerebral hypoperfusion may occur, leading to unbalance, gait instability or even transient loss of consciousness. The study by Rivasi et al. suggests that older people using BZDs have a higher risk of OH due to an exaggerated immediate (within the first 10 s post-stand) blood pressure drop. The association between BDZs and the immediate blood pressure drop derives from increased venous pooling due to muscular relaxation. Another possible hypothesis includes possible sympathetic hypo-responsiveness resulting from regular use of BZDs [53]. Long-term use of BZDs and Z-drugs was associated with lower DBP and SBP in older, but not in younger, individuals [49]. Postural instability is more pronounced in older patients after BZD administration than in the young. The effect on postural instability is dose-dependent and apparent for BZDs and Z-drugs, but not to the same degree, and depending on the differences in pharmacokinetics (half-life) and affinity for the subtypes of the BZD receptor, GABAA [48].
Effect on cognition
The acute cognitive effects of BZDs are well known. They can cause short-term cognitive deficits, especially in memory, learning and attention [54]. In addition, some observational studies demonstrated an association between BZDs use and dementia [55, 56]. The association between BZD use and cognitive outcomes can be partially explained by the binding of those molecules to the α5 subunit of the BZD receptor in the hippocampus [56]. However, the impact of long-term use of BZDs on cognitive impairment and/or cognitive decline remains unclear and the existing evidence is ambiguous [57]: some evidence indicates an accelerated rate of cognitive decline [58], while other evidence indicates that cognitive decline is transient [59]. The recent review of Ferreira et al. suggests an association between BZDs and the development of dementia, especially for agents with long half-life, extended use (the use of a BZD and Z-drug for 6 months or longer during a time period of 1 year regardless of whether the use was daily or infrequent) and earlier exposure (previous initiation of a BZD or Z-drug) [56, 57, 60]. It also seems that, after withdrawal of BZDs, patients recover in many domains of cognitive function, but still remain impaired compared with non-BZD users [61]. Furthermore, even after BZDs are discontinued, the cognitive function of long-term users is reported to remain impaired in most cognitive domains, suggesting possibly irreversible cognitive deficits associated with BZDs use [24]. However, there is need for future studies with proper design to answer this research question.
Alternatives for benzodiazepines and Z-drugs
BZDs and the related Z-drugs have shown their effectiveness for the symptomatic short-term treatment of insomnia and anxiety in older people [9, 18]. However, as discussed above, the prolonged use has been associated with several adverse effects, whereby the risks outweigh the benefits [18]. In contrast, the benefits of BZDs fade after 4 weeks of use. As a consequence, these medication classes have been included in different explicit criteria for the identification of potentially inappropriate medications (PIMs) in older people [47, 62, 63]. These expert consensus criteria strongly advise against the use of BZDs in older people, especially when used longer than 4 weeks [47, 62, 63]. Explicit criteria and tools are commonly used within the scope of a medication review to identify PIMs use and to prevent, detect and help solving drug-related problems.
An important first step in the management of sleep complaints in older adults is to perform a comprehensive medication review as different drug classes can contribute to insomnia. Examples of insomnia contributing medications are cardiovascular medications (alpha- and beta-blockers, amiodarone, calcium channel blockers, etc.), antidepressants (SSRIs, serotonin–norepinephrine reuptake inhibitors (SNRIs), monoamine oxidase inhibitors), acetylcholinesterase inhibitors, corticosteroids and antimicrobial agents [64, 65]. If treatment is required, a non-pharmacological approach should always be considered first, including relaxation techniques, improving sleep hygiene, and cognitive behavioural therapy for insomnia (CBT-I), such as psychoeducation. Sleep hygiene includes, for example, avoiding daytime naps and limiting substances (such as caffeinated drinks) that adversely affect sleep. CBT-I is the gold standard treatment for chronic insomnia and has demonstrated efficacy in older adults [66,67,68]. CBT-I focusses on cognitive beliefs and counterproductive behaviours that interfere with sleep. A clinical review by Riemann and colleagues compared the effectiveness of pharmacological treatment with BZDs and psychological and/or behavioural interventions. They conclude that both BZDs hypnotics and psychological interventions are effective to treat insomnia in the short-term (for primary insomnia) but that psychological interventions may be superior for sleep initiation. Moreover, these psychological/behavioural interventions appear to have more durable effects with persistent gains at follow-up, up to 8 months [65, 69]. Another non-pharmacological approach is sleep restriction (restricting the time in bed to the actual sleeping time) [70].
Frequently, melatonin is prescribed as an alternative for BZDs for the treatment of insomnia [71]. Melatonin is a physiological indole amine that modulates circadian rhythms. Melatonin slightly improves sleep onset and sleep duration although the evidence remains inconclusive [72,73,74]. However, there are concerns about product quality and efficacy which may vary depending on the preparation [64].
Also, for the management of anxiety disorders, a non-pharmacological approach should be considered first. It has been demonstrated that CBT-I substantially reduces worrying and depressive symptoms and improves the general mental health in older patients [75, 76]. If pharmacological treatment is indicated, not BZDs but SSRIs and SNRIs are first choice. These medications have showed positive effects relative to placebo for the treatment of anxiety in older people [77].
Furthermore, if BZD treatment is indicated, it is important to sufficiently inform patients and their carers about the benefit–risk ratio and to discuss both the potential benefits and potential harms.
Deprescribing of benzodiazepines and Z-drugs
When BZDs and/or Z-drugs are not (longer) indicated, they should be discontinued. However, to avoid the withdrawal syndrome with worsening of insomnia or anxiety symptoms, a gradual reduction is required, as described below. Other common withdrawal symptoms are irritability, restlessness, sweating, headache, muscle cramps, gastrointestinal symptoms, delirium or convulsions [15, 17]. Most often, withdrawal symptoms occur after 12 weeks of habitual use, but tapering is already advised after 4 weeks [17]. Tapering will reduce, but might not eliminate, withdrawal symptoms. Deprescribing is defined as “the withdrawal of an inappropriate medication, supervised by a healthcare professional with the goal of managing polypharmacy and improving outcomes” [78] or “the planned and supervised process of dose reduction or stopping of medication that might be causing harm or no longer providing benefit” [17]. The aim of deprescribing is to reduce medication burden and harm while maintaining or improving patients’ quality of life. Numerous interventions have been proposed to support deprescribing of BZDs and Z-drugs. However, those strategies are often diverse and/or reported poorly detailed [79]. Deprescribing is challenging, because patients and physicians are often reluctant out of fear for the potential risk of the withdrawal syndrome [80]. In addition, another important barrier for deprescribing, from the patient perspective, is the belief that an alternative effective treatment of their insomnia is lacking [81]. Patients’ personality profile, dose and half-live of BZDs and Z-drugs, duration of treatment and mode of withdrawal have been identified to affect withdrawal success rate [15]. On the other hand, important facilitators to discontinue BZDs are expected improvements in cognition and reductions in other adverse reactions [17].
A systematic review by Rasmussen and colleagues evaluated the barriers and facilitators of different stakeholders when deprescribing BZDs in older people [82]. Patients and physicians were most often targeted in interventions toward deprescribing of BZDs in older people, while relatives, pharmacists or other professional caregivers were often not involved [80, 82]. Remarkably, it was found that patients are willing to deprescribe their BZDs treatment, while doctors consider that patients will resist this [82]. Lack of knowledge, both physical and psychological dependence and patients’ confidence in their physician’s approval to continue BZDs treatment were the most important identified barriers in patients using BZDs. For Z-drugs, identified barriers were factors related to their insomnia (including need for effective treatment of their insomnia), healthcare system factors (including a desire for personalised care), and own positive personal experiences with Z-drugs [81]. Furthermore, nurses and caregivers mentioned the feeling that their options were not valued by physicians and are currently an unused source of support in the deprescribing process [82]. Challenges to deprescribe Z-drugs, from the clinician perspective, were a lack of institutional structures and resources to support deprescribing, the attitudes and practices of previous clinicians, and patient-related factors such as dependence and a lack of alternatives to treat insomnia [81].
In contrast to the general view, studies have shown that deprescribing of BZDs appears to be feasible and safe in older people [83,84,85,86]. Importantly, studies show comparable or better quality of life and sleep patterns after deprescribing BZDs [83]. In 2014, Tannenbaum et al. showed in the EMPOWER-trial that a deprescribing patient empowerment intervention describing the risk of BZDs use and using a stepwise tapering protocol, resulted in more dose reductions and higher discontinuation rates (27% of the intervention group had discontinued BZD use compared with 5% in the control group) [87]. Patients who did not taper BZD use, mentioned physician’s or pharmacist’s discouragement as the major impediment [87]. Therefore, the D-PRESCRIBE trial was conducted, where the intervention consisted of sending patients an educational deprescribing brochure in parallel to sending their physicians an evidence-based pharmaceutical opinion to recommend deprescribing. This approach yielded in greater discontinuation of prescriptions for PIMs after 6 months [88].
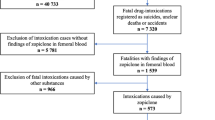
It remains unclear whether BZD and Z-drugs deprescribing, and FRID deprescribing in general, is effective as a stand-alone intervention in fall prevention [89]. Nevertheless, fall prevention guidelines emphasise the importance of FRID deprescribing as part of a multifactorial fall prevention strategy. And recently, medication review was confirmed to be an effective component of multifactorial fall preventive interventions in a network meta-analysis [7, 90]. The EuGMS Task and Finish Group on FRIDs developed deprescribing recommendations to facilitate optimal deprescribing in fall-prone older patients, including practical deprescribing decision-trees for 14 drug classes, including BZDs [8]. There is a digital and interactive version of the STOPPFall tool available via https://kik.amc.nl/falls/decision-tree/. Figure 2 displays the STOPPFall decision tree for BZD withdrawal in patients who have fallen. Specific for the withdrawal of BZDs, first of all, the indication of BZDs should be re-evaluated. If there is still an indication present, a safer alternative for BZDs or a dose reduction of BZDs should be considered. If the indication does not (longer) exist, BZD should be stopped in a stepwise manner, by tapering the dose gradually on. For example, a 25% reduction every 2 weeks with a 12.5% reduction near the end of the process. Alternatively, the BZD can be switched to a long-acting equivalent BZD (e.g., diazepam). Each schedule is best tailored to the patient's needs and preferences. To calculate the corresponding mg equivalent dosage of diazepam, an online query ‘CalcBenzo’ can be used http://wiki.psychiatrienet.nl/wiki/Special:RunQuery/CalcBenzo. However, this approach has not been shown to reduce the incidence of withdrawal symptoms or improve cessation rates more than tapering shorter acting BZDs does [17]. As discussed before, a tapering approach will reduce, but might not eliminate withdrawal symptoms. Therefore, during tapering or after withdrawal it is important to monitor patients for changes in symptoms (e.g., sedation, dizziness), fall incidents and anxiety, insomnia and agitation [8]. This monitoring should be planned on a regular basis, for example by a scheduled appointment or through a telephone call [17]. If withdrawal symptoms do occur and at a severity and frequency that is bothersome for the patient, a next dose reduction should be delayed with 1–2 weeks, where after the stepwise tapering can be continued, however, at a slower rate [17].
Decision tree for benzodiazepine (BZD) withdrawal in patients who have fallen [8]
Conclusions
Falls and fall-related injuries represent a common problem among older people. Psychotropic medications, and especially BZDs and Z-drugs, have consistently been reported to increase the risk of falls. This clinical review provides an overview of the current literature regarding BZD-related falls and the different fall-related adverse effects of BZDs in older people. The risk of falling is amplified by age, certain diseases and by use of BZDs and Z-drugs which explains why these drugs are considered as potentially inappropriate medications. In this paper, we provide clinicians with alternative treatment strategies, as well as different strategies to increase the appropriate use of BZDs including deprescribing initiatives.
Data availability
Data sharing not applicable to this review article as no datasets were generated or analysed during the current study.
References
World Health Organization. Fact sheet: Falls. 26 April 2021 [Accessed 31/08/2022; Available from: https://www.who.int/news-room/fact-sheets/detail/falls.
Haagsma JA, Olij BF, Majdan M et al (2020) Falls in older aged adults in 22 European countries: incidence, mortality and burden of disease from 1990 to 2017. Inj Prev 26(Supp 1):i67–i74
Bergen G, Stevens M, Burns E (2016) Falls and fall injuries among adults aged ≥65 years—United States, 2014. MMWR Morb Mortal Wkly Rep 65:993–998
Deandrea S, Lucenteforte E, Bravi F et al (2010) Risk factors for falls in community-dwelling older people: a systematic review and meta-analysis. Epidemiology 21(5):658–668
National Institute for Health and Care Excellence (NICE). Falls in older people: assessing risk and prevention—Clinical guideline [CG161]. 12 June 2013 [Accessed 31/08/2022]; Available from: https://www.nice.org.uk/Guidance/CG161/Evidence.
Seppala LJ, Wermelink A, de Vries M et al (2018) Fall-risk-increasing drugs: a systematic review and meta-analysis: II. Psychotropics. J Am Med Dir Assoc 19(4):371.e11-371.e17
Seppala LJ, van der Velde N, Masud T et al (2019) EuGMS task and finish group on fall-risk-increasing drugs (FRIDs): position on knowledge dissemination, management, and future research. Drugs Aging 36(4):299–307
Seppala LJ, Petrovic M, Ryg J et al (2021) STOPPFall (screening tool of older persons prescriptions in older adults with high fall risk): a Delphi study by the eugms task and finish group on fall-risk-increasing drugs. Age Ageing 50(4):1189–1199
Holbrook AM, Crowther R, Lotter A et al (2000) Meta-analysis of benzodiazepine use in the treatment of insomnia. CMAJ Can Med Assoc J. 162(2):225–233
Ma H, Huang Y, Cong Z et al (2014) The efficacy and safety of atypical antipsychotics for the treatment of dementia: a meta-analysis of randomized placebo-controlled trials. J Alzheimer’s Dis 42(3):915–937
Wilkinson P, Ruane C, Tempest K (2018) Depression in older adults. BMJ 363:k4922
Vilaça A, Vieira A, Fernandes A et al (2019) Characterisation of benzodiazepine use in an older population registered in family health units in the region of Minho, Portugal. Geriatrics 4(1):27
Griffin CE 3rd, Kaye AM, Bueno FR et al (2013) Benzodiazepine pharmacology and central nervous system-mediated effects. Ochsner J 13(2):214–223
Cheng T, Wallace DM, Ponteri B et al (2018) Valium without dependence? Individual GABA(A) receptor subtype contribution toward benzodiazepine addiction, tolerance, and therapeutic effects. Neuropsychiatr Dis Treat 14:1351–1361
Petrovic M, Mariman A, Warie H et al (2003) Is there a rationale for prescription of benzodiazepines in the elderly? Review of the literature. Acta Clin Belg 58(1):27–36
Foley DJ, Monjan A, Simonsick EM et al (1999) Incidence and remission of insomnia among elderly adults: an epidemiologic study of 6800 persons over three years. Sleep 22(Suppl 2):S366–S372
Pottie K, Thompson W, Davies S et al (2018) Deprescribing benzodiazepine receptor agonists: evidence-based clinical practice guideline. Can Fam Physician 64(5):339–351
Glass J, Lanctôt KL, Herrmann N et al (2005) Sedative hypnotics in older people with insomnia: meta-analysis of risks and benefits. BMJ 331(7526):1169
Geeraerts A, Dilles T, Foulon V et al (2017) The development of clinical practice algorithms for the appropriate use of psychotropic drugs in older persons with high risk of falls. Tijdschr Gerontol Geriatr 48(5):195–202
Yu NW, Chen PJ, Tsai HJ et al (2017) Association of benzodiazepine and Z-drug use with the risk of hospitalisation for fall-related injuries among older people: a nationwide nested case-control study in Taiwan. BMC Geriatr 17(1):140
Carrier H, Cortaredona S, Philipps V et al (2020) Long-term risk of hip or forearm fractures in older occasional users of benzodiazepines. Br J Clin Pharmacol 86(11):2155–2164
Frey DJ, Ortega JD, Wiseman C et al (2011) Influence of zolpidem and sleep inertia on balance and cognition during nighttime awakening: a randomized placebo-controlled trial. J Am Geriatr Soc 59(1):73–81
Woolcott JC, Richardson KJ, Wiens MO et al (2009) Meta-analysis of the impact of 9 medication classes on falls in elderly persons. Arch Intern Med 169(21):1952–1960
Markota M, Rummans TA, Bostwick JM et al (2016) Benzodiazepine use in older adults: dangers, management, and alternative therapies. Mayo Clin Proc 91(11):1632–1639
Treves N, Perlman A, Geron LK et al (2018) Z-drugs and risk for falls and fractures in older adults-a systematic review and meta-analysis. Age Ageing 47(2):201–208
Belgian Center for Pharmacotherapeutic Information (BCFI). Belgian commented drugs repertory: benzodiazepines. 2022 [Accessed 31/08/2022; Available from: https://www.bcfi.be/nl/chapters/11?frag=7476.
Chen Y, Zhu LL, Zhou Q (2014) Effects of drug pharmacokinetic/pharmacodynamic properties, characteristics of medication use, and relevant pharmacological interventions on fall risk in elderly patients. Ther Clin Risk Manag 10:437–448
Passaro A, Volpato S, Romagnoni F et al (2000) Benzodiazepines with different half-life and falling in a hospitalized population: The GIFA study. Gruppo Italiano di Farmacovigilanza nell’Anziano. J Clin Epidemiol 53(12):1222–1229
van Strien AM, Koek HL, van Marum RJ et al (2013) Psychotropic medications, including short acting benzodiazepines, strongly increase the frequency of falls in elderly. Maturitas 74(4):357–362
de Vries OJ, Peeters G, Elders P et al (2013) The elimination half-life of benzodiazepines and fall risk: two prospective observational studies. Age Ageing 42(6):764–770
Xing D, Ma XL, Ma JX et al (2014) Association between use of benzodiazepines and risk of fractures: a meta-analysis. Osteoporos Int 25(1):105–120
Park H, Satoh H, Miki A et al (2015) Medications associated with falls in older people: systematic review of publications from a recent 5-year period. Eur J Clin Pharmacol 71(12):1429–1440
Huang AR, Mallet L, Rochefort CM et al (2012) Medication-related falls in the elderly: causative factors and preventive strategies. Drugs Aging 29(5):359–376
Ballokova A, Peel NM, Fialova D et al (2014) Use of benzodiazepines and association with falls in older people admitted to hospital: a prospective cohort study. Drugs Aging 31(4):299–310
Herings RM, Stricker BH, de Boer A et al (1995) Benzodiazepines and the risk of falling leading to femur fractures. Dosage more important than elimination half-life. Arch Intern Med 155(16):1801–1807
Sterke CS, van Beeck EF, van der Velde N et al (2012) New insights: dose-response relationship between psychotropic drugs and falls: a study in nursing home residents with dementia. J Clin Pharmacol 52(6):947–955
Berry SD, Placide SG, Mostofsky E et al (2016) Antipsychotic and benzodiazepine drug changes affect acute falls risk differently in the nursing home. J Gerontol Series A Biol Sci Med Sci. 71(2):273–278
Shuto H, Imakyure O, Matsumoto J et al (2010) Medication use as a risk factor for inpatient falls in an acute care hospital: a case-crossover study. Br J Clin Pharmacol 69(5):535–542
Díaz-Gutiérrez MJ, Martínez-Cengotitabengoa M, de Sáez Adana E et al (2017) Relationship between the use of benzodiazepines and falls in older adults: a systematic review. Maturitas 101:17–22
Wang PS, Bohn RL, Glynn RJ et al (2001) Hazardous benzodiazepine regimens in the elderly: effects of half-life, dosage, and duration on risk of hip fracture. Am J Psychiatry 158(6):892–898
Airagnes G, Pelissolo A, Lavallée M et al (2016) Benzodiazepine misuse in the elderly: risk factors, consequences, and management. Curr Psychiatry Rep 18(10):89
Fan-Lun C, Chung C, Lee EHG et al (2019) Reducing unnecessary sedative-hypnotic use among hospitalised older adults. BMJ Qual Saf 28(12):1039–1045
Peklar J, O’Halloran AM, Maidment ID et al (2015) Sedative load and frailty among community-dwelling population aged ≥65 years. J Am Med Dir Assoc 16(4):282–289
Schroeck JL, Ford J, Conway EL et al (2016) Review of safety and efficacy of sleep medicines in older adults. Clin Ther 38(11):2340–2372
Thürmann PA (2020) Pharmacodynamics and pharmacokinetics in older adults. Curr Opin Anaesthesiol 33(1):109–113
American Geriatrics Society (2019) Updated AGS Beers Criteria® for potentially inappropriate medication use in older adults. J Am Geriatr Soc 67(4):674–694
O’Mahony D, O’Sullivan D, Byrne S et al (2015) STOPP/START criteria for potentially inappropriate prescribing in older people: version 2. Age Ageing 44(2):213–218
Allain H, Bentué-Ferrer D, Polard E et al (2005) Postural instability and consequent falls and hip fractures associated with use of hypnotics in the elderly: a comparative review. Drugs Aging 22(9):749–765
Brandt J, Leong C (2017) Benzodiazepines and Z-Drugs: an updated review of major adverse outcomes reported on in epidemiologic research. Drugs R&D 17(4):493–507
Mets MA, Volkerts ER, Olivier B et al (2010) Effect of hypnotic drugs on body balance and standing steadiness. Sleep Med Rev 14(4):259–267
Gibbons CH, Freeman R (2020) Delayed orthostatic hypotension. Auton Neurosci Basic Clin 229:102724
Perlmuter LC, Sarda G, Casavant V et al (2013) A review of the etiology, associated comorbidities, and treatment of orthostatic hypotension. Am J Ther 20(3):279–291
Rivasi G, Kenny RA, Ungar A et al (2020) Effects of benzodiazepines on orthostatic blood pressure in older people. Eur J Intern Med 72:73–78
Barker MJ, Greenwood KM, Jackson M et al (2004) Persistence of cognitive effects after withdrawal from long-term benzodiazepine use: a meta-analysis. Arch Clin Neuropsychol 19(3):437–454
Zhong G, Wang Y, Zhang Y et al (2015) Association between benzodiazepine use and dementia: a meta-analysis. PLoS ONE 10(5):e0127836
Ferreira P, Ferreira AR, Barreto B et al (2022) Is there a link between the use of benzodiazepines and related drugs and dementia? A systematic review of reviews. Eur Geriatr Med 13(1):19–32
Nader D, Gowing L (2020) Is long-term benzodiazepine use a risk factor for cognitive decline? Results of a systematic review. J Addict 2020:1569456
Mura T, Proust-Lima C, Akbaraly T et al (2013) Chronic use of benzodiazepines and latent cognitive decline in the elderly: results from the Three-city study. Eur Neuropsychopharmacol 23(3):212–223
Paterniti S, Dufouil C, Alpérovitch A (2002) Long-term benzodiazepine use and cognitive decline in the elderly: the epidemiology of vascular aging study. J Clin Psychopharmacol 22(3):285–293
Picton JD, Marino AB, Nealy KL (2018) Benzodiazepine use and cognitive decline in the elderly. Am J Health-Syst Pharm 75(1):e6–e12
Stewart SA (2005) The effects of benzodiazepines on cognition. J Clin Psychiatry 66(Suppl 2):9–13
Foubert K, Capiau A, Mehuys E et al (2021) Ghent older people’s prescriptions community pharmacy screening (GheOP(3)S)-tool version 2: update of a tool to detect drug-related problems in older people in primary care. Drugs Aging 38(6):523–533
Pazan F, Kather J, Wehling M (2019) A systematic review and novel classification of listing tools to improve medication in older people. Eur J Clin Pharmacol 75(5):619–625
Abad VC, Guilleminault C (2018) Insomnia in elderly patients: recommendations for pharmacological management. Drugs Aging 35(9):791–817
Reynolds AC, Adams RJ (2019) Treatment of sleep disturbance in older adults. J Pharm Pract Res 49(3):296–304
Siebern AT, Manber R (2011) New developments in cognitive behavioral therapy as the first-line treatment of insomnia. Psychol Res Behav Manag 4:21–28
Riemann D, Baglioni C, Bassetti C et al (2017) European guideline for the diagnosis and treatment of insomnia. J Sleep Res 26(6):675–700
Conn DK, Hogan DB, Amdam L et al (2020) Canadian Guidelines on benzodiazepine receptor agonist use disorder among older adults title. Can Geriatr J 23(1):116–122
Riemann D, Perlis ML (2009) The treatments of chronic insomnia: a review of benzodiazepine receptor agonists and psychological and behavioral therapies. Sleep Med Rev 13(3):205–214
Bloom HG, Ahmed I, Alessi CA et al (2009) Evidence-based recommendations for the assessment and management of sleep disorders in older persons. J Am Geriatr Soc 57(5):761–789
Dagan Y, Zisapel N, Nof D et al (1997) Rapid reversal of tolerance to benzodiazepine hypnotics by treatment with oral melatonin: a case report. Eur Neuropsychopharmacol 7(2):157–160
Morera-Fumero AL, Fernandez-Lopez L, Abreu-Gonzalez P (2020) Melatonin and melatonin agonists as treatments for benzodiazepines and hypnotics withdrawal in patients with primary insomnia. A systematic review. Drug Alcohol depend 212:107994
Li T, Jiang S, Han M et al (2019) Exogenous melatonin as a treatment for secondary sleep disorders: a systematic review and meta-analysis. Front Neuroendocrinol 52:22–28
Morales-Delgado R, Cámara-Lemarroy CR, Salinas-Martínez R et al (2018) A randomized placebo-controlled trial evaluating the effect of melatonin on sleep quality in patients with mild-moderate dementia. European Geriatr Med 9(4):449–454
Stanley MA, Wilson NL, Novy DM et al (2009) Cognitive behavior therapy for generalized anxiety disorder among older adults in primary care: a randomized clinical trial. JAMA 301(14):1460–1467
Hall J, Kellett S, Berrios R et al (2016) Efficacy of cognitive behavioral therapy for generalized anxiety disorder in older adults: systematic review, meta-analysis, and meta-regression. Am J Geriatr Psychiatr 24(11):1063–1073
Ramos K, Stanley MA (2020) Anxiety disorders in late life. Clin Geriatr Med 36(2):237–246
Reeve E, Gnjidic D, Long J et al (2015) A systematic review of the emerging definition of “deprescribing” with network analysis: implications for future research and clinical practice. Br J Clin Pharmacol 80(6):1254–1268
Pollmann AS, Murphy AL, Bergman JC et al (2015) Deprescribing benzodiazepines and Z-drugs in community-dwelling adults: a scoping review. BMC Pharmacol Toxicol 16:19
Ng BJ, Le Couteur DG, Hilmer SN (2018) Deprescribing benzodiazepines in older patients: impact of interventions targeting physicians, pharmacists, and patients. Drugs Aging 35(6):493–521
Kuntz J, Kouch L, Christian D et al (2018) Barriers and facilitators to the deprescribing of nonbenzodiazepine sedative medications among older adults. Perm J 22:17–157
Rasmussen AF, Poulsen SS, Oldenburg LIK et al (2021) The barriers and facilitators of different stakeholders when deprescribing benzodiazepine receptor agonists in older patients-a systematic review. Metabolites 11(4):254
Reeve E, Ong M, Wu A et al (2017) A systematic review of interventions to deprescribe benzodiazepines and other hypnotics among older people. Eur J Clin Pharmacol 73(8):927–935
Gould RL, Coulson MC, Patel N et al (2014) Interventions for reducing benzodiazepine use in older people: meta-analysis of randomised controlled trials. Br J Psychiatr 204(2):98–107
Bourgeois J, Elseviers MM, Van Bortel L et al (2014) Feasibility of discontinuing chronic benzodiazepine use in nursing home residents: a pilot study. Eur J Clin Pharmacol 70(10):1251–1260
Iyer S, Naganathan V, McLachlan AJ et al (2008) Medication withdrawal trials in people aged 65 years and older: a systematic review. Drugs Aging 25(12):1021–1031
Tannenbaum C, Martin P, Tamblyn R et al (2014) Reduction of inappropriate benzodiazepine prescriptions among older adults through direct patient education: the EMPOWER cluster randomized trial. JAMA Intern Med 174(6):890–898
Martin P, Tamblyn R, Benedetti A et al (2018) Effect of a pharmacist-led educational intervention on inappropriate medication prescriptions in older adults: the D-PRESCRIBE randomized clinical trial. JAMA 320(18):1889–1898
Gillespie LD, Robertson MC, Gillespie WJ et al (2012) (2012) Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev 9:007146
Dautzenberg L, Beglinger S, Tsokani S et al (2021) Interventions for preventing falls and fall-related fractures in community-dwelling older adults: a systematic review and network meta-analysis. J Am Geriatr Soc 69(10):2973–2984
Acknowledgements
This paper was written on behalf of the EuGMS Task and Finish group on FRIDs. The T&F group consists of the following members: Austria: Heinrich Thaler; Belgium: Mirko Petrovic; Czech Republic: Eva Topinková, Denmark: Jesper Ryg; Finland: Sirpa Hartikainen; France: Hubert Blain, Jean Bousquet; Ireland: Irene O’Byrne-Maguire, Rose Anne Kenny; Italy: Francesco Landi; Netherlands: Tischa van der Cammen, Marielle Emmelot-Vonk, Eveline van Poelgeest, Lotta Seppälä, Nathalie van der Velde; Poland: Katarzyna Szczerbińska; Spain: Leocadio Rodriguez Mañas, Marta Gutiérrez Valencia, Maria Angeles Caballero-Mora; Sweden: Lucie Laflamme, Gösta Bucht, Yngve Gustafsson, Olle Svensson, Patrik Eklund, Ulrika Pettersson-Kymmer; Turkey: Gulistan Bahat, Birkan Ilhat; UK: Tash Masud, Alpana Mair, Tomas Welsh, Yvonne Morrissey.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethical approval
This study does not contain any studies with human participants performed by any of the authors.
Informed consent
For this type of study, formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Capiau, A., Huys, L., van Poelgeest, E. et al. Therapeutic dilemmas with benzodiazepines and Z-drugs: insomnia and anxiety disorders versus increased fall risk: a clinical review. Eur Geriatr Med 14, 697–708 (2023). https://doi.org/10.1007/s41999-022-00731-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41999-022-00731-4