Key summary points
This narrative review aims to find and summarize recent publications on definitions, epidemiology and clinical consequences of polypharmacy.
AbstractSection FindingsNumerous definitions of polypharmacy and associated terms were found. The prevalence of polypharmacy greatly varies, and numerous adverse clinical outcomes were associated with polypharmacy.
AbstractSection MessageThe clinically oriented definitions of polypharmacy are more useful and relevant. Regardless of the definition, polypharmacy is highly prevalent in older adults. Approaches to increase the appropriateness of polypharmacy can improve clinical outcomes in older adults.
Abstract
Background
The number of older adults has been constantly growing around the globe. Consequently, multimorbidity and related polypharmacy have become an increasing problem. In the absence of an accepted agreement on the definition of polypharmacy, data on its prevalence in various studies are not easily comparable. Besides, the evidence on the potential adverse clinical outcomes related to polypharmacy is limited though polypharmacy has been linked to numerous adverse clinical outcomes. This narrative review aims to find and summarize recent publications on definitions, epidemiology and clinical consequences of polypharmacy.
Methods
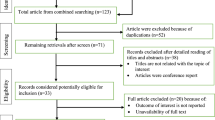
The MEDLINE database was used to identify recent publications on the definition, prevalence and clinical consequences of polypharmacy using their respective common terms and their variations. Systematic reviews and original studies published between 2015 and 2020 were included.
Results
One hundred and forty-three definitions of polypharmacy and associated terms were found. Most of them are numerical definitions. Its prevalence ranges from 4% among community-dwelling older people to over 96.5% in hospitalized patients. In addition, numerous adverse clinical outcomes were associated with polypharmacy.
Conclusion
The term polypharmacy is imprecise, and its definition is yet subject to an ongoing debate. The clinically oriented definitions of polypharmacy found in this review such as appropriate or necessary polypharmacy are more useful and relevant. Regardless of the definition, polypharmacy is highly prevalent in older adults, particularly in nursing home residents and hospitalized patients. Approaches to increase the appropriateness of polypharmacy can improve clinical outcomes in older adults.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Multimorbidity is highly prevalent in our aging societies and it often leads to the use of multiple medications in older patients [1,2,3,4,5]. There are also a number of other factors which are associated with an increased use of drugs in older people such as the wider and growing availability of effective medications in developed countries, and the numerous guidelines that encourage the use of multiple drugs for the management of common diseases [4, 6, 7]. While there is still no consensus on what should be regarded as polypharmacy, there are ongoing efforts to improve its definition and shift the focus from the mere number of drugs to their appropriateness, effects and, ultimately, to related clinical outcomes in older patients [6, 8]. These efforts of course need to be backed by evidence.
In this context, it is important to understand that the process of biological aging is often accompanied by changes in pharmacokinetics and pharmacodynamic in older people [9]. Consequently, there should have been more efforts towards clinical testing of medications specifically in older adults. Regrettably, an exclusion of older adults from clinical approval trials is often observed that has led to a lack of evidence regarding the safety and efficacy of many medications in this population [10, 11]. Thus, the appropriateness of many drugs in an increasing number of older multimorbid patients remains still undetermined. Inevitably, this lack of evidence has often led to inappropriate drug treatment and, consequently, to various adverse clinical outcomes. This large-scale issue was also recognized by the World Health Organization and led to the initiation of the ongoing patient safety campaign called “The third Global Patient Safety Challenge: Medication without harm” with “the goal of reducing severe, avoidable drug-related harm worldwide by 50%” until 2022 [12].
Therefore, to differentiate between appropriate and inappropriate drug treatment numerous listing tools/approaches (prescribing appropriateness assessment tools and criteria) have been proposed [4].
In this work, we searched for the existing definitions of polypharmacy, its prevalence among older adults in various clinical settings and evidence for its clinical consequences in geriatric patients.
Search strategy
This work represents a narrative review that provides an overview of the recent publications on polypharmacy. It is focused on definition, epidemiology, and outcomes of polypharmacy in older adults. For this purpose, we used MEDLINE to search for related publications. The search terms were the following: (polypharmacy OR multiple medication* OR multiple medicine* OR multiple drug* OR Polypharmacy [Mesh] OR many medication* OR definition of polypharmacy OR prevalence of polypharmacy or epidemiology of polypharmacy OR consequences of polypharmacy OR outcomes of polypharmacy). The following filters were used to narrow our search: free full text, full text, review, systematic review, publication date: from November 2015 to November 2020, Humans, English, Aged: 65+ years, 80 and over: 80+ years. In addition, the period for our search was limited to the past 5 years because we aimed to find the most recent literature which would add to the results from the existing reviews also included in this narrative review. All papers found in MEDLINE were assessed for eligibility by title and abstract screening. In addition to the database search, we performed manual searches from the reference lists of some selected articles.
Definition of polypharmacy
We found that there is no generally accepted definition for polypharmacy. This fact has also been acknowledged in a recent report from the World Health Organization (WHO) which stated that:
“Polypharmacy is the concurrent use of multiple medications. Although there is no standard definition, polypharmacy is often defined as the routine use of five or more medications. This includes over-the-counter, prescription and/or traditional and complementary medicines used by a patient” [12].
Certainly, the concurrent intake of five or more drugs is the most common definition of polypharmacy in the literature [13]. Nevertheless, about 143 definitions of polypharmacy and associated terms exist according to a systematic review of definitions of polypharmacy [14] and other more recent publications [7, 8, 11, 15, 16]. The vast majority of those (n = 112) are mere numerical definitions, meaning that only the number of drugs is used to check for the presence of polypharmacy in an individual [14]. These numerical definitions are very heterogenous and partly include associated terms such as minor [17,18,19], mild [20], moderate [21], major [19, 22,23,24,25] and excessive polypharmacy [24, 26,27,28,29] to characterize the severity of polypharmacy [14]. Besides, the threshold for these numerical definitions of polypharmacy ranges from 2 or more to 11 or more drugs [14] and the cut-off/range for the associated terms partly varies as well. For instance, moderate polypharmacy is defined as the daily intake of 4–5 medication in one source [14] and as the intake of 5–9 drugs in another [21].
In addition, there are 11 numerical definitions of polypharmacy which also classify the duration of drug treatment, about 4 numerical definitions which also include the health care setting and 16 descriptive definitions of polypharmacy [8, 14,15,16, 30]. However, the few numerical definitions including the health care setting can be regarded as only numerical definitions which were used in a specific clinical setting. Categories [14] and examples for various definitions of polypharmacy and associated terms are depicted in Table 1. Examples for the more recent definitions of polypharmacy have been underlined in this table. Other new definitions of polypharmacy included unnecessary polypharmacy, and polypharmacy of unclear benefit [8].
Epidemiology
The prevalence of polypharmacy found in the literature greatly varies. It ranges from around 4% to about 96.5% depending on the age group, definition, healthcare setting and region [7, 11].
A cross-sectional analysis [43] from “wave 6” of the Survey of Health, Ageing, and Retirement in Europe (SHARE) database including data from 34,232 participants (mean age: 75.1 ± 7.2 years) revealed that the prevalence of polypharmacy, defined as the concurrent use of five or more medications, in older community-dwelling older adults (aged 65 years or more) ranges from 26.3 to 39.9% across 17 European countries plus Israel [43]. It is noteworthy that the medication use in this study was self-reported and a high number of older adults with comorbidities might have been excluded [43].
The overall prevalence of polypharmacy across all countries was 32.1% (95% CI 31.5–32.7). Besides, the lowest prevalence of polypharmacy was found in Switzerland (26.3%; 95% CI 25.8–26.8), Croatia (27.3%; 95% CI 26.8–27.9) and Slovenia (28.1%; 95% CI 27.6–28.6), while Portugal (36.9%; 95% CI 36.3–37.5), Israel (37.5%; 95% CI 36.9–38.2) and the Czech Republic (39.9%; 95% CI 39.3–40.5) had the highest prevalence of polypharmacy [43].
The prevalence rates were also standardized by three age groups: 65–74, 75–84 and 85 years or older. As anticipated, in higher age groups the overall prevalence of polypharmacy was also greater. The overall prevalence for each age group was as follows: 25.3% (95% CI 24.6–26.0) for participants aged 65–74, 36.4% (95% CI 35.4–37.5) for participants aged 75–44 and 46.5% (95% CI 44.6–48.4) for participants aged 85 years or older [43]. The overall prevalence of polypharmacy was almost identical for women (32.1%; 95% CI 31.3–32.9) and men (32.2%; 95% CI 31.4–33.0) [43]. The prevalence of polypharmacy across 17 European countries and Israel according to Midão et al. [43] is depicted in Fig. 1.

(Reprinted from Midão et al. [43], Copyright (2018), with permission from Elsevier. https://doi.org/10.1016/j.archger.2018.06.018)
Prevalence of polypharmacy (defined as the concurrent use of five or more medications per day) in older adults across 17 European countries and Israel according to “wave 6” of the Survey of Health, Ageing, and Retirement in Europe (SHARE) [43]
Based on the publications from the European Union funded “Stimulating Innovation in the Management of Polypharmacy and Adherence in the Elderly (SIMPATHY) project” [44, 45] the prevalence of polypharmacy (defined as taking ten or more medications) using population-level data from “The Information Services Division (ISD), a division of National Services Scotland” [46], ranged from approximately 6–36% in older adults. According to this data, deprivation had a profound impact on the prevalence of polypharmacy in all age groups. For instance, in people aged 65–69 the prevalence of polypharmacy was about 24% in the most deprived vs. around 7% in the least deprived [45]. In people aged 85 or older, the prevalence of polypharmacy for the two most deprived group of participants (around 33% in the most deprived and about 30% in the second most deprived) was unexpectedly lower as compared to the younger counterparts aged 80–84 (around 36% in the most deprived and about 31% in the second most deprived) [44, 45].
The analysis of the population-level data from a prospective survey investigating the biological and genetic determinants of cardiovascular disease in the population of Lausanne (CoLaus study, Switzerland) revealed that 25.5% of people aged from 65 to 81 years regularly used five or more medications [47]. Another study based on claims data from the largest health insurance in Switzerland revealed that 41.2% of older adults concurrently received 5 or more medications [48].
In a repeated cross-sectional large-scale study (between 338,025 and 539,752 older individuals) from Ireland using electronic data from pharmacy claims over 15 years (1997–2012), the prevalence of polypharmacy (five or more regular prescription medications) increased from 17.8% in 1997 to 60.4% in 2012. In addition, excessive polypharmacy (ten or more regular prescription medications) showed a similar trend. It increased from 1.5 to 21.9% in people aged 65 years or older [49].
In a cross-sectional analysis of adult electronic primary healthcare records from Scotland, the prevalence of polypharmacy (the use of 4–9 medications) was 28.6% in adults aged 60–69 years and 51.8% in those aged 80+ years [50]. In this study, the term polypharmacy was not clearly stated. Instead, the “higher” consumption of drugs was categorized into either using 4–9 medications or ten or more. In addition, the prevalence of patients taking ten or more medications was 7.4% in people aged 60–69 years and 18.6% in those aged 80+ years [50].
Another repeated cross-sectional analysis of community-dispensed prescribing data in the Tayside region of Scotland showed that the use of ten or more drugs in older adults more than tripled from 4.9% in 1995 to 17.2% in 2010 [51]. In the same time period, the use of five or more medications was also increased by twofold from around 20% to around 40% among older adults aged 65–69 years old [51].
In the U.S., population-level data from the National Health and Nutrition Examination Survey (NHANES) revealed a significant increase in the prevalence of polypharmacy (five or more prescription medications) from 24% (95% CI 21–26) to 39% (95% CI 35–44) among older adults between 1999/2000 and 2011/2012 [52].
In a large observational cohort study including 2057 older emergency department patients from Ancona in Italy [53]. The prevalence of polypharmacy (the concomitant use of 6–9 drugs in the last 3 months) was 30.3% and excessive polypharmacy (the concomitant ten or more drugs in the last 3 months) was observed in 17.8% of the patients [53].
A large (N = 1,742,336) prospective, longitudinal, register-based cohort study specifically analyzed the epidemiology of polypharmacy in older adults between 2010 and 2013 in Sweden [54]. This study showed that the prevalence of polypharmacy (5+ drugs) was 44% and 11.7% of the individuals included had excessive polypharmacy (used ten or more drugs) [54]. The incidence rate of newly developed polypharmacy was 19.9 per 100 person-years, and the incidence rate of excessive polypharmacy was 8.0 per 100 person-years [54].
A longitudinal study from The Netherlands including data from elderly patients visiting general practices in Groningen between 1994 and 1997 showed a prevalence of “major polypharmacy” (long-term use of six or more drugs; long-term was defined as “for over 240 days in a year” [23]) in only 4% of cases at the end of 1997. Besides, at the end of the study 9% of the participants were prescribed 4–5 drugs (long-term) which was considered as moderate polypharmacy and 28% of the patients 2–3 drugs (long-term) defined as minor polypharmacy in this study [23]. Over the course of four years, about 20% of older people developed polypharmacy in this population [23].
According to another study based on the Korea Health Insurance Review and Assessment Service—National Patient Sample (HIRA-NPS) data from 2010 and 2011, polypharmacy (six or more medications) was found in 86.4% of older people in Korea [24]. Major polypharmacy (11 medications or more) and excessive polypharmacy (21 medications or more) was observed in 44.9% and 3% of cases each [24].
A longitudinal observational study from Taiwan, which included frail Taiwanese older adults with long-term care needs also revealed a high prevalence of polypharmacy (prescribed with five or more drugs) in about 84% of cases [24]. However, persistent polypharmacy (polypharmacy for 181 days or more) was observed in only 31% of cases [55]. Another study from Taiwan, which used Taiwan’s Longitudinal Health Insurance Database to assess drug use for older adults showed that polypharmacy (use of five or more drugs) was present in 28.2% of cases [56].
In the GLISTEN (Gruppo di Lavoro Italiano Sarcopenia—Trattamento e Nutrizione; Italian working group on sarcopenia—nutrition and treatment) study, the prevalence of polypharmacy (using five or more medications daily) in patients admitted to geriatric and internal medicine acute care ward of 12 Italian hospitals was 70.2%. In the same cohort, the prevalence of hyper-polypharmacy (using ten or more medications daily) was 13% [57]. Another study in older hospitalized patients (aged 60 or over) from India showed that 45% of the patients presented with polypharmacy (used 5–9 medications) and 45.5% with high-level polypharmacy (used ten or more drugs) [58]. According to a cross-sectional study in older (aged 80 years or older) hospitalized patients from China, the prevalence of “hyper-polypharmacy” (11 or more drugs) was 96.5% [59].
In a cross-sectional analysis on nursing home residents participating in the “Services and Health for Elderly in Long TERm care” (SHELTER) project the prevalence of polypharmacy (5–9 drugs) and excessive polypharmacy (ten or more drugs) were 49.7% and 24.3% each [60]. Other studies assessing medication use in nursing home residents reported a prevalence of polypharmacy (five or more drugs) between 38.1 and 91.2% [61]. In addition, the prevalence of polypharmacy defined as the use of ten or more drugs ranged between 10.6 and 65% [61].
Clinical consequences of polypharmacy
Polypharmacy has been linked to numerous negative clinical outcomes such as frailty, hospitalization and even mortality [62, 63]. Here, we report the results from previous reviews and recent studies on the association between polypharmacy and major clinical outcomes in older adults.
Polypharmacy and frailty
While polypharmacy and frailty are highly prevalent in older adults the causal relationship between them is still unclear [11]. According to a recent systematic review and meta-analysis [64] which investigated the cross-sectional association between polypharmacy/hyper-polypharmacy and the presence of prefrailty/frailty as well as the risk of incident prefrailty/frailty in adults with polypharmacy, a strong and bidirectional association between both polypharmacy and hyper-polypharmacy and frailty was found [64]. This study indicated that 75% of adults with polypharmacy are pre-frail/frail. Besides, only a few longitudinal studies on the risk of incident prefrailty/frailty in adults with baseline polypharmacy were found [64]. In a meta-analysis of three of those studies, a significantly higher odd of developing prefrailty in robust persons was found in the presence of polypharmacy [64]. In a longitudinal study [65], taking seven or more medications was associated with a 2.5 increased risk of developing frailty over 8 years [64]. This systematic review concluded that more research is needed to assess the causal relationship between polypharmacy and frailty [64]. Another systematic review indicated that polypharmacy could play a major role in the development of frailty and stated that the causal relationship is uncertain and appears to be bidirectional [66]. Besides, a cohort study of 772 Spanish older adults showed that polypharmacy is associated with death, incident disability, hospitalization, and emergency department visits in frail and prefrail older adults, but not in robust older people [67].
Polypharmacy and death
A systematic review and meta-analysis by Leelakanok et al. revealed a significant association between mortality and polypharmacy [68]. Besides, when polypharmacy was defined categorically, a dose–response relationship was seen across escalating thresholds (namely 1–4 medications, five medications, 6–9 medications and ten or more medications) [68]. It is important to mention that in patients with polypharmacy the risk of mortality may also be increased by the presence of more chronic conditions. Hence, confounding by indication has to be addressed when assessing the relationship between polypharmacy and mortality [62]. For instance, in a study by Schöttker et al. addressing this issue, polypharmacy was not independently associated with non-cancer mortality after adjustment for chronic conditions and by using propensity score matching [62, 69, 70]. Conversely, in a recent nationwide longitudinal cohort study from Korea, polypharmacy was associated with a higher risk of all-cause death, even after adjustment for comorbidities and propensity-score matching [71]. In addition, a danish nationwide population-based cohort study showed an association between increasing number of medications and mortality. In brief, for each extra medication the mortality increased by over 3% in the fully adjusted model which included diseases and Barthel Index [72].
Polypharmacy and hospitalization
Several studies in community-dwelling older adults [73] and nursing home residents [74] have shown an association between polypharmacy and hospitalization [11, 62]. The association has been shown for any hospitalization, unplanned hospitalization, and re-hospitalization in hospital-based samples [62]. For instance, a longitudinal health insurance database study from Taiwan investigating the association between polypharmacy and all-cause and fracture-specific admission to hospital [56], showed an independent association between polypharmacy and all-cause and fracture-specific hospitalization [56]. In another study including nursing home residents from Australia, polypharmacy (defined as nine or more regular medications) was associated with time to the first hospitalization, number of hospitalizations and hospital days per person-year [75]. Furthermore, in a large observational cohort study in a geriatric hospital, polypharmacy (having 6–9 drug prescriptions in the last 3 months) and excessive polypharmacy (ten or more drug prescriptions in the last 3 months) were both associated with emergency department revisit and hospital admission [53]. In the aforementioned nationwide longitudinal cohort study from Korea polypharmacy was associated with a higher risk of hospitalization as well [71].
Polypharmacy and falls
Numerous studies have shown an association between polypharmacy and falls [62, 76]. For example, a register-based study from Sweden confirmed the association between polypharmacy and risk of falling [77]. However, an adjustment for fall-risk-inducing drugs (FRIDs) weakened this association [77]. In a longitudinal study from England, the rate of falls was 21% higher in older adults with polypharmacy (five or more drugs) compared with people without polypharmacy [78]. Using a lower threshold of four or more drugs for polypharmacy, the rate of falls was 18% higher in people with polypharmacy compared with people without [78]. Hyper-polypharmacy (ten or more drugs) was associated with a 50% higher rate of falls [78]. In another study, the number of fall-risk medications was associated with fall-related hospital admissions though polypharmacy could not be identified as an independent risk factor [79]. Recently, a prospective cohort study also revealed that polypharmacy is associated with an increased falls risk in UK care home residents [80].
Polypharmacy and cognitive impairment
Polypharmacy and specially psychotropics and anticholinergic drugs have been associated with cognitive impairment in various studies [62, 81].
For example, in a 12-year longitudinal register-based study from South Korea, polypharmacy was associated with the development of dementia [82]. Another longitudinal study in nursing home residents showed associations between polypharmacy and excessive polypharmacy and the decline in cognitive function [83]. In Japan, a study in community-dwelling older adults also found an association between polypharmacy and cognitive impairment [81]. According to a cross-sectional study in patients with newly diagnosed Parkinson’s disease, those participants with polypharmacy had significantly lower Mini-Mental State Examination scores as compared to other patients with no polypharmacy [84]. In another study investigating the associations between polypharmacy and cognitive and physical capability, polypharmacy and longstanding polypharmacy were associated with poorer cognitive capability; an even stronger negative association was observed in individuals with longstanding polypharmacy [85].
Polypharmacy and physical function
Polypharmacy has been shown to be associated with a physical impairment in older adults [36, 85, 86]. A systematic review on the association between polypharmacy and physical function in older adults concluded that there is a strong bidirectional relationship between polypharmacy and physical function [87]. However, a causal relationship based on the 18 observational studies included in that review could not be proven [87]. The authors concluded that objective measures of physical function and polypharmacy are necessary to prove this causal relationship in future studies [87]. Interestingly, in a multicenter study of European nursing homes polypharmacy was not associated with a faster decline in functional status [83]. Besides, disability has also been associated with polypharmacy [67, 88].
Conclusion
The term polypharmacy is imprecise and its definition is yet subject to an ongoing debate [89]. Our findings regarding the definition of polypharmacy are in line with several previous studies [7, 11, 14, 90]. The most common definition still is the concomitant use of five or more medications.
While there was a wide range for the prevalence of polypharmacy (4–96.5%), all studies showed an increase in the prevalence of polypharmacy in older adults over time and most of them included community-dwelling older people. In addition, in almost all studies the prevalence of polypharmacy directly correlated with age. Besides, the degree of deprivation seems also to affect the prevalence of polypharmacy in older adults [44, 45]. The highest prevalence of polypharmacy (over 96.5%) was observed in older hospitalized patients in China [59]. Interestingly, the prevalence of polypharmacy among community-dwelling older adults from Korea (86.4%) appeared to be higher than in any other region of the world [24].
The imprecise and heterogenous definition of polypharmacy complicates the analysis of its prevalence and impact on relevant health outcomes. Generally, polypharmacy can only serve as an indicator for adverse clinical outcomes, a causal relation with clinical outcomes has not been unequivocally proven as prospective interventional trials on its clinical impact are largely missing. Association rather than causation has been the most prevalent outcome from studies correlating clinical outcomes and polypharmacy. The descriptive definitions of polypharmacy found in this review such as appropriate/necessary polypharmacy are potentially more useful for clinical projections. The rational use of even many drugs can be beneficial and sometimes would simply reflect the results from large randomized controlled trials, thereby limiting the role of the mere number of drugs for clinical predictions. In other words, the quality of drug treatment is crucial for a successful or beneficial therapy rather than the number of drugs used in the same patient.
Best approaches towards appropriate polypharmacy should address both over- as well as under-treatment in older patients [4, 6]. To increase the appropriateness of drug therapy at least 73 listing tools/approaches have been developed. Most of them are designed to tackle the problem of over-treatment and polypharmacy and do not address the problem of undertreatment [4]. Hence, individualized and appropriate polypharmacy is not sufficiently addressed by most of these tools. In addition, only a minority of listing tools/approaches have been validated in randomized controlled trials with relevant clinical outcomes, e.g. on physical function, hospitalization or death [4]. Of those, only the FORTA (Fit fOR The Aged) list [91] and the screening tool of older people’s prescriptions (STOPP) and screening tool to alert to right treatment (START) criteria [92] have shown a positive impact on relevant clinical endpoints in randomized controlled trials [4].
The further improvement of drug treatment in older people by interventional trials on such instruments is strongly recommended; it should lead to a better understanding of polypharmacy and of the true clinical effects of medication optimization that are not necessarily linked to the mere number of drugs.
References
United Nations, D.o.E.a.S.A., Population Division (2020) World Population Ageing 2019 (ST/ESA/SER.A/444). https://www.un.org/en/development/desa/population/publications/pdf/ageing/WorldPopulationAgeing2019-Report.pdf. Accessed 2 Nov 2020
Mc Namara KP et al (2017) Health professional perspectives on the management of multimorbidity and polypharmacy for older patients in Australia. Age Ageing 46(2):291–299
Molokhia M, Majeed A (2017) Current and future perspectives on the management of polypharmacy. BMC Fam Pract 18(1):70
Pazan F, Kather J, Wehling M (2019) A systematic review and novel classification of listing tools to improve medication in older people. Eur J Clin Pharmacol 75(5):619–625
Gutiérrez-Valencia M, Martínez-Velilla N, Vilches-Moraga A (2019) Polypharmacy in older people: time to take action. Eur Geriatr Med 10(1):1–3
Rankin A et al (2018) Interventions to improve the appropriate use of polypharmacy for older people. Cochrane Database Syst Rev 9:CD008165
Guillot J, Maumus-Robert S, Bezin J (2020) Polypharmacy: a general review of definitions, descriptions and determinants. Therapies 75(5):407–416
Lee EA et al (2020) Refining the definition of polypharmacy and its link to disability in older adults: conceptualizing necessary polypharmacy, unnecessary polypharmacy, and polypharmacy of unclear benefit. Perm J 24(18):212
Mangoni AA, Jackson SH (2004) Age-related changes in pharmacokinetics and pharmacodynamics: basic principles and practical applications. Br J Clin Pharmacol 57(1):6–14
Shenoy P, Harugeri A (2015) Elderly patients’ participation in clinical trials. Perspect Clin Res 6(4):184–189
Khezrian M et al (2020) An overview of prevalence, determinants and health outcomes of polypharmacy. Ther Adv Drug Saf 11:1–10
World Health Organization (2019) Medication Safety in Polypharmacy (WHO/UHC/SDS/2019.11). https://apps.who.int/iris/bitstream/handle/10665/325454/WHO-UHC-SDS-2019.11-eng.pdf?ua=1. Accessed 13 Aug 2019
Varghese D, Ishida C, Haseer Koya H (2020) Polypharmacy. StatPearls, Treasure Island
Masnoon N et al (2017) What is polypharmacy? A systematic review of definitions. BMC Geriatr 17(1):230
Gomes MS et al (2019) Polypharmacy in older patients at primary care units in Brazil. Int J Clin Pharm 41(2):516–524
McMahon M, Hatton C, Bowring DL (2020) Polypharmacy and psychotropic polypharmacy in adults with intellectual disability: a cross-sectional total population study. J Intellect Disabil Res 64(12):834–851
Jorgensen TL et al (2012) Polypharmacy and drug use in elderly Danish cancer patients during 1996 to 2006. J Geriatr Oncol 3(1):33–40
Lu J et al (2014) Polypharmacy among nonagenarians/centenarians in rural China. Intern Med J 44(12a):1193–1199
Housley BC et al (2015) Comorbidity-polypharmacy score predicts readmission in older trauma patients. J Surg Res 199(1):237–243
Trevisan C et al (2019) Mild polypharmacy and MCI progression in older adults: the mediation effect of drug-drug interactions. Aging Clin Exp Res 33(1):49–56
Gallagher C et al (2020) Polypharmacy and health outcomes in atrial fibrillation: a systematic review and meta-analysis. Open Heart 7(1):e001257
Ferreira AR et al (2015) P.5.f.007 Comorbidity and polypharmacy in residential care and community-dwelling elderly in Portugal. Eur Neuropsychopharmacol 25:S595
Veehof L et al (2000) The development of polypharmacy. A longitudinal study. Fam Pract 17(3):261–267
Kim HA et al (2014) Prevalence and predictors of polypharmacy among Korean elderly. PLoS ONE 9(6):e98043
Veehof LJG, Jong BMd, Haaijer-Ruskamp F (2000) Polypharmacy in the elderly -a literature review. Eur J Gen Pract 6(3):98–106
Walckiers D, Van der Heyden J, Tafforeau J (2015) Factors associated with excessive polypharmacy in older people. Arch Public Health 73:50
Diez-Manglano J et al (2015) Excessive polypharmacy and survival in polypathological patients. Eur J Clin Pharmacol 71(6):733–739
Hovstadius B, Petersson G (2013) The impact of increasing polypharmacy on prescribed drug expenditure-a register-based study in Sweden 2005–2009. Health Policy 109(2):166–174
Dorks M et al (2016) Polypharmacy and renal failure in nursing home residents: results of the inappropriate medication in patients with renal insufficiency in nursing homes (IMREN) study. Drugs Aging 33(1):45–51
Kadam UT et al (2019) Conceptualizing multiple drug use in patients with comorbidity and multimorbidity: proposal for standard definitions beyond the term polypharmacy. J Clin Epidemiol 106:98–107
Nobili A et al (2011) Association between clusters of diseases and polypharmacy in hospitalized elderly patients: results from the REPOSI study. Eur J Intern Med 22(6):597–602
Kuzuya M et al (2006) Underuse of medications for chronic diseases in the oldest of community-dwelling older frail Japanese. J Am Geriatr Soc 54(4):598–605
Narayan SW, Nishtala PS (2015) Associations of potentially inappropriate medicine use with fall-related hospitalisations and primary care visits in older new zealanders: a population-level study using the updated 2012 beers criteria. Drugs Real World Outcomes 2(2):137–141
Vetrano DL et al (2014) Predictors of length of hospital stay among older adults admitted to acute care wards: a multicentre observational study. Eur J Intern Med 25(1):56–62
Nishtala PS, Salahudeen MS (2015) Temporal trends in polypharmacy and hyperpolypharmacy in older new zealanders over a 9-year period: 2005–2013. Gerontology 61(3):195–202
Sganga F et al (2014) Physical performance measures and polypharmacy among hospitalized older adults: results from the CRIME study. J Nutr Health Aging 18(6):616–621
Schuler J et al (2008) Polypharmacy and inappropriate prescribing in elderly internal-medicine patients in Austria. Wien Klin Wochenschr 120(23–24):733–741
Kann IC, Lundqvist C, Luras H (2015) Polypharmacy among the elderly in a list-patient system. Drugs Real World Outcomes 2(3):193–198
Cadogan C et al (2015) Dispensing appropriate polypharmacy to older people in primary care: a qualitative, theory-based study of community pharmacists’ perceptions and experiences. IJPP Supplement 2:32–33
Herr M et al (2015) Polypharmacy and frailty: prevalence, relationship, and impact on mortality in a French sample of 2350 old people. Pharmacoepidemiol Drug Saf 24(6):637–646
Jiron M et al (2015) Prevalence and determinants of potentially inappropriate medication prescribing among older US adults according to STOPP criteria. Pharmacoepidemiol Drug Saf 24(S1):1–587
Fulton MM, Allen ER (2005) Polypharmacy in the elderly: a literature review. J Am Acad Nurse Pract 17(4):123–132
Midao L et al (2018) Polypharmacy prevalence among older adults based on the survey of health, ageing and retirement in Europe. Arch Gerontol Geriatr 78:213–220
Mair A, Wilson M, Dreischulte T (2020) Addressing the challenge of polypharmacy. Annu Rev Pharmacol Toxicol 60:661–681
Mair A et al (2017) Polypharmacy Management by 2030: a patient safety challenge. https://ec.europa.eu/chafea/health/newsroom/news/documents/polypharmacy-handbook-second-edition_en.pdf. Accessed 8 Nov 2020
Division T.I.S. (2017) National data from ISD Scotland. https://www.isdscotland.org. Accessed 8 Nov 2020
Castioni J et al (2017) Prevalence and determinants of polypharmacy in Switzerland: data from the CoLaus study. BMC Health Serv Res 17(1):840
Blozik E et al (2013) Polypharmacy and potentially inappropriate medication in the adult, community-dwelling population in Switzerland. Drugs Aging 30(7):561–568
Moriarty F et al (2015) Trends and interaction of polypharmacy and potentially inappropriate prescribing in primary care over 15 years in Ireland: a repeated cross-sectional study. BMJ Open 5(9):e008656
Payne RA et al (2014) Prevalence of polypharmacy in a Scottish primary care population. Eur J Clin Pharmacol 70(5):575–581
Guthrie B et al (2015) The rising tide of polypharmacy and drug-drug interactions: population database analysis 1995–2010. BMC Med 13:74
Kantor ED et al (2015) Trends in prescription drug use among adults in the United States from 1999–2012. JAMA 314(17):1818–1831
Salvi F et al (2017) Is polypharmacy an independent risk factor for adverse outcomes after an emergency department visit? Intern Emerg Med 12(2):213–220
Morin L et al (2018) The epidemiology of polypharmacy in older adults: register-based prospective cohort study. Clin Epidemiol 10:289–298
Chan DC, Hao YT, Wu SC (2009) Characteristics of outpatient prescriptions for frail Taiwanese elders with long-term care needs. Pharmacoepidemiol Drug Saf 18(4):327–334
Lu WH et al (2015) Effect of polypharmacy, potentially inappropriate medications and anticholinergic burden on clinical outcomes: a retrospective cohort study. CMAJ 187(4):E130–E137
Agosta L et al (2019) Polypharmacy and sarcopenia in hospitalized older patients: results of the GLISTEN study. Aging Clin Exp Res 31(4):557–559
Harugeri A et al (2010) Prescribing patterns and predictors of high-level polypharmacy in the elderly population: a prospective surveillance study from two teaching hospitals in India. Am J Geriatr Pharmacother 8(3):271–280
Lai X et al (2018) Polypharmacy in the oldest old (≥80 years of age) patients in China: a cross-sectional study. BMC Geriatr 18(1):64
Onder G et al (2012) Polypharmacy in nursing home in Europe: results from the SHELTER study. J Gerontol Ser A 67A(6):698–704
Jokanovic N et al (2015) Prevalence and factors associated with polypharmacy in long-term care facilities: a systematic review. J Am Med Dir Assoc 16(6):535 e1-612
Wastesson JW et al (2018) An update on the clinical consequences of polypharmacy in older adults: a narrative review. Expert Opin Drug Saf 17(12):1185–1196
Khezrian M et al (2019) The association between polypharmacy and late life deficits in cognitive, physical and emotional capability: a cohort study. Int J Clin Pharm 41(1):251–257
Palmer K et al (2019) Association of polypharmacy and hyperpolypharmacy with frailty states: a systematic review and meta-analysis. Eur Geriatr Med 10(1):9–36
Veronese N et al (2017) Polypharmacy is associated with higher frailty risk in older people: an 8-year longitudinal cohort study. J Am Med Dir Assoc 18(7):624–628
Gutierrez-Valencia M et al (2018) The relationship between frailty and polypharmacy in older people: a systematic review. Br J Clin Pharmacol 84(7):1432–1444
Bonaga B et al (2018) Frailty, polypharmacy, and health outcomes in older adults: the frailty and dependence in albacete study. J Am Med Dir Assoc 19(1):46–52
Leelakanok N et al (2017) Association between polypharmacy and death: a systematic review and meta-analysis. J Am Pharm Assoc 57(6):729-738.e10
Schottker B et al (2017) Polypharmacy and mortality: new insights from a large cohort of older adults by detection of effect modification by multi-morbidity and comprehensive correction of confounding by indication. Eur J Clin Pharmacol 73(8):1041–1048
Schottker B et al (2018) Updated analysis on polypharmacy and mortality from the ESTHER study. Eur J Clin Pharmacol 74(7):981–982
Chang TI et al (2020) Polypharmacy, hospitalization, and mortality risk: a nationwide cohort study. Sci Rep 10(1):18964
Brockhattingen KK et al (2020) Association between number of medications and mortality in geriatric inpatients: a Danish nationwide register-based cohort study. Eur Geriatr Med 11(6):1063–1071
Beer C et al (2011) Quality use of medicines and health outcomes among a cohort of community dwelling older men: an observational study. Br J Clin Pharmacol 71(4):592–599
Lalic S et al (2016) Polypharmacy and medication regimen complexity as factors associated with staff informant rated quality of life in residents of aged care facilities: a cross-sectional study. Eur J Clin Pharmacol 72(9):1117–1124
Lalic S et al (2016) Polypharmacy and medication regimen complexity as risk factors for hospitalization among residents of long-term care facilities: a prospective cohort study. J Am Med Dir Assoc 17(11):1067 e1-1067 e6
Fried TR et al (2014) Health outcomes associated with polypharmacy in community-dwelling older adults: a systematic review. J Am Geriatr Soc 62(12):2261–2272
Laflamme L et al (2015) Type, number or both? A population-based matched case-control study on the risk of fall injuries among older people and number of medications beyond fall-inducing drugs. PLoS ONE 10(3):e0123390
Dhalwani NN et al (2017) Association between polypharmacy and falls in older adults: a longitudinal study from England. BMJ Open 7(10):e016358
Ryan-Atwood TE et al (2017) Medication use and fall-related hospital admissions from long-term care facilities: a hospital-based case-control study. Drugs Aging 34(8):625–633
Izza MAD et al (2020) Polypharmacy, benzodiazepines, and antidepressants, but not antipsychotics, are associated with increased falls risk in UK care home residents: a prospective multi-centre study. Eur Geriatr Med 11(6):1043–1050
Niikawa H et al (2017) Association between polypharmacy and cognitive impairment in an elderly Japanese population residing in an urban community. Geriatr Gerontol Int 17(9):1286–1293
Park HY et al (2017) The association between polypharmacy and dementia: a nested case-control study based on a 12-year longitudinal cohort database in South Korea. PLoS ONE 12(1):e0169463
Vetrano DL et al (2018) Association of polypharmacy with 1-year trajectories of cognitive and physical function in nursing home residents: results from a multicenter european study. J Am Med Dir Assoc 19(8):710–713
Ishii N et al (2019) Polypharmacy associated with cognitive decline in newly diagnosed Parkinson’s disease: a cross-sectional study. Dement Geriatr Cogn Disord Extra 9(3):338–343
Rawle MJ et al (2018) Associations between polypharmacy and cognitive and physical capability: a British birth cohort study. J Am Geriatr Soc 66(5):916–923
George C, Verghese J (2017) Polypharmacy and gait performance in community-dwelling older adults. J Am Geriatr Soc 65(9):2082–2087
Katsimpris A et al (2019) The association between polypharmacy and physical function in older adults: a systematic review. J Gen Intern Med 34(9):1865–1873
Wang R et al (2015) Incidence and effects of polypharmacy on clinical outcome among patients aged 80+: a five-year follow-up study. PLoS ONE 10(11):e0142123
Johnell K (2018) The controversies surrounding polypharmacy in old age - where are we? Expert Rev Clin Pharmacol 11(9):825–827
Taghy N et al (2020) Failure to reach a consensus in polypharmacy definition: an obstacle to measuring risks and impacts-results of a literature review. Ther Clin Risk Manag 16:57–73
Wehling M et al (2016) VALFORTA: a randomised trial to validate the FORTA (Fit fOR The Aged) classification. Age Ageing 45(2):262–267
O’Mahony D et al (2015) STOPP/START criteria for potentially inappropriate prescribing in older people: version 2. Age Ageing 44(2):213–218
Funding
Open Access funding enabled and organized by Projekt DEAL. This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
MW was employed by AstraZeneca R&D, Mölndal, as director of discovery medicine (translational medicine) from 2003 to 2006, while on sabbatical leave from his professorship at the University of Heidelberg. Since returning to this position in January 2007, he has received lecturing and consulting fees from Sanofi-Aventis, Bayer, Berlin-Chemie, Boehringer Ingelheim, Aspen, Novartis, Takeda, Roche, Pfizer, Bristol-Myers, Daichii-Sankyo, Lilly, Otsuka, Novo-Nordisk, Shire and LEO Pharma. FP declares that he has no conflict of interest.
Ethical approval
Approval from a medical ethics committee was not necessary for this narrative review.
Informed consent
For this narrative review formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pazan, F., Wehling, M. Polypharmacy in older adults: a narrative review of definitions, epidemiology and consequences. Eur Geriatr Med 12, 443–452 (2021). https://doi.org/10.1007/s41999-021-00479-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41999-021-00479-3