Abstract
Purpose
The objective was to investigate whether the association of polypharmacy with non-cancer mortality is independent from comorbidity and is not a result of confounding by indication.
Methods
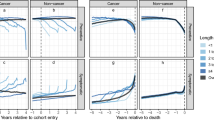
Analyses were conducted in 2687 participants of a German, population-based cohort of older adults with data collection 2008–2010. Polypharmacy was defined as ≥5 drugs and hyperpolypharmacy as ≥10 drugs. Drugs without relevant propensity of causing adverse drug reactions or drug-drug interactions were not counted. Confounding by indication was addressed by model adjustment for a propensity score for polypharmacy.
Results
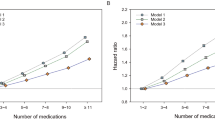
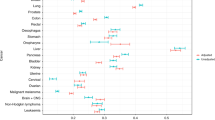
The median age of study participants was 70 years, 10.7% had multi-morbidity, and 47.4% took five drugs or more (8.6% took ≥10 drugs). During 4.4 years of follow-up, 87 participants died of a cause other than cancer. Statistically significant, more than twofold increased non-cancer mortality was observed for subjects with polypharmacy or hyperpolypharmacy in a model adjusted for age, sex, education, lifestyle variables, and comorbidity, but associations lost statistical significance after additional adjustment for a propensity score for polypharmacy. However, a significant interaction of hyperpolypharmacy and multi-morbidity was detected (p = 0.019). The hazard ratio for the association of hyperpolypharmacy with non-cancer mortality was 1.42 (95%CI 0.57; 3.57) in subjects without multi-morbidity and 0.51 (95%CI 0.11; 2.27) in subjects with multi-morbidity.
Conclusions
Polypharmacy was not independently associated with non-cancer mortality. This study highlights the importance to adjust for confounding by indication in studies on polypharmacy by a propensity score. The detected interaction suggests that hyperpolypharmacy can be indicated in subjects with multi-morbidity and may only be harmful in subjects without multi-morbidity.


Similar content being viewed by others
References
Junius-Walker U, Theile G, Hummers-Pradier E (2007) Prevalence and predictors of polypharmacy among older primary care patients in Germany. Fam Pract 24:14–19
Charlesworth CJ, Smit E, Lee DS, Alramadhan F, Odden MC (2015) Polypharmacy among adults aged 65 years and older in the United States: 1988–2010. J Gerontol A Biol Sci Med Sci 70:989–995
Hughes LD, McMurdo ME, Guthrie B (2013) Guidelines for people not for diseases: the challenges of applying UK clinical guidelines to people with multimorbidity. Age Ageing 42:62–69
Field TS, Gurwitz JH, Harrold LR et al (2004) Risk factors for adverse drug events among older adults in the ambulatory setting. J Am Geriatr Soc 52:1349–1354
Johnell K, Klarin I (2007) The relationship between number of drugs and potential drug-drug interactions in the elderly: a study of over 600,000 elderly patients from the Swedish Prescribed Drug Register. Drug Saf 30:911–918
Fried TR, O’Leary J, Towle V, Goldstein MK, Trentalange M, Martin DK (2014) Health outcomes associated with polypharmacy in community-dwelling older adults: a systematic review. J Am Geriatr Soc 62:2261–2272
Schöttker B, Saum KU, Jansen EH, Holleczek B, Brenner H (2016) Associations of metabolic, inflammatory and oxidative stress markers with total morbidity and multi-morbidity in a large cohort of older German adults. Age Ageing 45:127–135
Nathan A, Goodyer L, Lovejoy A, Rashid A (1999) ‘Brown bag’ medication reviews as a means of optimizing patients’ use of medication and of identifying potential clinical problems. Fam Pract 16:278–282
Hudon C, Fortin M, Vanasse A (2005) Cumulative Illness Rating Scale was a reliable and valid index in a family practice context. J Clin Epidemiol 58:603–608
Voorrips LE, Ravelli AC, Dongelmans PC, Deurenberg P, van Staveren WA (1991) A physical activity questionnaire for the elderly. Med Sci Sports Exerc 23:974–979
Desquilbet L, Mariotti F (2010) Dose-response analyses using restricted cubic spline functions in public health research. Stat Med 29:1037–1057
Espino DV, Bazaldua OV, Palmer RF et al (2006) Suboptimal medication use and mortality in an older adult community-based cohort: results from the Hispanic EPESE Study. J Gerontol A Biol Sci Med Sci 61:170–175
Richardson K, Ananou A, Lafortune L, Brayne C, Matthews FE (2011) Variation over time in the association between polypharmacy and mortality in the older population. Drugs Aging 28:547–560
Gomez C, Vega-Quiroga S, Bermejo-Pareja F, Medrano MJ, Louis ED, Benito-Leon J (2015) Polypharmacy in the elderly: a marker of increased risk of mortality in a population-based prospective study (NEDICES). Gerontology 61:301–309
Herr M, Robine JM, Pinot J, Arvieu JJ, Ankri J (2015) Polypharmacy and frailty: prevalence, relationship, and impact on mortality in a French sample of 2350 old people. Pharmacoepidemiol Drug Saf 24:637–646
Gnjidic D, Hilmer SN, Blyth FM et al (2012) Polypharmacy cutoff and outcomes: five or more medicines were used to identify community-dwelling older men at risk of different adverse outcomes. J Clin Epidemiol 65:989–995
Beer C, Hyde Z, Almeida OP et al (2011) Quality use of medicines and health outcomes among a cohort of community dwelling older men: an observational study. Br J Clin Pharmacol 71:592–599
Pozzi C, Lapi F, Mazzaglia G et al (2010) Is suboptimal prescribing a risk factor for poor health outcomes in community-dwelling elders? The ICARe Dicomano study. Pharmacoepidemiol Drug Saf 19:954–960
Lu WH, Wen YW, Chen LK, Hsiao FY (2015) Effect of polypharmacy, potentially inappropriate medications and anticholinergic burden on clinical outcomes: a retrospective cohort study. CMAJ 187:E130–E137
Wimmer BC, Bell JS, Fastbom J, Wiese MD, Johnell K (2016) Medication regimen complexity and polypharmacy as factors associated with all-cause mortality in older people: a population-based cohort study. Ann Pharmacother 50:89–95
Schisterman EF, Cole SR, Platt RW (2009) Overadjustment bias and unnecessary adjustment in epidemiologic studies. Epidemiology 20:488–495
Austin PC (2013) The performance of different propensity score methods for estimating marginal hazard ratios. Stat Med 32:2837–2849
Acknowledgements
This study was funded by the Federal Ministry of Education and Research (Berlin, Germany) [grant number 01GY1320A]. We are thankful to Walter Emil Haefeli and his employees at the Department of Clinical Pharmacology and Pharmacoepidemiology, University of Heidelberg, who designed the data collection procedure about drugs at the home visit and prepared the data. Andreas Meid (same institution) was one of the pharmacists who judged the ATC codes of all drugs available on the German market regarding their propensity of causing ADRs or drug-drug interaction.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The ESTHER study was approved by the ethics committees of the Medical Faculty of the University of Heidelberg and the Medical Association of Saarland and is being conducted in accordance with the Declaration of Helsinki.
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
ESM 1
(DOCX 107 kb)
Rights and permissions
About this article
Cite this article
Schöttker, B., Saum, KU., Muhlack, D.C. et al. Polypharmacy and mortality: new insights from a large cohort of older adults by detection of effect modification by multi-morbidity and comprehensive correction of confounding by indication. Eur J Clin Pharmacol 73, 1041–1048 (2017). https://doi.org/10.1007/s00228-017-2266-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-017-2266-7