Abstract
The aim of this study was to develop and characterize coatings of bioglass nanoparticles (BGNs) on biopolymer (poly [glycolide-co-L-lactide], (PGLA)) surgical sutures, and to investigate the effects of these coatings on the performance of the sutures as they slid through a skin substitute. Melt-derived BGNs were used to coat resorbable PGLA biopolymers, providing them with bioactivity, biocompatibility, and improved physical and mechanical properties. The structural, thermal, and physical properties of the coated and uncoated biopolymers were analyzed using Differential Scanning Calorimetry (DSC), Fourier Transform Infrared Spectroscopy (FTIR), Field Emission Scanning Electron Microscopy (FE-SEM) and Energy-Dispersive X-ray Spectroscopy (EDXS). The dissolution profiles and bioactivity of the BGNs-coated PGLA biopolymers were assessed through Inductively Coupled Plasma Optical Emission Spectrometry (ICP-OES). Tensile strength tests were conducted on the biopolymers before and after immersion in simulated body fluid to evaluate the impact of the BGNs coating on the degradation of PGLA biopolymers. Incorporating BGNs into PGLA resulted in improved tensile strength properties. The study also found that increasing the BGNs ions content facilitated the formation of a hydroxycarbonate apatite (HCA) layer in Dulbecco’s Modified Eagle Medium and medium with L-glutamine and sodium bicarbonate solutions. In vitro bioactivity tests demonstrated that the coated suture biopolymers exhibited enhanced attachment, migration, and proliferation of fibroblasts, indicating favorable biocompatibility of the biomaterial for clinical applications.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The use of surgical sutures remains prevalent in wound closure due to their easy availability, simplicity, and effectiveness, offering crucial mechanical support for wound healing and coming in various materials tailored to specific needs [1, 2]. Absorbable sutures are suitable for longer healing times, while non-absorbable ones provide extended mechanical support, with some materials minimizing tissue reaction or infection, making them ideal for high-risk wounds [3, 4]. Suture biomaterials play a vital role in wound closure, offering a diverse selection of polymers, including absorbable and non-absorbable types, sourced from natural or synthetic origins and structured as monofilament or multifilament strands [5]. Although non-absorbable sutures like nylon, silk, and polypropylene have long been favored for their durability and accessibility, concerns over chronic inflammation, infection, and tissue damage have spurred the search for alternative biomaterials [6, 7]. Researchers are exploring solutions such as absorbable sutures, including Polydioxanone, Polyglycolic acid, and Polyglactin 910, which offer advantages like reduced postoperative care. However, ensuring their degradation aligns with tissue healing and their by products are safe remains a technological challenge [8]. Thorough studies on the biocompatibility, biodegradability, and mechanical strength of absorbable sutures are underway to meet clinical standards where biocompatibility ensures safe interaction with the body, biodegradability enables safe absorption over time, and mechanical strength ensures sutures withstand tension and stress without damage [9]. Synthetic bioabsorbable sutures like Polyglactin 910, composed of polyglycolic acid (PGA), polylactic acid (PLA), and polyglycolide lactide copolymers (PGLA), have been extensively studied over the years [10]. Polyglactin 910 stands out for its remarkable attributes, including minimal tissue reactions, robust mechanical properties, and straightforward fabrication processes, making it a preferred choice for medical practitioners in various wound healing applications. However, suture biomaterials bioactivity can be enhanced by the addition of bioactive biomaterials such as bioactive glasses (BGs) [11]. Generally, bioactive glasses have shown high bioactivity and interactions with hard and soft tissues [12]. Various studies in the literature have shown that bioactive glasses, particularly those in the SiO2–CaO–P2O5–(Na2O) system, can establish a strong connection with both hard and soft tissues, although research on the interactions of hard ceramic particles in soft tissues is very limited. This is attributed to the rapid formation of a thin layer of hydroxycarbonate apatite (HCA) on the implant surface, closely resembling biological apatite with the bonding process occurring when the glass is implanted or comes into contact with biological fluids. Furthermore, researchers have discovered that bioactive glasses create an optimal environment for cell colonization, proliferation, and differentiation, which plays a crucial role in the formation of new tissue [13–14].
In the present experimental study, composite suture materials were fabricated by combining commercially available resorbable PGLA sutures with melt-derived bioactive glass (BGNs) powder using a slurry-dipping technique. This experimental study is based on the hypothesis that the presence of BGNs on the suture surface can enhance biocompatibility and stimulate cellular activity, thereby accelerating wound healing. Mechanical, thermal, physical, and biological properties were thoroughly investigated to assess the suitability of the composite suture materials, suggesting their potential for promoting wound healing.
Experimental study
Violet braided resorbable 3/0 Pegelak® (PGLA, (poly[glycolide-co-L-lactide], (90%:10%)) medical sutures were commercially obtained from Doğsan Inc. (İstanbul, Türkiye). (Melting point(Tm) ranging from 205 ≤ Tm ≤ 215 (℃) and inherent viscosity of 1.3 to 1.7 (dL/g). The Pegelak® suture, in its original commercial form, has an average diameter of 0.33 mm and comprises individual fibrils with diameters ranging from approximately 10–15 μm. Additionally, the suture is coated with a combination of lactide-glycolide copolymer and calcium stearate, creating a lubricant that is both absorbable and adherent, without flaking. To create 45S5 Bioactive glass nanoparticles (45 SiO2, 24.5 CaO, 24.5 Na2O, 6 P2O5 in (mol%) melt derived method), high purity powders of SiO2, Na2CO3, CaCO3, and P2O5 were weighted and combined. The raw powders were mixed for 6 h using a T2F turbula mixer, then melted at 1400 °C for 4 h in a Platinum crucible with a decarbonization phase of 5 h at 950 °C. Afterward, the melt was promptly quenched into distilled water (dH2O). The resulting frit glass was then ground down in a planetary ball mill using C2H5OH to a nanopowder size of ≤ 500 nm [15]. The composition of the bioglass was examined through chemical and spectral analysis to ensure no impurities were present after the preparation stages.
The composite sutures were produced using a slurry dipping technique, similar to the method used to coat surgical meshes and polymeric foams with 45S5 Bioglass particles, as reported earlier [16, 17], with some modifications. The slurry-dipping technique involved preparing an aqueous slurry consisting of a glass powder loading of 20 vol.-%. To prepare the solution, a 2% (w/v) solution of Sodium alginate (SA) was made by dissolving SA in dH2O at 80 °C while stirring constantly for 4 h. Prior to the coating process, the BGNs were dispersed in C2H5OH using ultrasonication (SONICS, VCX/750, Ultrasonic processors, Newtown, U.S.A.) for 1 h to ensure even distribution throughout the solution. The bath temperature was then heated to 45–50 °C, and a specific amount of CTAB (0.05 mol L− 1, CTAB/BGNs = 25 mmol/g) was added to the BGNs suspension under magnetic stirring. The mixture was kept at this temperature for 12 h with continuous stirring and aged for 24 h at RT. After centrifugation, the surface-modified BGNs precipitate was obtained. The surface-modified, dried BGNs were then dispersed in 1 mL of dH2O using ammonium polyacrylate solution (50 µl, DARVAN® 821-A) as a dispersing agent. Next, surface modified BGNs were gradually added to dH2O/SA and continuously mixed using a magnetic stirrer at 200 rpm to prevent particle sedimentation. The aqueous slurry was allowed to stabilize for 24 h at room temperature to achieve the desired composition. After 24 h, the suture samples were cut into 30 mm lengths and carefully dipped into the slurry using tweezers and left to immerse for 5 min. Following immersion, the samples were gently removed at a withdrawal velocity of ≈ 5 cm s− 1 to avoid damage. The suture samples were then dried on glass plates in a humid atmosphere at room temperature. The process involved dipping the coated sutures in a 0.1 M NaCl solution for 5 min for cross linking, followed by rinsing in warm dH2O for 10 min. The sutures were then dried on glass plates in a humid atmosphere at ambient temperature to prevent the formation of micro-cracks in the BGNs coating. The resulting samples were identified as PGLA (commercial) and PGLA/BGNs, respectively.
Biomaterials characterizations
Fourier transform infrared (FTIR) spectroscopy
For FTIR spectroscopy, the PGLA suture and the PGLA/BGNs suture samples were first dried in air before performing ATR-FTIR spectroscopy. The Bruker Alpha II FTIR Spectrophotometer (Germany) was used to collect the spectra, with 128 scans acquired in the wavenumber range from 400 to 4000 cm− 1. By comparing the spectra of the PGLA suture and the PGLA/BGNs suture samples, differences in their chemical composition and bonding were identified and provided insight into their physical properties and potential applications.
Field emission scanning electron microscopy and energy-dispersive X-ray spectroscopy (FE-SEM, EDXS) analyses
To analyze the morphologies of the coated and uncoated suture samples, FE-SEM instrument with an accelerating voltage of 15–25 kV was used. To prepare the samples, the suture samples were transferred onto a sample stage with carbon tape conductive film and coated with gold using an ion sputter coater (SCM-200 (Polaris), Republic of Korea). The surface composition analysis of the PGLA and PGLA/BGNs suture samples was carried out by using EDXS (INCA IE 350, U.K.) instrument, which was attached to a FE-SEM.
Differential scanning calorimetry (DSC), differential thermal analysis (DTA) and thermogravimetric analysis (TGA)
To analyze the thermal transitions of suture materials and evaluate the impact of the coating on the suture samples, thermal analysis was performed using a Perkin Elmer Pyris Diamond DSC Differential Scanning Calorimeter (Champaign, IL, U.S.A.) The samples tested were 4 mg of PLGA and PGLA/BGNs, placed in platinum pans in an N2 atmosphere [18]. A heating rate of 10 °C.min− 1 was applied to all samples, which were cooled to 0 °C and held for one minute before being heated to a temperature range of 0–220 °C. The resulting data showed heat flow versus temperature, and the glass transition temperature (Tg) was determined by observing a change in the upward direction of the heat flow, with the onset of change used to calculate the value. To analyze the thermal and degradation profiles of PLGA and PGLA/BGNs suture samples, DTA/TGA was performed using a DTG 60 series TG/DTA thermal analyzer (Schimadzu, Japan). The samples were scanned at a rate of 5 °C.min− 1 between 20 °C and 500 °C, and measurements were collected over three repeats using a 4 mg sample mass. DSC and TGA measurements were conducted in replicate.
Mechanical properties (tensile strength)
The AGX™-V2 Universal/Tensile testing machine (Schimadzu, Japan) was used to measure the mechanical properties of the PGLA and PGLA/BGNs suture samples. The testing was carried out using a gauge length of 20 mm and a crosshead speed of 20 mm/min [19]. Prior to mechanical testing, the PGLA and BGNs-coated suture samples were soaked in simulated body fluid (SBF) after they were received and produced. The SBF solution was prepared based on the recipe of Kokubo et al. found in the literature [20]. To avoid any biological degradation caused by bacteria or fungi, an antibiotic (Cefamezin 1000 mg IM/IV) was added at a concentration of 1% v/v. The pH of the solution was kept constant at 7.2. The suture samples were then immersed in the SBF solution and placed in a shaker at 150 rpm and 37 °C for 0, 7, 14, and 21 days. The SBF solution was replaced twice a week. After being taken out of the incubator, the suture samples were rinsed first with pure C2H5OH and then with dH2O. Mechanical testing was carried out on the suture samples immediately after being washed with dH2O. The stress and strain properties of both types of suture samples were recorded, and the mean and standard deviation are reported for n = 6.
In vitro cytocompatibility
L929 cells were cultured in DMEM supplemented with 1% (v/v) pre-made penicillin (100 units/mL) and streptomycin (100 units/mL) solution, as well as 10% (v/v) fetal bovine serum (FBS). 2 mg of the PGLA and PGLA/BGNs suture samples were added to 96-well plates, with some wells left empty as controls. L929 cells with a density of 1 × 104 cells/mL (200 µL) were then added to each well and incubated for 24 and 48 h. Afterward, XTT (2,3-Bis-(2-Methoxy-4-Nitro-5-Sulfophenyl)-2 H-Tetrazolium-5-Carboxanilide) solution (0.5% w/v) and fresh DMEM were added to each well and incubated for 4 hours at 37 °C. Optical density values of the resulting solutions were measured at 475 nm using a Multiskan Photometer (Thermo Scientific, U.S.A.). Triplicate conditions were included in each experiment, and three independent experiments were conducted [21].
Ion leaching experiments by ICP-OES
The dissolution of the suture samples in RPMI 1640 and DMEM cell culture medium was investigated through static dissolution studies. To verify the ionic leaching patterns of PGLA/BGNs suture samples ICP-OES (ICP-OES, iCAP 6000, Thermo Scientific, Waltham, MA, U.S.A.) was used. In these studies, 75 mg of PGLA/BGNs suture samples were dispersed in 50 mL of medium [22], and placed in an orbital shaker at 37 °C with agitation at 90 rpm for 4 h. The dissolution mediums pH was adjusted to 7.4 using a solution containing 1 M hydrochloric acid (HCl) and 0.5 M lactic acid (C3H6O3). Samples of the dissolution ion media were collected at various time points (10, 30, 60, 120, and 240 min) after immersion of the suture samples and filtered using a 0.22 μm pore filter from Millipore to remove contaminants and aggregates before being analyzed by ICP-OES.
Statistical analysis
Statistical analysis was conducted using the analysis of variance (ANOVA) method with a post-hoc Tukey test. A significance level of p < 0.05 was used to determine statistical significance. The data is indicated with * for p < 0.05 and ** for p < 0.01.
Results and discussion
FTIR Spectrum of suture samples
For the surgical suture samples, the stretching vibrations and symmetric or asymmetric bendings of the structure formed on the surface of the suture samples were investigated using FTIR spectroscopy, as shown in Fig. 1.
Signals corresponding to OH¯ functional groups were detected in the spectral range of 3867 cm− 1 to 3621 cm− 1 between the modified and non-modified suture samples. The shift in signals observed for the PGLA/BGNs sutures can be attributed to their interaction with the bioglass particles during the coating process, wherein H2O molecules reacted with the bioglass to form surface layers of OH¯ [23]. These hydroxides interacted with the suture surface, resulting in slight changes in the signals and producing slightly broader and sharper peaks. Signals corresponding to the vibration of νas(–CH2–), ν(–CH2–) and ν(–CH3) functional groups were detected in the spectral range of 2920 cm− 1 to 2350 cm− 1. The primary peak associated with the C − H group in this region was prominently observed in the uncoated PGLA suture. The incorporation of BGNs into the PGLA suture samples resulted in reduced intensities of the peaks between 1413 cm− 1-1746 cm− 1. This reduction is attributed to the sensitivity of these functional groups in PGLA to the electronegative disturbance caused by BGNs on the PGLA polymers surface. This causes a modification in the electronic cloud of the functional group through a Van der Waals repulsion phenomenon [24]. In the PGLA suture samples, another characteristic vibration of ν(C − O−C) was observed at 1068 cm− 1. However, this signal was degraded in PGLA/BGNs suture samples, indicating a strong interaction between BGNs and the suture surface. The bands at 1014 cm− 1 and 798 cm− 1 were associated with the robust vibrations of the SiO2 functional groups in the PGLA/BGNs suture samples, indicating a strong coupling between the BGNs. Moreover, signals associated with \( {\text{P}\text{O}}_{4}^{3-}\)of the BGNs were detected, which are highly sensitive to this wavenumber [25, 26].
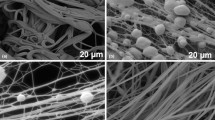
Examination of the morphology, distribution, and elemental composition of suture samples
To qualitatively evaluate the morphology and uniformity of the BGNs coatings on suture samples, visual inspection and FE-SEM analysis of the BGNs adhered to the PGLA surface were conducted. Figures 2 and 3 represent FE-SEM micrographs, while Fig. 4 shows elemental analysis using the EDXS spectrum of the PGLA and PGLA/BGNs suture samples. Results showed that BGNs produced more uniform, stable, and adherent coatings, which could be controlled to increase the coating thickness while reducing micro crack development. Coating with BGNs also resulted in slightly rougher fibers than uncoated sutures due to the presence of the coating. Furthermore, EDXS and FTIR analysis confirmed the presence of BGNs in the coated suture composites. The average diameter of the fibers for each suture samples was determined by Image J analysis software, with the PGLA and PGLA/BGNs samples achieving uniform, cylindrical, and stable fibers with a diameter of ~ 13.85 ± 0.11 μm and 19.25 ± 0.14 μm, respectively.
The adhesion strength of BGNs to coated suture surfaces is an important factor in determining the performance and reliability of the sutures in surgical applications. Quantitative evaluation of the adhesion strength of BGNs nanoparticles to the coated suture surfaces was not possible, but FE-SEM was used to qualitatively demonstrate that the coatings remained mostly intact after knotting and surgery. Microscopic photos revealed that suture samples coated with BGNs exhibited less exfoliation, which can be a common problem in surgical sutures (Fig. 3). This could be attributed to the surface modification of the BGNs particles during synthesis, which enhanced their compatibility with the suture material. It is believed that that the observed strong adhesion between the BGNs and the suture surfaces resulted from a mechanical interlocking mechanism between the nanoparticles and the suture surface structure. The mechanical interlocking mechanism is advantageous since it is not affected by environmental factors such as pH, temperature, and humidity, which can weaken chemical bonds [27, 28]. The observed mechanical interlocking mechanism between the nanoparticles and the suture surfaces is a promising approach for enhancing the performance and reliability of surgical sutures [29].
FE-SEM/EDXS spectra were used to analyze the composition of the crystalline particles present on the surface of the suture samples coated with BGNs and as received PGLA suture samples. The collected spectra and calculated values were presented in Fig. 4. The EDXS spectrum for coated samples demonstrated a high concentration of calcium, phosphorus, silicon, and sodium, which are all present in the bioglass composition [30]. This indicated that these ions were either incorporated into the BGNs layer or that the thickness of the coated layer was greater than that of uncoated suture samples. The EDXS results for PGLA/BGNs samples revealed inclusion peaks of silicon and sodium within the calcium phosphate phase, providing support for the difference in morphology observed in the FE-SEM images compared to uncoated suture samples.
The EDXS spectra of PLGA and PGLA/BGNs suture samples. PLGA exhibits peaks for carbon, nitrogen, oxygen, and chloride elements, validating its integrity for biomedical applications. In contrast, PGLA/BGNs suture shows peaks for calcium, phosphorus, silicon, sodium and magnesium, confirming successful integration of BGNs, potentially enhancing its bioactivity for surgical procedures
Thermal analysis studies
In this experimental study, the thermal transitions in both types of sutures were resolved by conducting DSC investigations using a constant heating rate. Figure 5 illustrates the distinctive DSC scans obtained during the heating and cooling of PGLA and PGLA/BGNs samples. The results were presented in Fig. 5 and Table 1 for PGLA and PGLA/BGNs sutures, respectively.
The PGLA and PGLA/BGNs samples displayed two Tg transitions each, as depicted in Fig. 5a with enlarged insets. These transitions can be attributed to distinct regions of the amorphous polymeric chains in this semi-crystalline polymer. The results indicate no significant differences between the PGLA and PGLA/BGNs samples when comparing them to each other. This double transition aligns with existing literature. For instance, Taddei et al. [31] observed two similar transitions at around 48 °C and 63 °C in their DSC study, characterizing polyglactin polymer membranes. Furthermore, third Tg transitions were distinctly detected for both samples, occurring at 120.6 ± 0.6 °C for PGLA and 117.9 ± 0.7 °C for PGLA/BGNs samples, respectively. Gilding et al. [32] also observed a third transition around 120 °C in the polyglactin and coated polyglactin polymer samples, which is consistent with the findings of this experimental study. Moreover, both types of sutures displayed a substantial melting peak at 195.6 ± 1.12 °C and 198.3 ± 0.9 °C, respectively. The degree of crystallinity (% Xc) was determined for these suture samples by measuring the enthalpy of melting (\( {\varDelta H}_{m}\)) in different samples and using the following Eq. (1) for calculation.
(\( {\varDelta H}_{m}\)) was determined by measuring the area under the melting peak, while (\( {\varDelta H}_{{m}^{0}}\)) represents the enthalpy of fusion of a 100% crystalline PGLA (the enthalpies of fusion of 139 J·g− 1, for 100% crystalline PGLA) [33, 34].
(a) DSC thermograms of PGLA and PGLA/BGNs samples, (b) enlarged inset graph highlighted in Fig. 5a
The results presented in Table 1 show that the degree of crystallinity varied slightly for the PGLA and PGLA/BGNs samples when measured up to 220 °C. Specifically, the degree of crystallinity for the PGLA sample was % Xc = 31.56, while for the PGLA/BGNs sample, it was % Xc = 29.31.
Thermal degradation analysis (TGA/DTA) was performed to evaluate the deterioration of the suture samples and determine the quantity of BGNs coating. The obtained results were illustrated in Fig. 6a and 6b, while Table 2 provides a summary of the transition regions observed for the PGLA and PGLA/BGNs samples. For the PGLA and PGLA/BGNs samples, melting occurred at 199.86 °C and 201.62 °C, respectively, as evidenced by the downward direction endothermic peaks [32]. Polymer degradation initiation was observed at temperatures exceeding 264.73 °C. The weight percentage of the BGNs coating was determined by comparing the mass percentages of the PGLA and PGLA/BGNs samples after each DTA run, assuming complete thermal degradation of the biopolymer.
The high residue amount observed in PGLA/BGNs samples was attributed to the presence of BGNs particles adhering to the suture surface. This finding shows enhanced adhesion of the coatings in the PGLA/BGNs suture samples, consistent with observations made using FE-SEM and EDXS techniques, thus confirming the findings. Conversely, the low residue amount detected in PGLA samples compared to PGLA/BGNs samples can be attributed to the zinc stearate coating material in its commercial form on the surface, as well as the dye applied to the surface of commercial PGLA materials [35].
Mechanical properties (tensile strength)
The mechanical performance of surgical suture material is its most defining characteristic. If a suture material lacks the durability to endure the pressures of surgical handling or lacks the strength to bring wound edges together, it fails to fulfill its primary purpose of closing wounds. On the other hand, if a suture material is excessively rigid and strong, it lacks the necessary elasticity to tie effective knots or expand appropriately with swelling, thereby hindering its performance and impeding wound healing [36]. It is crucial to strike a delicate balance between the tensile strength and elongation at break of suture materials. Consequently, these mechanical properties play a significant role in the development of innovative bioabsorbable sutures [37, 38]. The average maximum tensile strength of non-immersed suture samples of PGLA and PGLA/BGNs was determined to be approximately 470 MPa and 479 MPa, respectively. The presence of incorporated BGNs in PGLA slightly influences the tensile strength of the samples. However, notable changes were observed for both types of materials when subjected to immersion in SBF for different durations (0, 7, 14, and 21 days), as depicted in Fig. 7b. Initially, the sutures underwent alignment, with their fibers stretched along their axis. Subsequently, the tensile strength decreased with increasing immersion time from 0 to 21 days due to the failure of individual fibers before the ultimate fracture of the braided structure. When comparing the measurements at different immersion times for PGLA and PGLA/BGNs samples, the expected changes in tensile strength were observed, with slightly lower values calculated for longer immersion periods, as presented in Fig. 7b. Moreover, as degradation progressed, the results became more random, with slightly lower values recorded for longer immersion days. This behavior was also observed in the case of PGLA/BGNs suture samples, as indicated in Fig. 7b. Overall, the PGLA/BGNs suture samples exhibited marginally higher tensile strength compared to the PGLA samples. This discrepancy could potentially be attributed to the preparation technique used for the samples, wherein the sutures may not have suffered mechanical damage during the incorporation process of the BGNs.
(a) Schematic illustration of tensile test for surgical suture samples. (b) The results of a comprehensive study on the tensile strength of both PGLA and PGLA/BGNs suture samples. (c) Retention of tensile strength (%) and elongation at break (%) of PGLA and PGLA/BGNs suture samples as a function of incubation period in SBF. All data are represented as the mean (Standard deviation, ± SD) (p < 0.05; *Statistically significant differences between groups, n = 6)
In PGLA suture samples, the inclusion of BGNs particles in the structure and the mechanical bonding between each suture fiber led to an increase in tensile strength with prolonged immersion time, as compared to sutures without BGNs. Similar behavior was observed across all samples. In the case of PGLA/BGNs samples, preliminary experiments revealed that the non-uniform dispersion of BGNs particles created a heterogeneous environment within the structure, and the uneven distribution of grain sizes caused abrasion and tearing between the fibers. Therefore, achieving a homogeneous distribution of the coating throughout the structure and ensuring uniform particle distribution is of utmost importance. Figure 7c illustrates the percentage of strength retained ratio and elongation at break values for PGLA and PGLA/BGNs suture samples as a function of the number of days immersed in SBF. The decrease in tensile strength after 21 days of immersion in SBF ranged between 35% and 40%. The impact of shorter immersion periods on strength retention is less pronounced. However, as the immersion time increases, the values for strength retention decrease significantly.
According to the existing literature [39,40,41], degradation in biodegradable polymers typically initiates in the amorphous region before affecting the crystalline region. When a polymeric material is immersed in an aqueous solution, water molecules initially penetrate the amorphous regions while having limited access to the crystalline regions. As degradation progresses, tie-ends, chain-ends, and chain folds deteriorate into smaller fragments that eventually dissolve in the aqueous medium. Consequently, the previously occupied spaces within the chain segments become vacant, leading to the formation of visible cracks. These cracks are believed to originate on the PGLA fibers surface and propagate circumferentially towards the interior. As micro cracks develop, more water molecules can infiltrate these areas, further accelerating their propagation into the PGLA fiber’s interior until failure occurs. The remaining chain segments within the amorphous regions now exhibit increased mobility and are able to interact with each other more easily, leading to an observable rise in crystallinity [42]. The degree of crystallinity reaches its peak at the conclusion of the initial stage of degradation. Simultaneously, the maximum loss of tensile strength is observed during this first stage. In the subsequent stage, hydrolysis causes destruction of the crystalline lattice, resulting in reduced crystallinity. However, the complete loss of tensile strength, from the value achieved at the end of the first degradation stage to zero, occurs at a slower pace. Previous studies have indicated that the first stage of degradation prevails during the 21-day immersion period, while the significance of the second stage becomes more prominent thereafter [42, 43].
In this experimental study, the percentage of strength retained ratio (%) shows a decline after 7 days, and similar patterns were observed for PGLA/BGNs suture samples. The decrease in the strength retained ratio between day zero and the 7th day of degradation appears to be relatively gradual. However, a notable and significant change in the strength retained ratio (%) occurs, particularly for PGLA samples, after 14 days of immersion in SBF. An increased elongation at break typically enhances the handling characteristics, knot-tying capabilities, and knot tensile strength of suture materials, ultimately improving the overall performance of bioabsorbable sutures [36]. Upon analyzing the obtained elongation at break results, it was noted that the suture samples made of PGLA and PGLA/BGNs followed the degradation mechanisms described earlier. The incorporation of BGNs into the biopolymer system led to a slight reduction in the elongation at break compared to PGLA alone.
In vitro cytotoxicity assessment
The assessment of biocompatibility is an essential aspect of the development of biomaterials, which refers to the ability of the biomaterial to coexist with living tissue without causing any adverse effects. The biocompatibility of biomaterials is usually evaluated using in vitro tests. One of the most common in vitro tests used to evaluate biocompatibility is the cytotoxicity assay. This test involves exposing the material to living cells, typically in culture, to determine whether it causes any adverse effects on the cells. Cytotoxicity tests are a crucial step in the evaluation of biomaterials as they provide insights into the potential toxicity of the material, which can help ensure patient safety.
In this experimental study, cell viability (%) was measured using the XTT assay on three groups: a control group, a PGLA group, and a PGLA/BGNs group, all of which were cultured with mouse fibroblast L929 cells in 96-well plates. After 24 and 48 h in culture, the XTT activity of L929 cells treated with PGLA/BGNs groups was significantly higher than that of cells in the standard culture medium (Fig. 8). After 24 and 48 days in culture, the XTT activity in cells treated with dissolution ions from BGNs was significantly enhanced compared to the control and PGLA groups. Additionally, after 48 h in culture, the XTT activity was significantly greater in L929 cells treated with dissolution ions from BGNs-substituted PGLA compared to the PGLA group. At the beginning of the experiment, the metabolic activity of L929 cells that treated with PGLA and PGLA/BGNs groups was observed to be higher than the metabolic activity of cells treated with the control group, suggesting that the dissolution products of all groups did not show any harmful effects on the cells. Nonetheless, according to reference [44], the dissolution ions from the PGLA/BGNs groups containing BGNs increased the overall metabolic activity in cells after 24 and 48 h of being cultured, compared to both the control and PGLA groups. This finding supports previous research in the literature that has shown BGNs stimulate cell proliferation [45, 46]. It also suggests that the released ions from bioglass may have a synergistic effect with other ions, most likely silicon present in the synthesized BGNs. The interaction between the ions released from the bioglass and silicon from the BGNs could create a more conducive environment for cell proliferation and activity. This synergy may enhance cellular responses, such as increased proliferation rates or improved cell function, potentially leading to more effective tissue regeneration or repair outcomes.
(a) Schematic illustration for the in vitro cytotoxicity assessment steps. (b) Real photographs showing mouse fibroblast L929 cell viability in the control, PGLA, and PGLA/BGNs groups after 48 h. (c) The diagram shows the results of a cell viability assay using the XTT method, with the values representing the mean and ± SD of three independent experiments (n = 3). The asterisk symbol (*) indicates statistically significant differences between control groups, with a p-value of less than 0.05
Ion release profile and bioglass dissolution studies
An increasing amount of evidence in the literature suggests that the key factor to understanding the behavior of BGNs-based biomaterials in vitro and invivo is to study the stimulation effects of dissolution products released from BGNs during the tissue regeneration process [47, 48]. The biological response of cells/tissues to BGNs substituted PGLA, produced by a dip coating process and dissolution ions, will be discussed. To evaluate the ion dissolution behavior of all samples without having interference from the media with the ICP-OES measurement, DMEM and RPMI 1640 cell culture medium solution were selected. Samples were immersed in cell culture medium solutions under the same conditions as the previously described in vitro bioactivity studies in the literature [49–50]. The dissolution behavior of calcium (Ca), phosphorous (P) and silicon (Si) ions released from BGNs substituted PGLA samples into DMEM and RPMI 1640 in ppm was plotted as a function of time for 240 min in Fig. 9.
The findings, as revealed by ICP-OES data analysis, demonstrated that the concentrations of these ions exhibited differences over time during incubation period. Differences in the release rates observed for Ca, Si, and P elements in different cell culture media such as DMEM and RPMI 1640 are attributed to the varying compositions of salts, amino acids, vitamins, and other nutrients in DMEM and RPMI 1640 solutions [51]. These differences in media composition can impact the solubility and stability of calcium, silicon, and phosphorus compounds, thereby influencing their release rates.
As shown in Fig. 9a, in the analyzes performed in the DMEM cell culture environment, according to the results obtained at the 10 min. incubation time, the Ca concentration was measured as 65.2 ppm, the Si concentration was 8.51 ppm, and the P concentration was 26.14 ppm, respectively. The highest value was observed for Ca concentration, determined as 86.2 ppm at the 30 min. incubation time. As the incubation time increased from 10 min. to 240 min., it was observed that the Si concentration increased regularly (from 8.51 ppm to 44.74 ppm), while the P concentrations decreased linearly (from 26.14 ppm to 7.23 ppm). It was determined that the Ca concentration tends to first increase and then decrease (from 86.2 ppm to 72.6 ppm).
Interestingly, when comparing RPMI 1640 and DMEM, distinct data emerged regarding the changes in Ca concentration. In RPMI 1640, there was a noticeable decrease in Ca concentration with increasing incubation time. In contrast, DMEM showed relatively stable and higher Ca levels throughout the incubation period, as indicated by ICP-OES data. As shown in Fig. 9b, in the analyses performed in RPMI 1640 cell culture medium, the highest P concentration was measured as 181.2 ppm at the 10 min. During the same incubation period, the Ca concentration was measured as 22.5 ppm, and the Si concentration was 3.76 ppm. When the incubation time increased from the 10 min. to the 240 min., all ion release values showed a stable trend, while Ca and P concentrations decreased steadily, except for the Si concentration. As the incubation time increased from 10 min. to 240 min., it was observed that the Si concentration increased regularly (from 3.4 ppm to 6.2 ppm), while the P and Ca concentrations decreased linearly from 181.2 ppm to 156.2 ppm and 22.4 ppm to 17.7 ppm respectively. Especially considering that a significant phosphorus concentration reaching 156.2 ppm was observed in RPMI 1640 cell culture medium, the release of both Ca and P from BGNs could lead to the formation of a supersaturated solution in the medium. This supersaturated environment then enables amorphous Ca3(PO4)2 to precipitate. As time progresses, this amorphous Ca3(PO4)2 eventually undergoes crystallization and transforms into the apatite phase (a group of phosphate minerals, Ca5(PO4)3(F, Cl, OH)), which is renowned for its biocompatibility and bioactivity in the environment [50]. The presence of the apatite phase, highly desirable in living environments, renders it an ideal material for various biomedical applications, particularly in the field of hard and soft tissue regeneration.
As a result, the controlled release of several essential ions, including Si, Ca, Na and P, from the bioactive glass has been associated with numerous beneficial properties that facilitate bioactivity, angiogenesis, osteoconduction, and other critical processes involved in tissue regeneration [13, 52,53,54]. The orchestrated release of these ions from the BGNs creates a favorable microenvironment that promotes cell proliferation, differentiation, and tissue integration. The presence of Si, in particular, significantly contributes to the glass’s bioactive properties, enhancing its potential to stimulate tissue regeneration. Silicon, an element believed to be involved in the cell-stimulating activities of BGNs dissolution ions due to its crucial role in the formation of new tissue, gradually releases into the culture media [55]. Additionally, the controlled release of Ca and P not only aids in the formation of the Ca3(PO4)2 layer, as mentioned earlier, but also provides essential building blocks for the development and mineralization of new tissue. Figure 10 schematically illustrated the controlled release of Si, Ca, Na, and P ions from bioactive glass and their effects on bioactivity for tissue regeneration.
Conclusions
The application of bioglass nanoparticles (BGNs) coatings onto poly [glycolide-co-L-lactide] (PGLA) surgical sutures for biomedical purposes was accomplished through a slurry dip coating method. Employing several complementary thermal analysis techniques, spectral analyses, chemical and mechanical performance tests facilitated diverse characterizations, leading to a comprehensive comprehension of how the BGNs coating technique influenced the morphological properties of both the commercially received and prepared surgical suture biomaterials.
FTIR, EDXS, and FE-SEM analyses confirmed the presence of BGNs within the surgical sutures structure, obtained using the slurry dip coating technique. The results indicated that the surgical suture diameters increased from 13.85 ± 0.11 μm to 19.25 ± 0.14 μm with the penetration of BGNs into the biopolymer structure. The coating was observed to remain stable on the surfaces of the surgical suture samples even after knot tests were performed. In thermal analysis tests conducted at 10 °C.min− 1, the degree of crystallinity was found to be % Xc = 31.56 for the PGLA sample and % Xc = 29.31 for the PGLA/BGNs sample. Furthermore, downstream endothermic peaks provided evidence of melting points at 199.86 °C for PGLA and 201.62 °C for PGLA/BGN samples. The presence of incorporated BGNs in PGLA had a minor impact on the tensile strength of the surgical sutures. However, significant changes were observed for both material types when immersed in SBF for varying durations (0,7,14, and 21 days). Overall, the PGLA/BGNs suture samples showed slightly higher tensile strength (183 ± 4.2 MPa on day 21) compared to the PGLA samples (165 ± 7.5 MPa on day 21). Despite that, the BGNs coatings enhanced the strength retained ratio and elongation at break values during various degradation periods, suggesting a qualitative impact of the suture sample on the polymer degradation mechanism. On day 21, the strength retained ratio and elongation at break values were found to be 35.07 ± 2.32% and 6.7 ± 0.73%, respectively, for PGLA samples, while for PGLA/BGNs samples, they were determined to be 38.09 ± 2.24% and 3.25 ± 0.53%, respectively.
Furthermore, the in vitro cytotoxicity and ion release studies conducted on PGLA and PGLA/BGNs suture samples revealed intriguing findings. The presence of positively charged ions (such as \( {SiO}_{4}^{4-}, {Ca}^{2+}, {{{O}^{-}, Na}^{+}, PO}_{4}^{3-}),\)on the surgical suture surfaces appeared to promote cell proliferation, attributed to the dissolution of BGNs in the cell culture medium. The interaction of these ions with the cellular environment seemed to have a positive impact on cell growth. Moreover, the results obtained from the ICP-OES data analyses performed in different in vitro environments, namely RPMI 1640 and DMEM cell culture medium, further supported these findings. These analyses indicated that the concentrations of the aforementioned ions increased progressively over time during the incubation period. This observation suggests that the BGNs coatings on the suture surfaces facilitated the release of these beneficial ions, contributing to enhanced cellular responses and potential therapeutic effects. These promising outcomes open up new possibilities for developing advanced biomaterials with improved biocompatibility and soft tissue regeneration capabilities.
Data availability
The manuscript data and images are available upon request.
References
Spotnitz, W.D., Falstrom, J.K., Rodeheaver, G.T.: The role of sutures and fibrin sealant in wound healing. Surg. Clin. North. Am. 77(3), 651–669 (1997). https://doi.org/10.1016/s0039-6109(05)70573-9
Neligan, P.C.: Bioactive sutures. Plast. Reconstr. Surg. 118(7), 1645–1647 (2006). https://doi.org/10.1097/01.prs.0000248418.23513.1f
Akgun, U., Karahan, M., Randelli, P.S., Espregueira-Mendes, J.: Knots in Orthopedic Surgery. (2018). https://doi.org/10.1007/978-3-662-56108-9
Ajmeri, J.R.: M.C.J. Ajmeri Surgical sutures: The Largest Textile Implant Material. Med. Textiles Biomaterials Healthc. 432–440 https://doi.org/10.1533/9781845694104.7.432 (2006)
Joseph, B., George, A., Gopi, S., Kalarikkal, N., Thomas, S.: Polymer sutures for simultaneous wound healing and drug delivery– A review. Int. J. Pharm. 524(1–2), 454–466 (2017). https://doi.org/10.1016/j.ijpharm.2017.03.041
Nair, L.S., Laurencin, C.T.: Biodegradable polymers as biomaterials. Prog Polym. Sci. 32(9), 8 (2007). https://doi.org/10.1016/j.progpolymsci.2007.05.017
Setiawati, A., Jang, D., Cho, D., Cho, S., Jeong, H., Park, S., Gwak, J., Ryu, S.R., Jung, W.H., Ju, B., Jung, K., Kwon, O., Shin, K.: An accelerated wound-healing surgical suture engineered with an extracellular matrix. Adv. Healthc. Mater. 10(6), 2001686 (2021). https://doi.org/10.1002/adhm.202001686
Ai, C., Sheng, D., Chen, J., Cai, J., Wang, S., Jiang, J., Chen, S.: Surface modification of vascular endothelial growth factor-loaded silk fibroin to improve biological performance of ultra-high-molecular-weight polyethylene via promoting angiogenesis. Int. J. Nanomed. 12, 7737–7750 (2017). https://doi.org/10.2147/ijn.s148845
Pasternak, B., Missios, A., Askendal, A., Tengvall, P., Aspenberg, P.: Doxycycline-coated sutures improve the suture-holding capacity of the rat Achilles tendon. Acta Orthop. 78(5), 680–686 (2007). https://doi.org/10.1080/17453670710014392
Lee, K.H., Chu, C.C.: The role of superoxide ions in the degradation of synthetic absorbable sutures. J. Biomed. Mater. Res. 49(1), 25–35 (2000). https://doi.org/10.1002/(sici)1097-4636(200001)49:1%3C25: aid-jbm4 > 3.0.co;2-i
Chu, C.C.: The effect of pH on the in vitro degradation of poly(glycolide lactide) copolymer absorbable sutures. J. Biomed. Mater. Res. 16(2), 117–124 (1982). https://doi.org/10.1002/jbm.820160204
Jones, J.R., Brauer, D.S., Hupa, L., Greenspan, D.C.: Bioglass and Bioactive glasses and their impact on Healthcare. Int. J. Appl. Glass Sci. 7, 423–434 (2016)
Özer, A., Öksüz, K.: The effect of yttrium oxide in hydroxyapatite/aluminum oxide hybrid biocomposite materials: Phase, mechanical and morphological evaluation. Mater. Werkst. 50(11), 1382–1390 (2019). https://doi.org/10.1002/mawe.201800141
Göksen Tosun, N., Özer, A., Bektaş, T., Öksüz, K.E., Tayhan, E., Özdemir, S.: Silk sericin-hydroxyapatite nanoribbons toward structurally stable osteogenic scaffolds. J. Aust Ceram. Soc. 59, (1291-1301) (2023). https://doi.org/10.1007/s41779-023-00909-4
Öksüz, K.E., Kurt, B., Şahin İnan, Z.D., Hepokur, C.: Novel bioactive glass/graphene oxide-coated surgical sutures for soft tissue regeneration. ACS Omega. 8(24), 21628–21641 (2023). https://doi.org/10.1021/acsomega.3c00978
Roether, J., Boccaccini, A., Hench, L., Maquet, V., Gautier, S., Jérôme, R.: Development and in vitro characterisation of novel bioresorbable and bioactive composite materials based on polylactide foams and Bioglass® for tissue engineering applications. Biomater. 23(18), 3871–3878 (2002). https://doi.org/10.1016/s0142-9612(02)00131-x
Stamboulis, A., Boccaccini, A., Hench, L.: Novel biodegradable polymer/bioactive glass composites for tissue engineering applications. Adv. Eng. Mater. 4(3), 105 (2002). https://doi.org/10.1002/1527-2648(200203)4:3%3C105::aid-adem105%3E3.0.co;2-l
Öksüz, K.E.: Macro-porous aluminum oxide-boron carbide ceramics for hard tissue applications. Recep Tayyip Erdoğan Üniversitesi Fen Ve Mühendislik Bilimleri Dergisi. 4(2), 65–75 (2023). https://doi.org/10.53501/rteufemud.1293580
Peng, X., Liu, G., Zhu, L., Yu, K., Qian, K., Zhan, X.: In vitro and in vivo study of novel antimicrobial gellan–polylysine polyion complex fibers as suture materials. Carbohydr. Res. 496, 108115 (2020). https://doi.org/10.1016/j.carres.2020.108115
Ebisawa, Y., Kokubo, T., Ohura, K., Yamamuro, T.: Bioactivity of CaO.SiO2-based glasses: In vitro evaluation. J. Mater. Sci. Mater. Med. 1(4), 239–244 (1990). https://doi.org/10.1007/bf00701083
Öksüz, K.E., Özkaya, N.K., İnan, Z.D.A., Özer, A.: Novel natural spider silk embedded electrospun nanofiber mats for wound healing. Mater. Today Commun. 26, 101942 (2021). https://doi.org/10.1016/j.mtcomm.2020.101942
Maçon, A.L.B., Kim, T.B., Valliant, E.M., Goetschius, K., Brow, R.K., Day, D.E., Hoppe, A., Boccaccini, A.R., Kim, I.Y., Ohtsuki, C., Kokubo, T., Osaka, A., Vallet-Regí, M., Arcos, D., Fraile, L., Salinas, A.J., Teixeira, A.V., Vueva, Y., Almeida, R.M., Jones, J.R.: A unified in vitro evaluation for apatite-forming ability of bioactive glasses and their variants. J. Mater. Sci. Mater. Med. 26(2) (2015). https://doi.org/10.1007/s10856-015-5403-9
Öksüz, K.E., Kilinç, S., Özer, A.: Effect of calcination on microstructure development and properties of hydroxyapatite powders extracted from human and bovine bones. Trans. Indian Ceram. Soc. 78(1), 41–45 (2019). https://doi.org/10.1080/0371750x.2019.1588170
Ku Aizuddin, K.A., Chit, F., Gurmeet Kaur Surindar, S., Meor Mohd Redzuan, S.: Physicochemical characterization of astaxanthin-loaded PLGA formulation via nanoprecipitation technique. J. Appl. Pharm. Sci. (2020). https://doi.org/10.7324/japs.2021.110606
Hench, L.L., Polak, J.M.: Third-generation biomedical materials. Sci. 295(5557), 1014–1017 (2002). https://doi.org/10.1126/science.1067404
Cacciotti, I., Lombardi, M., Bianco, A., Ravaglioli, A., Montanaro, L.: Sol–gel derived 45S5 bioglass: Synthesis, microstructural evolution and thermal behaviour. J. Mater. Sci. Mater. Med. 23(8), 1849–1866 (2012). https://doi.org/10.1007/s10856-012-4667-6
Smeets, R., Tauer, N., Vollkommer, T., Gosau, M., Henningsen, A., Hartjen, P., Früh, L., Beikler, T., Stürmer, E.K., Rutkowski, R., Grust, A.L.C., Fuest, S., Gaudin, R., Aavani, F.: Tissue adhesives in reconstructive and aesthetic surgery—application of silk fibroin-based biomaterials. Int. J. Mol. Sci. 23(14), 7687 (2022). https://doi.org/10.3390/ijms23147687
Ma, Z., Yang, Z., Gao, Q., Bao, G., Valiei, A., Yang, F., Huo, R., Wang, C., Song, G., Ma, D., Gao, Z.H., Li, J.: Bioinspired tough gel sheath for robust and versatile surface functionalization. Sci. Adv. 7(15) (2021). https://doi.org/10.1126/sciadv.abc3012
Blaker, J., Nazhat, S., Boccaccini, A.: Development and characterization of silver-doped bioactive glass-coated sutures for tissue engineering and wound healing applications. Biomater. 25(7–8), 1319–1329 (2004). https://doi.org/10.1016/j.biomaterials.2003.08.007
Fredholm, Y.C., Karpukhina, N., Brauer, D.S., Jones, J.R., Law, R.V., Hill, R.G.: Influence of strontium for calcium substitution in bioactive glasses on degradation, ion release and apatite formation. J. R Soc. Interface. 9(70), 880–889 (2011). https://doi.org/10.1098/rsif.2011.0387
Taddei, P., Monti, P., Simoni, R.: Vibrational and thermal study on the in vitro and in vivo degradation of a poly(lactic acid)-based bioabsorbable periodontal membrane. J. Mater. Sci. Mater. Med. 13(5), 469–475 (2002). https://doi.org/10.1023/a:1014742003146
Gilding, D., Reed, A.: Biodegradable polymers for use in surgery—polyglycolic/poly(actic acid) homo- and copolymers: 1. Polymer. 20(12), 1459–1464 (1979). https://doi.org/10.1016/0032-3861(79)90009-0
Chen, Y., Xie, K., He, Y., Hu, W.: Fast-scanning chip-calorimetry measurement of crystallization kinetics of poly (glycolic acid). Polymers. 13(6), 891 (2021). https://doi.org/10.3390/polym13060891
Magazzini, L., Grilli, S., Fenni, S.E., Donetti, A., Cavallo, D., Monticelli, O.: The blending of poly(glycolic acid) with polycaprolactone and poly(l-lactide): promising combinations. Polymers. 13 (16), 2780 (2021). https://doi.org/10.3390/polym13162780
Chu, C.: Types and properties of surgical sutures. Biotextiles as Med. Implants. 231–273 (2013). https://doi.org/10.1533/9780857095602.2.232
De la Harpe, K.M., Marimuthu, T., Kondiah, P.P.D., Kumar, P., Ubanako, P., Choonara, Y.E.: Synthesis of a novel monofilament bioabsorbable suture for biomedical applications. J. Biomed. Mater. Res. B Appl. Biomater. 110(10), 2189–2210 (2022). https://doi.org/10.1002/jbm.b.35069
Polykandriotis, E., Daenicke, J., Bolat, A., Grüner, J., Schubert, D.W., Horch, R.E.: Individualized wound closure-mechanical properties of suture materials. J. Pers. Med. 12(7), 1041 (2022). https://doi.org/10.3390/jpm12071041
Khiste, S.V., Ranganath, V., Nichani, A.S.: Evaluation of tensile strength of surgical synthetic absorbable suture materials: An in vitro study. J. Periodontal Implant Sci. 43(3), 130–135 (2013). https://doi.org/10.5051/jpis.2013.43.3.130
Bohorquez-Moreno, C.D., Öksüz, K.E., Dinçer, E.: Porous polymer scaffolds derived from bioresources for biomedical applications. Cellul Chem. Technol. 57(1–2), 107–116 (2023). https://doi.org/10.35812/cellulosechemtechnol.2023.57.11
Ginde, R.M., Gupta, R.K.: In vitro chemical degradation of poly(glycolic acid) pellets and fibers. J. Appl. Polym. Sci. 33(7), 2411–2429 (1987). https://doi.org/10.1002/app.1987.070330712
Li, S.: Hydrolytic degradation characteristics of aliphatic polyesters derived from lactic and glycolic acids. J. Biomed. Mater. Res. 48(3), 342–353 (1999). https://doi.org/10.1002/(sici)1097-4636(1999)48:3%3C342::aid-jbm20%3E3.0.co;2-7
Zhang, Y., Chu, C.C.: Biodegradable dextran-polylactide hydrogel networks: Their swelling, morphology and the controlled release of indomethacin. J. Biomed. Mater. Res. 59(2), 318–328 (2001). https://doi.org/10.1002/jbm.1248
Migliaresi, C., Fambri, L., Cohn, D.: A study on the in vitro degradation of poly (lactic acid). J. Biomater. Sci. Polym. Ed. 5(6), 591–606 (1994). https://doi.org/10.1163/156856294x00220
Xynos, I.D., Edgar, A.J., Buttery, L.D., Hench, L.L., Polak, J.M.: Ionic products of bioactive glass dissolution increase proliferation of human osteoblasts and induce insulin-like growth factor ii mrna expression and protein synthesis. Biochem. Biophys. Res. Commun. 276(2), 461–465 (2000). https://doi.org/10.1006/bbrc.2000.3503
Nandhakumar, M., Thangaian, D.T., Sundaram, S., Roy, A., Subramanian, B.: An enduring in vitro wound healing phase recipient by bioactive glass-graphene oxide nanocomposites. Sci. Rep. 12(1), 16162 (2022). https://doi.org/10.1038/s41598-022-20575-z
Boonlom, T., Bryce, F., Paul, F.A., Wright, T., Turney, W.: Effect of pre-treatment of crystallized bioactive glass with cell culture media on structure, degradability, and biocompatibility. Mater. Sci. Eng. C. 97, 188–197 (2019). https://doi.org/10.1016/j.msec.2018.12.034
Hench, L.L.: The story of Bioglass®. J. Mater. Sci. Mater. Med. 17(11), 967–978 (2006). https://doi.org/10.1007/s10856-006-0432-z
Hench, L.L., Jones, J.R.: Bioactive glasses: Frontiers and challenges. Front. Bioeng. Biotechnol. 3 (2015). https://doi.org/10.3389/fbioe.2015.00194
Zhang, M., Wu, C., Lin, K., Fan, W., Chen, L., Xiao, Y., Chang, J.: Biological responses of human bone marrow mesenchymal stem cells to Sr-M‐Si (M = zn, mg) silicate bioceramics. J. Biomed. Mater. Res. A. 100 A 11, 2979–2990 (2012). https://doi.org/10.1002/jbm.a.34246
Gentleman, E., Fredholm, Y.C., Jell, G., Lotfibakhshaiesh, N., O’Donnell, M.D., Hill, R.G., Stevens, M.M.: The effects of strontium-substituted bioactive glasses on osteoblasts and osteoclasts in vitro. Biomater. 31(14), 3949–3956 (2010). https://doi.org/10.1016/j.biomaterials.2010.01.121
Cantor, J.R., Abu-Remaileh, M., Kanarek, N., Freinkman, E., Gao, X., Louissaint, A., Lewis, C.A., Sabatini, D.M.: Physiologic medium Rewires Cellular Metabolism and reveals uric acid as an endogenous inhibitor of UMP synthase. Cell. 169(2), 258–272e17 (2017). https://doi.org/10.1016/j.cell.2017.03.023
Cacciotti, I.: Cationic and anionic substitutions in hydroxyapatite. In: Antoniac, I.V. (ed.) Handbook of Bioceramics and Biocomposites, pp. 1–68. Springer, Heidelberg (2014)
Jones, J.R., Brauer, D.S., Hupa, L., Greenspan, D.C.: Bioglass and bioactive glasses and their impact on healthcare. Int. J. Appl. Glass Sci. 7(4), 423–434 (2016). https://doi.org/10.1111/ijag.12252
Lopes, J.H., Souza, L.P., Domingues, J.A., Ferreira, F.V., Alencar Hausen, M., Camilli, J.A., Martin, R.A., Duek, R., Mazali, E.A., Bertran, I.O.: In vitro and in vivo osteogenic potential of niobium-doped 45S5 bioactive glass: A comparative study. J. Biomed. Mater. Res. B Appl. Biomater. 108(4), 1372–1387 (2020). https://doi.org/10.1002/jbm.b.34486
Jones, J.R., Gentleman, E., Polak, J.: Bioactive glass scaffolds for bone regeneration. Elements. 3(6), 393–399 (2007). https://doi.org/10.2113/gselements.3.6.393
Funding
Open access funding provided by the Scientific and Technological Research Council of Türkiye (TÜBİTAK).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declares no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Öksüz, K.E. Bioactive coatings on biopolymer materials: evaluation of mechanical, physical, thermal, and in vitro properties. J Aust Ceram Soc (2024). https://doi.org/10.1007/s41779-024-01037-3
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s41779-024-01037-3