Abstract
Air pollution (AP) represents one of the main environmental threats to public health and exposure to AP has been connected to upper airway (UA) disease. We evaluated the relationships between the ENT urgent referrals recorded at the Hospital of Padua and the daily levels of particulate matter (PM) as well as other environmental factors in a single year. Patients with UA disorders were included in the study group while those referred for facial trauma or foreign body inhalation formed the control group. Daily PM concentrations, meteorological data and the concentrations of the commonest aeroallergens were obtained. 6368 patients formed the study group and 910 the control one. The concentration of compositae allergens showed a positive effect on the total number of admissions (p = 0.001). PM10 did not demonstrate an effect on the total number of admissions or either the study or control groups admissions (p = 0.25). Alternaria positively influenced admissions of patients in the study group (p = 0.005). Significant relationships were found between the following: PM10 measured on the seventh day before A&E admission and rhinosinusitis (p = 0.007), PM10 on the fifth day and laryngitis (p = 0.01), PM10 on the second day and otitis media (p = 0.03), PM10 on the admission day and epistaxis (p = 0.0198). Our study confirms the causal relationship between aeroallergen concentration and ENT admissions. The levels of PM10 at specific days preceding A&E admission correlated with certain UA disorders. This study strongly points towards the harmful effects of pollution and climate change on UA disease.
Article Highlights
-
Air pollution represents one of the main environmental threats to public health and exposure to pollutants has been connected to upper airway (UA) diseases.
-
The relationships between the ear, nose and throat (ENT) urgent referrals registered in a single year at the Hospital of Padua and the daily levels of particulate matter (PM10) as well as other environmental factors measured in the same period were evaluated.
-
Our study confirms the relationship between PM10 levels, climate change and pollens levels.
-
A significant influence of Alternaria on the number of ENT referrals for UA disorders was demonstrated.
-
Levels of PM10 at specific days preceding the Accident and Emergency admission were found to correlate with the number of ENT referrals for certain UA disorders.
-
Accurate identification of the atmospheric factors and processes responsible for the increased UA morbidity might allow appropriate protocols to be adopted to minimize their impact on health.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Air pollution (AP) represents one of the main environmental threats to public health (Jo et al. 2017; European Environment Agency 2019). It is a heterogeneous mixture of gases, liquids, and solid particles including particulate matter (PM), nitric oxides (NOx), sulphur oxides, carbon monoxide (CO), and ozone (O3) (Jo et al. 2017). Inhalable PM is further classified according to the aerodynamic equivalent diameter of its particles as coarse (2.5–10 μm), fine (0.1–2.5 μm) and ultrafine (< 0.1 μm) with fine PM being able to reach the lungs (Michalska et al. 2020). Vehicle traffic and heating systems represent some of the most common urban outdoor emission sources (Hime et al. 2018). Traffic-related AP is a complex mixture of primary gaseous emissions (such as NOx) which are derived from combustion (including elemental or black carbon) and non-combustion sources (e.g. road dust, tyre wear, and brake wear) (Hime et al. 2018). These primary emissions lead to the generation of secondary pollutants such as O3, nitrates and organic aerosol. Another important source of atmospheric pollutant is derived from heating systems and are considered as primary emitters of PM and CO (Burns et al. 2020). Industry is also an additional major source of PM release (Burns et al. 2020; Zhang et al. 2020).
As a consequence of growing urbanisation, more than 90% of the population live in places where air quality does not meet World Health Organization (WHO) recommendation. WHO sets daily exposure limits for PM2.5 and PM10 at 25 μg/m3 and 50 μg/m3 respectively, with an annual cumulative exposure limit for PM2.5 at less than 10 μg/m3 (World Health Organization 2021). In this regard, the European Environment Agency (EEA) reported that most city dwellers have been exposed in the last years to levels higher than those recommended by WHO (74% and 42%, respectively, for PM2.5 and PM10) (European Environment Agency 2019). Worldwide EEA estimates that 7 million people yearly die because of AP exposure and in Europe AP remains the single largest environmental health hazard leading to a reduced quality of life caused by AP-related illness (European Environment Agency 2020). The impact on health is due to both short- (over a few hours or days) and long-term (over months or years) AP exposure. Morbidity is mainly linked to respiratory and cardiovascular diseases (Abe and Miraglia 2016; Jo et al. 2017; Lokotola et al. 2020; Sompornrattanaphan et al. 2020) and encompasses acute illness, chronic disease and long-term disability, ranging from mild symptoms such as coughing to more severe conditions that may require hospitalization (Jo et al. 2017; Lokotola et al. 2020). Due to the fact AP affects the whole population on a daily basis, even the less severe effects might have significant public health implications (European Environment Agency 2019, 2020; World Health Organization 2021). In this regard, AP exposure has also been connected to respiratory allergy. In fact, exposure to AP, and in particular to PM, is considered a main driver of the significant increase in the prevalence of allergic respiratory diseases observed in the past decades (Chung et al. 2011; Zhang et al. 2015a, b; Zheng et al. 2015; Wise et al. 2018) and an important contributor to the development and exacerbation of asthma (Sompornrattanaphan et al. 2020). Moreover, it has been suggested that PM can also interact with airborne allergens, whereas AP acts as adjuvant by altering the immunogenicity of allergenic proteins (Reinmuth-Selzle et al. 2017). As a contributing factor, climate change (in particular temperature, relative humidity and ultraviolet radiations) is known to affect abundance and properties of bioaerosols as carriers of aeroallergens (Reinmuth-Selzle et al. 2017).
Veneto is one of the most industrialized regions in Italy (Masiol et al. 2017; Forlivesi et al. 2018), and the city of Padua, in particular, is one of the most PM-polluted cities in Europe (Tapparo et al. 2020). Due to the high AP levels observed in this area, we had the opportunity to explore and quantify the link between AP and upper airway (UA) morbidity. Therefore, the main aim of the present investigation was to evaluate the relationships between the ear, nose and throat (ENT) urgent referrals registered at the University Hospital of Padua in one year and the daily levels of PMs as well as other environmental factors such as rainfall, air temperature, and humidity measured in the same period. As a secondary end-point, we investigated the influence of aeroallergens levels on these relationships.
Materials and Methods
This retrospective study was conducted in accordance with the principles of the Helsinki Declaration. Data were examined in agreement with the Italian privacy and sensitive data laws, and the internal regulations of Padua University’s Otolaryngology Section.
Population Considered
Azienda Ospedale Università Padova (AOUP) is a Tertiary (teaching) hospital in the Italian region of Veneto covering a population of roughly 210.000 people and recording more than 70.000 referrals to A&E every year.
In this study, only patients admitted to the Accident and emergency (A&E) department and then referred to the ENT urgent clinic during the year 2017 were considered. Patients with UA disorders were included in the study group while those referred for facial trauma or foreign body inhalation formed the control group.
Pollution and Meteorological Data
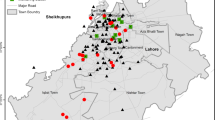
Daily AP concentrations (μg/m3), wind speed (km/h), rainfall depth (mm), air temperature (°C), minimum and maximum relative humidity (%) and the concentrations of the commonest aeroallergens in the Padua urban area (Alternaria, Betulaceae, Compositae, Corylaceae, Graminae) (g/m3) were obtained from fixed-site monitoring stations operated by ARPAV (Regional Agency for Environmental Protection and Prevention of the Veneto Region) and working 24 h a day.
Statistical Analysis
Pollution and meteorological daily mean values were calculated as the average of 24-hourly measurements in the same day. Data on referrals have been aggregated by day and the Bravais-Pearson correlation coefficient has been used to measure the marginal relation between the different indicators. Multiple Poisson count regression was fitted to explain the number of referrals with all daily variables (PM10 of the admission day and PM10 of the single days of the previous week, weather factors, aeroallergens), by allowing also quadratic effects (Agresti 2013). The joint effect of sex with PM10, obtained by considering the daily access by sex and estimating the interaction between sex and pollutant concentration, was also evaluated. p values have been calculated for all tests, and 5% was considered as the critical level of significance. Values in the range of 0.15 > p value ≥ 0.05 were assumed to indicate a marginal significance. All analyses were performed using the R: a language and environment for statistical computing (R Foundation for Statistical Computing, Vienna, Austria).
Results
Population
In total, 7278 patients (3604 males and 3674 females) were referred to the ENT urgent clinic in 2017. Of these, 910 were referred for facial trauma or foreign body inhalation and formed the control group. Table 1 reports patients’ demographics, PM10/PM2.5, weather factors and aeroallergen recorded levels and the characteristics of the ENT referrals in the year 2017.
PM 2.5 /PM 10 Concentrations
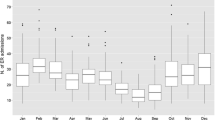
There was a strong positive correlation between PM10 and PM2.5 concentrations (Fig. 1a). For simplicity and without loss of generality, we further considered only PM10 levels as potential explanatory variable in view of the fact that statistical results and inferences remained unchanged when PM2.5 concentrations were used in the analysis in place of PM10. The 2017 mean PM10 level was 38.8 μg/m3 and PM10 levels were between 50 μg/m3 and 99 μg/m3 for 76 days and above 100 μg/m3 for 14 days, with the coldest months being the worst in terms of PM10 levels (Fig. 1b). Table 1 reports the mean PM10 and PM2.5 levels.
PM 10 Concentration and Weather Factors
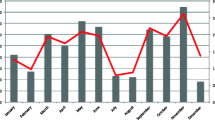
Significant correlations were found between PM10 levels and the mean air temperature (Fig. 2a; Table 2) and the minimum and the maximum relative humidity level (Fig. 2b, c; Table 2). There was a significant correlation between maximum and minimum relative humidity level.
PM 10 Concentration and Aeroallergens
Among the aeroallergens considered, only Betullaceae and Corylaceae showed a significant positive correlation with PM10 levels (Fig. 3a, b).
Weather Factors and Aeroallergens
Negative correlations were found between maximum relative humidity level and Alternaria, Gramineae and Compositae allergens, with the latter being a marginal one. (Table 2). Mean air temperature significantly correlated with all the studied allergens, positively with the Gramineae and Alternaria allergens, while negatively with the others allergens (Table 2). Rainfall depth (mm) significantly correlated only with Compositae allergens (Table 2).
Influence of Available Variables on the Number of Admissions During the Year
PM10 levels did not show any effect on the admissions when comparing the study group—which includes all the admissions except facial traumas and foreign body inhalations—and the control group. Considering the influence of the other variables (weather factors and common aeroallergens), only Alternaria positively influenced admissions of patients in the study group if compared to those in the control group.
In the study group PM10 concentrations did not show an effect on the admission rate, regardless of the sex. At the Multiple Poisson count regression, considering also the influence of weather factors and common aeroallergens, the maximum relative humidity, and Compositae allergens showed a positive effect on admissions.
Influence of Air Pollution and Meteorological Conditions on the Admissions for Upper Airway Disorders
Table 1 shows the distribution of the patients in the study group according to the different diagnoses. We did not observe any influence of PM10 on the number of admissions in the sub-cohort of patients affected by disorders possibly related to AP (patients with a diagnosis of rhinitis/rhinosinusitis, acute otitis media, pharyngitis, laryngitis, tracheitis and tonsillitis) (n = 1502). The same result was also found when we considered the effects of the most common aeroallergens and the weather factors.
Once we considered each disease separately and the effect of PM10 level on the day of A&E admission, a marginal effect was found only for rhinosinusitis when taking into account the influence of the weather and aeroallergens. This effect became significant when we considered the PM10 level measured on the seventh day before A&E admission when the influence of the aeroallergens was included. Similarly, the PM10 level measured on the second day before admission showed a positive effect on the admissions for otitis media when considering the influence of the weather and aeroallergens, while that registered on the fifth day before admission had a positive effect on the admissions for laryngitis when including the influence of the weather factors. Influence of PM10 levels on upper airway disorders on the day of admission (Day 0) and at different days before it is reported in Table 3.
Influence of Air Pollution and Meteorological Conditions on the Admissions for Upper Airway Disorders
The admissions for other UA disorders were further investigated. When we analysed the PM10 values at the day of the admission in comparison with that of the control group, also considering the effects of the most common aeroallergens and the weather factors, PM10 levels showed a positive effect on the number of admissions only for epistaxis. When we took into account the effects of the most common aeroallergens and the weather factors, the effect did not change.
Considering the PM10 levels of the whole week before A&E admission, the PM10 level measured on the third day before the admission showed a marginally positive effect on the admissions for other UA disorders. This effect became significant when we considered the additional effect of the maximum relative humidity level, while it remains marginally significant when the influence of air temperature was added.
Discussion
Environmental PM is an atmospheric aerosol which is able to reach the nose, pharynx, larynx, trachea, bronchi, and distal lung. This results in the respiratory tract being the most highly exposed system. In particular, coarse PM, with an aerodynamic diameter of 2.5–10 μm, mainly deposits in the nose, pharynx, and large conducting airways. Exposure to PM may increase the risk of infection by altering various defence mechanisms of the respiratory tract and leading to impaired mucociliary function and decreased phagocytosis by macrophages (Yang et al. 2020). PM often contains various immunogenic substances, such as fungal spores and pollen, which have been independently associated with exacerbation of asthma symptoms. Experimental exposure to PM causes oxidative stress, airway hyper-responsiveness, and airway remodelling, either alone or in combination with allergic sensitization (Qiu et al. 2022). Moreover, the existence of a dose–response relationship between PM and the risk of infection has been reported (Stanek et al. 2011).
In the present study, PM10 levels correlated with weather factors confirming the already known close relationship between PM and meteorological variables (Perez et al. 2020). In particular, a negative correlation was found between PM10 levels and air temperature, while PM10 showed a positive correlation with humidity (both minimum and maximal). The PM10 increase found in cold seasons/days could be caused by an increase in the use of heating systems in that period and possibly to a more intense vehicular traffic (Hime et al. 2018; Burns et al. 2020), but also to the inversion of temperature (Wallace et al. 2010; Cichowicz et al. 2017).
It is now accepted that the prevalence of allergic disease has increased in recent decades throughout the industrialized world (Wise et al. 2018) and our results confirm a significant correlation between Betullaceae, Corylaceae and PM10 levels. AP, in fact, can influence aeroallergens, and in heavily polluted zones pollens can express a larger number of proteins described as being allergenic (Bartra et al. 2007). The constituents of AP can disrupt pollen particles. This leads to the release of pauci-micronic (diameter of 2–5 μm) molecules which increases the penetration into the upper airway (D'Amato 2001). Moreover, climate change has led to temperature variations during the seasons. As a result, plants may vary their pollination calendar and/or prolong their pollination period (Bartra et al. 2007; Cichowicz et al. 2017; Cane 2021), as reported for Betullaceae (Zhang et al. 2014) which in the present study has been found to be associated with PM10 levels. AP may also exert a direct influence on allergen production and concentration of fungal spores such as Alternaria. Fungal spores are more influenced by atmospheric variables when compared to pollens (Bartra et al. 2007). Table 2 shows the correlation between the aeroallergens considered and weather factors.
We did not observe effects of PM10 levels on the total number of ENT urgent referrals. However, when we took into account the influence of other variables (weather factors and aeroallergens), maximum relative humidity showed a negative effect on the total number of ENT referrals. This result could be explained by the fact that 1502 admissions occurred for acute inflammatory response of UA epithelium, with 19.9% (299/1.502) of them diagnosed with rhinosinusitis. Moreover, a significant effect of Compositae allergens on the admissions was also observed regardless of the sex. When comparing the study group of ENT urgent referrals with the control group, the influence of PM10 levels was not observed. However, whilst taking into account the influence of other variables (weather factors and aeroallergens), only Alternaria allergens had a significant influence on the number of ENT referrals observed in the study group. Alternaria has very small spores (1–20 µm in diameter) (Bartra et al. 2007) which can easily reach the upper and lower airways causing inflammation and asthmatic flare-ups (Williams et al. 2016; Tham et al. 2017). Alternaria spores represents one of the main risk factors for fatal asthma (Vianello et al. 2016). Considering the different UA disorders separately, a marginal effect of PM10 levels on rhinosinusitis was demonstrated (p = 0.07); this effect became significant (p = 0.007) when we considered the levels of PM10 measured 7 days before the admission to the A&E department. The influence of PM10 on rhinosinusitis observed in our study confirms previous results reported on large cross-sectional studies which suggest a relationship between rhinosinusitis and AP (Bhattacharyya 2009; Park et al. 2019). Moreover, the significant effect of PM10 levels on epistaxis (p = 0.0198) demonstrated by our data could be a consequence of the nasal mucosal inflammation caused by AP (Bhattacharyya 2009; Park et al. 2019). Additionally, high PM10 levels measured five days before the admission to the emergency department had a significant effect on the incidence of laryngitis (p = 0.01), whereas PM10 levels registered 2 days before the admission significantly influenced the occurrence of acute otitis media (p = 0.03). A relationship between otitis media and AP had already been reported by Zemek et al. who found an association between A&E access for otitis media and interquartile increase in CO and NOx-2 levels, in the warmest months in girls and all patients with regards to CO and NOx-2 exposure, and in boys for CO exposure in the 2 days before the A&E access (Zemek et al. 2010). Similarly, Park et al. showed in a population-based study a significant relationship between AP, especially PM10, and the incidence of otitis media in paediatric patients (Park et al. 2018).
The present investigation has its limitations. Although our study was conducted in one of the most polluted urban areas (Padua) both in Italy and in Europe, it remains a single-centre study and a comparison with other urban areas with lower PM levels is warranted for future studies. Second, we analysed only hospital-based ENT referrals for UA disease which required A&E access even though the incidence of UA disease registered at a primary care level might have been different (possibly higher).
Conclusions
Our study confirms the relationship between PM10 levels, climate change and pollen levels (Betullaceae and Corylaceae) highlighting a significant influence of Alternaria on the number of ENT referrals for UA disorders. We did not find a clear link between air pollution and the number of ENT referrals, even though the experimental exposure to PM has been reported to cause oxidative stress, airway hyper-responsiveness, and remodelling (Stanek et al. 2011), with previous studies showing an association between AP and the number of ENT referrals (Zhang et al. 2015a, b; Choi et al. 2019; Kim et al. 2020). However, we did show that the levels of PM10 at specific days preceding the A&E admission were found to correlate with the number of referrals for certain UA disorders which may help in predicting and better managing UA disorders. Accurate identification of the atmospheric factors and processes responsible for the increased UA morbidity might allow appropriate protocols to be adopted to minimize their impact on health.
References
Abe KC, Miraglia SG (2016) Health impact assessment of air pollution in Sao Paulo, Brazil. Int J Environ Res Public Health 13(7):694
Agresti A (2013) Categorical data analysis, 3rd edn. Wiley
Bartra J, Mullol J, del Cuvillo A, Davila I, Ferrer M, Jauregui I, Montoro J, Sastre J, Valero A (2007) Air pollution and allergens. J Investig Allergol Clin Immunol 17(Suppl 2):3–8
Bhattacharyya N (2009) Air quality influences the prevalence of hay fever and sinusitis. Laryngoscope 119(3):429–433
Burns J, Boogaard H, Polus S, Pfadenhauer LM, Rohwer AC, van Erp AM, Turley R, Rehfuess EA (2020) Interventions to reduce ambient air pollution and their effects on health: an abridged Cochrane systematic review. Environ Int 135:105400
Cane J (2021) Global warming, advancing bloom and evidence for pollinator plasticity from long-term bee emergence monitoring. Insects 12(5):457
Choi HG, Min C, Kim SY (2019) Air pollution increases the risk of SSNHL: a nested case-control study using meteorological data and national sample cohort data. Sci Rep 9(1):8270
Chung KF, Zhang J, Zhong N (2011) Outdoor air pollution and respiratory health in Asia. Respirology 16(7):1023–1026
Cichowicz R, Wielgosinski G, Fetter W (2017) Dispersion of atmospheric air pollution in summer and winter season. Environ Monit Assess 189(12):605
D’Amato G (2001) Airborne paucimicronic allergen-carrying particles and seasonal respiratory allergy. Allergy 56(12):1109–1111
European Environment Agency. (2019) EEA report No 10/2019. Retrieved 6 Oct 2021, from https://www.eea.europa.eu/publications/air-quality-in-europe-2019.
European Environment Agency. (2020) Air pollution: how it affects our health. Retrieved 6 Oct 2021, from https://www.eea.europa.eu/themes/air/health-impacts-of-air-pollution.
Forlivesi S, Turcato G, Zivelonghi C, Zannoni M, Ricci G, Cervellin G, Lippi G, Bovi P, Bonetti B, Cappellari M (2018) Association of short- and medium-term particulate matter exposure with risk of mortality after spontaneous intracerebral hemorrhage. J Stroke Cerebrovasc Dis 27(9):2519–2523
Hime NJ, Marks GB, Cowie CT (2018) A comparison of the health effects of ambient particulate matter air pollution from five emission sources. Int J Environ Res Public Health 15(6):1206
Jo EJ, Lee WS, Jo HY, Kim CH, Eom JS, Mok JH, Kim MH, Lee K, Kim KU, Lee MK, Park HK (2017) Effects of particulate matter on respiratory disease and the impact of meteorological factors in Busan, Korea. Respir Med 124:79–87
Kim SY, Min C, Choi J, Park B, Choi HG (2020) Air pollution by NO2 is associated with the risk of Bell’s palsy: a nested case-controlled study. Sci Rep 10(1):4221
Lokotola CL, Wright CY, Wichmann J (2020) Temperature as a modifier of the effects of air pollution on cardiovascular disease hospital admissions in Cape Town, South Africa. Environ Sci Pollut Res Int 27(14):16677–16685
Masiol M, Squizzato S, Formenton G, Harrison RM, Agostinelli C (2017) Air quality across a European hotspot: Spatial gradients, seasonality, diurnal cycles and trends in the Veneto region, NE Italy. Sci Total Environ 576:210–224
Michalska M, Zorena K, Waz P, Bartoszewicz M, Brandt-Varma A, Slezak D, Robakowska M (2020) Gaseous pollutants and particulate matter (PM) in ambient air and the number of new cases of type 1 diabetes in children and adolescents in the Pomeranian Voivodeship, Poland. Biomed Res Int 2020:1648264
Park M, Han J, Jang MJ, Suh MW, Lee JH, Oh SH, Park MK (2018) Air pollution influences the incidence of otitis media in children: a national population-based study. PLoS ONE 13(6):e0199296
Park M, Lee JS, Park MK (2019) The effects of air pollutants on the prevalence of common ear, nose, and throat diseases in South Korea: a national population-based study. Clin Exp Otorhinolaryngol 12(3):294–300
Perez IA, Garcia MA, Sanchez ML, Pardo N, Fernandez-Duque B (2020) Key points in air pollution meteorology. Int J Environ Res Public Health 17(22):8349
Qiu H, Niu XY, Cao JJ, Xu HM, Xiao S, Zhang NN, Xia X, Shen ZX, Huang Y, Lau GN, Yim SH, Ho KF (2022) Inflammatory and oxidative stress responses of healthy elders to solar-assisted large-scale cleaning system (SALSCS) and changes in ambient air pollution: a quasi-interventional study in Xi’an, China. Sci Total Environ 806(Pt 3):151217
Reinmuth-Selzle K, Kampf CJ, Lucas K, Lang-Yona N, Frohlich-Nowoisky J, Shiraiwa M, Lakey PSJ, Lai S, Liu F, Kunert AT, Ziegler K, Shen F, Sgarbanti R, Weber B, Bellinghausen I, Saloga J, Weller MG, Duschl A, Schuppan D, Poschl U (2017) Air pollution and climate change effects on allergies in the anthropocene: abundance, interaction, and modification of allergens and adjuvants. Environ Sci Technol 51(8):4119–4141
Sompornrattanaphan M, Thongngarm T, Ratanawatkul P, Wongsa C, Swigris JJ (2020) The contribution of particulate matter to respiratory allergy. Asian Pac J Allergy Immunol 38(1):19–28
Stanek LW, Brown JS, Stanek J, Gift J, Costa DL (2011) Air pollution toxicology—a brief review of the role of the science in shaping the current understanding of air pollution health risks. Toxicol Sci 120(Suppl 1):S8-27
Tapparo A, Di Marco V, Badocco D, D’Aronco S, Solda L, Pastore P, Mahon BM, Kalberer M, Giorio C (2020) Formation of metal-organic ligand complexes affects solubility of metals in airborne particles at an urban site in the Po valley. Chemosphere 241:125025
Tham R, Vicendese D, Dharmage SC, Hyndman RJ, Newbigin E, Lewis E, O’Sullivan M, Lowe AJ, Taylor P, Bardin P, Tang ML, Abramson MJ, Erbas B (2017) Associations between outdoor fungal spores and childhood and adolescent asthma hospitalizations. J Allergy Clin Immunol 139(4):1140–1147
Vianello A, Caminati M, Crivellaro M, El Mazloum R, Snenghi R, Schiappoli M, Dama A, Rossi A, Festi G, Marchi MR, Bovo C, Canonica GW, Senna G (2016) Fatal asthma; is it still an epidemic? World Allergy Organ J 9(1):42
Wallace J, Corr D, Kanaroglou P (2010) Topographic and spatial impacts of temperature inversions on air quality using mobile air pollution surveys. Sci Total Environ 408(21):5086–5096
Williams PB, Barnes CS, Portnoy JM, Environmental Allergens W (2016) Innate and adaptive immune response to fungal products and allergens. J Allergy Clin Immunol Pract 4(3):386–395
Wise SK, Lin SY, Toskala E, Orlandi RR, Akdis CA, Alt JA, Azar A, Baroody FM, Bachert C, Canonica GW, Chacko T, Cingi C, Ciprandi G, Corey J, Cox LS, Creticos PS, Custovic A, Damask C, DeConde A, DelGaudio JM, Ebert CS, Eloy JA, Flanagan CE, Fokkens WJ, Franzese C, Gosepath J, Halderman A, Hamilton RG, Hoffman HJ, Hohlfeld JM, Houser SM, Hwang PH, Incorvaia C, Jarvis D, Khalid AN, Kilpelainen M, Kingdom TT, Krouse H, Larenas-Linnemann D, Laury AM, Lee SE, Levy JM, Luong AU, Marple BF, McCoul ED, McMains KC, Melen E, Mims JW, Moscato G, Mullol J, Nelson HS, Patadia M, Pawankar R, Pfaar O, Platt MP, Reisacher W, Rondon C, Rudmik L, Ryan M, Sastre J, Schlosser RJ, Settipane RA, Sharma HP, Sheikh A, Smith TL, Tantilipikorn P, Tversky JR, Veling MC, Wang Y, Westman M, Wickman M, Zacharek M (2018) International consensus statement on allergy and rhinology: allergic rhinitis. Int Forum Allergy Rhinol 8(2):108–352
World Health Organization (2021) Ambient (outdoor) air pollution. Retrieved 6 Oct 2021, from https://www.who.int/news-room/fact-sheets/detail/ambient-(outdoor)-air-quality-and-health.
Yang L, Li C, Tang X (2020) The impact of PM2.5 on the host defense of respiratory system. Front Cell Dev Biol 8:91
Zemek R, Szyszkowicz M, Rowe BH (2010) Air pollution and emergency department visits for otitis media: a case-crossover study in Edmonton, Canada. Environ Health Perspect 118(11):1631–1636
Zhang Y, Bielory L, Georgopoulos PG (2014) Climate change effect on Betula (birch) and Quercus (oak) pollen seasons in the United States. Int J Biometeorol 58(5):909–919
Zhang F, Xu J, Zhang Z, Meng H, Wang L, Lu J, Wang W, Krafft T (2015a) Ambient air quality and the effects of air pollutants on otolaryngology in Beijing. Environ Monit Assess 187(8):49
Zhang Q, Qiu Z, Chung KF, Huang SK (2015b) Link between environmental air pollution and allergic asthma: East meets West. J Thorac Dis 7(1):14–22
Zhang F, Xing J, Zhou Y, Wang S, Zhao B, Zheng H, Zhao X, Chang H, Jang C, Zhu Y, Hao J (2020) Estimation of abatement potentials and costs of air pollution emissions in China. J Environ Manage 260:110069
Zheng XY, Ding H, Jiang LN, Chen SW, Zheng JP, Qiu M, Zhou YX, Chen Q, Guan WJ (2015) Association between air pollutants and asthma emergency room visits and hospital admissions in time series studies: a systematic review and meta-analysis. PLoS ONE 10(9):e0138146
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ottaviano, G., Pendolino, A.L., Marioni, G. et al. The Impact of Air Pollution and Aeroallergens Levels on Upper Airway Acute Diseases at Urban Scale. Int J Environ Res 16, 42 (2022). https://doi.org/10.1007/s41742-022-00420-x
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s41742-022-00420-x