Abstract
Background and Objective
Haemophilia B is a rare genetic disease that is caused by a deficiency of coagulation factor IX (FIX) in the blood and leads to internal and external bleeding. Under the current standard of care, haemophilia is treated either prophylactically or on-demand via intravenous infusions of FIX. These treatment strategies impose a high burden on patients and health care systems as haemophilia B requires lifelong treatment, and FIX is costly. Etranacogene dezaparvovec (ED) is a gene therapy for haemophilia B that has been recently approved by the United States Food and Drug Administration and has received a recommendation for conditional marketing authorization by the European Medicines Agency. We aimed to examine the cost-effectiveness of ED versus extended half-life FIX (EHL-FIX) prophylaxis for moderate-to-severe haemophilia B from a German health care payer perspective.
Methods
A microsimulation model was implemented in R. The model used data from the ED phase 3 clinical trial publication and further secondary data sources to simulate and compare patients receiving ED or EHL-FIX prophylaxis over a lifetime horizon, with the potential for ED patients to switch treatment to EHL-FIX prophylaxis when the effectiveness of ED waned. Primary outcomes of this analysis included discounted total costs, discounted quality-adjusted life years (QALYs), incremental cost-effectiveness, and the incremental net monetary benefit. The annual discount rate for costs and effects was 3%. Uncertainty was examined via probabilistic analysis and additional univariate sensitivity analyses.
Results
Probabilistic analysis indicated that patients treated with ED instead of EHL-FIX prophylaxis gained 0.50 QALYs and experienced cost savings of EUR 1,179,829 at a price of EUR 1,500,000 per ED treatment. ED was the dominant treatment strategy. At a willingness to pay of EUR 50,000/QALY, the incremental net monetary benefit amounted to EUR 1,204,840.
Discussion
Depending on the price, ED can save costs and improve health outcomes of haemophilia patients compared with EHL-FIX prophylaxis, making it a potentially cost-effective alternative. These results are uncertain due to a lack of evidence regarding the long-term effectiveness of ED.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Avoid common mistakes on your manuscript.
Etranacogene dezaparvovec has the potential to be cost-effective in Germany when compared to prophylactic extended half-life factor IX, even at high prices. |
True cost-effectiveness is subject to uncertainty due to the lack of evidence on the long-term effectiveness of etranacogene dezaparvovec. |
1 Introduction
Haemophilia is a rare genetic disease that hinders blood clotting. Haemophilia B (HB) is caused by an insufficient concentration of coagulation factor IX (FIX) in the blood. This lack of FIX leads to internal and external bleeding, which can have both acute and chronic consequences. Over time, bleeding into the joints can lead to long-term arthropathy [1], reducing quality of life for patients [2]. There is also an increased risk of intracranial haemorrhages, which can be disabling [3] or fatal [4].
Under the current standard of care, HB is treated with either prophylaxis or on-demand via intravenous infusions of FIX. HB requires lifelong treatment and FIX is costly, which imposes a high burden on both patients and health care systems [5]. The standard of care varies greatly depending on the national income. In low- and middle-income countries, patients generally receive on-demand treatment or do not have access to coagulation factor at all. In high-income countries, including Germany, prophylaxis has established itself as the standard of care for severe HB, as most individuals receive this treatment. For moderate HB, the treatment strategies in Germany are mixed, but the trend has been a move towards prophylaxis [6, 7]. Studies comparing prophylaxis with on-demand treatment in high-income countries have generally found prophylaxis to be cost-effective [8,9,10,11], though these studies examined haemophilia A and not B, and it is uncertain to what extent these results are transferrable. Extended half-life FIX (EHL-FIX) products maintain a sufficient level of FIX in the blood for a longer period than conventional FIX products and thereby reduce the frequency of prophylactic infusions. A real-world burden of illness study found that EHL-FIX was the most common form of FIX prophylaxis in Germany [12]. Studies comparing real-world outcomes between standard half-life (SHL) and EHL [13,14,15] found mean annualized bleed rates (ABRs) of 2.1–2.9 for SHL and 0.3–1.4 for EHL in patient populations that had mixed moderate and severe HB.
Etranacogene dezaparvovec (ED) is a gene therapy for HB that is based on an adeno-associated virus vector carrying an FIX gene to liver cells, bearing the FIX-R338L-Padua mutation that causes affected liver cells to produce an FIX protein, with an activity that is 6 to 8 times as high as that of the wildtype FIX [16]. This treatment leads to a sustained increase of FIX activity in the blood and therefore to a reduction in the bleed rate, while also greatly reducing the need for FIX infusions. However, it remains uncertain whether the effectiveness of the gene therapy will persist over a patient’s lifetime or wane over time.
ED has recently received marketing approval by the Food and Drug Administration in the United States and has received a recommendation for conditional marketing authorization by the European Medicines Agency. The list price in the United States has been announced at USD 3.5 million [19]. It is expected that the actual prices paid by health care payers in Europe will be substantially lower. Net prices are nonetheless expected to be high and should therefore be examined critically. The objective of this study is to assess the cost-effectiveness of ED compared to EHL-FIX prophylaxis in patients with moderate-to-severe HB from a German health care payer perspective.
2 Methods
2.1 Overview
We built a decision-analytic microsimulation model and analysed the decision problem for the cost year 2022. A willingness to pay of EUR 50,000 per quality-adjusted life year (QALY) was assumed for the base-case analysis, based on a prior analysis by the Ständige Impfkommission (STIKO) [20], though no official threshold exists for Germany. An annual discount rate of 3% was chosen for costs and outcomes as recommended by the German Institut für Qualität und Wirtschaftlichkeit (IQWiG) [21]. Outcomes included life years, QALYs, the net monetary benefit (NMB), and the incremental cost-effectiveness.
For ED, we assumed that patients would be treated a single time and that re-treatment would not be possible, as viral vectors trigger an immune response [22]. It was assumed that each patient would receive exactly one dose of ED, even in the case of treatment failure. Patients switched treatment to EHL-FIX prophylaxis if the effectiveness of ED waned sufficiently. Patients receiving EHL-FIX prophylaxis were assumed to receive regular FIX infusions for their entire life.
2.2 Model Structure
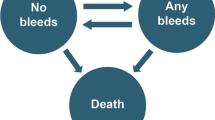
The model was implemented in the statistical software R. The R code is provided via GitHub (https://github.com/NiklausMeier/HB_CE_microsimulation). The use of a microsimulation is particularly relevant for haemophilia due to the accumulation of chronic symptoms over time for a heterogenous patient population and the potential for treatment effectiveness to wane over the lifetime of patients treated with ED. The microsimulation used a 3-month cycle length and a lifetime horizon, assuming that treatment assignment could only change every 3 months. The 3-month cycle length was chosen as a compromise between computational speed and the precision of the simulation in regard to time-sensitive events. The 3-month bleed rate served as a key model parameter that was influenced by patient characteristics and treatment. The cumulative number of joint bleeds at each point in time was calculated as a patient’s historic number of bleeds at model baseline plus the cumulative number of joint bleeds since model baseline. Associated clinical outcomes such as hospitalizations, arthropathy, and mortality were modelled for every patient as functions of either 3-month or cumulative joint bleed rates, and patient characteristics. The technical aspects of the model are described in greater detail in the appendix (see the Electronic Supplementary Material [ESM]).
Bleeds were classified either as joint bleeds or as any other kind of bleed. The accumulation of joint bleeds led to worsening arthropathy over time, quantified via the Pettersson score (PS). The total number of bleeds increased the probability of dying in each cycle. The frequency of bleeds in the model was defined via the ABR, meaning the expected number of bleeds per year for a given patient. At population generation, each patient in the model was assigned an individual untreated ABR, drawn from a distribution to reflect between-patient heterogeneity, and a historic ABR. Untreated ABR was defined as the average number of annual bleeds a patient would experience if they did not receive any ABR-lowering treatment. The specific untreated ABR of each individual in the model was lowered by the relative bleed reduction of their treatment (ED or EHL-FIX prophylaxis), ensuring that ABR was reduced in a proportional manner. Historic ABR was defined as the average number of annual bleeds prior to the start of the model.
Survival status in each cycle was implemented as a survival probability based on the probabilities of death in all previous cycles. It was adjusted via the life-table method [23] as a form of half-cycle correction, assuming that on average patients would die mid-cycle. As the model did not use any state transitions, the probability of death was the only aspect that required an active half-cycle correction. The correction was carried forward to all other outcomes, as they were calculated as functions of survival and treatment assignment.
Quality of life was modelled for each 3-month cycle via a baseline utility that was modified based on sex, age, arthropathy, the total number of bleeds during the cycle, and the burden of prophylactic infusions.
For both deterministic and probabilistic analysis, heterogeneous populations were generated, varying in terms of age, sex, untreated ABR, and historic ABR. Age was varied at the patient level, but not as a probabilistic parameter. Sex and untreated ABR were varied both probabilistically and as patient-level attributes, described in further detail below. The historic ABR of each patient was the product of their individual untreated ABR and the mean of the probabilistic historic ABR. In all analyses, the generated patients were duplicated and treated with either ED or EHL-FIX prophylaxis, creating perfectly matched populations for both the deterministic and probabilistic analysis.
The probabilistic distributions are described in Table 1. Beta distributions were used for probabilities and ratios. Gamma distributions were used for continuous, positive parameters. Given the lack of randomized data comparing ED with untreated patients, the ABRs of untreated patients, patients with ED, and patients with EHL-FIX, were sampled independently in the probabilistic analysis, rather than as relative risk reductions. Uniform distributions were chosen for the properties of ED for which there was no data (described further in Sect. 2.4, “Etranacogene Dezaparvovec”).
Probabilistic analysis considered both the heterogeneity of patients (first-order uncertainty) as well as statistical uncertainty of input parameters (second-order uncertainty) in a single analysis. More detail on the distributions and their parameters is included in the ESM appendix (Sect. 1, “Probabilistic distribution”).
The probabilistic analysis was used to generate our main results. 2000 simulations were run with random draws of the probabilistic parameters. Per simulation, 100 patients were generated, and treated with either ED or EHL-FIX, creating a perfectly matched population of 200 patients with 50:50 treatment assignment. 2000 simulations with 200 patients each resulted in a total of 400,000 simulated individuals. The deterministic analysis was used as a reference for the probabilistic analysis, as well as for univariate sensitivity analyses and scenario analyses, since using the probabilistic analysis for these analyses would not be computationally feasible. For the deterministic sensitivity analysis, 10,000 patients were generated, and treated with either ED or EHL-FIX, creating a perfectly matched population of 20,000 patients with 50:50 treatment assignment.
2.3 Population
The population was designed to be representative of adult patients with moderate-to-severe HB in Germany in 2022 and included patients at different stages of their disease history. 4.7% of patients in the model were female [24]. The average age of patients at the start of the model was 36.3 years based on the average age of HB patients in the Socioeconomic Survey (CHESS) study [25], and the minimum age was 18. The weight of patients was determined via the mean weight of German individuals, stratified by age and sex, and was updated as patients aged in the model at the start of every 3-month cycle [26]. As the relation between EHL-FIX dosage and weight is completely linear, and as only EHL-FIX dosage depends on weight in the model, weight was not varied between patients of the same sex and age, or as a probabilistic parameter.
The mean untreated ABR was 32.9 and was obtained from a clinical study of patients with moderate-to-severe HB receiving on-demand treatment [27]. As patients with moderate-to-severe HB in Europe all receive at least on-demand treatment [25], it was assumed that the ABR under on-demand treatment would be a satisfactory proxy for the ABR when receiving neither EHL-FIX prophylaxis nor gene therapy, and that bleed reductions could be calculated relative to the on-demand ABR. The mean historic ABR in the model was 4.6 and was based on a study of real-world outcomes of HB patients in Europe [25], who received a mix (44% on-demand and 56% prophylaxis) of different treatment strategies. Based on the mean historic ABR of 4.6 and the mean age of 36.3, the average patient in the model had 130.68 cumulative bleeds at the start of the model.
2.4 Etranacogene Dezaparvovec
The effectiveness of ED was drawn primarily from the publication of the phase 3 HOPE-B clinical trial [16]. 52 out of 54 patients were able to discontinue EHL-FIX prophylaxis after ED treatment. This observation was implemented as a 96.3% treatment success probability. Success and failure were drawn randomly for each patient in the simulation. A mean ABR of 1.51 was achieved during a period of 18 months after being treated with ED.Footnote 1 The mean ABR was transformed into a relative bleed reduction via the ratio of the trial ABR to the assumed untreated ABR of 32.9, yielding a relative bleed reduction of 95.4%.
In the absence of evidence on long-term effectiveness of ED in the HOPE-B clinical trials, it was assumed that the relative bleed reduction of 95.4% would be maintained for 10 years [17, 18]. Both animal [17] and human [18] studies showed transgene expression to last for up to 10 years and potentially longer for haemophilia. It was further assumed that after 10 years, the relative bleed reduction would decline gradually by 10 percentage points per year. There is no clinical evidence available for this assumption, but given the biological mechanisms, it did not seem plausible that the effectiveness of ED would wane completely from one cycle to the next. A clinical expert for haemophilia within the group of authors considered this to be a plausible assumption, given the lack of evidence. Patients who received ED switched to EHL-FIX prophylaxis when their ABR exceeded a value of 4, ensuring that patients would not be under-treated after loss of treatment benefit. The threshold of 4 was chosen as it is the closest integer to the 4.19 ABR of FIX prophylaxis in the HOPE-B trial, and in the absence of further evidence, a simplifying assumption seemed most reasonable [16].
2.5 EHL-FIX Prophylaxis
The effectiveness of EHL-FIX prophylaxis was drawn from the publication of the phase 3 HOPE-B clinical trial [16]. In this trial, a mean ABR of 4.19 was achieved during a lead-in period of at least 6 months, during which patients received FIX prophylaxis with a dose and product determined by their physician. The relative bleed reduction of 87.3% of EHL-FIX prophylaxis compared to on-demand treatment was calculated based on the 4.19 ABR under FIX prophylaxis and the untreated ABR of 32.9. The specific FIX products were not described in the study, and the market shares of EHL-FIX products could not be sourced for Germany. We thus modelled the costs of EHL-FIX based on the price of nonacog beta pegol. Out of the three EHL-FIX products included in the CHESS II study [12], nonacog beta pegol had the middle price, and as the choice of EHL-FIX product mainly affected costs, we deemed this to be the most representative, lacking further information. This choice affected the price, the dosage, and the treatment frequency with EHL-FIX.
2.6 Bleeding and Arthropathy
In the deterministic analysis, the fraction of bleeds which occurred in the joints was 61.7% of all bleeds, based on patterns observed in patients with severe haemophilia in a UK patient registry [28]. PS increased by 1 point whenever a patient accumulated 13 additional joint bleeds [29]. Joint surgery occurred in the first cycle in which PS reached the threshold for clinically relevant damage, which lies at 28 out of 78 points [30].
2.7 Mortality
The background mortality of the German general population was drawn from the Human Mortality Database [31]. The effects of bleeding on mortality were derived from an observational study of Dutch patients with haemophilia, which showed an age-adjusted standardized mortality ratio of 2.4 for patients with severe haemophilia [32]. It was assumed that this standardized mortality ratio would apply for patients with the historic ABR of 4.6. In each cycle, patients with a current ABR less than the historic ABR of 4.6 [25] were assumed to have a lower standardized mortality ratio and a higher probability to survive a cycle, and vice versa, relative to background mortality. The precise assumptions and mathematical functions required to model this relationship between bleeds and mortality are described in the ESM appendix (Sect. 2.5, “Mortality”).
2.8 Quality of Life
The non-disease specific utilities were based on a regression equation from a study on the Health Survey for England data [33], considering sex and age. The disutilities for arthropathy were derived from an analysis of multiple studies (which included X-rays and SF-36 questionnaires) for patients with moderate-to-severe haemophilia, which the authors used to calculate an association between PS and utility [2]. This study showed a disutility of 0.03 for a PS between 12 and 21, and an additional disutility of 0.07 for a PS of 22 or higher. The disutilities from bleeds were based on a phase 4 diary study (DOSE) in the United States, which analysed the daily quality of life of patients in relation to haemophilic bleeding events [34]. Each bleed led to a disutility of 0.2, which lasted for 1 day; the number of bleeds in a cycle was multiplied by the disutility of 0.2 and then divided by the cycle length (measured in days) to calculate the average bleed-disutility for that cycle, which was then applied to the entire cycle. The disutilities from joint surgeries were based on EQ-5D-5L questionnaire data collected in France and the UK to assess the quality of life of patients with haemophilia [35]. This comparison showed a utility difference of 0.18 between patients with and without joint surgery, which was implemented as a disutility that lasted for 27 days after surgery [38]. The disutilities from prophylactic FIX infusion were based on a vignette-based time trade-off study [36]. This time trade-off study showed that each coagulation factor infusion led to a one-time utility decrement of −0.0003, and since prophylactic nonacog beta pegol treatment requires 52 infusions per year, this is equivalent to a disutility of 0.0156 per life year. This 0.0156 disutility was subtracted from each patient’s quality of life in each cycle that they received EHL-FIX prophylaxis.
2.9 Resource Use
We considered medical resources with potential major cost implications. For patients treated with ED, treatment occurred immediately at the start of the simulation. For nonacog beta pegol, the dosage of EHL-FIX per treatment was 40 international units (IU) per kilogram of body weight [37]. All patients in the model were treated with this dosage after every bleed, and additionally once per week for patients receiving EHL-FIX prophylaxis. Perfect vial sharing with no wastage of EHL-FIX was assumed. The probability of hospitalization per bleed was 27.8% [12]. The length of stay at the hospital after a bleed was 1.5 days, and the length of stay after surgery was 27 days [38].
2.10 Unit Costs
For ED, a price of EUR 1,500,000 was assumed. In the United States, a list price of USD 3,500,000 has been announced; the price that will actually be paid by health care systems is expected to be substantially lower. We obtained costs of EHL-FIX (nonacog beta pegol) (EUR 1.70 per IU), intensive care (EUR 1469 per day), non-intensive inpatient care (EUR 597.20 per day), and joint surgery (EUR 866 per procedure, excluding costs for hospital days) from the CHESS I and II studies [12, 39]. All prices were adjusted for inflation to the cost year 2022 [40].
2.11 Uncertainty Analyses
Probabilistic analysis The probabilistic analysis was used for the main results and to evaluate the probability of ED being cost-effective over EHL-FIX.
Univariate sensitivity analysis The model was run using the lower and upper bound value of each uncertain parameter, one by one, holding all other parameters constant at their deterministic values. For the parameters with assigned second-order probability distributions based on published data, the lower and upper bounds were equivalent to the 2.5% and 97.5% percentiles of the respective distributions. For the parameters with uniform probabilistic distributions based on assumptions, the lower and upper values of those uniform distributions were used for the lower and upper bounds in the univariate analysis. Wide value ranges were chosen for the assumed and therefore highly uncertain properties of ED.
Scenario analyses The prices of ED and the EHL-FIX product were varied incrementally to see at which price levels ED would have a positive incremental NMB and therefore be cost-effective. Additionally, the following scenarios were run and compared with the probabilistic analysis.
-
Bleed disutility for 7 days: In the probabilistic analysis, it was assumed that the disutility from a bleed only lasted for 1 day. However, acute symptoms may last longer. Since the exact duration of the disutility is not known, a disutility per bleed lasting 7 days was examined.
-
5 × costs per day in intensive care unit (ICU): In the probabilistic analysis, the costs of treating bleeds were based on an analysis from the secondary literature, which may be conservative and not consider all potential costs due to bleed hospitalizations. To test an especially extreme hypothetical assumption not captured in the other uncertainty analyses, these costs were increased fivefold.
-
No treatment switching: In the probabilistic analysis, it was assumed that patients switch from ED to EHL-FIX prophylaxis when their ABR exceeded a threshold of 4. In this scenario, patients did not switch treatments.
-
No vial sharing: In the probabilistic analysis, it was assumed that vials of EHL-FIX were shared perfectly, with no waste. This assumption was relaxed, and EHL-FIX was instead consumed in discrete package sizes of 500 IU (the smallest available package).
-
Cost-minimization: In the probabilistic analysis, a willingness to pay of EUR 50,000/QALY was assumed. In this scenario, the willingness to pay was set to EUR 0/QALY, making incremental NMB equivalent to incremental costs. This analysis shows the lifetime per-patient cost impact of ED compared to EHL-FIX prophylaxis.
-
Age of 18/60: In the probabilistic analysis, the simulated population included patients of different ages. In two scenario analyses, the baseline ages of all patients were set to either 18 or 60 years to assess the impact of age on cost-effectiveness.
-
German non-disease specific utilities: In the probabilistic analysis, non-disease specific utilities were based on a study using English data [24]. In this scenario, alternative utilities from a quality-of-life study from Germany [41] were used for the baseline, sex, and age.
-
Duration of maximum bleed reduction 20/30 years: In the probabilistic analysis, the duration of the maximum bleed reduction ranged from 5 to 15 years. In this scenario, the impact of assuming even higher values, 20 or 30 years, is shown.
-
Bleed rate increase per year 20/30%: In the probabilistic analysis, the bleed rate increase per year ranged from 5% to 15%. In this scenario, the impact of assuming even higher values, 20% or 30%, is shown.
3 Results
3.1 Probabilistic and Deterministic Analysis
In the probabilistic analysis, patients treated with ED gained expected 0.50 discounted QALYs per patient and discounted expected cost-savings of EUR −1,179,829 per patient compared with EHL-FIX prophylaxis. The incremental discounted NMB amounted to EUR 1,204,840 for ED, which dominated EHL-FIX prophylaxis. Table 2 shows both probabilistic and deterministic results, the latter providing a reference point for the deterministic sensitivity analyses. The distribution of outcomes across the individual patients in the deterministic analysis can be found in the ESM appendix (Sect. 3.2, “Outcome distribution of individual patients”).
The lower costs from the ED strategy mainly resulted from savings in EHL-FIX, despite patients switching treatments to EHL-FIX prophylaxis if their ABR exceeded the threshold of 4 (Table 3). These savings exceeded the additional cost of EUR 1,500,000 of the gene therapy substantially. The costs for hospitalization and surgery were relatively minor in both arms, though somewhat higher for EHL-FIX prophylaxis due to the higher bleed rate.
Most simulations showed a QALY benefit between 0 and 1 and cost savings of EUR 0–3 million in favour of ED (Fig. 1). ED dominated EHL-FIX prophylaxis in almost all simulations (97.95%) despite substantial uncertainty in input variables.
Scatterplot of the probabilistic analysis. Each blue dot represents one out of 2000 simulations with a random draw of the probabilistic parameters and 100 patients per simulation, showing the mean QALY and cost difference of those 100 patients. The black diamond represents the mean of all simulations. QALY quality-adjusted life year
3.2 Univariate Sensitivity Analysis
The maximum bleed reduction period of ED had the largest impact on incremental QALYs, as this determined for how long patients would experience the lower bleed rate of the gene therapy before switching treatments (Fig. 2). The second most important parameter was the relative bleed reduction of EHL-FIX prophylaxis, as a higher relative bleed reduction lowered the amount of incremental QALYs in favour of ED. The most influential clinical input was the bleed mortality ratio, i.e. the standardized mortality ratio that was adjusted for the number of bleeds that patients experienced. The parameters of the treatments had relatively large impacts, whereas most utility and resource inputs were rather negligible.
Tornado diagram showing the influence of individual, uncertain parameters on the incremental outcomes between ED and FIX prophylaxis. The values by the ends of the bars represent the assumed parameter values at the lower and upper bound, using the units shown in Table 1 for each parameter. Panel A shows the tornado diagram for incremental QALYs. Panel B shows the tornado diagram for incremental costs. ED etranacogene dezaparvovec, FIX factor IX, LOS length of stay, PS Pettersson score, QALY quality-adjusted life year
The maximum bleed reduction period of ED had by far the largest impact on incremental costs, as reducing the bleeds for a long period would delay the treatment switch to EHL-FIX prophylaxis for the longest amount of time. The maximum bleed reduction period was followed by the other treatment parameters of ED, as a more effective treatment lowered the costs by lowering the need for on-demand EHL-FIX to treat bleeds and hospitalizations.
3.3 Scenario Analyses
In the base case, a price of EUR 1.5 million per treatment with ED was assumed (Fig. 3). This price was varied to determine at what price ED ceased to be cost-effective. It was found that the incremental NMB remained positive up to a price of approximately EUR 2.75 million. In the base case, the cost of EHL-FIX was EUR 1.70 per IU. This price was varied to determine by how much the price of EHL-FIX could decrease before ED ceased to be cost-effective. It was found that the incremental NMB remained positive as long as the approximate cost per IU was at least EUR 0.85.
Relationship between treatment prices and the incremental NMB. Panel A shows the relationship between ED price and incremental NMB. Panel B shows the relationship between EHL-FIX price and incremental NMB. ED etranacogene dezaparvovec, EHL-FIX extended half-life factor IX, IU international unit, NMB net monetary benefit
Table 4 shows the results of the discrete scenarios. Several scenarios (bleed disutility for 7 days, 5 x costs per day in ICU, cost-minimization, age 18, and German non-disease specific utilities) only had a very limited impact on the results. The following scenarios had greater impacts:
-
No treatment switching: When patients did not switch treatments after ED effectiveness waned, treatment with ED led to less instead of more QALYs than EHL-FIX prophylaxis, such that ED was no longer dominant, but instead in the south-west quadrant of the cost-effectiveness plane. Avoiding a treatment switch from ED to EHL-FIX led to cost savings of approximately 2,600,000 EUR, as patients did not receive prophylactic EHL-FIX infusions after ED effectiveness waned. These cost savings led to a large increase in the incremental NMB, despite ED no longer being dominant. The incremental cost-effectiveness ratio was 1,814,626 EUR/QALY.
-
No vial sharing: Incremental costs decreased by about EUR 200,000 in favour of ED, as EHL-FIX prophylaxis became more expensive when IU were wasted due to the lack of vial sharing.
-
Age of 60: Incremental QALYs increased by 0.46, but the cost savings from ED were reduced by about EUR 400,000, which in turn also reduced the NMB. The increased incremental effectiveness occurred as patients lived a longer percentage of their remaining lives with the maximum bleed reduction from ED. At a higher age, reducing the number of bleeds also prevented more excess mortality. Despite the lower cost savings, ED remained dominant in older patients.
-
Duration of maximum bleed reduction 20/30 years: Increasing the duration with which ED reduced the bleed rate at its maximum effectiveness increased the incremental QALYs by about 0.3 QALYs at 20 years and about 0.6 QALYs at 30 years. It increased the cost savings of ED by about EUR 1,500,000 at 20 years and EUR 2,500,000 at 30 years, as it delayed the treatment switching of patients. These scenarios greatly increased the INMB, showing the high relevance of this parameter for the cost-effectiveness of ED.
-
Bleed rate increase per year 20/30%: Increasing the bleed rate increase per year, once the effectiveness of ED begins to wane, slightly lowered the incremental QALYs, and lowered the incremental costs by about EUR 150,000, as it made ED patients treatment switch slightly earlier.
4 Discussion
The results showed that ED has the potential to be cost-effective and dominant in comparison to EHL-FIX prophylaxis in Germany at the assumed price of EUR 1,500,000 per dose. This result is mainly driven by the avoided EHL-FIX costs over patients’ lifetime horizon. Under the model’s assumption of temporary treatment benefits, cost-effectiveness was not very sensitive to decreases in patient age. The greatest amount of uncertainty arose from the properties of ED itself. In particular, the duration of maximum effectiveness had a large impact on both effectiveness and costs. The earlier the effect of ED begins to wane and bleed rates begin to increase, the more its cost-effectiveness would deteriorate.
As both ED and EHL-FIX prophylaxis are highly expensive treatments, it could be beneficial for health care systems to reduce the overall cost of treating haemophilia. The prices of coagulation factors have remained very high, and it is unlikely that these high prices are driven purely by high manufacturing costs [42]. If the price of EHL-FIX fell below a certain threshold, the price of ED would also need to decrease under the assumed 1,500,000 EUR, for ED to remain cost-effective. Competition from gene therapies may drive EHL-FIX prices down, providing a chance to make treatment for HB more cost-effective as a whole. This could especially hold true if non-viral vectors could be employed in future gene therapies, reducing the immune response and allowing for patients to be potentially re-treated if effectiveness wanes [43], thereby reducing the need for EHL-FIX prophylaxis further. Even though SHL-FIX products cost less per IU than EHL-FIX, when the recommended dosages of IU/kg of body weight are also considered, the mean annual costs per year are similar for both types of factor products in Germany [12]. The main results should therefore hold for both SHL- and EHL-FIX. The cost calculations for the considered FIX products are included in the ESM appendix (Sect. 5. “FIX prices Germany”).
Health care payers may have concerns about paying large sums up-front for gene therapies if the long-term effectiveness is uncertain and not currently supported by robust evidence. Performance-based pricing models could be a solution to this dilemma, as manufacturers could agree to be paid for every year in which the ABR of a patient stays below a pre-determined threshold without the need for EHL-FIX prophylaxis, up to an agreed-upon maximum price. In this manner, some of the risk could be transferred from health care payers to manufacturers, while still rewarding the cost-saving potential of ED when setting the price. Such pricing models would also allow the adjustment of ED fees after future price decreases of EHL-FIX products.
A prior cost-effectiveness study of gene therapy for HB also found adeno-associated virus gene therapy to be cost-effective at a price of USD 2,000,000 and a willingness to pay of USD 150,000 QALY for the United States [44]. Similar to our results, the majority of the cost-effectiveness stemmed from a reduction in costs compared to EHL-FIX prophylaxis. The Institute for Clinical and Economic Review found ED to be dominant at a price of USD 4,000,000 compared with EHL-FIX prophylaxis in the United States, again primarily due to cost savings [45]. Both studies showed relatively minor incremental effectiveness but large cost savings due to gene therapy for HB when compared with EHL-FIX prophylaxis, despite making some different modelling assumptions than the current study. These studies and ours therefore all support similar conclusions.
The cost-effectiveness of a gene therapy for spinal muscular atrophy, onasemnogene abeparvovec (Zolgensma), has also been debated due to the high price per dose. A Dutch study found that while Zolgensma promised large QALY gains over its comparators, it was also far more expensive, and that its price should not exceed EUR 680,000 [46]. On the other hand, a study from the United States found Zolgensma to be cost-effective at the list price of USD 2,125,000 [47]. However, the comparators for Zolgensma are far less expensive than the standard-of-care for HB, which makes it difficult to compare to ED. Haemophilia seems likely to be a special case, and is not necessarily comparable to other gene therapies in this regard.
This study has multiple limitations. All model inputs were drawn from the literature and selected with the help of clinical expert opinion, as the authors did not have access to individual patient data from clinical trials or other primary data sources. Two of the effectiveness parameters for ED, the duration of the maximum bleed reduction and the bleed rate increase per year, had to be assumed based on highly limited evidence, and clinical expertise by the authors. Various assumptions had to be made when interpreting ABRs and calculating relative bleed reductions in order to make multiple sources of evidence cohere in the model. It was not possible to adjust for different patient characteristics in different sources of evidence, or to consider the covariance of most parameters, meaning that the uncertainty in our model may be overestimated. This is especially the case for the independently sampled ABRs, as there is no evidence providing randomized data for a comparison of untreated patients with ED. The results generally showed little impact of quality of life on the incremental QALYs, but this may be due to gaps in the quality-of-life data for haemophilia, particularly haemophilic arthropathy. The limited evidence on haemophilic arthropathy also affected the modelling of joint surgery, where we made a simplifying assumption that joint surgery only occurred a single time when arthropathy reached a threshold, even though this could occur multiple times, especially for different joints. Although the effect of EHL-FIX infusions on quality of life was included in the model, a reduction of the bleeds to a very low level could have an additional positive effect on anxiety and stress [48], but no estimate for this effect exists in the literature. The haemophilia-specific utility parameters required for this model could not be sourced specifically for Germany. Any between-country differences we could not account for may have influenced the results in an unknown direction, though we do not have any evidence for the magnitude of these differences. Based on the low impact of utility parameters in the sensitivity analyses, we do not expect that this potential bias would have major implications for the results. Finally, resource inputs could not be sourced specifically for Germany, and not all potential resources, such as general practitioner visits, specialist visits, or some diagnostic tests, could be included, due to a lack of data. In light of the dominance of EHL-FIX costs in the model, the lack of consideration of these more minor sources of costs should not have substantially distorted the final results.
Once more evidence on the long-term effectiveness of viral gene therapies becomes available, it may be possible to update this model. Similarly, it may be possible to add more treatment strategies for a richer analysis. The R code for the microsimulation is uploaded to GitHub (https://github.com/NiklausMeier/HB_CE_microsimulation), and we encourage further development in this direction.
In conclusion, this study showed that while there is considerable uncertainty regarding the costs and effects of treatments for haemophilia, ED was dominant over EHL-FIX prophylaxis under a wide range of modelling assumptions and parameter values. This result could inform reimbursement decisions by health care payers, while also keeping in mind the fact that both treatment options are highly expensive and a burden on health care systems.
Notes
Based on the publication for the HOPE-B clinical trial, it was not possible to filter out the treatment failures from the mean ABR after treatment with ED. This means that the mean ABR of 1.51 may be an overestimation for ABR under treatment success, but due to the lack of further data, it was not possible to correct for this.
References
Gualtierotti R, Solimeno LP, Peyvandi F. Hemophilic arthropathy: Current knowledge and future perspectives. J Thromb Haemost. 2021;19:2112–21. https://doi.org/10.1111/jth.15444.
Fischer K, de Kleijn P, Negrier C, Mauser-Bunschoten EP, van der Valk PR, van Galen KPM, et al. The association of haemophilic arthropathy with Health-Related Quality of Life: a post hoc analysis. Haemophilia. 2016;22:833–40. https://doi.org/10.1111/hae.13120.
Zanon E, Pasca S. Intracranial haemorrhage in children and adults with haemophilia A and B: a literature review of the last 20 years. Blood Transfus. 2019;17:378–84. https://doi.org/10.2450/2019.0253-18.
Zwagemaker A-F, Gouw SC, Jansen JS, Vuong C, Coppens M, Hu Q, et al. Incidence and mortality rates of intracranial hemorrhage in hemophilia: a systematic review and meta-analysis. Blood. 2021;138:2853–73. https://doi.org/10.1182/blood.2021011849.
Knobe K, Berntorp E. New treatments in hemophilia: insights for the clinician. Ther Adv Hematol. 2012;3:165–75. https://doi.org/10.1177/2040620712440007.
Mahn R, Schilling K, Klamroth R, Kentouche K, Aumann V, Fischer L, et al. Entwicklung der Hämophiliebehandlung im Osten Deutschlands in den letzten 10 Jahren – eine Untersuchung des Kompetenznetz Hämorrhagische Diathese Ost (KHDO). [Development of Haemophilia Treatment in the Eastern Part of Germany over the Last Decade in the Kompetenznetz Hämorrhagische Diathese Ost (KHDO)]. Hamostaseologie. 2020;40:119–27. https://doi.org/10.1055/s-0039-3399493.
Ndoumba-Mintya A, Diallo YL, Tayou TC, Mbanya DN. Optimizing haemophilia care in resource-limited countries: current challenges and future prospects. J Blood Med. 2023;14:141–6. https://doi.org/10.2147/JBM.S291536.
Colombo GL, Di Matteo S, Mancuso ME, Santagostino E. Cost-utility analysis of prophylaxis versus treatment on demand in severe hemophilia A. Clinicoecon Outcomes Res. 2011;3:55–61. https://doi.org/10.2147/CEOR.S16670.
Coppola A, D’Ausilio A, Aiello A, Amoresano S, Toumi M, Mathew P, Tagliaferri A. Cost-effectiveness analysis of late prophylaxis vs. on-demand treatment for severe haemophilia A in Italy. Haemophilia. 2017;23:422–9. https://doi.org/10.1111/hae.13185.
Farrugia A, Cassar J, Kimber MC, Bansal M, Fischer K, Auserswald G, et al. Treatment for life for severe haemophilia A- A cost-utility model for prophylaxis vs. on-demand treatment. Haemophilia. 2013;19:e228–38. https://doi.org/10.1111/hae.12121.
Miners A. Revisiting the cost-effectiveness of primary prophylaxis with clotting factor for the treatment of severe haemophilia A. Haemophilia. 2009;15:881–7. https://doi.org/10.1111/j.1365-2516.2009.02019.x.
Burke T, Asghar S, O’Hara J, Chuang M, Sawyer EK, Li N. Clinical, humanistic, and economic burden of severe haemophilia B in adults receiving factor IX prophylaxis: findings from the CHESS II real-world burden of illness study in Europe. Orphanet J Rare Dis. 2021;16:521. https://doi.org/10.1186/s13023-021-02152-1.
Oldenburg J, Yan S, Maro G, Krishnarajah G, Tiede A. Assessing bleeding rates, related clinical impact and factor utilization in German hemophilia B patients treated with extended half-life rIX-FP compared to prior drug therapy. Curr Med Res Opin. 2020;36:9–15. https://doi.org/10.1080/03007995.2019.1662675.
Malec LM, Cheng D, Witmer CM, Jaffray J, Kouides PA, Haley KM, et al. The impact of extended half-life factor concentrates on prophylaxis for severe hemophilia in the United States. Am J Hematol. 2020;95:960–5. https://doi.org/10.1002/ajh.25844.
Chhabra A, Spurden D, Fogarty PF, Tortella BJ, Rubinstein E, Harris S, et al. Real-world outcomes associated with standard half-life and extended half-life factor replacement products for treatment of haemophilia A and B. Blood Coagul Fibrinolysis. 2020;31:186–92. https://doi.org/10.1097/MBC.0000000000000885.
Pipe SW, Leebeek FWG, Recht M, Key NS, Castaman G, Miesbach W, et al. Gene therapy with etranacogene dezaparvovec for hemophilia B. N Engl J Med. 2023;388:706–18. https://doi.org/10.1056/NEJMoa2211644.
Nguyen GN, Everett JK, Kafle S, Roche AM, Raymond HE, Leiby J, et al. A long-term study of AAV gene therapy in dogs with hemophilia A identifies clonal expansions of transduced liver cells. Nat Biotechnol. 2021;39:47–55. https://doi.org/10.1038/s41587-020-0741-7.
Nathwani AC. Gene therapy for hemophilia. Hematol Am Soc Hematol Educ Program. 2022;2022:569–78. https://doi.org/10.1182/hematology.2022000388.
Tanne JH. FDA approves $3.5m gene therapy for adults with haemophilia B. BMJ. 2022;379:o2858. https://doi.org/10.1136/bmj.o2858.
Ständige Impfkommission. Beschluss und Wissenschaftliche Begründung der Ständigen Impfkommission (STIKO) für die Aktualisierung der Influenza-Impfempfehlung für Personen im Alter von ≥ 60 Jahren. Epidemiologisches Bulletin. 2021.
Institut für Qualität und Wirtschaftlichkeit im Gesundheitswesen. Allgemeine Methoden: Version 6.1. 2022. https://www.iqwig.de/methoden/allgemeine-methoden-v6-1.pdf. Accessed 30 Nov 2022.
Earley J, Piletska E, Ronzitti G, Piletsky S. Evading and overcoming AAV neutralization in gene therapy. Trends Biotechnol. 2023;41:836–45. https://doi.org/10.1016/j.tibtech.2022.11.006.
Barendregt JJ. The half-cycle correction: banish rather than explain it. Med Decis Making. 2009;29:500–2. https://doi.org/10.1177/0272989X09340585.
World Federation of Hemophilia. Annual Global Survey. 2015. https://www.hemophilia.org/research/research-projects/the-wfh-annual-global-survey-gender-distribution. Accessed 24 Nov 2022.
Booth J, Oladapo A, Walsh S, O’Hara J, Carroll L, Garcia Diego D-A, O’Mahony B. Real-world comparative analysis of bleeding complications and health-related quality of life in patients with haemophilia A and haemophilia B. Haemophilia. 2018;24:e322–7. https://doi.org/10.1111/hae.13596.
Gesundheitsberichterstattung des Bundes. Durchschnittliche Körpermasse der Bevölkerung. 2017. https://www.gbe-bund.de/gbe/!pkg_olap_tables.prc_set_orientation?p_uid=gast&p_aid=57250655&p_sprache=D&p_help=2&p_indnr=223&p_ansnr=26787077&p_version=4&D.000=3&D.002=2&D.003=1&D.100=1.
Kavakli K, Smith L, Kuliczkowski K, Korth-Bradley J, You CW, Fuiman J, et al. Once-weekly prophylactic treatment vs. on-demand treatment with nonacog alfa in patients with moderately severe to severe haemophilia B. Haemophilia. 2016;22:381–8. https://doi.org/10.1111/hae.12878.
Stephensen D, Tait RC, Brodie N, Collins P, Cheal R, Keeling D, et al. Changing patterns of bleeding in patients with severe haemophilia A. Haemophilia. 2009;15:1210–4. https://doi.org/10.1111/j.1365-2516.2008.01876.x.
Fischer K, van Hout BA, van der Bom JG, Grobbee DE, van den Berg HM. Association between joint bleeds and Pettersson scores in severe haemophilia. Acta Radiol. 2002;43:528–32. https://doi.org/10.1258/rsmacta.43.5.528.
Fischer K, Pouw ME, Lewandowski D, Janssen MP, van den Berg HM, van Hout BA. A modeling approach to evaluate long-term outcome of prophylactic and on demand treatment strategies for severe hemophilia A. Haematologica. 2011;96:738–43. https://doi.org/10.3324/haematol.2010.029868.
Max Planck Institute for Demographic Research (Germany), University of California, Berkeley (USA), and French Institute for Demographic Studies. HMD. Human Mortality Database. 2020.
Hassan S, Monahan RC, Mauser-Bunschoten EP, van Vulpen LFD, Eikenboom J, Beckers EAM, et al. Mortality, life expectancy, and causes of death of persons with hemophilia in the Netherlands 2001–2018. J Thromb Haemost. 2021;19:645–53. https://doi.org/10.1111/jth.15182.
Ara R, Brazier JE. Populating an economic model with health state utility values: moving toward better practice. Value Health. 2010;13:509–18. https://doi.org/10.1111/j.1524-4733.2010.00700.x.
Neufeld EJ, Recht M, Sabio H, Saxena K, Solem CT, Pickard AS, et al. Effect of acute bleeding on daily quality of life assessments in patients with congenital hemophilia with inhibitors and their families: observations from the dosing observational study in hemophilia. Value Health. 2012;15:916–25. https://doi.org/10.1016/j.jval.2012.05.005.
Carroll L, Benson G, Lambert J, Benmedjahed K, Zak M, Lee XY. Real-world utilities and health-related quality-of-life data in hemophilia patients in France and the United Kingdom. Patient Prefer Adherence. 2019;13:941–57. https://doi.org/10.2147/PPA.S202773.
Johnston K, Stoffman JM, Mickle AT, Klaassen RJ, Diles D, Olatunde S, et al. Preferences and health-related quality-of-life related to disease and treatment features for patients with hemophilia A in a canadian general population sample. Patient Prefer Adherence. 2021;15:1407–17. https://doi.org/10.2147/PPA.S316276.
European Medicines Agency. Refixia Product Information: Annex I Summary of Product Characteristics. 2017. https://www.ema.europa.eu/en/documents/product-information/refixia-epar-product-information_en.pdf. Accessed 25 Nov 2022.
Ballal RD, Botteman MF, Foley I, Stephens JM, Wilke CT, Joshi AV. Economic evaluation of major knee surgery with recombinant activated factor VII in hemophilia patients with high titer inhibitors and advanced knee arthropathy: exploratory results via literature-based modeling. Curr Med Res Opin. 2008;24:753–68. https://doi.org/10.1185/030079908X273048.
O’Hara J, Hughes D, Camp C, Burke T, Carroll L, Diego D-AG. The cost of severe haemophilia in Europe: the CHESS study. Orphanet J Rare Dis. 2017;12:106. https://doi.org/10.1186/s13023-017-0660-y.
The Campbell and Cochrane Economics Methods Group (CCEMG), Evidence for Policy and Practice Information and Coordinating Centre (EPPI-Centre). CCEMG - EPPI-Centre Cost Converter. 2023. https://eppi.ioe.ac.uk/costconversion/default.aspx.
Grochtdreis T, Dams J, König H-H, Konnopka A. Health-related quality of life measured with the EQ-5D-5L: estimation of normative index values based on a representative German population sample and value set. Eur J Health Econ. 2019;20:933–44. https://doi.org/10.1007/s10198-019-01054-1.
Puetz J, Wurm FM. Recombinant proteins for industrial versus pharmaceutical purposes: a review of process and pricing. Processes. 2019;7:476. https://doi.org/10.3390/pr7080476.
Ramamoorth M, Narvekar A. Non viral vectors in gene therapy- an overview. J Clin Diagn Res. 2015;9:GE01-6. https://doi.org/10.7860/JCDR/2015/10443.5394.
Bolous NS, Chen Y, Wang H, Davidoff AM, Devidas M, Jacobs TW, et al. The cost-effectiveness of gene therapy for severe hemophilia B: a microsimulation study from the United States perspective. Blood. 2021;138:1677–90. https://doi.org/10.1182/blood.2021010864.
Tice JA, Walton S, Herce-Hagiwara B, Fahim SM, Moradi A, Sarker J, Chu J, Agboola F, Pearson SD, Rind DM. Gene therapy for hemophilia B and an update on gene therapy for hemophilia A: effectiveness and value; Evidence Report: Institute for Clinical and Economic Review; November 2, 2022.
Broekhoff TF, Sweegers CCG, Krijkamp EM, Mantel-Teeuwisse AK, Leufkens HGM, Goettsch WG, Vreman RA. Early cost-effectiveness of onasemnogene Abeparvovec-xioi (Zolgensma) and nusinersen (Spinraza) treatment for spinal muscular atrophy I in The Netherlands with relapse scenarios. Value Health. 2021;24:759–69. https://doi.org/10.1016/j.jval.2020.09.021.
Dean R, Jensen I, Cyr P, Miller B, Maru B, Sproule DM, et al. An updated cost-utility model for onasemnogene abeparvovec (Zolgensma®) in spinal muscular atrophy type 1 patients and comparison with evaluation by the Institute for Clinical and Effectiveness Review (ICER). J Mark Access Health Policy. 2021;9:1889841. https://doi.org/10.1080/20016689.2021.1889841.
Skinner MW, Nugent D, Wilton P, O’Mahony B, Dolan G, O’Hara J, Berntorp E. Achieving the unimaginable: health equity in haemophilia. Haemophilia. 2020;26:17–24. https://doi.org/10.1111/hae.13862.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This project has been funded, in part, by the European Union’s Horizon 2020 research and innovation programme under Grant agreement No. 825730.
Conflict of Interest/Competing Interests
CH has received consulting fees from CSL Behring, Sobi, Novo Nordisk, and Uniqure. CH has received payment for lectures from CSL Behring, Sobi, and Novo Nordisk. All received payments were unrelated to this study. KG is employed by F. Hoffmann-La Roche AG. MP is employed by Novartis AG. This employment is unrelated to the study. NM, HF, and MS have declared no conflict of interest.
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Availability of Data and Material
All data generated or analysed during this study are included in this published article (and its supplementary information files) or are available from the corresponding author (NM) on reasonable request for non-commercial purposes.
Code Availability
The model was implemented in R, and the full code is available from GitHub (https://github.com/NiklausMeier/HB_CE_microsimulation).
Authors’ Contributions
NM, MP, and MS conceived and designed the study. NM gathered the parameter inputs from the literature, implemented the model in R, and drafted the manuscript. CH contributed disease-area expertise and validated the clinical assumptions of the model in regard to haemophilia and its treatment strategies. KG contributed to the technical implementation and reviewed the R code during development of the model. HF, MP, and MS performed detailed reviews of the initial manuscript drafts. All authors were involved in the interpretation of the model results, reviewed the manuscript for important intellectual content, commented on it, and approved the final version.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Meier, N., Fuchs, H., Galactionova, K. et al. Cost-Effectiveness Analysis of Etranacogene Dezaparvovec Versus Extended Half-Life Prophylaxis for Moderate-to-Severe Haemophilia B in Germany. PharmacoEconomics Open 8, 373–387 (2024). https://doi.org/10.1007/s41669-024-00480-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41669-024-00480-z