Abstract
Purpose
Bladder cancer is the ninth most frequent cancer worldwide with the twelfth highest incidence. However, its treatment has financial impacts that directly affect health burden. There is a scarcity of data about the costs related to healthcare in Brazil, especially in the public setting. As previously demonstrated, despite not being one of the most frequent cancers, bladder cancer appears to be one of the most expensive. The present study aimed to assess the costs related to the treatment of bladder cancer in the public setting in Brazil.
Patients and Methods
Retrospective data of patients treated for urothelial bladder carcinoma from 2019 to 2020 were retrieved at a single center. All charts were reviewed, with the assessment of clinical data, exams, surgical data, and post-procedure outcomes. The hospital finance department calculated the costs for outpatient evaluation, inpatient procedures, complementary exams, materials, drugs, and professionals' fees throughout all operations.
Results
A total of 107 patients with bladder cancer were analyzed, representing a total expenditure of BRL 5,671,042.70 and a mean cost of BRL 53,000.04 per patient (US$1.00 = BRL 5.60). Median costs were progressively higher for patients with stages I, II, III, and IV. Patients who underwent radical cystectomy (n = 14) had a median treatment cost of BRL 136,606.25 ± 96,059.08, during a mean follow-up of 9.2 months. Hospitalization costs represented 25% (range 20–43% according to the stage) of all expenditure. Medications and medical supplies represented 18% (16–23% according to the stage) of expenditure. Medical fees represented 31% of costs for stage I disease, but only 4% in stage II, III, and IV. Costs associated with emergency room visits were only observed in stage III and IV disease, representing 1% of all expenditure.
Conclusions
The management of bladder cancer resulted in a significant economic burden on our public health system. The costs associated with stage I bladder cancer were 4–12 times higher than those related to the treatment of other common malignancies at initial stages. Treatment was also expensive during the first months with more advanced stages.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Bladder cancer is an expensive disease that results in significant burden to the health system. |
The costs associated with stage I bladder cancer were 4–12 times higher than those related to the treatment of other common malignancies at initial stages. |
1 Introduction
Bladder cancer (BC) figures as the ninth most frequent neoplasm worldwide with the twelfth highest incidence [1, 2]. In Brazil, it figures as the seventh most common neoplasm in men and the fourteenth in women, with a 5-year prevalence of 118,293 cases between 2018 and 2019. The Brazilian Cancer Institute (INCA) estimated 7590 new BC cases/year in men and 3050 new BC cases in women between 2020 and 2022 [3]. A recent population-based study demonstrated a significant increase in BC-related hospital admissions in Brazil. There were 7277 BC admissions in public institutions in 2008 while in 2017 BC admissions reached 16,547 [4]. Given the clinical characteristics of BC that manifest primarily as gross or microscopic hematuria with a recurrent pattern, patients diagnosed with BC frequently require multiple procedures and hospitalizations in order to achieve cure or to control the disease [5]. Thus, although it might not figure on the top of the list of the more frequent neoplasms, due to the disease’s characteristics, its treatment demands significant resources that markedly burden the health system. The evaluation of the actual costs of BC management in our country is of utmost importance, especially in the light of the deep underlying problems in the Brazilian public health system (SUS).
There is an estimated yearly cost of almost 20 billion Brazilian reais (BRL) (3.57 billion US dollars [US$]) to treat all cancers in Brazil. These expenses consider both the public and the private health systems. In Brazil, about 78% of the population rely exclusively on the public health system (SUS), 15.1% have a corporate health plan, and 6.9% have a private health plan [6]. When evaluating the expenses of oncologic treatment, the numbers are much different in each setting. Of all expenditure for oncologic diseases in Brazil, 77% comes from the private setting. Only 23% of expenditure comes from 78% of the population treated in the public system. The spending with oncologic diseases in SUS comprises BRL 4.5 billion yearly (800 million US dollars). Of this total, 25% is applied to intra-hospital procedures. This estimate is even higher in the private sector, with BRL 14.5 billion (35%) spent on in-hospital procedures [7]. Bladder cancer treatment, on the other hand, is also associated with elevated expenses. It is one of the malignancies with the highest lifetime costs per patient. In the US it is estimated that US$4 billion (BRL 22.4 billion) is spent each year to treat patients with bladder cancer [8]. This amount is BRL 2.4 billion higher than the amount spent in Brazil on all cancer treatments.
There is a scarcity of data about the costs related to healthcare in Brazil, especially in the public setting. A recent report has evaluated cancer treatment costs in Brazil, but only the most frequent diseases were assessed [7]. As previously demonstrated, despite not being one of the most frequent cancers, bladder cancer represents one of the most expensive.
It is generally expected that the treatment costs of cancer increases as the stage becomes more advanced. For instance, in the public health system, whereas a prostate cancer treatment costs around BRL 4800.00 for stages I and II, it increases to BRL 15,694.00 when in stage IV [7]. For bladder cancer, these numbers are unknown in Brazil. Therefore, the present study aimed to assess the costs related to the treatment of bladder cancer in the public setting in Brazil.
2 Patients and Methods
Retrospective data of all patients treated for urothelial bladder carcinoma from 2019 to 2020 were retrieved at Hospital Municipal da Vila Santa Catarina, which is a dedicated public oncology hospital managed by Hospital Israelita Albert Einstein under a public–private partnership. This project (PROADI-SUS) is an action by the Brazilian Ministry of Health (MS) aimed at strengthening the SUS in partnership with philanthropic hospitals of recognized quality. Patients were treated following best clinical practice according to international urologic and oncology guidelines [5]. Costs originated from workup and treatment and comprised outpatient evaluation (urology, oncology, and nursing clinic visits), pre-operative workup (i.e., laboratory tests, imaging, and anesthesiology visits), and inpatient procedures (i.e., transurethral bladder resections, cystoscopies, open surgeries, and intravesical instillations).
All patient charts were reviewed, assessing clinical data, exams, surgical data, and post-procedure outcomes. The hospital finance department calculated the hospital cost of the outpatient evaluation, inpatient procedures, complementary exams, materials, drugs, and professionals' fees throughout all operations. After analyzing the total costs of each patient’s treatment, comparisons were made considering patients’ staging, treatment modalities, ancillary treatments, and additional procedures.
The expenditure was analyzed according to the Absorption Costing methodology, in which the calculation of results per cost center (e.g., administrative, assistance support, and final activity) is done monthly, according to the Competency Accounting System. The calculation of costs was carried out monthly at the end of the accounting closure, allowing the calculation of cost per patient, according to the actual consumption of materials, medication, and use of services (hospitalization, exams, and procedures) per cost center. The costs of the services demanded by the programs are calculated by the average of the direct and indirect costs at each stage of patient care.
As this study was conducted in a public institution in Brazil, hospital costs are equivalent to payer costs since all procedure and treatment costs of philanthropic institutions linked to PROADI-SUS are funded by resources from the social contributions that these centers are not entitled to by law.
All procedures were performed in an academic institution that treated patients from the public health system. Treatment protocols followed best clinical practice. Pathology reports and clinical and imaging exams followed the TNM Staging System for Bladder Cancer 8th Ed., 2017 classification [9].
2.1 Statistical Analysis
Statistical analysis was performed using STATA 14.0 (StataCorp LP, College Station, TX, USA). Median time and costs were presented to mitigate the effect of the eventual outliers in the sample. Our study was conducted after Institutional Review Board approval (IRB number 40836920.0.0000.0071). All costs were recorded in Brazilian real (BRL) at the time of data acquisition and converted to US dollars to standardize understanding for foreign readers following the exchange rate of 5.6 as at October 2021.
3 Results
A total of 107 patients with bladder cancer were analyzed, representing a total expenditure of BRL 5,671,042.70 and a mean cost of BRL 53,000.04 per patient during the period studied (January 2019 to December 2020). Eleven patients were referred to our center with suspicious exams for bladder cancer, but cystoscopy turned out to be normal (stage 0). After a single cystoscopy and pre-operative workup, all 11 patients were discharged from clinic. These patients represented an individual cost of BRL 7997.51 each.
Most patients with confirmed bladder cancer had stage I disease (n = 64), as depicted in Table 1. Median costs were progressively higher for patients with stages I, II, III, and IV (Table 2). The median treatment costs during the study period were BRL 48,626.90 (US$8683.37), BRL 61,787.35 (US$11,033.45), BRL 53,198.48 (US$9499.72), and BRL 82,643.96 (US$14,757.85) for Stages I, II, III and IV, respectively.
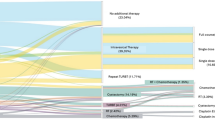
For stage I disease, additional treatments for urinary tract diseases were required during follow-up. In two patients, bladder stones were treated endoscopically, and in two patients, ureteral stones were also treated endoscopically. In one patient, urethrotomy was required. In three patients, nephroureterectomy was required for upper tract urothelial cancer detected during follow-up. Radical prostatectomy was also necessary for two patients to diagnose prostate cancer during follow-up of bladder cancer. If we calculate the expenditure for stage I bladder cancer patients without these additional procedures, the mean cost of treatment reduced to BRL 24,850.33 (US$4437.55) during a mean follow-up of 7.45 months. That represented a mean monthly cost of BRL 3337.34 (US$595.95) The 64 patients with stage I disease received 173 transurethral resections of the bladder (TURBT) or cystoscopies and one radical cystectomy (RC) (Fig. 1).
Treatment costs and characteristics for patients with stage I bladder cancer (BC). Y axis shows follow-up time in months while X axis represents costs in Brazilian reais (BRL). Horizontal bars represent each of the 64 patients with stage I BC in the study. Green bars highlight patients who have received nephrectomy/nephroureterectomy. Blue bars represent patients who have received radical cystectomy. TURBT transurethral resection of bladder tumor
Patients who underwent radical cystectomy (n = 13) had a median treatment cost of BRL 136,899.50 ± 92,681.05 (US$24,446.33 ± $16,550.18) (range BRL 30,234.68–BRL 309,889.00) during a mean follow-up of 9.2 months. The patients with ileal conduit (IC) urinary diversion had a mean age of 62 years and median treatment cost was BRL 140,035.07 (US$25,006.26) while the median cost for patients treated with cutaneous ureterostomy (CU) was BRL 180,658.91 (US$32,260.52) and the median age was 71 years. There was no statistical difference for age and costs between these two groups.
When considering ancillary treatments, the median cost of treatments for patients who underwent intravesical Bacillus Calmette-Guérin (BCG) instillations was BRL 25,040,01 (US$4471.43) and the cost for patients who did not receive this treatment was BRL 21,568,00 (US$3855.12). There was no statistical difference between the costs in both groups. Likewise, there was an increment of BRL 10,174.61 (US$1816.89) in the treatment cost for patients who received intravesical chemotherapy.
Only two patients underwent trimodal therapy (TMT), consisting of combined TURBT, chemotherapy, and radiotherapy. These patients had a mean treatment cost of BRL 17,115.39 and were followed for 5.3 months (Fig. 2). One of the patients died during treatment.
Treatment costs and characteristics for patients with stage II, III, and IV bladder cancer. Y axis shows follow-up time in months while X axis represents costs in Brazilian reais (BRL). Each horizontal bar represents a patient from the study. Blue bars represent patients who have received radical cystectomy. Black bars represent patients who received TURBT. Red bars represent patients who received TMT. TMT trimodal therapy, TURBT transurethral resection of bladder tumor
Costs were composed distinctively according to stages. Hospitalization costs represented 25% (range 20%–43% according to the stage) of all expenditure. Medications and medical supplies represented 18% (16–23% according to the stage) of expenditure. Medical fees represented 31% of costs for stage I disease, but only 4% in stage II, III, and IV. Costs associated with emergency room visits were only observed in stage III and IV disease, representing 1% of all expenditure.
4 Discussion
There are almost 10,000 new cases of bladder cancer every year in Brazil [4]. However, the prevalence is much higher as it is, in most cases, a chronic disease. A characteristic of the management of bladder cancer is the requirement for expensive cystoscopies that in many centers are performed in operating rooms under anesthesia and involve lifelong follow-up in all stages of the disease. Urinary diversions, required for advanced disease, are also associated with many complications and high costs. A previous study has estimated that 43% of the costs associated with the treatment of bladder cancer come from diagnostics and surveillance of recurrences, while 37% is attributable to complications [10]. Extremely high costs associated with the treatment of bladder cancer have been previously described [8]. In the Brazilian health system, however, these data were unknown. Furthermore, it is crucial to understand these numbers to help to create appropriate public health policies. Our study has some important findings.
First, we observed that 65% of our cohort of patients treated during the evaluated period had stage I disease, whereas 35% had more advanced disease. These numbers are worse than that reported in developed countries, where around 75% of cases are diagnosed at earlier stages [11, 12]. Additionally, 11 patients were referred to a tertiary care center to have a cystoscopy performed in the operating room under anesthesia, which turned out to be normal. Just these three patients burdened the hospital with a total cost of BRL 85,186.31. These expenditures could have been saved if cystoscopies had been performed using other techniques, such as flexible outpatient cystoscopy.
Second, stage I disease was associated with a median cost of BRL 48,626.90 (US$8683.37) per patient. This is a very high cost for the Brazilian public health system. For instance, in the same system, stage I prostate cancer costs BRL 4823.00 (US$861.25) for initial treatment and BRL 841.00 (US$150.00) yearly after that. Rectal, colon, and breast cancer cost BRL 4033.00 (US$720.17), BRL 4156.00 (US$742.14), and BRL 11,373.00 (US$2030.89), respectively, when in stage I [7]. These values are 4- to 12-fold lower than the cost of stage I bladder cancer in our cohort of patients. Moreover, our patients were followed for a relatively short period, with a median cost of BRL 6946.70/month (US$1240.48). Since follow-up of stage I bladder cancer is long, for more than 10 years usually, these numbers might become much higher.
Some of the costs observed were not directly associated with bladder cancer. Some of them were related to tumors frequently associated with bladder cancer, such as upper tract urothelial tumor. Some were related to urinary tract comorbidities, such as stone disease, and some were related to complications of multiple endoscopic procedures, such as urethrotomy for urethral stricture. These occurrences might not be exceptions in patients with bladder cancer. For that reason, we did not exclude these patients from further analysis. Since bladder cancer commonly occurs in a subset of patients with advanced disease and multiple comorbidities, it might represent their reality.
Even so, if we calculate the expenditure with our stage I patients without these additional procedures, they would have a mean cost of treatment reduced to BRL 24,850.33 (US$4437.55), during a mean follow-up of 7.45 months, representing a mean monthly cost of BRL 3337.34 (US$595.95). This might be the value that has to be projected to estimate the yearly cost of stage I bladder cancer at our service. If projected to 12 months, each stage I patient costs the system around BRL 40,000.00/year (US$7142.85). If complications and additional procedures such as nephroureterectomies and cystectomies are considered, the estimated yearly cost for stage I bladder cancer is exceedingly higher, at BRL 83,360.40 (US$14,885.78). For a projection of at least 5 years of follow-up, these patients might cost the system around BRL 200,000 (US$35,714.28) to BRL 400,000 (US$71,428.57) during this period.
Third, advanced stages (II, III, and IV) were also associated with high treatment costs. For these patients, treatment tends to be expensive right from the beginning. In contrast with stage I disease, higher expenditure tends to mount over time. For advanced stages, expensive treatments are required straight away. For instance, patients who underwent radical cystectomy (n = 14) had a median treatment cost of BRL 136,606.25 ± 96,059.08 (US$6589.19 ± 16,550.18) (range BRL 8746.86 to BRL 309,889.00). Radical cystectomy is a major procedure, with frequent complications and the requirement of additional interventions. It is more frequently indicated for stage II or III bladder cancer. However, almost half of these patients will also require systemic treatment for progression to stage IV disease during follow-up. Therefore, these initial costs might become much higher during a longer follow-up. And for stage IV disease, they might become even higher in the years to come with the possible incorporation of new agents as immunotherapeutics [13, 14].
Interestingly, despite the absence of statistical significance (p = 0.526), the cost related to the treatment of patients who received IC was BRL 40,623.84 (US$7254.26) more than the cost of treatment for patients who received CU. This tendency might be related to the patients’ clinical status, as CU is the diversion of choice for more frail patients. Indeed, there was no severe comorbidity among patients selected for IC, while in the CU group there were patients with critical past conditions such as chronic kidney disease, coronary artery disease, and stroke with motor sequelae.
Trimodal therapy (TMT) has been more frequently applied to treat bladder cancer overtime [11]. Even though it has been demonstrated that it is a much more expensive treatment [15], we did not observe this difference. Of note, we had only two patients treated with TMT, both with a short follow-up, and one died because of the treatment. Therefore, we believe that the present study cannot evaluate the costs associated with TMT in our system.
Our study has some limitations. First, the time to follow-up was relatively short. This happened as our bladder cancer service is relatively new, and the contract with the municipality is recent. For this reason, we do not have a large number of patients with a longer follow-up. Long-term costs could only be estimated. Also, it was not possible to discriminate complication-related costs in the analysis; this cost appears indirectly in the patients’ total treatment cost.
However, a strength of the present study is our institution’s very well organized cost control center and its funding model, which allowed us to extract exact information. As part of The Institutional Development Program of the Unified Health System, our institution can perform with improved financial control, avoiding the traditional public health funding system that often leads to discrepancies between the amount transferred from the government and the actual treatment cost. In the PROADI-SUS management model, the funding comes integrally from social contributions that the philanthropic institution is not entitled to by law. Thus, all costs referenced in this study are actual hospital costs provided by the hospital’s finance department and correspond exactly to the expenses related to the treatment, exempt from any disparities and inaccuracies. Second, we could only evaluate the direct costs of in-hospital treatments. Additional charges could not be estimated, such as ancillary procedures performed at other institutions, medications, and patients' out-of-pocket costs. Losses to society such as those associated with years lost due to disability or years of life lost were also not within the scope of the present study but are associated with a high burden to society.
5 Conclusion
The management of bladder cancer resulted in a significant economic burden in our public health system. More cost-effective strategies to allow early diagnosis and outpatient cystoscopies might be of value. The costs associated with stage I bladder cancer were 4–12 times higher than those related to the treatment of other common malignancies at initial stages. Treatment was also expensive during the first months with more advanced stages.
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71(3):209–49.
GLOBOCAN 2020: Global Cancer Statistics - Cancer Incidence and Mortality Worldwide: IARC CancerBase [Internet]. Vol. 278. 2020 [cited 2021 May 2]. p. 1–2. https://gco.iarc.fr/today/data/factsheets/populations/76-brazil-fact-sheets.pdf
Schilithz A, Lima FCS, Oliveira JFP, Santos MO, Rebelo MS. Estimativa da Incidência e Mortalidade por Câncer no Brasil - 2020 [Internet]. Instituto Nacional do Cancer José Alencar Gomes da Silva- INCA. Rio de Janeiro: Fox Print; 2019. Available from: https://www.inca.gov.br/publicacoes/livros/estimativa-2020-incidencia-de-cancer-no-brasil
Timoteo F, Korkes F, Baccaglini W, Glina S. Bladder cancer trends and mortality in the brazilian public health system. Int Braz J Urol. 2020;46(2):224–33. https://doi.org/10.1590/S1677-5538.IBJU.2019.0198
Witjes JA, Bruins HM, Cathomas R, Compérat EM, Cowan NC, Gakis G, Hernández V, Linares Espinós E, Lorch A, Neuzillet Y, Rouanne M, Thalmann GN, Veskimäe E, Ribal MJ, van der Heijden AG. European Association of Urology Guidelines on Muscle-invasive and Metastatic Bladder Cancer: Summary of the 2020 Guidelines. Eur Urol. 2021;79(1):82–104. https://doi.org/10.1016/j.eururo.2020.03.055.
Saúde D, Beneficiários S, Planos OE. Caderno de Informação da Saúde Suplementar: Beneficiários, Operadoras e Planos, RJ - 2019. https://www.gov.br/ans/pt-br/arquivos/acesso-a-informacao/perfil-do-setor/dados-e-indicadores-do-setor/informacoes-gerais/total-cad-info-jun-2019.pdf
Câncer noBrasil. A jornada do paciente, no sistema de saúde e seus impactos sociais e financeiros. 2018. https://edisciplinas.usp.br/pluginfile.php/6231212/mod_resource/content/3/cancer-no-brasil-n-a-jornada-do-paciente-no-sistema-de-saude-e-seus-impactos-sociais-e-financeiros-interfarma.pdf.
Sievert KD, Amend B, Nagele U, Schilling D, Bedke J, Horstmann M, et al. Economic aspects of bladder cancer: What are the benefits and costs? World J Urol. 2009;27(3):295–300.
Amin MB, Greene FL, Edge SB, Compton CC, Gershenwald JE, Brookland RK, et al. The Eighth Edition AJCC Cancer Staging Manual: continuing to build a bridge from a population-based to a more “personalized” approach to cancer staging. CA Cancer J Clin [Internet]. 2017;67(2):93–9. https://doi.org/10.3322/caac.21388.
Avritscher EBC, Barton Grossman, Catherine Cooksley HD, Sabichic A l., Dinney LP, Colin H, S.Elting L. Clinical model of lifetime cost of treating bladder cancer and associated complications. Urology. 2006;68(3):549–53.
Lenis AT, Lec PM, Chamie K. Bladder cancer a review. JAMA. 2020;324:1980–91.
Schulz GB, Grimm T, Buchner A, Jokisch F, Kretschmer A, Stief CG, et al. Bladder cancer stage development, 2004–2014 in Europe Compared With the United States: Analysis of European Population-based Cancer Registries, the United States SEER Database, and a Large Tertiary Institutional Cohort. Clin Genitourin Cancer. 2020;18(3):162-170.e4.
Powles T, Park SH, Voog E, Caserta C, Valderrama BP, Gurney H, et al. Maintenance avelumab + best supportive care (BSC) versus BSC alone after platinum-based first-line (1L) chemotherapy in advanced urothelial carcinoma (UC): JAVELIN Bladder 100 phase III interim analysis. J Clin Oncol. 2020;38(18_suppl):LBA1.
Korkes F, Maluf F. Increasing costs from Bladder Cancer in the Brazilian Health System: the role of establishing public health policies. Int Braz J Urol. 2021. https://doi.org/10.1590/S1677-5538.IBJU.2020.0658
Williams SB, Shan Y, Jazzar U, Mehta HB, Baillargeon JG, Huo J, et al. Comparing survival outcomes and costs associated with radical cystectomy and trimodal therapy for older adults with muscle-invasive bladder cancer. JAMA Surg. 2018;77555:1–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for this work with the exception of the authors’ resources comprising office stationery costs.
Conflicts of interest/Competing interests
The authors have no conflicts of interest to declare.
Ethics approval
Our study was conducted after Institutional Review Board approval which is registered under IRB number 40836920.0.0000.0071.
Consent to participate
Considering the retrospective nature of this study and its focus on health economics, the need for informed consent was waived by the hospital’s ethics committee.
Consent for publication
Considering the retrospective nature of this study and its focus on health economics, the need of informed consent was waived by the hospital’s ethics committee.
Availability of data and material
The entirety of the data produced in this study is available from the corresponding author upon request.
Code availability
Not applicable.
Author contributions
Study design: FK, VT. Data acquisition: LCBSoledade, LSB, GAP. Data analysis: FK, FT. Drafting of the manuscript: FK, FT. Critical revision of the manuscript: SG.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Korkes, F., Timóteo, F., Soledade, L.C.B. et al. Stage-Related Cost of Treatment of Bladder Cancer in Brazil. PharmacoEconomics Open 6, 461–468 (2022). https://doi.org/10.1007/s41669-022-00325-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41669-022-00325-7