Abstract
Sleep is important for good physical and mental health. The COVID-19 pandemic lockdown created a unique context that impacted psychological and social drivers for sleeping well. The Pittsburgh Sleep Quality Index (PSQI) is a widely used measurement tool assessing subjective sleep quality. The traditional model of the PSQI (a one-factor model), whilst validated and used across different populations, has also been questioned with regards to data fit and representativeness of its global score in different social and work-related circumstances. Examination of the structure validity of the PSQI in the unique context of the pandemic has been scarce. This study determined the PSQI structure validity amongst employed women considered to experience increased stressors during the pandemic lockdown. The subjectively reported PSQI data from 498 female workers (mean age 44.6 years) collected during New Zealand’s first national COVID-19 lockdown (April, 2020) was used. Confirmatory factor analyses compared the original one-factor model of the PSQI with the two- and three-factor models used by Jia et al. (2019) within this pandemic context. Results showed that the two-factor model provided a superior fit of the PSQI data compared to the original one-factor or a three-factor model. These findings suggest that a sub-score of the PSQI with two factors appears to be better at describing the sleep quality of healthy working women during the constrained situation of the pandemic lockdown compared to a single global sleep quality score. This indicates the importance of considering the validity of subjective sleep measures when used within unique social contexts and stressors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sleep is an important foundation for good physical and mental health as it supports every system in the body including metabolic, immune, cognitive function and emotional regulation [1]. Sleep quality is a complex construct and includes quantitative characteristics such as sleep duration, number and length of awakenings, sleep regularity, as well as subjective aspects like perceived sleep depth and daytime functioning. Sleep health is multifaceted and influenced by biology behaviours as well as contextual and social factors including age, gender, social engagement, socio-economic and work status [1].
Within New Zealand (NZ) the COVID-19 pandemic and the mandatory lockdown that followed abruptly changed daily life for everyone, nationally as it was the case globally. In many countries, public health authorities enforced social restrictions such as closures of non-essential workplaces, school and day-cares as an epidemiological containment strategy impacting daily routines, physical activity, and other drivers of sleep. In pursuit of an elimination strategy, the early lockdowns in NZ were considered some of the strictest in the world whilst the infection rates remained low [2]. During the strictest level of lockdown (Level 4), only essential services were open, and the population (except essential workers) had to remain within their ‘house bubbles’ (close family members only), for 33 days. In the less rigorous lockdown level (Level 3) gatherings were restricted to up to 10 people [3]. Research suggests the stress associated with the COVID-19 lockdowns and associated social restrictions significantly affected sleep quality on a global scale [4,5,6]. A meta-analysis found the prevalence of sleep disturbances during the pandemic was higher in females (41%) compared to males (31%) [7]. Furthermore, females were identified as more likely to have taken on the task of home-schooling and full-time care for children whilst fulfilling work obligations from home [8]. Therefore, research focusing on the impact of the pandemic on sleep and wellbeing within stratified samples of working females are warranted.
A measure for sleep quality used extensively in sleep research is the Pittsburgh Sleep Quality Index (PSQI) [9] which is the focus of this study. The PSQI is a self-report questionnaire comprised of 19 items that assess subjective sleep quality during the previous month. It is one of the most widely used self-report measures for assessing subjective sleep quality and is well validated in clinical and community populations. Typically, all variables contribute to calculating one or more of the seven component scores which indicate various indicators of sleep health (or disturbance). They are then collapsed again to form a global score (between 0 and 21) making it an easy applicable instrument for research and clinical practice [10]. However, more recently, the performance of self-reported sleep scales has been debated. For example across time, clinical profiles, and age-groups or different cultures [11]. This calls to question how sleep quality scales such as the PSQI performed during the pandemic lockdown (a context which dramatically changed routines and behaviours). Few studies have assessed the PSQI structure validity during the COVID-19 pandemic [12] and in special populations such as working females.
To date, most researchers use the PSQI [9] with the global score (i.e. as a one-factor model) aiming to capture all attributes of subjective sleep quality. Prior the COVID-19 pandemic, some studies have shown that multifactorial models for PSQI can improve the probability of detailing the severity of sleep disturbance because components are represented and weighted across separate domains [13, 14]. Fabbri et al.’s recent systematic review of the PSQI psychometric properties reported good internal reliability and validity however, different factorial structures were noted; six papers reported a single dimension, six studies indicated a two-factor model and two papers a three-factor model [11]. Manzar et al. (2018) [15] conducted another meta-review of the PSQI factor structure, summarising 30 distinct PSQI models proposed in the literature. However, due to methodological discrepancies between the 45 studies included (for example, adequacy of sample evaluation, application of factor analysis, variation in software used, tests conducted, and outputs reported), the application of these findings is limited. To overcome these shortcomings, the authors proposed methodological guidelines for examining the structure validity of the PSQI in future studies. This is especially the case for habitual sleep quality under different environmental and social constraints. The internal factor validity may differ between circumstances that vary compared to those within which it was initally validated. Based on Manzar et al.’s (2018) [15] suggestions, Jia and colleagues [14] re-examined the PSQI structural validity in a large (N = 2189) non-clinical sample of Americans (64% female, mean age 35.9 years, SD = 12.2) by testing one, two, and three-factor models. Their results indicated that the two-factor model (which they named ‘sleep efficiency’ and ‘sleep latency’) and three-factor models (which they named ‘sleep efficiency’, ‘sleep latency’ and ‘sleep quality’) were statistically superior to the one-factor PSQI (i.e. the original global score). Because Jia et al.’s [14] models used a rigorous methodology to improve discrepancies in the validation literature, especially when the PSQI is used under different environmental and social constraints as described above, a similar approach was used in this study. Note, due to the naming of factors by Jia et al., the terminology around ‘sleep latency’ and ‘habitual sleep efficiency’ are used differently here compared to clinical definitions used elsewhere [16].
These works indicate the importance of considering the internal reliability of the PSQI items in various research contexts. The COVID-19 lockdowns created a situation where, due to the social restrictions, self-reported sleep status changed [4,5,6]. However, the interpretation and reliability of responses to items within surveys such as the PSQI may also have been affected. For example, the reliability of estimating bed and sleep times may have been hindered because, for many, the external drivers to physically attend work or educational facilities were dropped (and therefore regularity and remembrance of routines and use of aids such as alarm clocks reduced). Furthermore, it is anticipated that how participants interpret and estimate frequencies of issues such as having “trouble staying awake while driving, eating meals, or engaging in social activity?” may also be questionable during a period when confined to their homes with limited social engagement, despite having low infection rates (as was the case in NZ).
Given prior studies questioning the use and interpretation of the PSQI in various conditions [11, 14, 15], the current study aimed to assess the factorial validity of the PSQI amongst a unique population of working females during New Zealand’s first national lockdown (April–May 2020). This is novel as few studies have examined the structural validity of PSQI during the context of the COVID-19 pandemic restrictions. It is also the first study to assess factorial validity in this population who, as outlined above, have unique factors affecting their sleep. The structure validity of the original one-factor model (hypothesised to be superior due to its common-use, validity, and reliability across different populations and contexts prior to the pandemic) was evaluated against Jia et al.’s (2019) [14] two- and three- factor models to evaluate which has the best model data fit within this unique context and population.
Methods
Participants and data collection
The data derived from an existing dataset (for reports from the entire dataset please see: [17]). The original online survey (‘Sleep and Well-being in NZ during COVID-19 Pandemic Restrictions Survey’) was launched through Qualtrics from the 11th of April to 11th of May 2020, covering New Zealand’s most rigorous lockdown restrictions (Level 4 and 3). The survey was advertised via social media, press-releases, national television, and radio. Of the original sample (N = 723), 69% (N = 498) self-identified as female workers aged over 18 years (age range: 21–83 years) and were included in the present analyses. Workers were defined as participants who reported working full-time, part-time, or as self-employed/contractors prior to lockdown.
Measures
Demographic variables included age, education, marital, employment, lifestyle, and health status (described in full in [17]). Subjective sleep quality was assessed using the PSQI, a self-report questionnaire comprised of 19 items concerning sleep during the previous month. These items are used to compute seven component scores: (1) Sleep quality; (2) sleep latency; (3) sleep duration; (4) habitual sleep efficiency; (5) sleep disturbances; (6) use of sleep medication; and (7) daytime dysfunction (see Buysse,1989 [9] for specific compositions of each score). Each component was weighted equally on a 0 to 3 scale and summed to provide a one-factor global PSQI score ranging from 0 (no sleep problems) to 21 (severe sleep problems) with scores > 5 considered indicative of 'problem sleep' according to the original validation and scoring reference [9]. In a pre-pandemic context, the PSQI had good internal reliability (α = 0.83) [9].
Statistical analysis
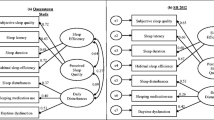
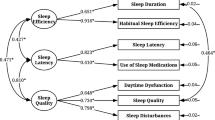
Confirmatory factor analysis (CFA) was used to examine the PSQI factor models. Then the original one-factor model (named ‘sleep quality’ including all seven PSQI component scores) was compared with sub-scored multifactorial models as developed and labelled by Jia et al. (2019) using exploratory factor analysis [14]. Jia et al. applied a re-grouping of the original seven PSQI components and binned them differently. Firstly, a two-factor model was developed. To ensure accurate replication, the specifics of the two-model structure was reported by the original authors by personal communication (March 4th, 2022) and involves one factor being named ‘sleep efficiency’ (comprised of original PSQI component scores for: sleep duration and habitual sleep efficiency), and the second factor being named ‘sleep latency’ (comprised of original PSQI component scores for: sleep quality, sleep latency, sleep disturbances, use of sleep medication, and daytime dysfunction). Then a three-factor model was developed with one factor being named ‘sleep efficiency’ (comprised of original PSQI component scores for: sleep duration and habitual sleep efficiency), another being named ‘sleep latency’ (comprised of original PSQI component scores: sleep latency and use of sleep medication), and the third factor being named ‘sleep quality’ (comprised of original PSQI component scores: sleep quality, sleep disturbances, and daytime dysfunction).
The estimation method used by Jia et al. as well as for the present study, was the Maximum Likelihood method which assumes multivariate normality of the observed variables and requires large sample sizes [18]. Skewness and kurtosis of the PSQI variables was determined to assess the normality of PSQI with values. For the analysis, all PSQI variables had to be smaller or equal to 3.0 since values greater than 3.0 indicate severe skewness and 8.0–20.0 as severe kurtosis [19]. Due to the study design, all PSQI items were mandatory within the survey. Therefore, there was no missing data. Full information maximum likelihood estimation, within Analysis of Moment Structures (AMOS), was employed using all available data to estimate the model parameters. Results using this method have shown to produce unbiased parameter estimates and are generally the default option in many software programs.
The fit indices to determine the adequacy of the hypothesised data-model fit included the Comparative Fit Index (CFI) and Tucker-Lewis Index (TLI), with values close to 0.95 or greater represent a well-fitting model [20]; Root-Mean-Square Error of Approximation (RMSEA) which are less than 0.06 indicate a good fit [20], 0.08 a mediocre fit and greater than 0.10 a poor fit [21]. The precision of RMSEA estimates was reported with 0.90% confidence intervals. No post hoc modifications were made to the models. All descriptive statistics were analysed using IBM SPSS 29.0. The CFA was conducted with IBM Amos version 29.0. The internal-consistency reliability was assessed by Cronbach’s alpha coefficient.
Results
Demographic characteristics
The participants included were 498 female workers living across NZ during the first 2020 COVID-19 lockdown. A description of the participants, demographic information and the PSQI items can be found in Table 1. The skewness of the global PSQI scores was 0.87 and kurtosis 0.66 indicating a normal distribution (mean = 6.6, Standard Deviation; SD = 3.5) Scores indicative of ‘poor sleep’ (PSQI > 5) were present amongst 54.2% of the participants.
Internal-consistency reliability
Reliability estimates for the PSQI one-factor sleep quality model was 0.73 (Cronbach’s α). For the two-factor model the α estimates were 0.73 for the sleep duration factor and 0.64 for the sleep latency factor. For the three-factor model the α estimates were 0.73 for the sleep efficiency factor, 0.38 for the sleep latency factor, and 0.63 for the sleep quality factor.
Confirmatory factor analysis
The CFA model fit indices are displayed in Table 2. Of the three models specified, the two-factor model was deemed to be the best fitting. This was because, across the three fit indices, the estimates were better compared to the other models. The model fit indices for the two-factor model showed the RMSEA of 0.08 (90% C.I.: 0.06, 0.11) and the CFI and TLI of 0.94 and 0.90 indicated a good fit.
The three different models are shown in Figs. 1, 2, 3 presented with their standardised factor loading and correlations. The standardised factor loadings for the two factors (sleep efficiency and sleep latency) and the PSQI item scores ranged from 0.30 (use of sleep medication) and 0.95 (habitual sleep efficiency). The latent factor correlation between the sleep quality and sleep factors was 0.54.
PSQI One-Factor Model for NZ female workers during lockdown, One-Factor model where all seven PSQI components are hypothesised as one-factor model being ‘sleep quality’ [9]. RMSEA: Root-Mean-Square Error of Approximation 0.16, CFI: Comparative Fit Index 0.75, and the TLI: Tucker-Lewis Index 0.65 all suggested poor fit, e1-e7 = error. *p < 0.05, **p < 0.01, ***p < 0.001
PSQI 2-Factor Model for NZ female workers during lockdown Two-factor model was specified using the seven PSQI components into two separate correlated factors being ‘sleep efficiency’ or ‘sleep latency’ as per Jia et al. [14]
PSQI 3-Factor Model for NZ Female Workers The three-factor model was specified using the seven PSQI components into three separate correlated factors ‘sleep efficiency’, ‘sleep latency’, or ‘sleep quality’ as per Jia et al. [14]. RMSEA: Root-Mean-Square Error of Approximation, CFI: Comparative Fit Index, TLI: Tucker-Lewis Index all suggested lower (poor-adequate) fit compared to the two-factor model, e1-e7 = error. *p < 0.05, **p < 0.01, ***p < 0.001
RMSEA: Root-Mean-Square Error of Approximation, CFI: Comparative Fit Index, TLI: Tucker-Lewis Index all suggested good model data fit, e1-e7 = error. *p < 0.05, **p < 0.01, ***p < 0.001.
Discussion
This study examined the structure validity of the PSQI in a sample of working females during the first national COVID-19 lockdown in NZ. The PSQI is one of the most widely used assessment tools for measuring subjective sleep quality. However, evidence for its structure validity during the COVID-19 pandemic is needed to help facilitate and advance reliable understandings of sleep, and sleep quality amongst a range of behavioural, social, and health factors during this unique probably stressful context.
Previous research has validated the original PSQI one-factor model [22]. However, it was validated within American college students as participants who were predominantly young, white, of high socioeconomic status, and included both sexes. Furthermore, limitations of the PSQI one-factor model (in relation to its structure validity) have been noted for use in the general population prior to the pandemic [11, 15]. Other evidence suggests that subjective sleep quality may be better assessed by the PSQI two-factor model [23,24,25,26,27]. The present findings corroborate this, at least under the general constraint of a pandemic situation. For this sample of working females within the context of New Zealand’s pandemic lockdown, the traditional one-factor model did not fit as well as the two-factor model. The unique context of the pandemic lockdowns with their strict social restrictions (particularly in countries like NZ) created a situation within which the routines of waking and sleeping life were affected [2]. Such changes have been identified as impacting sleep [4,5,6, 17] and potentially how participants interpret questions concerning their wellbeing [28]. The female worker population may also be highly unusual compared to characteristics of other populations that have previously been used to validate the PSQI. For example, the added stress many females were facing during the lockdown by having a higher proportion of the childcare and home-schooling burden whilst also working, may have led to compromised sleep patterns [5, 29, 30].
Results from this study suggest that multifactorial models of the PSQI might provide stronger data fit of the seven components compared to the original one-factor model. This is in line with Jia et al.’s (2019) findings [14]. However, out of the three hypothesised models, only the two-factor model met the threshold for good model fit to the PSQI data of the present NZ female worker population. The two-factor model had a good internal consistency for the latent factor ‘sleep efficiency’ and but below threshold reliability for latent factor ‘sleep latency’ (for recommended thresholds see [31]). These results likely reflect the nature and weighting of the scoring system of the seven individual components of the PSQI in the social constraints of the pandemic. As the base scoring system uses one or more subjective sleep variables to inform each of the seven sleep-related component scores [9], it is difficult to truly determine the contribution of one specific variable within measures like the PSQI when it has been combined and collapsed into component scores and then a single global score (or in the present case binned into two or three-factor sub scores) [32]. This may be problematic when applied in contexts like the pandemic, where the variables of self-reported sleep of the global PSQI have been affected differently than under ‘normal’ situations. In addition, some individuals reported better sleep quality compared to pre-pandemic estimates, while for others it was worse [17]. Similarly, for some, sleep disturbances associated with their home and sleeping environment or work schedules improved during lockdown, whereas for others it became more challenging [3,4,5,6, 17].
In this pandemic context, the PSQI with revised factors differentiating between ‘sleep efficiency’ (incorporating PSQI component scores for sleep duration and habitual sleep efficiency) and ‘sleep quality’ (incorporating PSQI component scores for sleep latency, use of medications, daytime dysfunction, sleep disturbances, and self-rated sleep quality) provided a better fit than the traditional single factor ‘sleep quality’ score (incorporating all seven PSQI component scores). This two-factor model may have been a superior fit for this population at this time due to its ability to account for the nuanced and sometimes contradictory differences observed in reports of changes to times in bed and sleep durations during the pandemic compared to perceptions of sleep status and changed factors disturbing sleep [3,4,5,6, 17]. In other words, for this sample of working women, the specific stress situation of the pandemic did not appear to affect all components of the PSQI in the same way as would be expected under ‘normal’ conditions. These findings indicate the importance of understanding the factor structure within component-based scales of the PSQI (and other such measures using a similar approach to component scoring) prior to its application and interpretation in general research settings. Greater attention towards the analysis and interpretation of the PSQI is required to better interpret and differentiate the contribution of single variables in both the estimation of reliability and the factor models.
There are several considerations concerning the present study which may inform future research. First, the original online survey was collected within a limited timeframe (≈30 days) and aimed at recruiting a heterogenous sample. However, the sample was a convenience sample with majority being female, highly educated, of NZ European ethnicity and therefore not representative of the NZ population limiting generalisability [17]. This study worked to the strength of the dataset and focused on a stratified sample of working females. The pandemic was unprecedented with a limited time prior the announcement of the lockdown, yet the original survey managed to collect the data at this time as opposed to other research which used retrospective surveys (e.g. [33]). Second, there was an underrepresentation of Māori and Pasifika in the cohort compared to the NZ population indicating response bias. Previous research has identified disparity in these populations with lower socio-economic status, sleep disturbances and mental health problems [34]. Thus, the prevalence of sleep problems is likely greater in the NZ population than reported here. Finally, as this is the first PSQI-related structural validity study in NZ, it is not possible to compare the difference in validity of the scale among working NZ females to pre-pandemic. Therefore, it is recommended that future research is required to validate the PSQI in a NZ representative sample and explore the factor structure as well as cut-off scores to identify problem sleep (in the various factor structures) for unique populations and contexts across genders, different age groups, and ethnicities separately.
Consideration of which subjective variables drive sleep-related concept outcomes is important. Factors of the scored components are typically labelled to represent the composition of its items. In the present sample, the names for the factors were informed by Jia et al. [14]. However, these are considered limited with regards to their wording for the dimensions of sleep with respect to the official PSQI metrics and those commonly used in research related to sleep health and clinical practice [1, 16, 35]. For example, it does not account for the regularity of sleep or napping. Nor does it differentiate between work- and free-days, so components associated with chronotype and social jetlag are not represented. Furthermore, the magnitude of specific external social stressors is not captured by the PSQI. Previous research has highlighted changes to such dimensions of sleep are important and were found to change within lockdown situations [4, 17]. In the future it will be important to determine more suitable concepts which reflect sleep under different circumstances and living conditions. Such approaches may also create new opportunities to diagnose sleep problems and improve aspects of sleep quality in a more individually tailored way. A final consideration is that the PSQI as well as other subjective sleep measures do not always reflect objective sleep measures such measures of sleep latency and fragmentation as recorded and defined using polysomnography or actigraphy [36]. This highlights the importance of using mixed methods and multiple measures for assessing sleep status. An assessment of the factor validity of the PSQI in research alongside objectives measures may be of interest.
Conclusion
This study is the first to examine the PSQI structure validity during the unique context of the COVID-19 lockdown in a NZ working female cohort. Overall, the findings suggest the PSQI two-factor model was statistically superior to the original one-factor model and a three-factor model in detecting sleep impairment among working NZ females within a pandemic context. Although the factor structure requires further validation in other crisis situations across different populations, it indicates that internal validity of subjective sleep quality is better assessed by a PSQI two-factor model in line with some previous findings. This highlights the need to consider the different contexts in which the PSQI is used and its factor structure to differentiate between ‘good’ and ‘poor’ sleepers, as well as consider the weighting and interpretation of the PSQI global score.
References
Grandner MA. Sleep and Health. Academic Press; 2019. p. 45–53. https://doi.org/10.1016/B978-0-12-815373-4.00005-8.
Fouda A, Mahmoudi N, Moy N, Paolucci F. The COVID-19 pandemic in Greece, Iceland, New Zealand, and Singapore: health policies and lessons learned. Health Policy Tech. 2020;9(4):510–24. https://doi.org/10.1016/j.hlpt.2020.08.015.
New Zealand Government. History of the COVID-19 alert system. 2022. https://covid19.govt.nz/about-our-covid-19-response/history-of-the-covid-19-alert-system/. Accessed 20 April 2023.
Blume C, Schmidt MH, Cajochen C. Effects of the COVID-19 lockdown on human sleep and rest-activity rhythms. Curr Biol. 2020;30(14):795–7. https://doi.org/10.1016/j.cub.2020.06.021.
Jahrami HA, Alhaj OA, Humood AM, Alenezi AF, Fekih-Romdhane F, AlRasheed MM, Saif ZQ, Bragazzi NL, Pandi-Perumal SR, BaHammam AS, Vitiello MV. Sleep disturbances during the COVID-19 pandemic a systematic review meta-analysis and meta-regression. Sleep Med Rev. 2022. https://doi.org/10.1016/j.smrv.2022.101591.
Rezaei N, Grandner MA. Changes in sleep duration, timing, and variability during the COVID-19 pandemic: Large-scale Fitbit data from 6 major US cities. Sleep Health. 2021;7(3):303–13. https://doi.org/10.1016/j.sleh.2021.02.008.
Alimoradi Z, Gozal D, Tsang HWH, Lin C-Y, Broström A, Ohayon MM, Pakpour AH. Gender-specific estimates of sleep problems during the COVID-19 pandemic: systematic review and meta-analysis. J Sleep Res. 2022;31(1):e13432. https://doi.org/10.1111/jsr.13432.
Zamarro G, Prados MJ. Gender differences in couples’ division of childcare, work and mental health during COVID-19. Rev Econ Household. 2021;19(1):11–40. https://doi.org/10.1007/s11150-020-09534-7.
Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. https://doi.org/10.1016/0165-1781(89)90047-4.
Mollayeva T, Thurairajah P, Burton K, Mollayeva S, Shapiro CM, Colantonio A. The Pittsburgh Sleep Quality Index as a screening tool for sleep dysfunction in clinical and non-clinical samples: a systematic review and meta-analysis. Sleep Med Rev. 2016. https://doi.org/10.1016/j.smrv.2015.01.009.
Fabbri M, Beracci A, Martoni M, Meneo D, Tonetti L, Natale V. Measuring subjective sleep quality: a review. Int J Environ Res Public Health. 2021;18(3):1082. https://doi.org/10.3390/ijerph18031082.
Wang L, Wu YX, Lin YQ, Wang L, Zeng ZN, Xie XL, Chen QY, Wei SC. Reliability and validity of the Pittsburgh Sleep Quality Index among frontline COVID-19 health care workers using classical test theory and item response theory. J Clin Sleep Med. 2022;18(2):541–51. https://doi.org/10.5664/jcsm.9658.
Cole JC, Motivala SJ, Buysse DJ, Oxman MN, Levin MJ, Irwin MR. Validation of a 3-factor scoring model for the pittsburgh sleep quality index in older adults. Sleep. 2006;29(1):112–6. https://doi.org/10.1093/sleep/29.1.112.
Jia Y, Chen S, Deutz NEP, Bukkapatnam STS, Woltering S. Examining the structure validity of the Pittsburgh Sleep Quality Index. Sleep Biol Rhythms. 2019;17(2):209–21. https://doi.org/10.1007/s41105-018-00201-0.
Manzar MD, BaHammam AS, Hameed UA, Spence DW, Pandi-Perumal SR, Moscovitch A, Streiner DL. Dimensionality of the Pittsburgh Sleep Quality Index: a systematic review. Health Qual Life Outcomes. 2018;16:89. https://doi.org/10.1186/s12955-018-0915-x.
Ohayon M, Wickwire EM, Hirshkowitz M, Albert SM, Avidan A, Daly FJ, et al. National sleep foundation’s sleep quality recommendations: first report. Sleep Health. 2017;3(1):6–19. https://doi.org/10.1016/j.sleh.2016.11.006.
Gibson R, Shetty H, Carter M, Münch M. Sleeping in a bubble: factors affecting sleep during New Zealand’s COVID-19 lockdown. SLEEP Adv. 2022. https://doi.org/10.1093/sleepadvances/zpac017.
Byrne BM. Structural equation modeling with AMOS: Basic concepts, applications, and programming. 2nd ed. Routledge; 2010. https://doi.org/10.4324/9781315757421.
Kline RB. Principles and practice of structural equation modelling. 4th ed. Guilford Press; 2016.
Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct Equ Model. 1999;6(1):1–55. https://doi.org/10.1080/10705519909540118.
MacCallum RC, Browne MW, Sugawara HM. Power analysis and determination of sample size for covariance structure modeling. Psychol Method. 1996;1(2):130–49. https://doi.org/10.1037/1082-989X.1.2.130.
Dietch JR, Taylor DJ, Sethi K, Kelly K, Bramoweth AD, Roane BM. Psychometric evaluation of the PSQI in U.S college students. J Clin Sleep Med. 2016;12(8):1121–9. https://doi.org/10.5664/jcsm.6050.
Al Maqbali M, Hughes C, Gracey J, Rankin J, Dunwoody L, Hacker E. Validation of the Pittsburgh Sleep Quality Index (PSQI) with Arabic cancer patients. Sleep Biol Rhythms. 2020;18(3):217–23. https://doi.org/10.1007/s41105-020-00258-w.
Hita-Contreras F, Martínez-López E, Latorre-Román PA, Garrido F, Santos MA, Martínez-Amat A. Reliability and validity of the Spanish version of the Pittsburgh sleep Quality Index (PSQI) in patients with fibromyalgia. Rheumatol Int. 2014;34(7):929–36. https://doi.org/10.1007/s00296-014-2960-z.
Kotronoulas GC, Papadopoulou CN, Papapetrou A, Patiraki E. Psychometric evaluation and feasibility of the Greek Pittsburgh Sleep Quality Index (GR-PSQI) in patients with cancer receiving chemotherapy. Support Care Cancer. 2011;19(11):1831–40. https://doi.org/10.1007/s00520-010-1025-4.
Skouteris H, Wertheim EH, Germano C, Paxton SJ, Milgrom J. Assessing sleep during pregnancy. A study across two time points examining the Pittsburgh Sleep Quality Index and associations with depressive symptoms. Women’s Health Issues. 2009;19(1):45–51.
Qui C, Gelay B, Zhong QY, Enquobahrie DA, Frederik IO, Williams MA. Construct validity and factor structure of the Pittsburgh Sleep Quality Index among pregnant women in Pacific-Northwest cohort. Sleep Breath. 2016;20(1):293–301. https://doi.org/10.1007/s11325-016-1313-4.
Ransing R, Ramalho R, Orsolini L, Adiukwu F, Gonzalez-Diaz JM, Larnaout A, Pinto da Costa M, Grandinetti P, Bytyçi DG, Shalbafan M, Patil I, Nofal M, Pereira-Sanchez V, Kilic O. Can COVID-19 related mental health issues be measured? Brain Behav Immun. 2020;88:32–4. https://doi.org/10.1016/j.bbi.2020.05.049.
Alon T, Doepke M, Olmstead-Rumsey J, Tertilt M. The impact of the coronavirus pandemic on gender equality. National Bur Econ Res Work Pap Ser. 2020;4:62–85. https://doi.org/10.3386/w26947.
Farré L, Fawaz Y, González L, Graves J. Gender inequality in paid and unpaid work during Covid-19 times. Review Income Wealth. 2022;68(2):323–47. https://doi.org/10.1111/roiw.12563.
Nunnally JC, Bernstein IH. Psychometric theory. 3rd ed. McGraw-Hill; 1994.
Little TD, Rhemtulla M, Gibson K, Schoemann AM. Why the items versus parcels controversy needn’t be one. Psychol Methods. 2013;18(3):285–300. https://doi.org/10.1037/a0033266.
Fowler LA, Kumte N. The effect of COVID-19 pandemic stay-at-home orders on sleep deprivation in medical students: a retrospective study. SN Social Sci. 2022;2(3):29. https://doi.org/10.1007/s43545-022-00323-w.
Paine SJ, Gander PH, Harris RB, Reid P. Prevalence and consequences of insomnia in New Zealand: disparities between Maori and non-Maori. Aust N Z J Public Health. 2005;29(1):22–8. https://doi.org/10.1111/j.1467-842x.2005.tb00743.x.
Buysse DJ. Sleep health: can we define it? Does it matter? Sleep. 2014;37(1):9–17. https://doi.org/10.5665/sleep.3298.
Buysse DJ, Hall ML, Strollo PJ, Kamarck TW, Owens J, Lee L, Reis SE, Matthews KA. Relationships between the pittsburgh sleep quality index (PSQI), epworth sleepiness scale (ESS), and clinical/polysomnographic measures in a community sample. J Clin Sleep Med. 2008;04(6):563–71. https://doi.org/10.5664/jcsm.27351.
Acknowledgements
The authors would like to acknowledge the participants who took part in this survey during a potentially challenging time as well as the students, Harshi Shetty and Mikaela Carter, helping with the processing of the survey data, and the team at the Sleep/Wake Research Centre for their initial support in launching this project. No external funding was received for performing this research. The analyses presented here were supported as a part of a NZ Lotteries Health Research Project grant (RG: LHR-2021-154506).
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no potential conflict of interest to declare.
Ethical approval
The dataset was derived from an anonymous online survey (see [15]). The study procedure was approved by Massey University Northern Ethics Committee (NOR 20/14). Participation was voluntary and anonymous, and implicit consent was obtained from all participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Helles, M., Fletcher, R., Münch, M. et al. Examining the structure validity of the Pittsburgh Sleep Quality Index among female workers during New Zealand’s initial COVID-19 lockdown. Sleep Biol. Rhythms 22, 217–225 (2024). https://doi.org/10.1007/s41105-023-00509-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41105-023-00509-6