Abstract
The COVID-19 pandemic required medical schools to transition to online learning due to mandated stay-at-home orders. This created a drastic change in the learning environment and behavior of medical students, as well as increased stress about school and the pandemic, which may have impacted sleep. This study assessed medical student sleep timing, duration and quality retrospectively using the Pittsburgh Sleep Quality Index (PSQI) and a sleep questionnaire to determine changes prior to and following the stay-at-home orders. In addition, perceptions of stress related to COVID-19 and to school, as well as age and gender, were examined using a survey to determine relationships to sleep variables. Repeated-measures MANOVAs showed that medical student sleep timing changed significantly, shifting sleep and wake times later on both weekdays and weekends (p < 0.001). In addition, sleep quality significantly worsened post-COVID as compared to pre-COVID, with most subscales of the PSQI worsening after the stay-at-home order, especially in males. Older students had significantly longer sleep duration than younger students post-COVID. Sleep duration did not change significantly, and stress was not significantly related to sleep quality. Interestingly, sleep medication usage significantly increased post-COVID, with more students using sleep medications more frequently after the stay-at-home order (p < 0.05). This study represents the first research to assess how medical student sleep timing, quality and medication use was affected by the stay-at-home order due to the COVID-19 pandemic.
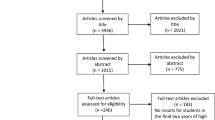
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In November 2019, the virus SARS-CoV-2, which leads to an acute respiratory syndrome, COVID-19, began spreading from Asia to other continents across the globe, with community transmission in the United States likely starting in late January 2020 (Jorden and Rudman 2020). In March 2020 the World Health Organization declared a global pandemic, prompting states to begin mandating shelter in place orders to promote physical distancing. On March 13, 2020, the governor of South Carolina declared a state of emergency due to the COVID-19 pandemic, and he later issued a state-wide stay at home order on April 6, 2020 (Exec and Order No, 2020. The stay-at-home order created drastic changes in the behavior of the population of the state, including medical students. Medical students were removed from the clinical learning environment and all educational sessions were moved to virtual sessions. This transition from the face-to-face learning environment to an online learning environment drastically altered medical student behavior and potentially altered sleep habits and sleep quality in the medical students.
Medical student sleep duration is similar to that of the general population, averaging around 6.5 h per night (Jahrami et al. 2019; Ahmed et al. 2017; Frank et al. 2006), although medical students tend to report higher levels of sleep hygiene than general university populations (Brick et al. 2010). However, medical student sleep disturbances and daytime dysfunction are elevated compared to the general population (Jahrami et al. 2019; Ahmed et al. 2017; Ayala et al. 2017). Brick (2010) found that more than half of their US medical student sample met the clinical criteria for poor sleep quality (Brick et al. 2010), and this effect was elevated in those who were older, those who spent more time in a clinical setting, and in minorities (Ayala et al. 2017). These sleep problems can lead the medical students to utilize sleep medication, with one sample reporting 13% using prescription and/or over-the-counter sleeping pills often or daily, and 14% using them occasionally/monthly (Ahmed et al. 2017). Decreased sleep duration and sleep restriction (hereafter referred to as sleep deprivation) and poor quality in medical students has been found to lead to negative perceptions about emotional stimuli and increased stress (Papp et al. 2006), which can then continue to lead to sleep problems in the students.
Extensive research has demonstrated that both acute and chronic stress can result in detrimental changes in sleep (Lavie 2001; Philbert et al. 2011; Touma et al. 2009). Specifically, medical student stress has been shown to be inversely related to sleep quality (Almojali et al. 2017). All medical students, especially first year students, appear to have increased vulnerability to sleep problems related to new physical and emotional stressors (Ayala et al. 2017). The COVID-19 pandemic that swept around the world acted as a major stressor, even for households free from the virus or economic difficulties (Bavel et al. 2020). Recent research has shown that mental health concerns about stress and anxiety from COVID-19 were higher than physical and economic concerns in the general public (Brenan 2020). This increased anxiety due to COVID-19 extends to university students as well (Cao et al. 2020), although no studies as yet report effects on medical students. The self-isolation policies that were mandated in order to decrease the spread of disease likely exacerbated stress from the pandemic, given that social connections and interactions with others act as a coping mechanism when people are stressed (Williams et al. 2018). The stress from COVID-19 and the resulting stay-at-home orders/quarantine have been shown to be risk factors for sleep deprivation and sleep problems (Casagrande et al. 2020), especially in women. Thus the COVID-19 pandemic and the stay-at-home orders could lead to increased sleep problems and sleep deprivation in medical students.
The abrupt change in the medical students’ daily routine, the forced confinement due to stay-at-home measures, and the uncertainty of what is to come, both personally and professionally, can lead to changes in sleep. This study was designed to assess how the COVID-19 pandemic and resulting stay-at-home order influenced medical student sleep quality, deprivation, duration and timing, and whether age and gender play a role in these effects. We hypothesize that medical student sleep quality will be adversely affected by the COVID-19 stay-at-home order, and we expect sleep timing to be delayed. We do not expect gender to play a role in sleep quality based on previous studies in medical students (Ayala et al. 2017; Papp et al. 2006), but we expect older medical students to have worse sleep quality than younger students (Ayala et al. 2017).
Materials and methods
One hundred and four first year medical students from the University of South Carolina School of Medicine Greenville were invited to participate in this study. Forty-nine students participated in this study, however only participants who completed all materials (N = 41) had their data analyzed (39% of the first-year class). Of the 41, 29 were female, 10 were male, and 2 preferred not to answer. Participant average age was 23.94 years (SD 1.76), with a range from 21 to 30 years. First year students were chosen for this sample due to the fact that all of the students were in the same courses together at the time of the stay-at-home order. Since all students had the same coursework and academic demands, this limits possible variability that would be seen by assessing students in other years. In addition, previous research has shown that first year medical students have poorer sleep quality than students in other years of medical school (Ayala et al. 2017).
On March 16th, 2020 all University of South Carolina classes were transitioned to online courses, and the first-year medical students at University of South Carolina School of Medicine Greenville began their Neuroscience module as a virtual module. Prior to this, the students had spent approximately seven months and four modules completing their learning in a predominantly face-to-face environment, with some virtual elements included (all lectures were recorded and available online, except for anatomy lab sessions). The students had a one-week Spring Break between the Neuroscience module and the previous module.
Institutional Review Board approval was obtained from University of South Carolina (IRB#00,099,883) to conduct research with the medical students. Participants were asked to volunteer to participate in the study through email recruitment, and all students who consented to participate received a link for participation. All data were collected using RedCap (Research Electronic Data Capture) on an electronic device. First year medical students were emailed an invitation to participate in a study to assess changes in sleep approximately one month after the stay-at-home order. Each student was asked to complete a demographics form and a retrospective sleep survey and Pittsburgh Sleep Quality Index (PSQI) based on their memory of their sleep prior to the stay-at-home order and transition to the online learning environment. In addition, the students were asked to complete the same sleep survey and PSQI based on their sleep for the past month, a time period that was after the stay-at-home order. Specifically, students were asked to consider their sleep characteristics during the last month of their Structure and Function module (retrospective for before the stay-at-home order) and then to consider their sleep characteristics for the previous month, during their Neuroscience module (after the stay-at-home order). All students were in the same course with the same learning demands during the time of testing.
Sleep quality was assessed using PSQI, which is the most widely used sleep quality assessment in both clinical and research settings. The PSQI has demonstrated reliability and validity across both medical and non-medical populations (Wolf and Rosenstock 2017; Mollayeva et al. 2016 Feb). In addition, the PSQI has been shown to be valid in even small sample sizes (Mollayeva et al. 2016 Feb). The PSQI measures seven dimensions of sleep, including perceived sleep quality, sleep duration, sleep latency, habitual sleep efficiency, sleep disturbances, use of sleeping medications, and daytime dysfunction. Each of the seven dimensions is scored from 0–3, and all dimensions are summed to give a total sleep quality score. Higher scores indicate lower sleep quality, and a total PSQI score greater than five indicates poor sleep quality (Wolf and Rosenstock 2017).
To assess sleep timing and duration, participants completed questions to document the time they went to bed and got up on weekdays and weekends prior to the stay-at-home order. Participants then completed the same questions with a focus on the previous month, which took place after the stay-at-home order.
Student perceptions of their stress about school were assessed with the following question, developed within our research lab, “Compared to your stress level ABOUT SCHOOL to the shelter-in-place order, do you feel your stress level ABOUT SCHOOL is: Much higher (5), higher (4), the same (3), less (2), or much less (1).” In addition, participants were given the question, “How stressed do you feel about the COVID-19 pandemic and asked to rate it on a similar five-point scale: Extremely stressed (5), very stressed (4), moderately stressed (3), not very stressed (2), not stressed at all (1).” These questions were included on a survey given to participants with their sleep timing and duration questions, as well as their demographics. In total, participants completed two PSQI’s (one for pre-COVID and one post-COVID stay at home orders, as well as one survey that included demographics, sleep timing and duration, and perceptions of stress.
Results
Sleep timing and duration
Sleep timing was assessed to determine changes prior to and following the COVID-19 pandemic stay-at-home order on both weekdays and weekends. Average bedtime on weekdays was 22:20 (Standard Deviation [SD] 1:12 h) pre-COVID and 23:45 (SD 2:02 h) post-COVID. Average weekday wake time pre-COVID was 06:20 (SD 1.12 h) and 08:30 (SD 1:58 h) post-COVID. On weekends, average bedtime pre-COVID was 23:20 (SD 3:26 h) and 00:15 (SD 1:46 h) post-COVID. Weekend average wake time pre-COVID was 08:20 (SD 1:40 h) and post-COVID was 09:05 (SD 1:44 h). Data were not normally distributed for sleep timing (Shapiro–Wilk p < 0.05). A Wilcoxin-signed-rank test found that bed-timing and wake-timing pre- and post-COVID were significantly different, both for weekends and weekdays (p < 0.001).
Sleep duration was assessed so that participants identified sleep times prior to and following the stay-at-home order. Participants were asked the number of hours of sleep received nightly for the previous month, as a part of the PSQI, as well as in a separate question. The PSQI subscale addressing sleep duration is found in Table 1, however it does not elaborate on the actual sleep time. Prior to the stay-at-home order, average sleep duration was 7:56 h (SD 1.01 h), and following the stay-at-home order, average sleep duration was 8:10 h (SD 1.17 h). A repeated-measures multivariate analysis of variance (MANOVA) comparing the two time periods showed that this difference was not significant (p > 0.05).
Sleep quality
The PSQI global and subscale scores were used to assess sleep quality characteristics. The higher the score on the PSQI the worse the participant rates the sleep quality characteristic. The mean pre-COVID PSQI global score was 5.02 (SD 2.42), with 41.46% (n = 17) above a score of 5. Post-COVID PSQI global scores averaged 7.34 (SD 3.62). A majority of students post-COVID, 65.85% (n = 27), were above the clinical cutoff (> 5) for poor sleep quality. PSQI scores were normally distributed (Shapiro–wilk p > 0.05). A repeated-measures MANOVA comparing pre- and post-COVID-19 samples showed that PSQI global scores increased significantly as a result of the COVID-19 pandemic and the resulting stay-at-home orders, F(1, 40) = 13.53, p < 0.001, ηp2 = 0.253, Hotelling’s Trace = 0.464, Pillai’s Trace = 0.369.
Individual components of the PSQI were assessed to determine differences in pre- and post-COVID-19 samples using repeated-measures MANOVA for each component. The results of the MANOVA, as well as the descriptive statistics for each PSQI dimension prior to and following the stay-at-home order, are shown in Table 1.
Relationships between student age, perceived stress, PSQI subscales, and PSQI global scores were examined using Spearman’s rank correlation. Student age was not related to PSQI global or subscale scores except for sleep duration. Older students slept significantly longer post-COVID than did younger students, rho(41) = 0.31, p < 0.05. In addition, older students had more perceived stress about COVID-19 specifically (not about school) than did younger students, rho(41) = 0.37, p < 0.05. Perceived stress specifically about school was not significantly related to either the global or the PSQI subscales.
The PSQI subscale to assess sleep medication use (PSQI subscale six) showed a significant difference in medication use, as revealed in Table 1. A repeated-measures MANOVA revealed a significant difference between pre- and post-scores, F(1,40) = 4.99, p < 0.05, Hotelling’s Trace = 0.167, Pillai’s Trace = 0.143. Post-hoc ANOVAs revealed significant differences in medication use by stay-at-home order time period, with students more likely to use medication less than once a week prior to the stay-at-home order (p < 0.05), and more likely to use medication once or twice a week (p < 0.01) or three or more times a week (p < 0.05) after the stay-at-home order. Refer to Fig. 1 for a graphical representation of the differences in drug use by time period (number of participants for each category are shown).
A one-way MANOVA was conducted to examine the role of gender on each of the PSQI subscales and the PSQI global score. Data from the two participants who did not indicate gender were not included in these analyses. Gender had a significant impact on many PSQI subscales, as well as the global score, after the stay-at-home order. Only perceived sleep quality was affected by gender prior to the stay-at-home order, F (1,36) = 4.79, p < 0.05. In that situation women were more likely to perceive poor sleep quality, with a PSQI of 1.00 (SD 0.53) as compared to men who had a PSQI for perceived sleep quality of 0.56 (SD 0.53). However, after the stay-at-home order, men were significantly more likely to perceive poor sleep quality, with PSQI perceived sleep quality scores of 1.89 (SD 0.93) as compared to women’s scores of 1.24 (SD 0.629), F (1,36) = 5.13, p < 0.05. The PSQI global and five of the PSQI subscales were significantly different between genders post-COVID. However, when student age and perceived stress (about school and COVID) were factored out of the analysis using a Multivariate Analysis of Covariance (MANCOVA), only two of the subscales and the global PSQI score were significantly different. Details on the post-stay-at-home order PSQI and gender descriptive statistics, as well as the MANCOVA scores, can be found in Table 2. Only significant results are shown.
Discussion
This study assessed the effects of the COVID-19 pandemic stay-at-home orders on medical student sleep quality, deprivation, duration, and timing. In addition, variables such as gender, age, and perceived stress about school and about the COVID-19 pandemic were assessed to determine if they influenced changes in sleep.
Retrospective analysis shows that sleep timing in medical students was significantly different following the stay-at-home order. Student times-to-bed and waking times were phase-delayed by approximately an hour for both weekdays (when they had school lectures) and weekends. Weekday rising times showed the largest shift, with a two-hour delay post-COVID as compared to pre-COVID. It should be noted that variability in sleep timing increased post-COVID, especially on weekends, so the effects of the stay-at-home order on sleep in medical students was not uniform. While there are no studies that examine the effects of stay-at-home orders on sleep timing in medical students currently available, this shift in sleep timing is similar to what is seen in free running rhythms when certain zeitgebers are removed from the environment. While light is the main zeitgeber that resets the circadian clock, several other factors, such as social cues, food timing, and sleep/activity cycles can also exert an influence on the phase of the daily rhythm (Duffy et al. 1996). These results are also similar to changes in sleep behavior seen in several other university students’ sleep since COVID (Zakariya and Low 2020; Martínez-Lezaun et al. 2020; Alyoubi et al. 2021 Jan), although the scholastic demands and scheduling for medical students is a unique environment.
Sleep duration was assessed to determine if the change in students’ responsibilities on campus due to virtual delivery of the curriculum had an effect. No significant changes to sleep duration were found, for either weekdays or weekends, based upon the stay-at-home order. Much of this can be attributed to the fact that there was enormous variability in sleep duration after the stay-at-home order, with some people sleeping many more hours than prior to COVID, and some people sleeping fewer hours. Overall, no effect was found, but further investigation into characteristics related to duration changes may be warranted.
Several aspects of sleep quality were impacted by the stay-at-home order, including the PSQI global score of overall sleep quality. Prior to COVID-19 the majority of medical students reported good sleep quality scores, but after COVID-19 more than 65% of medical students reported poor sleep quality, with the average of all students assessed meeting the clinical cutoff of the PSQI for poor sleep quality (Shad et al. 2015). Perceived sleep quality, sleep latency, sleep efficiency, and daytime dysfunction all worsened significantly after the stay-at-home order. This is especially concerning, given that poor sleep efficiency and quality increase the incidence of depression and burnout in medical students (Zakariya and Low 2020). Additionally, daytime dysfunction almost doubled post-COVID, and poor daytime dysfunction is significantly related to burnout and disengagement in medical students (Martínez-Lezaun et al. 2020).
The use of sleep medications as assessed by the PSQI demonstrated that student use of sleep medication increased significantly after the stay-at-home order. Prior to the COVID-19 pandemic, the few students (32%) who used sleep medication used it sparingly, less than once a week. However, following the COVID-19 pandemic, use of sleep medication less than once a week decreased, but medication use twice a week or three times a week more than doubled, with a 5% overall increase in sleep medication use after COVID-19. There is a paucity of research on medical student use of sleep medication and its effects, and given that more than 30% of students used sleep medications regardless of stay-at-home order, this is an area that should receive more attention.
Stress from COVID-19 and the resulting stay-at-home orders have been shown to create greater sleep problems for women than men (Casagrande et al. 2020). The results from this study did not find this to be the case in the medical student population. Prior to the stay-at-home order, females reported significantly lower sleep quality than males, but after the stay-at-home order, males reported significantly worse sleep quality than females. Specifically, males in this study reported significantly worse sleep duration, sleep efficiency, daytime dysfunction, and global PSQI scores. Once age and stress were controlled for, however, only perceived sleep quality, daytime dysfunction, and the global PSQI were significantly different, with men having higher (worse) scores on each of those. However, this study only had 9 males who completed all aspects of the study, which severely limits the generalizability of the results, so more research with a larger sample size is needed. In addition, stress about COVID and stress about school were assessed through only two questions. Future research related to COVID and social isolation should utilize validated measures of perceived stress.Medical students, much like the general public (Brenan 2020) and other students (Cao et al. 2020), reported that they felt elevated stress due to the COVID-19 pandemic (Guo et al. 2021 Jan). This effect was significantly higher in older first year medical students as compared to the younger students. However, unlike previous research (Lavie 2001; Philbert et al. 2011; Touma et al. 2009; Almojali et al. 2017; Casagrande et al. 2020), medical student stress about the COVID-19 pandemic and about school was not related to any PSQI global or subscale scores. This was an unexpected finding and raises the question about why this student population’s stress did not appear to influence their sleep quality. It also raises a question about the causes of decreases in sleep quality post-COVID-19 if stress was not responsible for this change.
This study was limited by the small sample size (41) and incomplete data from some of the subjects. Subjective sleep quality, as assessed by the PSQI, and surveys were used to assess sleep variables in medical students, but no physiological factors were assessed. Since self-report is notoriously unreliable, future research should include objective measures of sleep, in addition to self-report. In addition, the retrospective nature of the surveys required participants to think back and make judgements about their sleep perceptions four weeks prior to the stay-at-home order, during the previous module and compare them to their current module (post stay-at-home order). Future studies should attempt to include prospective analyses or control groups, if possible.
Conclusions
In conclusion, this study represents the first known research to demonstrate possible effects of the COVID-19 stay-at-home orders on sleep disturbances in medical students in the United States, specifically in deprivation, duration, timing, quality and sleep medication. In addition, this research furthers the work by Xiao (2020) showing that social isolation due to the stay-at-home orders can result in changes detrimental to sleep (Xiao et al. 2020). Sleep is a vital factor for medical students, and social isolation and changes in the learning environment can have a detrimental effect on sleep quality and timing. Based on this research, medical educators and medical schools should consider giving more attention to helping medical students address factors related to their sleep, including the use of sleep medications. This is especially important as the medical school learning environment continues to adapt to the COVID-19 pandemic.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Code availability
N/A.
References
Ahmed N, Sadat M, Cukor D (2017) Sleep knowledge and behaviors in medical students: results of a single center survey. Acad Psychiatry. https://doi.org/10.1007/s40596-016-0655-3
Almojali AI, Almalki SA, Alothman AS, Masuadi EM, Alaqeel MK (2017) The prevalence and association of stress with sleep quality among medical students. J Epidemiol Global Health 7(3):169–174
Alyoubi A, Halstead EJ, Zambelli Z, Dimitriou D (2021) The Impact of the COVID-19 Pandemic on Students’ Mental Health and Sleep in Saudi Arabia. Int J Environ Res Public Health 18(17):9344
Ayala EE, Berry R, Winseman JS, Mason HR (2017) A cross-sectional snapshot of sleep quality and quantity among US medical students. Acad Psychiatry 41(5):664–668
Brenan, M. “Americans say COVID-19 hurting mental health most.” Gallup. April 15, 2020. https://news.gallup.com/poll/308420/americans-say-COVID-hurting-mental-health.aspx
Brick CA, Seely DL, Palermo TM (2010) Association between sleep hygiene and sleep quality in medical students. Behav Sleep Med 8:113–121
Cao W, Fang Z, Hou G et al (2020) The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res 287:112934. https://doi.org/10.1016/j.psychres.2020.112934
Casagrande M, Favieri F, Tambelli R, Forte G (2020) The enemy who sealed the world: Effects quarantine due to the COVID-19 on sleep quality, anxiety, and psychological distress in the Italian population. Sleep Medicine, Advance Online Publication. https://doi.org/10.1016/j.sleep.2020.05.011
Duffy JF, Kronauer RE, Czeisler CA (1996) Phase-shifting human circadian rhythms: influence of sleep timing, social contact and light exposure. J Physiol 495(1):289–297
Frank E, Carrera JS, Elon L, Hertzberg VS (2006) Basic demographics, health practices, and health status of U.S. medical students. Am J Prev Med 31(6):499–505
Guo AA, Crum MA, Fowler LA (2021) Assessing the psychological impacts of CoViD-19 in undergraduate medical students. Int J Environ Res Public Health 18(6):2952
Jahrami H, Dewald-Kaufmann J, AlAnsari AM, Taha M, AlAnsari N (2019) Prevalence of sleep problems among medical students: a systematic review and meta-analysis. J Public Health 28:1–18
Jorden MA, Rudman SL et al (2020) Evidence for limited early spread of COVID-19 Within the United States, January–February 2020. MMWR Morb Mortal Wkly Rep 69:680–684. https://doi.org/10.15585/mmwr.mm6922e1
Lavie P (2001) Sleep disturbances in the wake of traumatic events. N Engl J Med 345(25):1825–1832. https://doi.org/10.1056/NEJMra012893
Martínez-Lezaun I, Santamaría-Vázquez M, Del Líbano M (2020) Influence of confinement by COVID-19 on the quality of sleep and the interests of university students. Nat Sci Sleep 12:1075
Mollayeva T, Thurairajah P, Burton K, Mollayeva S, Shapiro CM, Colantonio A (2016) The Pittsburgh sleep quality index as a screening tool for sleep dysfunction in clinical and non-clinical samples: A systematic review and meta-analysis. Sleep Med Rev 1(25):52–73
Papp KK, Miller CM, Strohl KP (2006) Graduate medical training, learning, relationships, and sleep loss. Sleep Med Rev 10(5):339–345
Philbert J, Pichat P, Beeske S, Decobert M, Belzung C, Griebel G (2011) Acute inescapable stress exposure induces long-term sleep disturbances and avoidance behavior: a mouse model of post-traumatic stress disorder (PTSD). Behav Brain Res 221(1):149–154. https://doi.org/10.1016/j.bbr.2011.02.039
Shad R, Thawani R, Goel A. Burnout and sleep quality: a cross-sectional questionnaire-based study of medical and non-medical students in India. Cureus. 7(10)
South Carolina Exec. Order No, 2020–21 (April 6, 2020), https://governor.sc.gov/executive-branch/executive-orders
Touma C, Fenzl T, Ruschel J, Palme R, Holsboer F, Kimura M et al (2009) Rhythmicity in mice selected for extremes in stress reactivity: behavioural, endocrine and sleep changes resembling endophenotypes of major depression. PLoS ONE 4(1):e4325. https://doi.org/10.1371/journal.pone.0004325
Van Bavel, J.J., Baicker, K., Boggio, P.S., Capraro, V., Cichocka, A., Cikara, M., Crockett, M.J., Crum, A.J., Douglas, K.M., Druckman, J.N. and Drury J. (2020) Using social and behavioural science to support COVID-19 pandemic response. Nature Human Behaviour
Williams WC, Morelli SA, Ong DC, Zaki J (2018) Interpersonal emotion regulation: Implications for affiliation, perceived support, relationships, and well-being. J Pers Soc Psychol 115:224–254
Wolf MR, Rosenstock JB (2017) Inadequate sleep and exercise associated with burnout and depression among medical students. Acad Psychiatry 41(2):174–179
Xiao H, Zhang Y, Kong D, Li S, Yang N (2020) Social capital and sleep quality in individuals who self-isolated for 14 days during the coronavirus disease 2019 (COVID-19) outbreak in January 2020 in China. Medical Science Monitor: International Medical Journal of Experimental and Clinical Research 26:e923921–e923931
Zakariya MZ, Low JM (2020) The effects of confinement on sleep quality and level of interest in University students. Nat Sci Sleep 12:1225–1226
Acknowledgements
The authors wish to thank the Class of 2023 medical students at the University of South Carolina School of Medicine Greenville for the contribution of their time during the stay-at-home order due to COVID-19 in 2020.
Funding
This research received no external funding.
Author information
Authors and Affiliations
Contributions
Conceptualization, LF; methodology LF and NK; data collection NK and LF; data analysis LF and NK; original draft preparation, LF; review and editing, NK and LF. Both authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
Institutional Review Board approval was obtained from University of South Carolina (IRB#00099883) to conduct research with the participants in this study.
Consent to participate
All participants consented to participate in this study.
Consent for publication
All participants consented to have deidentified data used for presentation and publication.
Rights and permissions
About this article
Cite this article
Fowler, L.A., Kumte, N. The effect of COVID-19 pandemic stay-at-home orders on sleep deprivation in medical students: a retrospective study. SN Soc Sci 2, 29 (2022). https://doi.org/10.1007/s43545-022-00323-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s43545-022-00323-w