Abstract
Introduction
Available therapies for acute cough, a condition frequently caused by a viral upper respiratory tract infection (URTI), have shown limited evidence of efficacy. Gefapixant, a P2X3-receptor antagonist, has demonstrated efficacy and safety in studies of the treatment of refractory or unexplained chronic cough, but its efficacy for treating acute cough has not been previously studied.
Methods
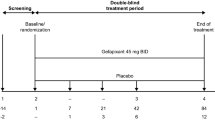
This was a phase 2a, randomized, double-blind, placebo-controlled, parallel-group, pilot study. Healthy volunteers were randomized 1:1 to receive twice-daily gefapixant 45 mg or placebo and inoculated with human rhinovirus 16 to induce URTI and cough. Participants were observed while quarantined for 7 days after the start of treatment. The primary endpoint was awake cough frequency on day 3, which was objectively measured with a cough-recording device. Secondary endpoints included change from baseline to day 3 in subjective cough severity measures (cough severity visual analog scale, Cough Severity Diary) and cough-specific quality of life (Leicester Cough Questionnaire–acute).
Results
Of the 46 participants who met inclusion criteria [mean (standard deviation, SD) age, 24.6 (6.5) years; females, n = 8], 40 completed the study (gefapixant, n = 21; placebo, n = 19). There was no significant difference in awake cough frequency on day 3 between the gefapixant and placebo groups [least squares means, 2.4 versus 2.7 coughs per hour, respectively; mean difference (95% confidence interval, CI), −0.3 (−2.3, 1.7); P = 0.75]. There were no significant between-group differences for any of the secondary endpoints. Peak cough frequency was low and occurred later in the study than expected (days 4–5). The safety profile was consistent with that of previous studies of gefapixant.
Conclusion
Compared with placebo, gefapixant did not reduce the frequency or severity of acute cough secondary to induced URTI. Induced viral URTI produced mild symptoms, including lower cough frequency than observed in previous studies of patients selected for acute cough associated with naturally occurring URTI.
Trial Registration
ClinicalTrials.gov, NCT03569033; EudraCT, 2017-000472-28; protocol number, MK-7264-013.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Acute cough, defined as cough lasting less than 3 weeks, can be a bothersome symptom of the common cold, and current available treatments often do not provide cough relief or have unwanted side effects. |
This study investigated whether gefapixant, a drug recently shown to be safe and effective in the treatment of chronic cough (i.e., cough lasting more than 8 weeks) in clinical trials, is effective in treating acute cough after voluntary infection with a virus that causes the common cold. |
What was learned from the study? |
Among participants with acute cough receiving gefapixant versus placebo, there were no differences in number of coughs per hour or in participant perceptions regarding cough. |
This is the first study investigating the effect of a cough treatment on acute cough in participants voluntarily infected with the common cold, and symptoms including cough were found to be mild overall. |
Introduction
Acute cough, defined as a cough lasting less than 3 weeks, is a common condition that is most frequently caused by an acute viral upper respiratory tract infection (URTI), otherwise known as the common cold [1, 2]. It has been estimated that between 69% [3] and 80% [4] of patients with a URTI will develop a cough. In prior studies of otherwise healthy patients complaining of acute cough related to a naturally occurring URTI, initial cough frequency was approximately 12–14 coughs per hour, followed by a progressive reduction in cough frequency [5, 6]. Although a cough due to a viral URTI is typically transient and self-limiting, patients with a bothersome acute cough may be treated with symptomatic therapies [2]. However, available therapies for acute cough (e.g., narcotic, non-narcotic, and over-the-counter medications) have limited or unproven efficacy and undesirable side effects [7,8,9].
Studies that include individuals with natural URTIs (rather than induced URTIs) are challenged by uncontrollable variability in viral incubation times and viral agents and serotypes that cause URTIs [10, 11]. Additionally, early symptoms may go unnoticed by patients, and time to intervention may be delayed [10]. Because viral URTI-associated cough is often short-lived and self-limiting, induced URTIs in an investigational setting could be valuable for initial proof of concept when evaluating acute cough treatments by improving the precision in measuring viral incubation times and timing of intervention [10].
The leading cause of URTIs, human rhinovirus (HRV), can be induced via intranasal or conjunctival inoculation [12] and has the advantage of replicating the pathology of an acute URTI [13]. Previous studies have induced URTIs in healthy volunteers to evaluate efficacy of potential cold treatments, such as zinc lozenges and probiotics [14, 15]. To the authors’ knowledge, prior studies implementing virally induced URTI models have not objectively monitored cough or assessed antitussives for acute cough.
Gefapixant, a P2X3-receptor antagonist, has demonstrated efficacy and safety in refractory chronic cough (RCC) and unexplained chronic cough (UCC) in several clinical trials [16,17,18]. P2X3 receptors are ligand-gated ion channels that respond to adenosine triphosphate and are expressed by sensory nerves that mediate cough [19,20,21]. In previous trials, gefapixant demonstrated reduced cough frequency [17, 18] and cough-reflex sensitivity [22] in patients with RCC or UCC. Patients with acute cough share some features with patients with RCC or UCC, including hypersensitivity of the cough reflex to inhaled irritants and throat irritation/sensitivity to environmental exposures [23, 24], raising the possibility of similar underlying mechanisms and the possibility that gefapixant might be beneficial in acute cough associated with viral URTI. This pilot study was conducted to assess the efficacy, safety, and tolerability of gefapixant for the treatment of acute cough associated with virally induced URTI.
Methods
Study Design
This was a phase 2a, randomized, double-blind, placebo-controlled, parallel-group study (ClinicalTrials.gov, NCT03569033; EudraCT, 2017-000472-28). The study was performed in accordance with the Declaration of Helsinki, Good Clinical Practice requirements, and applicable country/local statutes and regulations regarding ethics committee review. The study protocol and amendments, information provided to participants, and recruitment material were reviewed and approved by East of England–Essex Research Ethics Committee (Nottingham, UK). All participants provided written informed consent before enrollment.
The study had an adaptive design with two planned stages separated by an interim analysis. Stage 1 compared twice-daily gefapixant 45 mg versus placebo (1:1 randomization via computer-generated permuted-block algorithm) at a single center. If the predefined futility criteria for the interim analysis after stage 1 were not met, stage 2 was planned to compare twice-daily gefapixant 45 mg versus placebo (1:1 randomization) or twice-daily gefapixant 45 mg versus twice-daily gefapixant 15 mg versus placebo (1:2:1 randomization) at more than one center.
Participant Eligibility
Eligible participants were male and female volunteers aged between 18 and 55 years who were in good general health with no clinically relevant abnormalities and were determined to be susceptible to HRV-16, as evidenced by a serum-neutralizing antibody titer of 1:4 or less. Exclusion criteria included pregnancy; recent history of URTI or lower RTI; a significant change in pulmonary status within 4 weeks of baseline; a body mass index < 18 or ≥ 40 kg/m2; an estimated glomerular filtration rate < 50 mL/min/1.73 m2; or use of medications for an acute viral URTI within 24 h of study enrollment. Current smokers, smokers within 5 years of screening, and former smokers with a smoking history of > 20 pack-years were also excluded.
Study Procedure
After screening, participants were confined to the clinic for 2 days for baseline observation before treatment initiation. If no signs or symptoms of a URTI or other infections were observed, participants were randomized 1:1 on day 1 to receive twice-daily gefapixant 45 mg or matching placebo for 7 days. Randomization was stratified according to sex (male, female) and site.
Upper respiratory tract infections were induced with HRV-16 to assess the study treatment. After randomization on day 1, participants were intranasally inoculated with HRV-16, immediately followed by administration of the first dose of gefapixant or placebo. All participants were required to demonstrate viral shedding via nasal swab testing 72 h after HRV-16 inoculation to continue in the trial and be included in the final analysis. Participants remained in the facility for the 7-day treatment period and were discharged the following day. A safety follow-up was conducted by telephone approximately 2 weeks after discharge.
Endpoints and Assessments
The primary endpoint was awake cough frequency on day 3 of the treatment period. Day 3 was selected as the primary timepoint on the basis of previous author experience that suggested increases in individuals’ subjective cough perceptions after HRV infection occur around this time. Cough was measured using a digital-recording cough-monitoring device (VitaloJAK; Vitalograph Ltd, Buckingham, UK). The device was worn during the entirety of the 7-day treatment period (except during approximately 15 min of “off-time” permitted for showering each day). Two channels were used for sound recording: one channel recorded sounds from the lungs and trachea via a chest contact sensor, and the other channel captured ambient sounds through a lapel air microphone. To reduce review time, the 24-h recordings were processed through a computerized algorithm that removed periods of silence and noncough sounds; a cough analyst subsequently evaluated for cough sounds [25]. Cough counts were quantified and expressed as coughs per hour.
Secondary endpoints included change from baseline to day 3 on subjective measures of cough severity and impact on cough-specific quality of life. Patient-reported cough severity was assessed using a cough severity visual analog scale (VAS), a single-item questionnaire with a recall period of “today,” in which patients rate severity of their cough on a 100-mm scale, with 0 indicating “no cough” and 100 indicating “extremely severe cough.” Patient-reported cough severity was also assessed via the Cough Severity Diary (CSD), a seven-item questionnaire assessing cough frequency, intensity, and disruption, with a recall period of “today” [26]. Each item of the CSD is rated on a scale of 0–10, with higher scores reflecting greater severity. The CSD total score, ranging from 0 to 10, was calculated by averaging scores from all seven items. Cough-specific quality of life was measured using the Leicester Cough Questionnaire (LCQ)–acute, a 19-item questionnaire that measures the impact of cough-specific quality of life on physical, psychological, and social domains [27]. Each item on the LCQ-acute is rated on a scale of 1–7, for a total score range of 3–21 and domain scores ranging from 1 to 7. Lower LCQ-acute scores reflect a more impaired quality of life. Vital signs, physical evaluations, electrocardiograms, laboratory tests, and the number of participants experiencing adverse events (AEs) or discontinuing treatment because of AEs were recorded and subsequently analyzed to evaluate safety and tolerability.
Exploratory endpoints included additional measures of objective cough frequency. Using the VitaloJAK device, 24-h cough frequency (on day 3) and awake cough frequency (on days 1, 2, 4, 5, 6, and 7) were assessed. Change from baseline to day 3 on the Wisconsin Upper Respiratory Symptom Survey–24 (WURSS-24) score was assessed as an additional patient-reported outcome. WURSS-24 is a 24-item quality-of-life instrument designed to assess the negative effects of URTI symptoms on a 7-point scale ranging from 1 (very mild) to 7 (severe) [28, 29]. Finally, blood samples were collected on days 1, 2, 4, and 7 to analyze pharmacokinetic parameters, including time to reach maximum observed concentration and accumulation ratio (measured by area under the concentration–time curve ratio of day 7 to day 1).
Post hoc analyses included 24-h cough frequency and change from baseline on the cough severity VAS, CSD, LCQ-acute, and select symptom scores from the WURSS-24 (i.e., cough, runny nose, plugged nose, sneezing) for days 1–7.
Statistical Analysis
Efficacy was assessed in a modified full analysis set that consisted of all randomized participants who received at least one dose of trial treatment and had confirmed HRV-16 infection at 72 h after inoculation. Safety was assessed in all randomized participants who received at least one dose of trial treatment. An interim analysis was planned after randomization of approximately 50 participants (stage 1); if the study was deemed nonfutile, enrollment was planned to continue to stage 2. The prespecified futility criteria were based on an observed relative reduction of < 5% versus placebo in the primary endpoint of awake cough frequency on day 3, as well as the clinical relevance of the reduction. The observed relative reduction of 5% was based on the posterior probability of 19% that the true relative reduction is > 15% (considered a low level of efficacy).
Objective cough frequency endpoints, including the primary endpoint, were analyzed using a longitudinal data analysis model consisting of non-log-transformed (i.e., original scale) daily coughs per hour at each postbaseline visit as the response vector, with treatment, visit, treatment-by-visit interaction, sex, and site as covariates. A post hoc analysis using log-transformed data was also performed. The patient-reported endpoints were analyzed using a longitudinal analysis of covariance model, with treatment, visit, treatment-by-visit interaction, sex, site, and baseline value as covariates. Safety events were summarized with descriptive statistics.
Results
Baseline Characteristics and Demographics
The study was conducted from 4 July 2018 to 19 November 2018. Of 156 individuals assessed, a total of 46 participants met eligibility criteria and were randomized to receive either twice-daily gefapixant 45 mg (n = 23) or matching placebo (n = 23; Fig. 1) in stage 1. The most common reasons for study exclusion due to screening failure were a lack of general good health or lack of HRV-16 susceptibility. Two participants receiving gefapixant withdrew before study completion, and four participants receiving placebo had a negative nasal swab for HRV-16 and were discontinued from treatment. Accordingly, the final sample size for analyses included 21 and 19 participants in the gefapixant and placebo (i.e., untreated) groups, respectively. Most enrolled participants were white males, and baseline demographics and characteristics were well balanced between groups (Table 1).
Primary Endpoint
In the interim analysis after stage 1, the primary endpoint for the study was not met. There was no significant difference in least squares (LS) means of awake cough frequency between the gefapixant and placebo groups on day 3 [2.4 versus 2.7 coughs per hour, respectively; mean difference (95% CI), −0.3 (−2.3, 1.7); P = 0.75; Table 2]. The awake cough frequency ranges on day 3 were 0–11.8 coughs per hour (gefapixant group) and 0–12.5 coughs per hour (placebo group). The interim analysis results met the predefined futility criteria after stage 1, and the study was terminated. A post hoc analysis of the primary endpoint using log-transformed awake cough frequency revealed similar results (data not shown).
Secondary Efficacy Endpoints
There were no significant differences between the gefapixant and placebo groups among the secondary efficacy endpoints (i.e., cough severity VAS score, CSD score, or LCQ-acute score change from baseline to day 3; Table 2).
Exploratory Endpoints
In an exploratory analysis of awake cough frequency at timepoints during the treatment period other than day 3, no significant differences in awake cough frequency between groups were observed (Fig. 2). Peak model-based estimated mean awake cough frequency values were observed on days 4 and 5 for both groups.
Gefapixant did not yield an improvement over placebo in any of the other exploratory efficacy endpoints. There was no significant difference in LS means of 24-h cough frequency between the gefapixant and placebo groups on day 3 [1.9 versus 1.9 coughs per hour, respectively; mean difference (95% CI), 0.01 (−1.4, 1.4); P = 0.99]. There was also no significant difference in LS means of WURSS-24 total scores between the gefapixant and placebo groups on day 3 [13.1 versus 21.5, respectively; mean difference (95% CI), −8.4 (−17.0, 0.3); P = 0.06].
The median time to reach maximum observed concentration after gefapixant administration was 2 h on both day 1 and day 7 of the treatment period. Repeated administration resulted in a gefapixant plasma accumulation ratio of approximately 1.5 between day 7 and day 1.
Post Hoc Analyses
Similar to awake cough frequency, peak 24-h cough frequency occurred on day 4 for both gefapixant and placebo (Fig. 3a). Peaks in changes from baseline in cough severity VAS (Fig. 3b), CSD (Fig. 3c), LCQ-acute (Fig. 3d), and WURSS-24 cough scores (Fig. 4a) were observed on days 4 and 5, consistent with the trends in objective cough frequency. In contrast, peak changes from baseline in WURSS-24 scores for runny nose (Fig. 4b), plugged nose (Fig. 4c), and sneezing (Fig. 4d) were observed a bit earlier on days 3 and 4. For all symptoms rated on the WURSS-24, mean daily scores of all participants were below the WURSS-24 threshold for “mild” (i.e., scores ≤ 3) [28] throughout the duration of the study.
Post hoc analyses over treatment period of a 24-h cough frequency, b change from baseline in cough severity VAS scores, c change from baseline in CSD scores, and d change from baseline in LCQ-acute scores. Error bars represent SE (panel A) and SD (panels B–D). BID twice daily, CSD Cough Severity Diary, LCQ Leicester Cough Questionnaire, LS least squares, VAS visual analog scale
Safety
Overall incidences of AEs were comparable between the treatment groups, though treatment-related AEs were observed only in the group receiving gefapixant (Table 3). Six participants in the gefapixant group reported treatment-related AEs, of whom four reported AEs related to taste disturbance (including three who reported hypogeusia and two who reported dysgeusia) and three reported nausea. The most frequent AE in both groups was URTI (an expected event due to the study design). The second most frequent AE was erythema at the site of the VitaloJAK cough-monitor chest sensor.
Discussion
This pilot study represents the first time a virally induced URTI model was implemented to objectively monitor cough and assess the antitussive effect of a drug (gefapixant) on acute cough in a healthy population. Although gefapixant previously demonstrated efficacy in reducing cough frequency and improving cough-specific quality of life in phase 3 studies enrolling participants with chronic cough (RCC or UCC) [30], the current study using an acute cough model found no significant differences between the twice-daily gefapixant 45-mg and placebo groups in awake cough frequency, 24-h cough frequency, cough severity (as measured by the cough severity VAS and CSD), or cough-specific quality of life (as measured by the LCQ-acute). The gefapixant safety profile was comparable between this study in acute cough and studies of patients with RCC or UCC, with the most commonly reported treatment-related AEs being taste related [16,17,18].
Although the infection rate in the study was high (> 90%), cough frequency and other URTI symptoms were overall mild for both treatment groups. A previous report suggested that symptoms of acute cold (e.g., rhinorrhea, nasal obstruction) were more severe in individuals with natural colds compared with those infected with induced rhinovirus [31]. Although it is possible that rhinovirus models induce less severe illness than natural colds, comparisons with natural cold studies are challenging. The authors acknowledge that rhinovirus models will likely include all participants with confirmed infection, including those who develop the mildest of symptoms in response to the virus. However, in a real-world setting, individuals with mild symptoms are less likely to volunteer for a clinical study of natural colds; therefore, selection bias may ultimately favor participants with more severe symptoms in studies of natural cold. As it is unclear how individuals’ past experiences with symptoms during naturally acquired colds (i.e., mild versus severe symptoms) would affect their willingness to volunteer for an induced rhinovirus study, the direct impact of selection bias on this study is difficult to estimate. Additionally, comparisons between this study model and naturally acquired colds is further complicated by the fact that naturally acquired colds may occur as a consequence of different rhinoviruses associated with varying degrees of symptoms, whereas this study assessed only one rhinovirus that ultimately induced mild symptoms.
Consistent with this notion, in the current induced-URTI study, participants demonstrated an average of approximately two to three awake coughs per hour on day 3, peaking to approximately five to seven awake coughs per hour on days 4 and 5. This cough frequency was much lower than that reported in a study of awake cough frequency in healthy volunteers complaining of cough due to naturally acquired URTI, who demonstrated ~ 19 daytime coughs per hour [6]. Subjective measures of cough severity were also less severe in participants from the current study than those previously reported by otherwise healthy volunteers with acute cough due to acquired URTI for both cough severity VAS scores (10 versus 46 mm, respectively) and LCQ-acute scores (20 versus 14, respectively) [5]. Overall symptom severity using the WURSS-24 revealed that the highest mean WURSS-24 scores were ≤ 3, indicating that symptoms were on average “very mild” to “mild” for both treatment groups across the study duration [28]. Ultimately, the mild symptoms (including cough) with this induced rhinovirus model may not have been ideal for evaluating antitussives for acute cough in its current study design.
Although cough frequency and severity in this study were generally mild, there were similarities between the study data and previous studies. The peak of WURSS-24 nasal symptom scores on day 3, followed by the peak of awake cough frequency and other cough-specific measures on day 4 or 5, is consistent with findings from a previous study of virally induced URTI that reported peak symptom severity for nasal symptoms (e.g., sneezing, rhinorrhea, and nasal obstruction) occurring 2–3 days after inoculation but peak cough severity occurring ~ 4 days after inoculation [10].
The low cough frequency and mild symptom severity observed in this study could be explained by multiple factors. First, the virus used for induction of URTI caused only mild symptoms. Second, prior studies of participants with naturally acquired colds selected for participants complaining of acute cough, whereas the current study did not. Third, participants remained in the clinic for the entirety of the study, so the stable clinical environment may not have exposed them to other potential cough triggers. Fourth, in the clinical setting, participants did not participate in typical daily activities, which may have influenced their perception of cough severity (i.e., URTI-related disruption of daily activities was not a concern). Finally, participants in this study were predominantly male, but previous studies report that females have a higher URTI-related cough frequency, 24-h cough frequency related to chronic cough, and cough-reflex sensitivity in response to cough challenges [5, 32, 33]. Demographic characteristics of the study population may, therefore, partially explain the lower-than-anticipated cough frequency.
There were limitations to this model in its current form, but because objective cough frequency has not been assessed in individuals with virally induced URTIs to date, this study may provide insight into the future use of this approach to assess other antitussives for acute cough. For example, the preselected timing of the primary endpoint did not match the natural course of this virally induced model, leading to a limited window of time to observe a potential effect of gefapixant on acute cough. Although the selected primary endpoint was awake cough frequency on day 3, the higher cough frequency on days 4 and 5 suggests that one of these timepoints may have been preferable for the primary analysis. It should also be acknowledged that there is natural variability in symptomatology across individuals [6], and the use of a single-day endpoint may not be optimal. An alternative approach could evaluate cough either as a total cumulative cough or as a mean of the maximum cough throughout the course of infection. Taken together, future studies evaluating novel antitussives for acute cough using virally induced URTI models might benefit from a different study design (including a different timepoint or approach for primary analysis, different rhinovirus).
Conclusions
Collectively, data from this pilot study indicate that the P2X3-receptor antagonist gefapixant did not reduce acute cough resulting from virally induced URTI relative to placebo. However, there were limitations to the study design. Compared with the primary analysis, future studies that use different timepoints or approaches may be useful for evaluating other novel antitussives for acute cough.
References
Irwin RS, French CL, Chang AB, Altman KW, Chest expert cough panel. Classification of cough as a symptom in adults and management algorithms: CHEST guideline and expert panel report. Chest. 2018;153:196–209.
Morice AH, McGarvey L, Pavord I, British Thoracic Society Cough Guideline Group. Recommendations for the management of cough in adults. Thorax. 2006;61(suppl 1):i1–i24.
Witek TJ, Ramsey DL, Carr AN, Riker DK. The natural history of community-acquired common colds symptoms assessed over 4-years. Rhinology. 2015;53:81–8.
Curley FJ, Irwin RS, Pratter MR, et al. Cough and the common cold. Am Rev Respir Dis. 1988;138:305–11.
Lee KK, Matos S, Evans DH, White P, Pavord ID, Birring SS. A longitudinal assessment of acute cough. Am J Respir Crit Care Med. 2013;187:991–7.
Sunger K, Powley W, Kelsall A, Sumner H, Murdoch R, Smith JA. Objective measurement of cough in otherwise healthy volunteers with acute cough. Eur Respir J. 2013;41:277–84.
Eccles R, Morris S, Jawad M. Lack of effect of codeine in the treatment of cough associated with acute upper respiratory tract infection. J Clin Pharm Ther. 1992;17:175–80.
Lee PCL, Jawad MS, Eccles R. Antitussive efficacy of dextromethorphan in cough associated with acute upper respiratory tract infection. J Pharm Pharmacol. 2000;52:1137–42.
Schroeder K, Fahey T. Systematic review of randomised controlled trials of over the counter cough medicines for acute cough in adults. BMJ. 2002;324:329–31.
Gwaltney JM Jr, Hendley JO, Patrie JT. Symptom severity patterns in experimental common colds and their usefulness in timing onset of illness in natural colds. Clin Infect Dis. 2003;36:714–23.
Atkinson SK, Sadofsky LR, Morice AH. How does rhinovirus cause the common cold cough? BMJ Open Respir Res. 2016;3: e000118.
Jacobs SE, Lamson DM, St George K, Walsh TJ. Human rhinoviruses. Clin Microbiol Rev. 2013;26:135–62.
Rao SS, Hendley JO, Hayden FG, Gwaltney JM Jr. Symptom expression in natural and experimental rhinovirus colds [abstract]. Am J Rhinol Allergy. 1995;9:49–52.
Farr BM, Conner EM, Betts RF, Oleske J, Minnefor A, Gwaltney JM Jr. Two randomized controlled trials of zinc gluconate lozenge therapy of experimentally induced rhinovirus colds. Antimicrob Agents Chemother. 1987;31:1183–7.
Turner RB, Woodfolk JA, Borish L, et al. Effect of probiotic on innate inflammatory response and viral shedding in experimental rhinovirus infection—a randomised controlled trial. Benef Microbes. 2017;8:207–15.
Abdulqawi R, Dockry R, Holt K, et al. P2X3 receptor antagonist (AF-219) in refractory chronic cough: a randomised, double-blind, placebo-controlled phase 2 study. Lancet. 2015;385:1198–205.
Smith JA, Kitt MM, Butera P, et al. Gefapixant in two randomised dose-escalation studies in chronic cough. Eur Respir J. 2020;55:1901615.
Smith JA, Kitt MM, Morice AH, et al, for the Protocol 012 investigators. Gefapixant, a P2X3 receptor antagonist, for the treatment of refractory or unexplained chronic cough: a randomised, double-blind, controlled, parallel-group, phase 2b trial. Lancet Respir Med. 2020;8:775–85.
Hermes SM, Andresen MC, Aicher SA. Localization of TRPV1 and P2X3 in unmyelinated and myelinated vagal afferents in the rat. J Chem Neuroanat. 2016;72:1–7.
Undem BJ, Chuaychoo B, Lee M-G, Weinreich D, Myers AC, Kollarik M. Subtypes of vagal afferent C-fibres in guinea-pig lungs. J Physiol. 2004;556(pt 3):905–17.
Kwong K, Kollarik M, Nassenstein C, Ru F, Undem BJ. P2X2 receptors differentiate placodal vs. neural crest C-fiber phenotypes innervating guinea pig lungs and esophagus. Am J Physiol Lung Cell Mol Physiol. 2008;295:L858–65.
Morice AH, Kitt MM, Ford AP, et al. The effect of gefapixant, a P2X3 antagonist, on cough reflex sensitivity: a randomised placebo-controlled study. Eur Respir J. 2019;54:1900439.
Dicpinigaitis PV. Effect of viral upper respiratory tract infection on cough reflex sensitivity. J Thorac Dis. 2014;6(suppl 7):S708–11.
Song WJ, Morice AH. Cough hypersensitivity syndrome: a few more steps forward. Allergy Asthma Immunol Res. 2017;9:394–402.
Smith JA, Holt K, Dockry R, et al. Performance of a digital signal processing algorithm for the accurate quantification of cough frequency. Eur Respir J. 2021;58:2004271.
Martin Nguyen A, Bacci E, Dicpinigaitis P, Vernon M. Quantitative measurement properties and score interpretation of the Cough Severity Diary in patients with chronic cough. Ther Adv Respir Dis. 2020;14:1753466620915155.
Yousaf N, Lee KK, Jayaraman B, Pavord ID, Birring SS. The assessment of quality of life in acute cough with the Leicester Cough Questionnaire (LCQ-acute). Cough. 2011;7:4.
Barrett B, Brown R, Mundt M, et al. The Wisconsin Upper Respiratory Symptom Survey is responsive, reliable, and valid. J Clin Epidemiol. 2005;58:609–17.
Barrett B. Wisconsin Upper Respiratory Symptom Survey—WURSS-24—Daily Symptom Report. 2006. https://www.fammed.wisc.edu/files/webfm-uploads/documents/research/wurss-24.pdf. Accessed 3 Nov 2021.
McGarvey L, Birring SS, Morice AH, et al. Efficacy and safety of gefapixant, a P2X3 receptor antagonist, in chronic cough (COUGH-1 and COUGH-2): results from two double-blind, randomised, placebo-controlled phase 3 trials. Lancet. 2022;399:909–23.
Turner RB, Witek TJ, Riker DK. Comparison of symptom severity in natural and experimentally induced colds [abstract]. Am J Rhinol Allergy. 1996;10:167–72.
Kastelik JA, Thompson RH, Aziz I, Ojoo JC, Redington AE, Morice AH. Sex-related differences in cough reflex sensitivity in patients with chronic cough. Am J Respir Crit Care Med. 2002;166:961–4.
Kelsall A, Decalmer S, McGuinness K, Woodcock A, Smith JA. Sex differences and predictors of objective cough frequency in chronic cough. Thorax. 2009;64:393–8.
Acknowledgments
Funding
This study and any journal-associated fees were supported by Merck Sharp & Dohme LLC, a subsidiary of Merck & Co., Inc., Rahway, NJ, USA.
Medical Writing and Editorial Assistance
Writing and editorial assistance were provided under the direction of the authors by Alexandra Kennedy, PhD, and Jenna Lewis, MA, ELS, of MedThink SciCom, with support from Merck Sharp & Dohme LLC, a subsidiary of Merck & Co., Inc., Rahway, NJ, USA.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
JAS, MMK, AB, NN, MMS, and SL were involved in the conception or design of the study. AB and NN were involved in the acquisition of data. JAS, MMK, NN, AT, AB, and SL were involved with data analysis or data interpretation. All authors participated in drafting the manuscript or revising it critically for important intellectual content, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosures
Jaclyn A. Smith reports grants and personal fees related to the submitted work from Afferent Pharmaceuticals/Merck & Co., Inc.; grants from Ario Pharma, Bayer, Bellus, GlaxoSmithKline, Menlo, and NeRRe Pharmaceuticals; personal fees from Ario Pharma, Bayer, Bellus, Boehringer Ingelheim, Chiesi, Genentech, GlaxoSmithKline, Menlo, Neomed, and NeRRe Pharmaceuticals; and nonfinancial support from Vitalograph. The VitaloJAK algorithm is licensed to Vitalograph Ltd by Manchester University NHS Foundation Trust, which receives royalties that may be paid to the clinical division in which JAS works. Jaclyn A. Smith is also funded by the NIHR Manchester Biomedical Research Centre and a Wellcome Investigator Award and is an NIHR Senior Investigator. Michael M. Kitt is a former employee of Merck Sharp & Dohme LLC, a subsidiary of Merck & Co., Inc., Rahway, NJ, USA. Alan Bell and Nicolas Noulin are employees of hVIVO, a subsidiary of Open Orphan Plc, and may hold stock or stock options in hVIVO. Anjela Tzontcheva, Megan McGratty Seng, and Susan Lu are employees of Merck Sharp & Dohme LLC, a subsidiary of Merck & Co., Inc., Rahway, NJ, USA, and may hold stock or stock options in Merck & Co., Inc., Rahway, NJ, USA.
Compliance with Ethics Guidelines
The study was performed in accordance with the Declaration of Helsinki, Good Clinical Practice requirements, and applicable country/local statutes and regulations regarding ethics committee review. The study protocol and amendments, information provided to participants, and recruitment material were reviewed and approved by East of England–Essex Research Ethics Committee (Nottingham, United Kingdom). All participants provided written informed consent before enrollment.
Data Availability
All data generated or analyzed during this study are included in this published article or are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Smith, J.A., Kitt, M.M., Bell, A. et al. Treatment with the P2X3-Receptor Antagonist Gefapixant for Acute Cough in Induced Viral Upper Respiratory Tract Infection: A Phase 2a, Randomized, Placebo-Controlled Trial. Pulm Ther 8, 297–310 (2022). https://doi.org/10.1007/s41030-022-00193-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41030-022-00193-w