Abstract
Introduction
To determine the optimal dose of sivopixant, a highly selective P2X3 receptor antagonist, for refractory or unexplained chronic cough (RCC/UCC).
Methods
In this phase 2b, randomized, double-blind, placebo-controlled, parallel-group, multicenter trial, patients received sivopixant 50, 150, or 300 mg or placebo once daily for 4 weeks. The primary endpoint was a change from baseline in 24-h cough frequency (coughs/h) with sivopixant vs placebo.
Results
Overall, 390/406 randomized patients completed the study. Placebo-adjusted changes in hourly cough count over 24 h were 13.17% (P = 0.3532), − 1.77% (P = 0.8935), and − 12.47% (P = 0.3241) and in cough severity (visual analog scale) were 1.75 mm (P = 0.5854), − 1.21 mm (P = 0.7056), and − 6.55 mm (P = 0.0433) with sivopixant 50, 150, and 300 mg, respectively. Placebo-adjusted changes from baseline in Leicester Cough Questionnaire total scores were − 0.37 (P = 0.4207), − 0.07 (P = 0.8806), and 0.69 (P = 0.1473) with sivopixant 50, 150, and 300 mg, respectively. Additionally, 61.3%, 78.3%, 86.8%, and 71.4% of patients receiving sivopixant 50, 150, and 300 mg and placebo, respectively, reported any improvements in Patient Global Impression of Change. The incidence of treatment-emergent adverse events (TEAEs) was 25.7%, 32.0%, 49.0%, and 20.6% in sivopixant 50, 150, and 300 mg and placebo groups, respectively; all TEAEs in the sivopixant group were mild-to-moderate.
Conclusion
Sivopixant did not demonstrate a statistically significant difference vs placebo in change from baseline in 24-h cough frequency. The dose of 300 mg has potential for RCC/UCC, showing the greatest improvements in cough frequency and patient-reported outcomes and dose-related mild to moderate reversible taste disturbance, although further trials are needed.
Clinical Trial Registration
ClinicalTrials.gov identifier NCT04110054; registered September 26, 2019.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic cough (CC), defined as cough lasting > 8 weeks, has an estimated global prevalence of 9.6% [1]. Refractory CC (RCC) is defined as CC that persists despite optimal treatment of associated conditions [2, 3] and unexplained CC (UCC) as CC with no known etiology despite extensive clinical assessment and therapeutic trials [3, 4]. Approximately 20–46% of patients presenting to specialist cough clinics have RCC/UCC [5, 6] and face significant physical, psychological, social, and financial burden, resulting in poor quality of life (QoL) [4, 7, 8]. Thus, a significant unmet need exists for safe and effective therapeutic agents for RCC/UCC that can be administered long-term [9, 10].
The P2X3 receptor, an adenosine triphosphate-gated ion channel primarily expressed by sensory nerves, including the airway vagal afferent nerves, has been implicated in cough reflex activation resulting in CC [11, 12]. Several randomized controlled trials (RCTs) have identified P2X3 receptor antagonists as promising therapeutic agents for CC; however, treatment with these agents has been associated with taste disturbances that may affect patients’ QoL and decrease treatment adherence [13,14,15,16]. Sivopixant (S-600918) is a potent P2X3 receptor antagonist with high selectivity for P2X3 over P2X2/3 that may offer advantages including reduced taste disturbance and once-daily (OD) dosing [17]. A phase 2a proof-of-concept crossover study in 31 patients with RCC/UCC found that treatment with sivopixant 150 mg OD for 2 weeks resulted in a − 31.6% and − 30.9% placebo-adjusted change from baseline in the daytime and 24-h average hourly cough frequency, respectively, and a significant improvement in the Leicester Cough Questionnaire (LCQ) total score without major safety concerns [18]. These data support the therapeutic effect of sivopixant. The purpose of this phase 2b study was to determine the optimal dose of sivopixant to treat adults with RCC/UCC.
Methods
Study Design
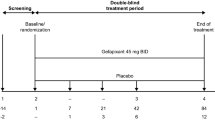
This multinational, multicenter, randomized, double-blind, placebo-controlled, parallel-group phase 2b trial was conducted at 112 study sites in Europe, the United States, and Japan (NCT04110054). Adults who met the inclusion criteria at screening Visit 1 (18–28 days before randomization) were enrolled and underwent 24-h cough monitoring using the VitaloJAK™ cough monitor [19]. At screening Visit 2 (1 day before randomization), patients underwent a further 24-h cough monitoring using the cough monitor. Cough count at Visit 1 was used to assess eligibility and for stratification, whereas cough count at Visit 2 was used as the baseline assessment.
Patients who continued to meet the screening criteria at Visit 3 were randomized in a 1:1:1:1 ratio (93 patients per treatment group) to receive sivopixant 50, 150, or 300 mg or placebo OD for 4 weeks (e-Fig. 1, Online Resource). Randomization was stratified by region (Europe, the United States, or Japan) and 24-h cough count at Visit 1 (≥ 30 or < 30 coughs/h).
The randomization schedule was maintained by interactive response technology until data lock. The sponsor, investigator, and all study-site personnel were blinded to treatment assignment until data lock.
Placebo tablets matched in appearance with the sivopixant 50-mg tablet, and the labeling and packaging of sivopixant and placebo were identical. Patients were followed up for safety for 2 weeks after their last dose.
Patients
Adults aged 18–80 years with RCC/UCC for ≥ 1 year with a cough severity visual analog scale (VAS) score ≥ 40 mm at both screening Visits 1 and 2 and ≥ 10 coughs/h on the 24-h cough count recording at Visit 1 were eligible. Most patients were recruited from pulmonology/respiratory or allergy sites. Diagnosis of RCC/UCC was made by the investigators, and the sponsor did not oversee the accuracy of the diagnosis. Detailed inclusion/exclusion criteria are listed in e-Appendix 1 (Online Resource).
Outcome Assessment and Statistical Analysis
The primary endpoint was the ratio of the number of coughs/h in 24 h at Week 4 to that at baseline. Secondary efficacy endpoints included the ratio of the number of coughs/h while awake/asleep to that at baseline and change from baseline in cough severity (VAS; 0–100 mm; 0: no cough, 100: worst cough ever) [20, 21], LCQ total score [22], and Patient Global Impression of Change (PGIC) [23], which consists of one item adapted from the Clinical Global Impressions scale [24]. Detailed definitions of the endpoints are provided in e-Appendix 2, Online Resource. An improvement in LCQ total score of ≥ 1.3 points identified a treatment responder [25, 26]. Safety assessments included monitoring treatment-emergent adverse events (TEAEs) at each visit, classified by System Organ Class and Preferred Terms using the Medical Dictionary for Regulatory Activities, version 23.0.
The previous phase 2a study observed a mean ± standard deviation (SD) log-transformed ratio of coughs/h in 24 h after 2 weeks of treatment to that at baseline of − 0.327 ± 0.379 with sivopixant 150 mg and − 0.160 ± 0.363 with placebo. The effect size between the placebo and sivopixant groups was assumed to be − 0.44 and the same at 4 weeks. Based on that, the sample size in the current study (80% power using a 2-sided 5% significance level) was calculated as 83 patients per group. By allowing a dropout rate of 10%, 93 patients per treatment group would be needed. Thus, the planned sample size at randomization was 372 patients.
All efficacy analyses were performed in the full analysis set (FAS), and safety analysis was performed in the safety population. The primary endpoint analysis was additionally performed in the per-protocol set (PPS) as supplemental analysis. The analysis sets have been described in e-Appendix 3 (Online Resource).
For the analysis of the primary efficacy endpoint, the ratio of the number of coughs/h in 24 h at each visit to that at baseline was transformed using the common logarithm. The primary endpoints were assessed using a mixed-effects model, with treatment group, week, and the interaction between treatment group and week as fixed effects; patient as random effect; and region and log-transformed coughs/h in 24 h at baseline as covariates. Missing data for cough frequency were not imputed, and observed data were used for the model. Baseline value was defined as the last valid assessment recorded prior to first administration of the study medication. The primary analysis summarized each of the three 2-way comparisons with placebo and presented the estimate for the difference in treatment effect at Week 4 and 95% confidence interval (CI) for this difference. The P value was generated based on the model described above; P < 0.05 was considered statistically significant. Multiplicity adjustment was not performed because this study was exploratory with multiple doses and not a confirmatory study.
In the proof-of-concept study, four patients with baseline hourly cough count values < 10 were included. However, the placebo-adjusted change in cough count was highly variable in this subgroup, and for this reason, patients with cough count < 10 at Visit 1 were excluded from this phase 2b trial. However, we did undertake a post hoc subgroup analysis for the primary and some secondary endpoints in patients with ≥ 10 and < 10 coughs/h in 24 h at Visit 2. All analyses and tabulations were performed using SAS, version 9.2 or higher.
Results
Patients
Between January and December 2020, 644 patients were screened and 406 were enrolled (Fig. 1). Six patients were excluded due to absence of postbaseline cough recordings, resulting in 400 patients in the FAS. Most patients (96.1%; 390/406) completed the study. Reasons for premature study discontinuation included adverse events (AEs; n = 9), patient withdrawal (n = 5), and COVID-19 event (n = 2) (Fig. 1).
Baseline demographic and disease characteristics were balanced between the treatment groups (Table 1). Mean (SD) age of the total population was 57.0 (11.9) years, and most patients were female (73.8%). Geometric mean hourly cough count in 24 h was similar between the groups at baseline (sivopixant 50 mg: 24.36; sivopixant 150 mg: 24.68; sivopixant 300 mg: 26.19; placebo: 24.47).
Change in Hourly Cough Count
Percent change from baseline in hourly cough counts in 24 h following 4 weeks of treatment was − 55.16%, − 61.08%, and − 65.32% with sivopixant 50, 150, and 300 mg, respectively, and − 60.38% with placebo (Fig. 2).
Geometric mean of percent change in hourly cough counts in 24 h from baseline to weeks 1 to 4 (FAS). Treatment effects and their 95% CIs plotted are based on a mixed-effects model for the log-transformed ratio of the number of coughs/h in 24 h at Weeks 1, 3 and 4, with treatment group, week, and interaction between treatment group and week as fixed effects; patient as random effect; and region and the log-transformed coughs/h in 24 h at baseline as covariates. Modeled estimates are presented as geometric mean of percent change from baseline. CI confidence interval, FAS full analysis set
In the FAS, placebo-adjusted changes from baseline in hourly cough counts in 24 h after 4 weeks of treatment were 13.17%, − 1.77%, and − 12.47% with sivopixant 50, 150, and 300 mg, respectively. No significant differences were observed across the sivopixant groups and placebo group (P > 0.05) (Table 2).
In the PPS, placebo-adjusted changes from baseline in hourly cough counts in 24 h following 4 weeks of treatment were 10.66%, − 6.26%, and − 19.29% with sivopixant 50, 150, and 300 mg, respectively (P > 0.05) (e-Table 1, Online Resource). Percent changes in awake/asleep hourly cough counts from baseline to Week 4 were consistent with the 24-h data (e-Table 2; e-Table 3; Online Resource).
Patient-Reported Outcomes
Changes in cough severity (VAS) and LCQ total score were greatest with sivopixant 300 mg (Fig. 3). Placebo-adjusted changes in VAS at Week 4 were 1.75 mm (P = 0.5854), − 1.21 mm (P = 0.7056), and − 6.55 mm (P = 0.0433) with sivopixant 50, 150, and 300 mg, respectively (e-Table 4, Online Resource).
Change from baseline in a weekly cough severity (VAS) and b LCQ total score (FAS). Change from baseline in a weekly cough severity (VAS) and b LCQ total score (FAS). Treatment effects and their 95% CIs plotted are based on a mixed-effects model for the change from baseline in a VAS and b LCQ total score at Weeks 1, 3 and 4, with treatment group, week, and interaction between treatment group and week as fixed effects; patient as random effect; and region and the weekly cough severity on VAS/LCQ total score at baseline as covariates. Modeled estimates are presented as percent change from baseline. CI confidence interval, FAS full analysis set, LCQ Leicester Cough Questionnaire, VAS visual analog scale
Placebo-adjusted changes from baseline to Week 4 in LCQ total score were − 0.37 (P = 0.4207), − 0.07 (P = 0.8806), and 0.69 (P = 0.1473) with sivopixant 50, 150, and 300 mg, respectively (e-Table 5, Online Resource). Overall, 61.6%, 68.3%, 76.9%, and 58.5% of patients receiving sivopixant 50, 150, and 300 mg and placebo, respectively, reported ≥ 1.3-point improvement (responders) in the LCQ total score at treatment completion. The percentage of responders in the sivopixant 300-mg group was 16.9% higher (risk difference, 16.9%; 95% CI 2.6, 31.2) than that in the placebo group (odds ratio [OR], 2.21; P = 0.0227) (Table 3).
Additionally, 61.3%, 78.3%, 86.8%, and 71.4% of patients receiving sivopixant 50, 150, 300 mg, and placebo, respectively, reported any improvements in PGIC. The percentage of patients who reported any improvement was 14.2% higher with sivopixant 300 mg (risk difference, 14.2%; 95% CI 2.7, 25.6) than with placebo (OR 2.54; P = 0.0182) (Table 3).
Post Hoc Subgroup Analysis
In the subgroup of patients with ≥ 10 coughs/h at both screening Visits 1 and 2, placebo-adjusted changes in hourly cough counts in 24 h at Week 4 were 3.51%, − 4.78%, and − 22.85% with sivopixant 50, 150, and 300 mg, respectively (Fig. 4; e-Table 6, Online Resource).
Percent change relative to placebo in hourly cough count in 24 h at Week 4: patients with a cough count of ≥ 10 at Visit 2 in the FAS. Treatment effects and their 95% CIs plotted are based on a mixed-effects model for the log-transformed ratio of the number of coughs/h in 24 h after 4 weeks of treatment, with treatment, week, and treatment by week as fixed effects; patient as random effect; and region and the log-transformed coughs/h in 24 h at baseline as covariates. Modeled estimates are presented as percent change relative to placebo from Visit 2. CC cough count, CI confidence interval, FAS full analysis set
In the small subgroup of patients with a cough frequency ≥ 10 coughs/h at screening Visit 1 that decreased to < 10 coughs/h at screening Visit 2 (sivopixant: 50 mg: 13 patients; 150 mg: 13 patients; 300 mg: 10 patients and placebo: 11 patients), no sivopixant arm showed improvements in cough reduction vs placebo (e-Table 7, Online Resource).
Similarly, consistently greater improvements were observed in VAS, LCQ total score, and PGIC with sivopixant vs placebo in patients with ≥ 10 coughs/h at screening Visits 1 and 2 than in patients with < 10 coughs/h at screening Visit 2 (e-Tables 8–11, Online Resource). In patients with ≥ 10 coughs/h at screening Visits 1 and 2, the percentage of patients who reported ≥ 1.3-point improvement in LCQ total score was 20.7% higher with sivopixant 300 mg than with placebo (OR 2.82; 95% CI 1.31, 6.07), and the percentage of patients who reported any improvements in PGIC was 18.7% higher with sivopixant 300 mg than with placebo (OR 3.59; 95% CI 1.51, 8.53) (e-Table 10, Online Resource). No improvements for any doses were observed for patients with < 10 coughs/h (e-Table 11, Online Resource).
Safety
TEAEs were reported in 25.7%, 32.0%, 49.0%, and 20.6% of patients receiving sivopixant 50, 150, 300 mg, and placebo, respectively. No deaths or serious TEAEs were observed. All TEAEs experienced by patients receiving sivopixant were mild to moderate in severity. Study discontinuation due to TEAEs was low and reported in 8 patients (sivopixant 50 mg, n = 1 [1%]; sivopixant 150 mg, n = 1 [1%]; sivopixant 300 mg, n = 4 [4%]; and placebo, n = 2 [2%]). Three patients (3%) receiving sivopixant 300 mg discontinued treatment due to TEAEs of skin and subcutaneous tissue disorders. The most frequent TEAEs (≥ 5%) in any treatment group were taste-related TEAEs of dysgeusia and hypogeusia with sivopixant and headache with placebo. The incidence of taste-related TEAEs was similar between patients receiving sivopixant 50 mg (2.0%) and those receiving placebo (2.9%), and higher in patients receiving sivopixant 150 mg (13.6%) and 300 mg (33.0%). One patient receiving sivopixant 300 mg (1%) discontinued the study due to ageusia. Most taste-related TEAEs were mild in severity and occurred within 1 week of the study intervention, and most participants recovered during the study treatment or within 1 week of study treatment completion. All treatment-related TEAEs of taste-related events were reversible (Table 4).
Discussion
This multinational, multicenter, randomized, controlled phase 2b trial assessed the impact of different doses of the P2X3 receptor antagonist sivopixant on patients with RCC/UCC over a 4-week period. No sivopixant dose showed a statistically significant difference vs placebo for 24-h cough count at the end of 4 weeks, and the primary study endpoint was not met. Nonetheless, sivopixant showed a dose-dependent effect in reducing the 24-h cough frequency. After 4 weeks of treatment, sivopixant 300 mg showed greater reductions in hourly cough counts over 24 h than placebo, with a − 12.47% placebo-adjusted change. Patient-reported outcomes (cough severity [VAS], LCQ total score, and PGIC responder analyses) suggest that sivopixant 300 mg may be effective for RCC/UCC. Along with the well-tolerated safety profile, sivopixant 300 mg shows promising potential for evaluation in further clinical trials.
While a response to placebo has been seen frequently in other CC trials, improvement in the 24-h cough count (at Week 4) in the placebo group in this study was larger than that reported in other CC trials, with a − 60.38% improvement in 24-h cough count vs a − 31.4% improvement at Week 2 in the phase 2a study [18]. The reasons for higher placebo response are unclear but could be related to the patient population and expectation bias. Patients who experienced spontaneous improvement or improved adherence to background medication during the clinical trial may have been included, further contributing to the high placebo response.
The observed absolute reductions in cough frequency with sivopixant in this study are consistent with other P2X3 receptor antagonist studies [26,27,28]. However, placebo-adjusted differences are smaller, driven by the larger reduction in cough frequency observed in the placebo-treated arm. Gefapixant 45 mg twice daily resulted in a 24-h placebo-adjusted change of − 18.5% at Week 12 in the COUGH-1 trial and − 14.6% at Week 24 in the COUGH-2 trial [28]. In other studies, larger treatment effects have been found with smaller placebo effects [26, 27].
A large proportion of subjects in the study were on concomitant medications to treat conditions with a potential effect on cough (approximately 70% across all treatment arms). Better compliance with these medications might have contributed to the lack of separation between active treatment and placebo. In a post hoc analysis (data not shown), the relative change in 24-h cough count vs placebo was very small in the subgroup with concomitant medications and was numerically larger in favor of sivopixant in the subgroup without concomitant medications. However, contrary to this notion, the magnitude of the improvement on placebo was similar in both subgroups. Careful monitoring of the treatments for comorbidities affecting cough and the use of concomitant medications might be advisable for future studies in RCC/UCC.
The phase 2a study identified that patients with < 10 coughs/h at baseline showed highly variable values of cough count during the trial, although the patient number was small. In this phase 2b study, the study protocol required a minimum of 10 coughs/h at the beginning of the screening period (Visit 1) but not at Visit 2, which was close to randomization and regarded as baseline. The 24-h cough count data at Visit 2 were not available by the time of randomization to exclude those with a cough frequency of < 10 coughs/h. Therefore, we conducted a post hoc analysis to exclude patients with < 10 coughs/h at Visit 2. The subgroup of patients with a 24-h cough frequency of ≥ 10 coughs/h at both screening Visits 1 and 2 had greater improvements in cough with sivopixant 300 mg at Week 4 achieving a − 22.85% placebo-adjusted change in hourly cough counts over 24 h. Based on this finding, we considered that a baseline cough count of ≥ 10 coughs/h might be necessary to detect a treatment response to sivopixant. In addition, other CC trials reported that baseline cough counts were related to efficacy [29, 30]. However, our additional subgroup analyses conducted at a higher cutoff value for 24-h cough frequency at Visit 2 (< or ≥ 15, 20, 25, 35, or 40 coughs/h) showed no clear trend between the subgroups in treatment efficacy (data not shown). Therefore, we cannot conclude that sivopixant has higher efficacy in patients with a higher baseline cough count.
Changes in cough severity (VAS), LCQ total score, and PGIC were more likely to show improvements with sivopixant 300 mg vs placebo. A significantly higher proportion of patients receiving sivopixant 300 mg achieved the minimal clinically important difference of a ≥ 1.3-point improvement [25, 31] in LCQ (OR 2.21; 95% CI 1.11, 4.39; P = 0.0227) or any improvements in PGIC (OR 2.54; 95% CI 1.17, 5.51; P = 0.0182) vs placebo after 4 weeks of treatment. The difference in the VAS, although statistically significant in favor of 300 mg vs placebo, was numerically small and of questionable clinical significance.
Taste-related TEAEs are expected with P2X3 receptor antagonists [28, 32]. In the current study, sivopixant was generally well tolerated, with 33.0% of patients reporting taste-related TEAEs with sivopixant 300 mg. Taste-related TEAEs increased in a dose-dependent manner; however, most of the events were mild, with few being moderate, and only one patient in the sivopixant 300 mg group discontinued treatment due to ageusia. Specific blockade of P2X3 receptors is not expected to result in a marked impairment in taste perception [18]. In this study, taste-related TEAEs with sivopixant 300 mg were lower [28] or comparable to outcomes in other P2X3 receptor antagonist trials [26, 27, 32, 33]. Studies with treatment duration > 4 weeks are needed to further examine taste-related TEAEs associated with sivopixant.
A strength of this study is the relatively large sample size of a broad population of patients with RCC/UCC from diverse geographical backgrounds, which supports data generalizability. This may mean that more patients were naïve to antitussive therapy. However, high placebo responses suggest that some patients might have had clinical courses not typical of RCC/UCC, and a high expectation bias may have played a role. Study limitations include a high placebo response and uncertainty regarding the clinical significance of the differences seen in the VAS assessment. Furthermore, objective measurement of cough frequency may not capture other features of cough such as cough intensity, which can only be assessed subjectively.
Conclusions
Sivopixant did not demonstrate a statistically significant difference vs placebo in change from baseline in 24-h cough frequency. Sivopixant 300 mg was well tolerated and demonstrated greater reductions in hourly cough counts over 24 h than lower doses tested or placebo, although no significant differences were observed across groups. Therefore, efficacy has not been confirmed. Cough frequency at baseline (< or ≥ 10 coughs/h) and its consistency from the screening period may be factors impacting the ability to show treatment efficacy. Cough severity (VAS), LCQ total score, and PGIC showed significant improvement in responses with sivopixant 300 mg vs placebo. A well-tolerated safety profile with mild-to-moderate reversible taste disturbances was reported. This study lays the foundation for further evaluation of sivopixant 300 mg in future RCTs, with protocol planning informed by this phase 2b study, including measures to reduce the placebo effect.
Data Availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Song WJ, Chang YS, Faruqi S et al (2015) The global epidemiology of chronic cough in adults: a systematic review and meta-analysis. Eur Respir J 45:1479–1481. https://doi.org/10.1183/09031936.00218714
Morice AH, Millqvist E, Bieksiene K et al (2020) ERS guidelines on the diagnosis and treatment of chronic cough in adults and children. Eur Respir J 55:1901136. https://doi.org/10.1183/13993003.01136-2019
Mukae H, Kaneko T, Obase Y et al (2021) The Japanese respiratory society guidelines for the management of cough and sputum (digest edition). Respir Investig 59:270–290. https://doi.org/10.1016/j.resinv.2021.01.007
Mazzone SB, McGarvey L (2021) Mechanisms and rationale for targeted therapies in refractory and unexplained chronic cough. Clin Pharmacol Ther 109:619–636. https://doi.org/10.1002/cpt.2003
Gibson PG, Vertigan AE (2015) Management of chronic refractory cough. BMJ 351:h5590. https://doi.org/10.1136/bmj.h5590
Kanemitsu Y, Kurokawa R, Takeda N et al (2019) Clinical impact of gastroesophageal reflux disease in patients with subacute/chronic cough. Allergol Int 68:478–485. https://doi.org/10.1016/j.alit.2019.04.011
Birring SS, Currie CJ, Holden SE et al (2021) The financial burden of treating patients presenting with acute and chronic cough. Curr Med Res Opin 37:2175–2184. https://doi.org/10.1080/03007995.2021.1982685
Everett CF, Kastelik JA, Thompson RH, Morice AH (2007) Chronic persistent cough in the community: a questionnaire survey. Cough 3:5. https://doi.org/10.1186/1745-9974-3-5
Morice A, Dicpinigaitis P, McGarvey L, Birring SS (2021) Chronic cough: new insights and future prospects. Eur Respir Rev 30:210127. https://doi.org/10.1183/16000617.0127-2021
Ryan NM, Vertigan AE, Birring SS (2018) An update and systematic review on drug therapies for the treatment of refractory chronic cough. Expert Opin Pharmacother 19:687–711. https://doi.org/10.1080/14656566.2018.1462795
Abdulqawi R, Dockry R, Holt K et al (2015) P2X3 receptor antagonist (AF-219) in refractory chronic cough: a randomised, double-blind, placebo-controlled phase 2 study. Lancet 385:1198–1205. https://doi.org/10.1016/S0140-6736(14)61255-1
Morice AH, Kitt MM, Ford AP et al (2019) The effect of gefapixant, a P2X3 antagonist, on cough reflex sensitivity: a randomised placebo-controlled study. Eur Respir J 54:1900439. https://doi.org/10.1183/13993003.00439-2019
Morice A, Smith JA, McGarvey L et al (2021) Eliapixant (BAY 1817080), a P2X3 receptor antagonist, in refractory chronic cough: a randomised, placebo-controlled, crossover phase 2a study. Eur Respir J 58:2004240. https://doi.org/10.1183/13993003.04240-2020
Smith JA, Kitt MM, Morice AH et al (2020) Gefapixant, a P2X3 receptor antagonist, for the treatment of refractory or unexplained chronic cough: a randomised, double-blind, controlled, parallel-group, phase 2b trial. Lancet Respir Med 8:775–785. https://doi.org/10.1016/S2213-2600(19)30471-0
Smith JA, Kitt MM, Butera P et al (2020) Gefapixant in two randomised dose-escalation studies in chronic cough. Eur Respir J 55:1901615. https://doi.org/10.1183/13993003.01615-2019
Wang T, Glendinning J, Grushka M, Hummel T, Mansfield K (2017) From the cover: drug-induced taste disorders in clinical practice and preclinical safety evaluation. Toxicol Sci 156:315–324. https://doi.org/10.1093/toxsci/kfw263
Kai H, Horiguchi T, Kameyma T et al (2021) Discovery of clinical candidate Sivopixant (S-600918): lead optimization of dioxotriazine derivatives as selective P2X3 receptor antagonists. Bioorg Med Chem Lett 52:128384. https://doi.org/10.1016/j.bmcl.2021.128384
Niimi A, Saito J, Kamei T et al (2022) Randomised trial of the P2X3 receptor antagonist sivopixant for refractory chronic cough. Eur Respir J 59:2100725. https://doi.org/10.1183/13993003.00725-2021
Smith JA, Holt K, Dockry R et al (2021) Performance of a digital signal processing algorithm for the accurate quantification of cough frequency. Eur Respir J 58:2004271. https://doi.org/10.1183/13993003.04271-2020
Martin Nguyen A, Bacci ED, Vernon M et al (2021) Validation of a visual analog scale for assessing cough severity in patients with chronic cough. Ther Adv Respir Dis 15:17534666211049744. https://doi.org/10.1177/17534666211049743
Morice AH, Fontana GA, Belvisi MG et al (2007) ERS guidelines on the assessment of cough. Eur Respir J 29:1256–1276. https://doi.org/10.1183/09031936.00101006
Birring SS, Prudon B, Carr AJ, Singh SJ, Morgan MD, Pavord ID (2003) Development of a symptom specific health status measure for patients with chronic cough: Leicester Cough Questionnaire (LCQ). Thorax 58:339–343. https://doi.org/10.1136/thorax.58.4.339
Martin Nguyen A, Bacci E, Dicpinigaitis P, Vernon M (2020) Quantitative measurement properties and score interpretation of the cough severity diary in patients with chronic cough. Ther Adv Respir Dis 14:1753466620915155. https://doi.org/10.1177/1753466620915155
Busner J, Targum SD (2007) The clinical global impressions scale: applying a research tool in clinical practice. Psychiatry (Edgmont) 4:28–37
Raj AA, Pavord DI, Birring SS (2009) Clinical cough IV: what is the minimal important difference for the Leicester Cough Questionnaire? In: Chung KF, Widdicombe J (eds) Pharmacology and therapeutics of cough. Handbook of experimental pharmacology, vol 187. Springer, Berlin, Heidelberg, pp 311–320
McGarvey L, Morice AH, Smith J et al (2021) Late breaking abstract—efficacy and safety of eliapixant in refractory chronic cough: results of the PAGANINI 12-week, randomized, placebo-controlled Phase 2b study. Eur Respir J 58:AP562. https://doi.org/10.1183/13993003.congress-2021.PA562
Bellus Health (2021) Phase 2b SOOTHE trial in refractory chronic cough topline results and P2X3 pipeline update. https://ir.bellushealth.com/static-files/db690b72-3721-4e78-b749-1708c49bfb1a. Accessed 27 Jan 2022
McGarvey LP, Birring SS, Morice AH et al (2022) Efficacy and safety of gefapixant, a P2X(3) receptor antagonist, in refractory chronic cough and unexplained chronic cough (COUGH-1 and COUGH-2): results from two double-blind, randomised, parallel-group, placebo-controlled, phase 3 trials. Lancet 399:909–923. https://doi.org/10.1016/S0140-6736(21)02348-5
Birring SS, Smith JA, Morice AH et al (2021) Improvements in cough severity and cough-related quality of life in a phase 2 trial (RELIEF) with the P2X3 antagonist BLU-5937 in refractory chronic cough (RCC). Eur Respir J 58:OA1199. https://doi.org/10.1183/13993003.congress-2021.OA1199
Smith J, Morice AH, Birring SS et al (2021) Improvements in cough frequency over 24 hours with BLU-5937, a selective P2X3 antagonist, in patient subgroups defined by baseline awake cough frequencies. Am J Respir Crit Care Med 203:A1019. https://doi.org/10.1164/ajrccm-conference.2021.203.1_MeetingAbstracts.A1019
Rebelo P, Oliveira A, Paixão C, Valente C, Andrade L, Marques A (2020) Minimal clinically important differences for patient-reported outcome measures of cough and sputum in patients with COPD. Int J Chron Obstruct Pulmon Dis 15:201–212. https://doi.org/10.2147/COPD.S219480
Taylor P (2021) Bayer’s eliapixant hits the right notes in PAGANINI cough study. https://pharmaphorum.com/news/bayers-eliapixant-hits-the-right-notes-in-paganini-cough-study/. Accessed 16 May 2022
Birring SS, Dicpinigaitis P, Morice A et al (2021) P60 Patient-reported improvements with gefapixant, a P2X3-receptor antagonist, over 52 weeks in two phase 3 clinical trials for refractory or unexplained chronic cough. Thorax 76:A99. https://doi.org/10.1136/thorax-2021-BTSabstracts.170
Acknowledgements
This study was sponsored by Shionogi & Co., Ltd. The authors thank the patients and investigators who participated in the clinical study. The authors wish to thank Ms. Haruna Hayashi of Shionogi & Co., Ltd. for collecting the feedback from all the co-authors and helping with the administrative aspects of the submission. Medical writing support was provided by Khi Khi Choo, PhD, of Cactus Life Sciences (part of Cactus Communications) and Nicola Welch, PhD, CMPP, for Cactus Life Sciences (part of Cactus Communications) and funded by Shionogi & Co., Ltd.
Funding
This study was sponsored by Shionogi & Co., Ltd. Medical writing support was funded by Shionogi & Co., Ltd.
Author information
Authors and Affiliations
Contributions
LMG, JAS, AMo, SSB, KFC, PVD, AN, MSB, MS, YM, SM, MM, HI, AMa, JG substantially contributed to conception, design, or planning of the study. LMG, SSB, MS, AMo substantially contributed to acquisition of the data. MM substantially contributed to analysis of the data. All authors substantially contributed to interpretation of the results and critically reviewing or revising the manuscript for important intellectual content. All authors reviewed the final version of the manuscript and are in agreement with its content and submission; have access to all relevant study data and related analyses and vouch for the completeness/accuracy of the presented data; and agree to be accountable for all aspects of the work and ensure that any questions related to the accuracy or integrity of any part of the work will be appropriately investigated and resolved.
Corresponding author
Ethics declarations
Competing Interests
LMG has received grants or contracts and consulting fees from Shionogi Inc., Bayer, Merck, Bellus Health, and Chiesi; consulting fees from AstraZeneca, Nocion, Trevi Therapeutics, Reckitt Benckiser Health Limited, NeRRe Therapeutics, and Bionorica; payment or honoraria from Merck, Chiesi, Bellus, Bionorica, GSK, and Shionogi Inc. and participated on a Data Safety Monitoring Board or the Advisory Board for Applied Clinical Intelligence. JAS has served as a consultant and helped in the setup of clinical studies for Shionogi; received grants or contracts from Wellcome Trust investigator award and NIHR Manchester Biomedical Research Centre; her hospital has received royalties from Vitalograph Ltd.; received consulting fee from Bellus Health, Axalbion, Merck, Bayer, Algernon, Nocion, Chiesi, Boehringer Ingelheim, and AstraZeneca; received honoraria from Merck and Boehringer Ingelheim; has a patent issued for cough monitoring; and received equipment supply from Vitalograph Ltd. AMo has received funding from Shionogi; received payment or honoraria from Merck, Bayer, and NeRRe; participated on a Data Safety Monitoring Board or an Advisory Board for Merck, Bayer, NeRRe, Shionogi, and Bellus; and served as the task force chair for the European Respiratory Society. SSB has received personal fees from Shionogi Inc., Merck, Bellus, Bayer, and Nocion. KFC has speaking engagements for Novartis and AstraZeneca; has participated on Advisory Boards for Roche, Merck, Reckitt Benckiser, and Shionogi & Co., Ltd., on asthma, COPD, and chronic cough; serves on Data Safety Monitoring Board for Nocion; and has received grants including MRC grant on Precision Medicine for severe asthma, an EPSRC grant on air pollution and asthma, and a GSK grant on mepolizumab and eosinophils in asthma. PVD has served as a consultant to Bayer, Bellus, Chiesi, Merck, and Shionogi Inc. and is the editor-in-chief of Lung. MSB has served as a consultant for Merck (2020) and Shionogi Inc. (2020) and received research funding from Merck. MS has served on the Medical Advisory Board and as a principal investigator for Bayer, Bellus, Merck, NeRRe, and Shionogi Inc.; serves on the Medical Advisory Board and Data Safety Monitoring Board for Nocion; and is a consultant for Soundable Health. YM is a former employee of Shionogi Inc. SM, MM, and HI are employees of Shionogi & Co. Ltd. JCG is an employee of Shionogi B.V. AMa is a medical consultant for Shionogi B.V. AN has no disclosures.
Ethical Approval
The institutional review board at each participating site approved the protocol and other relevant documents. The study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Consent to Participate
Written informed consent was obtained from all participants.
Consent to Publish
All patients signed an informed consent for publication of data for the present study.
Role of the Sponsors
The sponsor was involved in designing the study; collection, analysis, and interpretation of data; and writing the manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
McGarvey, L., Smith, J.A., Morice, A. et al. A Randomized, Double-Blind, Placebo-Controlled, Parallel-Group Phase 2b Trial of P2X3 Receptor Antagonist Sivopixant for Refractory or Unexplained Chronic Cough. Lung 201, 25–35 (2023). https://doi.org/10.1007/s00408-022-00592-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00408-022-00592-5